Abstract
Background
The use of noninvasive positive-pressure ventilation (NIPPV) for acute respiratory failure (ARF) has become more widespread over the past decade, but its prescription, use and outcomes in the clinical setting remain uncertain. The objective of this study was to review the use of NIPPV for ARF with respect to clinical indications, physician ordering, monitoring strategies and patient outcomes.
Methods
A total of 91 consecutive adult patients admitted between June 1997 and September 1998 to a university-affiliated tertiary care hospital in Hamilton, Ont., who received 95 trials of NIPPV for ARF were included in an observational cohort study. Data abstraction forms were completed in duplicate, then relevant clinical, physiologic, prescribing, monitoring and outcome data were abstracted from the NIPPV registry and hospital records.
Results
The most common indications for NIPPV were pulmonary edema (42 of 95 trials [44.2%]) and exacerbation of chronic obstructive pulmonary disease (23 of 95 trials [24.2%]). NIPPV was started primarily in the emergency department (62.1% of trials), however, in terms of total hours of NIPPV the most frequent sites of administration were the intensive care unit (30.9% of total hours) and the clinical teaching unit (20.2% of total hours). NIPPV was stopped in 48.4% of patients because of improvement and in 25.6% because of deterioration necessitating endotracheal intubation. The median time to intubation was 3.0 hours (interquartile range 0.8-12.2 hours). The respirology service was consulted for 28.4% of the patients. Physician orders usually lacked details of NIPPV settings and monitoring methods. We found no significant predictors of the need for endotracheal intubation. The overall death rate was 28.6%. The only independent predictor of death was a decreased level of consciousness (odds ratio 2.9, 95% confidence interval 1.0-8.4).
Interpretation
NIPPV was used for ARF of diverse causes in many hospital settings and was started and managed by physicians with various levels of training and experience. The use of this technique outside the critical care setting may be optimized by a multidisciplinary educational practice guidelin
Noninvasive positive-pressure ventilation (NIPPV) is a technique used to augment alveolar ventilation by nasal or full facial mask. NIPPV may be delivered by a mask fitted to a mechanical ventilator or a bilevel positive airway pressure unit, which provides both an inspiratory and an expiratory positive airway pressure.1
Uncontrolled studies,2,3,4 historically controlled studies5,6,7 and randomized trials8,9,10,11 have suggested that NIPPV is beneficial for patients with exacerbation of chronic obstructive pulmonary disease (COPD). A meta-analysis of 7 randomized trials showed that NIPPV is associated with lower rates of death (odds ratio [OR] 0.29, 95% confidence interval [CI] 0.15-0.59) and endotracheal intubation (OR 0.20, 95% CI 0.11-0.36) in patients with acute respiratory failure (ARF) compared with usual practice,12 with the greatest benefit in patients with exacerbation of acute COPD. NIPPV may be effective by resting chronically fatigued muscles,5,13 improving lung compliance or correcting alveolar hypoventilation.14 Additional advantages in COPD may be related to the improvement of exhalation in patients with raised intrinsic positive end-expiratory pressure, reducing the work of breathing.15,16
Although NIPPV holds the promise of making endotracheal intubation unnecessary in patients with ARF, the implementation of this technique outside a controlled trial setting remains uncertain. The objective of this study was to review the use of NIPPV in our hospital with respect to clinical indications, physician ordering, monitoring strategies and patient outcomes. We hypothesized that NIPPV may be inappropriately prescribed, insufficiently monitored and subject to "utilization drift" (application in settings beyond those for which clinical research supports efficacy and expertise supports safety).
Methods
This study was conducted at St. Joseph's Hospital, a university-affiliated tertiary care institution in Hamilton, Ont. The hospital has 386 beds, including 28 in the clinical teaching unit, 12 in the medical chest unit, 8 in the coronary care unit, 18 in the intermediate cardiac care unit and 15 in the intensive care unit (ICU). NIPPV was first implemented at the hospital in 1991 using the Respironics bilevel positive airway pressure machine (BiPAP machine; Respironics Inc., Murrysville, Pa.). In 1997, the Vision machine (Respironics Inc.) was introduced. This study was approved by the hospital's Ethics Committee.
We examined the NIPPV Respiratory Therapy Registry records and hospital charts of patients over 18 years of age admitted between June 1997 and September 1998 who received NIPPV for ARF. Patients were excluded if NIPPV was administered for respiratory distress after thoracotomy, palliation or sleep apnea, or as transition weaning from the ventilator.
We summarized the charts of 10 consecutive patients in duplicate (T.S., J.R.) and compared them. The data abstraction forms were then revised (T.S., D.J.C.). Subsequently, information was abstracted by one of us (T.S.) on patient characteristics, admission service, consultation by the respirology service, relevant physiologic measures and indications for use. The clinical indication for NIPPV was based on the emergency physician's notes and the admitting and progress notes of other physicians. If the records suggested 2 discordant clinical indications, the notes of the physician who prescribed NIPPV were used for the final determination. We also documented the duration of NIPPV, NIPPV settings, location of use, monitoring strategies, NIPPV complications, use of endotracheal intubation and in-hospital outcomes. We considered appropriate monitoring by nurses to include blood pressure, heart rate, respiratory rate, arterial oxygen saturation and clinical status and monitoring by respiratory therapists to include respiratory rate, arterial oxygen saturation, arterial blood gas levels and clinical status.
The results of our analysis are presented as absolute values and proportions, means and standard deviations, or medians and interquartile ranges for skewed data. We conducted logistic regression analyses to determine the predictors of endotracheal intubation and death. Independent variables included age, COPD, congestive heart failure, level of consciousness, hypercapnia, hypoxemia and monitoring by nurses and respiratory therapists. Independent variables that were univariately associated with either intubation or death (p < 0.10) were considered for the final regression models, which were built by backward stepwise logistic regression. Predictors are expressed using ORs and their 95% CIs. The mortality regression analysis excluded patients who died following delayed health care directives, referring to any situation in which a decision was made to limit the goals of care to exclude cardiopulmonary resuscitation or to change the goals of care to palliation. Inclusion of such patients in the mortality analysis could have artificially inflated the death rate.
Results
For the 104 registry patients who received NIPPV, 12 charts could not be located, because of incorrect hospital identification numbers (in 7 cases) or incomplete patient names (in 5 cases). One patient who was readmitted to have settings readjusted was also excluded. Therefore, we included 91 patients who received 95 trials of NIPPV (2 patients received 3 separate trials of NIPPV during the same hospital stay).
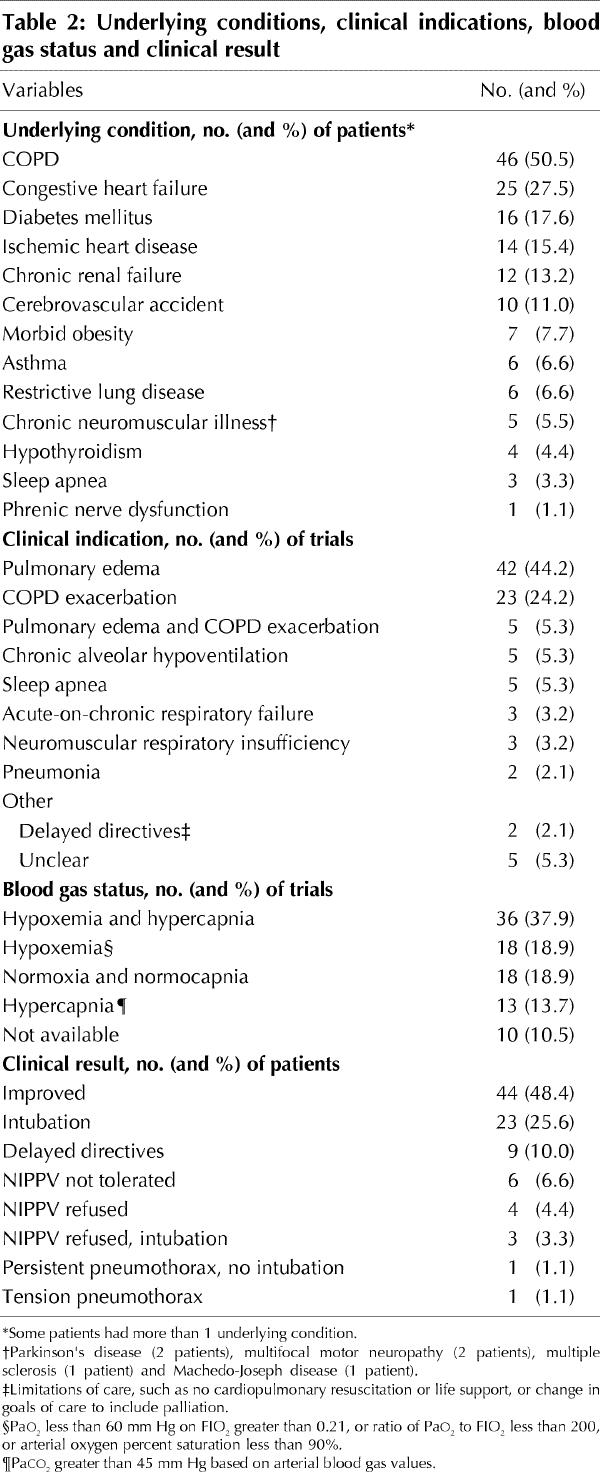
The patients' characteristics are presented in Table 1. Although most patients were alert when NIPPV was started, 6.6% had a severely decreased level of consciousness. Patients for whom arterial blood gas values were available were acidotic and had a median pH of 7.28 (interquartile range [IQR] 7.20-7.34) when NIPPV was started. The COPD subgroup had a median pH of 7.25 (IQR 7.22-7.34). The most common indications for NIPPV were pulmonary edema (44.2%) and exacerbation of COPD (24.2%) (Table 2). In most trials (37.9%), patients were both hypoxemic and hypercapnic before NIPPV was started. No baseline arterial blood gas values were determined for 10.5% of the patients. NIPPV was started before chest radiograph assessment in 17.8% of cases.
Table 1
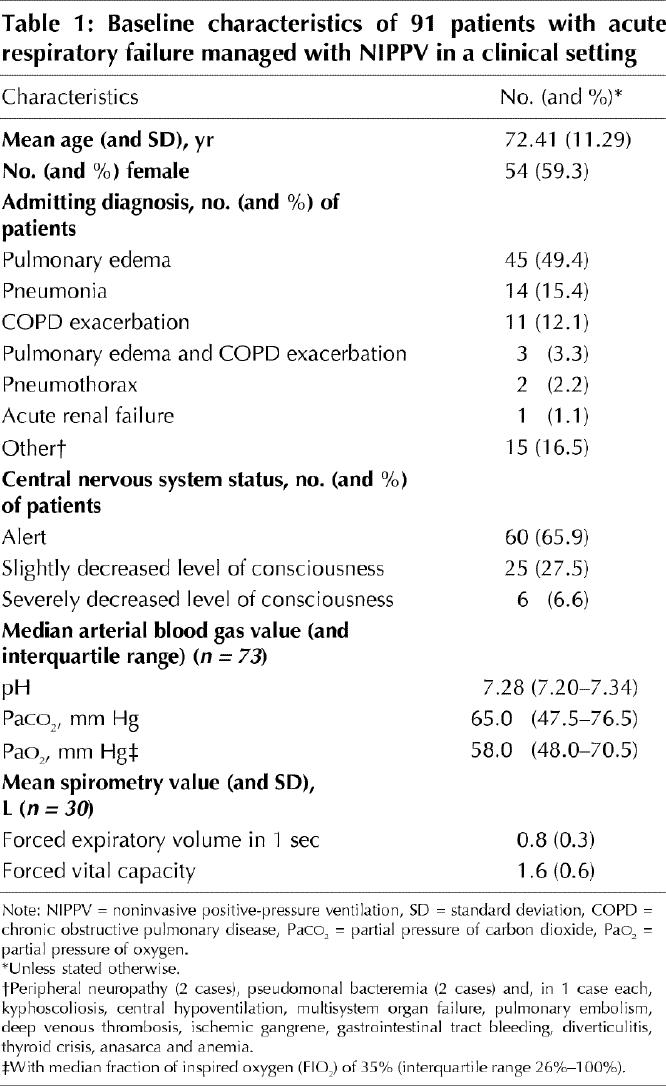
Table 2
Patients were most commonly admitted to the general internal medicine (46.1%), respirology (24.2%) or cardiology (19.8%) service. Physician orders were missing for 14.7% of the NIPPV trials. Most orders were written by housestaff (43.6%), emergency department physicians (36.4%) or respirologists (13.6%). The respirology service was consulted for 28.4% of the patients.
NIPPV was started primarily in the emergency department (62.1% of trials) (Fig. 1). The most common sites for NIPPV in terms of the number of hours were the ICU (30.9% of total hours) and the clinical teaching unit (20.2%) (Fig. 1). The interface was described as a full facial mask in 12.6% of the trials, nasal mask in 11.6%, both in 17.9% and tracheostomy in 1.1%; it was not documented for the remaining 56.8% of trials. The Respironics bilevel positive airway pressure machine was used in all patients but one, in whom the Vision machine was used. Cardiorespiratory monitoring was never explicitly ordered by physicians but was documented to occur by the nursing staff (in 89.5% of trials) and the respiratory therapy staff (in 93.7% of trials). Chest radiographs were assessed serially in 62.1% of cases, and arterial blood gas values were assessed serially in 47.4% of cases.
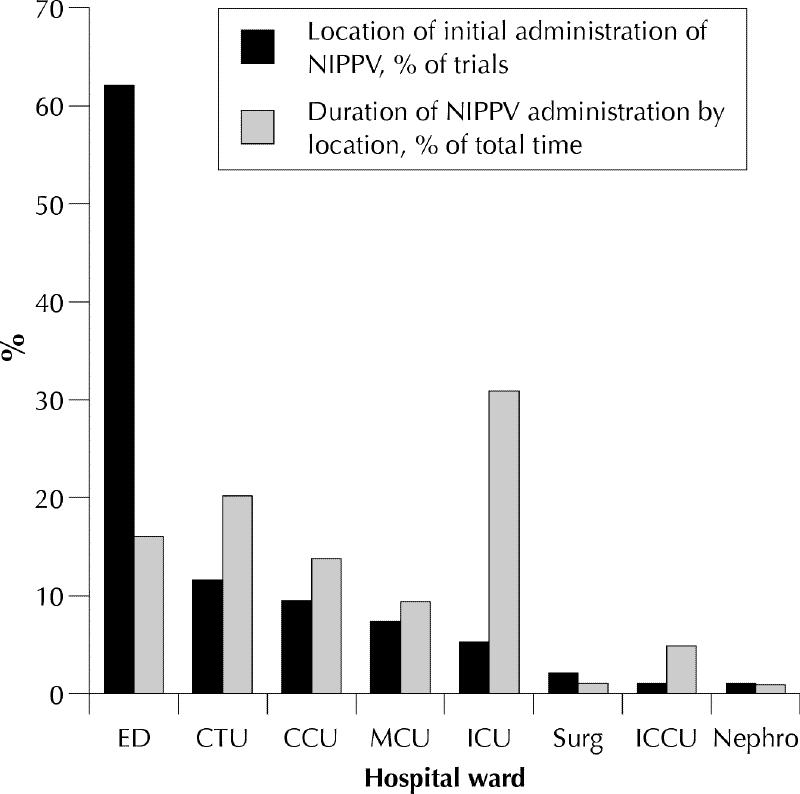
Fig. 1: Location of initiation of 95 trials of noninvasive positive-pressure ventilation (NIPPV) in 91 patients with acute respiratory failure (black bars) and proportion of total time of NIPPV administration (grey bars). ED = emergency department, CTU = clinical teaching unit, CCU = coronary care unit, MCU = medical chest unit, ICU = intensive care unit, Surg = surgical ward, ICCU = intermediate coronary care unit, Nephro = nephrology ward.
The median duration of NIPPV was 4.9 hours (IQR 1.8-15.5 hours). The median inspiratory positive airway pressure was 10 cm H2O (IQR 10-12 cm H2O) with a median expiratory positive airway pressure of 5 cm H2O (IQR 4-6 cm H2O).
NIPPV was stopped secondary to improved clinical status in 48.4% of the patients and because of delayed directives to forgo invasive or noninvasive life support in 10.0% of the patients; 25.6% required endotracheal intubation (Table 2). The median time to intubation was 3.0 hours (IQR 0.75-12.25 hours). NIPPV was stopped immediately in one patient after he was found to have a tension pneumothorax on chest radiography, which had not been ordered before NIPPV was started. Thirty-one patients (34.1%) subsequently underwent intubation: of the 31, 12 (38.7%) had exacerbation of COPD and 13 (41.9%) had pulmonary edema. The median duration of invasive ventilation was 5.0 hours (IQR 1.0-11.0 hours). Of the 91 patients, 39 (42.9%) were transferred to the ICU; of the 39, 27 (69.2%) were receiving NIPPV on transfer and 12 (30.8%) were receiving invasive ventilation.
Fifty-three patients (58.2%) were discharged from hospital with no ventilatory support, 8 (8.8%) were discharged home on NIPPV and 4 (4.4%) were transferred to another hospital. The overall death rate was 28.6%; when we excluded patients who had delayed directives to forgo life support, the death rate was 22.0%. We found no significant predictors of the need for endotracheal intubation. The only independent predictor of death was decreased level of consciousness (OR 2.9, 95% CI 1.0-8.4).
Interpretation
NIPPV was stopped in almost half of our patients because of clinical improvement, however, rates of endotracheal intubation and death were high compared with those reported in randomized trials.12,17 The reasons for the differences in outcome are probably multifactorial. Although favourable outcomes for patients receiving NIPPV for ARF have been reported, randomized trial results are rarely replicated precisely in the real world of practice. The reasons may include unmeasured differences between patients, different technical applications of NIPPV and unsystematic monitoring, to name a few. Moreover, our clinicians were often met with the challenge of dying patients with ARF or debilitating respiratory distress, representing situations in which advanced life support was not consistent with the overall goals of care, however, NIPPV was agreed upon.
Among our patients with COPD, the median arterial pH was 7.25. In other studies of patients with COPD who have ARF, severity of systemic acidosis was correlated with a poor short- and long-term prognosis.18,19 Jeffrey and colleagues20 reported an inverse relation between death and acidosis among patients with hypercapnic respiratory failure; the death rate was highest when the pH was less than 7.26. Two studies of NIPPV showed that patients with severe respiratory acidosis fared poorly compared with other patients,21,22 particularly if the acidosis was not corrected with NIPPV. Moreover, a lack of improvement in pH in the first hour or 2 after initiation of NIPPV has been associated with the need for intubation,3,7,23 and it has been proposed that NIPPV be administered earlier, before respiratory acidosis develops.24 Recently, Anton and coworkers25 corroborated the finding that an improvement in pH after 1 hour of NIPPV is associated with a successful outcome.
A total of 34.1% of our patients had a decreased level of consciousness when NIPPV was started. Depressed consciousness is a predictor of endotracheal intubation and death among patients receiving NIPPV.21 A recent prospectively validated multiple regression model of the use of NIPPV in patients with acute exacerbations of COPD confirmed that a higher level of consciousness before administration and significant improvements at 1 hour are both predictors of a successful trial of NIPPV.25 Although no patient in our study experienced myocardial infarction, Mehta and colleagues26 found a higher rate of myocardial infarction in patients with pulmonary edema who were randomly assigned to receive NIPPV (10/14 [71%]) than among those assigned to receive continuous positive airway pressure (4/13 [31%]).
In almost half of our patients, NIPPV was started by housestaff. Inexperience of the health care team administering NIPPV has been associated with a poor prognosis.24 Meduri and coworkers3 described a monthly NIPPV instructional videotape program for ICU fellows, nurses and respiratory therapists. Such educational programs should be part of institutional policies for NIPPV.
The clinical teaching unit was the second most common site, after the ICU, for NIPPV. Intensive cardiorespiratory monitoring is, however, not always possible on the clinical teaching unit, and unfortunately the medical step-down unit was closed. Accordingly, the clinical team unit may have been the best option because an ICU bed may not have been available at the time of initiation of NIPPV. The medical-ward monitoring in our study contrasts with that described for 20 general-ward patients in a Spanish study, who received intensive bedside monitoring during an "adaptation phase" for NIPPV, followed by an "implementation phase" during which problems such as air leaks could be identified and immediately rectified.23
The median duration of NIPPV in our study, 4.9 hours, is lower than that reported by Barbe and colleagues,23 who treated ward patients with NIPPV for 6 hours during the day for at least the first 3 days of the hospital stay. In several randomized trials NIPPV was administered for longer periods, ranging from 6 hours per day8,9,10 to almost continuously.11 Furthermore, the pressure levels in our study were lower than those in several randomized trials (median inspiratory positive airway pressure of 10 cm H2O with a median expiratory positive airway pressure of 5 cm H2O in our study, compared with 16-20 cm H2O and 5-10 cm H2O respectively in published trials).3,8,9,23 Although there is no established standard duration of administration or pressure levels, the literature suggests that longer duration and higher pressure levels may be necessary to rest fatigued respiratory muscles adequately before the benefits of NIPPV can be seen.
Although the intubation rate in our COPD subgroup was lower at 13.0%, compared with the pooled rate of 23.9% in randomized trials,12 the mortality rate was higher at 23.1% compared with the pooled rate of 8.9%.12 The mortality rate in our subgroup of patients with congestive heart failure was 50.0%, compared with the pooled rate of 10.1% in such patients treated with continuous positive airway pressure in randomized trials.17 This rate of 50.0% is also higher than that for the control population in these trials of 17.8%.17 When we excluded patients who had delayed directives to limit care, our overall death rate was still 22.0%. However, inferences about between-study differences in rates of endotracheal intubation and death must be made cautiously. Our study was observational and had no control group, and we did not restrict inclusion to the highly selected patients enrolled in randomized trials.
Although NIPPV can provide substantial clinical benefits in appropriately selected patients,12,17 careful analysis of the determinants and consequences of utilization drift are the foundation for quality-improvement initiatives. We are undertaking the development, implementation and evaluation of a practice guideline for the optimal use of NIPPV in ARF. Other institutions that use NIPPV may also have found this technique challenging and may use this type of utilization review to identify opportunities for improvement.
Acknowledgments
We thank the respiratory therapists, nurses, housestaff and attending physicians who participated in this study. We appreciate the support of Dr. Peter Powles, Dr. David Higgins, Barbara Hill, Valerie Fitzell and the physicians in the Firestone Chest and Allergy Unit.
Footnotes
This article has been peer reviewed.
This study was supported by a Resident Award to Dr. Sinuff from Regional Medical Associates, Hamilton, Ont. Dr. Cook is an Investigator with the Canadian Institutes of Health Research.
Reprint requests to: Dr. Deborah J. Cook, Department of Medicine, St. Joseph's Hospital, 50 Charlton Ave. E, Hamilton ON L8N 4A6; fax 905 521-6068; debcook@fhs.csu.mcmaster.ca
References
- 1.Meduri GU. Noninvasive positive-pressure ventilation in patients with acute respiratory failure. In: Physiological basis of ventilatory support. New York: Marcel Dekker; 1998. p. 921-96.
- 2.Confalonieri M, Aiolfi S, Gandola L, Scartabellati A, Della Porta R, Parigi P. Severe exacerbations of chronic obstructive pulmonary disease treated with BiPAP by nasal mask. Respiration 1994;61:310-6. [DOI] [PubMed]
- 3.Meduri GU, Turner RE, Abou-Shala N, Wundernik R, Tolley E. Noninvasive positive pressure ventilation via face mask: first line intervention in patients with acute hypercapneic and hypoxemic respiratory failure. Chest 1996; 109:179-93. [DOI] [PubMed]
- 4.Pollack C Jr, Torres MT, Alexander L. Feasibility study of the use of bilevel positive airway pressure for respiratory support in the emergency department. Ann Emerg Med 1996;27:189-92. [DOI] [PubMed]
- 5.Brochard L, Isabey D, Piquet J, Amaro P, Mancebo J, Messadi AA, et al. Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask. N Engl J Med 1990;323:1523-30. [DOI] [PubMed]
- 6.Confalonieri M, Parigi P, Scartabellati A, Aiolfi S, Scorsetti S, Nava S, et al. Noninvasive mechanical ventilation improves the immediate and long-term outcome of COPD patients with acute respiratory failure. Eur Respir J 1996; 9:422-30. [DOI] [PubMed]
- 7.Vitacca M, Clini E, Rubini F, Nava S, Foglio K, Ambrosino N. Noninvasive mechanical ventilation in severe obstructive lung disease and acute respiratory failure: short- and long-term prognosis. Intensive Care Med 1996;22:94-100. [DOI] [PubMed]
- 8.Bott J, Carroll MP, Conway JH, Keilty SE, Ward EM, Brown AM, et al. Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet 1993;341:1555-7. [DOI] [PubMed]
- 9.Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995;333:817-22. [DOI] [PubMed]
- 10.Kramer N, Meyer TJ, Meharg J, Cece RC, Hill NS. Randomized, prospective trial of noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med 1995;151:1799-806. [DOI] [PubMed]
- 11.Wysocki M, Tric L, Wolff MA, Millet H, Herman B. Noninvasive pressure support ventilation in patients with acute respiratory failure. A randomized comparison with conventional therapy. Chest 1995;107:761-8. [DOI] [PubMed]
- 12.Keenan SP, Kernerman PD, Cook DJ, Martin CM, McCormack D, Sibbald WJ. Effect of noninvasive positive pressure ventilation on mortality in patients admitted with acute respiratory failure: a meta-analysis. Crit Care Med 1997;25:1685-92. [DOI] [PubMed]
- 13.Renston JP, DiMarco AF, Supinski GS. Respiratory muscle rest using nasal BiPAP ventilation in patients with stable severe COPD. Chest 1994;105:1053-60. [DOI] [PubMed]
- 14.Bergofsky EH. Respiratory failure in disorders of the thoracic cage. Am Rev Respir Dis 1979;119:643-69. [DOI] [PubMed]
- 15.Goldberg P, Reissmann H, Maltais F, Ranieri M, Gottfried SB. Efficacy of noninvasive CPAP in COPD with acute respiratory failure. Eur Respir J 1995;8:1894-1900. [DOI] [PubMed]
- 16.Appendini L, Patessio A, Zanaboni S, Carone M, Gukov B, Donner CF, et al. Physiologic effects of positive end-expiratory pressure and mask pressure support during exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1994;149:1069-76. [DOI] [PubMed]
- 17.Pang D, Keenan SP, Cook DJ, Sibbald WJ. The effect of positive pressure airway support on mortality and the need for intubation in cardiogenic pulmonary edema: a systematic review. Chest 1998;114:1185-92. [DOI] [PubMed]
- 18.Asmundsson T, Kilburn KH. Survival of acute respiratory failure: a study of 239 episodes. Ann Intern Med 1969;70:471-85. [DOI] [PubMed]
- 19.Burk RH, George RB. Acute respiratory failure in chronic obstructive pulmonary disease. Immediate and long-term prognosis. Arch Intern Med 1973; 132:865-8. [PubMed]
- 20.Jeffrey AA, Warren PM, Flenley DC. Acute hypercapneic respiratory failure in patients with chronic obstructive lung disease: risk factors and use of guidelines for management. Thorax 1992;47:34-40. [DOI] [PMC free article] [PubMed]
- 21.Ambrosino N, Foglio K, Rubini F, Clini E, Nava S, Vitacca M. Non-invasive mechanical ventilation in acute respiratory failure due to chronic obstructive pulmonary disease: correlates for success. Thorax 1995;50:755-7. [DOI] [PMC free article] [PubMed]
- 22.Brown JS, Meechum Jones DJ, Mikelsons C, Paul EA, Wedzicha JA. Outcome of nasal intermittent positive pressure ventilation when used for acute-on-chronic respiratory failure on a general respiratory ward. J R Coll Physicians Lond 1998;32:219-24. [PMC free article] [PubMed]
- 23.Barbe F, Togores B, Rubi M, Pons S, Maimo A, Agusti AGN. Noninvasive ventilatory support does not facilitate recovery from acute respiratory failure in chronic obstructive pulmonary disease. Eur Respir J 1996;9:1240-5. [DOI] [PubMed]
- 24.Wedzicha JA. Delivery of noninvasive ventilation outside the intensive care unit. Clin Pulm Med 1998;5:364-9.
- 25.Anton A, Guell R, Gomez J, Serrano J, Castellano A, Carrasco JL, et al. Predicting the result of noninvasive ventilation in severe acute exacerbations of patients with chronic airflow limitation. Chest 2000;117:828-33. [DOI] [PubMed]
- 26.Mehta S, Jay GD, Woolard RH, Hipona RA, Connolly EM, Cimini DM, et al. Randomized, prospective trial of bilevel versus continuous positive airway pressure in acute pulmonary edema. Crit Care Med 1997;25:620-8. [DOI] [PubMed]


