Abstract
Objective Anxiety and depression rates are known to be elevated in prematurely-born children and adolescents. This prospective study examines demographic, academic, and physical health correlates of anxiety and depression symptoms in a sample of 10-year-old children who were born extremely preterm. Methods Participants were 889 (51.2% male; 62.3% White) children who were born <28 weeks gestation. Child and family demographic data were collected at birth. When the children were 10, parents (n = 871) and teachers (n = 640) rated the level of anxiety and depression in children through the Child Symptom Inventory-4. Child academic functioning was assessed via the Wechsler Individual Achievement Test-III. Parents completed questionnaires about child academic functioning and physical health issues. Data analyses were conducted with multivariate linear modeling. Results Level of prematurity was significantly related to both parent and teacher reports of anxiety. Public health insurance and individualized education program (IEP) status were associated with both parent and teacher reports of depression. Hispanic ethnicity, public insurance, IEP status, and asthma were significantly associated with both parent-reported anxiety and depression. Gross motor impairment was associated with parent-reported anxiety and teacher-reported depression. Child obesity was associated with teacher reports of anxiety, while male sex was significantly related to teacher reports of depression. Conclusion This pattern of findings may suggest hypotheses for future research on models of the development and persistence of anxiety and depression within this particularly vulnerable group of children.
Keywords: anxiety, depression, infancy and early childhood, intellectual disability, longitudinal research, mental health, parents, prematurity and low birthweight, psychosocial functioning, social skills
Introduction
Half of all lifetime cases of psychopathology manifest by age 14 (Kessler et al., 2005). Prevalence estimates of anxiety and depressive disorders indicate rates of 5–7% and 2%, respectively, at ages 9–11 years (Copeland et al., 2014; Costello et al., 2003; Ghandour et al., 2018), with some evidence that anxiety prevalence may be even higher (Cartwright-Hatton et al., 2006). These rates increase to 32% and 14%, respectively, in adolescence (Merikangas et al., 2011). As these internalizing disorders develop during childhood and adolescence, they are associated with poor adaptive functioning, learning disabilities, persistent and escalating psychopathology, and maladaptive outcomes later in life (Al-Yagon, 2010; Beesdo et al., 2009; Bonifacci et al., 2015; Gregory et al., 2007; Kendall et al., 2004; Kessler et al., 2005; Manikam et al., 1995).
Children born extremely preterm comprise a particularly vulnerable group that is at heightened risk for anxiety and depression during childhood and adolescence (Elgen et al., 2002; Hack et al., 2009) and in young adulthood (Boyle et al., 2011; Nosarti et al., 2012). However, the developmental processes by which these internalizing problems unfold in this population are unclear. One contributing factor may be chronic health disorders such as asthma, epilepsy, obesity, and neurosensory and neuromotor impairments for which children born extremely preterm are at higher risk (Belfort et al., 2013; Dombkowski et al., 2008; Douglass et al., 2017; Marlow et al., 2007; Wood et al., 2000). Learning difficulties and psychological stress in the school context also occur more frequently among children born extremely preterm (Akshoomoff et al., 2017; Joseph et al., 2016), and this may be associated with risk for anxiety and depression symptoms.
In turn, these health and academic difficulties have been found by numerous studies to relate to anxiety and depression symptoms or disorders in term-born samples (Hysing et al. 2007). Youth aged 11–17 years of age who have asthma have been found to experience an almost two-fold higher prevalence of comorbid anxiety and depressive disorders compared to control youth (Katon et al., 2007). A meta-analysis of studies on epilepsy in children and adolescents found increased levels of anxiety and depression in comparison to healthy controls (Scott et al., 2020). Studies of children (Fellinger et al., 2009) and adolescents (Van Gent et al., 2007) with hearing impairments have identified higher rates of psychopathology overall and specifically increased risk of depression in children (Theunissen et al., 2011). Visual impairments (VI) also affect child mental health; a systematic review of literature found overall elevated levels of emotional problems among children with VI compared to their sighted peers (Augestad, 2017), with high levels of anxiety and depression found particularly in girls with VI. Another recent meta-analysis has shown a significantly higher risk for major depressive disorder among children and adolescents with obesity (Rao et al., 2020), while a study of elementary school children in Japan found a significant association between obesity and the combination of hyperactivity and anxiety in females (Suzuki et al., 2020).
As with chronic health problems, academic difficulty and the need for academic support also are associated with anxiety and depression in youth. Anxiety can be an antecedent and consequence of academic problems, as experiences of failure can increase anticipatory fear, while the fear itself reduces performance on academic tasks. The relationship of anxiety to academic performance is fairly well established (Muris & Meesters, 2002). For example, in a study of 478 children aged 8–16 years, those with good or very good grades were significantly less likely to fall into the anxious range than their peers with insufficient grades (4% vs. 14%; Mazzone et al., 2007). A study of 227 children ages 7–14 years (Mychailyszyn et al., 2010) found that children with anxiety disorders had lower school functioning than their non-anxious peers, while in a study of 12–13 year olds in two UK schools, lower academic performance was associated with higher levels of both anxiety and depression (Owens et al., 2012). Additional studies have also found that depression is associated with academic difficulty in term-born child populations (e.g., Fröjd et al., 2008; Lundy et al., 2010).
Given the relationships between physical and academic problems and anxiety and depression symptoms in term-born child populations, a detailed exploration of these links in a sample of children born extremely preterm, who are more likely to experience such problems, can help to identify which specific problems might relate most to anxiety and depression in these children. Such an exploration will support generation of hypotheses about the role of physical and academic problems in the development of anxiety and depression in this vulnerable population. It also may serve as a starting point for research on which physical and/or academic indicators may be most useful in prompting screening and evaluation for anxiety and depression in children born extremely preterm.
From a methodological perspective, accurate measurement of anxiety and depression in school-age children can present a challenge. First, screening is often based on checklist measures completed by parents, teachers and/or other caretakers. Moreover, agreement between parents and other reporters (e.g., teachers or children themselves) on internalizing symptoms is typically low (De Los Reyes & Kazdin, 2005; Keiley et al., 2000), in part because the expression of these disorders may differ in school versus home contexts. Parent reports can also be subject to bias, reflecting parents’ own difficulties with mood and anxiety (De Los Reyes & Kazdin, 2005), while teachers may tend to under-report symptomatology, especially in internalizing disorders (Splett et al., 2019). Second, internalizing disorders can be hard to detect. Even when symptoms cause significant distress to the individual, children may not express these symptoms outwardly. Therefore, the use of a multi-informant approach is important when evaluating anxiety and depressive symptoms in youth populations (Navarro et al., 2020).
There are also known strong effects of both family and individual demographic factors on anxiety and depression in the general child and adolescent population; likewise, demographics may affect risk for and level of prematurity. Family factors such as race, ethnicity, and socioeconomic adversity are related to risk for anxiety and/or depression in child or youth populations, as are child factors like sex. For both anxiety and depression, sex differences are present but do not tend to manifest until adolescence or young adulthood (Copeland et al., 2014; Costello et al., 2003, 2006; Son & Kirchner, 2000). Findings on race and ethnicity have been mixed but trend toward increased risk for internalizing symptoms in minority racial groups (Assari et al., 2018; Emslie et al., 1990; Roberts et al., 1997) and in children with Hispanic ethnicity (Glover et al., 1999; Kennard et al., 2006; Varela et al., 2019). Socioeconomic disadvantage, in this project defined as lower economic status and indexed by reliance on public insurance, is positively related to anxiety and depression in children (Lemstra et al., 2008). These demographic factors also relate to premature birth (Blumenshine et al., 2010; Wong & Edwards, 2013) and therefore any research examining the other correlates of anxiety and depression in children must take the effects of these demographic factors into account. Finally, extent of prematurity itself is a child factor that may have a link to mental health outcomes (e.g., Santos et al., 2017), and so this variable is also considered in research on this topic; the gestational age range of our population of children born extremely preterm is 23–27 weeks.
In this study, we used the parent- and teacher-report forms of the Child Symptom Inventory-4 (CSI-4) (Gadow & Sprafkin, 2002) to measure anxiety and depression symptoms at age 10 in the Extremely Low Gestational Age Newborn (ELGAN) cohort, born between 2002 and 2004. We sought to evaluate demographic (sex, race, ethnicity, socioeconomic adversity, and extent of prematurity), academic, and physical functioning factors as they related to parent-and teacher-reported symptoms of anxiety and depression. Based on available empirical evidence, we hypothesized that, in this sample of children born extremely preterm, (1) academic difficulties would relate to higher levels of anxiety and depression symptoms; and that (2) physical health problems would also relate to higher levels of anxiety and depression symptoms.
Methods
Participants
The data for this study were collected as part of the ELGAN Study, a multi-center prospective observational study of structural and functional neurologic disorders in children born extremely preterm. A total of 1,506 infants born prior to the 28th full week of gestation and their parents were recruited to participate in the study from 14 U.S. sites between 2002 and 2004. Of these, 1,200 children survived past infancy, and 966 were eligible to participate in 10-year follow-up (eligibility criteria were based on availability of newborn proteomic data). Of these, 889 children (52% male) and their parents, and teachers of 640 of the children, participated in this study. Of participating families, 63% self-identified as white, about 10% as Hispanic, and 35% reported relying on public health insurance at the time of child’s birth. Maternal age ranged from 14 to 43 years at the time of child’s birth, with a mean of 29 years (SD = 6.7), and 22% of the mothers reported being single parents. Maternal education ranged from less than high school (15%) to graduate degree (16%), with 50% of mothers having high school/some college and 19% having 4-year college degrees.
Procedures
The institutional review boards at all participating sites approved enrollment and consent procedures for the 10-year follow-up study. Eligible families were contacted by mail and by phone to invite them to participate. Parents who enrolled their children in the 10-year follow-up completed a series of questionnaires while the children underwent a 3-hour assessment. With parental consent, teachers were asked to complete questionnaires regarding children’s functioning in school.
Measures
Anxiety and depression symptoms were assessed via parent and teacher reports on the CSI-4 Checklist (Gadow & Sprafkin, 2002; Sprafkin et al., 2002). The parent version of the CSI-4 contains 97 items that screen for 15 emotional and behavioral disorders, and the teacher version contains 73 items that screen for 13 disorders. An average of parent-reported T-scores on Generalized Anxiety Disorder, Social Phobia, and Separation Anxiety was used to represent global anxiety symptomatology (Compton et al., 2010). T-scores on Major Depressive Disorder and Dysthymic Disorder subscales were averaged to represent depression symptomatology. Teacher-reported anxiety symptomatology was calculated as a mean of Generalized Anxiety Disorder and Social Phobia T-scores (teachers did not report on separation anxiety symptoms), and teacher-reported depression symptomatology was calculated as a mean of Depressive Disorder and Dysthymic Disorder T-scores. The psychometric properties of the CSI-4 indicate stable internal consistency (αs ranging from .69 to.79 on the scales of interest) and test–retest reliability of at least .65 (Sprafkin et al., 2002). Within our sample, CSI-4 internal consistency was comparable, ranging from α =.69 to α =.89.
Demographic Information: Demographic characteristics, including child sex (race (White/non-White), ethnicity (Hispanic/non-Hispanic), gestational age (in days), and family reliance on publicly subsidized health insurance, were assessed at birth and tested as possible correlates of children’s symptoms of anxiety and depression. Percentages for dichotomous variables and mean/SD for continuous variables are also presented in Table I.
Table I.
Descriptive Statistics and Bivariate Correlations for Observed Study Variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex (male) | – | ||||||||||||
| 2. Race (White) | .03 | – | |||||||||||
| 3. Ethnicity (Hispanic) | −.05 | −.21 | – | ||||||||||
| 4. Public Insurance | −.05 | −.38 | .13 | – | |||||||||
| 5. Gestational age (days) | −.05 | .05 | −.02 | −.04 | – | ||||||||
| 6. IEP | .17 | −.14 | .00 | .17 | −.17 | – | |||||||
| 7. Academic skills composite | −.08 | .23 | −.09 | −.28 | .20 | −.47 | – | ||||||
| 8. Asthma | .00 | −.14 | .07 | .17 | −.00 | .10 | −.07 | – | |||||
| 9. Epilepsy | .02 | −.08 | .02 | .13 | −.07 | .19 | −.28 | .04 | – | ||||
| 10. Hearing impairment | −.01 | −.02 | .06 | .00 | −.09 | .14 | −.13 | .00 | .09 | – | |||
| 11. Vision impairment | .03 | .05 | −.01 | −.01 | −.22 | .22 | −.16 | .00 | .16 | .02 | – | ||
| 12. Gross motor impairment | .03 | −.01 | .02 | .11 | −.14 | .30 | −.43 | .06 | .30 | .15 | .23 | – | |
| 13. Obesity | .01 | −.09 | .06 | .09 | −.01 | .02 | −.12 | .04 | .03 | .04 | .04 | .07 | – |
| 14. Anxiety, parent report | −.07 | −.09 | .12 | .15 | −.08 | .21 | −.10 | .17 | .08 | .05 | .04 | .13 | .09 |
| 15. Depression, parent report | −.02 | −.04 | .12 | .15 | −.03 | .12 | −.02 | .12 | .09 | .01 | .01 | .09 | .09 |
| 16. Anxiety, teacher report | .03 | −.03 | .01 | .06 | −.09 | .12 | −.10 | .01 | .04 | −.04 | .05 | .02 | .10 |
| 17. Depression, teacher report | .08 | −.01 | −.01 | .14 | −.02 | .15 | −.10 | .06 | .00 | −.04 | .03 | .09 | .04 |
| N | 889 | 889 | 889 | 889 | 889 | 889 | 874 | 889 | 889 | 889 | 889 | 889 | 857 |
| M or % | 52.0% | 63.2% | 9.7% | 35.3% | 182.8 | 53.8% | 90.9 | 37.7% | 7.4% | 4.4% | 21.3% | 10.9% | 22.6% |
| SD | – | – | – | – | 9.0 | – | 19.2 | – | – | – | – | – | – |
| Min | – | – | – | – | 161 | – | 40.0 | – | – | – | – | – | – |
| Max | – | – | – | – | 195 | – | 131.7 | – | – | – | – | – | – |
| 14 | 15 | 16 | 17 | |
|---|---|---|---|---|
| 14. Anxiety, parent report | – | |||
| 15. Depression, parent report | .64 | – | ||
| 16. Anxiety, teacher report | .27 | .19 | – | |
| 17. Depression, teacher report | .28 | .32 | .66 | – |
| N | 871 | 871 | 640 | 637 |
| M or % | 54.0 | 53.9 | 54.4 | 55.4 |
| SD | 5.9 | 7.1 | 6.4 | 8.7 |
| Min | 50 | 50 | 50 | 50 |
| Max | 78 | 78 | 78 | 78 |
Note. All correlations at or above .08 are significant at p < .05.
Academic Factors: Academic skills were measured through the Wechsler Individual Achievement Test-III (WIAT-III; Wechsler, 2009) and calculated as the mean of four standardized subscales: Word Reading, Pseudoword Decoding, Spelling, and Numerical Operation subtests. The WIAT-III is a norm-standardized measure of academic achievement for children from pre-K through grade 12. Developer-reported psychometric data indicate high internal consistency within subtests, ranging from .80 to .98, with test–retest reliability ranging from .85 to .98. The internal consistency for the academic skills composite within our sample was α = .95. Parents also reported whether had an individualized education program (IEP) through the school.
Physical Health: Weight and height at 10 years were obtained by study personnel. Body mass index (BMI) was then calculated using the following formula: BMI = weight (in kilograms)/height2 (in meters). BMI Z-scores and percentiles for age and sex were then determined based on current CDC growth charts. A BMI percentile of ≥95 was considered obese. Parents completed a questionnaire about children’s medical history, including asthma, any significant visual or hearing impairment. Epilepsy was diagnosed by qualified specialists’ consensus (Douglass et al., 2017). The Gross Motor Function Classification System (GMFCS) was used to establish gross motor impairments. The GMFCS is a widely used 5-level system that provides a simple method for classifying gross motor functional abilities and limitations in children (Palisano et al., 2008). Versions of the GMFCS are available in at least 10 languages and demonstrate strong psychometric properties (Morris et al., 2004). In our study, a version for 2–12 years old children was used to define gross motor impairment as any gross motor limitations, such as having difficulties walking or balancing on uneven terrain or having to rely on railing or physical support to go up and down the stairs. The GMFCS was assessed based on parent information, with inter-rater reliability (kappa) above .80.
Data Analyses
Univariate statistics were used to describe the characteristics of the sample. Bivariate correlations describe the relations among all predictor variables and assess potential multicollinearity. Next, a series of multivariate linear regression models for each of four outcomes (parent- and teacher-reported anxiety and depression symptoms) were conducted to examine the relations between demographic factors and anxiety and depression symptoms among 10-year-old children born extremely preterm (Model 1 in Table II). Subsequent multivariate linear models (Models 2 and 3 in Table II) included these demographic variables as covariates to test the links between academic factors or physical health factors and anxiety and depression symptoms over and above demographic factors. The results have been adjusted for false discovery rate using Benjamini–Hochberg’s method (Haynes, 2013). All analyses were conducted in SAS 9.4., with statistical significance levels set at p < .05.
Table II.
Descriptive Data and Regression Analysis Predicting Children’s Anxiety and Depression Symptoms
| Anxiety, parent report |
Depression, parent report |
Anxiety, teacher report |
Depression, teacher report |
|||||
|---|---|---|---|---|---|---|---|---|
| 1. Demographics |
R2 = .04
|
R2 = .04
|
R2 = .02
|
R2 = .03
|
||||
| Β (SE) | β | Β(SE) | β | Β(SE) | β | Β(SE); | β | |
| Sex (male) | −.73 (.39) | −.06 | −.17 (.48) | −.01 | .34 (.51) | .03 | 1.40 (.68) | .08* |
| Race (White) | −.31 (.44) | −.03 | .61 (.54) | .04 | −.09 (.58) | −.01 | .87 (.78) | .05 |
| Ethnicity (Hispanic) | 1.77 (.68) | .09** | 2.58 (.82) | .11*** | −.08 (.90) | −.00 | −.54 (1.21) | −.02 |
| Public insurance | 1.45 (.44) | .12*** | 2.23 (.54) | .15*** | .71 (.57) | .05 | 3.04 (.77) | .17*** |
| Gestational age (days) | −.05 (.02) | −.09** | −.02 (.03) | −.03 | −.06 (.03) | −.09* | −.02 (.04) | −.02 |
| 2. Academic factors |
ΔR2 = .04
|
ΔR2 = .02
|
ΔR2 = .01
|
ΔR2 = .03
|
||||
|---|---|---|---|---|---|---|---|---|
| Β (SE) | β | Β(SE) | β | Β(SE) | β | Β(SE); | β | |
| Sex (male) | −1.05 (.39) | −.08 | −.34 (.48) | −.02 | .17 (.51) | .01 | 1.14 (.69) | .07 |
| Race (White) | −.11 (.44) | −.01 | .68 (.54) | .05 | .08 (.54) | .01 | 1.13 (.78) | .06 |
| Ethnicity (Hispanic) | 1.94 (.66) | .10** | 2.78 (.82) | .12*** | .07 (.90) | .00 | −.26 (1.20) | −.01 |
| Public insurance | 1.19 (.45) | .10** | 2.27 (.55) | .15*** | .34 (.59) | .03 | 2.53 (.79) | .14*** |
| Gestational age (days) | −.04 (.02) | −.05 | −.01 (.03) | −.02 | −.04 (.03) | −.06 | .02 (.04) | .02 |
| IEP | 2.61 (.44) | .22*** | 2.08 (.54) | .15*** | 1.05 (.58) | .08 | 2.08 (.78) | .12** |
| Academic skill composite | .02 (.01) | .05 | .04 (.02) | .09* | −.02 (.02) | −.04 | .01 (.02) | .03 |
| 3. Physical health |
ΔR2 = .04
|
ΔR2 = .02
|
ΔR2 = .01
|
ΔR2 = .01
|
||||
|---|---|---|---|---|---|---|---|---|
| Β (SE) | β | Β(SE) | β | Β(SE) | β | Β(SE); | β | |
| Sex (male) | −.66 (.39) | −.06 | −.06 (.48) | −.00 | .40 (.51) | .03 | 1.38 (.68) | .08 * |
| Race (White) | .06 (.45) | .01 | .84 (.55) | .06 | .09 (.59) | .01 | .75 (.79) | .04 |
| Ethnicity (Hispanic) | 1.16 (.70) | .06 | 2.24 (.86) | .09 ** | −.51 (.93) | −.02 | −.89 (1.24) | −.03 |
| Public insurance | 1.26 (.45) | .10 ** | 1.96 (.56) | .13 *** | .73 (.59) | .05 | 2.48 (.79) | .14 *** |
| Gestational age (days) | −.05(.02) | −.08* | −.02 (.03) | −.03 | −.07 (.03) | −.10* | −.01 (.04) | −.01 |
| Asthma | 1.88 (.41) | .16 *** | 1.34 (.50) | .09 ** | −.05 (.53) | −.00 | .69 (.71) | .04 |
| Epilepsy | .61 (.80) | .03 | 1.11 (.98) | .04 | .64 (1.07) | .03 | −1.53 (1.45) | −.04 |
| Hearing impaired | .07 (.99) | .00 | −.76 (1.22) | −.02 | −1.42 (1.30) | −.04 | −2.00 (1.74) | −.05 |
| Vision impaired | .11 (.51) | .01 | −.29 (.62) | −.02 | .28 (.65) | .02 | −.06 (.87) | −.00 |
| Gross motor impaired | 1.68 (.73) | .08 * | 1.06 (.89) | .04 | −.02 (.90) | −.00 | 2.38 (1.22) | .08 * |
| Obesity | .80 (.47) | .06 | 1.10 (.58) | .07 | 1.51 (.60) | .10 ** | .57 (.80) | .03 |
Note.
p < 0.001;
p ≤ 0.01;
p ≤ 0.05; Β = unstandardized parameter estimate; β = standardized parameter estimate; IEP = individualized education program; SE = standard error.
Results
In our sample of 889 children, parent-report data were available in full on most variables, and for 871 children on anxiety and depression symptomatology. Missing data were estimated using the Full Information Maximum Likelihood method. Teacher reports were available for 640 children. There were no demographic differences among children with (n = 871) and without (n = 18) on parent-reported anxiety or depression symptoms data. Children for whom teacher reports were not available (n = 249) did not differ from other children on any demographic characteristic, except on race; those with teacher data were more likely to be white than those without teacher data (t = 2.81, p = .005).
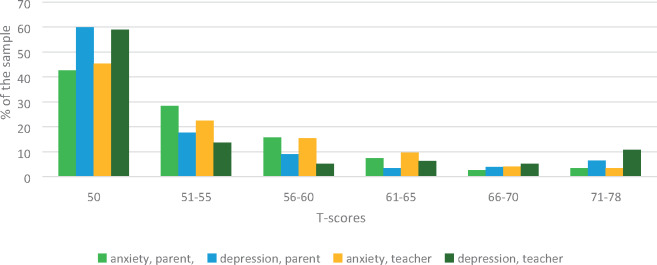
The mean T-score for anxiety symptoms was 54.0 (SD = 5.9) as reported by parents and 53.9 (SD = 7.1) as reported by teachers. The mean T-score for depression was 54.4 (SD = 6.4) and 55.4 (SD = 8.7) as reported by parents and teachers, respectively. The distribution of T-scores for the CSI-4 depression and anxiety scales is shown in Figure 1 in the following order: anxiety by parent report; depression by parent report; anxiety by teacher report; and depression by teacher report. For parent-reported anxiety, 13.3% of the sample had an elevated T-score (defined as T > 60), while for teacher-reported anxiety that percentage was 16.9%. For parent-reported depression, 13.5% of the sample had an elevated T-scores, whereas 22.3% had elevated teacher-reported depression T-scores. Looking at the internalizing symptom constructs across reporters, 22.1% of the sample had an elevated T-score for anxiety (parent and/or teacher reported), and 24.6% had an elevated T-score for depression (parent and/or teacher reported). The magnitude of zero-order correlations among parent and teacher ratings was moderate for both anxiety (r = .27, p < .001) and depression (r = .32, p < .001). The descriptive information of study variables is shown in Table I.
Figure 1.
T-score distribution for CSI-4 anxiety and depression.
Bivariate Correlations among Demographic, Academic, and Physical Health Factors in ELGANs
ELGAN children with higher gestational age had higher levels of academic achievement and were less likely to have an IEP. They were also less likely to have visual or significant gross motor impairments compared to ELGAN children with lower gestational age. ELGAN children born to families with greater socioeconomic disadvantage had lower academic achievement, were more likely to have an IEP, and were more likely to suffer from asthma, compared to children born to families with lower socioeconomic disadvantage. Additionally, children with gross motor impairment, although only 11% of our sample, were more likely to have lower levels of academic achievement and more likely to have comorbid physical health conditions, such as epilepsy and hearing or visual impairment.
Correlates of Parent-Reported Anxiety and Depression Symptomatology
Full results of regression analyses are presented in Table II. With regard to demographic correlates (Model 1), higher levels of anxiety symptoms were reported by parents of children with Hispanic ethnicity (β = .09, p < .01), those relying on public insurance at birth (β = .12, p < .001) and children with lower gestational age (β = −.09, p < .01). Higher levels of depression symptoms were likewise reported by parents of children with Hispanic ethnicity (β = .11, p = .002) and public insurance (β = .15, p < .001).
After accounting for demographic variables (Models 2 and 3), higher levels of anxiety were reported by parents if their child had an IEP (β = .20, p < .001), had asthma (β = .16, p < .001), or had gross motor functioning difficulties (β = .08, p = .004). Higher levels of depression were reported by parents whose child had an IEP (β = .15, p < .001) or had asthma (β = .09, p = .008).
Correlates of Teacher-Reported Anxiety and Depression Symptomatology
Regarding demographic findings (Model 1), teacher-reported anxiety symptoms were related to gestational age (β = −.09, p < .05), and teacher-reported depression symptoms were related to male sex (β = .08, p = .03), receipt of public health insurance at birth (β = .17, p = .005). For academic factors (Model 2), teacher-reported depression was related to having an IEP (β = .12, p < .05). For health factors (Model 3), teacher-reported depression was related to gross motor impairment (β = .08, p < .05), while teacher-reported anxiety was related to child obesity (β = .10, p < .01).
Discussion
Existing research tells us that children born extremely preterm are at increased risk for anxiety and depression during childhood and adolescence (Dvir et al., 2019; Elgen et al., 2002; Hack et al., 2009). However, the correlates of anxiety and depression in this population are not well known. Our aim in this study was to evaluate how child anxiety and depression symptoms related to demographic factors, academic difficulties, and physical health problems in a sample of children born extremely preterm, with a goal to enhance understanding of factors that might influence anxiety and depression within this group and to generate hypotheses for future research on pathways to anxiety and depression within this vulnerable population.
In the full sample, the mean scores on anxiety and depression, by both teacher and parent reports, were above the average of the normative sample (Gadow & Sprafkin, 2002) by about half of a standard deviation (T-scores ranged from 53.9 to 55.4). Moreover, nearly a quarter of the sample had an elevated T-score (T > 60) on depression (24.6%) noted by at least one reporter; this was similar for anxiety (22.1%). The next wave of assessment of the ELGAN population, at age 15, will provide more information on how this pattern of anxious and depressive symptoms may change as the children transition into adolescence. Notably, level of prematurity was a correlate in our models of child anxiety as reported by both teachers and parents. This effect size is relatively small (β = .09). However, this is of particular interest in that the entire sample was born extremely premature, and it indicates that even within this narrow range (from 23 to 27 weeks gestation), the more preterm the birth, the higher the risk for child anxiety that can be seen across contexts, by parents and teachers both. In addition, children with lower gestational age had lower level of academic achievement and were more likely to have visual and gross motor impairments, again suggesting that, even among children born extremely premature, lower gestational age at birth carries increased physical, academic, and mental health risks.
Other demographic variables showed significant relationships with anxiety and depression in our sample. Receipt of public health insurance, an index of socioeconomic disadvantage in the ELGAN cohort, was associated with higher levels of anxiety (by parent and teacher report) and depression (by teacher report) symptoms. The association of increased anxiety and depression with indices of social disadvantage has been previously reported in large pediatric cohorts (Spence et al., 2002; Bitsko et al., 2018). We also found an association between parent-reported anxiety and depression symptoms and Hispanic ethnicity, a correlation that has been found in other work using term-born samples (Kennard et al., 2006; Varela et al., 2019). Regarding sex-related findings, teachers reported higher levels of depression in boys. Our finding of higher levels of depression among boys contrasts with research findings that show, in general population studies, the sex ratio in prepubertal children is equal between boys and girls and then becomes 2:1 (female to male) during adolescence (Son & Kirchner, 2000).
We also hypothesized that anxiety and depression symptoms would be significantly related to physical health problems and academic challenges. Each construct tested in our Models 2 (academic factors) and 3 (physical health factors) has been found in the literature to have associations both with prematurity and with anxiety and depression. While not all variables were significantly related to anxiety and depression in our sample (notably, WIAT scores, epilepsy, and hearing and vision impairment were not), some significant relationships were found. Consistent with the research on term-born children (Katon et al., 2007), asthma was strongly related to parent-reported anxiety and depression symptoms. Impairment in gross motor function was associated with parent-reported anxiety as well as teacher-reported depression, indicating that parents see children with motor impairment as more nervous, worried, or socially withdrawn, while teachers of children with motor impairment may view them as more sad, irritable or globally withdrawn.
Childhood obesity was also associated with teacher-reported depression symptoms. Specifically for children born extremely preterm, exposure to higher levels of inflammatory factors in the pre/perinatal phase (Dammann et al., 2001; Fichorova et al., 2011) may contribute to the risk of later emerging obesity and depression (Kiecolt-Glaser et al., 2015; Luppino et al., 2010; Perrin et al., 2018). Consistent with our findings, a relationship between depression and obesity in adolescents has been found among term-born children and adolescents (Sjöberg et al., 2005). That the depressive symptoms were seen in the school setting, by teachers, is of interest and may indicate social effects of obesity on children as part of the depression picture.
Having an IEP was related to reports of depression from both parents and teachers, as well as reports of anxiety from parents. In contrast, academic achievement as measured directly by the WIAT-III was not significantly related to anxiety or depression symptoms. This may be because the WIAT- III may better measure the ability to achieve on academic achievement tests, in contrast to everyday academic performance, whereas the IEP may be a more direct index of how the child is functioning at school (requiring an IEP indicating higher need and lower functioning). This would indicate that an increased need for help and assistance in school is associated with increased levels of poor mood, irritability, or withdrawal in children, as reported by parents and teachers.
Our findings in this study, taken in combination with other existing research findings on anxiety and depression in children born extremely preterm, continue to support a potential benefit of monitoring these children for internalizing disorders, to ensure the timely implementation of best evidence-based practices to address anxiety and depression and prevent increasing distress and psychosocial impairment over time (Kessler et al., 2005). In addition, our findings show relationships between both physical and academic difficulties and internalizing symptoms that may be of interest for hypothesis generation about pathways to anxiety and depressive disorders in children born extremely preterm. While the lack of control group in this study precludes the ability to draw conclusions that relationships found in this study are unique to children born extremely preterm, the pattern of findings may serve as a launching point for study of factors contributing to the development and maintenance of anxiety and depression in this population. Relevant findings that invite further exploration include the negative relationship of gestational age to multi-informant reports of anxiety symptoms; specific correlations of demographic factors such as ethnicity and early socioeconomic adversity; the finding of higher rates of teacher-reported depression symptoms in males; and the potentially significant relationships of asthma, motor impairment, and obesity with mood and anxiety symptoms. The next wave of longitudinal ELGAN assessment will contribute further to this research, as it includes further measurement of anxiety and depressive symptoms and diagnoses at age 15. Studies including control groups of term-born youth will provide a clearer understanding of the developmental pathways or relationships that are unique to children born extremely preterm.
The current study has significant strengths. The large ELGAN sample was selected based on gestational age rather than birth weight, decreasing confounding by correlates of fetal growth restriction. Data were collected prospectively and sample attrition was modest. As noted above, a limitation of our study is the lack of a comparison group of children born at full term. In addition, teacher reports were missing for 26.6% of the sample. Finally, the CSI-4, while a reliable and valid screening measure for assessing psychiatric symptoms in children (Sprafkin et al., 2002), is not as valid as a structured interview for diagnosing anxiety and depression. In the next wave of the ELGAN study, at age 15, children will undergo diagnostic assessment for anxiety, depression, and other psychiatric disorders.
Conclusion
Our study identified several physical, demographic, and school factors associated with increased symptoms of anxiety and depression. These findings contribute to understanding how these factors, many of which are more common and severe in children born extremely preterm, may relate to difficulty with mood and anxiety as these high-risk children mature through the school years.
Acknowledgments
The authors express sincere gratitude to the study participants, their families, and their teachers for making this study possible.
Funding
This study was supported by the National Institute of Neurological Disorders and Stroke under Grant 5U01NS040069-09 and 5U01NS04006-05, the National Institute of Child Health and Human Development under Grant 5P30HD018655-28, the NIH ECHO Program under Grant UG3OD023348-01, and the National Institute of Nursing Research under Grant 1K23NR017898-01.
Conflicts of interest: The authors have indicated they have no potential conflicts of interest to disclose. Dr Jean A. Frazier has had research support from F. Hoffmann-La Roche Ltd., Fulcrum Therapeutics, Janssen Research & Development, LLC, and has served as a consultant for Takeda Pharmaceuticals. However, these activities were not related to the research contained in this manuscript.
Data Sharing/Availability Statement: Please go to the Archived Clinical Research Datasets and complete the NINDS Data Request Form, Ellen Rosenberg will process the request. If you send the form to CRLiaison@ninds.nih.gov, she’ll receive the e-mail.
References
- Akshoomoff N., Joseph R. M., Taylor H. G., Allred E. N., Heeren T., O'shea T. M., Kuban K. C. K. (2017). Academic achievement deficits and their neuropsychological correlates in children born extremely preterm. Journal of Developmental and Behavioral Pediatrics, 38, 627–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Yagon M. (2010). Maternal emotional resources and socio-emotional well-being of children with and without learning disabilities. Family Relations, 59, 152–169. [Google Scholar]
- Assari S., Gibbons F., Simons R. (2018). Depression among Black youth; Interaction of class and place. Brain Sciences, 8, 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augestad L. B. (2017). Mental health among children and young adults with visual impairments: A systematic review. Journal of Visual Impairment & Blindness, 111, 411–425. [Google Scholar]
- Beesdo K., Knappe S., Pine D. (2009). Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics, 32, 483–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belfort M. B., Gillman M. W., Buka S. L., Casey P. H., McCormick M. C. (2013). Preterm infant linear growth and adiposity gain: Trade-offs for later weight status and intelligence quotient. The Journal of Pediatrics, 163, 1564–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitsko R. H., Holbrook J. R., Ghandour R. M., Blumberg S. J., Visser S. N., Perou R., Walkup J. T. (2018). Epidemiology and impact of health care provider-diagnosed anxiety and depression among US children. Journal of Development & Behavioral Pediatrics, 39, 395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenshine P., Egerter S., Barclay C. J., Cubbin C., Braveman P. A. (2010). Socioeconomic disparities in adverse birth outcomes: A systematic review. American Journal of Preventive Medicine, 39, 263–272. [DOI] [PubMed] [Google Scholar]
- Bonifacci P., Storti M., Tobia V., Suardi A. (2015). Specific learning disorders: A look inside children's and parents' psychological well-being and relationships. Journal of Learning Disabilities, 49, 532–545. [DOI] [PubMed] [Google Scholar]
- Boyle M. H., Miskovic V., Van Lieshout R., Duncan L., Schmidt L. A., Hoult L., Paneth N., Saigal S. (2011). Psychopathology in young adults born at extremely low birth weight. Psychological Medicine, 41, 1763–1774. [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S., McNicol K., Doubleday E. (2006). Anxiety in a neglected population: prevalence of anxiety disorders in pre-adolescent children. Clinical Psychology Review, 26, 817–833. [DOI] [PubMed] [Google Scholar]
- Compton S. N., Walkup J. T., Albano A. M., Piacentini J. C., Birmaher B., Sherrill J. T., Ginsburg G. S., Rynn M. A., McCracken J. T., Waslick B. D., Iyengar S., Kendall P. C., March J. S. (2010). Child/adolescent anxiety multimodal study (CAMS): Rationale, design, and methods. Child and Adolescent Psychiatry and Mental Health, 4(1), 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland W. E., Angold A., Shanahan L., Costello E. J. (2014). Longitudinal patterns of anxiety from childhood to adulthood: the Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello E. J., Erkanli A., Angold A. (2006). Is there an epidemic of child or adolescent depression? Journal of Child Psychology and Psychiatry, 47, 1263–1271. [DOI] [PubMed] [Google Scholar]
- Costello E. J., Mustillo S., Erkanli A., Keeler G., Angold A. (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60, 837–844. [DOI] [PubMed] [Google Scholar]
- Dammann O., Phillips T. M., Allred E. N., O'Shea T. M., Paneth N., Van Marter L. J., Bose C., Ehrenkranz R. A., Bednarek F. J., Naples M., Leviton A. (2001). Mediators of fetal inflammation in extremely low gestational age newborns. Cytokine, 13, 234–239. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A., Kazdin A. E. (2005). Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131, 483–509. [DOI] [PubMed] [Google Scholar]
- Dombkowski K. J., Leung S. W., Gurney J. G. (2008). Prematurity as a predictor of childhood asthma among low-income children. Annals of Epidemiology, 18, 290–297. [DOI] [PubMed] [Google Scholar]
- Douglass L. M., Heeren T. C., Stafstrom C. E., DeBassio W., Allred E. N., Leviton A., O'Shea T. M., Hirtz D., Rollins J., Kuban K. (2017). Cumulative incidence of seizures and epilepsy in ten-year-old children born before 28 Weeks' gestation. Pediatric Neurology, 73, 13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvir Y., Frazier J. A., Joseph R. M., Mokrova I. L., Moore P. S., O'Shea T. M., Hooper S. R., Santos H. P., Kuban K. C. K. (2019). Psychiatric symptoms: Prevalence, co-occurrence and functioning among extremely low gestational age newborns at age ten years. Journal of Developmental & Behavioral Pediatrics, 40, 725–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgen I., Sommerfelt K., Markestad T. (2002). Population based, controlled study of behavioural problems and psychiatric disorders in low birthweight children at 11 years of age. Archives of Disease in Childhood. Fetal and Neonatal Edition, 87, 128–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emslie G. J., Weinberg W. A., Rush J. A., Adams R. M., Rintelmann J. (1990). Depressive symptoms by self-report in adolescence: Phase 1 of the development of a questionnaire by self-report. Journal of Child Neurology, 5, 114–121. [DOI] [PubMed] [Google Scholar]
- Fellinger J., Holzinger D., Sattel H., Laucht M., Goldberg D. (2009). Correlates of mental health disorders among children with hearing impairments. Developmental Medicine & Child Neurology, 51, 635–641. [DOI] [PubMed] [Google Scholar]
- Fichorova R. N., Onderdonk A. B., Yamamoto H., Delaney M. L., DuBois A. M., Allred E., Leviton A. (2011). Maternal microbe-specific modulation of inflammatory response in extremely low-gestational-age newborns. Molecular Biology, 2, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fröjd S. A., Nissinen E. S., Pelkonen M. U. I., Marttunen M. J., Koivisto A., Kaltiala-Heino R. (2008). Depression and school performance in middle adolescent boys and girls. Journal of Adolescence, 31, 485–498. [DOI] [PubMed] [Google Scholar]
- Gadow K. D., Sprafkin J. N. (2002). Child symptom inventory 4: Screening and norms manual. Checkmate Plus. [Google Scholar]
- Ghandour R. M., Sherman L. J., Vladutiu C. J., Ali M. M., Lynch S. E., Bitsko R. H., Blumberg S. J. (2018). Prevalence and treatment of depression, anxiety, and conduct problems in US children. The Journal of Pediatrics, 206, 256–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover S. H., Pumariega A. J., Holzer C. E., Wise B. K., Rodriguez M. (1999). Anxiety symptomatology in Mexican-American adolescents. Journal of Child and Family Studies, 8(1), 47–57. [Google Scholar]
- Gregory A. M., Caspi A., Moffitt T. E., Koenen K., Eley T. C., Poulton R. (2007). Juvenile mental health histories of adults with anxiety disorders. American Journal of Psychiatry, 164, 301–308. [DOI] [PubMed] [Google Scholar]
- Hack M., Taylor H. G., Schluchter M., Andreias L., Drotar D., Klein N. (2009). Behavioral outcomes of extremely low birth weight children at age 8 years. Journal of Developmental & Behavioral Pediatrics, 30, 122–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes W. (2013). Benjamini–Hochberg method. In Dubitzky W., Wolkenhauer O., Cho K. H., Yokota H. (Eds.) Encyclopedia of Systems Biology. Springer. [Google Scholar]
- Hysing M., Elgen I., Gillberg C., Lie S. A., Lundervold A. J. (2007). Chronic physical illness and mental health in children. Results from a large- scale population study. Journal of Child Psychology and Psychiatry, 48, 785–792. [DOI] [PubMed] [Google Scholar]
- Joseph R. M., OShea T. M., Allred E. N., Heeren T., Hirtz D., Jara H., Leviton A., Kuban K. C. K.; for the ELGAN Study Investigators (2016). Neurocognitive and academic outcomes at age 10 years of extremely preterm newborns. Pediatrics, 137, e20154343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W., Lozano P., Russo J., McCauley E., Richardson L., Bush T. (2007). The prevalence of DSM-IV anxiety and depressive disorders in youth with asthma compared with controls. Journal of Adolescent Health, 41, 455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keiley M. K., Bates J. E., Dodge K. A., Pettit G. S. (2000). A cross-domain growth analysis: externalizing and internalizing behaviors during 8 years of childhood. Journal of Abnormal Child Psychology, 28, 161–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall P. C., Safford S., Flannery-Schroeder E., Webb A. (2004). Child anxiety treatment: outcomes in adolescence and impact on substance use and depression at 7.4-year follow-up. Journal of Consulting and Clinical Psychology, 72, 276–287. [DOI] [PubMed] [Google Scholar]
- Kennard B. D., Stewart S. M., Hughes J. L., Patel P. G., Emslie G. J. (2006). Cognitions and depressive symptoms among ethnic minority adolescents. Cultural Diversity and Ethnic Minority Psychology, 12, 578–591. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Berglund P., Demler O., Jin R., Merikangas K. R., Walters E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J. K., Derry H. M., Fagundes C. P. (2015). Inflammation: depression fans the flames and feasts on the heat. American Journal of Psychiatry, 172, 1075–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemstra M., Neudorf C., D’Arcy C., Kunst A., Warren L. M., Bennett N. R. (2008). A systematic review of depressed mood and anxiety by SES in youth aged 10–15 years. Canadian Journal of Public Health, 99, 125–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundy S. M., Silva G. E., Kaemingk K. L., Goodwin J. L., Quan S. F. (2010). Cognitive functioning and academic performance in elementary school children with anxious/depressed and withdrawn symptoms. The Open Pediatric Medicine Journal, 14, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luppino F. S., de Wit L. M., Bouvy P. F., Stijnen T., Cuijpers P., Penninx B. W. J. H., Zitman F. G. (2010). Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry, 67, 220–229. [DOI] [PubMed] [Google Scholar]
- Manikam R., Matson J. L., Coe D. A., Hillman N. (1995). Adolescent depression: Relationships of self-report to intellectual and adaptive functioning. Research in Developmental Disabilities, 16, 349–364. [DOI] [PubMed] [Google Scholar]
- Marlow N., Hennessy E. M., Bracewell M. A., Wolke D.; for the EPICure Study Group (2007). Motor and executive function at 6 years of age after extremely preterm birth. Pediatrics, 120, 793–804. [DOI] [PubMed] [Google Scholar]
- Mazzone L., Ducci F., Scoto M. C., Passaniti E., D'Arrigo V. G., Vitiello B. (2007). The role of anxiety symptoms in school performance in a community sample of children and adolescents. BMC Public Health, 7(1), 347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas K. R., He J., Burstein M. E., Swendsen J., Avenevoli S., Case B., Georgiades K., Heaton L., Swanson S., Olfson M. (2011). Service utilization for lifetime mental disorders in US adolescents: Results of the national comorbidity Survey-Adolescent supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 50, 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris C., Galuppi B. E., Rosenbaum P. L. (2004). Reliability of family report for the Gross Motor Function Classification System. Developmental Medicine and Child Neurology, 46, 455–460. [DOI] [PubMed] [Google Scholar]
- Muris P., Meesters C. (2002). Symptoms of anxiety disorders and teacher-reported school functioning of normal children. Psychological Reports, 91, 588–590. [DOI] [PubMed] [Google Scholar]
- Mychailyszyn M. P., Méndez J. L., Kendall P. C. (2010). School functioning in youth with and without anxiety disorders: comparisons by diagnosis and comorbidity. School Psychology Review, 39(1), 106–121. [Google Scholar]
- Navarro M. C., Orri M., Nagin D., Tremblay R. E., Oncioiu S. I., Ahun M. N., Melchior M., van der Waerden J., Galéra C., Côté S. M. (2020). Adolescent internalizing symptoms: the importance of multi-informant assessments in childhood. Journal of Affective Disorders, 266, 702–709. [DOI] [PubMed] [Google Scholar]
- Nosarti C., Reichenberg A., Murray R. M., Cnattingius S., Lambe M. P., Yin L., MacCabe J., Rifkin L., Hultman C. M. (2012). Preterm birth and psychiatric disorders in young adult life. Archives of General Psychiatry, 69, 610–617. [DOI] [PubMed] [Google Scholar]
- Owens M., Stevenson J., Hadwin J. A., Norgate R. (2012). Anxiety and depression in academic performance: an exploration of the mediating factors of worry and working memory. School Psychology International, 33, 433–449. [Google Scholar]
- Palisano R. J., Rosenbaum P., Bartlett D., Livingston M. H. (2008). Content validity of the expanded and revised gross motor function classification system. Developmental Medicine and Child Neurology, 50, 744–750. [DOI] [PubMed] [Google Scholar]
- Perrin E. M., O'Shea T. M., Skinner A. C., Bose C., Allred E. N., Fichorova R. N., van der Burg J. W., Leviton A. (2018). Elevations of inflammatory proteins in neonatal blood are associated with obesity and overweight among 2-year-old children born extremely premature. Pediatric Research, 83, 1110–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao W., Zong Q., Zhang J., An F., Jackson T., Ungvari G. S., Xiang Y., Su Y., D'Arcy C., Xiang Y. (2020). Obesity increases the risk of depression in children and adolescents: Results from a systematic review and meta-analysis. Journal of Affective Disorders, 267, 78–85. [DOI] [PubMed] [Google Scholar]
- Roberts R. E., Roberts C. R., Chen Y. R. (1997). Ethnocultural differences in prevalence of adolescent depression. American Journal of Community Psychology, 25(1), 95–110. [DOI] [PubMed] [Google Scholar]
- Santos I. S., Barros F. C., Munhoz T., Matijasevich A. (2017). Gestational age at birth and behavioral problems from four to 11 years of age: Birth cohort study. BMC Pediatrics, 17(1), 184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott A. J., Sharpe L., Loomes M., Gandy M. (2020). Systematic review and meta-analysis of anxiety and depression in youth with epilepsy. Journal of Pediatric Psychology, 45, 133–144. [DOI] [PubMed] [Google Scholar]
- Sjöberg R.L., Nilsson K.W., Leppert J. (2005). Obesity, shame, and depression in school aged children: A population-based study. Pediatrics, 116, 389–392. [DOI] [PubMed] [Google Scholar]
- Son S. E., Kirchner J. T. (2000). Depression in Children and Adolescents. American Family Physician, 15, 2297–2308. [PubMed] [Google Scholar]
- Spence S. H., Najman J. M., Bor W., O'Callaghan M. J., Williams G. M. (2002). Maternal anxiety and depression, poverty and marital relationship factors during early childhood as predictors of anxiety and depressive symptoms in adolescence. Journal of Child Psychology and Psychiatry, 43, 457–469. [DOI] [PubMed] [Google Scholar]
- Splett J. W., Garzona M., Gibson N., Wojtalewicz D., Raborn A., Reinke W. M. (2019). Teacher recognition, concern, and referral of children’s internalizing and externalizing behavior problems. School Mental Health, 11, 1–12. [Google Scholar]
- Sprafkin J., Gadow K. D., Salisbury H., Schneider J., Loney J. (2002). Further evidence of reliability and validity of the child symptom inventory-4: Parent checklist in clinically referred boys. Journal of Clinical Child & Adolescent Psychology, 31, 513–524. [DOI] [PubMed] [Google Scholar]
- Suzuki Y., Ikeda A., Maruyama K., Sakamoto N., Wada H., Tanigawa T. (2020). The association between obesity and hyperactivity/anxiety among elementary school students in Japan. International Journal of Behavioral Medicine, 27(1), 79–86. [DOI] [PubMed] [Google Scholar]
- Theunissen S., Rieffe C., Kouwenberg M., Soede W., Briaire J. J., Frijns J. (2011). Depression in hearing-impaired children. International Journal of Pediatric Otorhinolaryngology, 75, 1313–1317. [DOI] [PubMed] [Google Scholar]
- Van Gent T., Goedhart A. W., Hindley P. A., Treffers P. D. (2007). Prevalence and correlates of psychopathology in a sample of deaf adolescents. Journal of Child Psychology and Psychiatry, 48, 950–958. [DOI] [PubMed] [Google Scholar]
- Varela R. E., Niditch L. A., Hensley-Maloney L., Moore K. W., Creveling C. C., Jones K. M. (2019). Culture specific influences on anxiety in Latino youth. Child & Youth Care Forum, 48(1), 1–17. [Google Scholar]
- Wechsler D. (2009). The Wechsler Individual Achievement Test-III. Pearson Assessment. [Google Scholar]
- Wong H. S., Edwards P. (2013). Nature or nurture: A systematic review of the effect of socio-economic status on the developmental and cognitive outcomes of children born preterm. Maternal and Child Health Journal, 17, 1689–1700. [DOI] [PubMed] [Google Scholar]
- Wood N. S., Marlow N., Costeloe K., Gibson A. T., Wilkinson A. R. (2000). The EPI Cure Study Group. Neurologic and developmental disability after extremely preterm birth. The New England Journal of Medicine, 343, 378–384. [DOI] [PubMed] [Google Scholar]