Abstract
Purpose of Review
Benign prostatic hyperplasia (BPH) and lower urinary tract symptoms (LUTS) is a disease complex with enormous societal burden and yet the pathogenesis of LUTS/BPH is poorly understood. We set out to review the literature on the relationship between depression, marijuana usage, and erectile dysfunction (ED) to LUTS/BPH.
Recent Findings
LUTS/BPH has independent associations with depression as well as with ED. In each case, the causality and mechanistic relationship is unknown. The impact of marijuana, as it increasingly pervades the general population, on the disease complex of LUTS/BPH is not well studied but recent results support short-term benefit and long-term caution.
Summary
Depression, a form of central nervous dysfunction, and ED, which is likely mediated via endothelial dysfunction, are independently associated with LUTS/BPH. The presence of cannabinoid receptors in urologic organs, coupled with recent population studies, supports a modulatory effect of marijuana on voiding although an enormous knowledge gap remains.
Keywords: BPH, Voiding, LUTS, Prostate, Marijuana, ED
Introduction
Benign prostatic hyperplasia (BPH) and BPH-associated lower urinary tract symptoms (LUTS) have a significant impact on men’s health. Globally, BPH carries the highest health burden of any urologic disorder, malignant or benign, and is poised to rise even more rapidly [1]. As the population ages and the societal burden of LUTS/BPH increases, better understanding of its underlying causes and associated disease processes becomes more critical. LUTS/BPH has multiple causative factors and many epidemiologic correlates, but an effective and unifying understanding of this heterogeneous disease has proven elusive.
Specific associations have been investigated in hopes of better understanding how to treat and avoid progression of BPH and LUTS. Metabolic syndrome (MetS) has been linked with the disease process of LUTS/BPH, but evidence has been variable and inconclusive [2•]. Hypertension (HTN), type 2 diabetes (DM), obesity, physical inactivity [3, 4], autonomic nervous system overactivity [5], prostate growth rates, and failure of senescence [6, 7] have all been found to contribute to or correlate with LUTS/BPH. Other community surveys of erectile dysfunction (ED) found that prostatitis and incontinence are strongly associated with LUTS/BPH [8], and a subsequent meta-analysis verified deep interrelationship between these two diseases of the aging male. Implicating central nervous system involvement in the process, depression has been linked with both LUTS and BPH although causality is unknown [9–12]. Furthermore, recent studies have shown a relationship between marijuana usage and LUTS/BPH that suggest short-term improvement in voiding but raise concerns about long-term usage [13–17]. However, we are unaware of any data showing impact on urinary function related to alcohol usage. We set out to review the latest literature on the relationship between LUTS/BPH, and these comorbid conditions and coexisting habits.
Marijuana Use and LUTS
Marijuana is a product derived from the cannabis plant, a flowering member of the family Cannabaceae. The genus is thought to be indigenous to central Asia. Medicinal uses for marijuana date back 5000 years across many cultures for a variety of medical problems. The active ingredients of marijuana include tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is a psychoactive compound which can induce euphoria, relaxation, altered perception of time, increased appetite, and heightened sensory perception [18]. CBD is a non-psychoactive substance that is hypothesized to have an effect on anxiety, cognition, movement disorders, and pain [19]. Suggestive of pharmacologic effect, usage for myriad processes has been reported in the modern medical literature for hundreds of years [20].
THC, the primary identified active agent in marijuana, mediates effect on target tissue via two primary receptors: CB-1 and CB-2. This identification of a direct effect of cannabinoids on the bladder, and the identification of the widespread cannabinoid receptor (CB-1) as a mechanism for the mediation of that effect, has led to studies, primarily in murine models. The second receptor, CB-2, shares 44% homology with CB-1 and is more limited in distribution, being mostly found in brain and testes [21].
Translational Studies of Cannabinoid Effects on Bladder and Voiding
Cannabinoids have been observed to modulate bladder function in animal models including an increase in voided volume, voiding pressure, and prolonged intermicturition intervals [22••]. Direct arterial injection of CB agonist also decreased bladder voiding threshold, both at baseline and in response to irritants [23]. This effect was ameliorated by competitive antagonists of the receptor. Intravesical instillation of synthetic cannabinoids also had an effect on bladder response pointing towards the involvement of CB-1 receptors when compared to the CB-2, with CB-1 appearing to be the primary mediator of voiding effects [24]. In a separate murine model of acrolein-induced cystitis, cannabinoids were found to significantly counteract the irritative effects of the chemical, suggesting a potential role for bladder pain management in humans [25, 26]. Overall, THC and synthetic cannabinoid agonists of the CB-1 and to a lesser extent CB-2 receptor appear to have generally beneficial short-term effects on voiding in animal models. Long-term effects and chronic adaptation are still mostly unknown.
Effects of Marijuana on Human Voiding
Human voiding response to cannabinoids has not been much studied, although an identifiable effect appears to exist. Cannabis usage induced intriguing responses in bladder and urine proteomics: increases in immune response pathways, and carbohydrate-related mechanisms, among others [27]. Two cross-sectional population studies have found a statistically significant association between marijuana usage and the presence of LUTS. First, 3037 men aged 20–59 and completing the National Health and Nutrition Examination Survey from 2005 to 2008 found that self-reported marijuana users experienced less LUTS [28•]. More recently, it was observed that in a sample of 173,469 men (aged 45 or over), those who were identified as using cannabis were significantly more likely to receive treatment for LUTS/BPH than men who were not [29]. This “substance use-symptom” relationship between marijuana and LUTS/BPH was not present in the same group when assessed for the effects of alcohol consumption.
These two findings address separate end points: self-reported voiding dysfunction is different than the receipt of treatment for LUTS/BPH. Additionally, the age groups were somewhat different in these two groups, and it was not possible to control the NHANES data for age-related correlation of usage. This is important because the use of marijuana decreases substantially with age: 30% of adults in the 18–25 age group reported marijuana usage in the past year, but this rate drops to 3.4% of those who are 50–64 years old and 0.6% in adults over 65 [30]. It seems likely that adult marijuana users represent a somewhat distinct population subset, behaviorally, socially, or biologically. Perhaps, men who use marijuana, especially those that use into adult life and past the age of 45, find it therapeutic in the same fashion that leads general and younger users to report lower baseline urinary symptoms. Alternatively, continued consumption in later life may be a marker for long-term exposure and a high cumulative dose of cannabinoid, which in turn may represent a damaging effect. It is not possible to draw conclusions regarding effects of chronic exposure to marijuana from these data. Other substances of abuse and toxins can result in severe and direct urinary morbidity, such as ketamine [31], although this pharmacological agent is unrelated to THC and marijuana.
In multiple sclerosis (MS) patients, cannabinoids showed some beneficial effects on muscular spasticity and on urinary function in men and women, although results have varied between the studies and formulation of cannabinoid administration [32]. A survey of MS patients using marijuana found that over half of patients reported subjective improvement in urinary symptoms, and others confirmed improvement in urge and incontinence, thereby, supporting self-selection for a perceived benefit of cannabinoids [14–17]. A controlled trial of cannabinoids and placebo in 24 patients with a variety of neurological symptoms, primarily from MS, showed a notable improvement in pain and other symptoms, including LUTS improvement in cannabinoid users.
Depression and LUTS
Depressive disorder is a common medical problem among older adult males. It has significant health-related quality of life implications including decreased functional status and increased mortality, and is a risk factor for the development of other chronic diseases [33]. Depression as a diagnosis is characterized by depressed mood and loss of interest in enjoyable facets of life and/or pleasure. The condition can manifest itself in a variety of ways both mentally and physically [34]. The prevalence of depression in adults is 7.7% in those age 20–39, 8.4% in those age 40–59, and 8.0% in those age 60 and over, according to the National Health and Nutrition Examination Survey (2013–2016). Clinical studies revealed a correlation between depression and the diagnosis of LUTS. A review of 547 men identified that the 22% who scored poorly on a geriatric depression scale were three times more likely to also have severe LUTS, as was defined by an IPSS score of > 20.9 Similar observations have been made in patients from Australia and Korea [35–37], and a systematic review of nocturia also found strong correlation with depression [38]. Our group was able to identify the same association in an American sample of 173,649 men, with the diagnosis of depression carrying an odds ratio of 2.05 (95% CI 1.95, 2.16) for requiring LUTS/BPH therapy after multivariable controls [29]. The range of depression prevalence in patients with LUTS lies within 11.5–12.3% [39, 40]. The severity of LUTS directly correlates with increasing severity of depressive symptoms, as well as with higher odds of suicidal ideation in cross-sectional studies [41, 42]. Whether this is a centrally mediated effect or whether the depressive state is a consequence of other symptoms and organ dysfunction is still unknown.
The causality underlying the correlation between LUTS/BPH and depression is unknown. A Taiwanese prospective study determined a significantly higher rate of developing depression in patients diagnosed with BPH at the study onset in comparison with those who did not have a diagnosis of BPH (2.01% vs 1.01%, 1-year follow-up). The likelihood ratio of developing depression in those with BPH was 1.87 (95% CI = 1.63–2.16, p < 0.001) [43, 44]. There appears to be a temporal relationship between onset of BPH and subsequent development of depressive symptoms at 2 years, and our group’s work on a large cross-sectional dataset found that depression carries a hazard ratio of 2.05 (95% CI: 1.95, 2.16, p < 0.001) which exceeds the ratio for diabetes, hypertension and obesity/metabolic syndrome. [29, 45] It has been suggested that the psychiatric effects of depression can manifest in worsened self-reported BPH symptoms as patient perspective is damaged [9]. Depression has also been shown to be an independent risk factor for progression of LUTS over time [9, 36, 41].
Whether the depressive state is a CNS-mediated effect, a consequence of other symptoms and organ pathology, or broad CNS dysfunction occurs in parallel to LUTS in the aging male is still unknown. Likely, a decline in organ function, for example, of the urinary bladder, might be paralleled or enhanced by a decrease in the function of the central or peripheral nervous system.
Adding to the myriad of interrelated factors is the apparent interaction between depression and cannabis usage. A study of 14,000 twins from Australia as well as other groups has suggested a correlation between heavy marijuana usage and depression [46–49]. The exact relationship between the two entities is not completely established, but studies suggest that regular marijuana use in adolescents results in a decrease in size in certain regions of the brain (hippocampus, amygdala, prefrontal cortex) that are dense in endocannabinoid receptors [50]. Furthermore, early cannabis use was also associated with anhedonia and decreased serotonin levels in adults [51]. The underlying deficiency in the intrinsic endocannabinoid system may be involved in heightened risk of post-traumatic stress development and may be the cause of increased cannabis use [52]. The use of cannabinoids may also play a role in other behavioral diseases where the intrinsic endocannabinoid system appears to mediate neurochemical changes underlying the placebo effect [53]. Could a subset of individuals similarly discover that the addition of exogenous cannabinoid to their own internal milieu corrects other forms of bother? There is a complex interaction between cannabinoid use, depression, and LUTS and further studies will be needed to understand their effects on each other (Fig. 1).
Fig. 1.
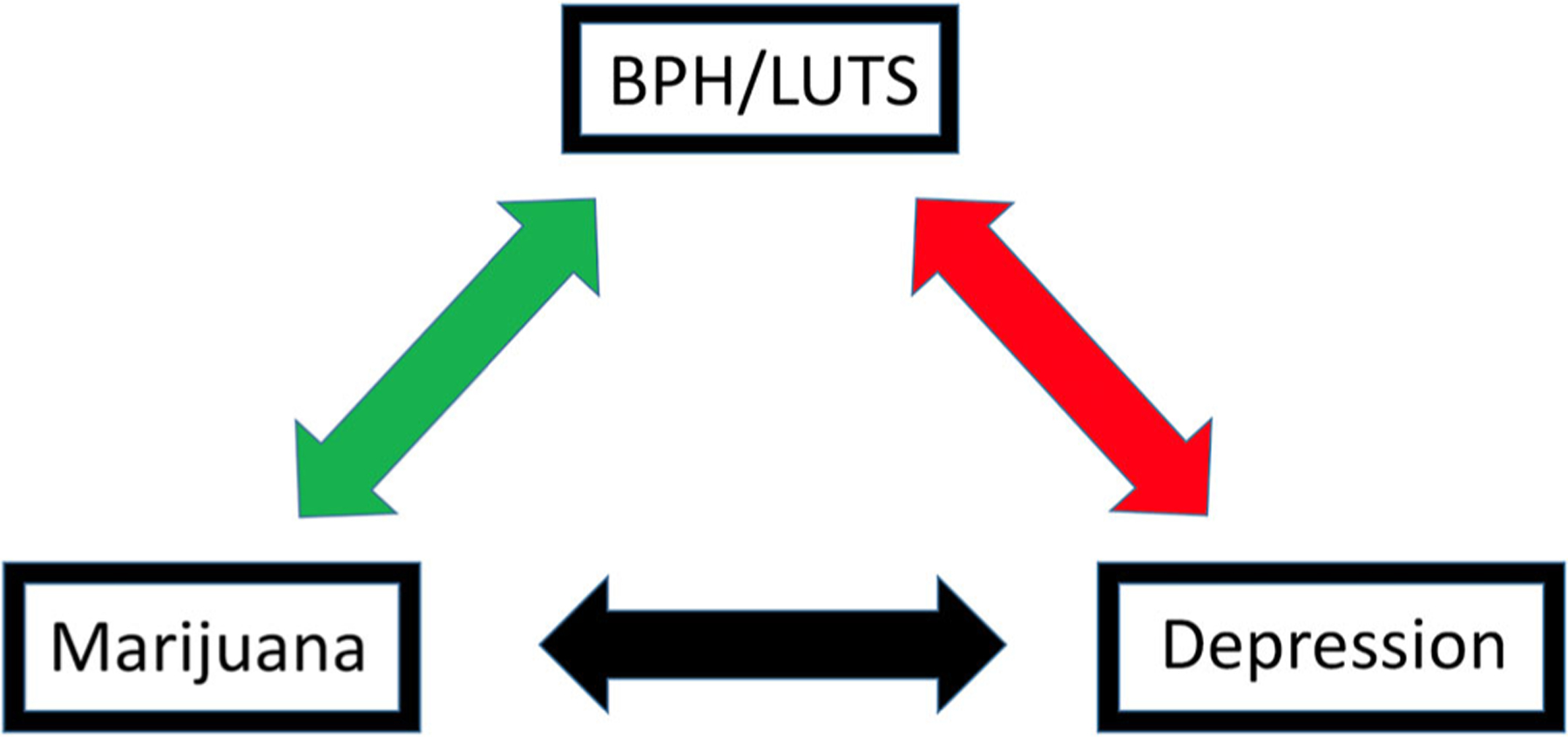
Complex interplay between LUTS, depression, and marijuana usage. A causative or primary factor has not been identified
Erectile Dysfunction
Erectile dysfunction (ED) and LUTS caused by BPH (LUTS/BPH) are highly common around the world. The prevalence of LUTS/BPH and ED in men increases with age, and both conditions have been found to coexist in many men [54]. Erectile dysfunction is defined as the inability to attain and maintain an erection sufficient for sexual intercourse at least 25% of the time [55]. The problem often develops gradually. The pathophysiology of ED in this group includes chronic ischemia, which leads to deterioration of cavernosal smooth muscle and the development of corporeal fibrosis [56]. Erectile dysfunction has diverse causality and includes side effects of some medications, iatrogenic nerve damage, and psychosocial causes: most but not all organic causes ultimately result in a failure of the vascular bed [57]. ED affects a large portion of the aging population, with the Massachusetts Male Aging Study finding that 52% of men aged 40–70 years develop some degree of ED. [58]
Although ED can be an isolated issue, often age and many of the same comorbidities that track with BPH also coexist with this disease. [59] Even a mild increase in LUTS/BPH severity parallels increases the incidence of ED, and also negatively affects quality of life in patients. A multinational prospective study of men describing sexual function and various comorbidities established that up to 90% of men had moderate to severe LUTS, the severity of which increased with age, while sexual dysfunction was reported at 82%. The level of sexual dysfunction directly correlated with the severity of LUTS [60]. Considering this data, LUTS itself is an independent risk factor for ED in addition to the commonly recognized risks factors such as age, diabetes, hypertension, and pelvic surgery [61]. Similarly, in a large cross-sectional analysis, the diagnosis of ED was associated with increased risk of being on a LUTS medication that persisted after controlling for other various comorbidities (OR 1.80, 95% CI 1.67, 1.94, p < 0.001) [29]. Overall, these data provide evidence of a consistent and strong relationship between LUTS and ED. [62, 63]
Many theories have been postulated regarding the tissue- and organ-level etiology of ED. One of the suggestions includes an imbalance in the autonomic control of penile smooth muscle contractions and relaxations which may play an important role in both LUTS and ED. [64] Additionally, endothelial dysfunction associated with impaired endothelium-dependent vasodilation resulting from the decreased bioactivity of nitric oxide can link the two pathological conditions [65]. ED has been studied as a marker for systemic endothelial dysfunction, and has been shown to provide an early clue, for example, to the presence of occult cardiovascular disease [66]. This endothelial failure may define a physiological vulnerability of the bladder that is exaggerated during obstruction-mediated stress secondary to BPH, further accelerating the development of LUTS [67]. Furthermore, the prostate has nitric oxide receptors that modulate smooth muscle tone in the prostate and urethra, and likely are the mechanism by which phosphoesterase-5 inhibitors (PDE-5I) are effective in the management of LUTS [68].
Marijuana and Erectile/Sexual Function
The prevalence of cannabinoid use in the adolescent population seems to be stable despite growing legalization; however, usage rates in the adult population show growth along with a decrease in the perception of potential harm [69]. Given the historical paucity of research on marijuana usage, there is an increasing need to elucidate possible health repercussions. One of the observed negative impacts of marijuana use is the linkage of the use of marijuana with the development of ED. [70•] Considering that the causes of ED may be psychological, organic, or likely a mix of both, there are many questions of etiologies, cofactors, and comorbidities to consider. One possible mechanism is mediation via the endocannabinoid system and the binding of receptors in the paraventricular nucleus of the hypothalamus which regulates erectile function and sexual behavior of males [49, 71]. In addition, there could be a direct influence on the penis from the cannabis itself. Both animal and human studies reported a peripheral effect of cannabis on ED, specifically on corpus cavernosum where cannabinoid receptors are present [72, 73]. CB1 and CB2 receptors are located on NOS-containing nerves in primate and human corpus cavernosum tissues [72]. In murine models, CB1 receptor antagonist induced penile erection when injected into the paraventricular nucleus of male rats. [73] Considering the high correlation between ED and cannabis use, as well as potential harmful effects of marijuana on male sexual and general health, it is necessary to increase and improve the knowledge on this topic in order to achieve the best clinical and public health strategies [74].
Conclusion
In summary, we found a significant evidence of linkage between voiding function, sexual response, and the use of cannabinoids in the published literature. Based on the possible pathophysiological mechanisms of LUTS/BPH and ED as well as other common comorbidities observed in aging men with these conditions, further multidisciplinary studies are warranted [75•]. Men presenting with LUTS should be evaluated for sexual dysfunction and ED, and those presenting with ED should be assessed for LUTS/BPH [68]. A thorough social history including illicit substance use is an important baseline set of data to register during patient evaluations.
Summary
Cumulative research in the domain of LUTS has shown an ever-more complex interaction between organs, systems, and environmental factors. LUTS/BPH is not purely consequent to processes occurring locally in the prostate, but involves processes and responses in the bladder, systemic microvascular bed, muscular system, and CNS. Establishing the relationships between comorbid conditions and their association with LUTS/BPH has proven useful to extend our understanding.
Depression
There is a clear association between LUTS/BPH and depression; however, the mechanisms underlying this comorbidity are not fully understood. Further studies are needed to better define this correlation, and broad assessment of quality of life issues, emotional states, and screening for depression in those afflicted with LUTS/BPH is encouraged.
Marijuana Usage
With the expanding legalization of marijuana and accompanying increases in usage, it is important to establish the effects of marijuana compounds on bladder, prostate function, and LUTS. Population-based studies showed that in the general population, men who use marijuana report a lower prevalence of LUTS. This effect is likely driven by the majority of younger users; however, men over 45 who use marijuana report a higher chance of requiring medical therapy for LUTS/BPH. Data from the MS population observed short-term subjective improvement in LUTS with marijuana use; it is unclear whether this effect is mediated at a CNS or organ level. There is currently limited information available to advance clinical practice and recommendations to patients when it comes to marijuana use and occurrence of LUTS, but caution certainly is prudent given that the long-term effects of prolonged marijuana use are unknown.
Erectile Dysfunction
There is a clear and distinct correlation between ED and LUTS. The pathophysiological mechanisms and causative relationships are not entirely clear, but in this instance may involve changes in the vascular tone and oxygenation of tissues in the prostate, urethra, and bladder. Established PDE5i effects in the improvement of LUTS seem to support this suggestion.
Other Patient Considerations
LUTS/BPH comprises an enormous portion of both general and urologic practice, and this disease harms a broad swathe of the general population. In order to provide the most comprehensive and holistic care for patients, an understanding of the interrelationship of LUTS/BPH and other disease states including depression, ED, and marijuana use is important. Specific advice is not able to be easily culled from the literature at present, but as the population ages and the prevalence of marijuana use increases in adults, these topics will become ever-more important.
Footnotes
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223. [DOI] [PubMed] [Google Scholar]
- 2.•.Gacci M, Corona G, Vignozzi L, et al. Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int. 2015;115(1):24–31. [DOI] [PubMed] [Google Scholar]; Excellent review of this topic.
- 3.Platz EA, Kawachi I, Rimm EB, Colditz GA, Stampfer MJ, Willett WC, et al. Physical activity and benign prostatic hyperplasia. Arch Intern Med. 1998;158(21):2349–56. [DOI] [PubMed] [Google Scholar]
- 4.Parsons JK, Kashefi C. Physical activity, benign prostatic hyperplasia, and lower urinary tract symptoms. Eur Urol. 2008;53(6):1228–35. [DOI] [PubMed] [Google Scholar]
- 5.McVary KT, Rademaker A, Lloyd GL, Gann P. Autonomic nervous system overactivity in men with lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2005;174(4 Pt 1): 1327–433. [DOI] [PubMed] [Google Scholar]
- 6.Castro P, Giri D, Lamb D, Ittmann M. Cellular senescence in the pathogenesis of benign prostatic hyperplasia. Prostate. 2003;55(1): 30–8. [DOI] [PubMed] [Google Scholar]
- 7.Vital P, Castro P, Tsang S, Ittmann M. The senescence-associated secretory phenotype promotes benign prostatic hyperplasia. Am J Pathol. 2014;184(3):721–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brookes ST, Link CL, Donovan JL, McKinlay JB. Relationship between lower urinary tract symptoms and erectile dysfunction: results from the Boston Area Community Health Survey. J Urol. 2008;179(1):250–5. discussion 255. [DOI] [PubMed] [Google Scholar]
- 9.Johnson TV, Abbasi A, Ehrlich SS, Kleris RS, Chirumamilla SL, Schoenberg ED, et al. Major depression drives severity of American Urological Association Symptom Index. Urology. 2010;76(6):1317–20. [DOI] [PubMed] [Google Scholar]
- 10.Johnson TV, Goodman M, Master VA. The efficacy of written screening tools in an inner city hospital: literacy based limitations on patient access to appropriate care. J Urol. 2007;178(2):623–9. discussion 629. [DOI] [PubMed] [Google Scholar]
- 11.Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol. 2004;46(5):547–54. [DOI] [PubMed] [Google Scholar]
- 12.Hagberg KW, Divan HA, Nickel JC, Jick SS. Risk of incident antidepressant-treated depression associated with use of 5alpha-reductase inhibitors compared with use of alpha-blockers in men with benign prostatic hyperplasia: a population-based study using the Clinical Practice Research Datalink. Pharmacotherapy. 2017;37(5):517–27. [DOI] [PubMed] [Google Scholar]
- 13.Lloyd GL, Carmichael H. Marijuana, alcohol, ED, and depression: epidemiologic correlations with BPH/LUTS. AUA. 2019;2019. [Google Scholar]
- 14.Nielsen S, Germanos R, Weier M, Pollard J, Degenhardt L, Hall W, et al. The use of cannabis and cannabinoids in treating symptoms of multiple sclerosis: a systematic review of reviews. Curr Neurol Neurosci Rep. 2018;18(2):8. [DOI] [PubMed] [Google Scholar]
- 15.Freeman RM, Adekanmi O, Waterfield MR, Waterfield AE, Wright D, Zajicek J. The effect of cannabis on urge incontinence in patients with multiple sclerosis: a multicentre, randomised placebo-controlled trial (CAMS-LUTS). Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(6):636–41. [DOI] [PubMed] [Google Scholar]
- 16.Brady CM, DasGupta R, Dalton C, Wiseman OJ, Berkley KJ, Fowler CJ. An open-label pilot study of cannabis-based extracts for bladder dysfunction in advanced multiple sclerosis. Mult Scler. 2004;10(4):425–33. [DOI] [PubMed] [Google Scholar]
- 17.Consroe P, Musty R, Rein J, Tillery W, Pertwee R. The perceived effects of smoked cannabis on patients with multiple sclerosis. Eur Neurol. 1997;38(1):44–8. [DOI] [PubMed] [Google Scholar]
- 18.Tackett BWD. The history of marijuana: learn about the origin of marijuana. In: Thomas S, ed. Recovery.org: American Addiction Centers; 2019. https://www.recovery.org/marijuana/history/. April 2020 [Google Scholar]
- 19.Black N, Stockings E, Campbell G, Tran LT, Zagic D, Hall WD, et al. Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(12):995–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.WB OS. On the preparations of the Indian Hemp, or Gunjah: Cannabis indica their effects on the animal system in health, and their utility in the treatment of tetanus and other convulsive diseases. Prov Med J Retrosp Med Sci. 1843;5:363–9. [PMC free article] [PubMed] [Google Scholar]
- 21.Zou S, Kumar U. Cannabinoid receptors and the endocannabinoid system: signaling and function in the central nervous system. Int J Mol Sci. 2018;19(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.••.Gratzke C, Streng T, Stief CG, et al. Effects of cannabinor, a novel selective cannabinoid 2 receptor agonist, on bladder function in normal rats. Eur Urol. 2010;57(6):1093–100. [DOI] [PubMed] [Google Scholar]; A key animal model result showing impact on voiding.
- 23.Dmitrieva NBK. Contrasting effects of WIN 55212–2 on motility of the rat bladder and uterus. J Neurosci. 2002;22(16):7147–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hiragata S, Ogawa T, Hayashi Y, Tyagi P, Seki S, Nishizawa O, et al. Effects of IP-751, ajulemic acid, on bladder overactivity induced by bladder irritation in rats. Urology. 2007;70(1):202–8. [DOI] [PubMed] [Google Scholar]
- 25.Wang ZY, Wang P, Bjorling DE. Treatment with a cannabinoid receptor 2 agonist decreases severity of established cystitis. J Urol. 2014;191(4):1153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bjorling DE, Wang ZY. Potential of endocannabinoids to control bladder pain. Front Syst Neurosci. 2018;12:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nedumaran B, Rudra P, Gaydos J, et al. Impact of regular cannabis use on biomarkers of lower urinary tract function. Urology. 2017;109:223 e229–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.•.Fantus RJ, Riedinger CB, Chang C, Helfand BT. The association between tetrahydrocannabinol and lower urinary tract symptoms utilizing the National Health and Nutrition Examination Survey. Urology. 2019;123:120–5. [DOI] [PubMed] [Google Scholar]; Report of associations in humans, key initial data on this topic.
- 29.Lloyd GL, Carmichael H. Marijuana, alcohol, ED and depression: epidemiologic correlations with BPH/LUTS. AUA 2019; 2019; Chicago. [Google Scholar]
- 30.Mauro PM SD, Hasin D, Sarvet AL, Rahim-Juwel R, Brown Q, Carliner H, Wall M, Martins SS. Age differences in adult past-year marijuana use and risk perceptions in the U.S., 2002–2013. Drug Alcohol Dependence. 2017;171:e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shahani R, Streutker C, Dickson B, Stewart RJ. Ketamine-associated ulcerative cystitis: a new clinical entity. Urology. 2007;69(5):810–2. [DOI] [PubMed] [Google Scholar]
- 32.Koppel BS, Brust JC, Fife T, et al. Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the guideline development Subcommittee of the American Academy of Neurology. Neurology. 2014;82(17):1556–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72(3):227–36. [DOI] [PubMed] [Google Scholar]
- 34.Association AP. Diagnostic and statistical manual of mental disorders: diagnostic and statistical manual of mental disorders. Vol 5. Fifth ed. Arlington: American Psychiatric Association; 2013. [Google Scholar]
- 35.Lee YI, Kim JW, Bae SR, Paick SH, Kim KW, Kim HG, et al. Effect of urgency symptoms on the risk of depression in community-dwelling elderly men. Korean J Urol. 2013;54(11): 762–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martin S, Vincent A, Taylor AW, Atlantis E, Jenkins A, Januszewski A, et al. Lower urinary tract symptoms, depression, anxiety and systemic inflammatory factors in men: a population-based cohort study. PLoS One. 2015;10(10):e0137903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koh JS, Ko HJ, Wang SM, Cho KJ, Kim JC, Lee SJ, et al. The relationship between depression, anxiety, somatization, personality and symptoms of lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Psychiatry Investig. 2015;12(2):268–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Breyer BN, Shindel AW, Erickson BA, Blaschko SD, Steers WD, Rosen RC. The association of depression, anxiety and nocturia: a systematic review. J Urol. 2013;190(3):953–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ou MJ, Huang CC, Wang YC, Chen YL, Ho CH, Wu MP, et al. Depression is a major risk factor for the development of dementia in people with lower urinary tract symptoms: a nationwide population-based study. PLoS One. 2019;14(6):e0217984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim TH, Han DH, Ryu DS, Lee KS. The impact of lower urinary tract symptoms on quality of life, work productivity, depressive symptoms, and sexuality in Korean men aged 40 years and older: a population-based survey. Int Neurourol J. 2015;19(2):120–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jeong SM, Suh B, Jang SH, Jin HS, Kim N, Kwon H, et al. Depression and its severity are strongly associated with both storage and voiding lower urinary tract symptoms independently of prostate volume. J Korean Med Sci. 2015;30(11):1646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Breyer BN, Kenfield SA, Blaschko SD, Erickson BA. The association of lower urinary tract symptoms, depression and suicidal ideation: data from the 2005–2006 and 2007–2008 National Health and Nutrition Examination Survey. J Urol. 2014;191(5):1333–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang CY, Chiu KM, Chung SD, Keller JJ, Huang CC, Lin HC. Increased risk of depressive disorder following the diagnosis of benign prostatic enlargement: one-year follow-up study. J Affect Disord. 2011;135(1–3):395–9. [DOI] [PubMed] [Google Scholar]
- 44.Dunphy C, Laor L, Te A, Kaplan S, Chughtai B. Relationship between depression and lower urinary tract symptoms secondary to benign prostatic hyperplasia. Rev Urol. 2015;17(2):51–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chung RY, Leung JC, Chan DC, Woo J, Wong CK, Wong SY. Lower urinary tract symptoms (LUTS) as a risk factor for depressive symptoms in elderly men: results from a large prospective study in southern Chinese men. PLoS One. 2013;8(9):e76017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Agrawal A, Nelson EC, Bucholz KK, Tillman R, Grucza RA, Statham DJ, et al. Major depressive disorder, suicidal thoughts and behaviours, and cannabis involvement in discordant twins: a retrospective cohort study. Lancet Psychiatry. 2017;4(9):706–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Volkow ND, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;371(9):879. [DOI] [PubMed] [Google Scholar]
- 48.Silins EHL, Patton GC, et al. Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry. 2014;1(4): 286–93. [DOI] [PubMed] [Google Scholar]
- 49.Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76(4):426–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gilman JM, Kuster JK, Lee S, Lee MJ, Kim BW, Makris N, et al. Cannabis use is quantitatively associated with nucleus accumbens and amygdala abnormalities in young adult recreational users. J Neurosci. 2014;34(16):5529–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bambico FR, Nguyen NT, Katz N, Gobbi G. Chronic exposure to cannabinoids during adolescence but not during adulthood impairs emotional behaviour and monoaminergic neurotransmission. Neurobiol Dis. 2010;37(3):641–55. [DOI] [PubMed] [Google Scholar]
- 52.Hill MN, Campolongo P, Yehuda R, Patel S. Integrating endocannabinoid signaling and cannabinoids into the biology and treatment of posttraumatic stress disorder. Neuropsychopharmacology. 2018;43(1):80–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marchant J Placebos: honest fakery. Nature. 2016;535(7611):S14–5. [DOI] [PubMed] [Google Scholar]
- 54.Dutkiewicz S, Skawinski D, Duda W, Duda M. Assessing the influence of benign prostatic hyperplasia (BPH) on erectile dysfunction (ED) among patients in Poland. Cent European J Urol. 2012;65(3):135–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yafi FA, Jenkins L, Albersen M, Corona G, Isidori AM, Goldfarb S, et al. Erectile dysfunction. Nat Rev Dis Primers. 2016;2:16003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Impotence: NIH Consensus Development Panel on Impotence. JAMA. 1993;270(1):83–90. [PubMed] [Google Scholar]
- 57.Ende J Organic impotence. In: rd, Walker HK, hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. Boston: 1990. [PubMed] [Google Scholar]
- 58.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151(1):54–61. [DOI] [PubMed] [Google Scholar]
- 59.Glina S, Glina FP. Pathogenic mechanisms linking benign prostatic hyperplasia, lower urinary tract symptoms and erectile dysfunction. Ther Adv Urol. 2013;5(4):211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li MK, Garcia L, Patron N, Moh LC, Sundram M, Leungwattanakij S, et al. An Asian multinational prospective observational registry of patients with benign prostatic hyperplasia, with a focus on comorbidities, lower urinary tract symptoms and sexual function. BJU Int. 2008;101(2):197–202. [DOI] [PubMed] [Google Scholar]
- 61.Braun MH, Sommer F, Haupt G, Mathers MJ, Reifenrath B, Engelmann UH. Lower urinary tract symptoms and erectile dysfunction: co-morbidity or typical “aging male” symptoms? Results of the “Cologne Male Survey”. Eur Urol. 2003;44(5):588–94. [DOI] [PubMed] [Google Scholar]
- 62.Rosen RC, Giuliano F, Carson CC. Sexual dysfunction and lower urinary tract symptoms (LUTS) associated with benign prostatic hyperplasia (BPH). Eur Urol. 2005;47(6):824–37. [DOI] [PubMed] [Google Scholar]
- 63.Rosen RC, Wei JT, Althof SE, Seftel AD, Miner M, Perelman MA, et al. Association of sexual dysfunction with lower urinary tract symptoms of BPH and BPH medical therapies: results from the BPH Registry. Urology. 2009;73(3):562–6. [DOI] [PubMed] [Google Scholar]
- 64.Shridharani AN, Brant WO. The treatment of erectile dysfunction in patients with neurogenic disease. Transl Androl Urol. 2016;5(1): 88–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kaya C, Uslu Z, Karaman I. Is endothelial function impaired in erectile dysfunction patients? Int J Impot Res. 2006;18(1):55–60. [DOI] [PubMed] [Google Scholar]
- 66.Billups KL. Erectile dysfunction as an early sign of cardiovascular disease. Int J Impot Res. 2005;17(Suppl 1):S19–24. [DOI] [PubMed] [Google Scholar]
- 67.Hughes FM Jr, Hill HM, Wood CM, et al. The NLRP3 inflammasome mediates inflammation produced by bladder outlet obstruction. J Urol. 2016;195(5):1598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gacci M, Andersson KE, Chapple C, Maggi M, Mirone V, Oelke M, et al. Latest evidence on the use of phosphodiesterase type 5 inhibitors for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. Eur Urol. 2016;70(1):124–33. [DOI] [PubMed] [Google Scholar]
- 69.Carliner H, Brown QL, Sarvet AL, Hasin DS. Cannabis use, attitudes, and legal status in the U.S.: a review. Prev Med. 2017;104: 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.•.Shamloul R, Bella AJ. Impact of cannabis use on male sexual health. J Sex Med. 2011;8(4):971–5. [DOI] [PubMed] [Google Scholar]; Important data for public health and clinical care.
- 71.Argiolas A, Melis MR. Central control of penile erection: role of the paraventricular nucleus of the hypothalamus. Prog Neurobiol. 2005;76(1):1–21. [DOI] [PubMed] [Google Scholar]
- 72.Gratzke C, Christ GJ, Stief CG, Andersson KE, Hedlund P. Localization and function of cannabinoid receptors in the corpus cavernosum: basis for modulation of nitric oxide synthase nerve activity. Eur Urol. 2010;57(2):342–8. [DOI] [PubMed] [Google Scholar]
- 73.Melis MR, Succu S, Mascia MS, Sanna F, Melis T, Castelli MP, et al. The cannabinoid receptor antagonist SR-141716A induces penile erection in male rats: involvement of paraventricular glutamic acid and nitric oxide. Neuropharmacology. 2006;50(2): 219–28. [DOI] [PubMed] [Google Scholar]
- 74.Pizzol D, Demurtas J, Stubbs B, Soysal P, Mason C, Isik AT, et al. Relationship between cannabis use and erectile dysfunction: a systematic review and meta-analysis. Am J Mens Health. 2019;13(6): 1557988319892464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.•.De Nunzio C, Roehrborn CG, Andersson KE, McVary KT. Erectile dysfunction and lower urinary tract symptoms. Eur Urol Focus. 2017;3(4–5):352–63. [DOI] [PubMed] [Google Scholar]; Excellent review of this topic.


