Abstract
Objective
Alien hand syndrome is a rare neurological disorder in which the patient makes seemingly purposeful movements of one hand, which are dissociated from any conscious intent. These abnormal movements are very annoying, and can be disabling, for the patient. There is no established effective treatment for alien hand syndrome.
Methods
Report of a case of a 61-year old man with frontal variant of alien hand syndrome following ischaemic stroke.
Results
During therapy, the patient unwittingly grabbed objects with his right hand and could not voluntarily release his grip. Multidisciplinary rehabilitation was started, with learning of compensation strategies and a focus on bimanual tasks. Follow-up after 5 months showed a major improvement in the Functional Index Measure (FIM) score, an improvement from 36 to 79 on 126 scored items.
CONCLUSION
It is important to recognize this rare syndrome because of its disabling character. Evidence about the best treatment for alien hand syndrome is scarce. There is an important role for specific exercises and patient education. During rehabilitation of the patient, most improvement occurred with bimanual tasks and different colours (black, white and other bright colours) to navigate the subject’s attention more to one side. Another exercise strategy was letting the alien hand catch a cube, after which the patient was able to perform more exercises with the other hand during one – handed training. In the current case, the alien hand syndrome resolved following specific and multidisciplinary rehabilitation.
LAY ABSTRACT
A 61-year-old man presented with specific difficulties after an ischaemic stroke. During rehabilitation for ischaemic stroke, he unwittingly grabbed objects with his right hand and could not voluntarily release his grip. His hand had become an “alien hand”, which he could no longer control voluntarily. This is a very disabling condition for the patient (and his family) and treatment options are limited. It is therefore important to draw attention to this condition and share learning in order to improve rehabilitation techniques.
Key words: alien hand syndrome, rare syndrome, case report, rehabilitation
Alien hand syndrome (AHS) is a rare neurological disorder, characterized by seemingly intentional, but involuntary, limb movements. The patient has no control over the movements. In normal circumstances we do not question ownership over our own body or limbs, nor do we reflect on the experience of initiating and controlling actions (1). Patients with AHS have a sense of loss of ownership of their limb. Common causes are neurodegenerative diseases, but AHS can also occur after stroke or neurosurgical operations (2, 3). Onset of AHS is usually subacute, as seen with neurodegenerative disorders. Yet, a sudden onset can occur after stroke. The syndrome usually affects the hands and arms, but it also occurs in the lower limbs (4). In general, it is unilateral, but there can be a bilateral evolution in case of neurodegenerative disorders. AHS was first described in 1908 by Kurt Goldstein, but it was not until 1972 that Brion & Jedynak used the term “alien hand”.
There are different clinical variants of AHS, depending partly on the location of the injury in the brain. In 1992 Feinberg et al. made a distinction between 2 variants: the frontal and the callosal variant (5). The frontal subtype typically presents with impulsive groping (the hand is constantly searching for nearby objects) and grasping or compulsively manipulating objects. It commonly affects the dominant (right) hand. This variant arises mostly from lesions of the supplementary motor area (SMA), cingulate cortex, dominant medial cortex or the corpus callosum. In addition, the callosal variant occurs mostly with lesions of the corpus callosum. Typical for this subtype is intermanual conflict: patient’s hands interfering each other. The callosal variant more commonly affects the non-dominant (mostly the left) hand in right-handed patients. Patients with this subtype can exhibit autocriticism, frustration and anxiety. This is certainly not always the case, but distress frequently arises due to the perception of onlookers. A posterior variant was first described by Kloesel et al, in 2010 (6). This subtype results from thalamic, posterolateral parietal or occipital lobe damage and affects the non-dominant (mostly the left) hand. These patients present with avoidance response: they pull the hand away from contact or stimuli or their arm rises unintentionally. They have strong feelings of estrangement from the affected limb. This variant can be accompanied by other symptoms, such as hemianaesthesia, hemianopia, visuospatial neglect and optical ataxia. The alien hand can assume abnormal positions.
Although AHS is rare, it is an important differential diagnosis. AHS is invalidating and disabling for the patient and affects most activities of daily living. There are no approved or recommended therapies for AHS. Management is based on anecdotal reports of both pharmacological and behavioural interventions. Long-term data on rehabilitation are scarce. Therefore reports of this rare syndrome serve to raise awareness and enable discussion of best treatments. Further research into the pathophysiology and treatment is recommended, but it is not possible to perform a randomized controlled trial on AHS due to the rarity of the syndrome. Most available treatments are individualized multidisciplinary approaches. Symptoms of AHS caused by stroke are often improving at followups visits, although this is less likely for the neurodegenerative types. We report here the rehabilitation of a patient with frontal variant of AHS after stroke.
CASE REPORT
A 61-year old man presented to the emergency department of a general hospital with progressive weakness of the right side of his body and speech difficulties, 3 years after his first transient ischaemic attack. Five days previously he had attended the emergency department because of loss of strength in his right foot. Examination at that time, at the department of neurosurgery, revealed a disc herniation, providing an explanation for his symptoms, and surgery was planned. In the following days, he developed new complaints, with difficulty speaking and movement problems of both the right arm and right leg. When he could no longer take care of himself, he again attended the emergency department, where investigation revealed a semirecent ischaemic stroke.
He had a history of diabetes mellitus type II, a transient ischaemic attack in 2016 (occlusion of the arteria cerebri media on the right side) with complete recuperation, and back surgery. On clinical examination, he was alert, but showed delayed movements on the right side. Cranial nerve examination was normal, except for a slight paresis of the facialis nerve on the right side. There was a right-sided hemiplegia, hyperreflexia and sensibility disturbances. There was spasticity grade 2 on the modified Ashworth Scale in the upper extremity and grade 1 in the lower extremity. There was dysarthria and word-finding problems. An unexpected sign was that he was unable to release his grip in the Jamar and pinch test. He was oriented in place and time, but there were moderate deficits in concentration and attention. There were no arguments for visual neglect. There were slight extrapyramidal symptoms, which were new and had not previously been described in his medical history. For treatment of his extrapyramidal symptoms, the neurologist was started medication (Prolopa, Levodopa, Roche Belgium) without further investigation.
Brain magnetic resonance imaging (MRI) revealed hyperintense signal changes periventricular to corticosubcortically. In addition, there were diffuse restrictive signal changes parafalcine left frontoparietal, as well as 2 foci left parietal and 1 at the rear of the left lateral ventricle. These were considered as semi-recent ischaemic signal changes, not degenerative.
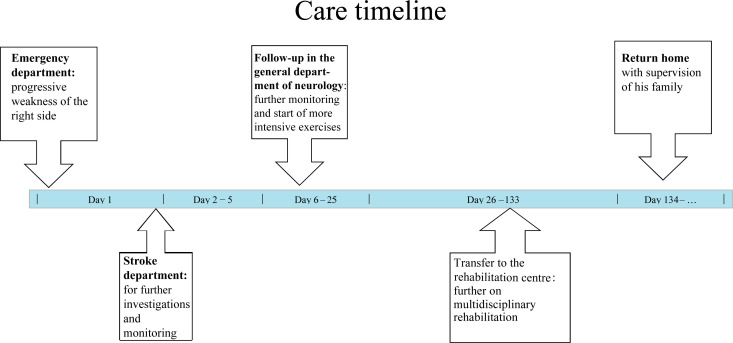
The patient was admitted to the stroke department of the hospital for further investigations and treatment, there were no diagnostic challenges. For the department of neurology it was clear that his symptoms were due to the semi-ischaemic stroke, but prior to the generalization of his complaints, a disc herniation diagnosis was considered, as described above. Looking for risk factors, other than the patient’s known diabetes and obesity, a small dilation of the left atrium of the heart was found, predisposing to atrial fibrillation. Holter monitoring was negative. There was no specific therapy for the patient’s symptoms before our rehabilitation. After 26 days he was transferred to a multidisciplinary rehabilitation centre (for an overview in time, Fig. 1). During the therapy sessions, it was noted that the patient’s right hand unwittingly grabbed objects during exercises and grabbed the door of the treatment room when driving out with his wheelchair. He could not voluntarily release his grip, but he needed help from his left hand. A diagnosis of AHS was made based on the fact that the involuntary movements of his hand hindered the patient during therapy and during activities of daily living such as washing, getting dressed, etc.
Fig. 1.
Care timeline for a case of alien hand syndrome (AHS) in a 61-year-old man following ischaemic stroke.
Multidisciplinary rehabilitation was started, consisting of speech therapy, occupational therapy, physiotherapy and neurocognitive training. Regarding AHS, compensation strategies were learned, and the focus was mainly on practicing bimanual tasks, engaging the alien hand during 2-handed tasks. Different colours (black, white and bright colours) were used to navigate the attention more to one side. An exercise strategy used was to let the alien hand catch a cube, after which more exercises could be performed with the other hand during one – handed training.
The patient was assessed using the Functional Index Measure (FIM) score. The FIM score of the upper limbs improved from 1/7 to 4/7 after 12 weeks of therapy. Total FIM score at admission to the rehabilitation centre was 36/126 and at discharge, after 19 weeks, 79/126.
DISCUSSION
There are no clear physiological or laboratory criteria for diagnosing AHS: diagnosis is based on clinical symptoms. Park et al. found 2 criteria to diagnose AHS: first the complaint of a foreign body (a feeling of foreigness of the limb) and, secondly, complex, autonomic, involuntary activity that does not fit within other movement disorders (7). If these 2 criteria are present, the diagnosis can be made.
In the literature, based on anecdotal reports of both pharmacological and behavioural interventions for AHS, there is no consensus about the best pharmacological treatment options and there are different rehabilitation approaches. Therefore, it is important to publish case reports of this rare condition, describing outcomes after any form of therapy. The majority of interventions described were behavioural, but generalization of the results is not possible (lack of long-term follow-up, evidence level C or D). There is limited evidence of medication benefiting AHS: botulinum toxin and clonazepam seem to be a reasonable adjuvant intervention in some cases.
In the field of rehabilitation most articles describe individualized multidisciplinary treatment in patients with AHS due to stroke. Most treatments focus on identifying the specific functional impairments and consist of education and learning compensation strategies. The treatment modalities described include cognitive behavioural therapy (CBT), distracting tasks, verbal cues, sensory tricks, and visualization strategies.
CBT can enable patients to control their anger and frustration about the involuntary movements. A useful coping strategy is provided by distracting the affected hand with an object (placing the hand in a pocket or presenting a ball to the affected hand). Visualizing every movement with both hands and organizing the sequence of the task can also allow functional independence to be regained. Verbal cues focus attention on important information and help people to understand and remember a sequence of movements. Placing the affected hand in an oven mitt limits sensory feedback and has sometimes been reported to be helpful.
Romano et al. propose mirror therapy as a possible treatment for a 62-year-old patient with frontal/posterior variant of AHS after stroke (8). Mirror box therapy was started, based on the hypothesis that observation of a reflection compatible with the image of the affected hand would help improve motor control. The patient performed some tasks, with the mirror was left uncovered for half of the time, thus providing visual feedback (mirror condition), and the mirror covered for the other half of the time, producing no feedback (no-mirror condition). Statistical comparison between the 2 conditions showed a significant difference in the tapping task, but no difference in the visual analogue scale (VAS). This means that there is an improvement, although it is not subjectively experienced by the patient. There are no other studies confirming these results. Braun et al. reviewed the neurocognitive background and therapeutic potential of sense of ownership (SoO) and sense of agency (SoA). AHS is an example of limb-specific disruption of SoA. They describe that experiencing SoA has the potential to enhance therapeutic interventions. Self-efficacy is an important condition for acquiring action. This is only possible by repeating many positive SoA experiences (1). This is a promising strategy to implement in therapy to motivate patients.
Regarding pharmacological options, Haq et al. published a case report in 2010 of a 13-year-old right-handed girl with symptoms of posterior type of alien hand after brain herniation 5 years previously (9). Initial treatment with baclofen had no significant results. Treatment with daily clonazepam resulted in a significant reduction in hand elevation and resolution of grasping. However, therapy was stopped after the occurrence of side-effects. Subsequently 600 units of botulinum toxin type A (first injection 300 units, second injection five years later with 600 units) were injected into the muscles of the right arm, which is high above the normal maximum dose of 200 units for pediatric patients, so unlicensed use. The patient experienced a favourable result from the botulinum injections. At the peak moment of effectiveness of the botulinum toxin (2 – 6 weeks after the injection) the AHS movements almost disappeared. Nevertheless, it is difficult to draw conclusions from the favourable result of a single case. In addition, this case was treated with a much larger dose of botulinum toxin than is normal for treatment of spasticity of a limb, especially in pediatric population.
In conclusion, no proven effective treatment for AHS has been described in the literature, and hence current treatment is based on anecdotal reports.
In the case of stroke, symptoms usually improve during the weeks and months after onset (2). However, in the case of neurodegenerative disorders, symptoms are unlikely to improve. At follow-up after the diagnosis of AHS, an improvement in FIM score can be seen, or a reduction in the number of abnormal movements. Reports by Nowak et al. describe the resolution of symptoms after 18 weeks of therapy and a report by Nicholas et al. describes the disappearance of symptoms when the patient placed his hand in an oven mitt (10, 11).
In the current case, therapy was hampered by neurocognitive problems. The patient had reduced attention and memory, which made the exercises more difficult during a focus on bimanual tasks. Individualized multidisciplinary therapy improved the symptoms of the current patient, but this can probably also be partly explained by spontaneous resolution. Adherence to and tolerability of the intervention was good, there were no adverse or unanticipated events. The patient stayed in hospital during rehabilitation, thus it was possible to monitor the intervention. The patient was initially frustrated, because his hand would not move in the way he wanted. Over time his frustration reduced and he became much calmer. It was difficult to investigate this patient’s perspective, because the patient still has important neurocognitive difficulties. Nevertheless, the patient was discharged home with family assistance.
In conclusion, AHS is a rare neurological disorder, typically characterized by abnormal movements over which the patient has no control. There are different variants of AHS, depending on the location of the injury, with different clinical presentations. AHS is an important differential diagnosis for rehabilitation, since it is very disabling, especially in activities of daily living. Once a diagnosis of AHS is established, the patient and their family can be informed and educated about this rare syndrome and how to deal with it. There is no published proven effective treatment, and AHS continues to be a challenge. Current management is based on case reports; most of the articles describe an individualized multidisciplinary approach with improvement in symptoms. In the case of stroke, spontaneous resolution can be expected, but this is not the case with neurodegenerative diseases.
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Braun N, Debener S, Spychala N, Bongartz E, Soros P, Muller H, et al. The senses of agency and ownership: a review. Front Psychol 2018; 9: 535: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hassan A, Jospehs KA. Alien hand syndrome. Curr Neurol Neurosci Rep 2016; 16: 73. [DOI] [PubMed] [Google Scholar]
- 3.Sarva H, Deik A, Severt WL. Pathophysiology and treatment of alien hand syndrome. Tremor Other Hyperkinet Mov (N Y) 2014; 4: 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graff-Radford J, Rubin MN, Jones DT, Aksamit AJ, Ahlskog JE, Knopman DS, et al. The alien limb phenomenon. J Neurol 2013; 260: 1880–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feinberg TE, Schindler RJ, Flanagan NG, Haber LD. Two alien hand syndromes. Neurology 1992; 42: 19–24. [DOI] [PubMed] [Google Scholar]
- 6.Kloesel B, Czarnecki K, Muir JJ, Keller AS. Sequelae of a left-sided parietal stroke: posterior alien hand syndrome. Neurocase 2010; 16: 488–493. [DOI] [PubMed] [Google Scholar]
- 7.Park YW, Kim CH, Kim MO, Jeong HJ, Jung Hy. Alien hand sydrome in stroke: case report and neurophysiologic study. Ann Rehabil Med 2012; 36: 556–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romano D, Sedda A, Dell’aquila R, Dalla Costa D, Beretta G, Maravita A, et al. Controlling the alien hand through the mirror box. A single case study of alien hand syndrome. Neurocase 2014; 20: 307–316. [DOI] [PubMed] [Google Scholar]
- 9.Haq IU, Malaty IA, Okun MS, Jacobson CE, Fernandez HH, Rodriguez RR. Clonazepam and botulinum toxin for the treatment of alien limb phenomenon. Neurologist 2010; 16: 106–108. [DOI] [PubMed] [Google Scholar]
- 10.Nowak DA, Bösl K, Lüdemann-Podubecka J, Gdynia H-J, Ponfick M. Recovery and outcome of frontal alien hand syndrome after anterior cerebral artery stroke. J Neurol Sci 2014; 338: 203–206. [DOI] [PubMed] [Google Scholar]
- 11.Nicholas JJ, Wichner MH, Gorelick PB, Ramsey MM. Naturalization of the alien hand: a case report. Arch Phys Med Rehabil 1998; 79: 113–114. [DOI] [PubMed] [Google Scholar]