Giske Opheim
Giske Opheim, MSc
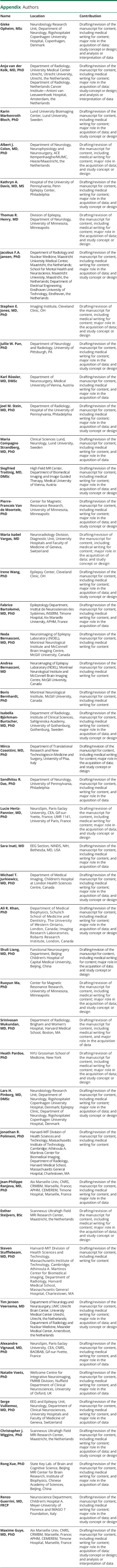
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,✉,
Anja van der Kolk
Anja van der Kolk, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Karin Markenroth Bloch
Karin Markenroth Bloch, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Albert J Colon
Albert J Colon, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Kathryn A Davis
Kathryn A Davis, MD, MS
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Thomas R Henry
Thomas R Henry, MD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Jacobus FA Jansen
Jacobus FA Jansen, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Stephen E Jones
Stephen E Jones, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Jullie W Pan
Jullie W Pan, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Karl Rössler
Karl Rössler, MD, DMSc
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Joel M Stein
Joel M Stein, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Maria C Strandberg
Maria C Strandberg, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Siegfried Trattnig
Siegfried Trattnig, MD, DMSc
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Pierre-Francois Van de Moortele
Pierre-Francois Van de Moortele, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Maria Isabel Vargas
Maria Isabel Vargas, MD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Irene Wang
Irene Wang, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Fabrice Bartolomei
Fabrice Bartolomei, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Neda Bernasconi
Neda Bernasconi, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Andrea Bernasconi
Andrea Bernasconi, MD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Boris Bernhardt
Boris Bernhardt, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Isabella Björkman-Burtscher
Isabella Björkman-Burtscher, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Mirco Cosottini
Mirco Cosottini, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Sandhitsu R Das
Sandhitsu R Das, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Lucie Hertz-Pannier
Lucie Hertz-Pannier, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Sara Inati
Sara Inati, MD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Michael T Jurkiewicz
Michael T Jurkiewicz, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Ali R Khan
Ali R Khan, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Shuli Liang
Shuli Liang, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Ruoyun Emily Ma
Ruoyun Emily Ma, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Srinivasan Mukundan
Srinivasan Mukundan, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Heath Pardoe
Heath Pardoe, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Lars H Pinborg
Lars H Pinborg, MD, DMSc
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Jonathan R Polimeni
Jonathan R Polimeni, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Jean-Philippe Ranjeva
Jean-Philippe Ranjeva, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Esther Steijvers
Esther Steijvers, BSc
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Steven Stufflebeam
Steven Stufflebeam, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Tim J Veersema
Tim J Veersema, MD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Alexandre Vignaud
Alexandre Vignaud, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Natalie Voets
Natalie Voets, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Serge Vulliemoz
Serge Vulliemoz, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Christopher J Wiggins
Christopher J Wiggins, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Rong Xue
Rong Xue, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Renzo Guerrini
Renzo Guerrini, MD, FRCP
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1,
Maxime Guye
Maxime Guye, MD, PhD
1From the Neurobiology Research Unit (G.O., L.H.P.), and Epilepsy Clinic (L.H.P.), Department of Neurology, Rigshospitalet Copenhagen University Hospital; Faculty of Health and Medical Sciences (G.O.), UCPH, Denmark; Departments of Neurology and Neurosurgery (T.J.V.), UMC Utrecht Brain Center, and Department of Radiology (A.v.d.K.), University Medical Center Utrecht, Utrecht University; Department of Radiology (A.v.d.K.), Netherlands Cancer Institute Antoni van Leeuwenhoek Hospital, Amsterdam; Lund University Bioimaging Center (K.M.B.), Lund University, Sweden; Department of Neurology (A.J.C.), Neurophysiology and Neurosurgery, ACE Kempenhaeghe/MUMC, Heeze/Maastricht, the Netherlands; Department of Radiology (J.M.S.) and Penn Epilepsy Center (K.D.), Hospital of the University of Pennsylvania, Philadelphia; Department of Neurology (T.R.H.) and Center for Magnetic Resonance Research (P.-F.V.d.M., R.E.M.), University of Minnesota, Minneapolis; Department of Radiology and Nuclear Medicine (J.F.A.J.), Maastricht University Medical Center; School for Mental Health and Neuroscience (J.F.A.J.), Maastricht University; Department of Electrical Engineering (J.F.A.J.), Eindhoven University of Technology, the Netherlands; Imaging Institute (S.E.J.) and Epilepsy Center (I.W.), Cleveland Clinic, OH; Department of Neurology and Radiology (J.W.P.), University of Pittsburg, PA; Department of Neurosurgery (K.R.), Medical University of Vienna, Austria; Departments of Neurology and Clinical Sciences (M.C.S.), Lund University Hospital, Sweden; Department of Biomedical Imaging and Image Guided Therapy (S.T.), High Field MR Center, Medical University of Vienna, Austria; Neuroradiology Division, Diagnostic Unit (M.I.V.), University Hospitals and Faculty of Medicine of Geneva, Switzerland; Epileptology Department - INS (F.B.) and CRMBM - CEMEREM (J.-P.R., M.G.), Timone Hospital APHM, Aix Marseille Univ, INSERM, CNRS, France; Neuroimaging of Epilepsy Laboratory (NOEL) (N.B., A.B.), Montreal Neurological Institute (B.B.), and McConnell Brain Imaging Centre (N.B., A.B.), McGill University, Montreal, Canada; Department of Radiology (I.B.-B.), Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Sweden; Department of Translational Research and New Technologies in Medicine and Surgery (M.C.), University of Pisa, Italy; Department of Neurology (S.R.D.), University of Pennsylvania, Philadelphia; NeuroSpin (L.H.-P., A.V.), Paris-Saclay University, CEA, CNRS, BAOBAB, Gif-sur-Yvette, France; UMR 1141 (L.H.-P), University of Paris, France; EEG Section (S.I.), NINDS, NIH, Bethesda, MD; Department of Medical Imaging (M.T.J.), Children’s Hospital at London Health Sciences Centre; Department of Medical Biophysics (M.T.J., A.R.K.), Schulich School of Medicine and Dentistry, The University of Western Ontario, London, Canada; Imaging Research Laboratories (A.R.K.), Robarts Research Institute, London, ON, Canada; Functional Neurosurgery Department (S.L.), Beijing Children’s Hospital of Capital Medical University, Beijing, China; Department of Radiology (S.M.), Brigham and Women’s Hospital, Harvard Medical School, Boston, MA; NYU Grossman School of Medicine (H.P.), New York; Harvard MIT Division of Health Sciences and Technology (J.R.P., S.S.), Massachusetts Institute of Technology, Cambridge; Athinoula A. Martinos Center for Biomedical Imaging (J.R.P., S.S.), Department of Radiology, Harvard Medical School, Massachusetts General Hospital, Charlestown, MA; Scannexus Ultrahigh Field MRI Research Center (E.S., C.J.W.), Maastricht; Department of Radiology and Nuclear Medicine (T.J.V.), Meander Medical Center, Amersfoort, the Netherlands; Wellcome Centre for Integrative Neuroimaging (N.V.), FMRIB Division, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom; EEG and Epilepsy Unit (S.V.), Neurology, Department of Clinical Neurosciences, University Hospitals and Faculty of Medicine of Geneva, Switzerland; State Key Lab of Brain and Cognitive Science (R.X.), Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, China; Neuroscience Department (R.G.), Children’s Hospital A. Meyer-University of Florence; and IMAGO 7 Foundation (R.G.), Florence, Italy
1