Abstract
Background
Daily attending rounds (AR) are a cornerstone of teaching and patient care in academic health centers. Interruptions in health care are common and can cause increased risk of errors, incomplete work, and decreased decision-making accuracy. Interruptions to AR may diminish a trainee's capacity to learn and retain information.
Objective
We characterized and quantified interruptions that occur during AR.
Methods
We used a mixed-methods design combining a prospective observational study with a qualitative study. AR were observed January to March 2020 to characterize interruptions, followed by semi-structured interviews with the observed physicians to elucidate the effect of interruptions on workflow and the educational value of rounds.
Results
There were 378 observed interruptions over the course of 30 AR sessions, averaging 12.6 (range 1–22, median 13) interruptions per rounding session. Bedside nursing staff was the most common source of interruptions (25%) and consultant recommendations was the most common topic of interruption (21%). Most interruptions occurred during patient presentations (76%), and the most common method of interaction was text message (24%). Most team members described negative effects of interruptions, including loss of focus and missing critical clinical information; some also reported that certain interruptions had positive effects on education and clinical care. Interns were more likely to report negative emotional reactions to interruptions.
Conclusions
AR are frequently interrupted for non-urgent topics by a variety of methods and sources. Negative effects included loss of focus, missed information, and increased stress. Proactive communication, particularly between physicians and nurses, was suggested to reduce interruptions.
Objectives
To characterize interruptions to attending physician rounds and evaluate their effect on medical education.
Findings
Interruptions to attending physician rounds are common and from a variety of sources; physicians identified negative impacts such as loss of focus, missing critical information, and increased stress.
Limitations
This study was performed at a single academic medical center with unique technological, operational, and cultural factors.
Bottom Line
While prior studies have shown the effects of interruptions on safety, interruptions can also have negative consequences for medical education.
Introduction
Attending rounds (AR), a cornerstone of training in academic hospitals, is comprised of experienced physicians facilitating clinical discussions with the medical team for 2 main purposes: trainee education and patient care. Rounds are characterized by a senior physician teaching the medical team clinical decision-making, the physical examination, pathophysiology, and high-value care in the context of their patients.1 This critical time is often the primary means by which the attending physician interfaces with the internal medicine team. AR has been an integral part of medical education for over a century; therefore, many studies have sought to refine and adapt AR in an increasingly complex health care environment.2–7 Interruptions to AR are common and can pose challenges to the educational experience of trainees.3,4
In workplace literature, Jett and George define interruptions as “incidents or occurrences that impede or delay organizational members as they attempt to make progress on work tasks.”8 In order to accommodate interruptions, physicians often employ task switching, which occurs when the interrupted person stops their current task, engages with a new task, and then subsequently returns to the initial task.9,10 It is well known that task switching can degrade performance and increase the rate of errors,9–13 but it also increases cognitive load and therefore can interfere with learning.14–16 Classroom investigators have shown that text messaging during lectures degrades recall and learning, and that frequent interruptions can disrupt encoding of new material into long-term memory.17,18 It follows that interruptions could have a similarly detrimental impact on the educational mission of AR. To date, there is limited literature detailing the effect of interruptions on the educational goal of rounds. Physicians have expressed minimizing interruptions as a goal to improve AR3,4; however, how these interruptions affect education and the characteristics of the interruptions (frequency, sources, time consumed by interruptions) were not explored. Ly and colleagues found that pages to ward residents increased trainee frustration and were frequently non-urgent; however, the many other modes of interruptions, or how page communication may have affected AR, were not studied.19
Interruptions in health care are inevitable and common,20 but the characteristics and impact of interruptions to the educational mission of attending rounds are not fully understood.21,22 In this study, we aimed to (1) characterize and quantify interruptions to attending rounds on an academic medicine service, and (2) understand the impact of interruptions on the medical team members.
Methods
Setting and Participants
This mixed-methods prospective observational study was conducted at the Veteran Affairs Palo Alto Health Care System (VAPAHCS), which serves approximately 85 000 veterans across 10 outpatient locations. The acute care hospital is a level 3 facility affiliated with Stanford University. The medicine service covers 3 medical-surgical floors and 1 intermediate (step-down) intensive care unit (IICU), totaling approximately 90 inpatient acute beds. Five medicine teams (teams A–E) rotate through a 5-day call cycle, where days 1 and 4 are “on call.” During days on call, the medicine teams receive handoffs of overnight admissions and new admissions from 7:00 am to 7:00 pm. Prior to attending rounds, each team meets with an interdisciplinary group during a preassigned 10-minute slot, starting with team A and ending with team E. Data collection for the quantitative portion of the study occurred over a continuous 6-week period between January and March 2020. The qualitative portion of the study occurred in April 2020. Our Institutional Review Board determined this study exempt from human subjects' review.
Quantitative Data Collection and Analysis
Attending rounds began when the attending physician met the team after the daily interdisciplinary meeting and ended when the attending physician left the team. An interruption was defined as communication from any person who was not part of the rounding team, which typically included an attending, resident, 2 interns, and a medical student. During some portions of rounds, the team also included a pharmacist, pharmacy student, bedside nurse, and a case manager. If any of these members were physically present with the team, their communication was not counted as an interruption. Medicine teams provided verbal consent to be observed, and observations were scheduled using a random number generator. An average of 5 observations occurred weekly during weekdays.
Three physician scribes (J.A., J.S., N.A.) acquired data utilizing an observation tool (provided as online supplementary data), which outlined strict definitions of the data collected for each interruption. Interrater agreement was tested for each of the 3 scribes prior to the observation period to ensure that data collection was performed consistently.23 This entailed training each scribe to use the tool, observing attending rounds in pairs, and comparing data from the observations. The scribes continued training on the tool until the interrater agreement reached ≥ 90%, after which the collection of study data began with a single scribe per rounding session. The data collected for each interruption included the person being interrupted; the activity they were performing; if they were at bedside; the source, topic, and urgency of the interruption; the method of contact; and the time needed to address the interruption. The tool defined urgency in terms of how quickly a response was required, with 4 categories: emergent, urgent, routine, or personal (Table 1). If the content or source of the interruption was not obvious by observation alone, the scribe clarified with that team member immediately after rounds were completed. Team census, acuity, day of the week, and day of the call cycle were also recorded for each rounding observation.
Table 1.
Interruption Urgency
| Urgency | Definition | Examples | Frequency, n (%) |
| Routine | Change in patient status or information not requiring attention within 1 hour |
|
302 (80) |
| Urgent | Change in patient status or information requiring attention within 1 hour |
|
18 (5) |
| Emergent | Change in patient status requiring immediate attention |
|
12 (3) |
| Personal | Non-work-related interruption |
|
46 (12) |
Note: N = 378 total interruptions (over 30 attending rounds observations). Details about personal interruptions were not obtained due to privacy.
Statistical Considerations
Summary statistics were used to describe the data numerically. We used means, standard deviations, medians, and ranges to describe continuous variables, and frequencies and proportions to describe categorical variables. Barplots were used to describe the data graphically. Linear regression methods were used to assess attending round characteristics as predictors of the number of interruptions. Potential risk factors for the number of interruptions included round length, patient census, number of IICU patients, team, day of the week, and day of the call cycle. To assess the association between attending round characteristics and number of interruptions, univariate analyses were initially performed using linear regression. Variables that were statistically significant (P < .05) at the univariate level were reassessed in a multiple linear regression model. Stepwise linear regression was used to create the final predictive model. The data were analyzed using the R software for statistical computing.24
Qualitative Data Collection and Analysis
Using an explanatory sequential design, we supplemented quantitative findings with qualitative data collected from semi-structured interviews with physicians (interview script provided as online supplementary data). Interview questions were designed to obtain a fuller understanding of providers' experiences and how the interruptions impact team members. All 52 physicians observed for the quantitative phase of this study were invited to participate in a one-on-one interview. Physicians were approached via phone or email, with a follow-up call or email in cases with no response. The research team sought to obtain a sample of at least 50% from each physician group (intern, resident, attending). Interviews lasted approximately 15 minutes and were conducted via video conferencing by one member of the research team (C.T.). With consent, interviews were digitally recorded and later transcribed.
A content analytic approach was used to analyze qualitative findings.25 Key components of interview transcripts were distilled into a matrix that allowed for identification of patterns across interviews.26 Next, interview responses were sorted into categories inductively from the transcripts, allowing for the frequency of different response types to be noted, a feature of content analysis approaches. For example, responses were categorized into 2 views of interruptions: generally negative versus a mixed perspective. Members of the qualitative team (C.T., N.A., C.G.) individually reviewed all transcripts, identified potential categories for analysis, and then agreed on final data categories using a process of “negotiated agreement.”27 Quotes were sorted into categories (by C.T.) with checks (performed by C.G. and N.A.) to ensure consistent coding and reliability. Finally, team members looked across interviews to identify discernible patterns and areas where interview participants' perspectives coalesced and diverged.
Results
Characteristics of Interruptions
Thirty attending rounds were observed over the 6-week period, with a total of 378 interruptions over 3757 minutes. Fifty-two physicians were observed: 26 interns, 10 residents, and 16 attendings. Characteristics of attending rounds are shown in Table 2.
Table 2.
Attending Round Characteristics
| Characteristic | Average | SD (Range) |
| Number of interruptions | 12.6 | 4.9 (1–22) |
| Team census | 10.9 | 2.6 (4–16) |
| Intermediate intensive care census | 2.1 | 1.5 (0–5) |
| Round length, minutes | 125 | 28 (59–182) |
| Day of call cycle | n (%) | |
| 1 | 8 (27) | |
| 2 | 5 (17) | |
| 3 | 4 (13) | |
| 4 | 4 (13) | |
| 5 | 9 (30) | |
| Day of week | n (%) | |
| Monday | 7 (23) | |
| Tuesday | 7 (23) | |
| Wednesday | 7 (23) | |
| Thursday | 4 (13) | |
| Friday | 5 (17) | |
Note: N = 30 observations of attending rounds.
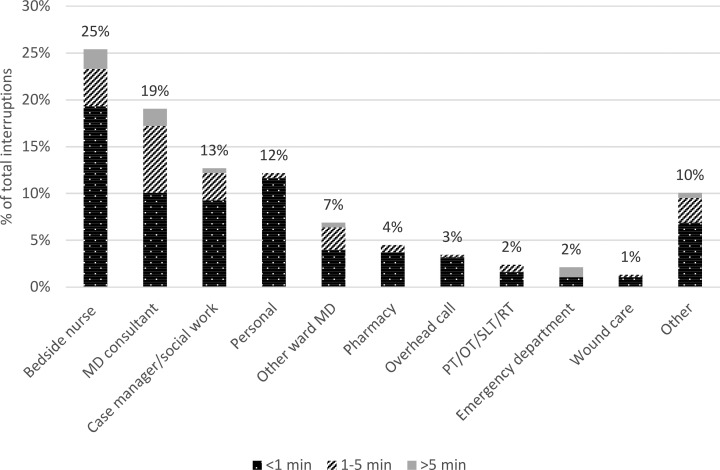
Characteristics of interruptions are shown in Table 3. The most common source of interruptions was bedside nursing, with most interruptions lasting less than 1 minute (Figure). Consultant interruptions were the most common interruptions lasting longer than a minute. Most interruptions were of routine urgency (Table 1).
Table 3.
Characteristics of Interruptions
| Characteristic | n (%) |
| Who was interrupted | |
| Intern | 136 (36) |
| Resident | 107 (28) |
| Attending | 46 (12) |
| Team | 89 (24) |
| Topic of interruption | |
| Consult | 81 (21) |
| Discharge planning | 66 (18) |
| Clarification/request for an order | 64 (17) |
| Personal | 46 (12) |
| Change in patient status | 44 (12) |
| New admission | 19 (5) |
| Administrative | 13 (3) |
| Misdirected | 7 (2) |
| Abnormal test result | 6 (2) |
| Other | 32 (9) |
| Method of interruption | |
| Text message | 92 (24) |
| Face-to-face | 85 (23) |
| Pager | 83 (22) |
| Vocera | 41 (11) |
| Phone call | 36 (10) |
| Instant message | 24 (6) |
| Overhead | 14 (4) |
| Other | 3 (1) |
| Length of interruption | |
| < 1 minute | 271 (72) |
| 1–5 minutes | 82 (22) |
| > 5 minutes | 25 (7) |
| Activity being interrupted | |
| Presenting/discussing patient | 287 (76) |
| At bedside | 61 (16) |
| Teaching | 6 (2) |
| In EHR, entering orders | 5 (1) |
| In EHR, not entering orders | 5 (1) |
| Other | 14 (4) |
| Location when interrupted | |
| Table rounding | 200 (53) |
| Walk rounding | 178 (47) |
Abbreviation: EHR, electronic health record.
Note: N = 378 total interruptions (over 30 attending rounds observations). Overhead calls included announcements for codes and rapid response teams. Emergent included calling a code or rapid response team and urgent included critical lab results. Text messages were received on physician personal phones. Vocera is a closed-loop hands-free wearable communication device. Instant message was done via Skype on desktop computer. Presenting/discussing patient included walking between patient rooms. Teaching included only didactics separate from discussion of patient.
Figure.
Source and Length of Interruptions
Abbreviations: PT, physical therapy; OT, occupational therapy; SLT, speech and language therapy; RT, respiratory therapy.
Note: 378 total interruptions; overhead calls include announcements for codes and rapid response teams.
In univariate analysis, patient census, round length, team B, and team E were significant independent predictors of the number of interruptions (Table 4a). With each additional patient on the census, the number of interruptions increased by approximately 1 (coef = 0.98, SE = 0.31, P = .003). With each 10-minute increase in the round length, there were on average 0.8 additional interruptions (coef = 0.08, SE = 0.02, P = .013). Team E had on average 7.25 fewer numbers of interruptions than the other teams (coef = -7.25, SE = 1.84, P = .0005). Team B had on average 4.42 more interruptions than the other teams (coef = -4.42, SE = 2.14, P = .048).
Table 4a.
Univariate Analyses of Attending Round Characteristics as Predictors of the Number of Interruptions
| Characteristic | Coefficient | 95% CI | P Value |
| Round length | 0.08 | 0.02, 0.14 | .013 |
| Team census | 0.98 | 0.38, 1.59 | .003 |
| IICU census | -0.90 | -2.11, 0.31 | .16 |
| Team A | 0.67 | -3.82, 5.16 | .77 |
| Team B | 4.42 | 0.23, 8.60 | .048 |
| Team C | -0.58 | -5.07, 3.90 | .80 |
| Team D | 2.75 | -1.63, 7.13 | .23 |
| Team E | -7.25 | -10.9, -3.65 | .0005 |
| Monday | 0.54 | -3.70, 4.78 | .80 |
| Tuesday | 1.84 | -2.35, 6.04 | .40 |
| Wednesday | 1.66 | -2.55, 5.86 | .45 |
| Thursday | -3.23 | -8.38, 1.92 | .23 |
| Friday | -2.52 | -7.25, 2.21 | .30 |
| 1st day of call cycle | 1.64 | -2.38, 5.66 | .43 |
| 2nd day of call cycle | -1.80 | -6.58, 2.98 | .47 |
| 3rd day of call cycle | 0.23 | -5.06, 5.52 | .93 |
| 4th day of call cycle | 3.40 | -1.73, 8.54 | .20 |
| 5th day of call cycle | -2.33 | -6.15, 1.49 | .24 |
Note: Team census is the total number of patients on team that day; IICU census is the number of intermediate (step-down) intensive care unit patients on team that day.
A multivariate analysis was then performed to identify a set of predictive variables. When included in the full multiple regression model, round length and team B were no longer significant predictors of interruptions, likely due to small sample size (Table 4b). The final model, obtained using stepwise regression, identified census and team E as being significantly associated with the number of interruptions (Table 4c).
Table 4b.
Multivariate Analyses of Attending Round Characteristics as Predictors of the Number of Interruptions
| Characteristic | Coefficient | 95% CI | P Value |
| Round length | 0.01 | -0.05, 0.07 | .72 |
| Census | 0.56 | -0.12, 1.24 | .12 |
| Team B | 1.49 | -2.28, 5.25 | .45 |
| Team E | -5.40 | -9.28, -1.51 | .012 |
Table 4c.
Multivariate Analyses of Attending Round Characteristics as Predictors of the Number of Interruptions after Stepwise Linear Regression
| Characteristic | Coefficient | 95% CI | P Value |
| Census | 0.70 | 0.15, 1.24 | .019 |
| Team E | -5.86 | -9.34, -2.38 | .003 |
Physician Interviews
Twenty-eight of 52 (54%) physicians participated in the interviews. Fifty-two percent of interns (13 of 25), 70% of residents (7 of 10), and 50% of attending physicians (8 of 16) were interviewed. For analysis purposes, the 5 interview questions were grouped into the 3 main discussion points below.
Impact of Interruptions on Attending Rounds:
Most interviewees (71%, 20 of 28) reported being negatively impacted by interruptions, while the remaining interviewees (29%, 8 of 28) stated that their experience with interruptions was both positive and negative. A majority also indicated that these interruptions impacted education (79%, 22 of 28). Interviewees described 4 main ways that interruptions negatively impacted attending rounds. These included (1) loss of focus; (2) missing critical clinical information; (3) creating downstream constraints on time; and (4) increased stress. Many physicians noted how interruptions diverted their attention away from their current task and that returning to that task required significant effort:
“When I get an interruption or a page, it can throw off my train of thought, and I find myself every once in a while not presenting problems that I wanted to talk about, and they do not get addressed.” (Intern 15)
Furthermore, because these interruptions refocused their attention, they missed key learning opportunities during rounds. Additionally, they described missing key components of patient care plans due to interruptions. For example, residents recalled instances of physically abandoning rounds to manage a request from an interruption, resulting in missed teaching sessions and patient care discussions. Lastly, interviewees stated that interruptions led to prolonged rounding, which may lead to further time constraints:
“The more interruptions you have, the longer rounds take, and the longer the rounds take, the less time there is for teaching. You feel more rushed during rounds, and that detracts from the time that the team sort of wants to devote to teaching.” (Resident 6)
Consequently, the educational component of rounds was sometimes not prioritized in favor of timely completion of rounds. The experience of being interrupted affected physicians emotionally, with junior physicians bearing a disproportionate burden of stress in our sample. There were 24 occurrences of “frustration,” “annoying,” “stress,” and “exhaustion” by interns (n = 13) compared to just 5 occurrences by residents and attending physicians (n = 15).
“…it is that exhaustion that really ends up depleting my energy, so I have less mental room to take in more educational things.” (Intern 2)
“…when you have a busy list, you're just getting paged nonstop during rounds. It's miserable.” (Resident 4, recalling being an intern on this rotation)
Despite the negative impact of interruptions, interviewees reported that some interruptions were constructive. Teams welcomed interruptions that addressed urgent patient care issues or offered learning opportunities:
“Interruptions in which we are given additional information about the patient—I would say the benefit of those outweighs any negative of the disruption.” (Attending 16)
Consultant interruptions were cited as having positive effects on both patient care and education.
Estimates and Predictions of Interruption Frequency and Their Sources:
Interviewees were asked to estimate the average number of interruptions to rounds and to identify the main sources of those interruptions. Compared to the quantitative results of this study, 43% (12 of 28) of interviewees overestimated the average number of interruptions, 36% (10 of 28) underestimated, and 21% (6 of 28) accurately predicted them. When interns overestimated, the emotional toll of the interruptions often followed:
“…it's fewer than I expected. I think maybe I'm just attributing the stress that is associated with each interruption and increasing the number in my mind. It can just get so overwhelming when you want to focus on something and can't.” (Intern 15)
Seventy-one percent of interviewees accurately predicted nursing as the largest source of interruptions, while the remaining 29% (8 of 28) predicted case management to be the largest source. Interviewees were provided with results from the quantitative portion of our study and asked to reflect on these findings, particularly when their perception of reality did not match what the data captured. Interviewees were generally not surprised by the average number of interruptions, but they were surprised by the range of the number of interruptions.
Recommendations to Improve Attending Rounds:
Recommendations included standardizing when and how to communicate with physicians, dedicated check-in times with interdisciplinary staff, and preemptive communication with interdisciplinary staff. Standardization of communication involved several sub-themes, including timing of interruptions, prioritizing information, batching communications, and utilizing the most appropriate communication method. Suggestions for standardization involved other disciplines changing their communication practices:
“..making it clear to nurses, case managers, and pharmacists that most medicine teams are going to round between the hours of 9 and 11, and during that time try to limit texts and pages to things that are actually time sensitive.” (Resident 6)
“I appreciate the nurses who are cognizant of when rounds typically happen and try to save non-urgent pages for later…instead of getting multiple pages for one patient asking about bowel regimen…you get those non-emergent requests at once.” (Intern 2)
“…something we are lacking is having a more consistent protocol for how to reach out for different levels of need, whether that's paging, vocera [closed-loop hands-free device], or in-person.” (Resident 9)
In contrast, when discussing check-in times and preemptive communication, physicians at all levels (interns, residents, attendings) provided examples of how changing their own behaviors may result in fewer interruptions. These ideas came in the form of personal experience and role modeling:
“Each team needs to work within themselves to optimize the flow. Like preemptively reaching out to nurses about major changes in the plan…” (Attending 13)
“…I would just meet with my case manager and social worker independently from the [interdisciplinary team meeting] and just tell them the patient plans for the day and what we needed. I did this either after rounds or right before. That can be helpful because they would only interrupt for critical communications.” (Resident 10)
“…there is a sweet spot from consulting early so that they get back to you before attending rounds…” (Intern 14)
Creating the expectation of face-to-face communication between the physicians and nurse at the bedside was a theme that appeared across multiple interviews:
“…trying to get better myself to page the nurse, ‘Hey we are rounding. Join us for rounds…we want to hear your input.' I feel sometimes people page a lot because they feel that they are not being heard, and I understand that.” (Intern 19)
Discussion
Our mixed-methods study found that AR are frequently interrupted by a variety of sources and methods, and physicians felt these interruptions often detracted from the educational mission of AR. Teams experienced an average 12.6 interruptions per AR session (range 1–22, median 13), averaging one interruption every 10 minutes. Nursing staff was the primary source of interruptions, but consultant recommendations also comprised a significant portion of interruptions and lasted longer than other sources. Higher team census was associated with more interruptions, and team E experienced fewer interruptions than other teams. While physicians identified some positive effects on education and streamlining patient care, the detrimental effects of interruptions dominated: loss of focus, missing information, increased time constraints, and heightened stress.
Ly and colleagues examined characteristics of pages to residents during business hours to a variety of services (surgical and medical), and also found nursing to be the primary source.19 However, paging comprised just 22% of all interruptions in our study, highlighting the need to identify and address additional methods of interruptions. Consultants comprised just 3% of pages, compared with 19% of interruptions in our study; this difference may be due to the time of observations (business hours vs AR) and cohort (variety of specialties vs medicine ward physicians). Urgent interruptions were rare in our data, consistent with prior data in the emergency department and inpatient wards.19,28 Despite the generally accepted notion of AR as trainee education, our study found that interruptions occurred at similar rates as the fast-paced emergency department setting.10,28,29
While the association of increased census with more interruptions is intuitive, interestingly, team E experienced fewer interruptions, even after adjusting for other variables (Table 4). In the morning schedule, team E is the last to attend interdisciplinary rounds, resulting in a later start of AR. This extra time could be leveraged for pre-rounding communication. It is also possible that team E more commonly utilized other communication behaviors recommended by interviewees, such as including nurses in bedside rounds and earlier consultant contact. Our data did not capture provider or team behaviors outside of AR, which may be helpful to identify additional variables impacting interruptions.
As noted by one resident, “not all interruptions are created equally,” correlating with past work where the positive impact of interruptions that facilitated exchange of critical information outweighed the negative impacts of task switching.8 While some physicians felt urgent interruptions or those that provided forward movement of daily work were positive, the negative impact predominated in our interviews. Many described a loss of focus and missing complex ideas, such as principles of patient management. This effect is consistent with classroom research which showed that frequent interruptions disrupted encoding content into long term memory.17,18 Loss of focus and inability to concentrate overlaps with patient safety literature; however, unlike nursing medication pass or physician order writing, errors in the AR context are often cognitive and may be more difficult to identify.
Team members cited increased stress and frustration when interrupted. Previous studies have also shown negative emotional reactions to pages19 and increased stress when asked to respond to communication about patients other than the one currently in their care.28 Our study suggests that interns may be particularly vulnerable to these negative emotional reactions and warrant special consideration in future interventions. Physicians at all levels referenced behaviors to “protect” or “offload” interns to manage interruptions; one physician suggested a designated team communicator, which was a successful strategy in a recent ICU study.30 Thus, more experienced physicians may be able to assist junior physicians during AR to maximize early trainee education, minimize cognitive load, and improve emotional well-being.
The theme of physicians initiating proactive communication, especially closed loop rather than unidirectional, emerged from solicitation of recommendations to decrease interruptions to AR. The recommendation to increase bedside rounds, specifically to include the nurse, is not novel, but interestingly standardizing AR to ensure such practices has had mixed results in trainee satisfaction and perception of teaching.2,7,31 Increasing bedside rounds, with the explicit goal to reduce interruptions, may improve trainee buy-in for standardizing AR.
There are several limitations to our findings. First, this was a single center observational study with cultural, equipment-related, and staffing factors unique to our institution. Secondly, the data was obtained by observers rather than video recording or other more reliable methods of data collection, resulting in possible differences in interpretation or missed interruptions. Thirdly, sampling error could have influenced our data. We used a random number generator to dictate which teams were observed each day, and factored census, day of call cycle, day of the week, and acuity into our data analysis. While the study description was not discussed during data collection, there may have been changes in behavior due to the observer's presence.
Our study finds that interruptions are common and impact the educational value of AR. To investigate this area further, our findings support identifying systems-based, multidisciplinary interventions to optimize communication of critical information while decreasing the frequency of nonurgent interruptions. The heightened negative emotional impact of interruptions on interns suggests that future interventions should pay particular focus to junior physicians. Lastly, physician descriptions of missing important information raise concerns for patient safety; therefore, more work is needed to understand the impact of AR interruptions on clinical errors.
Conclusions
Attending rounds are frequently interrupted for non-urgent topics by a variety of methods and sources. Physicians commonly identified negative effects of interruptions, including loss of focus, missed information, and increased stress. Our study suggests interruptions could be reduced by proactive communication, particularly with nursing, who were the most common interruption source.
Supplementary Material
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
The views expressed in this article are those of the authors and not necessarily those of the Department of Veterans Affairs.
This study was previously presented as an abstract and poster at the Stanford Quality Improvement & Patient Safety Symposium, May 18, 2020, and the Geriatric Research Education and Clinical Center Symposium, Palo Alto, California, June 16, 2020.
References
- 1.Stickrath C, Noble M, Prochazka A, et al. Attending rounds in the current era: what is and is not happening. JAMA Intern Med. 2013;173(12):1084–1089. doi: 10.1001/jamainternmed.2013.6041. [DOI] [PubMed] [Google Scholar]
- 2.Monash B, Najafi N, Mourad M, et al. Standardized attending rounds to improve the patient experience: a pragmatic cluster randomized controlled trial. J Hosp Med. 2017;12(3):143–149. doi: 10.12788/jhm.2694. [DOI] [PubMed] [Google Scholar]
- 3.Najafi N, Monash B, Mourad M, et al. Improving attending rounds: qualitative reflections from multidisciplinary providers. Hosp Pract. 2015;43(3):186–190. doi: 10.1080/21548331.2015.1043181. [DOI] [PubMed] [Google Scholar]
- 4.Roy B, Castiglioni A, Kraemer RR, et al. Using cognitive mapping to define key domains for successful attending rounds. J Gen Intern Med. 2012;27(11):1492–1498. doi: 10.1007/s11606-012-2121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonzalo JD, Masters PA, Simons RJ, Chuang CH. Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach Learn Med. 2009;21(2):105–110. doi: 10.1080/10401330902791156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chand DV. Observational study using the tools of lean six sigma to improve the efficiency of the resident rounding process. J Grad Med Educ. 2011;3(2):144–150. doi: 10.4300/JGME-D-10-00116.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calderon AS, Blackmore CC, Williams BL, et al. Transforming ward rounds through rounding-in-flow. J Grad Med Educ. 2014;6(4):750–755. doi: 10.4300/JGME-D-13-00324.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jett QR, George JM. Work interrupted: a closer look at the role of interruptions in organizational life. Acad Manage Rev. 2003;28(3):494–507. doi: 10.5465/amr.2003.10196791. [DOI] [Google Scholar]
- 9.Skaugset LM, Farrell S, Carney M, et al. Can you multitask? Evidence and limitations of task switching and multitasking in emergency medicine. Ann Emerg Med. 2016;68(2):189–195. doi: 10.1016/j.annemergmed.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 10.Westbrook JI, Raban MZ, Walter SR, Douglas H. Task errors by emergency physicians are associated with interruptions, multitasking, fatigue and working memory capacity: a prospective, direct observation study. BMJ Qual Saf. 2018;27(8):655–663. doi: 10.1136/bmjqs-2017-007333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall LM, Ferguson-Pare M, Peter E, et al. Going blank: factors contributing to interruptions to nurses' work and related outcomes. J Nurs Manag. 2010;18(8):1040–1047. doi: 10.1111/j.1365-2834.2010.01166.x. [DOI] [PubMed] [Google Scholar]
- 12.Monteiro SD, Sherbino JD, Ilgen JS, et al. Disrupting diagnostic reasoning: do interruptions, instructions, and experience affect the diagnostic accuracy and response time of residents and emergency physicians? Acad Med. 2015;90(4):511–517. doi: 10.1097/ACM.0000000000000614. [DOI] [PubMed] [Google Scholar]
- 13.Dadlez NM, Azzarone G, Sinnett MJ, et al. Ordering interruptions in a tertiary care center: a prospective observational study. Hosp Pediatr. 2017;7(3):134–139. doi: 10.1542/hpeds.2016-0127. [DOI] [PubMed] [Google Scholar]
- 14.Young JQ, Van Merrienboer J, Durning S, ten Cate O. Cognitive Load Theory: implications for medical education: AMEE Guide No. 86. Med Teach. 2014;36(5):371–384. doi: 10.3109/0142159X.2014.889290. [DOI] [PubMed] [Google Scholar]
- 15.Atkinson RC, Shiffrin R. Human memory: a proposed system and its control processes. In: Spence K, Spence J, editors. The Psychology of Learning and Motivation. New York, NY: Academic Press; 1968. pp. 89–195. [Google Scholar]
- 16.Salvucci DD, Taatgen NA. Toward a unified view of cognitive control. Top Cogn Sci. 2011;3(2):227–230. doi: 10.1111/j.1756-8765.2011.01134.x. [DOI] [PubMed] [Google Scholar]
- 17.Rosen LD, Lim AF, Carrier L, Cheever M. An empirical examination of the educational impact of text message-induced task switching in the classroom: educational implications and strategies to enhance learning. Educ Psychol. 2011;17(2):163–177. doi: 10.5093/ed2011v17n2a4. [DOI] [Google Scholar]
- 18.Oulasvirta A, Saariluoma P. Surviving task interruptions: investigating the implications of long-term working memory theory. Int J Hum Comput Stud. 2006;64(10):941–961. doi: 10.1016/j.ijhcs.2006.04.006. [DOI] [Google Scholar]
- 19.Ly T, Korb-Wells CS, Sumpton D, Russo RR, Barnsley L. Nature and impact of interruptions on clinical workflow of medical residents in the inpatient setting. J Grad Med Educ. 2013;5(2):232–237. doi: 10.4300/JGME-D-12-00040.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Westbrook JI. Interruptions to clinical work: how frequent is too frequent? J Grad Med Educ. 2013;5(2):337–339. doi: 10.4300/JGME-D-13-00076.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas I, Nicol L, Regan L, et al. Driven to distraction: a prospective controlled study of a simulated ward round experience to improve patient safety teaching for medical students. BMJ Qual Saf. 2019;24(2):154–161. doi: 10.1136/bmjqs-2014-003272. [DOI] [PubMed] [Google Scholar]
- 22.Fargen KM, O'Connor T, Raymond S, Sporrer JM, Friedman WA. An observational study of hospital paging practices and workflow interruption among on-call junior neurological surgery residents. J Grad Med Educ. 2012;4(4):467–471. doi: 10.4300/JGME-D-11-00306.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fleiss J. Statistical Methods for Rates and Proportions 3rd ed. Hoboken, NJ: John Wiley & Sons Inc; 2003. [Google Scholar]
- 24.The R Foundation. The R Project for statistical Computing. 2021 https://www.R-project.org/ Accessed February 17.
- 25.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 26.Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12(6):855–866. doi: 10.1177/104973230201200611. [DOI] [PubMed] [Google Scholar]
- 27.Campbell JL, Quincy C, Osserman J, Pedersen OK. Coding in-depth semistructured interviews: problems of unitization and intercoder reliability and agreement. Sociol Method Res. 2013;42(3):294–320. doi: 10.1177/0049124113500475. [DOI] [Google Scholar]
- 28.Weigl M, Beck J, Wehler M, Schneider A. Workflow interruptions and stress atwork: a mixed-methods study among physicians and nurses of a multidisciplinary emergency department. BMJ Open. 2017;7(12):e019074. doi: 10.1136/bmjopen-2017-019074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneider A, Williams DJ, Kalynych C, Wehler M, Weigl M. Physicians' and nurses' work time allocation and workflow interruptions in emergency departments: a comparative time-motion study across two countries. 2020] doi: 10.1136/emermed-2019-208508. [published online ahead of print August 5. Emerg Med J doi: [DOI] [PubMed]
- 30.Hascall RL, Perkins RS, Kmiecik L, et al. PAs reduce rounding interruptions in the pediatric intensive care unit. JAAPA. 2019;31(6):41–45. doi: 10.1097/01.JAA.0000533661.80449.da. [DOI] [PubMed] [Google Scholar]
- 31.Sandhu A, Amin H, McLaughlin K, Lockyer J. Leading educationally effective family-centered bedside rounds. J Grad Med Educ. 2013;5(4):594–599. doi: 10.4300/JGME-D-13-00036.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.