Abstract
Purpose
Food insecure cancer patients experience worse health outcomes and poorer quality of life than food secure patients. There has been little research in programs to alleviate food insecurity in cancer patients. The objective of this paper is to report on the food purchasing behaviors of cancer patients enrolled in a supplemental food voucher program.
Methods
This paper utilized data from a three-arm randomized controlled trial investigating the impact of food interventions on alleviating food insecurity in cancer patients receiving chemotherapy and/or radiation therapy. In one arm, patients received a monthly $230 voucher with which to purchase food. Receipts were collected for items purchased with the voucher and were coded to analyze purchasing behaviors.
Results
33 patients provided receipts for more than 11,000 individual items. Patients spent 50% of voucher funds on animal protein, fruits, and vegetables. Patients spent, on average, 77% of voucher funds on items categorized as “healthy”.
Conclusions
Patients who received a food voucher purchased more fruits and vegetables than national averages would suggest. They also spent less on sweetened beverages than national samples. Patients who were born outside of the US or who were limited English proficient purchased significantly more healthy foods than English-speaking and American-born study patients. Supplemental food vouchers for food insecure cancer patients resulted in the purchase of healthy food items.
Keywords: Food insecurity, cancer, supplemental nutrition, quality of life
INTRODUCTION
Food insecurity, which impacts more than one in ten American households and almost one in five households in New York City, is defined as lacking adequate food for a healthy and active lifestyle [4, 15]. In adults, food insecurity is associated with poor diet and nutritional intake, and with an increased risk of physical and mental health conditions such as cancer, diabetes, and depression [12, 14, 20, 22]. Food insecure households are constrained by financial, geographic, and logistical barriers that often result in the purchase of inexpensive, calorie-dense foods [1, 29, 35]. Food insecure households typically purchase more refined grains, foods with added fats and sugars, and unhealthy snacks than their economically advantaged counterparts [7].
Food insecurity is concentrated in minority and immigrant communities. Black and Hispanic households have more than double the rates of food insecurity compared to white households [4]. Immigrants with authorized status to live in the United States may have quadruple the national rate of food insecurity as white households, with limited English proficient individuals at more risk for being food insecure [3]. Current additional food resources, such as the Supplemental Nutrition Assistance Program (SNAP) and local food banks, are often not adequate to meet the food security needs of underserved, immigrant, and limited English proficient populations [9, 25]. The situation is often worse for mixed-status and unauthorized status immigrant households, as unauthorized persons are ineligible for SNAP and, because of fears of deportation and public charge status, often do not utilize other food assistance programs they may be able to access [34].
Food insecurity is also more prevalent in populations with chronic diseases, including cancer [26]. Food insecurity increases the risk of chronic conditions, but the relationship is bidirectional: chronic conditions increase the risk of food insecurity [30]. For cancer patients, the financial toxicity imposed by the cost of treatment, loss of employment, and underemployment create and exacerbate food insecurity [5, 10]. Financial hardships in cancer treatment are especially prevalent in minorities and immigrants. A study with minority patients at safety net cancer clinics in New York City (NYC) found that 60% of patients were food insecure, more than three times the NYC average [9].
Cancer patients are at increased risk for malnutrition, weight loss, and other nutrition-related side effects during their cancer treatment [18, 28]. It is important that, during treatment, patients have access to foods that provide adequate calories and nutrients, but that are also palatable to patients who may be suffering from nausea, constipation, anxiety and other treatment side effects that make it difficult to eat.
Despite the pressing need, there has been very little research on interventions to improve food security in underserved minority and immigrant cancer patients, and their impact on cancer outcomes. Previous studies have examined interventions to improve food security and nutritional intake among a general population of food insecure individuals. One randomized controlled trial implemented among food insecure individuals who were SNAP eligible, but not currently receiving SNAP benefits, analyzed the effect of financial restrictions and incentives on food purchases [8]. The study randomized participants so that some participants received discounts on fresh fruits and vegetables, others had to pay more for sugar sweetened beverages (SSBs), others had both the produce incentive and SSB restriction, and others had no conditions. Data for that study were collected via participant grocery receipts, which allowed researchers to categorize and analyze each item purchased by a participant. Findings suggested that the food purchasing behavior of food insecure households could be improved via financial incentives and restrictions. To date, no studies have analyzed food purchases of food insecure individuals with a chronic condition, such as cancer. Likewise, no studies have examined how providing funds to purchase food to individuals with a chronic disease impacts purchasing behavior in the absence of any restrictions or incentives.
This paper examines the food voucher purchasing behavior of food insecure, predominantly immigrant and minority cancer patients, without any stipulations on what types of food could be purchased with the voucher.
METHODS
Design and Sample
This is a nested cohort study of patients enrolled in the Food Insecurity Intervention Pilot Project Randomized Controlled Trial (FIIPP RCT). This three-arm study compared the impact of Hospital-based Food Pantries, Food Vouchers + Hospital-based Food Pantries, and Grocery Home Delivery + Hospital-based Food Pantries on cancer treatment completion, quality of life, food security, and nutritional status among immigrant and minority cancer patients with food insecurity. This paper focuses on data collected from the Food Voucher arm. The Food Voucher arm provided patients with a debit card credited with $230 each month to purchase food. This project received IRB approval from Memorial Sloan Kettering Cancer Center and from each study site.
Patients were recruited from four different cancer clinics in New York City, one each in the boroughs of Brooklyn, Queens, Manhattan, and the Bronx. The sites were chosen to optimize the geographic and socioeconomic diversity of study participants. The four study sites serve neighborhoods with higher levels of poverty, food insecurity, and cancer-related deaths than New York City as a whole.
Eligibility criteria for the study included being within two weeks of starting radiation therapy or within one month of starting chemotherapy. Patients also had to be 18 years of age or older, able to answer survey questions in English or in Spanish, and living independently, and had to score in the range of ‘low’ or ‘very low’ food security on the USDA Household Food Security Screener [33]. Patients who received or were in the process of applying for SNAP benefits were ineligible for participation.
Procedure
Patients were recruited for the study through the Integrated Cancer Care Access Network (ICCAN), described elsewhere, a program which utilizes Access Facilitators to connect recently diagnosed underserved cancer patients with non-medical resources [10]. ICCAN Access Facilitators approached patients whose preliminary eligibility (age and treatment for cancer) was determined through their electronic medical records. Interested patients were referred to research staff to complete the USDA Household Food Security Screener. Food insecure patients who were interested in enrolling completed written informed consent into the FIIPP RCT with research staff.
In the Food Voucher intervention, each patient received a debit card specifically created for this program. The debit card was restricted so that patients could not purchase items such as cigarettes or alcoholic beverages, or get cash back, however they could use the debit card to purchase any other beverages or food. Each month for the duration of study participation (6 months), the debit card was credited with $230 and given to the patient. Participants were instructed to use these cards only for food purchases and were reminded to use their vouchers for healthful foods. Patients received usual and customary nutrition counseling provided by their sites of care. Patients brought their receipts in each month and the receipt data were recorded. Receipts were only collected for purchases made with the voucher.
Measures
Upon enrollment into the FOOD RCT, patients completed an intake survey with research staff. The intake consisted of basic demographic and cancer history questions, and validated instruments, including the USDA Household Food Security Screener. Validated instruments were validated in all study languages. Patients also completed two follow-up surveys, one at 3 months and one at 6 months. In addition to remeasuring variables taken at baseline, the follow-up surveys also included a qualitative feedback instrument.
In addition to the capture of patient reported data across the RCT, in the Voucher arm, data from the patients’ grocery receipts were entered into a spreadsheet that contained the following fields: date of purchase, grocery items purchased, grocery items’ prices, and the store location, if available. Each food item was then coded by type of food by two research staff, using a codebook that was developed based on the Bureau of Labor Statistics (BLS) 2016 Consumer Expenditures Report and the USDA Food Pattern Categories [2, 31]. Each food item went through a multi-stepped coding process. After the name of each item was transcribed from the receipt to a spreadsheet, each item was coded into a series of broader categories: beans/nuts, eggs/healthy dairy (milk and yogurt), processed dairy (cheese, ice cream, flavored milks), oils/fats, fruits, vegetables, grains, processed salty foods, processed sweet foods, animal protein, sweet beverages, healthy beverages (e.g., water, seltzer, unsweetened tea), and cooking staples. Items were coded as either “healthy” or “non-healthy,” based on USDA food guidelines [32]. Whole foods, such as animal protein, fresh fruits and vegetables, and eggs, along with other items, such as bread, canned vegetables and beans, milk, and yogurt, were coded as “healthy.” The “non-healthy” category included processed meats, processed dairy, sweetened drinks, salty and sweet snacks, and ready to eat meals.
Statistical Analysis
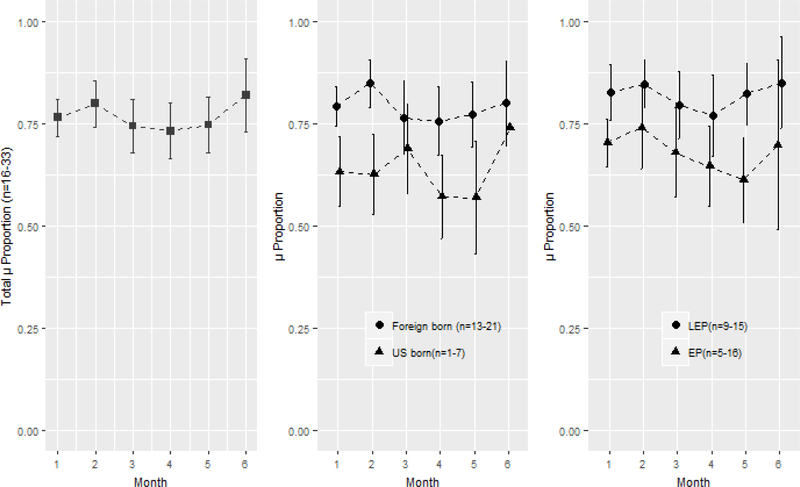
All analyses were conducted using SPSS version 22 and R software [16, 24]. The patients’ mean purchase of (1) each of the 13 broad food categories above, and (2) healthy food items per month, were plotted with a 95% confidence interval (CI). The mean proportion of healthy food items purchased, was also examined by the patients’ birth region (U.S., foreign-born) and English proficiency (EP, LEP).
The Generalized Estimation Equation (GEE) was used to fit repeated observations of the proportion of healthy food items purchased across the 6-month period based on the patients’ birth region and English proficiency. An exchangeable correlation structure specification was used because the measurements were equally spaced, on a monthly basis, and the data were balanced, excluding missing values due to attrition.
RESULTS
Thirty three out of 37 patients provided grocery receipts for a total of 11,106 individual items. One patient dropped out of the study and three patients did not return any receipts. Table 1 shows receipt provision by the 33 patients who returned at least one month’s worth of receipts. At month 1, all 33 patients returned their receipts to study staff. At month 6, 16 patients (48%) returned receipts.
Table 1.
Patients Returning Receipts by Month
| Month | N (%) |
|---|---|
| 1 | 33 (100%) |
| 2 | 31 (94%) |
| 3 | 29 (88%) |
| 4 | 27 (82%) |
| 5 | 26 (78%) |
| 6 | 16 (48%) |
The demographic and medical characteristics reported by patients during study enrollment are shown in Table 2. Sixty percent of patients were female. Patients identified as Black/African American (38%), Hispanic/Latino (34%), Asian, (15%), and White (13%). Thirty-six percent of patients were born in the Caribbean, 27% in Latin America, 21% in the United States, 9% in Africa, and 6% in Eastern Europe. A majority of patients preferred English (63%), with 37% preferring Spanish.
Table 2.
Sample Characteristics (n=33)
| Characteristics | N (%) / μ (SD)* | Range |
|---|---|---|
| Age¥ | 55.73 (10.97) | 36.10–83.36 |
| Gender¥ | ||
| Male | 13 (39.39%) | |
| Female | 20 (60.61%) | |
| Race¥ | ||
| White | 4 (12.50%) | |
| Black | 12 (37.50%) | |
| Asian | 5 (15.62%) | |
| Other | 11 (34.38%) | |
| Ethnicity¥ | ||
| Hispanic/Latino | 13 (40.62%) | |
| Non-Hispanic/Latino | 19 (59.94%) | |
| Household Size¥ | 3.06 (1.85) | 1.00–10.00 |
| Children under 18† | ||
| Yes | 4 (21.05%) | |
| No | 15 (78.95%) | |
| Marital status | ||
| Married/partnered | 15 (45.45%) | |
| Divorced | 2 (6.06%) | |
| Separated | 1 (3.03%) | |
| Widowed | 1 (3.03%) | |
| Single | 14 (42.42%) | |
| Educational Attainment¥ | ||
| 3rd–5th grade | 5 (15.62%) | |
| 6th–8th grade | 8 (25.00%) | |
| 9th–11th grade | 3 (9.38%) | |
| High school graduate | 9 (28.12%) | |
| Some college/more | 7 (21.88%) | |
| English Proficiency | ||
| English Proficient | 17 (53.13%) | |
| Limited English Proficient | 15 (46.87%) | |
| Language Preference¥ | ||
| English | 19 (63.33%) | |
| Spanish | 11 (33.67%) | |
| Country of Origin£ | ||
| United States | 7 (21.21%) | |
| Latin America | 14 (42.42%) | |
| Caribbean | 7 (21.21%) | |
| Africa | 2 (6.06%) | |
| Eastern Europe | 2 (6.06%) | |
| Employment Status¥ | ||
| Full-time | 2 (6.25%) | |
| Part-time | 1 (3.12%) | |
| Retired | 5 (15.62%) | |
| Student | 1 (3.12%) | |
| Unemployed | 21 (65.62%) | |
| Other | 2 (6.25%) | |
| Cancer Diagnosis¥ | ||
| Breast | 14 (45.16%) | |
| Gynecological (Cervical, Endometrial, Ovarian) | 4 (12.91%) | |
| Prostate | 3 (9.68%) | |
| Lymphoma | 3 (9.68%) | |
| Other | 7 (22.3%) | |
| Treatment Modality | ||
| Chemotherapy | 15 (45.45%) | |
| Radiation Therapy | 15 (45.45%) | |
| Chemotherapy and Radiation Therapy | 3 (9.09%) | |
| Insurance Type£ | ||
| Emergency Medicaid | 12 (46.15%) | |
| Medicaid - HMO | 8 (30.77%) | |
| Medicaid [fee for service / Medicaid only] | 2 (7.69%) | |
| Medicare | 1 (3.85%) | |
| Medicaid and Medicare | 1 (3.85%) | |
| Private HMO | 2 (7.69%) | |
The average age of patients was 56 years (range 36–83). Average household size was three people (range 1–10). Four households (12%) had children under the age of 18, three households had one child and one household had two children. Sixteen percent of patients had between 3–5 years of education, 25% between 6 and 8 years, 9% between 9 and 11 years, 28% graduated from high school, and 22% of patients had at least some college education. Most patients, (66%) were unemployed, 15% were retired, 9% were employed, and 3% were students.
Almost all patients (87%) had health insurance: 40% had Medicaid for the Treatment of an Emergency Medical Condition, 27% had Medicaid, and 20% had some other type of insurance. Breast cancer was the most common diagnosis (45%), followed by gynecologic cancers (13%), prostate (10%), and blood cancers (10%). Six other diagnoses accounted for the remaining 22% of patient diagnoses. Upon study enrollment, 45% of patients were receiving chemotherapy, 45% were receiving radiation therapy, and 10% were receiving both radiation therapy and chemotherapy.
Food category purchases
Table 3 summarizes the monthly food and beverage expenditures for items that were purchased with the voucher. Across all 6 months of the study, patients spent the largest portion of the voucher money on animal protein (22% of voucher money), fruits (15%), and vegetables (13%). Those three categories accounted for 50% of all the voucher funds used by patients. Patients also purchased grains (8% of voucher money), processed salty foods (7%), eggs/healthy dairy (7%), processed dairy (5%), healthy beverages (5%), processed sweet foods (5%), fats/oils (4%), sweetened beverages (4%), cooking staples (3%), and beans/nuts (2%) with the voucher money.
Table 3.
Mean proportion of food items purchased per month
|
Month μ (SD)* |
Total μ (SD)* |
||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 1–6 | |
| Beans/Nuts | 2.80% (3.67%) | 1.74% (2.62%) | 2.91% (3.36%) | 2.49% (4.11%) | 1.87% (2.69%) | 2.38% (2.59%) | 2.37% (3.26%) |
| Cooking Staples | 2.96% (3.34%) | 4.06% (6.16%) | 3.20% (3.83%) | 3.05% (3.43%) | 2.78% (3.62%) | 2.07% (1.86%) | 3.11% (4.05%) |
| Fats and Oils | 3.40% (3.65%) | 2.93% (3.63%) | 3.74% (3.74%) | 3.58% (6.67%) | 5.03% (3.98%) | 4.11% (8.25%) | 3.73% (4.89%) |
| Processed Sweets | 3.62% (4.40%) | 3.88% (3.82%) | 5.19% (6.71%) | 5.75% (6.46%) | 5.00% (5.13%) | 2.86% (3.91%) | 4.45% (5.25%) |
| Sweet Beverage | 4.09% (5.70%) | 3.47% (5.48%) | 4.30% (8.00%) | 3.78% (4.68%) | 3.61% (5.69%) | 1.15% (2.42%) | 3.59% (5.75%) |
| Healthy Beverages | 4.98% (5.83%) | 5.65% (9.03%) | 5.70% (8.37%) | 5.02% (8.95%) | 7.21% (10.24%) | 5.74% (7.44%) | 5.68% (8.31%) |
| Processed Dairy | 5.00% (5.06%) | 3.30% (3.91%) | 3.94% (4.14%) | 6.09% (4.80%) | 4.49% (4.31%) | 4.20% (4.12%) | 4.51% (4.47%) |
| Eggs/Healthy Dairy | 6.54% (5.28%) | 7.01% (7.58%) | 5.33% (5.63%) | 6.51% (5.81%) | 7.19% (6.62%) | 10.33% (10.73%) | 6.89% (6.81%) |
| Processed Salts | 7.41% (8.76%) | 6.56% (7.35%) | 8.49% (7.91%) | 7.63% (7.60%) | 7.19% (8.80%) | 5.69% (9.39%) | 7.27% (8.15%) |
| Grains | 7.67% (5.31%) | 8.43% (8.11%) | 8.13% (6.03%) | 10.23% (6.29%) | 7.94% (5.19%) | 9.41% (8.58%) | 8.54% (6.51%) |
| Vegetable | 12.75% (8.99%) | 14.96% (12.83%) | 13.34% (11.84%) | 9.90% (8.25%) | 11.88% (7.24%) | 12.77% (8.05%) | 12.67% (9.94%) |
| Fruit | 16.49% (11.17%) | 18.15% (10.40%) | 14.14% (11.69%) | 15.41% (10.56%) | 13.14% (9.72%) | 14.03% (12.47%) | 15.43% (10.9%) |
| Protein | 22.30% (14.49%) | 19.85% (15.03%) | 21.61% (15.06%) | 20.56% (15.68%) | 22.67% (17.09%) | 25.26% (17.15%) | 21.77% (15.43%) |
μ (SD): Mean and standard deviation
Figure 1 provides an overview of the portion of voucher funds that patients spent on food categorized as “healthy” across all six months of the study. On average, during each month of the study, 77% of voucher funds were spent on food in the “healthy” category. That category comprised foods coded as protein, fruits, vegetables, grains, eggs/healthy dairy, cooking staples, and beans/nuts. Conversely, 23% of funds were spent on unhealthy foods, which consisted of processed salty foods, processed dairy, processed sweet foods, fats/oils, and sweetened beverages.
Figure 1.
Plot μ proportion of health food items purchased (95% confidence interval)
Figure 1 also compares the proportion of voucher funds spent on healthy foods among LEP patients and non-LEP patients, and by foreign-born and US-born patients. Patients with limited English proficiency, on average, purchased a bigger proportion of healthy foods than their English-speaking peers (P=.01). Patients born outside of the United States also purchased significantly more healthy foods than US-born patients (P=.001).
DISCUSSION
This paper describes the food purchasing behavior of 33 food insecure cancer patients enrolled in the Food Insecurity Intervention Pilot Project RCT over a six-month period. Patients purchased a variety of foods and proportionately spent more on what was categorized as healthy items; fruits, vegetables, proteins, grains, and low-fat dairy. The receipts collected from patients in the FIIPP RCT showed that the participants used less of their voucher funds on sugary drinks, refined sweets and snacks, and processed meats and dairy compared to published national averages and to data collected from low-income households that receive SNAP funds [2, 11].
This study is the first to examine the food purchasing behaviors of low-income cancer patients who are given supplemental grocery funds. Other studies have observed how low-income households use their food dollars but not in a population with a specific chronic condition. Likewise, no previous studies have observed how food insecure patients with a chronic disease respond to supplemental food programs. The USDA publishes reports on the average food expenditures of SNAP (low-income) households but does not focus on populations with chronic diseases. Findings from this study make a much-needed contribution to the scholarship around food insecurity and chronic conditions. The more we understand about the food purchasing behaviors of low-income and food insecure cancer patients, the better we can tailor supplemental food services to address unmet needs in this vulnerable population. The findings suggest that in providing funds for food purchases, the FOOD RCT has provided patients with the capacity to purchase healthy, wholesome foods.
At month 6, during the qualitative feedback survey, 70% of patients reported that they ate most, or all the food purchased themselves. This patient feedback provides evidence that a majority of the food being purchased was being consumed specifically by the cancer patient, rather than by family, friends, or other household members. This study was not designed to capture changes in patients’ dietary intake, but patient feedback suggests that food funds given to cancer patients have a direct impact on the foods those patients consume.
One area of interest in this trial was sugar-sweetened beverages. Others have previously highlighted the deleterious impacts of sweetened beverages on health, especially among low-income and minority populations [13, 21]. This paper adds to the literature around sweetened beverages in medically underserved communities. According to the USDA, SNAP-households spend 9% of their SNAP and non-SNAP food funds on sweetened beverages, and non-SNAP households spend 7% of funds on sweetened beverages [11]. Across all six months, FIIPP RCT patients never spent more than 4% of their voucher funds on sweetened beverages, although it is unknown if they had spent other grocery money on such beverages and other unhealthy items.
Poor health is significantly associated with low fruit and vegetable intake [27]. The findings showed higher than average proportions of funds spent on fruits and vegetables. According to the USDA, SNAP households spend about 12% of their SNAP and non-SNAP dollars on fruits and vegetables. Non-SNAP households spend slightly more (16%). On average, voucher recipients spent more than 25% of their voucher funds on fruits and vegetables.
The results also show a negligible change over time in purchasing behaviors. Over the course of the 6-month study period, patients, on average, spent their money in a consistent way. One might expect purchasing patterns to change over time to reflect changing symptoms, or the extinguishing of healthful behaviors, but that was not observed in the sample.
We also saw no significant changes in BMI during the course of the study. Because many patients are advised to maintain their weight during treatment, BMI was not something the study aimed to promote.
It is interesting to note the impact of English proficiency and foreign-born status on the distribution of healthy versus non-healthy food purchases. Patients with limited English proficiency spent statistically significantly more of their funds on food categorized as healthy. Limited English proficiency is associated with a range of adverse health care outcomes, such as miscommunication with the provider and later cancer detection compared with English speaking populations [6, 17]. Limited English proficiency is also associated with food insecurity. However, in this sample, LEP patients spent significantly less on unhealthy items. A similar phenomenon was observed when comparing patients born outside of the US with patients born in the United States. Patients born outside of the US spent more of their funds on food categorized as healthy. These observations may support research that has shown that as immigrants acculturate to American diets, they increase their fat intake and decrease fruit and vegetable intake [23]. Acculturation to Western diets has also been associated with increased consumption of sugar-sweetened beverages and high-calorie convenience foods [19]. LEP patients and immigrants may have better food purchasing behaviors, focusing on whole, fresh foods, rather than the highly processed and refined foods that make up a larger portion of the average Americans’ diet. These salutary habits should be reinforced. Providers and nutrition educators should leverage the existing food purchasing behaviors and patterns of LEP patients, which show more of an inclination towards “healthy” foods.
This study has several limitations. It did not track food or beverages purchased with funds other than the voucher funds. It is possible that participants used the voucher to supplement unhealthy diets with healthy items that were accessible with the voucher. This study is also limited by a lack of data about food purchasing behavior before patients received the voucher. It is not possible to associate the supplementary food funds with changes in food purchasing behavior. Also, there was no assessment to see if these healthy purchasing habits carried over past study completion. Additionally, food preparation measures, which impact the nutrition qualities of foods, were not measured. However, the data do show that during the study period, patients largely purchased healthy, whole foods, rather than processed items. Future studies should aim for a baseline assessment of grocery purchasing behavior, post-study receipt collection, and include patient-reported information about cooking methods.
Another limitation is that these findings may be skewed by medical factors that were not captured at baseline or during follow-up. Providers may have recommended a high-fat diet, or encouraged patients to drink ginger ale, for example, for nausea. These may have come across in the analysis as “unhealthy” foods, even though they were consumed at the direction of a medical specialist. Another limitation was a decreased rate of receipt provision as the study progressed. From months 1 to 5, more than 75% of study participants returned their receipts at the end of the month. However, at the final time point (month 6), less than half of the participants returned receipts. The precipitous drop-off is likely related to the fact that during the final receipt collection, patients did not receive a new voucher and were less incentivized to meet with study staff. However, across the study, incomplete receipt collection may have biased the results.
A final limitation is the severe economic constraints faced by many patients in this study. High rates of unemployment and unmet social needs made this group of cancer patients particularly vulnerable. Results from this trial may not be applicable to other patient populations with fewer barriers to healthy food purchasing.
The Food Voucher arm of the FIIPP RCT study has provided important information on the food purchasing behaviors of food insecure cancer patients who are given a food voucher. It has also provided insights for future research and community programming activities. The results have shown that food insecure cancer patients make relatively good nutrition choices with funds given to spend on food. Importantly, patients spent less on sugary drinks and more on fruits and vegetables than national trends would suggest. Less than a quarter of purchases were spent on unhealthy items. To improve upon this, interventions aimed at food insecure and chronically ill patients should incorporate ongoing culturally and linguistically responsive nutrition education and counselling that is delivered in the context of a limited food budget, that can, hopefully, in the future be combined with food dollar supplementation.
Acknowledgments
This study was supported by National Cancer Institute P30 CA008748 Core Cancer Center Support Grant; National Cancer Institute R01 CA230446 FOOD (Food to Overcome Outcomes Disparities); National Cancer Institute U54 CA137788 08 the CCNY/MSKCC Partnership for Cancer Research Training & Community Outreach; Laurie Tisch Illumination Fund; New York Community Trust; New York City Council; AVON Foundation; Devika R. Jutagir was supported by T32 CA009461.
Footnotes
Compliance with Ethical Standards
Conflict of Interest
To the best of our knowledge, no conflict of interest, financial or other, exists for any of the authors.
This project received IRB approval from Memorial Sloan Kettering Cancer Center and from each study site. Informed consent was obtained from all individual participants included in the study.
We have full control of all primary data and agree to allow the journal to review our data if requested.
REFERENCES
- 1.Beaulac J, Kristjansson E, Cummins S (2009) A systematic review of food deserts, 1966–2007 J Preventing chronic disease 6 [PMC free article] [PubMed] [Google Scholar]
- 2.Bureau of Labor Statistics (2016) Composition of consumer unit: Annual expenditure means, shares, standard errors, and coefficients of variation, Consumer Expenditure Survey. In: Editor (ed)^(eds) Book Composition of consumer unit: Annual expenditure means, shares, standard errors, and coefficients of variation, Consumer Expenditure Survey, City. [Google Scholar]
- 3.Chilton M, Black MM, Berkowitz C, Casey PH, Cook J, Cutts D, Jacobs RR, Heeren T, De Cuba SE, Coleman S (2009) Food insecurity and risk of poor health among US-born children of immigrants J American journal of public health 99: 556–562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A (2016) Household Food Security in the United States in 2015. In: Editor (ed)^(eds) Book Household Food Security in the United States in 2015. United States Department of Agriculture, City. [Google Scholar]
- 5.De Boer AG, Taskila T, Ojajärvi A, Van Dijk FJ, Verbeek JH (2009) Cancer survivors and unemployment: a meta-analysis and meta-regression Jama 301: 753–762 [DOI] [PubMed] [Google Scholar]
- 6.Divi C, Koss RG, Schmaltz SP, Loeb JM (2007) Language proficiency and adverse events in US hospitals: a pilot study J International for quality in health care 19: 60–67 [DOI] [PubMed] [Google Scholar]
- 7.Drewnowski A, Specter SE (2004) Poverty and obesity: the role of energy density and energy costs The American journal of clinical nutrition 79: 6–16 [DOI] [PubMed] [Google Scholar]
- 8.French SA, Rydell SA, Mitchell NR, Oakes JM, Elbel B, Harnack L (2017) Financial incentives and purchase restrictions in a food benefit program affect the types of foods and beverages purchased: results from a randomized trial International Journal of Behavioral Nutrition Physical Activity 14: 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gany F, Bari S, Crist M, Moran A, Rastogi N, Leng J (2013) Food insecurity: limitations of emergency food resources for our patients Journal of Urban Health 90: 552–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gany F, Ramirez J, Nierodzick ML, McNish T, Lobach I, Leng J (2011) Cancer portal project: a multidisciplinary approach to cancer care among Hispanic patients Journal of oncology practice 7: 31–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garansky S, Mbwana K, Romualdo A, Tenaglio A, Roy M (2016) Foods Typically Purchased by Supplemental Nutrition Assistance Program (SNAP) Households. In: Editor (ed)^(eds) Book Foods Typically Purchased by Supplemental Nutrition Assistance Program (SNAP) Households, City. [Google Scholar]
- 12.Gregory CA, Coleman-Jensen A (2017) Food insecurity, chronic disease, and health among working-age adults. In: Editor (ed)^(eds) Book Food insecurity, chronic disease, and health among working-age adults, City. [Google Scholar]
- 13.Han E, Powell LM (2013) Consumption patterns of sugar-sweetened beverages in the United States Journal of the Academy of Nutrition Dietetics 113: 43–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holben DH, Pheley AM (2006) Diabetes risk and obesity in food-insecure households in rural Appalachian Ohio J Preventing chronic disease 3 [PMC free article] [PubMed] [Google Scholar]
- 15.Hunger Free America (2016) The State of the Working Hungry: Low Wages Chief Cause of Malnutrition. In: Editor (ed)^(eds) Book The State of the Working Hungry: Low Wages Chief Cause of Malnutrition, City. [Google Scholar]
- 16.IBM Corp (2016) SPSS Statistics for Windows. In: Editor (ed)^(eds) Book SPSS Statistics for Windows, City. [Google Scholar]
- 17.Johnson-Kozlow M, Roussos S, Rovniak L, Hovell M (2009) Colorectal cancer test use among Californians of Mexican origin: influence of language barriers J Ethnicity disease 19: 315. [PMC free article] [PubMed] [Google Scholar]
- 18.Laky B, Janda M, Bauer J, Vavra C, Cleghorn G, Obermair A (2007) Malnutrition among gynaecological cancer patients European journal of clinical nutrition 61: 642. [DOI] [PubMed] [Google Scholar]
- 19.Lesser IA, Gasevic D, Lear SA (2014) The association between acculturation and dietary patterns of South Asian immigrants J PloS one 9: e88495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leung CW, Epel ES, Willett WC, Rimm EB, Laraia BA (2015) Household food insecurity is positively associated with depression among low-income supplemental nutrition assistance program participants and income-eligible nonparticipants The Journal of nutrition 145: 622–627 [DOI] [PubMed] [Google Scholar]
- 21.Malik VS, Popkin BM, Bray GA, Després J-P, Hu FB (2010) Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk J Circulation 121: 1356–1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin KS, Ferris AM (2007) Food insecurity and gender are risk factors for obesity J Nutr Educ Behav 39: 31–36 [DOI] [PubMed] [Google Scholar]
- 23.Neuhouser ML, Thompson B, Coronado GD, Solomon CC (2004) Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington State Journal of the American Dietetic Association 104: 51–57 [DOI] [PubMed] [Google Scholar]
- 24.R Development Core Team (2008) R: A language and environment for statistical computing. In: Editor (ed)^(eds) Book R: A language and environment for statistical computing. http://www.R-project.org,City. [Google Scholar]
- 25.Seligman HK, Laraia BA, Kushel MB (2009) Food insecurity is associated with chronic disease among low-income NHANES participants The Journal of nutrition 140: 304–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simmons LA, Modesitt SC, Brody AC, Leggin AB (2006) Food insecurity among cancer patients in Kentucky: a pilot study Journal of oncology practice 2: 274–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Slavin JL, Lloyd B (2012) Health benefits of fruits and vegetables J Advances in nutrition 3: 506–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stone P (2002) The measurement, causes and effective management of cancer-related fatigue International journal of palliative nursing 8: 120–128 [DOI] [PubMed] [Google Scholar]
- 29.Stuff JE, Casey PH, Szeto KL, Gossett JM, Robbins JM, Simpson PM, Connell C, Bogle ML (2004) Household food insecurity is associated with adult health status The Journal of nutrition 134: 2330–2335 [DOI] [PubMed] [Google Scholar]
- 30.Tarasuk V, Mitchell A, McLaren L, McIntyre L (2013) Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity The Journal of nutrition 143: 1785–1793 [DOI] [PubMed] [Google Scholar]
- 31.USDA (2015) USDA Food Patterns. In: Editor (ed)^(eds) Book USDA Food Patterns, City. [Google Scholar]
- 32.USDA (2015) USDA Food Patterns: Healthy U.S.-Style Eating Pattern
- 33.USDA ERS (2012) US household food security survey module: three stage design, with screeners. In: Editor (ed)^(eds) Book US household food security survey module: three stage design, with screeners, City. [Google Scholar]
- 34.Vargas ED, Pirog MA (2016) Mixed-status families and WIC uptake: The effects of risk of deportation on program use J Social science quarterly 97: 555–572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ver Ploeg M, Mancino L, Todd JE, Clay DM, Scharadin B (2015) Where do Americans usually shop for food and how do they travel to get there? Initial findings from the National Household Food Acquisition and Purchase Survey. In: Editor (ed)^(eds) Book Where do Americans usually shop for food and how do they travel to get there? Initial findings from the National Household Food Acquisition and Purchase Survey, City. [Google Scholar]