Abstract
Background
Women in LMICs are important agricultural actors; however, these same women, and with their children, suffer high rates of acute malnutrition during armed conflicts.
Methods and Findings
A review was undertaken of peer-reviewed literature to describe how armed conflict drives acute malnutrition in pregnant and breastfeeding women and their children. Armed conflict factors driving malnutrition were conceptualized as belonging to one of eight overarching drivers.
Conclusion
Future research must examine the effect of specific drivers on acute malnutrition in order to improve predictive models; emphasize inclusion of pregnant and breastfeeding participants in studies; elucidate the role of peacekeepers in mitigating the risk of acute malnutrition; explore how to support breastfeeding women living in armed conflict situations; and explore how displaced populations affect host communities’ food systems.
Keywords: Food security, malnutrition, armed conflict, agriculture
1. Introduction
Approximately 2 billion people, over a quarter of the world’s population, live in countries affected by armed conflict (1). Armed conflict is an important driver of acute malnutrition, a rapid form of weight loss brought on by starvation and/or disease (2, 3). An estimated 124 million people are exposed to crisis-level food insecurity, a direct contributor to acute malnutrition, and, at present, all countries at risk of crisis levels of food insecurity experience significant armed conflict (3–5). For 60 percent of people experiencing acute food insecurity, armed conflict is a key precipitating factor (4). Malnutrition is an imbalance between the intake of energy or nutrients and the body’s nutrition requirements. While the term malnutrition encompasses both undernutrition (e.g., moderate and severe acute malnutrition; stunting, underweight; and micronutrient deficiencies) and overnutrition (e.g., overweight and diet-related noncommunicable diseases), phenomena that frequently exist simultaneously within a population, this article focuses exclusively on armed conflict as a driver of undernutrition-related acute malnutrition (6).
Women are critical actors in most low and middle-income country (LMIC) food production systems, but they and their children endure disproportionate burdens of malnutrition (7, 8). Due to their increased nutrition needs, pregnant and breastfeeding women are frequently at particularly high risk of experiencing acute malnutrition as a result of armed conflict (9, 10). Malnutrition during pregnancy can be deleterious to both child and mother by increasing the risk of obstructed labor, premature or low-birth-weight babies, postpartum hemorrhage, and increased maternal mortality due to severe anemia (11). Malnutrition’s effect on lactating mothers is less clear, but reports suggest that breastmilk quality is negatively impacted by maternal malnutrition (12, 13). Given their importance as agricultural production actors and as the primary caregivers to young children, women’s food security and nutritional status are strongly associated with their children’s nutritional status (14, 15). While acute malnutrition is damaging to individual’s health all along the life course, it is particularly harmful for young children. Acute malnutrition affects 51 million children under-five worldwide and is one of the greatest contributors to mortality within this age range (16, 17). Additionally, acute malnutrition drives morbidity in children by increasing susceptibility to infections and delaying illness recovery (17). Scholarship supports the theory that individuals’ health and development trajectories are heavily influenced by life conditions experienced between conception and the first two years of life (18, 19). Children who experience malnutrition in utero or during these first developmentally sensitive years of life risk never meeting their growth and cognitive potential (20, 21). Malnutrition in early childhood has been associated with reduce later-life brain size, reduced neural synapse formation, and lower concentrations of neurotransmitters and growth factors, leading to, among other outcomes, reduced sensitivity of cerebral cortex structures to neural stimulation (22). This reduction in cortical sensitivity may persist beyond the period of undernutrition and result in reduced lifelong cognitive functioning (20, 23). The developmentally sensitive 1,000 days between conception and two years of age demands that researchers assess the nutritional status of pregnant women and child/breastfeeding dyads when seeking to examine the full range of factors that influence children’s nutritional status.
Conceptual framework
This article adopts Young’s (2020) adaptation of the UNICEF conceptual framework on the causes of malnutrition and death (24, 25). The framework is an ecological model that suggests that malnutrition is the product of immediate, underlying, and basic/systemic events. Improvements to basic/systemic portion of the original UNICEF framework were made thanks to Young’s further elucidation of the upstream factors of acute malnutrition (figure 1). Within this revised model, additional emphasis has been placed on the systemic causes of acute malnutrition. This was accomplished by expanding on the basic/systemic causes section of the original UNICEF framework through the addition of the environment & seasonality, systems, formal, & informal institutions, and livelihood systems sections. While originally adapted for African dryland regions, this revised conceptual framework is relevant to any number of climatic and geographic regions because of its recognition that while climate change and resource scarcity are at the base of much of malnutrition, formal and informal institutions and political systems mediate their effects (24). This includes creating vulnerabilities to armed conflict.
Figure 1:
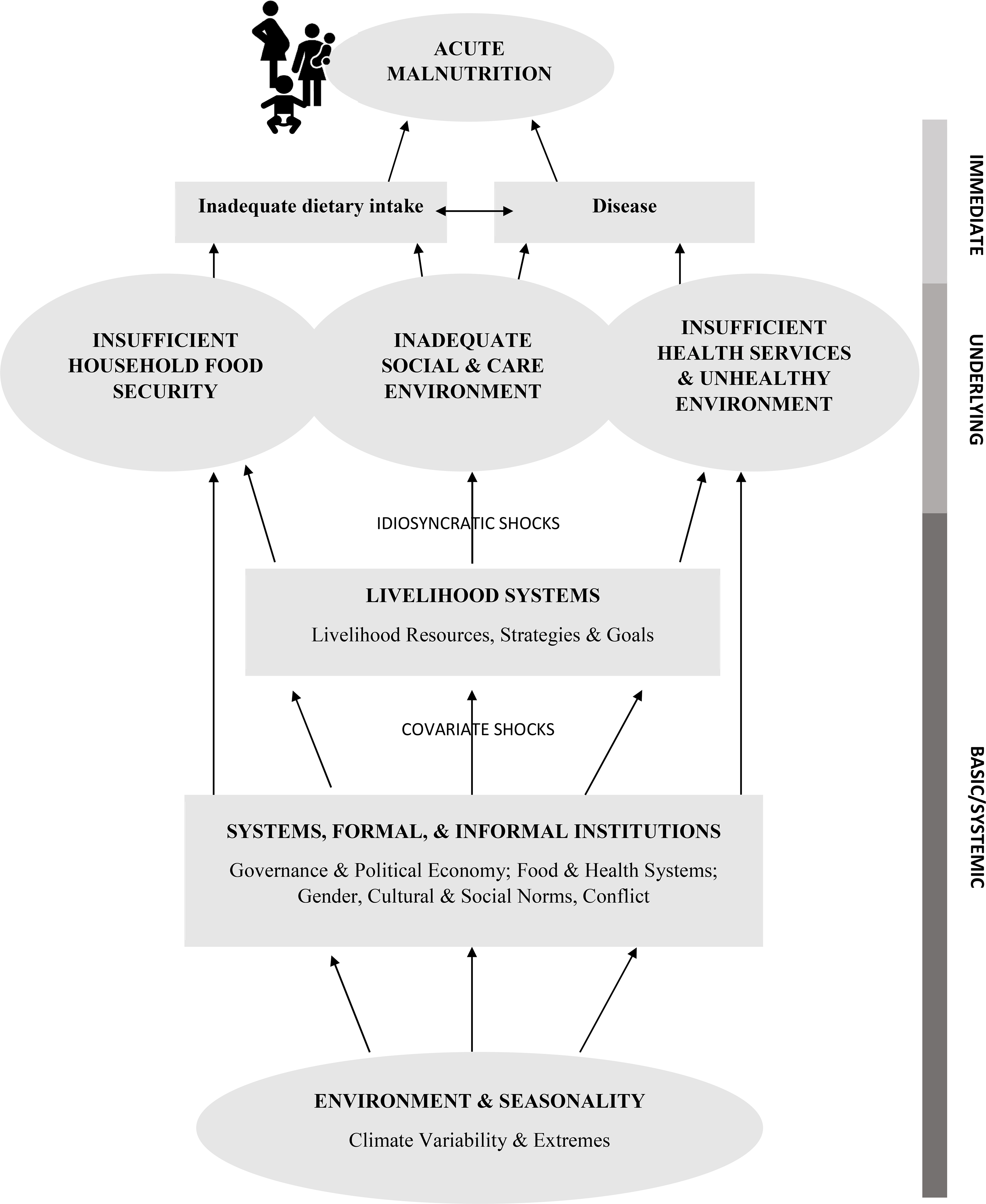
Young’s (2020) conceptual framework for addressing acute malnutrition
While there is common agreement that armed conflict is responsible for grave exacerbations in food insecurity, an exploration of the particular means by which armed conflict drives acute malnutrition does not yet appear to exist (3, 5). The objective of this review is to synthesize factors identified in peer-reviewed literature that relate armed conflict to acute malnutrition in children under 5 years and pregnant and breastfeeding women in order to inform the direction of future food security and malnutrition mitigation research.
2. Methods
A review of the literature was conducted to assess how armed conflict worsens acute malnutrition in pregnant and breastfeeding women and children. After collaborating with a medical research librarian to create a comprehensive search strategy, literature searches were conducted as recently as February 2019 in the literature databases PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Scopus. Search terms (table 1) were adapted to each database in order to optimize search results. Publications were restricted to those written in English and French language.
Table 1:
Key search terms used to detect database literature (CINAHL, PubMed, Scopus)*
| Armed conflict | Populations | Malnutrition |
|---|---|---|
| Warfare | Child | Nutrition |
| Armed | Infant | Malnutrition |
| Conflict | Toddler | Malnourish |
| Civil Unrest | Youth | Undernutrition |
| War | Pregnant women | Wasting |
| Military | Breastfeeding women | |
| Conflict | Lactating | |
| Prenatal care |
Index terms used when available.
Inclusion and exclusion criteria defined a priori guided the selection of publications for inclusion in the review (table 2). Four criteria were considered when reviewing publications for inclusion. Research described in the publication must have occurred during an armed conflict or within a post-conflict setting. The operational definition of armed conflict utilized was derived from Guha-Sapir’s definition as those political conflicts in which one or more armed factions seek to wrest control of a portion of all of the State, and in which 1,000 or more people have been killed during the course of the conflict (26). The populations of interest included pregnant or breastfeeding women and children as old as 18 years of age. Only reports documenting cases of moderate and severe acute malnutrition associated with armed conflict events taking place in countries with a lower or middle income per capita gross nation income were considered for inclusion (27). Cases of chronic malnutrition were excluded as their slow onset is not usually due to the immediate effects of armed conflict-related food or sanitation system destruction.
Table 2:
Review inclusion and exclusion criteria
| Criteria | Qualifications |
|---|---|
| Studies | Randomized control trials, quasi-experimental studies, non-experimental studies, and qualitative studies in which a clear link between armed conflict and malnutrition was stated. |
| Participants | Studies were included if participants were pregnant or breastfeeding women or children as old as 18 years of age who were living in a conflict zone or post conflict setting. Studies were not included if they did not include one of these populations of interest living within one of these contexts. |
| Settings | Studies were included if the study took place during an armed conflict or post conflict setting. Studies were also included if the study took place in a zone outside of the area of direct conflict but with participants who had been affected and displaced by the conflict. |
| Intervention | Studies were included if they documented the effects of an armed conflict between one or |
| Outcome measures | more state or non-state groups. Studies were included if an observation or hypothesis describing how armed conflict drove malnutrition. |
While assessment of nutritional status is dependent on an array of factors, such as age, sex, and genetic differences in growth, international anthropometric measurement standards for young children have been developed to help detect cases of acute malnutrition (6, 28, 29). For children aged six to 59 months, a weight-for-height (WHZ) z-score of less than −2 or mid-upper arm circumference (MUAC) of 11.5 to 12.5 cm is considered moderately malnourished, while a z-score of less than −3 or a MUAC of less 11.5 cm is considered severely malnourished (29). Findings of edema in the lower limbs upon examination in combination with one or more of these measurements is strongly suggestive of acute malnutrition. In pregnant and lactating women, no universal anthropometric standard for acute malnutrition exists; however, MUACs of between 18.5 and 22.9 cm and less than 18.5 cm have been described by humanitarian health guidelines as cutoff scores for moderate and acute malnutrition (6). Table 3 offers a comparison of Sphere Handbook anthropometric measurement standards across these groups (6).
Table 3:
Sphere anthropometric measurement standards for acute malnutrition in pregnant and breastfeeding children and young children
| Groups | Degree of severity | MUAC (mm)* | WHZ (SD) † | Nutritional edema |
|---|---|---|---|---|
| Pregnant women | Moderate | 18.5 – 22.9 cm | ||
| Severe | <18.5 cm | |||
| Breastfeeding women | Moderate | 18.5 – 22.9 cm | ||
| Severe | <18.5 cm | |||
| Children 6–59 months | Moderate | 11.5 – 12.5cm | <-2 SD | |
| Severe | <11.5 cm | <-3 SD | X |
Mid-upper arm circumference
Weight-for-Height Z-score
Body mass index-for-age
Operational definitions of moderate and severe malnutrition varied between publication authors; however, all were in near or complete agreement with the internationally recognized pediatric standards (30). While articles did not need to document prevalence or incidence rates for these anthropometric measures, they must have clearly indicated the focus was on moderate or severe malnutrition. Finally, articles’ authors or, in the case of qualitative studies, respondents must have made observation about how armed conflict served to destabilize food and sanitation systems and drive increased rates of acute malnutrition.
Following abstract and full-text review, data was extracted from selected publications and their level of evidence and quality were appraised using Dearholt and Dang’s Johns Hopkins Nursing Evidence Appraisal Tool (31). An inductive approach was employed during thematic synthesis. Within the approach studies were read and re-read to gain familiarity with findings and concepts were recorded. Overarching drivers for this review were then constructed to explain similar drivers of malnutrition described by the literature (32). Overarching drivers were placed within the Young’s adapted UNICEF conceptual framework on the causes of malnutrition (figure 1) and developed into the subsections of review results section (33).
Sixty articles were identified in CINAHL, 361 in PubMed, and 669 in SCOPUS using the above described search protocol. Of these 1,090 articles, 270 duplicates were removed. All remaining 820 articles’ titles and abstracts were reviewed for relevance. Six hundred fifty-four did not meet inclusion criteria during title and abstract screening. Following full-text review of the remaining 166 articles, 19 studies met all criteria required for inclusion in this review (figure 2).
Figure 2:
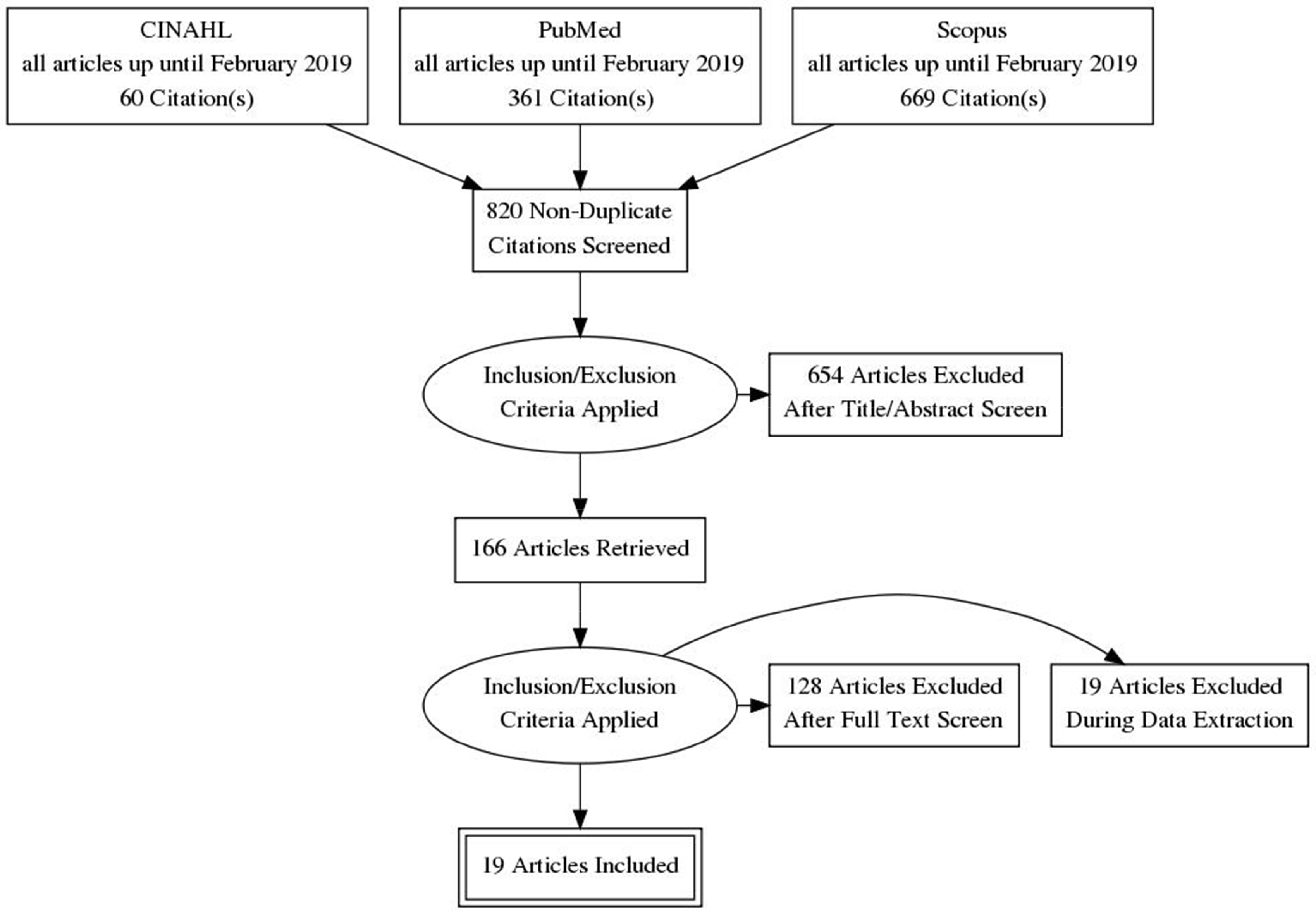
Flowchart of included and excluded literature.
3. Results
Table 4 provides the research methods and quality scores of the studies included in this review. In these publications, possible armed conflict drivers of acute malnutrition were extracted from study discussion sections in quantitative studies and from respondent quotes in qualitative studies. Individual study bias was not assessed because most studies did not test hypothetical armed conflict-related drivers of acute malnutrition. A meta-analysis of acute malnutrition prevalence was not conducted due to differences in how nutrition status was measured across studies.
Table 4:
Included articles methods and quality appraisals (n=19)
| Characteristic | No. |
|---|---|
| Research method employed | |
| Quasi-experimental | 3 |
| Non-experimental | 13 |
| Mixed methods | 1 |
| Qualitative | 2 |
| Quality score | |
| A: Comprehensive literature reviews, sufficient sample sizes, and generalizable results | 6 |
| B: Supporting literature reviews, sufficient sample sizes, but not broadly generalizable results | 12 |
| C: Little evidence and inconsistent results | 1 |
Eight overarching drivers emerged after reviewing the 19 included articles that help to explain how armed conflict drives acute malnutrition in pregnant and breastfeeding women and children. These drivers included (1) food as a weapon of war; (2) infrastructure destruction; (3) destruction of agriculture and persistent insecurity; (4) malabsorption malnutrition; (5) loss of family providers; (6) foreign economic embargoes; (7) the stress of displacement on host communities; and (8) maternal stress. Articles included in this review and the drivers emerging from each publication are provided in table 5. Drivers extracted from articles have been overlayed onto Young’s conceptual framework in order to illustrate how armed conflict disrupts food systems at multiple levels and serves to drive acute malnutrition (figure 3).
Table 5:
Included articles presented in chronological order by conflict years studied (1989–2017)
| Groups of interest included | Main outcome | ||||||
|---|---|---|---|---|---|---|---|
| Authors (pub. year) Quality * (Evidence level/Quality) Country |
Conflict (year(s) of study) | Study design &sample size | Pregnant | Breastfeeding | Children | Armed conflict drivers of acute malnutrition specific to studied conflict | Overarching themes |
| Reid et al. (2007) II/B Haiti |
Haitian coup d’état (1989–1996) | Quasi-experimental Interrupted time series. Children 0–24 mo. (n=1,593) |
X | Economic embargoes | Foreign economic embargoes | ||
| Ascherio et al. (1992) III/A Iraq |
Gulf War (1991) | Non-experimental Retrospective case- control. Children aged 0–60 months (n =16,076 living, 768 dead). |
X | Economic embargo resulting in increased food prices Water treatment infrastructure destruction |
Foreign economic embargoes Malabsorption malnutrition |
||
| Field & Russell (1992) III/B Iraq |
Gulf War (1991) | N on-experimental Observational study. Children 0–59 months (n =680). |
X | Water infrastructure damage resulting in increase in waterborne infectious diseases. Increase in food prices due to ongoing embargo. Deteriorating breast-feeding practices. |
Malabsorption malnutrition Foreign economic embargoes Maternal stress |
||
| Kinfu (1999) III/B Ethiopia |
Ethiopian Civil War (1992) |
Non-experimental Cross-sectional survey of children 6–59 mo. (n =11,088) |
X | Militarization of economy and neglect of agricultural and health sectors Reduced agricultural labor force due to coercive conscription for military service |
Infrastructure destruction Loss of family providers | ||
| Toole et al. (1993) III/C Bosnia and Herzegovina |
Bosnian War (1993) | N on-experimental Public health needs assessment. |
X | X | Economic embargoes Military restriction of food availability in predominantly Muslim regions of Bosnia Destruction of public water and sanitation systems |
Foreign economic embargoes Food as a weapon of war Malabsorption malnutrition |
|
| Curtis (1995) III/B Bosnia and Herzegovina |
Bosnian War (1994) | Qualitative Interviews with Muslim refugee households (n=5). |
X | X | Military restriction of food availability in predominantly Muslim regions of Bosnia. | Food as a weapon of war | |
| Andersson et al. (2010) III/A Bosnia and Herzegovina and the Republica Srpska |
Bosnian War (1994–1997) | Non-experimental Four cross-sectional cluster surveys. Children 1–12 months (n =1123). |
X | Poor breast-feeding practices | Maternal stress | ||
| Goma Epidemiology Group (1995) III/B Democratic Republic of the Congo |
Rwandan Genocide (1994) | Non-experimental Three cross-sectional surveys. Children 6–59 months (n =1,984). |
X | Conflict-induced displacement to regions unable to support nutritional needs of displaced. Malabsorption secondary to diarrheal disease related to poor hygiene. Military restriction of food delivery. |
Stress of displacement on host communities Malabsorption malnutrition Food as a weapon of war |
||
| Aaby et al. (1999) II/B Guinea-Bissau |
Guinea-Bissau Civil War (1998–1999) | Non-experimental Cross sectional survey. Children aged 9–23 months (n = 422). |
X | Communicable disease-related malnutrition caused by crowding and unhygienic conditions resulting from influx of internally displaced populations (IDPs) from conflict areas |
Malabsorption malnutrition Stress of displacement on host communities |
||
| McGadney- Douglass & Douglass (2008) III/B Ghana |
Konkomba- Nanumba Conflict (1999–2005) | Qualitative interviews Interviews with IDP women (n=20) |
X | Death or migration due to conflict of male providers Military curfews restricting agricultural and market activities |
Loss of family providers Food as a weapon of war |
||
| Guha-Sapir et al. (2005) III/B Angola Democratic Republic of the Congo South Sudan Ethiopia |
Angolan Civil War (2000–2004) War in Darfur (2000–2004) Second Congo War (2000–2004) Eritrean-Ethiopian War (2000–2004) |
Non-experimental Retrospective analysis in four sub-Saharan African countries. Children 6–59 months. |
X | Humanitarian aid organizations unable to access displaced populations in government- controlled cities and towns | Food as a weapon of war | ||
| Herp et al. (2003) III/B Democratic Republic of the Congo |
Second Congo War (2001) | Non-experimental Cross sectional study using two-stage cluster sampling of households (n =4,527). |
X | X | Government troops looting of food stocks | Destruction of agriculture and persistent insecurity | |
| Grandesso et al. (2005) III/A South Sudan |
War in Darfur (2004) | Non-experimental Three cross-sectional surveys of displaced population. Children 659 months (n =3,785). |
X | Lack of arable land for cultivation near displacement camps No nearby markets for affordable foods Unable to locate food outside of IDP camps due to chronic insecurity in regions |
Destruction of agriculture and persistent insecurity Infrastructure destruction Destruction of agriculture and persistent insecurity |
||
| Guerrier et al. (2009) III/B Chad |
War in Darfur/ Chadian Civil War (2006) |
Non-experimental Three cross-sectional studies of displaced population. Children 659 months (n =2,761). |
X | Exacerbation of food insecurity due to influx of IDPs from conflict areas Insecurity-driven food price increases partly due to disruptions in trade |
Stress of displacement on host communities Infrastructure destruction |
||
| Olwedo et al. (2008) III/B Uganda |
Lord’s Resistance Army insurgency (2006) | Mixed methods Cross sectional survey of displaced population. Children 359 mo. (n =678). Focus group and key-informant interviews of caretakers and camp and zone leaders. |
X | Lack of arable land due to displacement from home locales | Stress of displacement on host communities | ||
| Kandala et al. (2011) III/A Democratic Republic of the Congo |
Second Congo War (2007) | Non-experimental Cross sectional study of survey data. Children 0–59 mo. (n =3,663). |
X | Destruction of food production infrastructure Maintenance of low food reserves due to fears of insecurity Economic migration of family providers |
Destruction of agriculture and persistent insecurity Infrastructure destruction Loss of family providers |
||
| Ghazi et al. (2013) III/B Iraq |
Iraq War (2009) | Non-experimental Cross-sectional study. Children aged 3 to 5 years (n =220). |
X | Death due to armed conflict of one or more household provider. | Loss of family providers | ||
| Dunn (2018) II/A Nigeria |
Boko Haram insurgency (2009–2013) | Quasi-experimental Longitudinal analysis pre- (2008) and post-conflict (2013) of WHZ scores in affected and unaffected zones. Child under 60 months. (Pre-conflict n = 7,978; post-conflict n = 5,034) |
X | Reduced food production in conflict regions Increased food transportation costs into conflict zones Reduced availability in markets due to insecurity |
Destruction of agriculture Infrastructure destruction Food as a weapon of war |
||
| Tranchant et al. (2018) II/A Mali |
Northern Mali Conflict (2012 & 2017) | Quasi-experimental Longitudinal analysis. Children 2–5 years at baseline (2012 n = 2,449; 2017 n =1,634) |
X | Reduced mobility to markets and farms Inability of aid organizations to provide humanitarian assistance to areas experiencing armed conflict |
Destruction of agriculture Food as a weapon of war |
||
Figure 3:
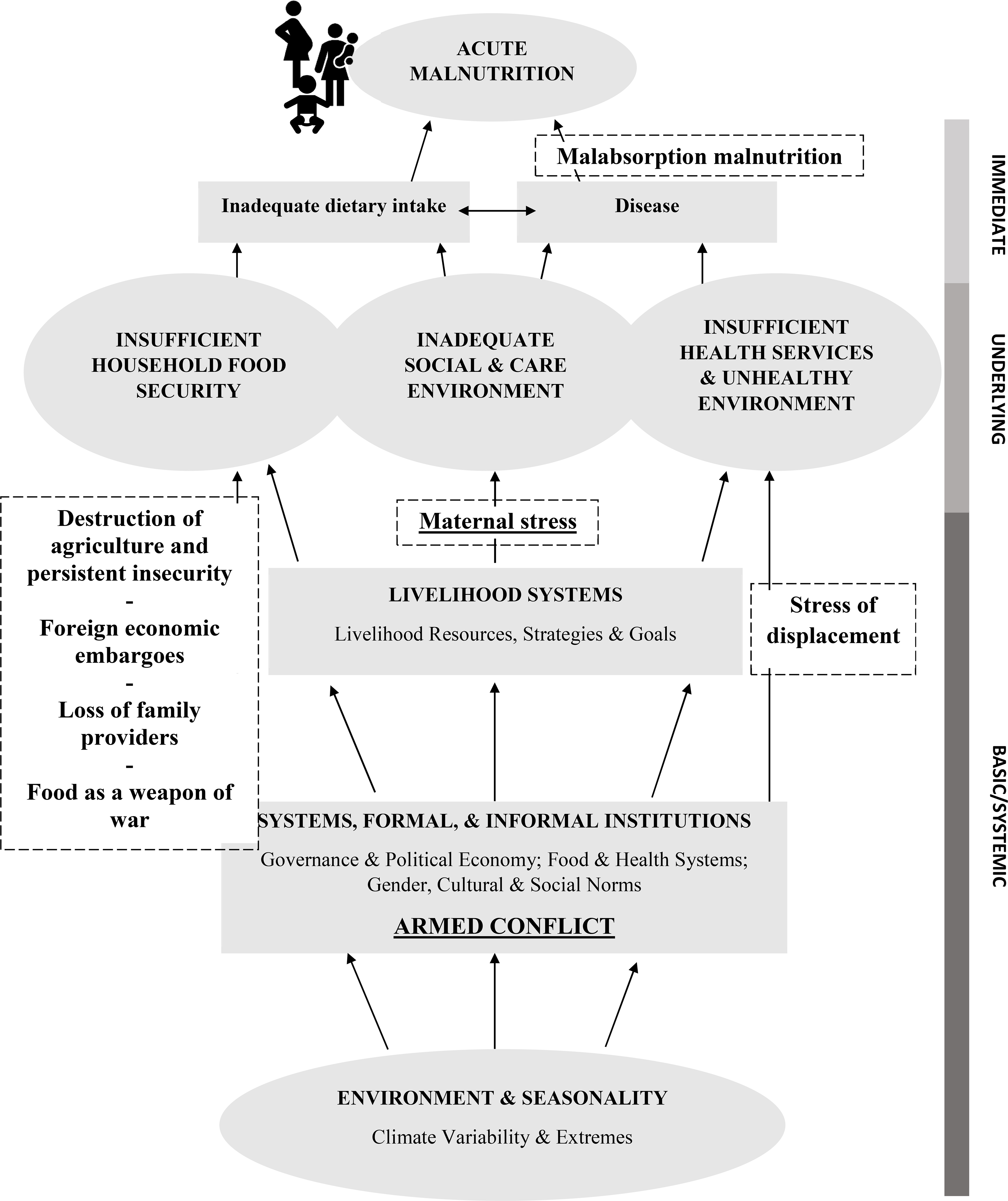
Armed conflict’s drivers of acute malnutrition
3.1. Food as a weapon of war
Seven publications described instances in which militaries and non-state armed groups punished civilian populations by limiting food. Intentionally restricting flows of humanitarian aid has serious health consequences for populations enduring armed conflict by contributing to increased food insecurity and malnutrition rates. While studying sectarian conflict in Northern Mali, Tranchant et al. (2018) determined that access to food aid decreased as proximity to armed group stronghold regions increased, resulting in a lower likelihood of adequate food consumption or micronutrient diversity (34). Similar restrictions to food markets were observed in Northern Nigeria during the Boko Haram insurgency (35).
Nations’ own armed forces have engaged in similar tactics (36). Researchers noted that during the displacement of ethnic Hutus from Rwanda into the Democratic Republic of the Congo (DRC) in the immediate aftermath of the Rwandan Genocide that Rwandan political and military leaders sought to reduce access by humanitarian organizations to refugee populations living in refugee camps along the Rwanda/DRC border (37). Military restriction of humanitarian aid organizations into conflict zones was also reported to have occurred during the Angolan Civil War, the War in Darfur, the Second Congo War, and the Eritrean-Ethiopian War (26). Lastly, military restriction of food availability within predominantly Muslim regions of Bosnia during the Bosnian War by Serbian forces was reported by two studies reporting on barriers to food security during the conflict (38, 39).
3.2. Infrastructure destruction
Six publications described how infrastructure destruction was perceived as having an important impact on food insecurity and acute malnutrition. Armed conflict upends delicate food systems by destroying infrastructure vital for transporting and delivering goods. Underinvestment in health systems and agricultural promotion in favor of military spending frequently precedes such collapses (40, 41). Violence disincentives travel along normal transit routes, discourages maintenance of commercial food stores in conflict regions, and hinders normal market activity. The collapse of logistics chains reduces food availability and drives up the price of remaining food items. At the height of their power, the Boko Haram insurgency was responsible for severe reductions in transportation through areas under their control as well as decreases in market functionality as many village-level traders became increasingly concerned for their safety (35).
The effect of armed conflict creates a gradient whereby those living closest to the conflict incur the greatest loss of food security. Studies from Northeast Nigeria, Chad, and South Sudan indicated that those living in rural regions with already tenuous links to outside food markets suffered high rates of acute malnutrition as they became the centers of ongoing large-scale violence (34, 35, 42, 43). Commercial food surpluses are also sometimes kept to a minimum in such insecure settings. In eastern provinces of the DRC, low commercial stores of food crops were maintained in case of destruction of food stores during the Second Congo War (41). Lacking the resilience necessary to endure these stresses, fragile infrastructure and logistic networks quickly collapsed under the weight of mass armed conflict (3). As a result, non-combatants are exposed to worsened food insecurity and increasing rates of acute malnutrition.
3.3. Destruction of agriculture and persistent insecurity
Five publications referenced destruction of agriculture and persistent insecurity as potential driver of acute malnutrition. Destruction of crops in fields as well as looting of stored agricultural products heavily contribute to food insecurity and malnutrition during armed conflict. In attempts to weaken resistance, armed groups raze fields, destroy or loot crop stores, and kill livestock of communities perceived hostile to their goals (41, 44). This tactic can be particularly devastating in LMIC countries in Latin America, sub-Saharan Africa, and Southeast Asia in which 70 percent of calories consumed are produced on smallholder farms by subsistence farmers (45, 46).
Persistent insecurity also reduces individuals’ capacity to travel to and from fields as well as engage in the numerous steps integral to agricultural production. As 60 percent of women employed in Oceania, sub-Saharan Africa, and Southeast Asia work in agriculture (47), ongoing insecurity poses a threat to women and children’s immediate safety and, by extension, future crop yields of family fields. This phenomenon has been observed in both rural home regions as well as in displaced population camps. In both the Mopti region of Mali and in the Lake Chad Basin region, chronic insecurity from sectarian violence has decreased household food consumption and micronutrient availability (34, 35). Even the protection of displaced population camps is oftentimes insufficient to ensure the safe movement of women. In South Sudan during the War in Darfur, women residing in internally-displaced persons (IDP) camps reported experiencing violence as they traveled to and from their fields (43).
3.4. Malabsorption malnutrition
Five publications included references to malnutrition related to infection. Malnutrition and infection exist in a reciprocal relationship. Malnutrition increases individuals’ susceptibility to communicable infections, while infection predisposes individuals to reduced nutrient absorption. Enteric infections exert a particularly strong influence on nutrient absorption and malnutrition (48, 49). Enteric infections due to Cholera, enterotoxic Eschericia, amoebic or bacillary dysentery, and Cryptosporidium parvum are common diarrheal diseases found in humanitarian settings that can cause intestinal malabsorption and impaired weight gain (50, 51). This reduced absorptive capacity is an important consideration at all life stages but is a particularly salient issue during early life when absorption of key nutrients is critical to normal growth and development (48). Armed conflict events can destroy many of the water sanitation and hygiene systems designed to safeguard public health, thereby increasing the likelihood of the spread of these enteric pathogens (52, 53).
In Guinea-Bissau, during its 1998–1999 civil war, increases in childhood malnutrition outside the zone of conflict were credited largely to unhygienic conditions resulting from overcrowding, created as waves of newly displaced persons fled from violence (54). The displacement of refugees from Rwanda during the Rwandan Genocide into the North Kivu region of the DRC triggered cholera outbreaks in the makeshift refugee camps, which were blamed for increasing child malnutrition to crisis levels (37). In the Basra region of Iraq during the Gulf War increased rates of childhood malnutrition followed as sanitation infrastructure was destroyed or fell into disrepair (52, 53). Similar attacks on the public water and sanitation systems in besieged towns of Bosnia and Herzegovina during the Bosnian War added the threat of enteric disease transmission and malnutrition during an ongoing religious pogrom (39).
3.5. Loss of family providers
Five articles included descriptions of how loss of family providers negatively affected pregnant and breastfeeding women’s and children’s food security and acute malnutrition. Most developing countries lack strong formal social safety services. As a result, children and other dependents are thrown into precarious situations when family providers and traditional community support structures are lost. During the Ethiopian Civil War, forced military conscription left whole communities without the labor force necessary to sustain sufficient agricultural production (40). In Baghdad City during the Iraq War, death of a household’s mother or father was positively associated with increased odds of children in the home being moderately malnourished (55). Abandonment of families during times of deprivation following armed conflicts commonly occurs when men and women leave their homes in search of economic opportunity elsewhere, sometimes never to return (36, 41).
3.6. Foreign economic embargoes
Four articles cited the damaging effect of foreign economic embargoes on food security and acute malnutrition. Economic embargoes are frequently instituted by the international community against nation-states engaged in armed conflicts that have violated international norms. These actions, though, may indirectly drive food insecurity and malnutrition within a population’s most vulnerable groups (39, 52, 53, 56). While the intent of such sanctions is to alter the behavior of elites within the country, the true victims are those with little control over the country’s political affairs.
After the invasion of Kuwait by Iraq in 1990 severe economic sanctions by coalition countries halted Iraqi economic growth and threatened the health of many citizens. Beginning in 1991, Iraq experienced increases in mortality in children under five years of age as compared to pre-war rates (52). Price surveys of standard food items in Southern Iraq during this same time indicated price increases of three- to twenty-fold their typical costs during this same time (53). As Iraq saw no direct military intervention by coalition forces during the war, these excess deaths have been credited to a constellation of factors, such as rising food prices related to embargoes (52).
An economic embargo instituted during Haiti’s 1991 coup d’état produced an increased incidence of severe malnutrition among children less than 24 months of age being followed by a medical non-governmental organization. It is important to note that even though sanctioning countries had made humanitarian and medical exceptions in their sanctions the researchers’ findings indicated that despite these exceptions vulnerable populations’ worsening nutritional statuses were closely correlated to the institution of these embargoes (56).
3.7. The stress of displacement on host communities
Four articles wrote about the stress placed on host communities following the influx of displaced populations. Armed conflict’s effect on food security and malnutrition are felt by populations who are within geographic proximity to areas enduring conflict as armed conflict triggers the displacement of civilian populations into safer surrounding regions. These displaced populations can overwhelm already strained food, water, sanitation, hygiene, and housing systems in these safer regions. Tenuous host community food security circumstances can quickly be tipped into a state of disaster by the influx of displaced populations seeking assistance.
During the Guinea-Bissau Civil War civilians living in the capital city of Bissau, the major site of conflict, fled into neighboring suburban regions. While fortunate to have fled heavy fighting, these individuals were forced to pack into the homes of friends and family or to amass into informal IDP camps. These crowded settings worsened existing drivers of acute malnutrition already mentioned (e.g., food unavailability and malabsorption malnutrition secondary to degraded sanitation and enteric diseases) for the displaced populations and members of the host community. Ultimately, elevated rates of childhood acute malnutrition in displaced and host community children did not improve until displaced populations moved back to their homes in the capital (54). Influxes of displaced populations stressing local capacity was also observed in Uganda during the Lord’s Resistance Army insurgency, in Eastern Chad during the Chadian Civil War and War in Darfur, and in Eastern DRC in the aftermath of the Rwandan Genocide (37, 42, 57). While not an immediate cause of acutely high levels of malnutrition, mass displacement serves an important moderating effect between armed conflict and food security for both displaced and non-displaced alike.
3.8. Maternal stress
Two studies reported on the negative effects of armed conflict on mothers’ breastfeeding practices. During the Bosnian War researchers found that infants were less likely to breastfeed longer than four months if living in communities near the frontlines of the conflict. While prevalence of breastfeeding remained stable in regions under study, rates of childhood malnutrition increased during the course of the three-year-long study (58). Further, mothers interviewed about breastfeeding practices during the Gulf War reported stressful life events and a perceived lack of breastmilk as reasons for cessation of breastfeeding in children older than 12-months in age (53).
4. Discussion
Most deaths related to armed conflict are not a direct result of violence itself, but rather due to the destruction of critical infrastructure, the tearing of social fabric, and the residual trauma that victims must endure for years after the conflicts end (35, 36). Armed conflict worsens conditions that were the main causes of morbidity and mortality before the conflict, such as malnutrition, diarrheal disease, and acute respiratory infections (35). Important drivers emerged from the literature describing how armed conflict disrupts food systems, increases food insecurity, and worsens acute malnutrition. Armed conflict has a general malevolent effect on society; however, key factors brought on by conflict are theorized to drive acute malnutrition (figure 3). While these drivers are not the exclusive factors by which populations grow increasingly malnourished, the literature does suggest that they can be found in multiple contexts and are posited to link armed conflict to increased food insecurity and malnutrition in pregnant and breastfeeding women and children.
4.1. Research implications
It is hoped that the conceptual framework with drivers of acute malnutrition described in this article will add to the overall body of literature necessary to inform the development of predictive models designed to estimate population-level rates of armed conflict-related acute malnutrition. Scholarship exists examining the relative impact of armed conflict on acute malnutrition (59–61). However, very few armed conflicts are followed by published accounts of how the conflict served to exacerbate food insecurity and increase malnutrition. Even fewer explore individual drivers of acute malnutrition. Only one study in this review tested a specific hypothesis about how an armed conflict-related driver would affect rates of acute malnutrition (56). As such, it is difficult to discern correct predictive patterns of expected mortality and nutrition (26). New research is needed that documents the effects of armed conflict on a population’s nutritional status. Given the complexity of the phenomenon, more qualitative inquiry is needed first in order to better understand how individuals living in armed conflict contexts and humanitarian aid stakeholders perceive how armed conflict drives acute malnutrition. Findings from qualitative inquiry will allow for the development of new testable hypotheses about the relative impact of specific armed conflict-related drivers on rates of acute malnutrition and serve to further refine acute malnutrition predictive models.
No identified publications specifically addressed how armed conflict drives malnutrition in pregnant women. The lack of available scholarship could be due to challenges in measurement. Pregnancy-related weight gain and edema makes body mass index (BMI), the gold standard of measuring adult body fat, less reliable in identifying malnutrition within this subpopulation. While MUAC has been shown to be a reliable alternative to BMI in measuring the nutritional status of pregnant women and the risk of low infant birthweight, the accuracy of cutoff values depend largely on geographic setting (Asia or Africa) (62). As such, little consensus exists around which cutoff values to use when seeking to identify pregnant women at risk of malnutrition or delivering a low-birth-weight infant during a humanitarian crisis (62, 63). Despite these challenges, many humanitarian aid organizations have adopted iteration’s of the Sphere Guideline’s MUAC ranges for moderate and severe acute malnutrition in pregnant women that have demonstrated acceptable sensitivity and specificity within their target population (64). The intent of this review was not to identify articles detailing measurement of malnutrition in pregnant women, however the absence of such research identified by the search criteria suggests that insufficient attention has been paid to how armed conflict drives malnutrition specifically in pregnant women. In order to account for their unique nutritional requirements and important role in the future health trajectories of children, research exploring how armed conflict drives acute malnutrition must be more intentional in including pregnant women.
Most publications included in this review discussed armed conflict-related drivers of acute malnutrition that were resolvable only by improvements in physical security. Studies suggest that increases in United Nations peacekeeping expenditures help to reduce the likelihood of renewed conflict after it has ended (65). For instance, a doubling of peacekeeping spending has been associated with a decrease in the risk of renewed conflict from 40 to 31 percent (66). Political scientists have an important part to play in exploring the factors associated with peacekeeping forces’ ability to ensure access by aid organizations to conflict-affected populations; secure or rebuild vital transport and storage infrastructure and sanitation systems; and to prevent violence against civilian populations by armed groups. Interdisciplinary research should examine how to improve peacekeeping missions’ effectiveness in mitigating the effects of armed conflicts on civilian food security and facilitating dialogue between parties.
Poor infant and young child feeding practices are prevalent even in the most peaceful of circumstances. Humanitarian emergencies and armed conflict only exacerbate this problem (67). Reduced breastfeeding during armed conflict is a complex topic that remains poorly understood. While maternal diet does appear to influence levels of essential fatty acids and certain micronutrient in breast milk, evidence also suggests that levels of most macronutrients are only weakly associated with maternal diet and that breastfeeding caregivers frequently produce relatively stable milk supplies except under the direst of nutritional circumstances (12, 68). Reports of poor breastfeeding practices in the humanitarian setting could be attributed to a complex array of psychosocial and environmental factors that impede feeding practices within the mother-infant dyad (69–71). Exclusive breastfeeding for the first six months of life, followed by the introduction of complementary solids at six months of age as breastfeeding continues for remainder of the first year of life, remains widely regarded as the best form of nutrition for infants as breastmilk provides sufficient nutrition to infants and serves to prevent infection by conferring immune system support (72, 73). Stress and trauma are important barriers to effective breastfeeding practices, but few supportive interventions have been trialed. In a review of infant and young child feeding supportive programs in humanitarian emergencies, Prudhon et al. found no studies reviewing the effectiveness of psychological support to caregivers (67). A review of existing psychological support interventions for pregnant and breastfeeding caregivers living through arm conflicts is needed in order to establish standards of care for these caregivers. Further, future research should further explore barriers to breastfeeding and to propose new behavioral health and psychosocial support interventions designed to promote breastfeeding initiation and duration during and following traumatic armed conflict.
Lastly, displacement can have a damaging effect on host communities living in equally fragile circumstances (42). As new arrivals strain available resources, host community members can develop many of the same needs as those of the displaced. Future research into displaced population health should be inclusive of vulnerable and marginalized populations from the host community who are most likely to be negatively affected by the arrival of those seeking help. Developing strategies to support the needs of displaced and non-displaced populations alike is a holistic approach to addressing the needs of all affected by armed conflict.
4.2. Limitations
Limitations exist in this review of the role of armed conflict in propagating food insecurity and malnutrition among pregnant and breastfeeding women and children. First, this review did not include grey literature, potentially missing other means by which armed conflict worsens food insecurity and acute malnutrition; however, as the objective of this review was to capture the peer-reviewed evidence base of this phenomenon these publications were not included. Second, most articles only discussed how armed conflict exacerbated issues of food insecurity and malnutrition as a secondary interest, typically following reports of malnutrition incidence or prevalence rates. Some researchers did treat this topic of primary interest in their publications and used informative qualitative and quantitative methods to contextualize these suspected drivers (38, 56, 58). Third, this review was conducted by a single author and cannot be considered a systematic review of the literature.
5. Conclusion
Acute malnutrition among vulnerable and marginalized populations due to armed conflict is a multidimensional problem that deserves a multi-disciplinary response. Future research must examine the effect of specific drivers on acute malnutrition in order to improve predictive models; emphasize the inclusion of pregnant and breastfeeding participants in studies; elucidate the role of peacekeepers in mitigating the risk of acute malnutrition; explore how to support breastfeeding women living in armed conflict situations; and explore how displaced populations affect host communities’ food systems.
Highlights:
Women play critical roles in agriculture in many low- and middle-income countries.
Women and children face high burdens of malnutrition during armed conflicts.
Malnutrition has lasting impacts on the developmental trajectory of children.
Similar themes link armed conflict to acute malnutrition across multiple contexts.
A clear research agenda can help to mitigate arm conflict-driven acute malnutrition.
Acknowledgements
The author would like to acknowledge the valuable feedback of Dr. Sarah Szanton and Lyndsay DeGroot on the design, composition, and revision of this review.
Financial support: This work was supported by the National Institutes of Health (1F31HD102091–01, 2020) and by Nurses Educational Funds, Inc. The funding sources were not involved in development of the study design; in the collection, analysis, or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Conflicts of interest: None
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Avis W Current trends in violent conflict. Brighton, UK: K4D Helpdesk Report; 565; 2019. [Google Scholar]
- 2.Loewenberg S Conflicts worsen global hunger crisis. Lancet, The. 2015;386(10005): 1719–21. [DOI] [PubMed] [Google Scholar]
- 3.Brück T, d’Errico M. Food security and violent conflict: Introduction to the special issue. World Development. 2019. May;117:167–71. [Google Scholar]
- 4.Food Security Information Network. Global Report on Food Crises; 2018. 2018. [Google Scholar]
- 5.Concern Worldwide. Conflict and Hunger: The Lived Experience of Conflict and Food Insecurity in South Sudan. 2018. August 15,. [Google Scholar]
- 6.The Sphere Project. Food Security and Nutrition Appendix 4: Measuring Acute Malnutrition. In: The Sphere Handbook 2018: Humanitarian Charter and Minimum Standards in Humanitarian Response. Geneva, Switzerland: Sphere Association; 2018. p. 225–6. [Google Scholar]
- 7.Carolyn Sachs, Anouk Patel-Campillo. Feminist Food Justice: Crafting a New Vision. Feminist Studies. 2014. July 1,;40(2):396–410. [Google Scholar]
- 8.Food and Agricultural Organization, (FAO). Peace and Food Security: Investing in Resilience to Sustain Rural Livelihoods Amid Conflic. Rome: 2016.
- 9.World Food Programme. Promoting Gender Equality and the Empowerment of Women in Addressing Food and Nutrition Challenges. 2009. February.
- 10.FAO, ABD. Gender Equality and Food Security—Women’s Empowerment as a Tool against Hunger. 2013. July 1,.
- 11.Martorell R, Zongrone A. Intergenerational influences on child growth and undernutrition. Paediatr Perinat Epidemiol. 2012;26:302–14. [DOI] [PubMed] [Google Scholar]
- 12.Valentine CJ, Wagner CL. Nutritional Management of the Breastfeeding Dyad. Pediatric Clinics of North America. 2013;60(1):261–74. [DOI] [PubMed] [Google Scholar]
- 13.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. 2013. [DOI] [PubMed] [Google Scholar]
- 14.Akombi BJ, Agho KE, Hall JJ, Wali N, Renzaho AMN, Merom D. Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review. International journal of environmental research and public health. 2017. August 1,;14(8):863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drammeh W, Hamid NA, Rohana AJ. Determinants of household food insecurity and its association with child malnutrition in Sub-Saharan Africa: A review of the literature. Current Research in Nutrition and Food Science Journal. 2019;7(3):610–23. [Google Scholar]
- 16.UNICEF, WHO, World Bank. Levels and trends in child malnutrition. Geneva, Switzerland: 2018. [Google Scholar]
- 17.Ahmed T, Hossain M, Sanin KI. Global Burden of Maternal and Child Undernutrition and Micronutrient Deficiencies. Annals of Nutrition and Metabolism. 2013. January;61(1):8–17. [DOI] [PubMed] [Google Scholar]
- 18.Wu G, Bazer FW, Cudd TA, Meininger CJ, Spencer TE. Maternal nutrition and fetal development. The Journal of nutrition. 2004. September;134(9):2169–72. [DOI] [PubMed] [Google Scholar]
- 19.Black MM, Pérez-Escamilla R, Rao SF. Integrating Nutrition and Child Development Interventions: Scientific Basis, Evidence of Impact, and Implementation Considerations. Advances in nutrition (Bethesda, Md.). 2015. November;6(6):852–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United Nations Children’s Fund, (UNICEF), World Health Organization, International Bank for Reconstruction and Development/The World Bank. Levels and trends in child malnutrition: key findings of the 2019 Edition of the Joint Child Malnutrition Estimates. Geneva: 2019. [Google Scholar]
- 21.Martin-Shields C, Stojetz W. Food security and conflict: Empirical challenges and future opportunities for research and policy making on food security and conflict. Rome: 2018. October 4,. [Google Scholar]
- 22.Cusick SE, Georgieff MK. The Role of Nutrition in Brain Development: The Golden Opportunity of the “First 1000 Days” Journal of Pediatrics, The. 2016;175:16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levitsky DA, Strupp BJ. Malnutrition and the Brain: Changing Concepts, Changing Concerns. The Journal of nutrition. 1995. August;125(8 Suppl):2212S–20S. [DOI] [PubMed] [Google Scholar]
- 24.Young H Nutrition in Africa’s drylands: A conceptual framework for addressing acute malnutrition. Boston, MA: Tufts University; 2020. [Google Scholar]
- 25.UNICEF. Strategy for improved nutrition of children and women in developing countries. 1990. [DOI] [PubMed]
- 26.Guha-Sapir D, van Panhuis WG, Degomme O, Teran V. Civil Conflicts in Four African Countries: A Five-Year Review of Trends in Nutrition and Mortality. Epidemiologic reviews. 2005;27(1):67–77. [DOI] [PubMed] [Google Scholar]
- 27.World Bank Country and Lending Groups [Internet]; 2019. [cited March 29, 2019]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 28.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization. 2007. September;85(9):660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO, UNICEF. WHO child growth standards and the identification of severe acute malnutrition in infants and children. 2009. [PubMed]
- 30.The Sphere Project. The Sphere Handbook: Humanitarian Charter and Minimum Standards in Humanitarian Response. 4th ed. Oxford University Press; 2018. [Google Scholar]
- 31.Dearholt S, Dang D. Johns Hopkins Nursing Evidence-Based Practice: Model and Guidelines. 2nd ed. Indianapolis, IN: Sigma Theta Tau International; 2012. [Google Scholar]
- 32.Noyes J, Lewin S. Chapter 5: Extracting qualitative evidence. In: Noyes J, Booth A, Hannes K, Harden A, Harris J, Lewin S, et al. , editors. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. Cochrane Collaboration Qualitative Methods Group; 2011. [Google Scholar]
- 33.FAO. Food Security Information for Action. 2008.
- 34.Tranchant J, Gelli A, Bliznashka L, Diallo AS, Sacko M, Assima A, et al. The impact of food assistance on food insecure populations during conflict: Evidence from a quasi-experiment in Mali. World Development. 2018. March. [Google Scholar]
- 35.Dunn G The impact of the Boko Haram insurgency in Northeast Nigeria on childhood wasting: a double-difference study. Conflict and health. 2018; 12(1):6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McGadney-Douglass B, Douglass R. Collective Familial Decision-Making In Times Of Trouble: Intergenerational Solidarity in Ghana. J Cross Cult Gerontol. 2008. June;23(2): 147–60. [DOI] [PubMed] [Google Scholar]
- 37.Goma Epidemiology Group. Public health impact of Rwandan refugee crisis: what happened in Goma, Zaire, in July, 1994? The Lancet. 1995. February 11,;345(8946):339–44. [PubMed] [Google Scholar]
- 38.Curtis P Urban Household Coping Strategies During War: Bosnia-Hercegovina. Disasters. 1995. March;19(1):68–73. [DOI] [PubMed] [Google Scholar]
- 39.Toole MJ, Galson S, Brady W. Are war and public health compatible? The Lancet. 1993;341(8854): 1193–6. [DOI] [PubMed] [Google Scholar]
- 40.Kinfu Y Child undernutrition in war-torn society: the Ethiopian experience. 1999. [DOI] [PubMed]
- 41.Kandala N, Madungu TP, Emina JBO, Nzita KPD, Cappuccio FP. Malnutrition among children under the age of five in the Democratic Republic of Congo (DRC): does geographic location matter? BMC public health. 2011. April 25,;11(1):261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guerrier Gilles, Zounoun Malaïka, Delarosa Olimpia, Defourny Isabelle, Lacharite Michelo, Brown Vincent, et al. Malnutrition and Mortality Patterns among Internally Displaced and Non-Displaced Population Living in a Camp, a Village or a Town in Eastern Chad. PLoS One. 2009. November 1,;4(11):e8077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grandesso F, Sanderson F, Kruijt J, Koene T, Brown V. Mortality and Malnutrition Among Populations Living in South Darfur, Sudan: Results of 3 Surveys, September 2004. JAMA. 2005. March 23,;293(12): 1490–4. [DOI] [PubMed] [Google Scholar]
- 44.Herp MV, Parqué V, Rackley E, Ford N. Mortality, Violence and Lack of Access to Healthcare in the Democratic Republic of Congo. Disasters. 2003. June;27(2):141–53. [DOI] [PubMed] [Google Scholar]
- 45.Rapsomanikis G The economic lives of smallholder farmers: An analysis based on household data from nine countries. Rome, Italy: FAO; 2015. [Google Scholar]
- 46.Samberg LH, Gerber JS, Ramankutty N, Herrero M, West PC. Subnational distribution of average farm size and smallholder contributions to global food production. Environmental Research Letters. 2016. December 1,;11(12):124010. [Google Scholar]
- 47.Commission on the Status of Women. Challenges and opportunities in achieving gender equality and the empowerment of rural women and girls. United Nations; 2017. December 20,. [Google Scholar]
- 48.Petri J, William A, Miller M, Binder HJ, Levine MM, Dillingham R, Guerrant RL. Enteric infections, diarrhea, and their impact on function and development. The Journal of clinical investigation. 2008. April; 118(4): 1277–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bhutta ZA, Yousafzai AK, Zipursky A. Pediatrics, War, and Children. Current Problems in Pediatric and Adolescent Health Care. 2010;40(2):20–35. [DOI] [PubMed] [Google Scholar]
- 50.Guerrant RL, Schorling JB, McAuliffe JF, de Souza MA. Diarrhea as a Cause and an Effect of Malnutrition: Diarrhea Prevents Catch-up Growth and Malnutrition Increases Diarrhea Frequency and Duration. The American journal of tropical medicine and hygiene. 1992. July;47(1 Pt 2):28–35. [DOI] [PubMed] [Google Scholar]
- 51.Thiagarajah JR, Donowitz M, Verkman AS. Secretory diarrhoea: mechanisms and emerging therapies. Nature reviews. Gastroenterology & hepatology. 2015. August;12(8):446–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ascherio A, Chase R, Coté T, Dehaes G, Hoskins E, Laaouej J, et al. Effect of the Gulf War on Infant and Child Mortality in Iraq. The New England Journal of Medicine. 1992. September 24,;327(13):931–6. [DOI] [PubMed] [Google Scholar]
- 53.Field JO, Russell RM. Nutrition Mission to Iraq for UNICEF. Nutrition reviews. 1992. February;50(2):41–6. [DOI] [PubMed] [Google Scholar]
- 54.Aaby P, Gomes J, Fernandes M, Djana Q, Lisse I, Jensen H. Nutritional status and mortality of refugee and resident children in a non-camp setting during conflict: follow up study in Guinea-Bissau. BMJ. 1999. October;319(7214):878–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ghazi HF, Mustafa J, Aljunid S, Isa ZM, Abdalqader MA. Malnutrition among 3 to 5 Years Old Children in Baghdad City, Iraq: A Cross-sectional Study. Journal of Health, Population, and Nutrition. 2013. January 1,;31(3):350–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Reid BC, Psoter WJ, Gebrian B, Wang MQ. The Effect of an International Embargo on Malnutrition and Childhood Mortality in Rural Haiti. International Journal of Health Services. 2007. July;37(3):501–13. [DOI] [PubMed] [Google Scholar]
- 57.Olwedo MA, Mworozi E, Bachou H, Orach CG. Factors associated with malnutrition among children in internally displaced person’s camps, northern Uganda. African health sciences. 2008. December;8(4):244–52. [PMC free article] [PubMed] [Google Scholar]
- 58.Andersson N, Paredes-Solís S, Legorreta-Soberanis J, Cockcroft A, Sherr L. Breast-feeding in a complex emergency: four linked cross-sectional studies during the Bosnian conflict. Public Health Nutrition. 2010. December 1,;13(12):2097–104. [DOI] [PubMed] [Google Scholar]
- 59.Brown ME, Backer D, Billing T, White P, Grace K, Doocy S, et al. Empirical studies of factors associated with child malnutrition: highlighting the evidence about climate and conflict shocks. Food Security. 2020:1–12. [Google Scholar]
- 60.Howell E, Waidmann T, Birdsall N, Holla N, Jiang K. The impact of civil conflict on infant and child malnutrition, Nigeria, 2013. Maternal & child nutrition. 2020;16(3):e12968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.How M, Chan YJ. Artificial Intelligence-Enabled Predictive Insights for Ameliorating Global Malnutrition: A Human-Centric AI-Thinking Approach. AI. 2020;1(1):68–91. [Google Scholar]
- 62.Tang AM, Chung M, Dong K, Terrin N, Edmonds A, Assefa N, et al. Determining a global mid-upper arm circumference cutoff to assess malnutrition in pregnant women. Food and Nutrition Technical Assistance. 2016. [Google Scholar]
- 63.Ververs M, Antierens A, Sackl A, Staderini N, Captier V. Which Anthropometric Indicators Identify a Pregnant Woman as Acutely Malnourished and Predict Adverse Birth Outcomes in the Humanitarian Context? PLoS Currents. 2013. June 7,;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gebre B, Biadgilign S, Taddese Z, Legesse T, Letebo M. Determinants of malnutrition among pregnant and lactating women under humanitarian setting in Ethiopia. BMC nutrition. 2018;4(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.FAO, IFAD, UNICEF, WFP, WHO. The State of Food Security and Nutrition in the World 2019. Safeguarding against economic slowdowns and downturns Rome: FAO; 2019. [Google Scholar]
- 66.Collier P, Hoeffler A, Söderbom M. Post-conflict risks. J Peace Res. 2008;45(4):461–78. [Google Scholar]
- 67.Prudhon C, Benelli P, Maclaine A, Harrigan P, Frize J. Informing infant and young child feeding programming in humanitarian emergencies: An evidence map of reviews including low and middle income countries. Maternal & Child Nutrition. 2018. January;14(1):e12457,n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Keikha M, Bahreynian M, Saleki M, Kelishadi R. Macro- and Micronutrients of Human Milk Composition: Are They Related to Maternal Diet? A Comprehensive Systematic Review. Breastfeeding Medicine. 2017;12(9):517–27. [DOI] [PubMed] [Google Scholar]
- 69.Lau C Effects of Stress on Lactation. The Pediatric Clinics of North America. 2001;48(1):221–34. [DOI] [PubMed] [Google Scholar]
- 70.Summers A, Bilukha OO. Suboptimal infant and young child feeding practices among internally displaced persons during conflict in eastern Ukraine. Public health nutrition. 2018. April;21(5):917–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Diwakar V, Malcolm M, Naufal G. Violent conflict and breastfeeding: the case of Iraq. Conflict and Health. 2019;13(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jakobsen M, Sodemann M, Nylén G, Balé C, Nielsen J, Lisse I, et al. Breastfeeding status as a predictor of mortality among refugee children in an emergency situation in Guinea Bissau. Tropical Medicine & International Health. 2003. November;8(11):992–6. [DOI] [PubMed] [Google Scholar]
- 73.Meek JY, Feldman-Winter L, Noble L. Optimal Duration of Breastfeeding. Pediatrics. 2020;146(5). [DOI] [PubMed] [Google Scholar]


