Introduction
Transitions of care occur every time an older adult moves from one physical care setting to another or when a new provider assumes care. Transitions of care are frequent for older adults who often have multiple comorbidities requiring an interdisciplinary team of providers across multiple care settings (Figure 1). Such transitions are often unplanned and occur when either an exacerbation of an underlying illness or an acute illness or injury results in a visit to the Emergency Department (ED). This may be due to frailty, where an older person is functioning well but does not have the physical or psychosocial reserve to compensate for an additional injury or illness, or due to the severity of the underlying medical condition. Fragmentation of outpatient care between multiple specialist providers has resulted in the ED becoming an important hub at the center of geriatric care. The ED visit may result in discharge back to the community with a new care plan, discharge to a new care setting, or hospital admission.
Figure 1:
An older adult entering the Emergency Department (ED) can expect to experience multiple care transitions and care providers. Systems issues such as limited Medicare funding for skilled nursing facility costs after hospitalization can lead to premature discharges to home without appropriate medications, therapy and handoffs to primary care in place. *SNF skilled nursing facility, PT physical therapy, and PCP primary care physician.
Adverse events with transitions to or from the ED are well documented. Adverse events during transitions can be life-threatening or life-altering for older adults and their loved ones, leading to a decline in independence and functional status.1 Within 3 months of an ED visit, almost one-third of older adults will experience an adverse outcome.2 Many of these adverse events are medication interactions or side effects. Over a third of patients (38%) prescribed medications from the ED have potential drug-drug interactions on pharmacist review.3 Prescribing from the ED is complicated by the fact that patient self-report of medications is poor, with older patients taking on average 3.8 more medications than they report.4 Additionally, emergency providers may feel medication reconciliation is too difficult or not in their scope of practice. Further barriers are created by health systems, as outpatient or clinic electronic health record (EHR) systems are often inaccessible to the ED provider. This is an example of how system, provider, and patient level factors can all interact to complicate transitions of care (Table 1). Patient factors contribute to the complexity of decision making and communication at the time of discharge or admission. Systems constraints include limited time in the ED for comprehensive geriatric assessments and the cognitive load of caring for multiple, acutely ill patients.5 Fragmentation of the patient’s healthcare team also plays a large role in how information is lost during transitions. Information that is critical to providing optimal care may be miscommunicated or inadequately communicated to other members of their interdisciplinary team and outpatient providers.6 Insurance issues, social services availability, and stress on family caregivers also play a role in adverse events with transitions of care.
Table 1:
System, provider, and patient level factors that can complicate safe discharges, collated from qualitative staff and patient studies.5,27-29
| System factors | Provider factors | Patient factors |
|---|---|---|
| Insurance issues: precertification for medications or home health or nursing facility placement | Patient load | Complex interacting comorbidities |
| Barriers to access to outpatient resources | Implicit biases | Polypharmacy |
| No communication between electronic health record systems | Lack of training | Cognitive impairment |
| Minimal face to face time with the patient and heavy charting requirements | Perception that it takes too much time | Low health literacy or educational level |
| Multiple handoffs and multiple providers | Focus on acute issue only in the ED leads to disregarding chronic issues | Lack of social support |
| Reduced services due to time of day or weekend transitions | Low engagement with community partners | Cultural preferences on communication and family involvement |
| Lack of in person or face-to-face handoffs | Difficulty tailoring instructions to individuals | Communication difficulties (e.g., sensory impairment, language barriers) |
| Poor integration of transitions of care services | Minimal planning time for discharge from the ED compared to inpatient time | |
| Lack of inpatient-outpatient continuity of providers | Limited training in transitional care principles | |
| ED crowding and/or inadequate staffing |
How then can emergency clinicians ensure safe transitions of care? One critical issue that is amenable to intervention by the ED team is communication with the patient. Communication with patients and ensuring understanding of diagnosis and care in this population is difficult. Only a fifth of older adults discharged from EDs can state their diagnosis, as opposed to 70-80% of younger adult ED patients.7,8 Communication barriers to patients include cognitive impairment, language and sensory barriers, small print instructions, and cultural differences on engagement in healthcare. In one study comparing understanding of return instructions in older adults with varying degrees of cognitive impairment (dementia, delirium, and normal cognition), understanding ranged from 10%-49% based on the level of cognitive impairment.9 This suggests that at best, only half of older adults discharged understand critical discharge instructions. Emergency clinicians are in a unique position to minimize risk to the patient at care transitions by improving communication and using cognitive screening and strategies such as teach-back to assess patient understanding.
The impact of care settings
There are a myriad of possible care settings that a patient may be coming from or transitioning to as well as additional services that can be of assistance in these different settings. Understanding the capabilities, advantages and disadvantages of different care settings is essential to determining the appropriate level of care and best transition for patients (Figure 2). Settings range from aging independently in the community to nursing facilities (skilled nursing facility, or SNF) with 24-hour medical support. The information required at discharge is similar no matter the living situation: medication information, appointments scheduled or needing to be scheduled, any treatments, wound care or therapies needed, and the level of assistance required with ambulation, toileting, and feeding.10 Many providers assume that home caregivers have been trained to provide services such as gastric tube care or incontinence care, but home caregivers are often very appreciative of further details regarding this care. The ability to discharge a patient to home with home health rather than admission to a SNF is often desired by patients, but this can create a burden on caregivers and has been associated with more ED revisits in the short term.11 The social support, abilities, and availability of caregivers must be clear and discussing alternative optionsin the event of caregiver burnout is very helpful.
Figure 2:
Older adults may inhabit a variety of care settings that change their ability to obtain assistance in the areas of mobility, medications, and activities of daily living. Assisted living facilities can greatly vary in what they provide for healthcare services, and a call to the facility can help clarify what resources are available to a patient returning from the Emergency Department.
Another frequent care transition that can lead to need for emergency care is SNF discharge to home. SNFs are pressured to discharge patients to home care, resulting in unexpected challenges for patients who often end up in the ED when family is unable to care for them.12 System factors such as insurance payments may contribute to precipitous care transitions. Patients on Medicare may be unable to afford the $170.50 daily copay (2019 rates) for skilled nursing care after the 20 days of 100% cost coverage elapse, resulting in premature discharges to home.13 In one study, 25% of older adults discharged from a skilled nursing facility where in the ED within 30 days, as compared to 12.6% when a specialized pharmacist/geriatrician discharge intervention was done in the SNF prior to discharge.14 This illustrates how a lack of attention during transitions can still end up with ED providers caring for these patients and attempting to resolve complicated home care needs and care transition issues.
Another alternative to hospital or SNF admission is Hospital in the Home, a care model for providing acute or subacute care for conditions such as cellulitis, COPD exacerbation, or CHF exacerbation that would usually require admission. The Hospital in the Home model has been shown to be feasible and efficacious as well as cost-effective.15 Patients are also more at ease and may be more active in their own home settings, mitigating the risks of functional decline and delirium seen with normal hospital admissions. Consider, for example, an older adult with COVID-19 stable on 2L of supplemental oxygen and requiring assistance with ADLs due to their illness. This patient may be a candidate for Hospital in the Home and receive in-home nursing care with frequent assessment of vitals and assistance with ADLs while avoiding inpatient admission.
Considering caregiver burden and wellbeing is crucial to ensuring that the older adult under their care receives adequate support. Respite care for older adults at a SNF or at an adult day care is an adjunct utilized to provide respite to caregivers on the order of days to weeks. Caregivers may also benefit from support groups and other community resources. If an older adult with care needs is in the ED for an issue that is subacute or chronic, the underlying reason may be caregiver stress rather than a health issue for the patient. Identifying and addressing this can improve both the patient’s and the caregiver’s health.
Choosing the appropriate care setting
Multiple risk screening tools have been developed to risk stratify older adults for adverse health events after an ED visit, but none has shown the necessary levels of sensitivity and specificity.16,17 This is likely due to the fact that there are a plethora of non-medical and non-quantifiable criteria not included in these scoring systems that influence care decisions. Every patient has a certain level of medical needs that determines the lowest level of care required. For example, a patient who medically needs intensive care would need intensive care regardless of their socioeconomic status, home safety, or cognition. On the opposite side of the spectrum, a patient whose medical needs require only outpatient care may require observation or inpatient floor care if they lack social support. Conversely, a patient who medically requires a high level of care may be best discharged to home if what matters most to the patient is not quantity, but rather quality of life.
One model of geriatric care from the Institute of Healthcare Improvement and John A Hartford Foundation uses the 4-MS: What Matters, Medications, Mentation, and Mobility.18 While this model was designed for clinics and inpatient settings, the model is also apropos to the ED visit. For the ED, we recommend including an “S” to this model: Safety and Social Support. There are also a number of validated screening tools that can aid with assessment (Table 2).
Table 2:
Formal, validated assessment tools and training for the 4-MS in the Emergency Department setting.
| Category | Assessment tools |
|---|---|
| What Matters Most? | Brief negotiated interview model, VitalTalks model, EPEC-EM (education on palliative and end-of-life care for emergency medicine)30 |
| Medications | Online medication interaction checkers |
| Mentation | Short Blessed Test, Brief Alzheimer’s Screen, Mini Mental Status Exam (MMSE), Montreal Cognitive Assessment (MoCA), 4AT |
| Mobility | Timed Up and Go, 4 Stage Balance Test, Sit to Stand Test |
What Matters Most? Person- and family-centered care is essential for all patients, but especially older adults making difficult decisions about their care. This conversation can start by asking the patient and caregivers what they are most concerned about and why. This helps guide the conversation on what the physician can offer. It is important to think creatively. Options such as hospital at home, overnight observation for further assessment and care coordination, and ED to hospice transitions need to be considered in addition to the traditional admit vs discharge decision. This is a type of goals of care conversation which involves the clinician learning about the patient as a person. Exploring the free resources at https://www.vitaltalk.org/ can help you learn how to map out what is most important to the patient, discuss patient goals with a surrogate, and more.
Medications: A full medication review includes which medications are taken, how and when they are taken, including over the counter medications or supplements. Medication review in the ED by a pharmacist identifies errors and medication interactions in 68% of patients, with a mean number of discrepancies of 3 per patient.19 Common classes of medications known for interactions include proton pump inhibitors, anticoagulants, and selective serotonin reuptake inhibitors.20 If a trained medication reviewer or pharmacist is not available in the ED, consider referral for outpatient follow-up with a pharmacist or polypharmacy clinic. This ED to outpatient review strategy led to an absolute 9% reduction in proportion of patients requiring admission to the hospital in the four months after an ED visit.4
Mentation: Evaluation of mentation requires understanding the patient’s baseline cognitive status as well as screening for delirium and cognitive changes with validated tools during the ED visit.21 Currently, ED providers rarely formally screen for cognitive changes.22,23 Ignoring cognitive limitations leads to difficulty understanding discharge instructions, which can result in return ED visits, medication misuse, or inability to care for the illness or injury properly at home. Subtle delirium is also often only noted with testing. Mentation is worsened by sensory impairment, such as lack of hearing aids or reading glasses, so if possible temporary use items should be stocked in the ED and hospital to help better assess cognition in the setting of sensory impairment.
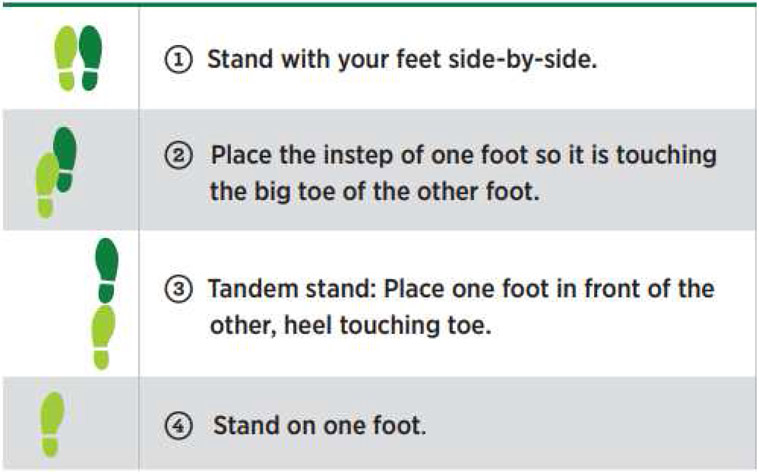
Mobility: Safe mobility requires an understanding of what assistive devices they require, what they have available, and the home living situation. Can they get in and out of the house safely, or are they newly homebound? Will this illness require temporary support? Some EDs have access to physical therapists for gait assessments and equipment training but most do not. ED nurses can often provide insightful information on gait and self-care ability as they are in the room and assisting with toileting and transfers. Mobility can be assessed using the Timed Up and Go (TUG) test, a validated tool accounting for both static and dynamic balance.24 This is performed by timing the patient when asked to perform the following: stand up from a chair, walk 3 meters at their normal pace, turn, and walk back to the chair and sit down (Figure 3). Patients can use their baseline assistive devices. Individuals with a TUG test >13.5 seconds are in a high-risk category for falls. For EDs that do not have the space for this test or when patients need to remain on telemetry or other monitors, the 4 Stage Balance Test is preferred (Figure 4). This can be done at the bedside and involves having the patient stand with progressively more difficult stances.
Safety and Social Support Consider the patient’s home safety and social support. Safety includes considering the possibility of elder abuse and neglect as well as the caregivers’ abilities to provide the support needed. Oftentimes a caregiver has as many chronic health issues as the patient in question. Assisting them in setting up home meal delivery (meals on wheels), home health aides or nursing, or a home safety assessment by a community paramedic team or your local Area Agency on Aging can make the difference between a supportive community dwelling adult and further functional decline.
Figure 3:

The Timed Up and Go (TUG) test is used to assess mobility. A time of greater than 13.5 seconds signifies abnormal mobility and high risk for falling.
Figure 4:
The 4 Stage Balance Test is a test of static balance and so assesses mobility differently than the TUG, but is very quick and able to be done at the bedside in the ED. Supportive devices such as a walker may be used to move into the appropriate stance. The ability to hold the tandem gait for >10 seconds demonstrates good balance. Adapted from CDC STEADI Guidelines, https://www.cdc.gov/steadi/pdf/STEADI-Assessment-4Stage-508.pdf.
One limitation to applying the 4-MS model in the ED is clinician time. A team approach can alleviate some of this burden. For example, a social worker or case manager can discuss Mobility and Safety/Social Support. A physical therapist or ED nurse can administer mobility testing. A pharmacy technician or pharmacist can assist by verifying medications. This multidisciplinary approach is very common in the inpatient setting, and case managers, social workers, and nurses in the ED can assist with gathering information to form a holistic care plan. Palliative medicine consultation can assist with determining what matters most and increases the likelihood a patient will be discharged to the community.25 If a patient has a complicated social situation or may need intensive intervention by case management, physical therapists, or pharmacists, an observation unit can be used for this holistic multidisciplinary assessment.26
Older adults can encounter significant challenges functioning at home with relatively minor illnesses. For example, a distal radius fracture is almost exclusively treated with a splint and referral to orthopedics in younger adults. But for older adults, a conversation about increased fall risk, self-care at homeand early physical therapy to avoid muscle atrophy in that arm are all essential. The older patient may already have limited range of motion or be unable to manage splint care if they live alone. Another example of a common ailment addressed on ED visit is a mild chronic obstructive pulmonary disease (COPD) exacerbation. An older adult with a COPD exacerbation is sent home with appropriate treatments and a new patient appointment with a pulmonologist. The patient, however, was not screened for cognitive deficits, and was unable to drive to the pulmonology clinic, a new and unfamiliar environment, and missed his appointment. He was never started on a long acting preventative inhaler and was back in the ED with another exacerbation two months later. This type of cycle can repeat indefinitely, and the patient is often labeled as “noncompliant” when in fact the patient has cognitive or transportation issues that would have been identified if the 4-MS model were used prior to discharge.
Once the disposition decision has been made by taking the 4-MS model into account, communication is key to ensure a successful transition. If the patient is being discharged back home, provide clear written and verbal instructions to the patient and caregivers. Most EHRs allow for large font printing for discharge instructions to ensure legibility. Return precautions are also an important component of discharge counseling. A brief call or message to the patient’s primary care providercan ensure that changes to the care plan are communicated directly and appropriate follow-up is in place. If the patient is discharged back to a facility, such as a SNF, a verbal handoff with the patient’s nurse can ensure their care team is aware of any medication changes, abnormal lab results, procedures, and follow-up needed. SNF nurses identify poor quality discharge communication as a major barrier to safe and effective transitions.10 SNFs rely heavily on discharge materials, so complete and accurate discharge information including wound care, medications, and upcoming appointments are crucial. SNFs often have central pharmacies and calling before discharge can ensure the patient is able to obtain all prescribed medications. If the patient is admitted, communicating directly with the inpatient team can avoid potentially dangerous omissions.
Case Studies: Applying the 4-MS model to Emergency Department cases
Case 1:
Mrs. Z is an 82 year old woman with diet-controlled diabetes, hypertension, and osteoarthritis. She presents to the ED with left sided flank pain and vomiting and is found to have an uncomplicated renal stone, 4mm in size. Her urine is concentrated but does not show signs of infection. She is treated with an IV fluid bolus, ondansetron for nausea and ketorolac for pain. She is now able to tolerate a few sips of juice. What is the appropriate disposition?
What Matters Most? She would like to be home if at all possible because she has two cats at home and doesn’t have anyone in the area to feed them if she is gone for a long time.
Medications A full medication review reveals that she is not on any QT prolonging drugs so ondansetron is reasonable for nausea. However, she does take celecoxib daily for arthritis pain, which is a non-steroidal anti-inflammatory medication. Adding an additional NSAID to this could cause significant and potentially dangerous side effects.
Mentation She scores a 7 on the Short Blessed Test, signifying some mild cognitive impairment mainly with short term recall. She is oriented fully.
Mobility Mrs. Z is able to ambulate well with her cane, which is what she uses at home for her arthritis pain.
Safety and Social Support Mrs. Z lives in her own two story home. She has a daughter who lives an hour away and visits more than weekly, but is unable to come daily.
Discussion:
You know that Mrs. Z is likely to pass the stone without trouble at home, but are concerned based on her memory issues, so you obtain her permission to speak with her daughter. The daughter cannot stay with Mrs. Z, but understands that she will need more support this week and arranges for family and friends to check in by phone or in person several times a day to encourage her to drink fluids and check her symptoms. You put her on acetaminophen instead of NSAIDs and arrange for a referral to your geriatric assessment clinic for further cognitive testing. Both the patient and her daughter are very happy with this plan. You send a brief message to the patient’s urologist to facilitate an outpatient appointment as well and ensure that she and her daughter are aware of the next steps in follow-up.
What if Mrs. Z lived in a senior assisted living complex? Depending on the resources of the facility, the facility may be able to provide daily wellness checks, monitor medications, or even check her vitals to assess for fever daily. Assisted living complexes vary greatly in the assistance they can provide post ED visit. It is important to have very clear instructions on the level of monitoring needed, sometimes written as a prescription or “doctor’s orders.” Speaking to a staff member at the facility is also helpful. If the patient presents from a long-term care facility, staff from the facility can be a valuable source of collateral information. Since staff often do not accompany the patient to the ED, calling the facility for a verbal handoff regarding any changes to the patient’s care plan can prevent errors. You can also ensure that written discharge instructions are clear and complete to reinforce the changes.
Case 2:
Mr. Y is a 75 year old man who presents to the ED for chest pain after eating dinner. He had a cardiac catheterization last year which showed diffuse coronary artery disease not amenable to cardiac stenting which is being medically managed. Medical evaluation including serial EKGs, basic labs, a chest x ray, d-dimer, and two troponins are all reassuring. He is eating and drinking well and says he gets these pains frequently. His initial blood pressure was high but after giving him his home evening blood pressure medication it comes back down to 130/80. What is the appropriate disposition?
What Matters Most? Mr. Y says the most important thing to him is to “keep on going” because he is a “tough old guy” and thinks his health is good.
Medications When asked if he takes all his medications, Mr. Y answer affirmatively. But he cannot tell you the names of all his medications. When pressed, he also can’t say how many he takes in the morning or evening. He just takes “whatever comes in those packets they send.” He admits to drinking daily, but will not say how much.
Mentation Mr. Y is circuitous to his answers. He confabulates when he doesn’t know the day of the week or the date (“I’m retired, I don’t need to know that anymore!”). A Brief Alzheimer’s Screen reveals that his short term recall is 1/3 and his fluency is diminished.
Mobility Mr. Y says he gets around fine in his house without any assistive devices, but when pressed he holds onto furniture and the walls for support. In the ED he has no difficulty getting out of the bed but then has an unsteady gait.
Safety and Social Support Mr. Y lives alone in an apartment. He doesn’t drive, but does take the bus or walks to the nearby corner store and pharmacy. He has family but they live several states away.
Discussion:
Many physicians, before going through the 4Ms, would discharge Mr. Y back to his living situation. With this additional knowledge however, it is clear that Mr. Y is not able to take his medications appropriately and has significant cognitive impairment. He is drinking daily and may not be caring for himself well. He has no social support structure. He would benefit from full cognitive assessment and arranging for resources such as a home health nurse to fill and monitor his pillboxes, a home safety check, a system to call for help if he falls, a physical therapy evaluation and recommendation for gait assistance, and a complete cognitive assessment to evaluate his ability to make healthcare decisions. An observation stay would allow the time needed to complete these evaluations and ensure that he is safe to go home. Given his cognitive issues, he is unlikely to be able to arrange all of this from home by himself. A brief call to his inpatient team ensures that they understand that his admission is not simply due to his chief complaint of chest pain workup, but rather due to your concerns regarding his fall risk, cognitive impairment, and need for additional resources at home.
Case 3:
Mr. X is an 89 year old male with stage 4 metastatic small cell lung cancer, presenting with worsening cough and fever. He is cachectic and ill appearing and at baseline uses 2 L supplemental oxygen. In triage he requires 3 L oxygen via nasal cannula to keep his pulse oximeter level >90%. He is febrile and chest X ray demonstrates a post-obstructive pneumonia.
What is the appropriate disposition?
What Matters Most? Mr. X says the most important thing to him is to spend the remaining time he has surrounded by his family at home. When you ask him, he states that he does not want to be admitted to the hospital even if the pneumonia is treatable because every time he comes in it results in at least a 2 week stay. With his permission his son joins the discussion and supports his father in his wishes. They would like to pursue home hospice and have been considering this even prior to this ED visit as his health has declined in the past couple of weeks.
Medications A full review of his medications is performed by the ED pharmacist. You come to the decision with the patient that he would like to treat the pneumonia at home for palliation. To avoid interactions with his other medications, evofloxacin is not an option. The hospice team is able to do IV ceftriaxone at home.
Mentation Mr. X scores 30/30 on a Mini Mental Status Exam. He displays no signs of cognitive impairment and clearly understands the risks and benefits of both inpatient admission and home hospice care. Since he clearly understands the medical decisions and options presented to him, he has medical decision-making capacity.
Mobility Mr. X is has very limited mobility at home, and can only ambulate a few steps with assistance due to his deconditioning and frailty. He mainly uses a wheelchair and walker. Hospice will help with arranging durable medical equipment such as hospital bed and bedside commode.
Safety and Social Support He lives with his son. His son cooks meals for him, assists him with the ADLs, and is his sole source of social support. This has taken a toll on his son as well, causing considerable stress. He would welcome additional assistance provided by hospice nurses to help treat his father’s pain and shortness of breath and home health aides to assist with other activities such as bathing and dressing. The ED social worker begins making arrangements for home hospice. The home hospice agency is also able to provide his son with additional resources for emotional and spiritual support.
Discussion:
If care had not been taken to address what matters most to Mr. X, he may have been admitted to the hospital which is not consistent with his goals of care. By enlisting the help of the ED social worker, Mr. X is able to return back home with additional support services including medical equipment, nursing care, and home health all through a home hospice agency. The needs of his son, who is his sole source of support, were also addressed during the visit.
Summary
Caring for older adults in the ED presents unique challenges and transitions are inherently risky. ED providers can play a crucial role in preventing adverse events by utilizing the 4-MS model and providing clear communication.
Clinical Care Points.
Common adverse events after a transition of care include medication interactions, injurious falls, and ED revisits or rehospitalizations.
Clear communication with the patient, caregiver, and outpatient care team (both from the facility if the patient is not community dwelling and the medical team) requires dedicated time to answer questions at discharge and verbal and written handoffs. At best, less than 50% of older adults understand their discharge instructions and diagnosis.
The Institute for Healthcare Improvement’s 4-MS model can be adapted to the ED setting and recommends assessing What Matters Most, Medications, Mentation, and Mobility. In the ED, add an S for assessing Safety (concerns for elder abuse and home safety) and Social Support.
Alternatives to hospital admission can include a short observation stay for multidisciplinary geriatric assessment, hospital-at-home programs, and hospice care.
Key Points.
Transitions of care represent a time at which older adults are particularly vulnerable to adverse events such as medication errors, difficulty recovering from the illness or injury, and miscommunication due to fragmented care.
Familiarizing yourself with the variety of care settings that older adults inhabit can help facilitate a safe disposition by understanding the level of care and adjuncts that are available.
The Institute for Healthcare Improvement (IHI) 4-MS model helps clinicians develop a safe discharge plan. This involves understanding Medications, Mentation, Mobility, what Matters most to the patient, as well as Safety and Social Support.
Goals of care conversations are about what matters most to the patient, which informs the level of care desired.
Communication is key to safe dispositions and ED physicians can take steps to ensure that changes to the patients care plan are understood by the patient, caregivers, and other members of their medical team.
Synopsis.
Each Emergency Department visit represents a crucial transition of care for older adults. Systems, provider, and patient factors are barriers to safe transitions and can contribute to morbidity and mortality in older adults. Safe transitions from ED to inpatient, ED to the SNF, or ED back to the community require a holistic approach such as the 4-MS: What Matters (patient goals of care), Medication, Mentation, Mobility, Safety, and Social Support. Clear written and verbal communication with the patient, caregivers, and other members of the interdisciplinary team is paramount in ensuring successful care transitions.
Acknowledgments
DISCLOSURE STATEMENT
LTS is funded to investigate geriatric emergency departments through NIH K23AG06128401. Reference to specific commercial products, manufacturers, companies, or trademarks does not constitute its endorsement or recommendation by the U.S. Government, Department of Health and Human Services, or Centers for Disease Control and Prevention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Nagurney JM, Fleischman W, Han L, Leo-Summers L, Allore HG, Gill TM. Emergency Department Visits Without Hospitalization Are Associated With Functional Decline in Older Persons. Ann Emerg Med 2017;69:426–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hastings SN, Oddone EZ, Fillenbaum G, Sloane RJ, Schmader KE. Frequency and predictors of adverse health outcomes in older Medicare beneficiaries discharged from the emergency department. Med Care 2008;46:771–7. [DOI] [PubMed] [Google Scholar]
- 3.Jawaro T, Bridgeman PJ, Mele J, Wei G. Descriptive study of drug-drug interactions attributed to prescriptions written upon discharge from the emergency department. Am J Emerg Med 2019;37:924–7. [DOI] [PubMed] [Google Scholar]
- 4.Briggs S, Pearce R, Dilworth S, Higgins I, Hullick C, Attia J. Clinical pharmacist review: a randomised controlled trial. Emerg Med Australas 2015;27:419–26. [DOI] [PubMed] [Google Scholar]
- 5.Lennox A, Braaf S, Smit V, Cameron P, Lowthian JA. Caring for older patients in the emergency department: Health professionals' perspectives from Australia - The Safe Elderly Emergency Discharge project. Emerg Med Australas 2018. [DOI] [PubMed] [Google Scholar]
- 6.Apker J, Mallak LA, Gibson SC. Communicating in the "gray zone": perceptions about emergency physician hospitalist handoffs and patient safety. Acad Emerg Med 2007;14:884–94. [DOI] [PubMed] [Google Scholar]
- 7.Leamy K, Thompson J, Mitra B. Awareness of diagnosis and follow up care after discharge from the Emergency Department. Australas Emerg Care 2019;22:221–6. [DOI] [PubMed] [Google Scholar]
- 8.Hastings SN, Barrett A, Weinberger M, et al. Older patients' understanding of emergency department discharge information and its relationship with adverse outcomes. J Patient Saf 2011;7:19–25. [DOI] [PubMed] [Google Scholar]
- 9.Han JH, Bryce SN, Ely EW, et al. The effect of cognitive impairment on the accuracy of the presenting complaint and discharge instruction comprehension in older emergency department patients. Ann Emerg Med 2011;57:662–71 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.King BJ, Gilmore-Bykovskyi AL, Roiland RA, Polnaszek BE, Bowers BJ, Kind AJ. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc 2013;61:1095–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Werner RM, Coe NB, Qi M, Konetzka RT. Patient Outcomes After Hospital Discharge to Home With Home Health Care vs to a Skilled Nursing Facility. JAMA Intern Med 2019;179:617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tyler DA, McHugh JP, Shield RR, Winblad U, Gadbois EA, Mor V. Challenges and Consequences of Reduced Skilled Nursing Facility Lengths of Stay. Health Serv Res 2018;53:4848–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Werner RM, Konetzka RT, Qi M, Coe NB. The impact of Medicare copayments for skilled nursing facilities on length of stay, outcomes, and costs. Health Serv Res 2019;54:1184–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reidt SL, Holtan HS, Larson TA, et al. Interprofessional Collaboration to Improve Discharge from Skilled Nursing Facility to Home: Preliminary Data on Postdischarge Hospitalizations and Emergency Department Visits. J Am Geriatr Soc 2016;64:1895–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A meta-analysis of "hospital in the home". Med J Aust 2012;197:512–9. [DOI] [PubMed] [Google Scholar]
- 16.Carpenter CR, Shelton E, Fowler S, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med 2015;22:1–21. [DOI] [PubMed] [Google Scholar]
- 17.Apostolo J, Cooke R, Bobrowicz-Campos E, et al. Predicting risk and outcomes for frail older adults: an umbrella review of frailty screening tools. JBI Database System Rev Implement Rep 2017;15:1154–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Improvement IfH. Age-Friendly Health Systems. 2019.
- 19.Choi YJ, Kim H. Effect of pharmacy-led medication reconciliation in emergency departments: A systematic review and meta-analysis. J Clin Pharm Ther 2019;44:932–45. [DOI] [PubMed] [Google Scholar]
- 20.Merel SE, Paauw DS. Common Drug Side Effects and Drug-Drug Interactions in Elderly Adults in Primary Care. J Am Geriatr Soc 2017;65:1578–85. [DOI] [PubMed] [Google Scholar]
- 21.Carpenter CR, Bassett ER, Fischer GM, Shirshekan J, Galvin JE, Morris JC. Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: brief Alzheimer's Screen, Short Blessed Test, Ottawa 3DY, and the caregiver-completed AD8. Acad Emerg Med 2011;18:374–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kennelly SP, Morley D, Coughlan T, Collins R, Rochford M, O'Neill D. Knowledge, skills and attitudes of doctors towards assessing cognition in older patients in the emergency department. Postgrad Med J 2013;89:137–41. [DOI] [PubMed] [Google Scholar]
- 23.Taylor A, Broadbent M, Wallis M, Marsden E. The use of functional and cognitive assessment in the emergency department to inform decision making: A scoping review. Australas Emerg Care 2018;21:13–22. [DOI] [PubMed] [Google Scholar]
- 24.Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr 2014;14:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scott M, Shaver N, Lapenskie J, et al. Does inpatient palliative care consultation impact outcomes following hospital discharge? A narrative systematic review. Palliat Med 2020;34:5–15. [DOI] [PubMed] [Google Scholar]
- 26.Southerland LT, Vargas AJ, Nagaraj L, Gure TR, Caterino JM. An Emergency Department Observation Unit Is a Feasible Setting for Multidisciplinary Geriatric Assessments in Compliance With the Geriatric Emergency Department Guidelines. Acad Emerg Med 2018;25:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tobiano G, Chaboyer W, Teasdale T, Raleigh R, Manias E. Patient engagement in admission and discharge medication communication: A systematic mixed studies review. Int J Nurs Stud 2019;95:87–102. [DOI] [PubMed] [Google Scholar]
- 28.Lee JS, Napoles A, Mutha S, et al. Hospital discharge preparedness for patients with limited English proficiency: A mixed methods study of bedside interpreter-phones. Patient Educ Couns 2018;101:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scott AM, Li J, Oyewole-Eletu S, et al. Understanding Facilitators and Barriers to Care Transitions: Insights from Project ACHIEVE Site Visits. Jt Comm J Qual Patient Saf 2017;43:433–47. [DOI] [PubMed] [Google Scholar]
- 30.Jain N, Bernacki RE. Goals of Care Conversations in Serious Illness: A Practical Guide. Med Clin North Am 2020;104:375–89. [DOI] [PubMed] [Google Scholar]