Abstract
Background:
Lysergic acid diethylamide (LSD) is an ergot alkaloid derivative with psychedelic properties that has been implicated in the management of persistent pain. Clinical studies in the 1960s and 1970s have demonstrated profound analgesic effects of full doses of LSD in terminally ill patients, but this line of research evaporated after LSD was scheduled worldwide.
Aim:
The present clinical study is the first to revisit the potential of LSD as an analgesic, and at dose levels which are not expected to produce profound mind-altering effects.
Methods:
Twenty-four healthy volunteers received single doses of 5, 10 and 20 µg LSD as well as placebo on separate occasions. A Cold Pressor Test was administered at 1.5 and 5 h after treatment administration to assess pain tolerance to experimentally evoked pain. Ratings of dissociation and psychiatric symptoms as well as assessments of vital signs were included to monitor mental status as well as safety during treatments.
Results:
LSD 20 µg significantly increased the time that participants were able to tolerate exposure to cold (3°C) water and decreased their subjective levels of experienced pain and unpleasantness. LSD elevated mean blood pressure within the normal range and slightly increased ratings of dissociation, anxiety and somatization.
Conclusion:
The present study provides evidence of a protracted analgesic effect of LSD at a dose that is low enough to avoid a psychedelic experience. The present data warrant further research into the analgesic effects of low doses of LSD in patient populations.
Keywords: LSD, CPT, pain
Introduction
Lysergic acid diethylamide (LSD) is a psychedelic compound that was synthesized by the Swiss chemist Albert Hofmann in 1938. He was also the first to describe the psychoactive properties of the compound (Hofmann, 1979) such as psychosensory changes, illusionary changes of perceived objects, synesthesia, enhanced mental imagery, hyperamnesia, mysticism and ego dissolution (Grof, 1975; Katz et al., 1968; Liechti, 2017; Liechti et al., 2017; Passie et al., 2008; Schmidt et al., 2018). The altered state of consciousness under LSD is mainly mediated by activation of the 5-HT2A receptors (Kraehenmann et al., 2017; Nichols, 2016; Preller et al., 2017). From a physiological perspective, LSD is known to be non-toxic and medically safe when taken at dosages below 200 µg (Nichols and Grob, 2018), but traumatic mental experiences have been reported (Passie et al., 2008).
LSD may also possess therapeutic properties (Liechti, 2017; Vollenweider and Kometer, 2010) and has been implicated in the management of pain (Whelan and Johnson, 2018). Serotonergic agents, such as ergot alkaloids, have traditionally been used for the acute and preventive treatment of cluster headache and other primary headaches (Lambru and Matharu, 2011). LSD is yet another ergot alkaloid derivative, but most data supporting the use of LSD as analgesic are based on reports of self-medication. Recent surveys (Andersson et al., 2017; Hutten et al., 2019; Schindler et al., 2015) among pain patients suggest that the use of psychedelics such as LSD can be effective for both prophylactic and acute treatment of cluster headache and migraines, even when used infrequently or at non-hallucinogenic doses. Moreover, cluster headache patients who had used LSD to treat their condition reported cluster period termination and extension of the remission period (Sewell et al., 2006).
Controlled studies on the efficacy of LSD as an analgesic are virtually absent or dated. A comparative study between LSD (100 µg), meperidine, and dihydromorphinone was conducted in terminally ill patients (N=50) who complained of severe intolerable pain (Kast and Collins, 1964). LSD showed more protracted and more effective action than the other drugs. LSD strongly reduced subjective pain ratings and increased the number of pain-free periods during the day. Apart from the profound analgesic effects, patients also experienced a psychedelic state, which to some was so disturbing that they refused a second administration of LSD. The same investigator later also reported that the same dose of LSD had significant analgesic action in an even larger case series of terminally ill (N=128) and reduced pain intensity for about 3 weeks (Kast, 1967). Likewise, administration of LSD-assisted psychotherapy to a case series of cancer patients (N=53) with pain, anxiety, and depression produced significant improvements in pain severity, pre-occupation with pain and physical suffering, anxiety, and depression (Grof et al., 1973; Pahnke et al., 1969). Another case series on treatment of phantom limb pain (N=9) with sub-hallucinogenic doses of LSD reported improvement in pain in five patients and decreased use of analgesics (Fanciullacci et al., 1977). Overall, these studies suggest a role for LSD in pain management but controlled research is warranted to provide further evidence.
From a medical point of view, controlled research on the efficacy of LSD in pain management should focus on non-hallucinogenic, low doses of LSD, which are more manageable and thus preferable over treatment with high doses of LSD that produce full-blown psychedelic effects. The present study was therefore designed to assess subjective pain perception in healthy volunteers who received three non-hallucinogenic “micro”-doses of LSD as part of a placebo-controlled trial. We measured their subjective response to pain evoked by a Cold Pressor Test (CPT) as well as their objective pain tolerance. Based on the preliminary evidence described above, it was expected that LSD would reduce pain perception as compared with placebo treatment. In addition, ratings of dissociation and other psychiatric symptoms as well as assessments of vital signs were included to monitor mental status as well as safety during treatments.
Methods
Design and treatments
Twenty-four healthy participants (12 male, 12 female) participated in a randomized, double-blind, placebo-controlled, within-subject study in which they received single oral doses of 5, 10, and 20 µg LSD (hydrate) and placebo on four separate test days. A minimum washout of 5 days proceeded in between to avoid carry-over effects. Treatment orders were randomly assigned to participants according to a balanced block design. LSD was formulated as a solution of 25 µg LSD base in 1 mL 96% ethanol according to GMP and administered orally (Holze et al., 2019). LSD doses (0.2, 0.4, and 0.8 mL for 5, 10, and 20 µg LSD, respectively) were supplemented with an ethanol solution up to a total volume of 1 mL and administered with a syringe under the tongue. Placebo consisted of a 1 mL ethanol solution only. Treatments were administered at 10 AM.
Participants
The mean (SD) age of participants was 22.7 (2.9) years. All participants had previous experience with psychedelics and their mean (SD) frequency of use in the year prior to the study was 2.8 (4.2) times. Reported use of psychedelics included psilocybin (N=19), LSD (N=11), DMT (N=1) and 2C-B (N=1). Other drugs that were reported included cannabis (N=23), ecstasy (N=14), amphetamines (N=7), cocaine (N=10), salvia (N=1), ketamine (N=1), and alprazolam (N=1). All participants reported the use of alcohol.
The study was conducted according to the code of ethics on human experimentation established by the declaration of Helsinki (1964) and amended in Fortaleza (Brazil, October 2013) and in accordance with the Medical Research Involving Human Subjects Act (WMO), and was approved by the Academic Hospital and University’s Medical Ethics committee. All participants were fully informed about all procedures, possible adverse reactions, legal rights and responsibilities, expected benefits, and their right for voluntary termination without consequences. The study was registered in the Netherlands Trial Register (Trial NL6907 (NTR7102)).
Procedures
Participants were recruited through advertisements at Maastricht University, via social media, and by word of mouth. Candidate participants were screened and examined by a study physician, who checked for general health, conducted a resting ECG, and took blood and urine samples in which hematology, clinical chemistry, urine, and virology analyses were conducted. Inclusion criteria consisted of written informed consent, age 18–40 years, previous use of a psychedelic drug but not within the past 3 months, proficient knowledge of the English language, good physical and mental health, free from psychotropic medication, body mass index between 18 and 28 kg/m2. Exclusion criteria included history of drug abuse or addiction according to DSM-5 criteria; history of psychiatric and neurological disorders, adverse response to psychedelic drugs (anxiety or panic attacks), cardiovascular abnormalities, hypertension, psychotic disorder in first-degree relatives, tobacco smoking of more than 20 cigarettes a day, excessive alcohol use (i.e. > 20 alcohol consumptions per week), pregnancy or lactation.
Prior to the first treatment day, participants were familiarized with tests and study procedures. Participants were instructed to refrain from drug use (⩾7 days) and alcohol use (⩾24 h) prior to their treatment day. They were also instructed to not consume caffeinated or alcoholic beverages on treatment days and to arrive well rested at the test facility. On arrival, participants were screened for the presence of drugs (THC, opiates, cocaine, amphetamine) in urine, and for alcohol in breath. An additional pregnancy test was given if participants were female. If all tests were found to be negative, participants were allowed to proceed.
At 1.5 and 5 h post treatment, participants conducted a CPT. The Brief Symptom Inventory (BSI) and the Clinician Administered Dissociation State Scale (CADSS) were administered prior to treatment administration (baseline) and at the end of a test day, i.e. at 6 h post dosing. Vital signs were recorded at baseline, every 30 min during the first 3 h after dosing, and at every hour thereafter. Blood samples were collected 1.5 and 6 h after drug administration. Participants resided in a secluded room that contained a bed, table and chairs. Standardized lunches were provided around 12 PM. The present study also included assessment of mood, cognition, empathy, and creativity that will be reported elsewhere. A permit for obtaining, storing, and administering LSD was obtained from the Dutch Drug Enforcement Administration. Participants were financially compensated (€300) for their participation in the study.
The Cold Pressor Test
The CPT was used to induce a painful sensation according to previously validated procedures (Smeets et al., 2012). A water tank was filled with water that was cooled to 3°C. Participants were informed that the procedure could be painful and that they could stop the task at any point without consequences. The instructions before immersion were as follows: “The aim of the task is to submerge your right hand in this cold water tank for as long as possible until you cannot take it anymore. When you cannot take it any longer, you are allowed to remove your hand from the water. Try, however, to hold on as long as possible.” The immersion duration was set to 3 min. Participants were not aware of this time limit. If the 3 min maximum was achieved, the experimenter would signal the participant to remove the hand from the water. Dependent measures of the CPT included pain tolerance (seconds), i.e. the number of seconds until withdrawal of the hand from the water tank, and subjective ratings of painfulness, unpleasantness and stress as assessed on 10 cm visual analog scales. Water temperature at onset and completion of the CPT were assessed as control measure.
Clinician Administered Dissociative States Scale
The CADSS comprises 19 subjective items, ranging from 0 “not at all” to 4 “extremely.” It is divided into three components: (1) depersonalization, (2) derealization, and (3) amnesia. Summed together, these subscales form a total dissociative score. The CADSS is specifically designed to be a standardized measure of present-state dissociative symptomatology (Bremner et al., 1998). Component scores above 15 (depersonalization), 36 (derealization), and 6 (amnesia) are considered severe. Component scores below 5 (depersonalization), 12 (derealization), and 2 (amnesia) indicate that symptoms are absent or mild. The scale has recently been shown to be sensitive to dissociative effects of psychedelics and drugs of abuse (Derntl et al., 2019; van Heugten-Van der Kloet et al., 2015).
Brief Symptom Inventory
The BSI is a shortened version of the widely used Symptom Check List 90. The BSI-18 contains only the three six-item scales somatization, anxiety, and depression (Spitzer et al., 2008). The scale was recently shown to be sensitive to the effects of psychedelics (Uthaug et al., 2019).
Vital signs
Heart rate (bpm) and blood pressure (mmHg) were repeatedly assessed using an Omron M6 (HEM-7321-E, Omron Healthcare Europe Bv) device.
Blood concentrations of LSD
Blood samples were centrifuged and plasma was frozen at −20°C until analysis for pharmacokinetic assessments. LSD plasma levels were analyzed by ultra-high-performance liquid chromatography tandem mass spectrometry (UHPLC–MS/MS) as described previously (Holze et al., 2019). PK Samples with a LSD concentration below 5 pg/mL were reanalyzed by a different extraction procedure. In brief, aliquots of 150 µL of plasma were extracted with 450 µL methanol. The samples were rigorously mixed and subsequently centrifuged. The supernatant was evaporated under a constant stream of nitrogen and re-suspended in 200 µL of mobile phase A and B (10:90 v/v). An LLOQ of 2.5 pg/mL was reached by this extraction.
Statistics
Analyses were carried out by means of the SPSS 25 program series to investigate whether the effects of LSD doses differed from those of placebo. CPT parameters and vital signs were analyzed using a GLM univariate model that included the fixed factors Treatment (4 levels), Time (2 or 10 levels) after treatment and the interaction Treatment × Time after treatment, as well as the random factor Participant (N=24). Baseline adjusted parameters of the BSI and CADSS were analyzed in the same manner but without a factor Time. Mean contrast (LSD dose versus placebo) tests were conducted for measuring the significance of individual dose effects, relative to placebo. Canonical correlation analyses were conducted to understand the association between a set of measures of pain (i.e. pain tolerance, painfulness, unpleasantness) and a set of measures of blood pressure (systolic and diastolic blood pressure) or dissociation (depersonalization and derealization). The alpha criterion for significance was set at p<0.05.
Results
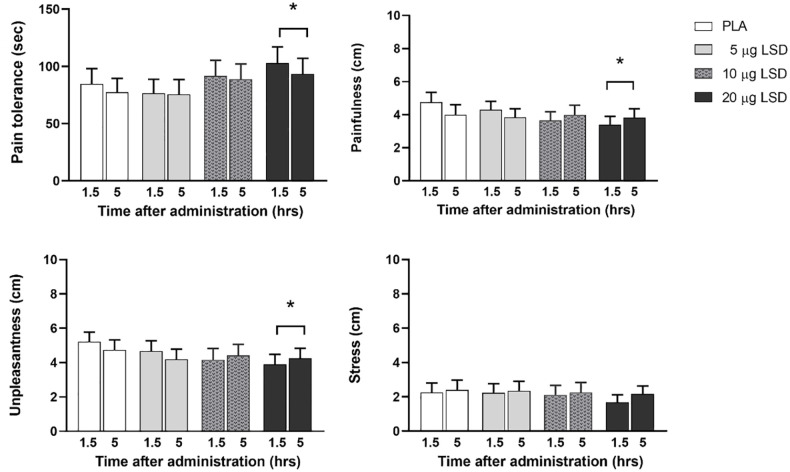
Mean (SE) pain tolerance and subjective ratings of painfulness, unpleasantness and stress during the CPT as a function of Treatment and Time after treatment administration are shown in Figure 1. ANOVA revealed significant main effects of Treatment on pain tolerance (F3,157=5.3, p=0.002, partial η2=0.09), rating of unpleasantness (F3,157=2.6, p=0.05, partial η2=0.05) and a near significant main effect of Treatment on rating of painfulness (F3,157=2.4, p=0.064, partial η2=0.044). The main factors Time after administration and the interaction Treatment × Time after administration did not reach significance for these measures. Separate LSD–placebo contrasts revealed that LSD 20 µg increased pain tolerance (p=0.006) and decreased painfulness (p=0.012) and unpleasantness (p=0.008). A decrement in unpleasantness caused by LSD 10 µg approached significance (p=0.051). Ratings of stress were not affected by Treatment, Time after treatment or their interaction. Mean (SD) water temperature at onset and end of the CPT was 2.9°C (.19) and 3.6°C (.47) and did not significantly differ between treatments and times of administration.
Figure 1.
Mean (SE) pain tolerance and subjective ratings of painfulness, unpleasantness, and stress during the Cold Pressor Test (CPT) as a function of treatment condition and time after treatment administration. *p<0.05, relative to placebo (PLA).
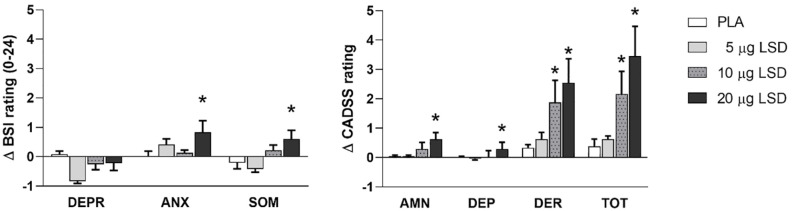
Mean (SE) BSI and CADSS ratings (changes from baseline) in every treatment condition are shown in Figure 2. Mean symptom severity ranged from not present to mild across all treatment conditions. Main Treatment effects were observed for the BSI items somatization (F3,67=3.5, p=0.02, partial η2=0.13) and anxiety (F3,67=3.1, p=0.03, partial η2=0.12) but not for depression. LSD–placebo contrasts revealed that LSD 20 µg slightly increased symptoms of somatization (p=0.006) as well as anxiety (p=0.006).
Figure 2.
The left panel shows mean (SE) change from baseline in subjective ratings of symptoms of depression (DEPR), anxiety (ANX) and somatization (SOM) in each treatment condition as assessed with the Brief Symptom Inventory (BSI). The right panel shows mean (SE) changes from baseline in subjective ratings of amnesia (AMN), depersonalization (DEP), derealization (DER) and total dissociation (TOT) as assessed with the Clinician Administered Dissociative State Scale (CADSS) in every treatment condition. BSI rating scales range from 0 to 24, whereas CADSS ranges differ per subscale: i.e. AMN (0–8), DEP (0–20), DER (0–48) and TOT (0–72). *p<0.05, relative to placebo (PLA).
Main Treatment effects were also observed for the CADSS items amnesia (F3,69=4.6, p=0.005, partial η2=0.16), depersonalization (F3,69=3.5, p<0.001, partial η2=0.22), derealization (F3,69=4.6, p=0.005, partial η2=0.17), and the total dissociation score (F3,69=6.1, p=0.001, partial η2=0.21). Separate contrasts indicated that LSD 10 µg slightly increased symptoms of derealization (p=0.027) as well as the total dissociation score (p=0.032). LSD 20 µg slightly increased symptoms of amnesia (p=0.002), depersonalization (p=0.001), derealization (p=0.002), and the total dissociation score (p<0.001), relative to placebo. Canonical correlation analysis indicated a significant association (F6,364=2.18, p=0.04, canonical r=0.25) between measures of dissociation and pain that explained about 6% of the total variance. The association suggested that increments in symptoms of dissociation are associated with increased pain tolerance and a decrease in subjective pain perception.
Mean (SE) heart rate, systolic and diastolic blood pressure as a function of treatment and time after treatment administration are shown in Figure 3. Systolic blood pressure was significantly affected by Treatment (F3,792=24.8, p<0.001, partial η2=0.09), Time after treatment administration (F8,792=2.0, p<0.04, partial η2=0.02), but not their interaction. Diastolic blood pressure was affected by Treatment (F3,792=6.5, p<0.001, partial η2=0.024), but not by Time after treatment administration or their interaction. Separate contrasts revealed that LSD 10 µg increased diastolic blood pressure (p<0.001), whereas LSD 20 µg increased systolic (p<0.001) and diastolic blood pressure (p=0.013). Heartrate was not affected by Treatment, Time after administration or their interaction. Canonical correlation analysis indicated a significant association (F6,360=5.27, p=<0.001, canonical r=0.37) between measures of blood pressure and pain that explained about 14% of the total variance. The association suggested that increments in blood pressure are associated with increased pain tolerance and a decrease in subjective pain perception.
Figure 3.
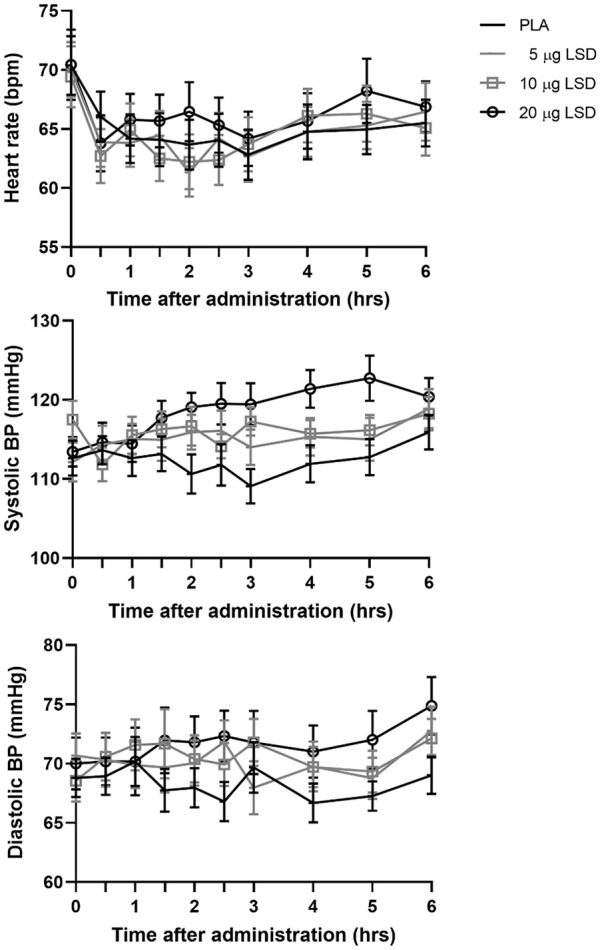
Mean (SE) heart rate, systolic and diastolic blood pressure (BP) after each LSD dose and placebo (PLA) and as a function of time after treatment administration.
Plasma samples could be collected in 13, 18, and 15 subjects after the 5, 10, and 20 µg dose, respectively. Pharmacokinetic analyses revealed mean (SD) plasma LSD concentrations of 150 (48), 278 (87), and 482 (150) pg/mL at 1.5 h after LSD 5, 10, and 20 µg respectively. At 6 h post treatment with LSD 5, 10, and 20 µg, plasma LSD concentrations were 54 (18), 108 (45), and 224 (102) pg/mL, respectively.
Discussion
Controlled studies on the therapeutic potential of LSD in pain management are scarce and date back to the 1960s and 1970s, before LSD was placed into the most restrictive drug control schedule in many countries worldwide. Yet, despite the lack of clinical research over the last 50 years, the practice of self-medication with LSD to treat persistent pain continued (Hutten et al., 2019; Schindler et al., 2015). The present controlled clinical study is the first to revisit the potential of LSD as an analgesic in a very long time, and at dose levels that are not expected to produce relevant mind-altering effects. The latter is of importance, as this would increase the acceptability of a psychedelic drug in the management of pain.
The current data consistently indicated that LSD 20 µg significantly reduced pain perception as compared with placebo, whereas lower doses of LSD did not. LSD 20 µg significantly increased pain tolerance (i.e. immersion time) by about 20%, while decreasing the subjective levels of experienced painfulness and unpleasantness. Changes in pain tolerance and subjective pain perception induced by LSD 20 µg were of medium to large effect size and comparable in magnitude to those observed with the CPT after administration of opioids, such as oxycodone 20 mg (Cooper et al., 2012) and morphine 10–20 mg (Ravn et al., 2013) to healthy volunteers. The findings were also statistically robust. All differences in pain perception between LSD 20 µg and placebo would also survive a conservative Bonferroni tests to correct for multiple comparisons (i.e. significance levels p<0.016), if applied. The reduction in subjective pain perception is remarkable, because it was measurable despite a prolonged exposure time to the pain stimulus in LSD 20 µg treatment condition. These phenomena, however, seem interrelated, as a reduction in subjective pain experience can explain why participants were able to tolerate pain for a longer period of time. The analgesic effects of LSD 20 µg were equally strong at 1.5 and 5 h after administration, as indicated by the lack of a Treatment × Time after treatment interaction. This speaks to a sustained efficacy profile for LSD which is fully in line with the well-established notion that pharmacological effects of LSD can be assessed up to 12 h after administration, even after low doses (Passie et al., 2008). The analgesic effects of LSD 20 µg therefore may outlast the 5 h time window that was applied in the current study.
LSD also induced some psychological and physical symptoms as assessed by the BSI and CADSS. LSD 10 µg increased ratings of derealization and the total dissociation score. LSD 20 µg increased symptoms of anxiety, somatization, amnesia, depersonalization, derealization, and dissociation. These subjective data clearly indicate that even these low doses of LSD produced pharmacological effects that were noticeable to the participants. However, the magnitude of these effects was small. Average ratings of all CADSS and BSI components indicated that symptom severity ranged between not present and mild. Increments in level of dissociation that were observed in the present study were also much lower than those observed after regular doses of other compounds that have been implicated in pain management such as ketamine and cannabis. CADSS ratings of dissociation after single doses of cannabis and ketamine (van Heugten-Van der Kloet et al., 2015) were about 3 and 10 times higher than the level of dissociation produced LSD 20 µg in the present study. Recent studies on the behavioral effects of low doses of LSD also reported that cognitive function, mood, perception, and state of consciousness were not or only mildly affected by doses up to 26 µg LSD tartrate (i.e. equal to LSD 21 µg hydrate) (Bershad et al., 2019; Yanakieva et al., 2019). Overall, these data suggest that the level of cognitive interference that is produced by LSD 20 µg is very mild and would not be expected to interfere with normal day-to-day operations.
LSD also increased mean blood pressure but did not affect heart rate. Increments in systolic and diastolic blood pressure were most prominent after LSD 20 µg. Mean changes in blood pressure were less than 10 mmHg at any time point, as compared with placebo. Overall, however, levels of systolic and diastolic blood pressure throughout all treatment conditions were well within the normal range, suggesting that the impact of LSD on blood pressure is of limited clinical relevance. The present findings are in line with another recent study (Bershad et al., 2019) that also reported that low doses of 13 and 26 µg LSD tartrate (corresponding to 11 and 21 µg LSD hydrate) produced small increments in blood pressure while not affecting heart rate and temperature. Elevations in blood pressure after LSD are well described and have been attributed to the vasoconstrictive properties of LSD (Passie et al., 2008). Previous studies have shown that full, psychedelic doses of LSD (i.e. 100 and 200 µg) produce more pronounced increments in blood pressure (Dolder et al., 2017; Schmid et al., 2015), but the current findings reveal the threshold dose at which LSD produces these effects. Overall, the physiological changes observed after low doses of LSD were mild and safe.
At present, it is unclear how LSD may influence pain perception. Explanatory models have focused on pharmacological changes in the processing of nociceptive information or on psychological changes in coping with pain. The latter explanation suggests that LSD does not alter nociception and that reductions in subjective pain perception arise from attentional reorienting from pain sensation to the psychedelic experience of LSD (Kast and Collins, 1964). Alternatively, LSD may be analgesic by promoting self-transcendence, in much the same way that meditation-induced self-transcendence is (Garland and Fredrickson, 2019; Garland et al., 2019); in essence, no self, no pain. Such analgesic mechanism might be most pronounced in moderate to high-dose LSD sessions, or potentially, in treatments that combine mindfulness meditation interventions with microdoses of LSD. In any of these scenarios one would expect the magnitude of pain relief to be intrinsically related to the intensity of the psychedelic experience. There was some evidence to support this view in the present study, as a significant canonical association was found between reduced levels of pain perception and increasing levels of dissociation across all treatments. This correlation, however, was relatively weak and explained only 6% of the variance, which is not surprising given that the levels of dissociation produced by LSD were almost negligible. But, these data do indicate that attentional reorientation or self-transcendence may contribute to some degree to the analgesic effect of LSD, even with low doses. The pharmacological view stresses the role of serotonin and 5HT2A receptors in peripheral and centrally mediated pain processes (Whelan and Johnson, 2018). In vivo electrophysiology studies in rats suggest that LSD has partial agonist actions at 5-HT2A receptors and full antagonistic action at 5-HT1A in the dorsal raphe, a structure known to be involved in actions of descending pain inhibitory processes (De Gregorio et al., 2016). However, the relationship between 5-HT and additional neurotransmitter systems implicated in nociception and how their interconnectivity may be affected by LSD needs further research (Whelan and Johnson, 2018).
An additional or alternative explanation for the analgesic effects of LSD could be hypertension-associated hypoalgesia. Previous studies in animals and humans have shown that blood pressure correlates positively with pain tolerance and negatively with the perception of the intensity of the painful stimulus in acute pain models such as the CPT (Sacco et al., 2013), even when blood pressure fluctuations are within the normal range (Ghione, 1996). Canonical correlations between measures of blood pressure and measures of pain confirmed these relationships in the present study and explained about 14% of the variance in pain levels across all treatment conditions. How alterations in blood pressure and perception of pain are related is poorly understood, but it has been suggested that pain activates the sympathetic nervous system with resulting increase in blood pressure, which, in turn, causes increased stimulation of baroreceptors that consecutively activate the inhibitory descending pathways that originate from the dorsal raphe nucleus and project to the spinal cord to release serotonin and reduce the perception of pain (Bruehl et al., 2010; Sacco et al., 2013). The current data suggest that LSD might enhance this mechanism of pain alleviation either by increasing blood pressure or by stimulation of 5HT1A and 5HT2 receptors in the inhibitory descending pathways (De Gregorio et al., 2016).
The present study provides compelling evidence of a moderate and protracted analgesic effect of LSD at a dose that is low enough to avoid a psychedelic experience. The study revealed the minimal dose at which analgesic activity of LSD is effective. Yet, an extended dose-finding study is needed to determine the dose at which analgesic effects of LSD are optimal, i.e. when efficacy is maximal and mental interference is minimal. Such a study could potentially explore the trade-off between increments in treatment efficacy and psychedelic symptoms in a low to medium dose range (i.e. 20–50 µg LSD). Further research is also needed to replicate the current findings in patient populations who suffer from persistent pain, and comorbid neuropsychiatric ailments, and to determine the potential for tolerance development after repeated dosing. The present data suggest that low doses of LSD might constitute a novel pharmacological therapy that can be efficacious in patients and is devoid of problematic sequelae that are associated with current mainstay drugs, such as opioids (Kertesz and Gordon, 2019).
In conclusion, the present study provides evidence for analgesic activity of LSD in healthy volunteers at doses that are low enough to avoid physiological or mental challenges. The present data warrant further research into the analgesic effects of low doses of LSD in patient populations.
Footnotes
Author contributions: JR, KK, PD, AF and EF designed the research. NH and NM were responsible for data collection. NH, NM, FH, ML, EL, KK and JR were involved in data analyses. JR wrote the paper with contributions from all co-authors.
Declaration of conflicting interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: A financial contribution was received from the Beckley Foundation.
ORCID iDs: Johannes G Ramaekers  https://orcid.org/0000-0003-4553-376X
https://orcid.org/0000-0003-4553-376X
Nadia Hutten  https://orcid.org/0000-0003-0033-8119
https://orcid.org/0000-0003-0033-8119
Natasha L Mason  https://orcid.org/0000-0001-7115-0389
https://orcid.org/0000-0001-7115-0389
Matthias E Liechti  https://orcid.org/0000-0002-1765-9659
https://orcid.org/0000-0002-1765-9659
Kim PC Kuypers  https://orcid.org/0000-0001-7634-3809
https://orcid.org/0000-0001-7634-3809
References
- Andersson M, Persson M, Kjellgren A. (2017) Psychoactive substances as a last resort—A qualitative study of self-treatment of migraine and cluster headaches. Harm Reduct J 14: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bershad AK, Schepers ST, Bremmer MP, et al. (2019) Acute subjective and behavioral effects of microdoses of lysergic acid diethylamide in healthy human volunteers. Biol Psychiatry 86: 792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Krystal JH, Putnam FW, et al. (1998) Measurement of dissociative states with the clinician-administered dissociative states scale (CADSS). J Trauma Stress 11: 125–136. [DOI] [PubMed] [Google Scholar]
- Bruehl S, Burns JW, Chung OY, et al. (2010) Hypoalgesia associated with elevated resting blood pressure: Evidence for endogenous opioid involvement. J Behav Med 33: 168–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ZD, Sullivan MA, Vosburg SK, et al. (2012) Effects of repeated oxycodone administration on its analgesic and subjective effects in normal, healthy volunteers. Behav Pharmacol 23: 271–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Gregorio D, Posa L, Ochoa-Sanchez R, et al. (2016) The hallucinogen d-lysergic diethylamide (LSD) decreases dopamine firing activity through 5-HT1A, D2 and TAAR1 receptors. Pharmacol Res 113: 81–91. [DOI] [PubMed] [Google Scholar]
- Derntl B, Hornung J, Sen ZD, et al. (2019) Interaction of sex and age on the dissociative effects of ketamine action in young healthy participants. Front Neurosci 13: 616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolder PC, Strajhar P, Vizeli P, et al. (2017) Pharmacokinetics and pharmacodynamics of lisdexamfetamine compared with D-amphetamine in healthy subjects. Front Pharmacol 8: 617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanciullacci M, Bene ED, Franchi G, et al. (1977) Brief report: Phantom limp pain—Sub-hallucinogenic treatment with lysergic acid diethylamide (LSD-25). Headache 17: 118–119. [DOI] [PubMed] [Google Scholar]
- Garland EL, Fredrickson BL. (2019) Positive psychological states in the arc from mindfulness to self-transcendence: Extensions of the Mindfulness-to-Meaning Theory and applications to addiction and chronic pain treatment. Curr Opin Psychol 28: 184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Hanley AW, Riquino MR, et al. (2019) Mindfulness-oriented recovery enhancement reduces opioid misuse risk via analgesic and positive psychological mechanisms: A randomized controlled trial. J Consult Clin Psychol 87: 927–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghione S. (1996) Hypertension-associated hypalgesia: Evidence in experimental animals and humans, pathophysiological mechanisms, and potential clinical consequences. Hypertension 28: 494–504. [DOI] [PubMed] [Google Scholar]
- Grof S. (1975) Realms of the Human Unconscious: Observations From LSD Research. New York: Viking Press. [Google Scholar]
- Grof S, Goodman LE, Richards WA, et al. (1973) LSD-assisted psychotherapy in patients with terminal cancer. Int Pharmacopsychiatry 8: 129–144. [DOI] [PubMed] [Google Scholar]
- Hofmann A. (1979) How LSD originated. J Psychedelic Drugs 11: 53–60. [DOI] [PubMed] [Google Scholar]
- Holze F, Duthaler U, Vizeli P, et al. (2019) Pharmacokinetics and subjective effects of a novel oral LSD formulation in healthy subjects. Br J Clin Pharmacol 85: 1474–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutten N, Mason NL, Dolder PC, et al. (2019) Self-rated effectiveness of microdosing with psychedelics for mental and physical health problems among microdosers. Front Psychiatry 10: 672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kast E. (1967) Attenuation of anticipation: A therapeutic use of lysergic acid diethylamide. Psychiatr Q 41: 646–657. [DOI] [PubMed] [Google Scholar]
- Kast EC, Collins VJ. (1964) Study of lysergic acid diethylamide as an analgesic agent. Anesth Analg 43: 285–291. [PubMed] [Google Scholar]
- Katz MM, Waskow IE, Olsson J. (1968) Characterizing the psychological state produced by LSD. J Abnorm Psychol 73: 1–14. [DOI] [PubMed] [Google Scholar]
- Kertesz SG, Gordon AJ. (2019) A crisis of opioids and the limits of prescription control: United States. Addiction 114: 169–180. [DOI] [PubMed] [Google Scholar]
- Kraehenmann R, Pokorny D, Vollenweider L, et al. (2017) Dreamlike effects of LSD on waking imagery in humans depend on serotonin 2A receptor activation. Psychopharmacology (Berl) 234: 2031–2046. [DOI] [PubMed] [Google Scholar]
- Lambru G, Matharu M. (2011) Serotonergic agents in the management of cluster headache. Curr Pain Headache Rep 15: 108–117. [DOI] [PubMed] [Google Scholar]
- Liechti ME. (2017) Modern clinical research on LSD. Neuropsychopharmacology 42: 2114–2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liechti ME, Dolder PC, Schmid Y. (2017) Alterations of consciousness and mystical-type experiences after acute LSD in humans. Psychopharmacology (Berl) 234: 1499–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols DE. (2016) Psychedelics. Pharmacol Rev 68: 264–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols DE, Grob CS. (2018) Is LSD toxic? Forensic Sci Int 284: 141–145. [DOI] [PubMed] [Google Scholar]
- Pahnke WN, Kurland AA, Goodman LE, et al. (1969) LSD-assisted psychotherapy with terminal cancer patients. Curr Psychiatr Ther 9: 144–152. [PubMed] [Google Scholar]
- Passie T, Halpern JH, Stichtenoth DO, et al. (2008) The pharmacology of lysergic acid diethylamide: A review. CNS Neurosci Ther 14: 295–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preller KH, Herdener M, Pokorny T, et al. (2017) The fabric of meaning and subjective effects in LSD-induced states depend on serotonin 2A receptor activation. Curr Biol 27: 451–457. [DOI] [PubMed] [Google Scholar]
- Ravn P, Secher EL, Skram U, et al. (2013) Morphine- and buprenorphine-induced analgesia and antihyperalgesia in a human inflammatory pain model: A double-blind, randomized, placebo-controlled, five-arm crossover study. J Pain Res 6: 23–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacco M, Meschi M, Regolisti G, et al. (2013) The relationship between blood pressure and pain. J Clin Hypertens (Greenwich) 15: 600–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schindler EA, Gottschalk CH, Weil MJ, et al. (2015) Indoleamine hallucinogens in cluster headache: Results of the Clusterbusters medication use survey. J Psychoactive Drugs 47: 372–381. [DOI] [PubMed] [Google Scholar]
- Schmid Y, Enzler F, Gasser P, et al. (2015) Acute effects of lysergic acid diethylamide in healthy subjects. Biol Psychiatry 78: 544–553. [DOI] [PubMed] [Google Scholar]
- Schmidt A, Muller F, Lenz C, et al. (2018) Acute LSD effects on response inhibition neural networks. Psychol Med 48: 1464–1473. [DOI] [PubMed] [Google Scholar]
- Sewell RA, Halpern JH, Pope HG., Jr (2006) Response of cluster headache to psilocybin and LSD. Neurology 66: 1920–1922. [DOI] [PubMed] [Google Scholar]
- Smeets T, Cornelisse S, Quaedflieg CW, et al. (2012) Introducing the Maastricht Acute Stress Test (MAST): A quick and non-invasive approach to elicit robust autonomic and glucocorticoid stress responses. Psychoneuroendocrinology 37: 1998–2008. [DOI] [PubMed] [Google Scholar]
- Spitzer C, Kendzierski T, Volkmann J, et al. (2008) The short form of Brief Symptom Inventory (BSI-18): First findings to the psychometric quality criteria. Psychother Psychosom Med Psychol 58: 82. [Google Scholar]
- Uthaug MV, Lancelotta R, van Oorsouw K, et al. (2019) A single inhalation of vapor from dried toad secretion containing 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) in a naturalistic setting is related to sustained enhancement of satisfaction with life, mindfulness-related capacities, and a decrement of psychopathological symptoms. Psychopharmacology (Berl) 236: 2653–2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Heugten-Van der Kloet D, Giesbrecht T, van Wel J, et al. (2015) MDMA, cannabis, and cocaine produce acute dissociative symptoms. Psychiatry Res 228: 907–912. [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Kometer M. (2010) The neurobiology of psychedelic drugs: Implications for the treatment of mood disorders. Nat Rev Neurosci 11: 642–651. [DOI] [PubMed] [Google Scholar]
- Whelan A, Johnson MI. (2018) Lysergic acid diethylamide and psilocybin for the management of patients with persistent pain: A potential role? Pain Manag 8: 217–229. [DOI] [PubMed] [Google Scholar]
- Yanakieva S, Polychroni N, Family N, et al. (2019) The effects of microdose LSD on time perception: A randomised, double-blind, placebo-controlled trial. Psychopharmacology (Berl) 236: 1159–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]