Abstract
Objectives & Hypothesis:
Children with home mechanical ventilation (HMV) require skilled care by trained caregivers, and their families feel the impacts of ubiquitous home nursing shortages. It is unknown which factors determine allocation; no standards for private duty nursing intensity exist. We sought to characterize provider experiences with and opinions on home nursing for children with HMV, hypothesizing providers would describe frequent home nursing gaps across clinical scenarios.
Methods:
Purposeful and snowball sampling identified key informant clinical providers. Survey topics included hours of home nursing received across clinical and family scenarios. Close-ended responses were analyzed using descriptive statistics and open-ended questions coded with iterative modification for major theme agreement.
Results:
A total of 59 respondents represented care of patients from 44 states; 49.2% physicians, 37.3% nurses, 10.2% respiratory therapists, and 3.4% case managers. Nearly all (97%) believed that families should receive more hours during initial home transition, yet less than half (47%) do. The majority (80.7%) thought the presence of other children in the home should influence nursing hours, yet only three (5.3%) reported other children have influence. Across hypothetical medical technology scenarios, providers consistently described children receiving fewer nursing hours than the providers’ ideal practice. A third (31.7%) described discharging patients without any home nursing arranged.
Conclusions:
This HMV provider sample highlights pervasive deficiency in home nursing provision with heterogenous interpretation of what constitutes ideal home care. Family and social contextual factors are infrequently considered in nursing allocations. Provider, community health, and family stakeholders must collaborate to generate national community practice standards for children with HMV.
Keywords: children with medical complexity, epidemiology, home nursing, mechanical ventilation, social dimensions of pulmonary medicine
1 |. INTRODUCTION
Children with medical complexity (CMC) who require skilled nursing care have the right to integrate into their homes and communities because of the Americans with Disabilities Act and the Olmsted v. L.C. Supreme Court decision.1 However, private duty and block home nursing services that allow these children to safely live in the community are limited,2–5 increasing the responsibilities of family caregivers, often to the detriment of their employment and health.6–11 Further, home nursing shortages are associated with increased length of hospital stay for children with new technologies.12,13
Medical and nursing professional organization policies address aspects of home nursing for CMC. An American Academy of Pediatrics Section on Home Care and Committee on Child Health Financing policy statement states that, “Payments for home health care services should be sufficient to maintain an adequate provider work force with the pediatric-specific expertise and skills to care for children with medical complexity or developmental disability.”2 The American Thoracic Society guidelines describe that children with home mechanical ventilator dependency (HMV) require an awake and attentive trained caregiver in the home at all times to safely supervise the ventilator and respond to alarms and suctioning needs.14 However, there are no guidelines on specific medical eligibility criteria for home nursing care as supplement to trained family caregivers in CMC populations. Furthermore, there are not standards for determining how many hours of nursing care patients should receive, and how social and family factors should inform service allocations. Nor is it known how current home care service allocation varies for patients who seem similar by either medical or family contextual characteristics.
To fill these gaps in knowledge, we sought to characterize variation in the provision of private duty nursing services and assess barriers to care by surveying expert providers of care for children with HMV. We hypothesized that providers would report differences between ideal and actual number of home nursing hours patients receive, which would reflect experiences with deficiencies in home nursing provision. We also predicted that due to lack of national standards for the appropriate amount of home healthcare, great variability between respondents would emerge across clinical scenarios.
2 |. METHODS
2.1 |. Participants: providers who care for children with HMV
Using a purposeful sampling method with capture-recapture and snowball sampling, this HMV Key informant list was initially generated for the first wave of this survey series using the Complex Care Listserv and the Children’s Hospital Association membership list.15 Respondents were practitioners from diverse disciplines: physicians, nurses, respiratory therapists, and case managers. First wave respondents were invited to the second wave. An updated invitation was sent to the Complex Care listserv to recruit new key informants; respondents were asked to suggest other potential participants. This study was presented informally at meetings of the Pediatric Acute Lung Injury and Sepsis Investigators—Long Term Ventilation Subgroup, and additional informants joined as a result.
2.2 |. Survey development
This survey was conducted via a web interface with a closed-survey design, (unique email links for each participant). Responses from repeat participants were linked. To minimize response burden, branching logic and adaptive questioning were used. Cognitive testing was completed with five healthcare professionals from diverse training and geographic regions to improve the survey content and interface.16 The survey was developed using Research Electronic Data Capture and included multiple choice and free response questions.17 An abridged version for prior participants excluded Wave 1 demographic questions. The full Wave 2 survey focused on discharge practices and home care services for children requiring HMV; a separate report focuses on discharge practices and includes items related to other essential components of discharge: medical stability before discharge and parent training.18 Institutional Review Board approval was obtained from the University of Chicago.
2.2.1 |. HMV Wave 2 survey
Respondent demographics
Individuals were asked about their training and professional background, years of experience with children with HMV assistance, their primary practice state and from which additional states their patients reside to capture patient populations that crossed state lines.
Home nursing care
Home nursing items aimed to query respondent opinion of best practice and practice realities of home nursing for children with HMV. Participants were asked whether families should receive more hours of home nursing during the initial period of transition home and whether families do receive more hours during transition.
2.2.2 |. Variation in home nursing due to clinical scenarios
Seven clinical scenarios were described; respondents indicated the IDEAL number of weekly nursing hours each patient ought to receive, the number of weekly hours they would be APPROVED to receive, and the number of weekly hours they actually RECEIVE (e.g., “In your primary practice region, please indicate below the number of hours per week of home nursing care for a patient with a gastrostomy plus noninvasive mask ventilation”). We presented a range of clinical scenarios which would likely be familiar to HMV practitioners (e.g., “a patient with a gastrostomy and no respiratory needs” and “a gastrostomy plus tracheostomy, oxygen, and ventilator 24 h/day) to make comparisons of nursing need, approval, and receipt across levels of medical complexity which included multiple technologies. We elected to include two clinical scenarios without respiratory needs to have comparison groups with our primary population of interest, children with tracheostomies and ventilators. To account for differing clinical practice experiences, respondents were able to select “I don’t know” as a response.
2.2.3 |. Variation in home nursing due to family context
Respondents were asked which family factors (e.g., number of caregivers, parental employment, number of children) DO influence the quantity of home nursing a family receives and which of those same factors they thought OUGHT to influence the quantity of home nursing.
2.2.4 |. Goal home nursing practices
Respondents were asked about nurse qualifications (e.g., “Do the number of staffed hours differ in your practice area based on whether an LPN vs. RN is required?” And “Is there anything else you think we should understand about nurse qualifications for home care?”). Additional items inquired whether their practice required home nursing care to be in place before discharge. If yes, respondents were asked, “What is the minimum number of approved hours that you require for discharge home?” When respondents did not stipulate units, we assumed integers ≤24 were hours/day (e.g., 16 was interpreted as 16 h/day); responses more than 24 were assumed to mean hours per week. Respondents were asked how frequently they discharge patients without home nursing in place, how frequently they require home nursing hours approved by insurance before discharge, and to what extent the hours actually need to be staffed to permit discharge. An open-ended question asked respondents to identify barriers to staffing nursing hours.
Delay of discharge
Respondents selected all factors that delayed discharge for their patients (e.g., home nursing, lack of second caregiver) and identified the most culpable.
2.3 |. Survey data collection
Key informants received closed survey invitations and up to two reminders. Electronic informed consent was obtained. Participant name and emails were used to contact participants, but not reported in data analyses or reports. Responses were completed within 3 months.
2.4 |. Analyses
Statistical analyses were completed using Stata/SE 14 (Stata Corp). Close-ended responses were analyzed using descriptive statistics. Two investigators (SS and AD) used an open-coding technique for the three open-ended questions, and on “other” responses which solicited detailed prose: coding items individually19 and resolving differences in theme categorization by discussing to agreement. Wilcoxon signed-rank tests were used to detect significant differences between clinical scenarios. For these analyses, due to the number of comparisons being made, a p < .0024 was considered statistically significant. Results were confirmed using repeated measures analysis of variance (ANOVA) and sign tests. The manuscript follows the Checklist for Reporting Results of Internet E-Surveys guidelines.20
3 |. RESULTS
3.1 |. Sample
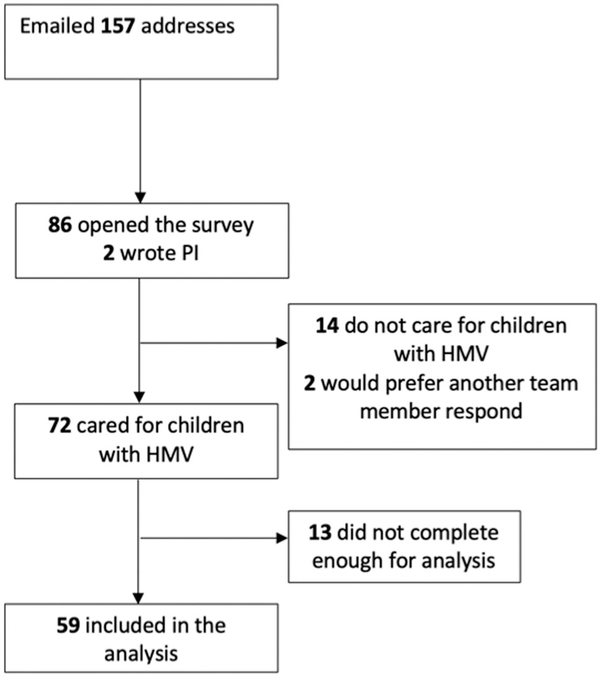
The overall response rate was 56% (Figure 1). We emailed 157 addresses and 88 opened the survey link or emailed the primary investigator to request another member of their team respond instead; the investigators invited the new key informant. Two respondents delegated another team member and 14 respondents were not involved in hospital discharge of children with HMV assistance and were routed out of the survey. Of the remaining 72 responses, 13 were determined to not be complete enough to include in the analysis. A total of 59 total surveys were analyzed. The calculation of response rate was conducted in the same fashion as the Wave 1 survey.15
FIGURE 1.
Flowchart illustrating study recruitment
3.2 |. Respondent demographics
The majority of respondents were physicians (29, 49.2%), with 22 (37.3%) nurses, 6 (10.2%) respiratory therapists, and 2 (3.4%) case managers. Respondents were from 23 states and reported seeing patients from an additional 21 states, therefore, reporting on care of patients from a total of 44 states. Over half of respondents were from the Midwest (30.5%) or the Northeast (28.8%). We did not have respondents caring for patients from Hawaii, Iowa, Louisiana, North Dakota, South Dakota, or South Carolina. The majority of respondents reported 1–40 years of experience (53.6%), 28.6% had 6–10 years of experience and 17.9% had 5 or fewer years. Over half (65.4%) of participants worked within a team dedicated to patients with long term ventilation (Table 1).
TABLE 1.
Respondent demographicsa (N = 59)
| % (N) | |
|---|---|
| Profession | |
| Physician | 49.2 (29) |
| Nurse | 37.3 (22) |
| Respiratory therapist | 10.2 (6) |
| Case manager | 3.4 (2) |
| Region of practice | |
| Midwest | 30.5 (18) |
| Northeast | 28.8 (17) |
| Southeast | 15.3 (9) |
| Southwest | 8.5 (5) |
| West | 16.9 (10) |
| Years of experience (N = 56) | |
| 1–5 | 17.9 (10) |
| 6–10 | 28.6 (16) |
| 11–15 | 7.1 (4) |
| 16–20 | 19.6 (11) |
| 21–30 | 17.9 (10) |
| 31–40 | 8.9 (5) |
| Institution has dedicated long term ventilation team | 65.4 (36) |
Due to rounding, percentages do not add up to 100%.
3.3 |. Home nursing by variable clinical scenarios
Across seven hypothetical clinical scenarios, respondents indicated that patients were approved for fewer home nursing hours than their ideal practice, and fewer hours were approved than received. Wilcoxon signed-rank tests confirmed significant differences between ideal/approved/received nursing hours within all scenarios, and significance was also found using repeated-measures ANOVA with Bonferroni correction and sign tests.
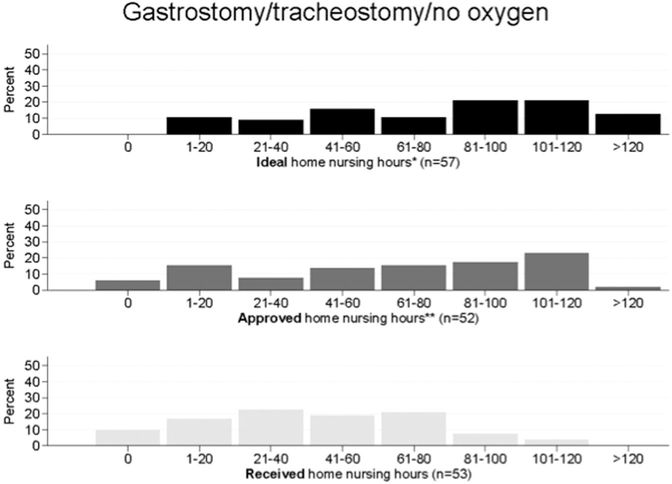
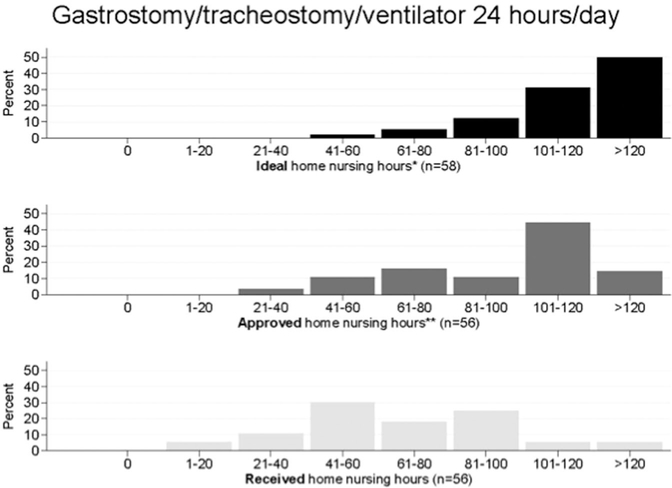
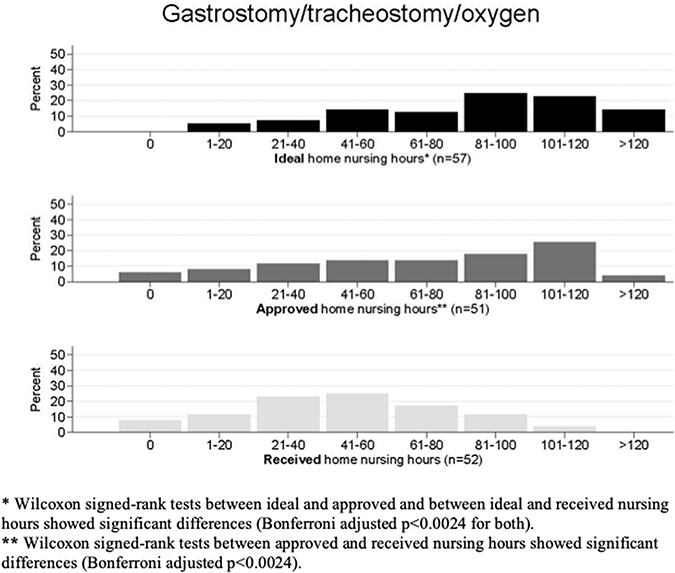
Greater variability in ideal/approved/received nursing was observed for clinical scenarios with lower complexity, for example, for a child with gastrostomy and tracheostomy without oxygen/ventilator requirements (Figure 2). Participants described significantly fewer hours approved than ideal across scenarios. They also reported fewer hours received than approved across scenarios. There was no clear consensus on ideal practice across scenarios. Greater agreement was seen for scenarios of children with higher complexity (Figure 3). For a child with 24-h ventilator needs, the most frequently described ideal practice was more than 120 h of home nursing care. The most frequently reported approved nursing hours were 101–120 h weekly and the most frequently reported received hours of home nursing were 41–60 h weekly with a range: 1–20 h to more than 120 h weekly. Distributions of responses across other clinical scenarios are available (Appendices A–E).
FIGURE 2.
Comparison of ideal, approved, received nursing hours for patient with gastrostomy and tracheostomy. Wilcoxon signed-rank tests between ideal and approved and between ideal and received nursing hours showed significant differences (Bonferroni adjusted p < .0024 for both). Wilcoxon signed-rank tests between approved and received nursing hours showed significant differences (Bonferroni adjusted p < .0024)
FIGURE 3.
Comparison of nursing hours for patient with gastrostomy, tracheostomy, and ventilator 24 h/day. Wilcoxon signed-rank tests between ideal and approved and between ideal and received nursing hours showed significant differences (Bonferroni adjusted p < .0024 for both). Wilcoxon signed-rank tests between approved and received nursing hours showed significant differences (Bonferroni adjusted p < .0024)
3.4 |. Family contextual factors influencing home nursing hours
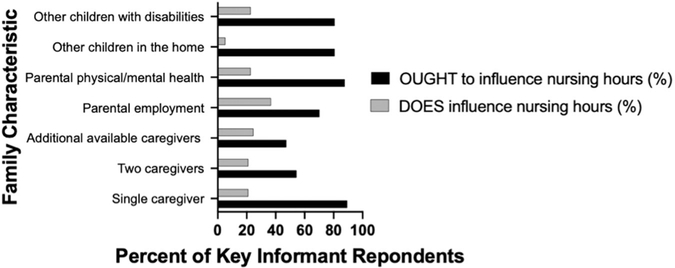
Providers asserted that family characteristics (single caregiver, two caregivers, additional caregivers, parental employment, parental physical/mental health, other children in the home, and other children with disabilities) ought to influence the number of nursing hours allocated, but in reality did not. The majority (80.7%) of respondents thought other children in the home should influence nursing hours, yet only three respondents (5.3%) reported that other children influenced received nursing hours (Figure 4).
FIGURE 4.
Comparison of participants’ responses to whether various family characteristics OUGHT to influence home nursing hours versus whether they DO influence nursing hours
3.5 |. Requirements for home nursing care before discharge
All respondents indicated that it was a practice goal for home nursing to be in place before discharge and 60% of respondents said there was always a requirement for home nursing hours to be approved by insurance. Nearly a third (31.7%) at least sometimes discharged patients without home nursing in place. Of those with an approval requirement, there was great variability in the minimum number of approved hours. A total of 15 respondents described a daily expectation, ranging 8–24 h/day with 16 h/day as the most common response. Eight respondents described a weekly expectation with a range of 30–84 h.
When asked, “To what extent do these actually need to be staffed for you to permit discharge home?” A total of 13 (24%) responded they always do and 24 (44%) responded they very often do. A total of 9 (17%) responded that they never need to be staffed to permit discharge. When asked the open-ended question, “What percentage of home nursing hours do you require are staffed before a child can be discharged home?” responses varied, including ranges provided or qualifying terms such as “generally about” or “prefer to have…” Approximately 1/3 responded less than 50% staffed and 2/3 responded with more than 50% staffed. Nine respondents (19%) described that 100% of nursing hours must be staffed before discharge.
3.6 |. Goals of initial nursing care
Nearly all of respondents, 97% (N = 57), described that families should receive more hours of home nursing during the initial transition period. Less than half, (47%, N = 28) responded that families do receive more hours during initial home transition.
3.7 |. Barriers to home nursing
A total of 54 open-ended responses to the inquiry about barriers to staffing nursing hours were thematically coded (Table 2). The most common theme was insufficient availability of skilled home health nurses in the overall workforce. Respondents described this shortage as “severe” and impacting both RN and LPN availability. Respondents also expressed concern about pediatric and complex care experiences, describing that sometimes nurses are “in a home with a vented patient on their own and have never taken care of a vent.”
TABLE 2.
Themes within provider responses to “What barriers do you experience staffing nursing hours?” (sample of quotes below, total N = 54)
| Theme 1: Insufficient availability of home health nurses with desired skills/experience. |
| 1 A: There is a general shortage in the nursing workforce and it unevenly impacts certain geographical areas |
| “Lack of RN and LPN availability. Difficulty retaining consistent staff. High staffing turnover.” |
| “The demand for home nursing far exceeds the supply of home care nurses.” |
| “Lack of nurses in the field in the biggest barrier.” |
| “Severe shortage of home nursing available.” |
| “Availability of nurses in the areas where families live” |
| “Not enough nurses in our area to staff cases.” |
| “[I practice] in a very rural state where there are pockets of areas with no home health nursing available. Some families have had to move.” |
| 1B: Home nurses lack core qualifications and skills e.g., trach/vent and medical complexity experience |
| “Nurses with poor skills/competencies which results in a lot of turnover.” |
| “first job for many nurses/lack clinical competencies” |
| “lack of trach/vent trained nurses” |
| “Very little training required by the homecare agencies to nurses. Some in a home with a vented patient on their own and have never taken care of a vent.” |
| “home health companies do not have qualified nurses to take care/cover of these medically complex children.” |
| 1 C: Inadequate supply of home nurses with pediatric experience |
| “We do not have adequate supply of home nurses with experience taking care of children with complex health care needs.” |
| “Not enough [pediatrics]-experienced nurses available.” |
| Theme 2: Nurses are not interested in home care sector due to core job characteristics. |
| 2 A: Low pay for nurses secondary to low wages |
| “Availability of nursing likely due to poor reimbursement rates from Medicaid” |
| “low reimbursement rates (nurses gravitate to higher paying hospital-based jobs)” |
| “rate that nurses receive for home care has not changed in 20 years until a month ago.” |
| 2B: Difficulty with staffing shifts based on time of day |
| “Overnight shifts and weekends are the toughest to staff.” |
| “Availability of day vs. night nursing” |
| Theme 3: Insurance approval is a barrier to providing home nursing to families. |
| “Insurance does not have the shift nursing benefit coverage.” |
| “Private insurance does not approve 24/7 [home nursing]; can often negotiate for 14 days worth.” |
| “not enough hours approved” |
| Theme 4: Barriers to home nursing due to location and condition of family home |
| 4 A: General location of home is a barrier to home nursing |
| “Location of patient’s home” |
| “Neighborhood where family lives.” |
| “zip code of parental home” |
| 4B: Patient being in rural and/or remote area is a barrier to home nursing |
| “rural areas and decreased nursing availability” |
| “Patient living in larger communities have better access to nursing than many of our patients living in remote, rural areas.” |
| “Not enough pedi experienced nurses available. Also live in a very rural state where there are pockets of areas with no home health nursing available. Some families have had to move.” |
| 4 C: Poor home conditions/safety issues deter home nurses |
| “poor home conditions” |
| “unfavorable housing settings, real/perceived risk to nursing staff related to housing, neighborhood, poverty, family conflict, substance use/abuse in family, moral distress for nursing when family’s care standards differ from nursing staff’s” |
| “family, home environment” |
| “family lives in unsafe area so nurses do not want to go to that location to work” |
| Theme 5: Family relationship with home nurse or agency is a barrier to home health care |
| 5 A: Dissatisfaction with nurse or agency |
| “Experienced parents who don’t like specific nurses/companies for home care” |
| “Family not happy with nurse interviewed. |
| Language/cultural differences” |
| 5B: Family relationship with nurses is a barrier to staffing |
| “The demand for home nursing far exceeds the supply of home care nurses. Barriers include but not limited to: compensation offered to RN’s, area that pt lives, family dynamics, medical complexity/amount of tasks needing to be performed on shift.” |
| “1. Shortage in home nursing nurses; 2. Family interaction/personality barriers; 3. Case complexity; 4. Funding for private duty nursing” |
| “parents do NOT want nurse in home-- feel like it’s a stranger in home” |
| Theme 6: Family factors which create barriers to staffing hours. |
| 6B: Lack of family knowledge about home nursing is a barrier to staffing nursing hours |
| “Family unaware of how to obtain nursing hours |
| Family unaware of independent nurses” |
| 6 C: Other family social factors impacting home nursing receipt |
| “lack of trach/vent trained nurses, unfavorable housing settings... family conflict, substance use/abuse in family, moral distress for nursing when family’s care standards differ from nursing staff’s” |
| “social complexity” |
| “social home considerations” |
| 6D: Language/cultural barriers |
| “language barriers” |
| “Language/cultural differences” |
Providers primarily believed that low wages were to blame for home healthcare workforce shortages. However, family home location, home condition, and neighborhood safety were frequently cited reasons for difficulty with staffing. “Family lives in unsafe area so nurses do not want to go to that location to work.”
3.8 |. Qualifications of home nurses
A total of 27 participants (47%) indicated that the number of hours staffed differs based on whether an LPN versus RN is required. A total of 35 open-ended responses about nurse qualifications for home care were analyzed. The most common themes were concerns about shortcomings in nursing qualifications for pediatric tracheostomy/ventilator care. Respondents also perceived a lack of training standardization across agencies.
3.9 |. Home nursing shortages impact discharge delays
Participants described factors impacting delays of discharge. Nearly all providers described patients experiencing delays due to family training (92%), 86% due to home nursing, and 86% due to lack of a second caregiver. Less commonly, 66% described medical delays, 54% equipment delays, 54% state funding delays, and 44% delays due to foster care status. When asked which factor most contributed to discharge delays, 60% of participants selected home nursing.
4 |. DISCUSSION
This national provider sample presents a description of pervasive discrepancies between individuals’ ideal best practice and experiences with actual practice realities for the provision of home nursing care for children with ventilators living in the community, suggesting that providers may be forced to act outside of their individual interpretation of best practice due to resource scarcity. The discrepancies were not only at the level of home healthcare availability, but also at the level of insurance approvals for home care, as demonstrated by the gap between approved and ideal home nursing. Providers consistently thought that family contextual factors such as the number of caregivers or siblings ought to influence homecare, yet infrequently had influence. When asked about barriers for home care, providers consistently described the shortage of skilled home care nurses, and attributed this shortage mostly to wages, but also to family home and core job characteristics.
Within clinical scenarios, providers demonstrated wide variability in perception of ideal care. Although Early and Periodic Screening, Diagnostic and Treatment services ought to cover all services determined to be medically necessary, determination of medical necessity is made “on a case-by-case basis, taking into account a particular child’s needs”.21 Because Medicaid services are determined at the state level, variability in interpretation and implementation might be expected nationally in the absence of a nationally accepted standard for the home nursing support children with ventilators ought to receive. If goal standards of nursing provision were established and complemented by professional and family expertise, there would likely be improved consistency in care. Creating standards is complicated; the amount of nursing required to enhance patient safety and provide relief to family caregivers is unknown, and in fact may vary widely between cases or even within cases over time. There may be initial intensity of nursing needs which may dissipate as parents gain mastery and comfort. Providers in our survey nearly universally supported increased home nursing support at the time of first home transition, yet only half described that patients receive additional support during this vulnerable period. Future work should explore family transition from being novice to expert caregivers at home, including the skills, experiences, and duration of time this typically takes. Further, nursing needs may need to be increased to prevent caregiver burnout, particularly if technology dependency takes a toll on parental employment and sibling needs.
Medical factors need not be the only contributor to determining overall nursing needs. In our cohort of providers, the majority thought that single caregiving, parental mental or physical health issues, and other children in the home should influence nursing hours, yet only one-in-five described that these family contextual factors had influence on a child’s home nursing allocation. The clearest example may be a child with 24/7 ventilatory needs; he would clearly need a trained caregiver at all hours, yet many of our respondents described patients receiving fewer than 16 h daily of nursing care, meaning that the baseline expectation would be for parent caregivers to consistently work overtime as nurses in the home. As we practice in an era of increased sensitivity to the social determinants of health, the AAP has recommended that pediatricians “screen for risk factors within social determinants of health during patient encounters”.22 Therefore, we believe social determinants, such as parental employment, housing security, sibling needs, and number of trained and available caregivers, should also factor into medical necessity determinations for community nursing.
Providers described an overall severe deficiency in the workforce, particularly nurses with expertise in pediatrics and ventilator management. The American Academy of Pediatrics Section on Home Care, Committee on Child Health Financing’s policy statement describes that, “Payments for home health care services should be sufficient to maintain an adequate provider work force with the pediatric-specific expertise and skills to care for children with medical complexity or developmental disability.”2 Despite strong support from pediatric leadership, we suspect that the largest limiting factor toward successful implementation of universal standards of care is severe resource scarcity which has been described as impacting care in several recent works.4,12,13 It would be predictably impossible to provide 24-h caregiving in a setting without ample home nursing support, and our study suggests that this is the case in the vast majority of regions. When home health resources are lacking, unfilled shifts fall squarely on the shoulders of family caregivers, and impact parent sleep, physical and mental health, and employment status. Unmet nursing needs become the responsibility of family caregivers10,23,24 who often experience resulting financial and emotional strain.3,11,25–28
Our survey respondents also described gaps in home nursing training and lack of standardization across agencies. Prior research has identified critical gaps in home nursing skills for the care of children with tracheostomy and ventilators,29,30 and has demonstrated that focused training for home health nurses can improve knowledge and skills for the management of children on ventilators in the home.31 Improving the preparedness of home health nurses for emergent events through standardized ongoing training is essential for the safe care of a child on a ventilator in the home.
It is important to note that our survey utilized key informant providers, many of whom work primarily in inpatient settings, to understand the provision of community home nursing services for children on ventilators. Inpatient providers may be acutely aware of the needs and impacts of home care, but they are also balancing competing priorities. The environment of care may influence, explicitly or implicitly, decisions about home nursing and readiness for discharge. For example, pressure to open critical care beds for other ill patients may influence discharge readiness. Or, the opposite, pressure to maximize productivity of an intensive care unit may disincentivize expeditious discharge of complex patients. In some regions, transitional care centers are utilized as intermediate models of care to prepare for complex discharges and can help to appropriately focus on transition readiness while liberating finite acute care beds.32 However, despite the complexity of discharge and parental desire for tailored discharge teaching,33 few transition-focused centers exist and efficient discharge is often limited by home healthcare shortages.12,34
Our study should be interpreted in light of several important limitations. While the respondents represent a diverse US provider sample, it is a convenience sample and may not represent the broad range of opinion of providers for children with HMV. Further, we acknowledge that all providers of care for children with HMV are not poised to report on home nursing receipt, since inpatient and outpatient healthcare systems are not always fluidly coordinated, and some providers of care for children with HMV are not also expert on other technologies queried in this survey. Although we specifically asked prior survey respondents to extend invitations to case managers and discharge planning team members, the response to this invitation was limited. Responses, particularly those asking for average experience across one’s practice, were also subject to recall bias, and we acknowledge that more challenging clinical cases with gaps in care may likely be more top of mind than well-staffed, resourced patients who needed fewer provider interventions to advocate for services. Also, we relied on provider report of services rather than verification from external records. Importantly, both home health nurses and family perspectives were not incorporated into this study, but ought to be incorporated into developing standards for nursing provision for this population. Parental preferences may diverge from the medical care teams, for example, limiting nursing hours in the home or desiring expediting discharge without nursing in place. It is possible that aiming to reduce contact with healthcare providers may be increased in the current COVID-19 pandemic, but has unique consequences for children with HMV. We need new research into innovative models including trained nonprofessional caregivers and remote monitoring to best optimize patient safety and parental preferences. Overall, we recognize that patient and family contexts have infinite potential variation on what home supports might be needed to address the medical complexity of the child within his/her family context, including family’s preference for home nursing; we tried to include common clinical and family scenarios. In designing this study, we decided to limit our informants to the United States to have relatively similar comparison between clinical contexts. Certainly, standards across the world are needed, and we acknowledge that there are no internationally accepted guidelines for nursing care in the community of children with ventilator assistance. Work on safe staffing for children in the home remains at early stages, yet evidence of unmet home nursing needs and detrimental impacts on parents and families exist in international studies.35,36
Future studies are needed to understand the most effective solutions to improving pediatric home healthcare for children with HMV in diverse contexts. Contributors to the home healthcare workforce include not only paid nursing staff, but unpaid family caregivers. Therefore, social factors not only determine health, but measure the capacity of the family caregiver workforce, and should be incorporated into calculations of home nursing approvals. Further, nonprofessional trained caregivers may be a potential source of untapped capacity to relieve caregivers from caring duties and provide meaningful support to persons on HMV when skilled nursing is not available,37,38 although there is generally a dearth of studies in pediatric care. Future investigations ought to solicit detailed input from family, provider, and the spectrum of home health workers to fully incorporate complex factors into creating home healthcare standards.
Finally, although not among the topics of this 2019 survey, we acknowledge that home healthcare models must also adapt to changes in the wake of the COVID-19 pandemic. Potential positive impacts on home healthcare are that infection consciousness which is now pervasive throughout society may have increased momentum to support home healthcare models which limit patient exposures and expand home healthcare scope of practice. The use of expanded telemedicine and remote monitoring capacity, for example, through virtual stethoscopes and transmitting data from monitoring devices, has potential to augment in-home nursing teams and provide greater linkages between hospital and community-based healthcare teams. Perhaps the shift of some healthcare delivery to virtual space creates opportunity to expand the home health workforce for children with complexity living at home. However, negative impacts may be further limitations on private duty nursing due to family preferences for limiting COVID-19 exposure risks because home health nurses often work in multiple family homes and in other healthcare settings. As able, private duty nursing staffing assignments ought to minimize exposures through primary nurse assignments versus rotating nurses through high numbers of family homes.
5 |. CONCLUSION
Health providers for pediatric patients with HMV report they receive fewer hours of home nursing than perceived best practice, which vary greatly between providers. Further, family and social contextual factors are not considered in nursing allocations. National standards for community supports for children on HMV, including not only nursing support but standardized training and alternatives in the setting of nursing shortages, should be determined to enable consistency of quality care which incorporate both medical and social risk.
ACKNOWLEDGEMENTS
The authors wish to acknowledge busy providers for their participation in this survey despite extraordinary demands on their time. We thank Kristen Wroblewski for her consultation on the analysis and graphical representation of clinical scenarios. Dr. Sobotka receives support from The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD, K23 HD097276) and the T73 Leadership Education in Neurodevelopmental and Related Disorders Training Program (LEND, T73MC11047).
Funding information
Eunice Kennedy Shriver National Institute of Child Health and Human Development, Grant/Award Number: K23 HD097276; Maternal and Child Health Bureau, Grant/Award Number: T73MC11047
Abbreviations:
- ATS
American Thoracic Society
- HMV
home mechanical ventilation
APPENDIX
See Appendix Figures A1, B1, C1, D1, E1
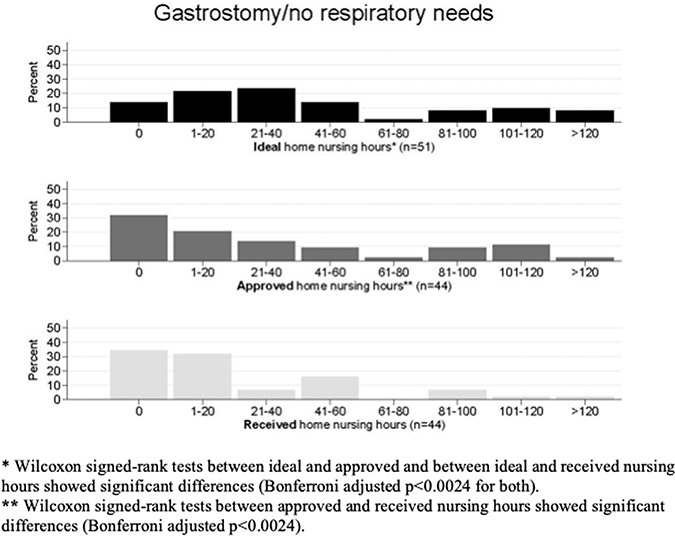
FIGURE A1.
Comparison of ideal, approved, and received nursing hours for patient with gastrostomy. Wilcoxon signed-rank tests between ideal and approved and between ideal and received nursing hours showed significant differences (Bonferroni adjusted p < .0024 for both). Wilcoxon signed-rank tests between approved and received nursing hours showed significant differences (Bonferroni adjusted p < .0024).
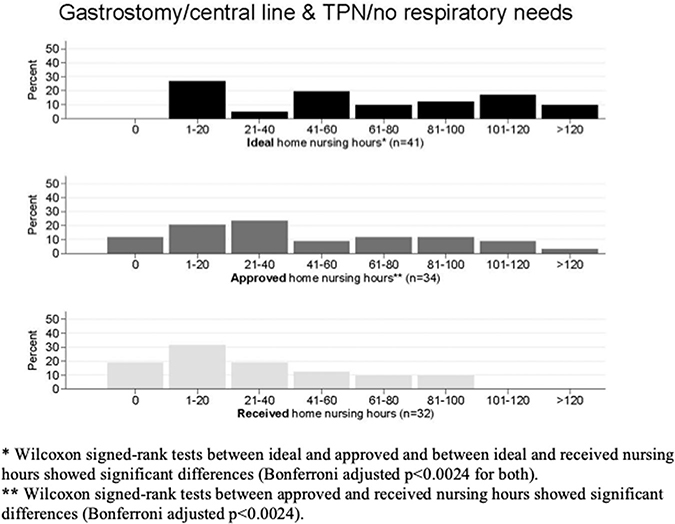
FIGURE B1.
Comparison of nursing hours for patient with gastrostomy, central line, and total parenteral nutrition (TPN). Wilcoxon signed-rank tests between ideal and approved and between ideal and received nursing hours showed significant differences (Bonferroni adjusted p < .0024 for both). Wilcoxon signed-rank tests between approved and received nursing hours showed significant differences (Bonferroni adjusted p < .0024).
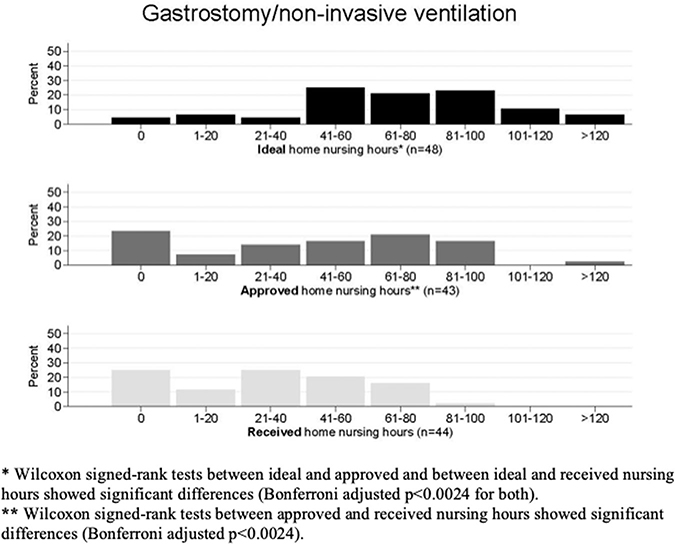
FIGURE C1.
Comparison of nursing hours for patient with gastrostomy and noninvasive ventilation. Wilcoxon signed-rank tests between ideal and approved and between ideal and received nursing hours showed significant differences (Bonferroni adjusted p < .0024 for both). Wilcoxon signed-rank tests between approved and received nursing hours showed significant differences (Bonferroni adjusted p < .0024).
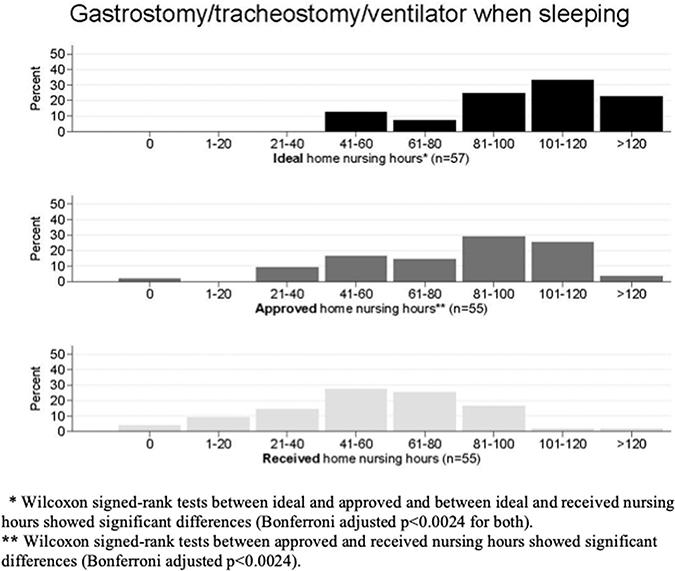
FIGURE D1.
Comparison of nursing hours for patient with gastrostomy, tracheostomy, and ventilator when sleeping. Wilcoxon signed-rank tests between ideal and approved and between ideal and received nursing hours showed significant differences (Bonferroni adjusted p < .0024 for both). Wilcoxon signed-rank tests between approved and received nursing hours showed significant differences (Bonferroni adjusted p < .0024).
FIGURE E1.
Comparison of nursing hours for patient with gastrostomy, tracheostomy, and oxygen. Wilcoxon signed-rank tests between ideal and approved and between ideal and received nursing hours showed significant differences (Bonferroni adjusted p < .0024 for both). Wilcoxon signed-rank tests between approved and received nursing hours showed significant differences (Bonferroni adjusted p < .0024).
Footnotes
CONFLICT OF INTERESTS
The authors have no conflict of interests.
REFERENCES
- 1.Olmstead vLC, (1999).
- 2.Simpser E, Hudak ML. Section on home care COCHF. Financing of pediatric home health care. Pediatrics. 2017;139:3. [DOI] [PubMed] [Google Scholar]
- 3.Hefner JL, Tsai WC. Ventilator-dependent children and the health services system. Unmet needs and coordination of care. Ann Am Thorac Soc. 2013;10(5):482–489. [DOI] [PubMed] [Google Scholar]
- 4.Foster CC, Agrawal RK, Davis MM. Home health care for children with medical complexity: workforce gaps, policy, and future directions. Health Aff (Millwood). 2019;38(6):987–993. [DOI] [PubMed] [Google Scholar]
- 5.Feudtner C The precarious imperative of home nursing for technology-dependent children. J Pediatr. 2019;212:10–12. [DOI] [PubMed] [Google Scholar]
- 6.Kaya K, Unsal-Delialioglu S, Ordu-Gokkaya NK, et al. Musculoskeletal pain, quality of life and depression in mothers of children with cerebral palsy. Disabil Rehabil. 2010;32(20):1666–1672. [DOI] [PubMed] [Google Scholar]
- 7.Miles MS, Holditch-Davis D, Burchinal P, Nelson D. Distress and growth outcomes in mothers of medically fragile infants. Nurs Res. 1999;48(3):129–140. [DOI] [PubMed] [Google Scholar]
- 8.Kirk S, Glendinning C, Callery P. Parent or nurse? The experience of being the parent of a technology-dependent child. J Adv Nurs. 2005; 51(5):456–464. [DOI] [PubMed] [Google Scholar]
- 9.Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: caregiver perspectives. Child Care Health Dev. 2007;33(2):180–187. [DOI] [PubMed] [Google Scholar]
- 10.Sobotka SA, Lynch E, Peek ME, Graham RJ. Readmission drivers for children with medical complexity: home nursing shortages cause health crises. Pediatr Pulmonol. 2020;55:1474–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weaver MS, Wichman B, Bace S, et al. Measuring the impact of the home health nursing shortage on family caregivers of children receiving palliative care. J Hosp Palliat Nurs. 2018;20(3):260–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maynard R, Christensen E, Cady R, et al. Home health care availability and discharge delays in children with medical complexity. Pediatrics. 2019;143:1. [DOI] [PubMed] [Google Scholar]
- 13.Sobotka SA, Foster C, Lynch E, Hird-McCorry L, Goodman DM. Attributable delay of discharge for children with long-term mechanical ventilation. J Pediatr. 2019;212:166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sterni LM, Collaco JM, Baker CD, et al. An Official American Thoracic Society Clinical Practice Guideline: pediatric chronic home invasive ventilation. Am J Respir Crit Care Med. 2016;193(8): e16–e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sobotka SA, Gaur DS, Goodman DM, Agrawal RK, Berry JG, Graham RJ. Pediatric patients with home mechanical ventilation: the health services landscape. Pediatr Pulmonol. 2019;54(1):40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Presser S, Couper MP, Lessler JT, et al. Methods for testing and evaluating survey questions. Public Opin Q. 2004;68(1):109–130. [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sobotka SA, Dholakia A, Agrawal RK, et al. Discharge practices for children with home mechanical ventilation across the United States: key informant perspectives [published online ahead of print August 11, 2020]. Ann Am Thorac Soc. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blair E A reflexive exploration of two qualitative data coding techniques. J Methods Meas Soc Sci. 2015;6(1):14–29. [Google Scholar]
- 20.Eysenbach G Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.EPSDT for States: Coverage in the Medicaid Benefit for Children and Adolescents - A Guide. Centers for Medicare & Medicaid Services; 2014. [Google Scholar]
- 22.Council On Community Pediatrics. Poverty and child health in the United States. Pediatrics. 2016;137:4–4A. [DOI] [PubMed] [Google Scholar]
- 23.Kirk S, Glendinning C. Developing services to support parents caring for a technology-dependent child at home. Child Care Health Dev. 2004;30(3):209–218. [DOI] [PubMed] [Google Scholar]
- 24.Dybwik K, Tollali T, Nielsen EW, Brinchmann BS. “Fighting the system”: families caring for ventilator-dependent children and adults with complex health care needs at home. BMC Health Serv Res. 2011;11:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Graham RJ, Rodday AM, Parsons SK. Family-centered assessment and function for children with chronic mechanical respiratory support. J Pediatr Health Care. 2014;28(4):295–304. [DOI] [PubMed] [Google Scholar]
- 26.Van Pelt DC, Milbrandt EB, Qin L, et al. Informal caregiver burden among survivors of prolonged mechanical ventilation. Am J Respir Crit Care Med. 2007;175(2):167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson S, Morse JM, Penrod J. Absolute involvement: the experience of mothers of ventilator-dependent children. Health Soc Care Community. 1998;6(4):224–233. [DOI] [PubMed] [Google Scholar]
- 28.Kirk S Families’ experiences of caring at home for a technology-dependent child: a review of the literature. Child Care Health Dev. 1998;24(2):101–114. [DOI] [PubMed] [Google Scholar]
- 29.Boroughs D, Dougherty JA. Decreasing accidental mortality of ventilator-dependent children at home: a call to action. Home Healthc Nurse. 2012;30(2):103–111. [DOI] [PubMed] [Google Scholar]
- 30.Kun SS, Beas VN, Keens TG, Ward SS, Gold JI. Examining pediatric emergency home ventilation practices in home health nurses: opportunities for improved care. Pediatr Pulmonol. 2015;50(7):691–697. [DOI] [PubMed] [Google Scholar]
- 31.Boroughs D, Dougherty JA. Care of technology-dependent children in the home. Home Healthc Nurse. 2009;27(1):37–42. [DOI] [PubMed] [Google Scholar]
- 32.Sobotka Saletwmm. Almost home kids: a unique hospital-to-home transitional care model for children with technology dependency. Complex Care Journal. 2019;1:1. [Google Scholar]
- 33.Leyenaar JK, O’Brien ER, Leslie LK, Lindenauer PK, Mangione-Smith RM. Families’ priorities regarding hospital-to-home transitions for children with medical complexity. Pediatrics. 2017;139:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sobotka SA, Foster C, Lynch E, Hird-McCorry L, Goodman DM. Attributable delay of discharge for children with long-term mechanical ventilation. J Pediatr. 2019;212:166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Suzuki S, Sato I, Emoto S, Kamibeppu K. Physio-psychological burdens and social restrictions on parents of children with technology dependency are associated with care coordination by nurses. J Pediatr Nurs. 2017;36:124–131. [DOI] [PubMed] [Google Scholar]
- 36.Impact Whiting M., meaning and need for help and support: the experience of parents caring for children with disabilities, life-limiting/life-threatening illness or technology dependence. J Child Health Care. 2013;17(1):92–108. [DOI] [PubMed] [Google Scholar]
- 37.Maddox C, Pontin D. Paid carers’ experiences of caring for mechanically ventilated children at home: implications for services and training. J Child Health Care. 2013;17(2):153–163. [DOI] [PubMed] [Google Scholar]
- 38.Israelsson-Skogsberg A, Lindahl B. Personal care assistants’ experiences of caring for people on home mechanical ventilation. Scand J Caring Sci. 2017;31(1):74. [DOI] [PubMed] [Google Scholar]