Abstract
Background
With the increasing number of patients undergoing arthroscopic rotator cuff repair (ARCR), postoperative pain control in these patients has become an important issue. We investigated and compared post-operative pain relief with intravenous acetaminophen (IA) and interscalene brachial plexus block (IBPB) after ARCR.
Methods
This prospective study involved 66 consecutive patients who underwent ARCR in 2019–2020 at our hospital. Overall, 23 and 43 shoulders were assigned to the IA and IBPB groups, respectively. We evaluated the visual analog scale (VAS) pain scores at rest, during activity, and at night for the first 72 h postoperatively. We compared the results statistically between the groups. A p-value <0.05 was considered statistically significant.
Results
VAS scores for night pain in the IBPB group were significantly lower than those in the IA group for the first 24 h postoperatively (p = 0.017). In contrast, the same scores were significantly lower in the IA group than in the IBPB group at 72 h postoperatively (p = 0.024). Other scores were not significantly different between the groups.
Conclusions
IBPB provides superior night pain control during the first 24 h postoperatively, and IA provides superior night pain control at 72 h postoperatively. However, there were no significant differences in other pain scores between the two groups.
Keywords: Arthroscopic rotator cuff repair, Postoperative pain control, Intravenous acetaminophen, Interscalene brachial plexus block
1. Introduction
The number of patients undergoing arthroscopic rotator cuff repair (ARCR) has been increasing, and postoperative pain control is considered challenging in these patients.1 Although a minimally invasive procedure, ARCR is particularly associated with considerable pain during the early postoperative period1,2; specifically, patients who undergo ARCR develop severe pain at 2–3 days postoperatively.3, 4, 5 However, sufficient postoperative pain control could help to reduce the length of hospital stay and may improve patients’ satisfaction and functional recovery.1 Multiple postoperative pain control modalities are used to manage pain among patients undergoing ARCR at shoulder surgery centers; they include oral or intravenous medications, a single local analgesic injection, continuous interscalene block, regional nerve blocks, periarticular multimodal drug injection (PMDI), and intravenous patient-controlled analgesia (IV PCA).2, 3, 4, 5, 6, 7, 8 In particular, the interscalene nerve block is being widely accepted for shoulder surgeries because of its effectiveness to control postoperative pain1, 2, 3, 4. Additionally, it reduces the use of narcotics and provides good analgesia in patients who undergo shoulder surgeries.1, 2, 3, 4
In contrast, the use of intravenous acetaminophen has become popular as one of the components of multimodal pain management.9,10 A prospective randomized controlled trial has demonstrated that repeated doses of 1 g intravenous acetaminophen administered over 24 h is safe and efficacious for managing pain10. To the best of our knowledge, no study has compared the clinical outcomes between intravenous acetaminophen and interscalene brachial plexus block for pain relief within 72 h after ARCR. Therefore, this study aimed to compare the efficacy of intravenous acetaminophen and interscalene brachial plexus block for postoperative pain relief during the first 72 h in patients undergoing ARCR. We hypothesized that the postoperative pain control of intravenous acetaminophen is comparable to that of interscalene brachial plexus block.
2. Materials and methods
2.1. Study participants
This prospective study involved 66 consecutive patients who underwent ARCR at our hospital and provided informed consent to participate in this institutional review board-approved study between April 2019 and January 2020. There were 66 patients randomly allocated to the two groups: 23 patients were categorized into the intravenous acetaminophen (IA) group and 43 patients into the interscalene brachial plexus block (IBPB) group, respectively. Tear size of the rotator cuff was evaluated by MRI. We measured the longitudinal and transverse dimensions of the tear on the preoperative MRI along the oblique coronal plane and oblique sagittal plane respectively.11 Tear size was categorized as small (<1 cm), medium (1–3 cm), large (3–5 cm), or massive (>5 cm), according to Cofield.12 Patients with either IA or IBPB after ARCR and those who underwent ARCR performed by a single surgeon were included in this study. Patients who underwent ARCR in combination with other procedures, who received different peri-operative pain control measures, and who required revision surgery following ARCR were excluded.
We evaluated the visual analog scale (VAS) for pain at rest, during activity, and at night for the first 72 h (at 24, 48, and 72 h) postoperatively. VAS was measured on a scale ranging from 0 (no pain) to 10 (worst imaginable pain). We statistically compared the results between the groups.
Additional patient data and characteristics were also recorded including sex, age, body mass index, size of rotator cuff tear, and procedure of long head of biceps (Table 1).
Table 1.
Patient demographics and clinical characteristics. There were no significant differences in other parameters. Values are presented as mean ± standard deviation or number of cases.
| Variables | IA group (n = 23) | IBPB group (n = 43) | p value |
|---|---|---|---|
| Male/Female | 9/14 | 20/23 | 0.611 |
| Age (years) | 61.6 ± 10.1 | 63.6 ± 9.3 | 0.209 |
| BMI (kg/m2) | 23.8 ± 4.6 | 24.4 ± 3.1 | 0.280 |
| Size of rotator cuff tear | |||
| small | 4 | 13 | 0.562 |
| medium | 14 | 25 | 0.913 |
| large | 4 | 5 | 0.714 |
| massive | 1 | 0 | 0.358 |
| Procedure of LHB | |||
| tenotomy | 11 | 20 | 0.951 |
| tenodesis | 1 | 3 | 0.687 |
| nothing | 11 | 20 | 0.951 |
| Pre-operative VAS | |||
| at rest | 1.8 ± 1.5 | 1.2 ± 1.4 | 0.116 |
| during activity | 5.0 ± 2.1 | 5.3 ± 2.1 | 0.339 |
| at night | 4.9 ± 2.2 | 5.1 ± 2.6 | 0.343 |
BMI: Body Mass Index.
LHB: Long Head of Biceps.
VAS: Visual Analog Scale.
2.2. Interventions
Patients in the IA group received 1 g acetaminophen intravenously every 6 h for 24 h postoperatively. This repeated dose regimen was chosen based on previously published trials that confirmed its safety and efficacy.10
Patients in the IBPB group received the block from a single skilled anesthesiologist under general anesthesia. Interscalene trunks were identified between the anterior and middle scalene muscles. After local anesthesia was administered to the skin with 1% lidocaine, the 50-mm 18-gauge insulated block needle (Contiplex® Tuohy, B. Braun Medical, Bethlehem, PA) was advanced from the lateral to the medial muscles so as to place the needle tip in the region between the upper and middle trunks (C5–C6) of the brachial plexus. The catheter was then advanced until it passed the needle tip, and the needle was withdrawn. 0.75% ropivacaine (20 ml) and 0.5% bupivacaine (10 ml) was administered to the brachial plexus nerve sheath. During insertion of the needle into the interscalene brachial plexus, real-time monitoring with ultrasonographic imaging was performed to facilitate accurate local anesthesia deposition. General anesthesia was administered to all patients; propofol, fentanyl were used in anesthesia induction, and sevoflurane was used in anesthesia maintenance.
Every patients in both group were administered 200 mg of a cyclo-oxygenase (COX)-2 inhibitor and a tablet containing a combination of 37.5 mg of tramadol and 325 mg of acetaminophen in the night until one postoperative week. Patients were also given oral medication (loxoprofen (60 mg)) as needed for severe pain.
2.3. Surgical technique
All surgical procedures were performed consistently under general anesthesia by a single skilled surgeon, with the patients assuming a beach chair position. Arthroscopy was performed through the posterior portal. The entire hypertrophic synovial tissue was cleaned up under visualization. The contracted capsular structures in the rotator interval regions were debrided. Suture anchors were used for standard ARCR. Repair of all rotator cuff tears was performed using the Healix Transtend™ Implant System (Healix BR; Depuy-Synthes Co., Raynham, MA, USA) loaded with 3 high-strength sutures (Versalok Anchor; Depuy-Synthes Co.). The number of anchors used depended on the tear size and repair configuration for suture-bridge repair. The patients underwent a tenotomy or tenodesis for lesions of the long head of the biceps.
The same postoperative protocol was used in both the IA and IBPB groups. An abduction brace was used to immobilize the shoulders for 4 weeks. On the day after the surgery, the patients began performing isometric rotator cuff exercises, passive exercises for forward flexion, and relaxation of the muscles around the shoulder girdle; this was followed by active and active-assisted exercises after the immobilization period. Six weeks postoperatively, the patients began performing exercises to strengthen the rotator cuff and scapular stabilizers. A physical therapist provided rehabilitation for more than 3 months. All patients required at least 6 months to fully resume sports or heavy physical labor.
2.4. Statistical analysis
Unpaired t-tests were used to compare the differences in the VAS scores between the groups at 24, 48, and 72 h postoperatively. Fisher's exact test was used for categorial variables. A p-value<0.05 was considered statistically significant. All the analyses were conducted using SPSS® v25.0 (IBM Inc., Armonk, NY, USA).
3. Results
The basic demographic characteristics of the patients are summarized in Table 1. The demographic data were not significantly different between the two groups.
The VAS scores for night pain in the IBPB group were significantly lower than those in the IA group for the first 24 h postoperatively (8.6 ± 1.6 vs. 7.1 ± 2.9, respectively, p = 0.017). In contrast, the VAS scores for night pain in the IA group were significantly lower than those in the IBPB group at 72 h postoperatively (3.3 ± 2.5 vs. 4.6 ± 2.5, respectively, p = 0.024). Other scores were not significantly different between the two groups (Fig. 1, Fig. 2, Fig. 3, Fig. 4).
Fig. 1.

The VAS scores were not different between the groups at preoperatively.
Fig. 2.
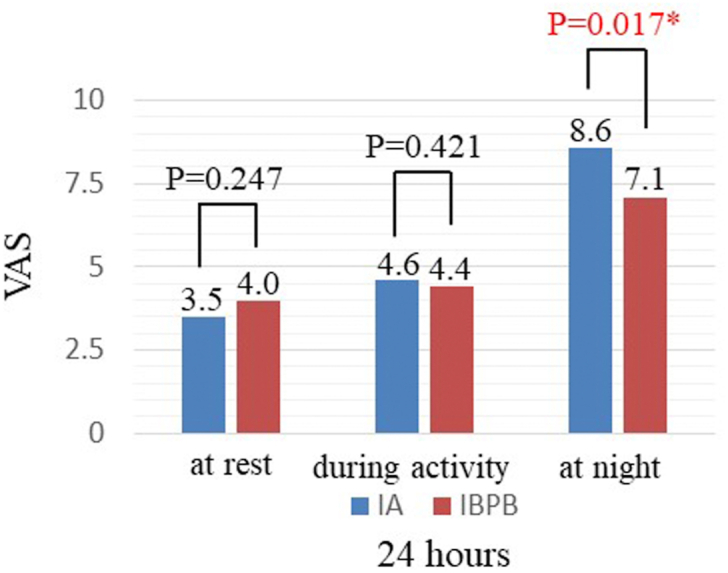
The VAS scores for night pain in the IBPB group were significantly lower than those in the IA group for the first 24 h postoperatively (8.6 ± 1.6 vs. 7.1 ± 2.9, respectively, p = 0.017).
Fig. 3.
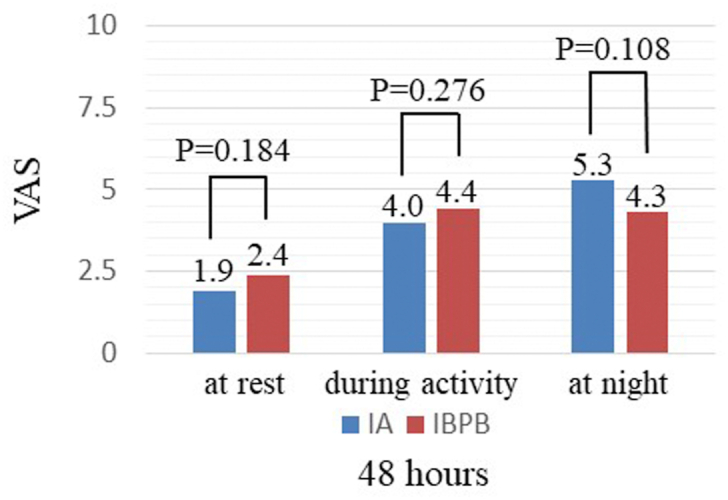
The VAS scores were not different between the groups at 48 h postoperatively.
Fig. 4.
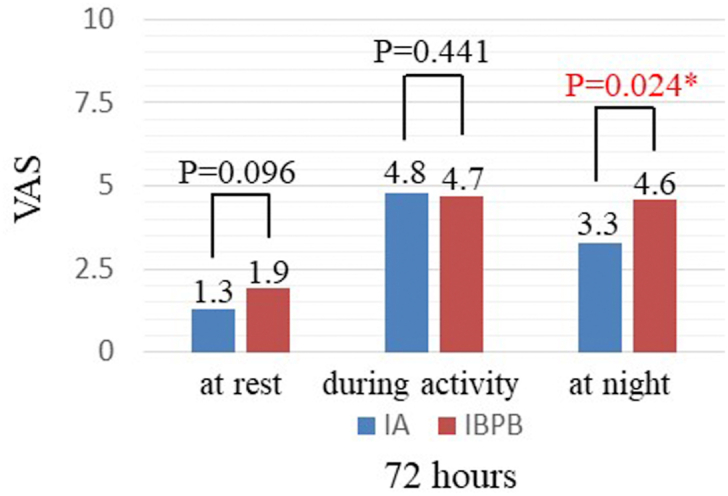
The VAS scores for night pain in the IA group were significantly lower than those in the IBPB group at 72 h postoperatively (3.3 ± 2.5 vs. 4.6 ± 2.5, respectively, p = 0.024).
4. Discussion
IBPB provided superior night pain control at 24 h following ARCR, whereas IA provided superior night pain control at 72 h postoperatively. To our knowledge, this is the first study to compare the effectiveness of postoperative pain control between IA and IBPB in patients who underwent ARCR. Studies have investigated the use of multiple approaches for postoperative pain control following ARCR, including local analgesic injection, continuous interscalene block, regional nerve block, PMDI, and IV PCA.2, 3, 4, 5, 6, 7, 8 However, a standard postoperative pain control strategy remains to be formulated, and such approaches have potential risks, limitations, and adverse effects.8,13,14
Several studies have reported satisfactory outcomes for postoperative pain control with PMDI.15,16 Parvataneni et al. reported that local periarticular injection of multimodal drugs plays the most important role in multimodal pain control.17 Moreover, Vendittoli et al. demonstrated favorable outcomes with a local injection to directly block the injured or stretched nerves or soft tissues.18 In contrast, Toyooka et al. reported that PMDI is inferior to continuous interscalene brachial plexus block (CISBPB) for early postoperative analgesia following ARCR.8 In their study, patients who received either PMDI or CISBPB following ARCR were evaluated based on their VAS scores at 3, 6, 12, 24, and 48 h postoperatively. Both treatment groups also received fentanyl by intravenous patient-controlled analgesia (IV-PCA). Toyooka et al. concluded that patients in the CISBPB group experienced a significantly better postoperative analgesia during the first 6 h, and total fentanyl consumption by IV-PCA during the first 8 postoperative hours was significantly greater in the PMDI group than in the CISBPB group.
There is no uniform consensus on the use of non-steroidal anti-inflammatory drugs (NSAIDs) or steroids as intraoperative local injections for pain relief. NSAIDs are presumed to effectively reduce pain and inflammation; therefore, they are commonly prescribed after orthopedic surgical procedures, with minimal requirement of narcotics. However, one study found that traditional NSAIDs, as well as a COX-2 inhibitor, might impair the tendon-to-bone healing process.19 Steroid injections are reported to diminish the mechanical properties of the tendons, potentially contributing to a higher rate of re-rupture following rotator cuff repair surgeries.20
The use of interscalene nerve block for shoulder surgeries has gained popularity due to its efficacy in controlling postoperative pain1,.21, 22, 23 Multiple studies have shown that it provides excellent pain relief, thereby reducing the need for narcotics use in patients undergoing shoulder surgeries. Ultrasound-guided injections enable the precise and targeted administration of drugs, further contributing to improved analgesia.24 The interscalene brachial plexus bolus blockade (IBPBB), which blocks the brachial plexus, including the sensory and motor innervations of the entire upper extremity, can effectively manage postoperative pain following ARCR.24
Interscalene nerve block can be administered as a single bolus injection at the brachial plexus or as continuous indwelling catheter infusion.1,23 Several recent studies have reported the benefits of both IBPBB and continuous indwelling catheter infusion for shoulder surgeries.1,3,25,26 Abdallah et al. showed that the analgesic effect of IBPBB lasts up to 8 h after a shoulder procedure.25 Fredrickson et al. reported that interscalene infusion of analgesics reduces pain within the first 2 days after a minor arthroscopic shoulder surgery, although no data were available for the first 24 h postoperatively26; the patients enrolled in Fredrickson et al.’s study underwent minor arthroscopic shoulder surgeries, such as acromioplasty, excision lateral clavicle, and labral repair, and not conventional rotator cuff repair surgery. Salviz et al. compared the recovery profiles of patients who received a single interscalene injection with those who received continuous interscalene brachial plexus block and general anesthesia following ARCR.3 The mean VAS scores were lower on postoperative days 1 and 2 in the continuous interscalene brachial plexus block group than in the single interscalene injection and general anesthesia group. Moreover, the requirement for narcotics for the first 3 days postoperatively was less in the former group than in the latter. Kim et al. performed a randomized controlled study to evaluate the clinical outcomes of IBPBB and patient-controlled interscalene indwelling catheter analgesia (PCIA) for relieving pain within 48 h after ARCR.1 The patients enrolled in their study were randomized into three groups according to the postoperative analgesia method: IBPBB, PCIA, and control. Their study results revealed that the VAS scores for the first 2 h postoperatively were significantly lower in the IBPBB group than in the PCIA and control groups. However, the VAS scores in the IBPBB group were significantly higher at 12 and 24 h postoperatively than those in the PCIA group. No significant difference was observed in the VAS scores at 48 h postoperatively between the three groups. The analgesic approach was the only factor that affected the VAS scores at 24 h postoperatively. Moreover, a 2–4% incidence of complications has been reported, including brachial plexus injuries and complications related to the respiratory, central nervous, and cardiovascular systems.27 Additionally, catheter placement is a more time- and labor-intensive process than a single bolus injection of a nerve block. A previous study reported that the average time required for catheter placement was 30–40 min as compared to 5–7 min required for a single bolus injection of a nerve block.23
Intravenous acetaminophen is widely used as one component of multimodal therapy for pain management.9,10 A prospective, randomized, controlled trial reported that multiple doses of intravenous acetaminophen (1 g) for 24 h was safe and effective for pain control after orthopedic surgery.10 Philip et al.9 reported that intravenous acetaminophen was effective for pain control following total joint arthroplasty; they concluded that intravenous acetaminophen significantly reduced not only the postoperative VAS scores but also the requirement for opioids within the first 24 h after primary total knee arthroplasty.
In our study, although VAS scores for night pain in the IBPB group were significantly lower than those in the IA group for the first 24 h postoperatively and the scores in the IA group were significantly lower than those in the IBPB group at 72 h postoperatively, other scores were not significantly different between the groups. Therefore, IA may be almost equivalent to IBPB in terms of pain control in the first 72 h postoperatively following ARCR.
There are several limitations to our study. First, the sample size was small, and it contained unequal numbers of patients in each group. Second, we did not evaluate or compare the two groups in terms of the size of rotator cuff tear. Third, we did not evaluate the long-term differences in the functional outcomes between the groups.
In conclusion, intravenous acetaminophen demonstrated effective postoperative pain control that was comparable to that of interscalene brachial plexus block. However, achieving adequate pain control within the first 72 h after a surgery remains challenging. More effective and safer pain control approaches are required.
Disclosure statement
No specific grant from funding agencies in the public, private, or not-for-profit sectors were received in this study.
Acknowledgements
None.
References
- 1.Kim J.H., Koh H.J., Kim D.K. Interscalene brachial plexus bolus block versus patient-controlled interscalene indwelling catheter analgesia for the first 48 hours after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2018 Jul;27(7):1243–1250. doi: 10.1016/j.jse.2018.02.048. [DOI] [PubMed] [Google Scholar]
- 2.Oh J.H., Kim W.S., Kim J.Y., Gong H.S., Rhee K.Y. Continuous intralesional infusion combined with interscalene block was effective for postoperative analgesia after arthroscopic shoulder surgery. J Shoulder Elbow Surg. 2007 May-Jun;16(3):295–299. doi: 10.1016/j.jse.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 3.Salviz E.A., Xu D., Frulla A. Continuous interscalene block in patients having outpatient rotator cuff repair surgery: a prospective randomized trial. Anesth Analg. 2013 Dec;117(6):1485–1492. doi: 10.1213/01.ane.0000436607.40643.0a. [DOI] [PubMed] [Google Scholar]
- 4.Trompeter A., Camilleri G., Narang K., Hauf W., Venn R. Analgesia requirements after interscalene block for shoulder arthroscopy: the 5 days following surgery. Arch Orthop Trauma Surg. 2010 Mar;130(3):417–421. doi: 10.1007/s00402-009-0959-9. [DOI] [PubMed] [Google Scholar]
- 5.Cho N.S., Ha J.H., Rhee Y.G. Patient-controlled analgesia after arthroscopic rotator cuff repair: subacromial catheter versus intravenous injection. Am J Sports Med. 2007 Jan;35(1):75–79. doi: 10.1177/0363546506291632. [DOI] [PubMed] [Google Scholar]
- 6.Ruiz-Suarez M., Barber F.A. Postoperative pain control after shoulder arthroscopy. Orthopedics. 2008 Nov;31(11):1130. doi: 10.3928/01477447-20081101-25. [DOI] [PubMed] [Google Scholar]
- 7.Sinatra R.S., Torres J., Bustos A.M. Pain management after major orthopaedic surgery: current strategies and new concepts. J Am Acad Orthop Surg. 2002 Mar-Apr;10(2):117–129. doi: 10.5435/00124635-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Toyooka S., Ito M., Kakinuma A. Periarticular multimodal drug injection does not improves early postoperative analgesia compared with continuous interscalene brachial plexus block after arthroscopic rotator cuff repair: a retrospective single-center comparative study. J Orthop Sci : official journal of the Japanese Orthopaedic Association. 2019 May;29 doi: 10.1016/j.jos.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Huang P.S., Gleason S.M., Shah J.A., Buros A.F., Hoffman D.A. Efficacy of intravenous acetaminophen for postoperative analgesia in primary total knee arthroplasty. J Arthroplasty. 2018 Apr;33(4):1052–1056. doi: 10.1016/j.arth.2017.10.054. [DOI] [PubMed] [Google Scholar]
- 10.Sinatra R.S., Jahr J.S., Reynolds L.W., Viscusi E.R., Groudine S.B., Payen-Champenois C. Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology. 2005 Apr;102(4):822–831. doi: 10.1097/00000542-200504000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Manaka T., Ito Y., Matsumoto I., Takaoka K., Nakamura H. Functional recovery period after arthroscopic rotator cuff repair: is it predictable before surgery? Clin Orthop Relat Res. 2011 Jun;469(6):1660–1666. doi: 10.1007/s11999-010-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cofield R.H., Parvizi J., Hoffmeyer P.J., Lanzer W.L., Ilstrup D.M., Rowland C.M. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Jt Surg Am Vol. 2001 Jan;83(1):71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Capdevila X., Barthelet Y., Biboulet P., Ryckwaert Y., Rubenovitch J., d'Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999 Jul;91(1):8–15. doi: 10.1097/00000542-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Bishop J.Y., Sprague M., Gelber J. Interscalene regional anesthesia for shoulder surgery. J Bone Jt Surg Am Vol. 2005 May;87(5):974–979. doi: 10.2106/JBJS.D.02003. [DOI] [PubMed] [Google Scholar]
- 15.Cho C.H., Song K.S., Min B.W. Multimodal approach to postoperative pain control in patients undergoing rotator cuff repair. Knee Surg Sports Traumatol Arthrosc : official journal of the ESSKA. 2011 Oct;19(10):1744–1748. doi: 10.1007/s00167-010-1294-y. [DOI] [PubMed] [Google Scholar]
- 16.Tang R., Evans H., Chaput A., Kim C. Multimodal analgesia for hip arthroplasty. Orthop Clin N Am. 2009 Jul;40(3):377–387. doi: 10.1016/j.ocl.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 17.Parvataneni H.K., Ranawat A.S., Ranawat C.S. The use of local periarticular injections in the management of postoperative pain after total hip and knee replacement: a multimodal approach. Instr Course Lect. 2007;56:125–131. [PubMed] [Google Scholar]
- 18.Vendittoli P.A., Makinen P., Drolet P. A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. J Bone Jt Surg Am Vol. 2006 Feb;88(2):282–289. doi: 10.2106/JBJS.E.00173. [DOI] [PubMed] [Google Scholar]
- 19.Cohen D.B., Kawamura S., Ehteshami J.R., Rodeo S.A. Indomethacin and celecoxib impair rotator cuff tendon-to-bone healing. Am J Sports Med. 2006 Mar;34(3):362–369. doi: 10.1177/0363546505280428. [DOI] [PubMed] [Google Scholar]
- 20.Tempfer H., Gehwolf R., Lehner C. Effects of crystalline glucocorticoid triamcinolone acetonide on cultured human supraspinatus tendon cells. Acta Orthop. 2009 Jun;80(3):357–362. doi: 10.3109/17453670902988360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saito M., Tsukada S., Fujita N. Post-operative pain control following arthroscopic rotator cuff repair: peri-articular injection versus interscalene brachial plexus block. Int Orthop. 2019 Jun;43(6):1435–1441. doi: 10.1007/s00264-018-4096-3. [DOI] [PubMed] [Google Scholar]
- 22.Gurger M., Ozer A.B. A comparison of continuous interscalene block versus general anesthesia alone on the functional outcomes of the patients undergoing arthroscopic rotator cuff repair. Eur J Orthop Surg Traumatol : Orthop Traumatol. 2019 Dec;29(8):1659–1666. doi: 10.1007/s00590-019-02482-8. [DOI] [PubMed] [Google Scholar]
- 23.Malik T., Mass D., Cohn S. Postoperative analgesia in a prolonged continuous interscalene block versus single-shot block in outpatient Arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2016 Aug;32(8):1544–15450 e1. doi: 10.1016/j.arthro.2016.01.044. [DOI] [PubMed] [Google Scholar]
- 24.Singh S., Goyal R., Upadhyay K.K., Sethi N., Sharma R.M., Sharma A. An evaluation of brachial plexus block using a nerve stimulator versus ultrasound guidance: a randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2015 Jul-Sep;31(3):370–374. doi: 10.4103/0970-9185.161675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abdallah F.W., Halpern S.H., Aoyama K., Brull R. Will the real benefits of single-shot interscalene block please stand up? A systematic review and meta-analysis. Anesth Analg. 2015 May;120(5):1114–1129. doi: 10.1213/ANE.0000000000000688. [DOI] [PubMed] [Google Scholar]
- 26.Fredrickson M.J., Ball C.M., Dalgleish A.J. Analgesic effectiveness of a continuous versus single-injection interscalene block for minor arthroscopic shoulder surgery. Reg Anesth Pain Med. 2010 Jan-Feb;35(1):28–33. doi: 10.1097/AAP.0b013e3181c771bd. [DOI] [PubMed] [Google Scholar]
- 27.Lenters T.R., Davies J., Matsen F.A., 3rd The types and severity of complications associated with interscalene brachial plexus block anesthesia: local and national evidence. J Shoulder Elbow Surg. 2007 Jul-Aug;16(4):379–387. doi: 10.1016/j.jse.2006.10.007. [DOI] [PubMed] [Google Scholar]


