Abstract
Background
Iodine deficiency disorder is one of the major hidden hunger for poverty-stricken coastal rural areas of Bangladesh. Despite various programs, including universal salt iodization, IDD is significantly persistent due to poverty, inadequate knowledge, poor attitude, and practice of iodized salt consumption. The present study aimed to determine iodine concentration in salt at the household level as well as the magnitude of knowledge, attitude, and practice related to iodized salt utilization and iodine deficiency disorders (IDDs).
Material and method
A population-based cross-sectional study was carried out using multistage sampling among 400 households in four coastal districts in Bangladesh. A standard pretested questionnaire was used to determine the knowledge, attitude, and practice towards iodized salt consumption. The iodine level was measured using the gold standard iodometric titration technique in the collected salt samples from the selected households.
Result
The study results revealed that almost half of the participants had good knowledge regarding a balanced diet, whereas the positive attitude and practice of balanced diet consumption was relatively low (only 16.2% and 11.3%, respectively). The respondents' education profile and age were strongly correlated with knowledge and attitude; however, the practice was not significantly correlated with age and education. The concentration of iodine in salt at household levels was strongly associated with the practice of using iodized salt. Use of adequate iodized salt was 2.838 times (OR: 2.838, 95% CI: 1.7–4.735) and 3.884 times (OR: 3.884, 95%CI: 2.029–7.433) more likely to have a positive attitude and good practice towards iodized salt and IDDs respectively.
Conclusion
Proper knowledge about iodized salt and IDDs should be introduced to all public education premises levels. Interventions and programs can be formulated to enhance knowledge, attitude, and practice at the household level so that the consumption of adequate iodized salt can be ensured to reduce iodine deficiency problems.
Keywords: Iodine, Salts, Knowledge, Attitudes, Practice, Goiter
Iodine; Salts; Knowledge; Attitudes; Practice; Goiter
1. Introduction
The proper amount of iodine is needed in the human diet to ensure good health and regulate physical growth and neural development [1]. Humans require iodine to sustain their regular metabolism, physical growth, and cognitive development. Psychological growth disorders (cretinism, dwarfism), goiter, muscular dystrophy, spontaneous miscarriages, and hypothyroidism may occur due to inadequate intake or storage of iodine. Nearly all of these cases are found among newborn children due to iodine deficiency in their mothers during pregnancy [2, 3].
Mild to moderate iodine deficiency disorders (IDDs) remains a substantial public health crisis, particularly in the least developed and developing countries. However, a significant reduction in the prevalence of IDDs has been achieved worldwide by implementing universal salt iodization programs, other food fortifications, and the use of dietary supplements [4]. Iodine deficiency is one of the world's most common causes of mental delays. Every year, in developing countries, almost 38 million newborns suffer from the enduring impacts of neurological disorders associated with IDDs [5]. The mean Intellectual Quotient (IQ) scores are reduced to 13.5 due to iodine deficiency [6]. IDD is one of the major micronutrient deficiencies in Bangladesh. The prevalence of iodine deficiency varies from districts to districts, and the proportion of the population of school-age children with inadequate iodine (UIC<100μg/l) at the national level was 40.0 %. The proportion of the population with severe, moderate, and mild deficiency of iodine was 5.6%, 13.0%, and 21.4%, respectively [7].
Universal salt iodination program is an effective measure to maintain the iodine status, with the recommended threshold for household level is between 20 to 40 ppm depending on typical use and availability of iodine from other dietary sources. Adequate iodized salt in more than 90 percent of households represents iodine deficiency elimination [8]. Households with low economic status have a higher tendency to consume under-iodized salt [9].
The Bangladesh Government has set its requirements for adequate salt iodination rates at the production site at 45–50 ppm, at retail sites at 20 ppm, and in households at 15 ppm [10]. After initiation in 1989, the salt iodination program of Bangladesh started to address IDDs by improving iodized salt utilization, proper monitoring of iodized salt production and storage [11]. Despite this program, a recent study in Bangladesh found that among 18 iodinated salts commonly found in the Bangladesh market, 17% of the sample contained less than the recommended level of iodine [12].
Only the presence of iodine in salt is not enough for preventing IDDs. Proper utilization of iodized salt is necessary as iodine can be lost due to different types of cooking practices such as pressure cooking, boiling, deep-frying, and shallow frying [13]. Nearly 69% of the Bangladeshi population has an iodine deficiency. The iodized salt campaign brought remarkable improvement in reducing goiter and cretinism. However, assessing the knowledge, attitude, and practice regarding iodized salt consumption has not been done yet in all parts of the country to maximize its utilization. It is crucial to assess knowledge, attitude, and practice about utilizing iodized salt, its consumption, and iodine deficiency disorder such as goiter and cretinism as consumption of iodized salt is associated with them. However, few studies were done to determine the utilization of iodized salt at national and regional household levels. Once we could identify the reason behind not using iodized salt or loss of iodine due to malpractice in rural households, it will help us maximize the use of iodized salt in mass people and play a role in reducing the incidence of goiter and cretinism. Therefore, this study aimed to determine iodine concentration in salt at household levels, knowledge, attitude, and practice (KAP) related to iodized salt and IDDs and the effects of KAP on the utilization of iodized salt. The findings of this study will open new doors for future research in this field.
2. Material and Method
2.1. Study design and settings
It was a population-based cross-sectional study. Face-to-face interviews were carried out using a standard questionnaire in the local language (the English version of the questionnaire is attached as “KAP Questionnaire on iodized salt”). Android-based Kobo Collect (version 1.23.3k) software was used for data collection purposes.
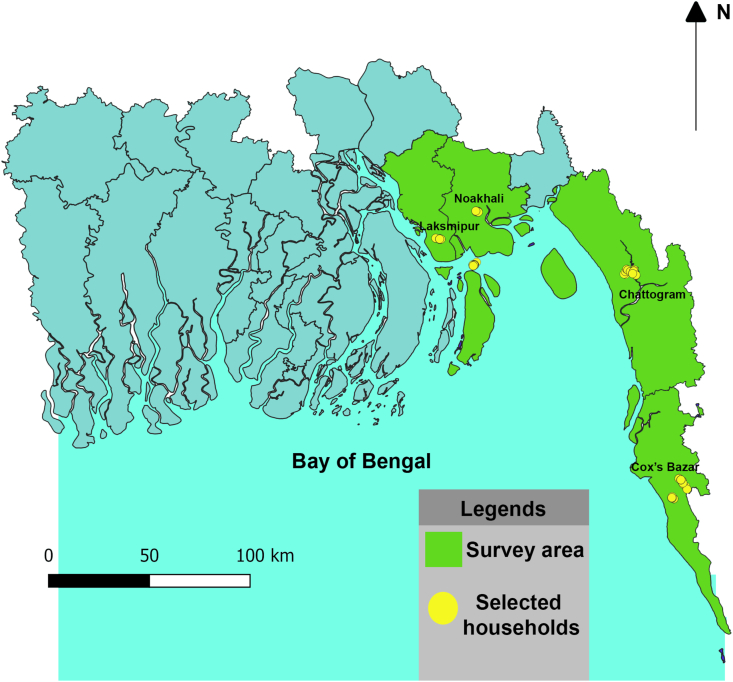
The green shaded areas represent the survey area, and yellow circles indicate the sample households.
2.2. Sample size and sampling procedure
At first, we selected four districts out of the nineteen coastal districts by convenient sampling (Figure 1). Then, participants were selected employing a simple random sampling technique.
Figure 1.
Map of the coastal regions of Bangladesh.
The sample size was computed using the following formulae,
Sample size, ; where n is the smallest sample size to be achieved; p is the expected prevalence using iodized salt at household level = 0.25; q is the rate of not using iodized salt at household level = 0.75; e is the marginal error = 0.05; Z is a statistic for a confidence level of 95% = 1.96. The sample size calculation required 289 samples, including a 10% non-response rate; the sample size was 318 households. However, we collected information from 400 households from different districts by a multistage with a three-stage sampling technique. In the first stage, four districts from the southeastern region of Bangladesh were selected randomly. In stages 2, both urban and rural areas were selected, and in the final stage, households were selected following systematic random sampling.
2.3. Inclusion criteria
Respondents who were 18 years old or above and were involved in cooking were included in the study. Written informed consent was obtained from each participant prior to the interview. Mainly the women are responsible for cooking, and if the women were absent or not responsible for cooking, then we collected our data from the person who was responsible for cooking during the study period. Respondents who have declined consent or incapable of interacting properly during data collection were excluded from the study.
2.4. Variable and scores
A structured questionnaire was formulated for data collection. A pilot survey was carried out in a nearby location of the study sites to standardize the questionnaire. The pilot study gave us the validity of our questionnaire, and after the pilot study, we have changed it according to the respondent's responses to each question and their understanding of the questions that we have asked during the pilot study. The reliability of the questionnaire was measured using Cronbach's alpha (α) test, and it was 0.72.
In the questionnaire, there were 14 questions for knowledge about iodized salt, five questions for attitude regarding iodized salt, and six questions for their practices about using iodized salt in cooking and preserving. All the KAP questions were are set to think about cooking and preserving iodized salt.
Scores on iodized salt knowledge and practice ranged from 0-1. When the respondent could not tell about iodized salt and did not practice using iodized salt, ‘0’ was assigned as a score. If their response was ‘No’, the score was ‘0’, while if they answer ‘Yes’ and ‘practice’, the score was ‘1’. Scores on attitude were according to the Likert scale stated in positive question with score ‘4’ for strongly agree, Score ‘3’ for agreeing, score ‘2’ for disagree, and score 1 for “strongly disagree”, while for negative questions were scored 4 for “strongly disagree”, score ‘3’ for disagree, score ‘2’ for agreeing, and score ‘1’ for strongly agree. KAP categorization was used as follows: 6.80th, 50th, and 87.24th, from lowest to highest percentile as per the profiles from the cluster analysis [14].
After the interview session, approximately 15 g (three teaspoons) of table salt was collected from each household for further analysis. This sample was taken from the salt used for cooking purposes. The samples were collected in a moisture-free, clean plastic bag from the top, middle, and bottom of the respondent's container. The sampling date, respondent's name, and house number were labeled in the sample collection bag. Gold standard iodometric titration technique was used to measure the iodine concentration of collected salt at household levels [8]. The concentration of iodine in salt was categorized into adequate (≥15ppm), inadequate (≥5ppm), and no iodized salt (0ppm) [15].
2.5. Statistical analysis
From KoBoCollectv1.27.3k software, the data were first entered into Microsoft Excel, and then data were transferred and analyzed using Statistical Package for Social Sciences (SPSS) Version 23.0. The data were analyzed for percentages, mean, standard deviation for continuous variables, and frequency measured for the categorical variables. Chi-square test was employed to assess the degree of correlation between dependent (good, moderate, and poor KAP) and independent variables (religion, educational status, and iodine concentration). Multinomial regression analysis was performed to determine independent association after preliminary analysis to find out odds ratios. Odds ratios (OR) were calculated to determine the strength of associations of the independent variables with the outcome variable at a 95% Confidence interval (CI). The level of significance for all statistical tests was set at 0.05.
2.6. Ethics approval
The ethical approval was obtained from the institutional ethics committee of the Noakhali Science and Technology University.
3. Result
3.1. Socio-demographic and other characteristics of household respondent
From this study, it was found that only 6.4% of participant's educational levels were certified or above. Most of the households were Muslim (76.6%) in this study (Table 1). The percentage of good, moderate, and poor knowledge scores regarding iodized salt among households were 46.3, 35.3, and 18.5, respectively. Among 400 respondents, only 16.2% had a positive attitude score on using iodized salt, and the rest of them had an indifferent (41.0%) and negative attitude (42.8%). While talking about the practice, it was found that 71.7% of households had a moderate practice score (Table 2).
Table 1.
Frequency distribution of demographic characteristics (n = 400).
| Demographic Characteristics | ||||||
|---|---|---|---|---|---|---|
| Characteristics | Frequency | Percentage | Mean difference | p-value | 95% Confidence Interval |
|
| Lower | Upper | |||||
|
Age | ||||||
| 18–29 Years | 158 | 39.5 | 1.818 | 0.000 | 1.74 | 1.89 |
| 30–44 Years | 157 | 39.3 | ||||
| ≥44 Years | 85 | 21.2 | ||||
|
Educational Status | ||||||
| No formal education | 117 | 29.3 | 2.113 | 0.000 | 2.02 | 2.20 |
| Elementary | 145 | 36.3 | ||||
| High School | 112 | 28.0 | ||||
| Certified and above | 25 | 6.4 | ||||
|
Religion | ||||||
| Muslim | 306 | 76.6 | 1.278 | 0.000 | 1.22 | 1.33 |
| Hindu | 75 | 18.8 | ||||
| Christian | 18 | 4.6 | ||||
Table 2.
Frequency distribution of KAP status (n = 400).
| KAP Status | Frequency | Percentage | Mean difference | p-value | 95% Confidence Interval |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
|
Knowledge Score | ||||||
| Good | 185 | 46.2 | 5.725 | 0.000 | 5.4071 | 6.0429 |
| Moderate | 141 | 35.3 | ||||
| Poor | 74 | 18.5 | ||||
|
Attitude Score | ||||||
| Negative | 171 | 42.8 | 5.717 | 0.000 | 5.2441 | 6.1909 |
| Indifferent | 164 | 41.0 | ||||
| Positive | 65 | 16.2 | ||||
|
Practice Score | ||||||
| Good | 45 | 11.3 | 3.880 | 0.000 | 3.7513 | 4.0087 |
| Moderate | 287 | 71.7 | ||||
| Poor | 68 | 17.0 | ||||
3.2. The concentration of iodine in the salt collected from households
The iodometric titration technique was employed to determine the iodine content in the salt samples. The iodometric titration technique showed that 317 (79.2%) salt samples had no iodine (0ppm) in the salt, 36 (9.0%) had an inadequate level of iodine (1.1–14.8ppm), and only 47 (11.8%) had an adequate amount of iodine in the household salts.
3.3. Correlation of knowledge, attitude, and practice with iodine concentration and other variables
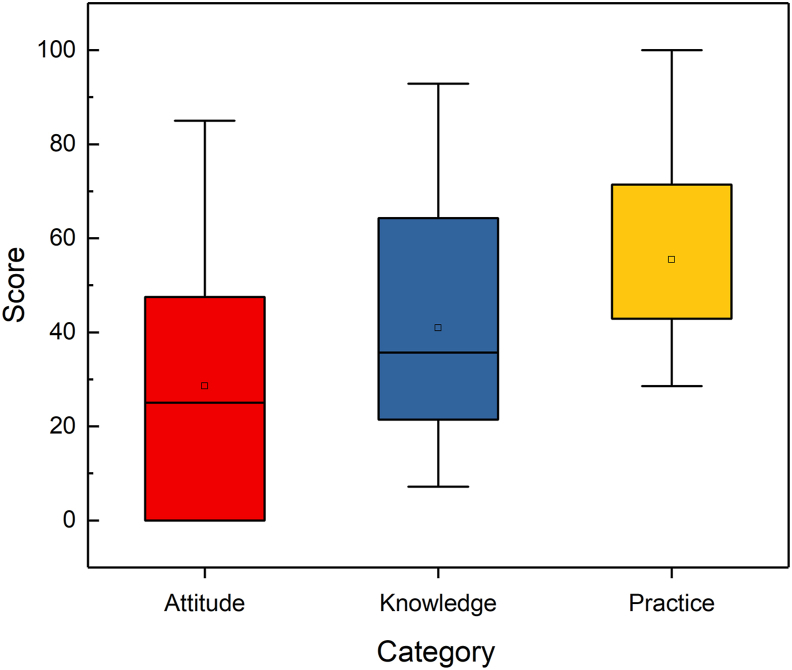
A Chi-square test was performed to see the correlation of knowledge, attitude, and practice with iodine concentration and other variables. There was a statistically significant correlation between knowledge and attitude with the educational status of the respondent (p < 0.05), and there was no correlation between the education of respondents with practice (p > 0.05). The respondents' age showed a strong correlation with knowledge, attitude, and practice (p < 0.05). The respondent's knowledge score strongly correlated with the attitude score but not correlated with the practice score (P > 0.05). There was no correlation between attitude and practice score (P > 0.05). The percentage of using non-iodized salt was higher (81.1%) among good knowledge scored people, which was not significant (P > 0.05). The percentage of using iodized salt was lower (21.5%) among those who had a positive attitude, and it was significant (P < 0.05). It was found from the study that the practice of using iodized salt was much lower among good-practiced scored people (Table 3). Box plots of the Knowledge and attitude category showed that the knowledge and attitude (Mean ± SD) score (40.8923.10, 31.7626.75 respectively) was lower, indicating that most households had moderate knowledge attitude on iodized salt consumption. Nevertheless, the practice (Mean ± SD) score (55.4218.70) was higher than the knowledge and attitude score, which indicated that most households had a good practice on iodized salt consumption (Figure 2).
Table 3.
Correlation between KAP with other characteristics of respondents and iodine concentration in salt.
| Characteristics | Knowledge Score |
Attitude Score |
Practice Score |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Good (%) | Moderate (%) | Poor (%) | X2 p-value |
Positive (%) | Indifferent (%) | Negative (%) | X2 p-value |
Good (%) | Moderate (%) | Poor (%) | X2 p-value |
|
|
Education | ||||||||||||
| No formal education | 65 (55.6) | 46 (39.3) | 6 (5.1) | 72.353 | 4 (3.4) | 44 (37.6) | 69 (59.0) | 66.099 | 12 (10.3) | 87 (74.4) | 18 (15.4) | 9.146 |
| Elementary | 75 (51.7) | 51 (35.2) | 19 (13.1) | 0.000 | 17 (11.7) | 61 (42.1) | 67 (46.2) | 0.000 | 29 (20.0) | 99 (68.3) | 17 (11.7) | 0.166 |
| High School | 42 (37.5) | 39 (34.8) | 31 (27.7) | 30 (26.8) | 51 (45.5) | 31 (27.7) | 20 (17.9) | 83 (74.1) | 9 (8.0) | |||
| Certified and above | 2 (8.0) | 5 (20.0) | 18 (72.0) | 14 (56.0) | 8 (32.0) | 3 (12.0) | 6 (24.0) | 18 (72.0) | 1 (4.0) | |||
|
Age | ||||||||||||
| 18–29 Years | 62 (39.2) | 50 (31.6) | 46 (29.1) | 21.422 | 38 (35.4) | 64 (40.5) | 38 (24.1) | 15.510 | 18 (11.4) | 102 (64.6) | 38 (24.1) | 11.851 |
| 30–44 Years | 78 (49.7) | 57 (36.3) | 22 (14.0) | 0.000 | 69 (43.9) | 68 (43.3) | 20 (12.8) | 0.004 | 19 (12.1) | 115 (73.2) | 23 (14.6) | 0.018 |
| ≥44 Years | 45 (52.9) | 34 (40.0) | 6 (7.1) | 46 (54.2) | 32 (37.6) | 7 (8.2) | 8 (9.4) | 70 (82.4) | 7 (8.2) | |||
|
Knowledge | ||||||||||||
| Good | 12 (6.5) | 52 (28.1) | 121 (65.4) | 35 (18.9) | 131 (70.8) | 19 (10.3) | ||||||
| Moderate | 19 (13.5) | 76 (53.9) | 46 (32.6) | 115.69 | 18 (12.8) | 102 (72.3) | 21 (14.9) | 5.548 | ||||
| Poor | 34 (45.9) | 36 (48.6) | 4 (5.5) | 0.000 | 15 (20.3) | 54 (73.0) | 5 (6.8) | 0.236 | ||||
|
Attitude | ||||||||||||
| Negative | 36 (21.1) | 114 (66.7) | 21 (12.3) | 4.476 | ||||||||
| Indifferent | 22 (13.4) | 124 (75.6) | 18 (11.0) | 0.345 | ||||||||
| Positive | 10 (15.4) | 49 (75.4) | 6 (9.2) | |||||||||
|
Iodine concentration | ||||||||||||
| Adequate | 17 (9.2) | 19 (13.5) | 11 (14.9) | 2.555 | 14 (21.5) | 25 (15.2) | 8 (4.7) | 17.697 | 2 (4.4) | 28 (9.8) | 17 (25.0) | 19.521 |
| Inadequate | 18 (9.7) | 11 (7.8) | 7 (9.5) | 0.635 | 7 (10.8) | 11 (6.8) | 18 (10.5) | 0.001 | 1 (2.2) | 27 (9.4) | 8 (11.8) | 0.001 |
| No iodized | 150 (81.1) | 111 (78.7) | 56 (75.7) | 56 (75.7) | 128 (78.0) | 145 (84.8) | 42 (93.3) | 232 (80.8) | 43 (63.2) | |||
Figure 2.
Distribution of the scores of knowledge, attitudes, and practices. The box plots indicate the minimum, the maximum, and the 25th, 50th, and 75th percentiles.
3.4. Factors affecting adequate iodized salt consumption
Both univariate and multivariate logistic regression analyses were used to examine the association of variables (knowledge, attitude, and practice) with iodine concentration in used salt. In univariate analysis, practice (OR 3.184; 95% CI: 1.752–5.786) and attitude (OR 2.295; 95% CI: 1.50–3.513) were significantly associated with adequately iodized salt, and only practice (OR 2.042; 95%CI: 1.048–3.981) was significantly associated with inadequately iodized salt. In multivariate analysis, both attitude and practice showed statistically significant association with adequately iodized salt, and practice was significantly associated with inadequately iodized salt (OR 2.056; 95% CI: 1.050–4.025) (Table 4).
Table 4.
Univariate and Multivariate analysis of knowledge, attitude, and practice associated with iodine concentration.
| Iodine content category | Univariate |
Multivariate |
|||
|---|---|---|---|---|---|
| OR (95%CI) | p-value | OR (95% CI) | p-value | ||
| Inadequately iodized | Attitude | 1.027 (0.630–1.674) | 0.916 | 1.103 (0.619–1.965) | 0.739 |
| Knowledge | 0.984 (0.620–1.561) | 0.945 | 0.953 (0.556–1.633) | 0.860 | |
| Practice | 2.042 (1.048–3.981) | 0.036 | 2.056 (1.050–4.025) | 0.035 | |
| Adequately iodized | Attitude | 2.295 (1.500–3.513) | 0.000 | 2.838 (1.700–4.735) | 0.000 |
| Knowledge | 1.332 (0.897–1.976) | 0.155 | 0.795 (0.497–1.270) | 0.593 | |
| Practice | 3.184 (1.752–5.786) | 0.000 | 3.884 (2.029–7.433) | 0.000 | |
"No iodized salt" was set as the reference category, level of significance at 5%.
4. Discussion
This study aimed to assess knowledge, attitude, and practice regarding iodized salt and iodine deficiency, factors affecting adequately iodized salt utilization, and iodine concentration in salt collected from households. Although the prevalence of goiter and iodine deficiency has been reduced due to 10 years of universal iodized intervention initiated in the mid-90s in Bangladesh, iodine deficiency disorders are still persistent due to improper utilization of iodized salt [16]. Our result presented that only 11.8% of the households in Bangladesh's selected coastal areas had access to sufficiently iodized salt, which is considerably smaller than the WHO recommended level of 90% of households [17]. This percentage was also significantly lower when comparing with studies from other countries like India and South Africa, where the percentage of iodized salt utilization was 65% and 63%, respectively [6, 9]. The percentage of access to adequately iodized salt within the present study was dissimilar to the report of the National Micronutrients status Survey (2011–12), Bangladesh [7], wherever it indicated that 80.3% family used iodized salt, and among those, only 57.6% of the households used adequate quantity of iodized salt.
The current study found that 46.3% had good knowledge about iodine and iodine-related deficiency and knew the importance of iodized salt. The percentage of poor knowledge among respondents was not much satisfied (18.5%), which was divergent to a study where 59.3% had a sound idea about the beneficiary effects of iodized salt, and 41.1% had a proper understanding of the pernicious effects of iodine deficiencies [18]. Only about 40% of respondents of this study knew the importance of iodized salt, and 71% knew its' role in goiter prevention. On further inquiry on iodine deficiency, 0.5% of respondents replied that iodine deficiency might cause neurological disorders, and 1.25% had reported hampered immunity; however, the different results were obtained from other studies that do not correspond with the findings of the present study [19, 20]. While identifying the factors correlated with knowledge and iodine concentration of respondents, it was found that over 80% of the study population consumed non-iodized salt though they had adequate knowledge about iodized salt. Surprisingly it was found that the percentage of using iodized salt was higher among those who had moderate knowledge about iodine and iodized salt, which was not significantly correlated and was not similar to the findings reported by Roy et al. [21], where it was indicated that type of salt used by people was affected by their knowledge. In the case of regression analysis to know about the associated factors of knowledge, it was found that educational status and attitude score were significantly associated with knowledge score (p < 0.01). However, age was not statistically significant (p > 0.05), which was similar to a study conducted in southeast Ethiopia where researchers said that the knowledge of respondents reduced with low educational status determined by binary logistic regression [22].
In our study, the percentage of positive attitude was lower (16.2%) than the percentage of respondents being indifferent (41%) and having negative (42.8%) attitudes. Among them, 41.7% reported positive attitudes in utilizing iodized salt for their health benefits, which were better than findings from some other studies where only 18.9% [19] and 13.3% [23] reported that iodized salt is good for health. In a study conducted in Sindh and Punjab, participants reported that using iodized salt is better for physical growth and prevents goiter and other health problems [24], similar to our study where 31.5% agreed that iodized salt utilization could prevent goiter. In another study, 58.2% of the respondents opined that iodized salt should be consumed [25]. Few studies reported unavailability (52.2%), high cost (12%), and taste as the primary reasons for not using iodized salt [21, 26, 27] not much similar to our study as 27.3% of respondents did not use iodized salt as it is a bit expensive. In the present study, it was also found that the attitude of respondents was significantly correlated with age, educational status, and knowledge of respondents, which was similar to Karmakar et al., where the value of chi-square and p-value for education and age were X2 = 17.337, p = 0.000, and X2 = 7.772, p = 0.005 respectively [19].
In our study, only 11.3% of respondents were reported to have good practice, and 71.7% had moderate practice scores, which indicated that iodine deficiency could be a significant problem in the future. However, it showed a slight contrast to Karmakar et al., where 83.3% had a good practice, and 16.7% had inappropriate practice regarding the use of iodized salt [19]. A significant inverse relationship was found between iodized salt consumption and the prevalence of iodine deficiency in another study [28]. In this study, 65% of respondents utilized packed salt, and 27.7% of respondents used unpacked salt. Dissimilar findings were found in some other studies [21, 26, 29]. The current study also revealed that 14.25% of the respondents identified a salt type, whether it is iodized or not, by seeing the label in the packet, only 4% identified by hearing the name of the brand, and the rest of them did not respond to anything. The majority (67.5%) of them stored salt for less than two-months; almost similar to Karmakar et al., where 76% of women stored salt for less than one month [19]. Nevertheless, dissimilar to Dida et al. as in his study, almost all people (93%) preserved salt for less than sixty days [22].
The current study described that educational status was statistically associated with the respondents' practice regarding iodized salt utilization. However, there was no significant association found between respondents' practice and respondents' age and attitude. The odds of practice stated that the practice of respondents was higher among those certified or well-educated. It was similar to another study in which their findings showed that participants with secondary and tertiary education were double and 17 times more likely to consume iodized salt than the illiterate counterpart [18]. The practice of the respondents was strongly correlated with the adequate presence of iodine in salt; similar to studies of Roy et al. where findings indicated that type of salt used were significantly correlated with appropriate practice, and Gerensea's study demonstrated that proper utilization of iodized salt is much affected by the practice of using it in different households [21, 30].
A significant proportion of the population not using iodized salt were doing so because of concerns about its use. The foremost common reasons for not using iodized salt in the household were accessibility and price. Each of these barriers could be removed if all edible salts were adequately iodized. This implies that it might not be an effective use of funds to focus future communication messages on addressing what seems to be only a perceived prevalence of misconceptions regarding the adverse effects of iodized salt.
However, this study has some limitations. This study was carried out in only four districts, and these findings may not be generalized to national levels. Furthermore, the lack of knowledge on the household members' iodine status is typically assessed using urinary iodine concentrations. This effect was ignored during the sample size calculation, and the cross-sectional study design restricts the factors to establish a causal relationship.
5. Conclusion
Still, an enormous percent of rural people in Bangladesh's coastal area consume inadequately iodized or non-iodized in their daily food. Additionally, non-iodized salts are frequently produced and retailed in local marketplaces as properly iodized salt for human consumption. They contain an inadequate iodine level that does not facilitate anyone to meet up their daily iodine needs. Therefore, the general population should be informed of the importance of iodized salt and its correct handling. Effective use of media for disseminating health education programs in addition to regular visits by public health workers should be undertaken to sustain and expand the utilization of iodized salt at the household level. The current study may also play a role in improving national policy and could help in the modification of current policy, such as the enforcement of salt iodization by monitoring the market, the access to iodized salt by mass people, as well as implementation of effective strategies for better education and communication regarding this issue to prevent IDDs throughout the country. It is crucial to place KAP within this context in order to consider the influence of factors as the ease of access to iodized salt (availability, price, etc.). KAP is a crucial element to healthy dietary choices, as the use of iodized salt, but a successful salt iodization policy depends on policy implementation to create and sustain healthier food environments and protect the population. Hence, bolstering efforts to enhance public awareness on the practice and attitude towards iodized salt is crucial to boost the availability and accessibility of iodized salt.
Declarations
Author contribution statement
Mohammad Asadul Habib, Mohammad Rahanur Alam: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Susmita Ghosh, Tanjina Rahman, Sompa Reza, Sumaiya Mamun: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Health, F.M.o. Federal Ministry of Health, Family Health Department Addis Ababa, Ethiopia; 2010. National Guideline for Control and Prevention of Micronutrient Deficiencies. [Google Scholar]
- 2.Association, AT, American Thyroid Association Task Force on Thyroid and Pregnancy Iodine needs in the pregnant and postpartum women. www.thyroid.org/thyroid-physiciansprofessionals0education-research/pregnancy-and-hypothyroidism/Becks Available at:
- 3.Verma M., Raghuvanshi R.S. Dietary iodine intake and prevalence of iodine deficiency disorders in adults. J. Nutr. Environ. Med. 2001;11(3):175–180. [Google Scholar]
- 4.Zimmermann M.B., Andersson M. Update on iodine status worldwide. Curr. Opin. Endocrinol. Diabetes Obes. 2012;19(5):382–387. doi: 10.1097/MED.0b013e328357271a. [DOI] [PubMed] [Google Scholar]
- 5.Zimmermann M.B. Thyroid size and goiter prevalence after introduction of iodized salt: a 5-y prospective study in schoolchildren in Cote d'Ivoire. Am. J. Clin. Nutr. 2003;77(3):663–667. doi: 10.1093/ajcn/77.3.663. [DOI] [PubMed] [Google Scholar]
- 6.Bhat S.L. Harvard University; 2009. Element of Survival: Isolating the Causal Effect of Access to Iodized Salt on Child Health in India. [Google Scholar]
- 7.UNICEF, B . Vol. 16. Institute of Public Health and Nutrition; 2013. National Micronutrients Status Survey; p. 2018. Accessed August. [Google Scholar]
- 8.Organization, WH . 2007. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: a Guide for Programme Managers. [Google Scholar]
- 9.Jooste P.L., Weight M.J., Lombard C.J. Iodine concentration in household salt in South Africa. Bull. World Health Organ. 2001;79:534–540. [PMC free article] [PubMed] [Google Scholar]
- 10.Gazette B. Google Scholar; Bangladesh: 1994. Iodine Deficiency Disease Prevention regulation. Government of the Peoples Republic of Bangladesh; pp. 5261–5270. [Google Scholar]
- 11.De Benoist B. World Health Organization; Geneva: 2004. Iodine Status Worldwide: WHO Global Database on Iodine Deficiency. [Google Scholar]
- 12.Prodhan U. Measurement of iodine availability and stability of some iodized salts in Bangladesh. Int. J. Res. Eng. Technol. 2014;3:470–474. [Google Scholar]
- 13.Sikdar K.Y.K. Estimation of loss of iodine from edible iodized salt during cooking of various Bangladeshi food preparations. Dhaka Univ. J. Pharm. Sci. 2016;15(2):161–165. [Google Scholar]
- 14.Higuera-Mendieta D.R. KAP surveys and dengue control in Colombia: disentangling the effect of sociodemographic factors using multiple correspondence analysis. PLoS Neglected Trop. Dis. 2016;10(9) doi: 10.1371/journal.pntd.0005016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alam M.R. Determination of iodine content of commercially available table salts at the retailer level in selected areas of Bangladesh. Eur. J. Nutr. Food Saf. 2019:284–288. [Google Scholar]
- 16.Organization W.H. 2014. Guideline: Fortification of Food-Grade Salt with Iodine for the Prevention and Control of Iodine Deficiency Disorders; p. 45. Geneva. [PubMed] [Google Scholar]
- 17.WHO U. World Health Organization; Geneva: 2007. ICCIDD. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination. A Guide for Programme Managers; pp. 1–94. [Google Scholar]
- 18.Sarah N.A. Knowledge on iodized salt use and iodine content of salt among households in the Hohoe municipality, Volta region-Ghana. Afr. J. Public Health. 2016;2(1):1–10. [Google Scholar]
- 19.Karmakar N. knowledge, attitude, and practice regarding household consumption of iodized salt among rural women of Tripura, India: a mixed-methods study. J. Educ. Health Promot. 2019;8 doi: 10.4103/jehp.jehp_248_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar P., Tiwari V., Gautam R. Knowledge, attitude and behaviour regarding use of iodised salt: an evaluation of national iodine deficiency disorders control programme in India. OIDA Int. J. Sustain. Dev. 2013;5(12):95–106. [Google Scholar]
- 21.Roy R. Household use of iodized salt in rural area. J. Fam. Med. Prim. Care. 2016;5(1):77. doi: 10.4103/2249-4863.184628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dida N. Availability of adequately iodised salt at household level and its associated factors in Robe town, Bale Zone, South East Ethiopia: community-based cross-sectional study. S. Afr. J. Clin. Nutr. 2018:1–6. [Google Scholar]
- 23.Gebreegziabher T., Stoecker B. Knowledge, attitudes, and practices of rural women from Sidama zone, southern Ethiopia concerning iodized salt, iodine and goiter (804.19) FASEB J. 2014;28(1_supplement):804–819. [Google Scholar]
- 24.Khan G.N. A study on the household use of iodised salt in Sindh and Punjab provinces, Pakistan: implications for policy makers. J. Pharm. Nutr. Sci. 2012;2(2):148–154. [Google Scholar]
- 25.Sen T.K. Limited access to iodized salt among the poor and disadvantaged in North 24 Parganas district of West Bengal, India. J. Health Popul. Nutr. 2010;28(4):369. doi: 10.3329/jhpn.v28i4.6043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Banumathi P. KAP study on iodized salt usage among household level in Tirunelveli District, Tamil Nadu. Natl. J. Res. Community Med. 2016;5:145–148. [Google Scholar]
- 27.Gidey B. Availability of adequate iodized salt at household level and associated factors in rural communities in Laelay Maychew District, Northern Ethiopia: a cross sectional study. J. Nutr. Health Sci. 2015;2(1):1. [Google Scholar]
- 28.Yusuf H.K. Iodine deficiency disorders in Bangladesh, 2004-05: ten years of iodized salt intervention brings remarkable achievement in lowering goitre and iodine deficiency among children and women. Asia Pac. J. Clin. Nutr. 2008;17(4) [PubMed] [Google Scholar]
- 29.Lowe N. Increasing awareness and use of iodised salt in a marginalised community setting in North-West Pakistan. Nutrients. 2015;7(11):9672–9682. doi: 10.3390/nu7115490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gerensea H. knowledge, attitude and practice (KAP) towards iodized salt utilization in HaweltiKebelle, Axum, Tigray, Ethiopia, 2015. Edorium J. Nutr. Diet. 2016;2:1–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.