Abstract
Since the first case report on COVID-19, its transmission took place rapidly across the globe. Currently, it is reported to be spread into a total of 216 countries and territories. The suppression on industrial and gasoline burning activities accompanied after COVID-19 lock down favorably boosted the nature to restore its deteriorated sections such as in air with the improved Air quality index and in water bodies with the natural tone of purity. Increased use of anti-viral drugs along with herbal therapies has been observed at mass scale as global intervention to prevent the disease. The use of personal protective equipment and disinfection strategies for the control of pandemic has dramatically increased the pollution of plastic and medical waste. This article aims to forecast and highlight the evidence-based impact/changes (+ive and -ive) of coronavirus on the environment, global interventions to prevent the disease along with the levels of effectiveness of personal used protective equipment to stop the spread of coronavirus.
Keywords: Coronavirus, Environmental prospective, Global public intervention, Preventing disease, Viral diseases
1. Introduction
An ancient Greek writing around 400 BCE “Book of Epidemics” by Hippocrates accounts for winter epidemics of respiratory infectious diseases (Pappas et al., 2008). A number of viruses causing respiratory illnesses have been reported so far as the etiological agents of such epidemics. Virology and immunology embraced remarkable advances to expound the fundamental root of such cyclical infections. In spite of remarkable efforts put toward public health, epidemics/pandemics of viral respiratory system infections can prevail even amongst healthy human beings to lead to lethal consequences at worst (Fendrick, 2003). In the recent past (e.g., 2002–2003), the outbreaks of acute respiratory syndrome virus epidemics of SARS-CoV and current respiratory viral infection (SARS-C0V-2/COVID-19) were observed in winter season to evidence the blowout of a variety of respiratory tract viral infections (Li, 2020, Paules et al., 2020). Published reports revealed that seasonal factors in respiratory virus epidemics along with the host determinants affected by causative factors, including absolute humidity (AH), seasonal temperature variation, vitamin status, sunlight, and host behavior (Sloan et al., 2011, Peci, 2019, Moriyama et al., 2020). These determinants can be clustered as seasonal variation/changes in environmental conditions, behavioral pattern of human, and viral infection patterns. Environmental determinants impact on host predisposition by curbing air-pathways defensive response and viability, and spread of viruses. Factors of human behavior impact on transmission through contact rate between susceptible and infected bodies. Seasonality, temperature fluctuation, and humidity have been proposed as critical factors among all potential drivers to increase respiratory epidemics (Moriyama et al., 2020, Shoji et al., 2011).
A current respiratory viral infection of Corona Virus-2019 (COVID-19) was for the first time reported from Wuhan city, China in December 2019 where seafood market was declared culprit of this spread (Huang, 2020). Since the first report of COVID-19, it has been spreading rapidly to be reported from 216 countries and territories. As such, World Health Organization (WHO) has categorized COVID-19 as pandemic (WHO, 2020). WHO declared this pandemic as global emergency on 2020 January 30 due to continuous increase in reported/notified cases from many parts of the globe. The detection of COVID-19 cases is increasing day by day as tracked on WHO website and other media sources. China faced high morbidity and mortality rate in the month of February 2020, whereas boosted morbidity and mortality rate was reported from Italy and Spain in the month of March. The highest death and detection cases till April 2020 were reported from the United States of America, Spain, Italy, United Kingdom, France, Germany, and Belgium (Belgium bear rapid deaths) along with the boost of confirmed cases across the majority of global countries (WHO, 2020).
Corona viruses were first time studied in 1966 when Tyrell and Bynoe cultured them from a common cold patient (Kooraki, 2020). In light of projections and shells on outer surface with spherical virion morphology, they were named as coronavirus, whereas corona is a Latin word used to imply crown or wreath (Lexico. covid., 2020). Coronavirus is subdivided into four subfamilies (i.e., α-coronavirus, β-coronavirus, γ-coronavirus, and δ-coronavirus). Mammalians, especially bats were proposed as the sources responsible for α and β coronaviruses, while γ and δ coronaviruses are supposed to instigate from pig and birds, respectively (Amber Ather and Nikita, 2020). Alpha-coronavirus results asymptomatic or even mildly symptomatic infection while β coronavirus could cause severe infection and mortalities (Kucharski, 2020, Cao et al., 2020).
Since the pandemic started, the quality of different environmental segments (including atmosphere, water system, and wildlife freedom) has been reported to improve the deterioration of plastic and medical waste generations and susceptibility of coronavirus prevalence in sewage and fecal matters. Increased use of anti-viral drugs along with herbal therapies has been observed at mass scale as global intervention to prevent the disease (Kanniah, 2020, NASA, 2020, NASA, 2020, Aura, 2020, IQAir, 2020, Häder, 2020, Yunus et al., 2020, Clifford, 2020, ESA, 2020, Saadat et al., 2020, Corlett, 2020, Rutz, 2020, Diamant, 2020, Mandal and Pal, 2020, Thomson and Barclay, 2020). We aimed to organize a detailed study to forecastimmediate and long-term impact of COVID-19 on environment, global interventions to prevent the disease along with the levels of effectiveness of personal used protective equipment to stop the spread of coronavirus. It is expected that this study will help researchers gain a better knowledge for the assessment of various environmental changes and their corresponding implications. Further, we also highlighted some effective intervention activities that may help curve the spread of CVOID-19.
2. Global public intervention to prevent Covid-19
2.1. Research and effectiveness of anti-viral drugs against COVID-19
The COVID pandemic, infect people across the world and considered as a global medical risk to the public and healthcare workers. Being an emerging viral infection, there is no precise antiviral treatment or vaccine for COVID-19. Thus, it is urgently needed to develop a safe and stable coronavirus vaccine and scientific community is working in this field. The scientific community revealed that chloroquine and hydroxychloroquine are found to be effective anti-viral drugs against COVID-19 in-vivo and in laboratory studies, which has been stopped now due to its poor results (Rolain et al., 2007, WHO, 2020). A recent study by Wang and Su (2020) investigates the effectiveness of five FAD-approved drugs including ribavirin, penciclovir, nitazoxanide, nafamostat, chloroquine as well as two well-recognized broad-spectrum antiviral drugs remdesivir and favipiravir against 2019-nCoV. The study concluded that remdesivir and chloroquine were highly effective in the control of 2019-nCoV in vitro. Any vaccine operational against RNA viruses such as measles, polio, encephalitis B and influenza may perhaps be the most auspicious substitutes for SARS, an enveloped RNA virus (Lu, 2020, Liu, 2020). Thus, it will remain a prime area of research to develop vaccine to prevent and treat corona virus ailment (Chakraborty and Maity, 2020).
2.2. Effectiveness of indigenous herbal medicines
According to the available literature, 80% of the world’s population is dependent on herbal drugs (Sultana, 2012). In China, on the onset of disease rhizome of Scythian lamb or extract, compound have been testified for anti-SARS-Coronavirus-1 in Vero cells with SARS-Coronavirus-1 contagion model and reported to be effective against SARS (Chen, 2008, Hoever, 2005, Li, 2005, Wen, 2011).
In Pakistan, an exponential rise in consumption of Senna (Cassia angustifolia Vahl.) has been witnessed to treat and prevent covid-19 virus. Current reports have showed that Senna is not much effective against coronavirus disease due to that its consumption decreased exceptionally. However, the head of Infection Control Society of Pakistan stated that proliferating untested assertions related to senna use is harmful as it produces an incorrect sense of satisfaction (Tribune, 2020). There are some natural products such as baicalein and baicalin that are reported to act as inhibitors of SARS-CoV-2 (Su, 2020). However, there is no publication related to any herb, extract or bioactive compounds that may act against SARS-CoV-2 (Ding, 2017, Runfeng, 2020). SARS-CoV-2 is associated to cause hazardous and possibly lethal diseases through the respiratory route. Henceforth, investigating the effect of a specific bioactive compound against SAR-CoV-2 entails an extremely controlled laboratory with inward directional airflow (Biosafety level 3; BSL-3) (WHO, 2020, Wang and Su, 2020, Lu, 2020, Liu, 2020, Chakraborty and Maity, 2020, Sultana, 2012, Chen, 2008, Hoever, 2005, Li, 2005, Wen, 2011, Tribune, 2020, Su, 2020, Ding, 2017, Runfeng, 2020, Panyod et al., 2020) posing challenges for most researchers.
2.3. Declined consumption of bats, frogs and other wild animals
It is reported that coronavirus pandemic is likely to be initiated at Chinese wet markets. The ingestion of wild animals, especially wild mammals, supposed to be carriers of COVID 19 that can cross the species barrier, and pose a significant risk to human health (BBC, 2020). Bats and other wild animals serve to be the ecological reservoir of covid-19 and are responsible for transmission of this virus to humans while transmission through intermediary animal that may be domestic, wild or wild-domestic in nature is currently unidentified (WHO, 2020). In addition, pangolins are also found to be infected with SARS-CoV-2-related coronavirus. These pangolin coronavirus genomes contain 85.5% to 92.4% sequence correspondence to SARS-CoV-2. Hence, their part in the advent of human SARS-CoV-2 remains to be definite. Though the epidemiology, pathogenicity, interspecies infectivity and transmissibility of coronaviruses in pangolins and other wild animals is a subject of interest but the data presented here advises that handling of such animals entails substantial care and their dealing in wet markets must be stringently banned (Lam, 2020), thus be less consumed by the public (CRS, 2020).
2.4. Use of personal protective equipment
Coronavirus disease is primarily instigated by interaction or droplet spread attributed to comparatively out size respirational units which are matter of mobility for approximately 1 m from affected person (Murphy, 2020). It is reported that corona virus is predominately spread via contact (directly or via fomite); droplet transmission (coughing and sneezing by an infected person); aerosols (principally during intubation) and faeco-orally (CEBM, 2020) and (Ong, 2020) described that SARS-CoV-2 sustain longer than other artificially aerosolized respiratory viruses.
Personal protective equipment used as preventive action in hospital and household settings including eye protection, surgical or respirator masks, aprons or gowns, and gloves (Santarpia, 2020). Filtering face piece class 3 (FFP3) respirators, fluid-resistant (Type IIR) surgical masks (FRSM), particulate respirator Grade N95, powered air purifying respirator and elastomeric respirators are recommended to be used by patients, health care workers and general public. As a reduction measure of coronavirus spread and transmission from affected persons everyone need to use face protective (ECDC, 2020). It is recommended to discontinue the use of PPE if damaged, soiled, compromised, and uncomfortable or in other circumstances (CDC, 2020, Public-Health-England, 2020).
Table 1 demonstrates the WHO’s recommendations for the coherent utilization of personal protective equipment (PPE) in health care center and in houses, as well as all through the handling of cargo. Data related to shoe protective equipment is scarce in the context of any respiratory disease (CEBM, 2020). The chief threat of communication of respiratory viruses is in the course of AGPs (Aerosol Generating Procedures) of the respiratory tract, and use of improved respiratory shielding equipment is specified for health and social care workforces carrying out or supporting in such procedures. A long-sleeved one-use fluid repellent gown or disposable fluid repellent coveralls, a filtering face cover class 3 (FFP3) respirator, a full-face visor and gloves are suggested in the course of AGPs on potential and confirmed cases, irrespective of the clinical locale and thus used by public and healthcare workers as per needs (Public-Health-England, 2020).
Table 1.
WHO recommendations for the use of PPE.
| Personal Protective Equipment | Characteristics | Standards |
|---|---|---|
| Masks (Medical Health Worker) |
|
|
| Face Shield |
|
|
| Particulate Respirator, Grade N95 or FFP2 or higher |
|
|
2.5. Continuous sanitization at individual and mass levels
Cleaning along with disinfection is a finest practice to prevent COVID-19 and other viral respiratory illnesses in households and community settings (CDC, 2020). To lessen the threat of disease spread in the community, it is recommended to prioritize better hygiene practices including washing hands frequently and thoroughly (Güner et al., 2020). Individually, people are observed to be using alcohol based hand sanitizer with 60–70% alcohol as suggested by CDC (2020), regularly upon meeting other individuals outside or on return back to home (UNICEF, 2020) suggests that an untidy surface must be cleansed with soap or detergent with water followed by the use of disinfectant containing alcohol (70%) or bleach. Vinegar and other natural products are not suggested.
Public is also observed to be disinfected via spraying disinfecting substances in public places, such as super marts, offices, industrial units, massive gathering spots. However, (WHO, 2020) recommended to prohibit drenching of persons with antiseptics (as in tunnel, cabinet, or chamber) in any condition. This exercise is considered to be physically and psychologically damaging and is not effective to decrease a septic person’s capability to spread the virus through droplets or contact when speaking, coughing or sneezing. It is reported that spraying of individual with substances such as chlorine is responsible for the toxic influence on entities and lead towards eye and skin irritation, bronchospasm due to inhalation, and possibly gastrointestinal effects such as vomiting and nausea (Mahmood, 2020). It is suggested to use EPA-registered disinfectants with label by the employers to clean and disinfect environments potentially contaminated with SARS-CoV-2 (OSHA, 2020).
2.6. Smart lockdown strategy
Contrary to the earlier harsher lockdowns, which led the world economies to a grinding halt in different countries of Europe, now a number of countries are opting for smart or selective lockdowns (The News, 2020). The National Command and Operation Centre (NCOC) after undertaking a comprehensive review identified 20 cities in the country which are reporting large numbers of coronavirus cases. In Pakistan, the Federal Ministry on Health voiced legislators at a briefing that these targeted hotspots must be considered for limited locality-based lockdowns in the face of present economic situation. According to Government of Pakistan, a balance must be maintained between life and livelihood by adopting smart lockdowns and keeping businesses open, and implement strict SOPs that will be ensured through awareness and administrative actions (Al-Jazeera, 2020).
2.7. Limited mass gathering and social distancing
Social distance measures to duck the blowout of this virus is presented in Table 2 (Güner et al., 2020). Social distancing is aimed to decrease physical communications among peoples in a broad community (Wilder-Smith and Freedman, 2020). Working places are among high risk units for coronavirus spread. Many researches have supported the infectiousness of SARS-CoV-2 in the pre-symptomatic stage; thus social distancing is of serious significance in instituting control over the pandemic (Wei, 2020). Government of various countries have suspended all types of religious, cultural, social, scientific, sport, and political mass gathering events in different parts of the world. Thus, limiting mass gathering could be the prime preventive tactic for COVID-19 (Chakraborty and Maity, 2020).
Table 2.
Preventive and control measures adopted by community ().
| Quarantine | Other Measures |
|---|---|
| Voluntary quarantine (self‐quarantine) | Avoiding crowding |
Mandatory quarantine
|
Hand hygiene |
| Isolation | |
| Personal protective equipment | |
| School measures/closures | |
| Social distancing | |
| Workplace measures/closures |
Source:GÜNER et al., 2020
Considering the available studies, quarantine is the most effective measure adopted to control both the number of infected and dead individuals (Pan, 2020, Iwasaki and Grubaugh, 2020). It is seem to be effective where it was implemented since the outbreak.
3. Effectiveness of personal level prevention
3.1. Effectiveness on the basis of face mask types
Preventing a respiratory infection at origin by a face mask is an entrenched strategy (Esposito, 2020). Asymptomatic patients in large number unaware of their own infection (Day, 2020a, Day, 2020b), the analogous viral load in their upper respiratory tract (Zou, 2020), droplet and aerosol spreading during talking and breathing (Lewis, 2020), and protracted viral capability outside our body (Van Doremalen, 2020) strongly advocate use of face mask as a protective measure to control transmission of COVID 19 at source in mass gatherings and public places during the COVID-19 pandemic (Esposito, 2020).
To manufacture highly effective a tall degree of obedience is required that will maximize the influence of covers used by public (Esposito, 2020, Van Doremalen, 2020, BSI, 2020, Rosenstock, 1996). The W.H.O. recommended that unspoiled FFP2 or FFP3 with N-95 masks can be operated for up to 04 h, that is an average health-care worker’s lenience time (WHO, 2020, Murphy, 2020, Radonovich, 2009). Such intermediation is expected to be life-saving in various resource limited settings (Esposito, 2020).
3.2. Effectiveness on the basis of virus clearance
Coronavirus can transmit either via airborne aerosols or through contact with the contaminated surfaces such as keyboard, toys counter top, door knobs and others. Many studies conclude that SARS.CoV-2 remains intact on the surfaces of objects for hours and even days. It is recommended to clean the dirty surfaces should be cleaned by disinfectants to prevent the transmission and spreading of COVID-19 in humans through contaminated surfaces of objects and considered as best preventive action. For effective cleaning and disinfection of high touch surfaces especially common household objects by using EPA and WHO recommended disinfectant at least once a day. Virus clearance from the hands is also an important factor to be considered for effective control of virus spreading (CDC, 2020). It is recommend to use alcohol based hand sanitizer or frequent hand washing with soap (WHO, 2020b, Rabenau, 2005) conducted a study to investigate the efficiency of different hand sanitizers against SARS coronavirus. Eights disinfectants were investigated sterillium, based on 45% iso-propanol, 30% n-propanol and 0.2% mecetronium etilsulphate, SterilliumRub, based on 80% ethanol, SterilliumGel, based on 85% ethanol and SterilliumVirugard, based on 95% ethanol. The study concludes that SARS CoV was inactivated by all disinfectants.
It is reported that room ventilation is really effective against the clearance of COVID 19 aerosols. (Murphy, 2020) reported that a single air exchange removes about 63% of virus aerosols and after two fresh air exchange events there is 14% and after five exchanges there is only less than 1% of virus load remains there in the room. After number of air exchanges only 0.37n of virus load remains there. The evidences reveal that improved ventilation is associated with the removal of respiratory droplets from the air in a period of short time and helps to reduce the susceptibility of being ill with COVID-19 (CDC, 2020).
3.3. Prevention of cross infection
To control cross contamination of COVID, there is considerable focus on the use and proper disposal of personal protective equipment such as mask and gloves, excessive hand washing with WHO recommended alcohol based hand sanitizer or wash with soap and water for better personal hygiene, isolation if symptoms of COVID-19 appear, social distancing, retain distance of at least 1 m between yourself and other, frequent cleaning of contaminated surface by using disinfectants, in hospitals restrict the movement of people near or within the specific COVID-19 wards (Murphy, 2020, WHO, 2020a, WHO, 2020b). Effectiveness to reduce the risk of cross infection depends on the way we follow guidelines provided by different organizations including W.H.O., E.C.D.C. (European Centre for Disease Control) P.H. (Public Health) England, and E.S.I.C.M.S.C.C.M. (European Society of Intensive Care Medicine and Society of Critical Care Medicine). As it is considered that air is the main vehicle for the transmission of COVID-19 each organization states the preventive measures against transmission of virus through air. These airborne prevention includes, FFP2 or FFP3 mask, gogglesss, full sleeved fluid repellent gowns and gloves (Murphy, 2020). Social distancing and isolation can be effective to control and to reduce the risk of cross infection otherwise it became a cause of second peak in coronavirus pandemic (Laguipo, 2020).
4. Conclusions
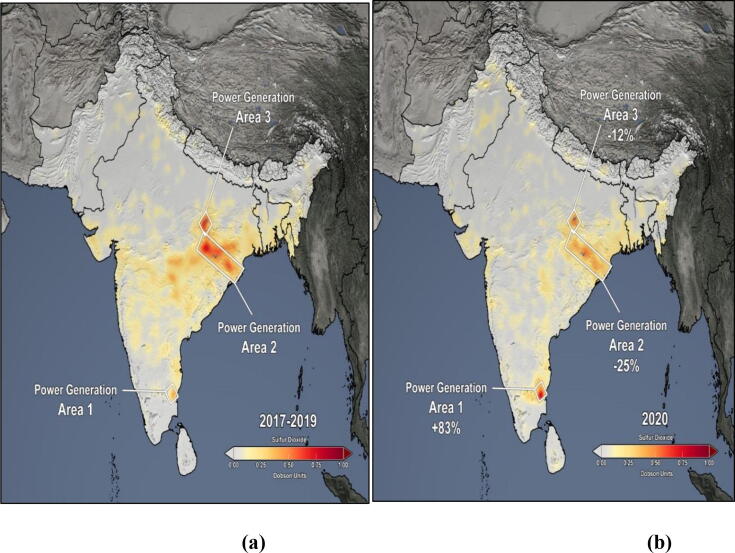
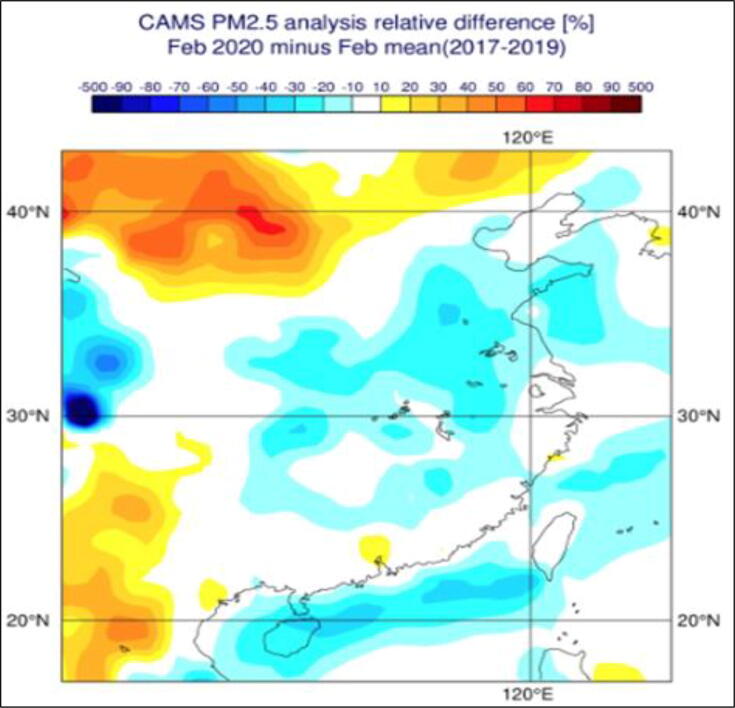
A manuscript on available reports of COVID-19 and its impact on environment along with forecasting and to highlight the impact on society and environment was aimed and compiled to ease the access of available information in one draft. Air Quality (NO2, SO2, PM2.5) and water bodies have been improved in term of pollution reduction (Fig. 1, Fig. 2). Global interventions to prevent the pandemic resulted in survival and freedom of wildlife. Personal protective equipment and disinfection strategy have resulted in increased plastic pollution and compromised human health. Cleaning staff, metropolitan sanitary workers and people who work at public places are at more risk for contamination by COVID-19 and other infectious diseases like hepatitis, influenza, AIDS etc., as masks can carry mucus and other body droplets from infected patient/person. Usage of anti-viral drugs with multiple herbal therapies has been reported to gain attention among different societies across the globe. It is important to note that all the herbal therapies are non-scientific therapies and W.H.O. is not in support of such practices.
Fig. 1.
Variation in SO2 concentration before and after COVID-19 pandemic (Source: Aura, 2020).
Fig. 2.
Map indicates percentiles difference of PM2.5 between 2020 and mean of 2017–19. (Source: ECMWF Copernicus Atmosphere Monitoring System, 2020).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The author extends her appreciation to the Deanship of Scientific Research at King Khalid University, Abha, Saudi Arabia for funding this work through research groups program under grant number R.G.P-2/135/42.
Footnotes
Peer review under responsibility of King Saud University.
References
- Al-Jazeera. Smart lockdown' in Pakistan to target 500 coronavirus hotspots. 2020; Available from: https://www.aljazeera.com/news/2020/06/lockdown-pakistan-target-500-coronavirus-hotspots-200623072202544.html.
- Amber Ather B., Nikita B. Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care. J. Endodontics. 2020;46(5) doi: 10.1016/j.joen.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aura. Reductions in Sulfur Dioxide & Nitrogen Dioxide Air Pollution over South Asia Associated with Efforts to Control the Spread of COVID-19. 2020; Available from: https://aura.gsfc.nasa.gov/science/feature-20200501.html.
- BBC. Coronavirus: Putting the spotlight on the global wildlife trade. 2020; Available from: https://www.bbc.com/news/science-environment-52125309.
- BSI. Personal Protective Equipment Standards. 2020; Available from: https://www.bsigroup.com/en-GB/topics/novel-coronavirus-covid-19/medical-devices-ppe/.
- Cao Y.-C., Deng Q.-X., Dai S.-X. Remdesivir for severe acute respiratory syndrome coronavirus 2 causing COVID-19: An evaluation of the evidence. Travel Med. Infect. Dis. 2020:101647. doi: 10.1016/j.tmaid.2020.101647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . Cleaning and Disinfection for Households; 2020. (a); Available from. [Google Scholar]
- CDC, 2020c. When and How to Wash Your Hands.
- CEBM, 2020. What is the evidence that COVID-19 personal protective equipment should include shoe covers?
- Chakraborty I., Maity P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total Environ. 2020:138882. doi: 10.1016/j.scitotenv.2020.138882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C.-J. Toona sinensis Roem tender leaf extract inhibits SARS coronavirus replication. J. Ethnopharmacol. 2008;120(1):108–111. doi: 10.1016/j.jep.2008.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford, C. The water in Venice, Italy's canals is running clear amid the COVID-19 lockdown — take a look. 2020. Available from: https://www.newsbreak.com/news/0OTLqTTy/the-water-in-venice-italys-canals-is-running-clear-amid-the-covid-19-lockdown-take-a-look.
- Corlett R.T. Impacts of the coronavirus pandemic on biodiversity conservation. Biol. Conserv. 2020;246:108571. doi: 10.1016/j.biocon.2020.108571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CRS. Wildlife Trade, COVID-19, and Other Zoonotic Diseases. 2020; Available from: https://crsreports.congress.gov/product/pdf/IF/IF11494.
- Day M. Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ: British Med. J. (Online) 2020;368 doi: 10.1136/bmj.m1165. [DOI] [PubMed] [Google Scholar]
- Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. British Med. J. Publ. Group. 2020 doi: 10.1136/bmj.m1375. [DOI] [PubMed] [Google Scholar]
- Diamant, E. People Staying Home, Wildlife Occupying the Streets: Lessons from COVID-19 Lockdowns. 2020; Available from: https://www.thenatureofcities.com/2020/04/22/people-staying-home-wildlife-occupying-the-streets-lessons-from-covid-19-lockdowns/.
- Ding Y. The Chinese prescription lianhuaqingwen capsule exerts anti-influenza activity through the inhibition of viral propagation and impacts immune function. BMC Compl. Alternat. Med. 2017;17(1):130. doi: 10.1186/s12906-017-1585-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC, 2020. Using face masks in the community reducing COVID-19 transmission from potentially asymptomatic or presymptomatic people through the use of face masks.
- ECMWF implements the Copernicus Atmosphere Monitoring Service (CAMS) on behalf of the European Union, 2020. Available from: https://www.ecmwf.int/en/about/what-we-do/environmental-services/copernicus-atmosphere-monitoring-service.
- ESA. European Space Agency (ESA). Deserted Venetian Lagoon. 2020 (a); Available from: https://www.esa.int/ESA_Multimedia/Images/2020/04/Deserted_Venetian_lagoon.
- Esposito S. Universal use of face masks for success against COVID-19: evidence and implications for prevention policies. Eur. Respir. J. 2020 doi: 10.1183/13993003.01260-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fendrick A.M. The economic burden of non–influenza-related viral respiratory tract infection in the United States. Arch. Intern. Med. 2003;163(4):487–494. doi: 10.1001/archinte.163.4.487. [DOI] [PubMed] [Google Scholar]
- Güner H.R., Hasanoğlu İ., Aktaş F. COVID-19: Prevention and control measures in community. Turkish J. Med. Sci. 2020;50(SI-1):571–577. doi: 10.3906/sag-2004-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Häder D.-P. Anthropogenic pollution of aquatic ecosystems: Emerging problems with global implications. Sci. Total Environ. 2020;713:136586. doi: 10.1016/j.scitotenv.2020.136586. [DOI] [PubMed] [Google Scholar]
- Hoever G. Antiviral Activity of Glycyrrhizic Acid Derivatives against SARS− Coronavirus. J. Med. Chem. 2005;48(4):1256–1259. doi: 10.1021/jm0493008. [DOI] [PubMed] [Google Scholar]
- Huang C. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IQAir. REPORT: COVID-19 impact on air quality in 10 major cities. 2020; Available from: https://www.iqair.com/blog/air-quality/report-impact-of-covid-19-on-global-air-quality-earth-day.
- Iwasaki A., Grubaugh N.D. Why does Japan have so few cases of COVID-19? EMBO Mol. Med. 2020;12(5):e12481. doi: 10.15252/emmm.202012481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanniah K.D. COVID-19's impact on the atmospheric environment in the Southeast Asia region. Sci. Total Environ. 2020:139658. doi: 10.1016/j.scitotenv.2020.139658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kooraki S. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J. Am. College Radiol. 2020 doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucharski A.J. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet. Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laguipo, A.B.B., 2020. How effective is social distancing in fighting COVID-19? Available from: https://www.news-medical.net/news/20200329/How-effective-is-social-distancing-in-fighting-COVID-19.aspx.
- Lam T.T.-Y. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature. 2020:1–4. doi: 10.1038/s41586-020-2169-0. [DOI] [PubMed] [Google Scholar]
- Lewis D. Is the coronavirus airborne? Experts can’t agree. Nature. 2020;580(7802):175. doi: 10.1038/d41586-020-00974-w. [DOI] [PubMed] [Google Scholar]
- Lexico. covid. 2020; dictionary]. Available from: https://www.lexico.com/search?filter=en_dictionary&query=corona.+04.
- Li S.-Y. Identification of natural compounds with antiviral activities against SARS-associated coronavirus. Antiviral Res. 2005;67(1):18–23. doi: 10.1016/j.antiviral.2005.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W. Learning from the past: possible urgent prevention and treatment options for severe acute respiratory infections caused by 2019-nCoV. ChemBioChem. 2020 doi: 10.1002/cbic.202000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H. Drug treatment options for the 2019-new coronavirus (2019-nCoV) Biosci. Trends. 2020;14(1):69–71. doi: 10.5582/bst.2020.01020. [DOI] [PubMed] [Google Scholar]
- Mahmood A. COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.140561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal I., Pal S. COVID-19 pandemic persuaded lockdown effects on environment over stone quarrying and crushing areas. Sci. Total Environ. 2020:139281. doi: 10.1016/j.scitotenv.2020.139281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Ann Rev. Virol. 2020;7 doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- Murphy J. Personal protective equipment during the COVID-19 pandemic: a comment. Anaesthesia. 2020 doi: 10.1111/anae.15145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NASA. NASA Satellite Data Show Air Pollution Decreases over Southwest U.S. Cities. 2020 (a); Available from: https://www.nasa.gov/feature/goddard/2020/nasa-satellite-data-show-air-pollution-decreases-over-southwest-us-cities/.
- NASA. NASA Reports Arctic Stratospheric Ozone Depletion Hit Record Low in March. 2020; Available from: https://www.nasa.gov/feature/goddard/2020/nasa-reports-arctic-stratospheric-ozone-depletion-hit-record-low-in-march/.
- Ong S.W.X. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OSHA. Covid-19, 2020. control and prevention. Available from: https://www.osha.gov/SLTC/covid-19/controlprevention.html.
- Pan A. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. Jama. 2020;323(19):1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panyod S., Ho C.-T., Sheen L.-Y. Dietary therapy and herbal medicine for COVID-19 prevention: A review and perspective. J. Tradit. Compl. Med. 2020 doi: 10.1016/j.jtcme.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappas G., Kiriaze I.J., Falagas M.E. Insights into infectious disease in the era of Hippocrates. Int. J. Infect. Dis. 2008;12(4):347–350. doi: 10.1016/j.ijid.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Paules C.I., Marston H.D., Fauci A.S. Coronavirus infections—more than just the common cold. JAMA. 2020;323(8):707–708. doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- Peci A. Effects of absolute humidity, relative humidity, temperature, and wind speed on influenza activity in Toronto, Ontario, Canada. Appl. Environ. Microbial. 2019;85(6) doi: 10.1128/AEM.02426-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public-Health-England. COVID-19: infection prevention and control guidance. 2020; Available from: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control.
- Rabenau H. Efficacy of various disinfectants against SARS coronavirus. J. Hosp. Infect. 2005;61(2):107–111. doi: 10.1016/j.jhin.2004.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radonovich L.J. Respirator tolerance in health care workers. JAMA. 2009;301(1):36–38. doi: 10.1001/jama.2008.894. [DOI] [PubMed] [Google Scholar]
- Rolain J.-M., Colson P., Raoult D. Recycling of chloroquine and its hydroxyl analogue to face bacterial, fungal and viral infections in the 21st century. Int. J. Antimicrob. Agents. 2007;30(4):297–308. doi: 10.1016/j.ijantimicag.2007.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock, L., 1996. NIOSH Guide to the selection and use of particulate respirators certified under 42 CFR 84. DHHS (NIOSH) Pub No. 96–101.
- Runfeng L. Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2) Pharmacol. Res. 2020:104761. doi: 10.1016/j.phrs.2020.104761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutz C. COVID-19 lockdown allows researchers to quantify the effects of human activity on wildlife. Nat. Ecol. Evol. 2020:1–4. doi: 10.1038/s41559-020-1237-z. [DOI] [PubMed] [Google Scholar]
- Saadat S., Rawtani D., Hussain C.M. Environmental perspective of COVID-19. Sci. Total Environ. 2020:138870. doi: 10.1016/j.scitotenv.2020.138870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santarpia, J.L., et al., , 2020. Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska Medical Center. medRxiv.
- Shoji M., Katayama K., Sano K. Absolute humidity as a deterministic factor affecting seasonal influenza epidemics in Japan. Tohoku J. Expe. Med. 2011;224(4):251–256. doi: 10.1620/tjem.224.251. [DOI] [PubMed] [Google Scholar]
- Sloan C., Moore M.L., Hartert T. Impact of pollution, climate, and sociodemographic factors on spatiotemporal dynamics of seasonal respiratory viruses. Clin. Transl. Sci. 2011;4(1):48–54. doi: 10.1111/j.1752-8062.2010.00257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su H. Discovery of baicalin and baicalein as novel, natural product inhibitors of SARS-CoV-2 3CL protease in vitro. bioRxiv. 2020 [Google Scholar]
- Sultana S. Authentication of herbal drug Senna (Cassia angustifolia Vahl.): A village pharmacy for Indo-Pak Subcontinent. Afric. J. Pharm. Pharmacol. 2012;6(30):2299–2308. [Google Scholar]
- Thomson D.J., Barclay D.R. Real-time observations of the impact of COVID-19 on underwater noise. J. Acoustical Soc. Am. 2020;147(5):3390–3396. doi: 10.1121/10.0001271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tribune, 2020. Tribune Fact Check: Sana Makki — a cure for Covid-19? Available from: https://tribune.com.pk/story/2234073/1-tribune-fact-check-sana-makki-cure-covid-19.
- UNICEF, 2020. Cleaning and hygiene tips to help keep the COVID-19 virus out of your home 2020; Available from: https://www.unicef.org/coronavirus/cleaning-and-hygiene-tips-help-keep-coronavirus-covid-19-out-your-home#cleaning-home.
- Van Doremalen N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Su M. A preliminary assessment of the impact of COVID-19 on environment–A case study of China. Sci. Total Environ. 2020:138915. doi: 10.1016/j.scitotenv.2020.138915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei W.E. Presymptomatic Transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. Morb. Mortal. Wkly Rep. 2020;69(14):411. doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen C.-C. Traditional Chinese medicine herbal extracts of Cibotium barometz, Gentiana scabra, Dioscorea batatas, Cassia tora, and Taxillus chinensis inhibit SARS-CoV replication. J. Tradit. Compl. Med. 2011;1(1):41–50. doi: 10.1016/S2225-4110(16)30055-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Personal protective equipment for COVID 19. 2020 (c); Available from: https://www.who.int/medical_devices/priority/COVID_19_PPE/en/.
- WHO, 2020d. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19). Available from: https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV IPCPPE_use2020.2-eng.pdf?sequence=1&isAllowed=y.
- WHO, Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance, 28 January 2020. 2020 (a), World Health Organization.
- WHO, 2020b. WHO recommendations to reduce risk of transmission of emerging pathogens from animals to humans in live animal markets or animal product markets.
- WHO, 2020d. Laboratory Biosafety Guidance Related to the Novel Coronavirus (2019-nCOV). Available from: https://www.who.int/publications/i/item/laboratory-biosafety-guidance-related-to-coronavirus-disease-(covid-19).
- Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 2020;27(2):taaa020. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yunus A.P., Masago Y., Hijioka Y. COVID-19 and surface water quality: Improved lake water quality during the lockdown. Sci. Total Environ. 2020:139012. doi: 10.1016/j.scitotenv.2020.139012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]