Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) represents respiratory symptoms as the most common clinical manifestations. Similar to some other viral infections, it can cause severe neurological damages. Here, we describe a 40-year-old man case who initially was admitted to a major hospital with presenting 7 days with weak flu-like symptoms (cough) and fever then presented neurology signs for 3 days. Physical examination and brain magnetic resonance imaging (MRI) showed cerebral vasculopathy. Molecular testing was performed on nasopharyngeal swab by real-time reverse transcription polymerase chain reaction (RT-PCR) which was positive for SARS-CoV-2. The patient received supportive cares and was treated with routine antiplatelet therapy. He was improved and discharged 10 days after admission with no symptoms. Our findings report a 40-year-old man with flu-like symptoms that indicate cerebral vasculopathy that was discharged with no symptoms. Therefore, physicians should be monitor patients with worsening or progressive central nervous system results. The pathobiology of this virus is still incompletely known; therefore, extensive studies are needed to reveal the effect of COVID-19 on the nervous system.
Keywords: SARS-CoV-2, COVID-19, Vasculopathy, Central nervous system, Iran
Background
The first case of infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) had been reported in China in December 2019, while the number of Coronavrus Disease 2019 (COVID-19) cases has increased 110 million people globally (Halaji et al. 2020; Moriguchi et al. 2020; Sheikhshahrokh et al. 2020). The disease commonly indicates respiratory tract disease with shortness of breath, fever, and cough and that may development to acute respiratory distress syndrome (ARDS), multiple organ failure, and even death (Singhal 2020).
To date, the cases with neurologic manifestations have been reported. COVID-19 patients often endure from severe hypoxia, that it can cause further nervous system damage (Moriguchi et al. 2020; Wu et al. 2020).
Previous studies have reported acute central nervous system (CNS)-associated symptoms including cerebrovascular disease, muscle injuries, and encephalopathies in COVID-19 (Tsai et al. 2005). Furthermore, central nervous system vasculopathy associated with COVID-19 have revealed complications such as stroke, dissection, aneurysm, and hemorrhage (Wu et al. 2020).
Here, we report a case with COVID-19-associated cerebral vasculopathy to highlight the clinical features and neurological complications of COVID-19 infection. To the best of our knowledge, this is the first report of the case of a COVID adult patient diagnosed for cerebral vasculopathy.
Case presentation
A patient from the community was admitted and managed to general wards in May 2020. The clinical laboratory and radiological findings of a community-acquired COVID-19 patient were assessed. Moreover, neurological findings obtained by reviewing medical records and the physician team were collected. Nasopharyngeal swab samples were taken with dacron swabs as previously describe (Moriguchi et al. 2020). To detect SARS-CoV-2, real-time reverse transcription polymerase chain reaction (RT-PCR) was performed by as previously describe (Moriguchi et al. 2020).
A 40-year-old male, with a past contact with SARS-CoV-2 positive patients (his co-workers were positive for COVID-19), was admitted to the emergency ward of a major hospital in Tehran, Iran, with 7-day history of weak flu-like symptoms (cough), fever, and neurological signs. On neurological evaluation, he had double vision (diplopia), nystagmus, and gait disorders. A nasopharyngeal swab was used for testing the SARS-CoV-2 virus, and RT-PCR showed positive result for SARS-CoV-2.
Laboratory tests indicated no abnormalities except for high WBC count (12.2 × 109/L) and C-reactive protein; liver and renal function tests were normal.
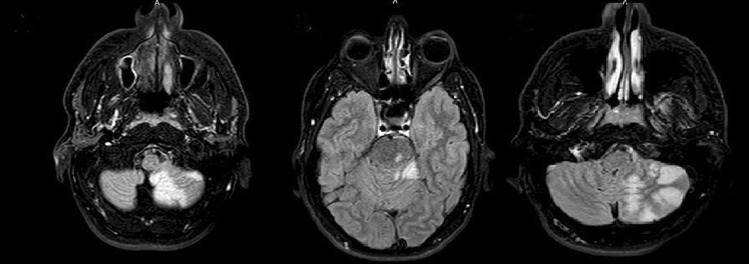
Chest radiograph, echocardiogram of the heart, and chest computerized tomography (CT scan) were normal. Moreover, the initial cerebral angiography and electroencephalography were also normal. Brain magnetic resonance imaging (MRI) showed cerebral vasculopathy with possible stroke and inflammation of the arteries associated with COVID-19 (Fig. 1). MRI with Gd injection had no enhancing lesion. The patient received supportive cares and was treated with routine antiplatelet therapy. Finally, the patient did not present post-operative neurological complication and his symptoms improved completely and discharged 10 days after admission with no symptoms.
Fig. 1.
Vascular impairment in posterior cerebral circulation
Discussion and conclusion
Coronavirus interacts with the target cells of host via membrane-bound spike proteins. The Angiotensin-Converting Enzyme 2 (ACE2) has been recognized as a SARS-CoV-2’s entry receptor. Owing to its extensive-expression pattern, SARS-CoV-2 can influence several organs such as endothelial cells and the nervous system in which the receptor is expressed predominantly by the neurons (Mohammadpour et al. 2021). Previously, vasculopathy was reported in the SARS-CoV and MERS-CoV (Tsai et al. 2005; Yuan et al. 2017). The reports on COVID-19-related unusual neurological manifestations are limited (Ye et al. 2020).
The definitive recognition of COVID-19 is difficult, though viral vasculopathy depends largely on the virus isolation since SARS-CoV-2 dissemination is transient with probably very low CSF titer (Ye et al. 2020). In patients with COVID-19, injury of vascular may arise via indirect and/or direct mechanisms: the first is due to viral affinity to ACE2 represented by host cells such as endothelial cells and the second is induces coagulopathy and vasoconstriction as results of misdirected host immune response (Matos et al. 2020). Physical assessment of neurological symptoms is vital to diagnose cerebral vasculopathy presumptively diagnosis. Consequently, cerebral vasculopathy is assessed in terms of the MRI and CT results of the brain.
A case with the concurrent infection with COVID-19 and an infection associated with vasculopathy was reported in Portugal by Matos et al. where no particular SARS-CoV-2 nucleic acid was found in CSF; however, it was found in nasopharyngeal swab (Matos et al. 2020).
Furthermore, Mirzaee et al. represented focal cerebral arteriopathy and ischemic stroke in a pediatric patient with COVID-19 in Iran. Accordingly, the major findings in this patient were the presence of unilateral focal vasculopathy. The SARS-CoV-2 nucleic acid in the nasopharyngeal swab and CSF was positive (Mirzaee et al. 2020).
Likewise, mild flu-like signs were found in four weeks prior to initiating the neurologic symptoms, which indicates a parallel course of the disease. In this regard, Matos et al. demonstrated that “The clinical presentation of altered mental status and dysexecutive syndrome, 1 week after being diagnosed with COVID-19, made us consider a probable causal association” (Matos et al. 2020).
Neurologic signs explained after both MERS-CoV and SARS-CoV infection include peripheral neuropathy, myopathy, Bickerstaff brainstem encephalitis (BBE), and Guillain–Barre syndrome (GBS) that are developed 2 or 4 weeks after initiating the respiratory symptoms (Ng Kee Kwong et al. 2020).
In this regard, in Iran, several case report studies reported different patients with neurologic manifestations such as meningoencephalitis associated with SARS-COV-2 (Mardani et al. 2020) and ischemic stroke (Ahmadi Karvigh et al. 2020).
In conclusion, COVID-19 infection leads to damage in multiple organs such as pulmonary, renal, cardiovascular, gastrointestinal tract, muscles, and coagulation. Our findings report a 40-year-old man with flu-like symptoms that indicate cerebral vasculopathy that was discharged with no symptoms. Also, the present study support that CNS may be another target for SARS-CoV-2 infection, so, physicians must be monitor patients with worsening or progressive CNS results. Given no complete information exists regarding the pathobiology of this virus, wide studies are required to discover the effect of CoV infections on the nervous system.
Acknowledgements
Thanks to guidance and advice from Clinical Research Development Unit of Baqiyatallah Hospital, Tehran, Iran. We thank the head and manager of Erfan Hospital for their supports. We thank also the patient and his family for their willingness to share case information and images.
Declarations
Ethics approval
This study was approved by the head and manager of Erfan Hospital. However, any permission from the hospital was not required. This was because of all data was obtained from usual clinical process.
Consent for publication
Written consent for publication of this case report and clinical details or any accompanying images were obtained from the patient.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mohammad Javad Hosseini and Mehrdad Halaji contributed equally as first authors to this work.
References
- Ahmadi KS, Vahabizad F, Banihashemi G, Sahraian MA, Gheini MR, Eslami M, Marhamati H, Mirhadi MS (2020) Ischemic stroke in patients with COVID-19 disease: a report of 10 cases from Iran Cerebrovasc Dis 1–6 10.1159/000513279 [DOI] [PMC free article] [PubMed]
- Halaji M, Farahani A, Ranjbar R, Heiat M, Dehkordi FS. Emerging coronaviruses: first SARS, second MERS and third SARS-CoV-2: epidemiological updates of COVID-19. Infez Med. 2020;28:6–17. [PubMed] [Google Scholar]
- Mardani M, Nadji SA, Sarhangipor KA, Sharifi-Razavi A, Baziboroun M. COVID-19 infection recurrence presenting with meningoencephalitis. New Microbes New Infect. 2020;37:100732. doi: 10.1016/j.nmni.2020.100732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matos AR, Quintas-Neves M, Oliveira AI, Dias L, Marques S, Carvalho R, Alves JN (2020) COVID-19 associated central nervous system vasculopathy Can J Neurol Sci 1–6 10.1017/cjn.2020.1092020.1092020.1092020.109 [DOI] [PMC free article] [PubMed]
- Mirzaee SMM, Gonçalves FG, Mohammadifard M, Tavakoli SM, Vossough A. Focal cerebral arteriopathy in a COVID-19 pediatric patient. Radiology. 2020;297:274–275. doi: 10.1148/radiol.2020202197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammadpour S, Torshizi Esfahani A, Halaji M, Lak M, Ranjbar R. An updated review of the association of host genetic factors with susceptibility and resistance to COVID-19. J Cell Physiol. 2021;236:49–54. doi: 10.1002/jcp.29868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, Myose N, Nakao A, Takeda M, Haro H, Inoue O, Suzuki-Inoue K, Kubokawa K, Ogihara S, Sasaki T, Kinouchi H, Kojin H, Ito M, Onishi H, Shimizu T, Sasaki Y, Enomoto N, Ishihara H, Furuya S, Yamamoto T, Shimada S. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng Kee Kwong KC, Mehta PR, Shukla G, Mehta AR. COVID-19, SARS and MERS: a neurological perspective. J Clin Neurosci. 2020;77:13–16. doi: 10.1016/j.jocn.2020.04.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikhshahrokh A, Ranjbar R, Saeidi E, Dehkordi FS, Heiat M, Ghasemi-Dehkordi P, Goodarzi H. Frontier therapeutics and vaccine strategies for sars-cov-2 (COVID-19): a review. Iran J Public Health. 2020;49:18–29. doi: 10.18502/ijph.v49iS1.3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singhal T. A review of Coronavirus Disease-2019 (COVID-19) Indian J Pediatr. 2020;87:281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai LK, Hsieh ST, Chang YC. Neurological manifestations in severe acute respiratory syndrome. Acta Neurol Taiwan. 2005;14:113–119. [PubMed] [Google Scholar]
- Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C (2020) Nervous system involvement after infection with COVID-19 and other coronaviruses Brain Behav Immun 18–22 10.1016/j.bbi.2020.03.0312020.03.0312020.03.0312020.03.031 [DOI] [PMC free article] [PubMed]
- Ye M, Ren Y, Lv T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav Immun. 2020;88:945–946. doi: 10.1016/j.bbi.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J, Yang S, Wang S, Qin W, Yang L, Hu W. Mild encephalitis/encephalopathy with reversible splenial lesion (MERS) in adults-a case report and literature review. BMC Neurol. 2017;17:103. doi: 10.1186/s12883-017-0875-5. [DOI] [PMC free article] [PubMed] [Google Scholar]