Abstract
There is currently a shortage of neurologists in the United States. Multiple efforts are underway to increase the strength of the neurology workforce. One potential approach is early exposure to neurology research and clinical care to pique interest and promote the specialty as a career choice. This study details the rewarding experience of working with undergraduate students, both in clinical research and clinical care. The logistics, benefits to students, and positive aspects for neurologists are outlined. Examples provided by undergraduate students who have participated in neurology research and clinical care are presented. The ultimate goals of this work are to encourage and inspire academic neurologists to involve undergraduate students in research and clinical care, to facilitate this process by outlining the steps needed to make this pairing successful, and to ultimately promote a pathway to build the neurology pipeline.
Introduction
Academic neurologists have the privilege of interacting with a wide variety of learners, including medical students, residents, and fellows. In addition, some have the opportunity to work with undergraduate students. As clinician-researchers in neurology who combined have mentored over 50 undergraduate students over the past 7 years, we are inspired to share our experiences in mentoring undergraduate students and the rewarding and logistical processes of incorporating undergraduates in clinical and research work.
In this “Contemporary Issues” article, we discuss how working with undergraduate students represents a unique opportunity to expose students to neurology through research and clinical care while also generating many beneficial experiences for the student and the neurologist. We outline potential benefits, and logistical considerations, involved in working with undergraduate students. Neurology is a unique specialty with an abundance of fascinating diseases that can be explored, a significant number of treatments available for patients, and additional needed treatments ripe for development and discovery. Research and clinical care are excellent opportunities to excite students to these facets of neurology.
We incorporated undergraduate student perspectives regarding the impact of their experiences on their personal and professional lives. In total, we received reflections (n = 32), emails (n = 4), applications for opportunities (n = 7), and a program feedback survey (n = 1). In a process considered exempt by the Wake Forest Baptist Institutional Review Board, we qualitatively analyzed these data into themes with representative examples to best understand each theme. The student reflections illustrate how much undergraduate students crave hands-on clinical experiences and appreciate the opportunity to work alongside a neurologist through clinical research and patient care. Such experiences can guide career choices for whether to enter the field of medicine and neurology.
The Importance of Building the Neurology Pipeline
There is currently a shortage of neurologists in the United States. The demand for neurologists is projected to grow faster than supply, with an expected need of an additional 21,400 neurologists by 2025, leading to at least an 18% shortfall.1
Multiple efforts have been made by the American Academy of Neurology (AAN) to alleviate this neurology provider shortage, from revitalizing the medical student Special Interest Groups in Neurology to developing a program specifically for increasing advanced practice providers in neurology.2 In this “Contemporary Issues” article, we demonstrate the potential power and downstream effects of an earlier onset broader scope approach starting at the undergraduate level of education. Specifically, the neurology pipeline could be enhanced by focusing on engaging undergraduate students. Interest in neurosciences at the college level is increasing, demonstrated by the dramatic increase in neuroscience programs and majors across US undergraduate institutions from 9 programs with 99 graduates in 1989 to 223 programs with 7,208 graduates in 2018. Nearly 20% of neuroscience majors aspire to apply to medical school.3 Neuroscience and psychology are the 2 most common undergraduate majors of those entering the field of neurology. In a study of graduating medical students, of the nearly 100 listed undergraduate majors they might have chosen from, those entering neurology were more likely to list an undergraduate neuroscience major or psychology major (13.3%, 8.0%, respectively) compared with those not entering neurology (4.5%, 5.1% respectively).4
Unfortunately, many undergraduate neuroscience majors are only exposed to basic science and not clinical neurology. For example, students may be more likely to be partnered with basic science mentors for thesis completion than with clinician researchers. With this growth in neuroscience majors at institutions across the country, an opportunity exists to develop appropriate curricula, training, mentoring, and research experiences for those interested in a career in the neurosciences.3 Gaining exposure to clinical neurology at this critical time in a person's career development could have significant impact on career choice. Unlike primary care or certain surgical specialties (e.g., orthopedics), neurology is not widely known or considered as a future career by undergraduate students. Of students matriculating into medical school, neurology is only considered as a future specialty by 2.7% of students.
The Undergraduate Years are Formidable Years When Clinical Research Experiences Can Foster Interest in Science, Technology, Engineering, and Medicine
Previous research has shown that undergraduate clinical and research experiences can increase interest in science, technology, engineering, and medicine (STEM). In a longitudinal evaluation of 149 high school and undergraduate students who gained hands-on research experience in Aspiring Scientists Summer Internship Programs at George Mason University, hands-on laboratory work was stated as sustaining their interest in STEM (92.6%). Furthermore, close to 74% of students who previously planned to stop their educational pursuits after earning a bachelor's degree stated interest in obtaining an advanced degree. Of the 19 students who changed their mind, they cited a desire to earn a master's degree (47.4%), MD (15.8%), or PhD (10.5%).5 In another study of the Arkansas Institutional Development Award Networks of Biomedical Research Excellence (INBRE) undergraduate summer student-mentored research program, since 2001, nearly half of the 202 participants enrolled in graduate school or a licensed medical professional program.6 Furthermore, in a study examining the perceptions of an undergraduate pathology and laboratory medicine research program on career development, researchers surveyed 102 former interns from a 15-year period. Just over half (57%) responded and 96% (46/48) strongly agreed/agreed that the perceived internship was advantageous when applying for career/professional opportunities, 93% strongly agreed/agreed that the internship was an important part of their career development, and 44% received additional education after completing their undergraduate degree with 25% receiving a doctoral degree. Importantly, based on their internship experience, 55% strongly agreed/agreed that they positively considered pathology or laboratory medicine as a career choice.7 Thus, not only have programs helped students pursue advanced degrees in the health professions and in research, programs in other fields such as pathology have helped to develop interest in that specific field.
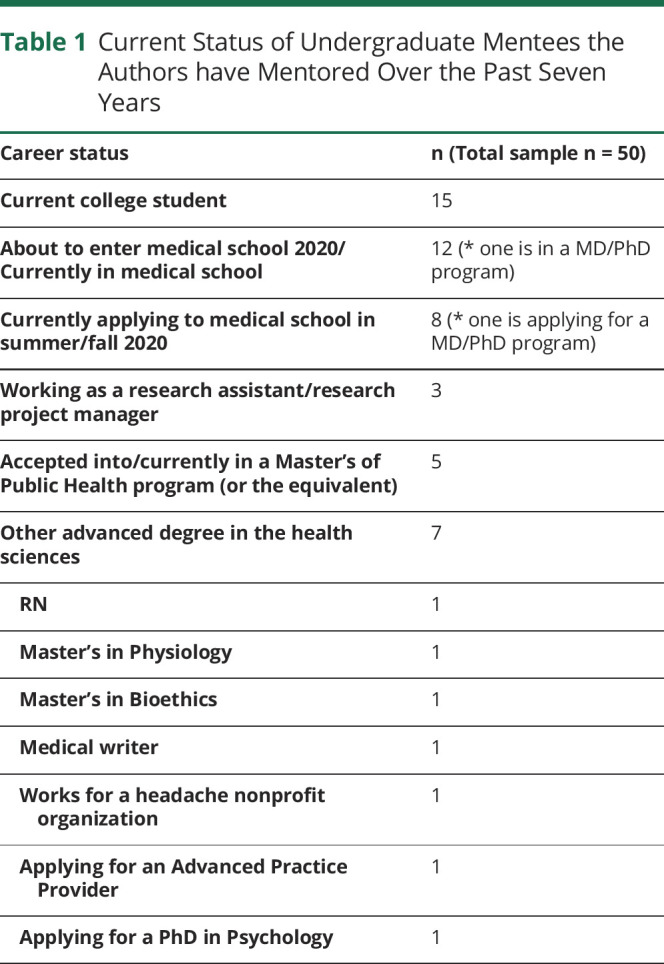
Among the 50 undergraduate students we have mentored over the past 7 years, 80% (40) of the undergraduates were female, which could reflect the gender alignment of the authors with students or the increasing matriculation of women in medicine.8 As shown in table 1, at the time of submission, 20 of 50 were applying to, accepted into, or matriculated in medical school, 15 of 50 remained as college students, and 7 of 50 were applying to/accepted into/matriculated in master's programs related to health. Future longitudinal work may help us determine whether they choose neurology residency.
Table 1.
Current Status of Undergraduate Mentees the Authors have Mentored Over the Past Seven Years
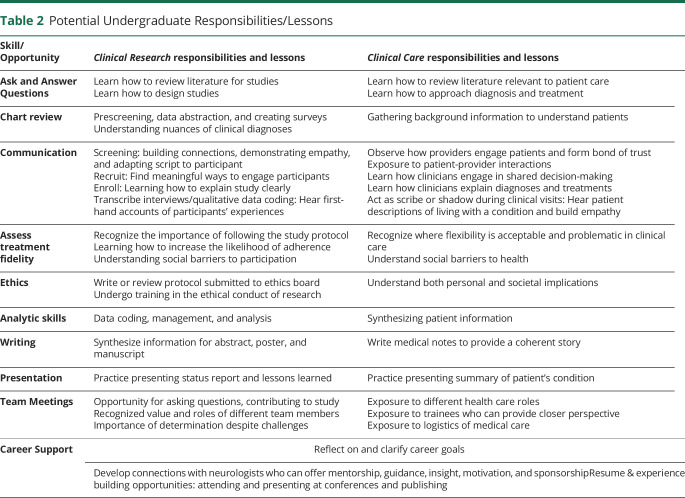
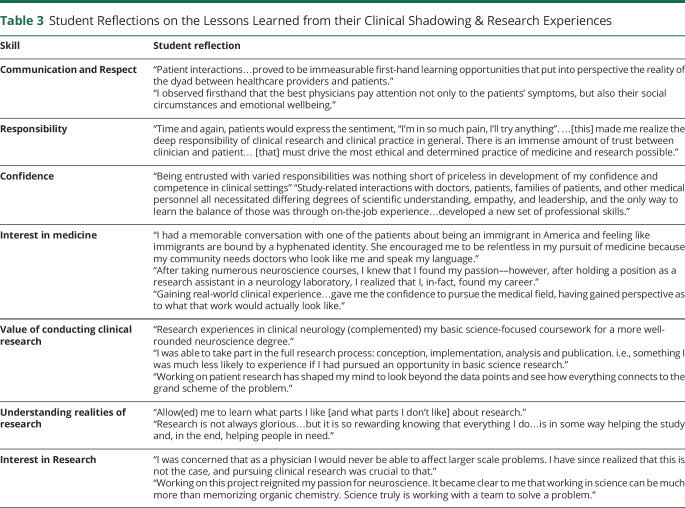
How Undergraduate Students Benefit From Opportunities With Neurologists
Undergraduate students want to learn and grow. They desire opportunities to be challenged and stimulated, and the experience of shadowing neurologists in the clinical setting and serving on a clinical research team has a powerful impact on their careers, with meaningful responsibilities and valuable lessons learned (table 2). Students are able to learn how to ask and answer questions, conduct background research, perform chart reviews, build communication skills, gain perspective from a patient or participant's viewpoint, assess and maximize treatment fidelity, grasp ethical dilemmas and challenges, observe visits, build analytic, writing, and presentation skills, and engage in meaningful group communication. Themes from the students' reflections about exposure to clinical research and clinical shadowing include learning about communication and respect, responsibility, confidence, interest in medicine, the value of conducting clinical research, understanding the realities of research, and interest in research (table 3).
Table 2.
Potential Undergraduate Responsibilities/Lessons
Table 3.
Student Reflections on the Lessons Learned from their Clinical Shadowing & Research Experiences
The Positive Impact on the Neurologists: How Opportunities Can Be Maximized and Mutually Beneficial For Undergraduate Students and Neurologists
Although faculty are invaluable in creating a positive experience for the students, the benefits are mutual. Faculty can gain a sense of purpose, accomplishment, and meaning in their roles, and this can potentially alleviate burnout.9
In addition, because students can be a very valuable asset to help conduct research and support clinical work, they can help to advance healthcare goals in a multitude of ways with appropriate training and supervision (table 2). Students often bring a fresh perspective and younger mindset to the work being conducted. They may be aware of effective advertising platforms or tools that can significantly increase recruitment rates for a study. Students are also often adept at technology and can help develop online studies or develop patient- and participant-facing materials for clinicians and researchers.
Students can also be involved in the abstract, poster, and/or manuscript preparation process. Students can either develop their own abstracts for research programs at their schools and/or can help develop abstracts and poster presentations for an instructional neurology department (or population health department or neuroscience department or quality or hospital) research day, the State Neurologic Society meeting, or a national meeting. The AAN has traditionally waived the annual meeting registration fee for undergraduate students who are presenting posters at the meeting. In our experience, students have obtained travel funds from their university to cover the cost of travel to the meeting. Students who put in excellent effort may also be included as a coauthor on a publication.
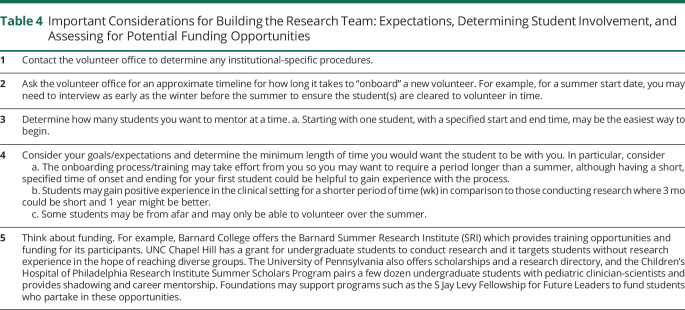
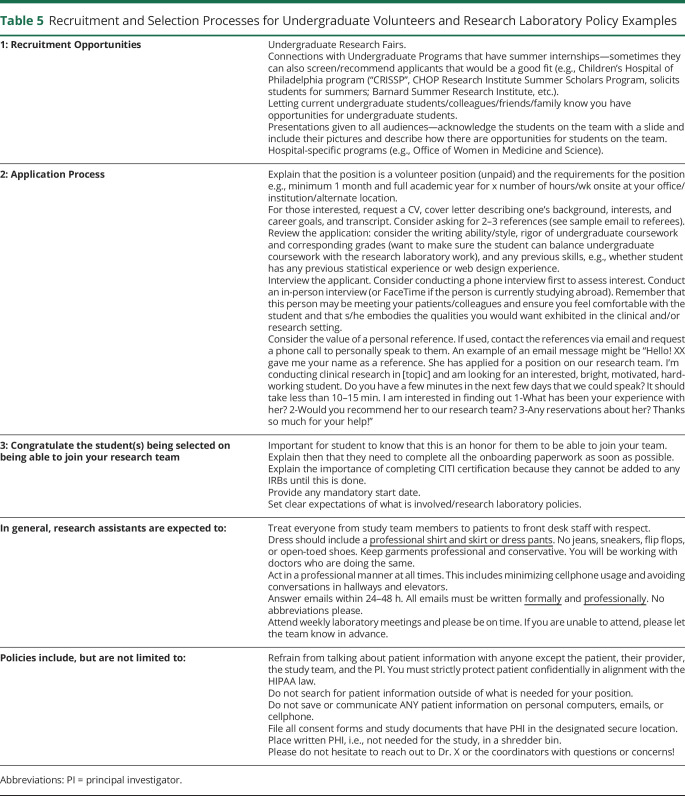
The Logistics of How to Include Students in Clinical and/or Research Programs
It is important to understand specific institutional policies for involving undergraduate volunteers (who may even be called “nontraditional volunteers” or a similar name by your institution since they are volunteering for you with specific duties) and to work with your institution's volunteer office to ensure appropriate “onboarding” or “credentialing.” Taking into account the length of the institution's onboarding process and any necessary training, the neurologist should consider the minimum time commitment they require for the student(s). Having mentored medical students, residents, and fellows, undergraduate students tend to have the most time available in blocks or over time to partake in the research laboratory experience, whether for a single summer or for as long as 4 years. Defining expectations, determining student involvement, and assessing for potential funding opportunities are helpful early steps (table 4). Understanding effective recruitment and selection processes for undergraduate volunteers is invaluable (table 5). Students come from a variety of backgrounds, although most often from neuroscience, biology, or psychology majors.
Table 4.
Important Considerations for Building the Research Team: Expectations, Determining Student Involvement, and Assessing for Potential Funding Opportunities
Table 5.
Recruitment and Selection Processes for Undergraduate Volunteers and Research Laboratory Policy Examples
Other key aspects to consider for including undergraduate students in your clinical and/or research work include coordinating and overseeing students, team meetings, communication, space, and dissemination of educational opportunities.
Coordinating/Overseeing Students
Typically, the neurologist or principal investigator (PI) is the senior supervisor and mentor for undergraduate students. If available, a full-time research study staff member, a hired part-time postbaccalaureate student, or a “Chief” laboratory member may manage the students. Having help to coordinate onboarding, student shifts, and other administrative duties can be extremely valuable.
Clearly defining expectations for students can ensure a smooth experience, such as defining expected weekly hours of effort, establishing parameters on working from home vs in-person, research responsibilities, and required readings. Students can be informed that, with appropriate hard work, dedication, and fulfillment of expected responsibilities, the faculty member will provide a letter of recommendation for graduate or medical school. Once expectations are clearly defined, it is much easier to have a frank discussion regarding a student's goals and whether the student is still a good fit for the team if expectations are not being met.
Professionalism & Communication
Many students may have limited previous exposure to the healthcare environment, so discussions on the importance of professionalism and policies in the workplace are critical. Table 4 provides a sample of laboratory policies that can be customized and shared with students. Defining best forms of receiving and responding to information also helps ensure effective communication (e.g., email and texts).
Laboratory/Team Meetings
Student availability for team meetings is often dictated by the timing of their undergraduate classes, with weeknight or weekend meetings sometimes needed. Meetings can serve 2 functions: educating students on research processes and conducting research protocols and tasks. Witnessing the multitude of elements involved in conducting clinical research is invaluable, such as study team members' roles, study logistics, and coordination. Time for discussion of their perspectives and experiences can provide critical information because they can serve as the “eyes and ears” of the study. They may also have ideas on how to better organize laboratory tasks and reach study subjects. Team meetings are also an important time to engage, inspire, motivate, and create a group bond. One might set time aside to hear “personal updates” from each team member. This can help connect team members and help the PI know the realities of the life the students are living. Keeping track of students' upcoming deadlines, holidays, examinations, and celebrating birthdays or other accomplishments, such as having taken the Medical College Admissions Test or Graduate Record Examination, can help unite the group. Finding time to get together outside of the work environment can also help with team cohesion. Whether it is a meal out at a restaurant, at a faculty member's home, or having a fun outing as a group, this time together can increase unity and strength of the team unit.
Resources From the Department
In most cases, few resources are required from the department, although physical space is often the most valued commodity. Some students have shared office space, whereas others may need to work off-site. It may be helpful to define and create an electronic, secure, HIPAA-compliant space within which students and the PI can collaborate and share documents such as a shared network drive.
Disseminating Information About Other Educational Opportunities
In addition to all of the opportunities provided by the direct experience and exposure of working together, undergraduate students appreciate being updated about other potential educational opportunities across the medical center, for example, Grand Rounds, medical student problem-based learning sessions you are leading. Allowing students to participate in and observe meaningful conversations between providers and medical trainees can also offer valuable learning.
Funding
Most undergraduate students volunteer their time and energy for the opportunity to work with a neurologist (e.g., a nonpaid position). There are opportunities in which undergraduate students might be able to seek funding through their institution, such as through a department grant or internship placement program, or external organizations offering stipends in STEM opportunities. We are very excited by the new AAN Neuroscience is Rewarding Program,10 an internship program intended to provide an “opportunity to experience working in a clinic, research, or academic environment with mentorship from an AAN member. The goal of the internship is to provide college students with an experience working in neuroscience and exposure to patient care in neurology.” The program is currently in its second year, and it is a prestigious opportunity for both the PI and for the student.
Future Directions
Collaboration with undergraduate schools could be considered on a local level, through individual academic medical institutions or private neurology practices, and at the national level, such as through the NIH and the AAN Institute (AANI).
Local Level
Locating undergraduate institutions with neuroscience offerings can be challenging because there are different websites but not all websites may be inclusive. Currently, the Association of Neuroscience Departments and Programs has a website with search capability for neuroscience programs in the United States, Canada, and abroad, but has a membership fee. The website for the National Center for Education Statistics, a branch of the Institute of Education Sciences of the US Department of Education, includes a College Navigator search engine that is searchable by program/major. Although some schools offer neuroscience majors, other schools include them as concentrations within the biology or psychology major or may use alternate terms such as “cognitive science” or “biopsychology.”11
Developing relationships and collaborative programs may also enhance current clinical neuroscience programs or help develop neuroscience majors. Engaging undergraduate students in clinical neurology practice and research should be as important a priority as engaging students in basic neuroscience research, and additional efforts need to be made on this path. One profound example of the impact of such a program is the universally positive response and feedback of students who have participated in the Virginia Tech School of Neuroscience “Clinical Neuroscience in Practice” course. This formal course of weekly 75-minute seminars covering diseases affecting the nervous system, along with weekly half-day intensive clinical experiences throughout the hospital, has been described by students as the “most valuable and insightful experience they had in their college career.”12 Summer programs such as “PURE” developed to improve the pipeline of pain medicine specialists can also be used as models. “PURE” is a program for undergraduate students that integrates pain research, clinical opportunities, pain journal club, and an ethics program and culminates in a pain conference.13
The field of neuroscience has done an excellent job of specifically targeting and reaching out to those at the undergraduate level, and the field of neurology could learn from their efforts. The Faculty for Undergraduate Neuroscience (FUN; funfaculty.org) has developed a journal devoted to undergraduate neuroscience education (funjournal.org) and has held workshops to develop undergraduate education including new faculty development programs, for example, Support for Mentors and their Students.14 In addition, they have worked with the Society for Neuroscience (SfN) to have undergraduate members, encourage undergraduate attendance at the SfN meeting (may have had more than 2,000), and hold undergraduate poster sessions (which have been extremely popular with up to 400–500 people in attendance).14 They have also sponsored travel awards for students to attend the meeting. Finally, they have developed regional neuroscience meetings such as “NEURON (Northeast), SYNAPSE (Southeast), and MIDBRAIN (Midwest) for undergraduates to have research symposia and networking.14 A study surveying the FUN faculty revealed, “Many of the faculty responses about their former travel award students spoke to the student's indecision regarding postgraduate plans-but that attendance at SfN convinced these students to pursue graduate school.”14
National Level
The NIH, foundations including the AANI, and the undergraduate schools could also help fund programs to connect undergraduate students with interested clinicians and those conducting clinical neurology research and to recognize the mentors for their work in increasing awareness about the field. The NIH has a program to “stimulate research in educational institutions that provide baccalaureate or advanced degrees for a significant number of the Nation's research scientists, but that have not been major recipients of NIH support. These grants are intended to create a research opportunity for scientists and institutions otherwise unlikely to participate extensively in NIH programs to support the Nation's biomedical and behavioral research effort.”15 The National Institute of Neurologic Disorders and Stroke is one of the arms of the NIH that is distributing the award. The expansion of this program to emphasize including undergraduate trainees in the research or the creation of new grants to help fund students involved in clinical research could make a significant difference in increasing undergraduates' involvement in clinical neurology research. The benefits of foundational grants that provide funding to undergraduate students, for example, S. J Levy Fellowship,16 are significant, and more spots in programs such as these and the development of more programs is needed. It would also be helpful to have a centralized website for students and faculty mentors that describes the various opportunities for undergraduates across the country.
Diversity
Increasing diversity in the medical workplace is an important priority to the AAN, as evidenced by the creation of the AAN Joint Coordinating Council on Equity, Diversity, Inclusion, and Disparities and Diversity Officer Workgroup.17 Involving diverse undergraduate students in clinical research and clinical care experiences may have a long-term impact on increasing the diversity of our field. Additional funding programs for undergraduate students to participate in research will increase access of such opportunities for students of all backgrounds. If a research position is unpaid, it can unintentionally limit access to only those who have the resources to participate in such volunteer work. Creating funded positions, and recruiting students from all backgrounds, may have a significant impact to help increase the diversity of undergraduates conducting research. We also note that the vast majority of our undergraduate trainees were women, and this can help the women in neurology pipeline, including perhaps women conducting neurology research.18
Conclusion
Engaging undergraduate students in clinical neurology practice and research provides extraordinary opportunities for both the student and the neurologist. Undergraduate students can meaningfully contribute in a variety of ways as part of a clinical research team and a clinical care team. These opportunities provide students with exposure to a variety of aspects of clinical research and patient care that can 1) provide direct learning experiences, 2) help develop and refine personal and professional attributes, 3) influence personal and professional development, and 4) fuel interest in medicine and neurology. Furthermore, the ability for faculty to engage with students and help shape their careers can provide a tremendous sense of accomplishment and meaning to help offset the challenges of medicine today and risks of burnout. Increasing interest in neurology at the undergraduate level may have a profound impact on expanding the neurology pipeline, which is critical for our nation to care for the neurologic needs of our patients in the future.
Acknowledgment
We thank Dr. Raddy Ramos for his guidance in finding valuable articles that could strengthen our study. We thank Ms. Sarah Corner for her help coordinating this submission. We have sincere gratitude for all of the trainees who have worked with us to date. Without their help, we would not have been able to accomplish all of the research we have conducted. Moreover, we have grown from them personally and professionally. In particular, we would like to thank the following individuals who conducted research with us as undergraduates and who provided us with the written communication from which this article is based. We appreciate all our students' dedication and hard work, including Vinish Kumar, Rosalia Arnolda, Paige Brabant, Danika Berman, Flora Chang, Caitlyn Margo, Easton Howard, Geena George, Camden Nelson, Reid Anderson, Mariam Shakir, Anissa Berger, Summer Beeghly, Grace Posney, Kailyn Witonsky, Hannah Mumber, Rachel Gerard, Robert Rennie, Gerardo Velasquez, Clare Stoyell-Mulholland, Pratishtha Panigrahi, Adama Jalloh, Alexandra Boubour, Ashna Shome, Talia Boyers, Emma Ortega, Gabriella Sahyoun, Jana Jaran, Ariana Gopal, Fatoumata Sow, Sarah Jinich, Mia Chin, Seher Ali, Tyler Gumpel, Valeria Grajales, Kaitlyn Toy, and Jonathan Tratner.
We are grateful for funding that helped support our undergraduate students' efforts. The AAN's Neuroscience is Rewarding scholarship has provided funding for many of our students, including those of Drs. Minen, Cartwright, and Wells. Dr. Minen appreciates the funding provided to some of her students from the Barnard Summer Research Institute and from the S. Jay Levy Fellowship for Future Leaders. Dr. Wells appreciates the matching financial support from the Department of Neurology at Wake Forest Baptist Health. Dr. Szperka's students have received funding from the Children's Hospital of Philadelphia Research Institute Summer Scholars Program funded by NIH R25HD082842 (Advancing Child Health: Preparing the Next Generation of Pediatric Researchers), from the CHOP Neurology High School Summer Scholars Program, and from a donation from Miles for Migraine.
Contributor Information
Christina L. Szperka, Email: szperka@email.chop.edu.
Michael S. Cartwright, Email: mcartwri@wakehealth.edu.
Rebecca Erwin Wells, Email: rewells@wakehealth.edu.
Study Funding
Dr. Minen is supported by the National Center for Complementary & Integrative Health (NCCIH) of the NIH under Award Number NCCIH K 23 AT009706. She is also recipient of the Doris Duke Fellowship to Retain Clinical Scientists. Dr. Szperka receives research funding from NIH K23NS102521. Dr. Cartwright receives royalties from Elsevier for the textbook Neuromuscular Ultrasound. Dr. Wells is supported by the NCCIH of the NIH under Award Number K23AT008406. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure
Dr. Minen is supported by the National Center for Complementary & Integrative Health (NCCIH) of the National Institutes of Health (NIH) under Award Number NCCIH K 23 AT009706. She is also recipient of the Doris Duke Fellowship to Retain Clinical Scientists; Dr. Szperka receives research funding from NIH K23NS102521; Dr. Cartwright receives royalties from Elsevier for the textbook Neuromuscular Ultrasound; Dr. Wells is supported by the NCCIH of the NIH under Award Number K23AT008406.
References
- 1.Dall TM, Storm MV, Chakrabarti R, et al. Supply and demand analysis of the current and future US neurology workforce. Neurology 2013;81:470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morgenlander JC, Blessing R. The duke neurology advanced practice provider residency: its time has come. Neurol Clin Pract 2016;6:277–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramos RL, Guercio E, Levitan T, O'Malley S, Smith PT. A quantitative examination of undergraduate neuroscience majors applying and matriculating to osteopathic medical school. J Undergrad Neurosci Educ 2016;14:A87–A90. [PMC free article] [PubMed] [Google Scholar]
- 4.Gutmann L, Cahill C, Jordan JT, et al. Characteristics of graduating US allopathic medical students pursuing a career in neurology. Neurology 2019;92:e2051–e2063. [DOI] [PubMed] [Google Scholar]
- 5.VanMeter-Adams A, Frankenfeld CL, Bases J, Espina V, Liotta LA. Students who demonstrate strong talent and interest in STEM are initially attracted to STEM through extracurricular experiences. CBE Life Sci Educ 2014;13:687–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McSweeney JC, Hudson TJ, Prince L, et al. Impact of the INBRE summer student mentored research program on undergraduate students in Arkansas. Adv Physiol Educ 2018;42:123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howell LP, Wahl S, Ryan J, Gandour-Edwards R, Green R. Educational and career development outcomes among undergraduate summer research interns: a pipeline for pathology, laboratory medicine, and biomedical science. Acad Pathol 2019;6:2374289519893105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.AAMC. AAMC Applicant Matriculant Data File as of 11/26/2018: AAMC; 2018. [Google Scholar]
- 9.LaFaver K, Miyasaki JM, Keran CM, et al. Age and sex differences in burnout, career satisfaction, and well-being in US neurologists. Neurology 2018;91:e1928–e1941. [DOI] [PubMed] [Google Scholar]
- 10.2018 Neuroscience is… Rewarding Internship program. American Academy of Neurology. Available at: aan.com/education-and-research/neuroscience-is/neuroscience-is-rewarding/internship-program/. Accessed April 1, 2020. [Google Scholar]
- 11.Ramos RL, Fokas GJ, Bhambri A, Smith PT, Hallas BH, Brumberg JC. Undergraduate neuroscience education in the U.S.: an analysis using data from the national center for education statistics. J Undergrad Neurosci Educ 2011;9:A66–A70. [PMC free article] [PubMed] [Google Scholar]
- 12.Simonds GR, Marvin EA, Apfel LS, et al. Clinical neuroscience in practice: an experiential learning course for undergraduates offered by neurosurgeons and neuroscientists. J Undergrad Neurosci Educ 2018;16:A112–A119. [PMC free article] [PubMed] [Google Scholar]
- 13.Kolber BJ, Janjic JM, Pollock JA, Tidgewell KJ. Summer undergraduate research: a new pipeline for pain clinical practice and research. BMC Med Educ 2016;16:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hardwick JC, Smith JS. Undergraduate neuroscience faculty: results from a survey of faculty for undergraduate neuroscience members. J Undergrad Neurosci Educ 2010;8:A101–A107. [PMC free article] [PubMed] [Google Scholar]
- 15.NIH R15 Academic Research Enhancement Award (AREA). National Institute of Neurological Disorders and Stroke, NINDS Grant Mechanisms, Research Project Grants. Available at: ninds.nih.gov/Funding/About-Funding/Grant-Mechanisms#R15%20Academic%20Research%20Enhancement%20Award%20(AREA). Accessed April 1, 2020. [Google Scholar]
- 16.S Jay Levy Fellowship for Future Leaders. The City College of New York. Available at: ccny.cuny.edu/sjaylevy. Accessed April 1, 2020. [Google Scholar]
- 17.Equity, Diversity, and Inclusion. American Academy of Neurology. Available at: aan.com/conferences-community/member-engagement/diversity/?utm_source=Informz&utm_medium=Email&utm_campaign=Letter%20from%20AAN%20President&_zs=auLlW1&_zl=w2vX5. Accessed June 24, 2020. [Google Scholar]
- 18.Minen M, Law EF, Harriott A, et al. Challenges to successful research careers in neurology: how gender differences may play a role. Neurology 2020;95:349–359. [DOI] [PMC free article] [PubMed] [Google Scholar]