Abstract
Introduction
The COVID-19 pandemic has impacted biopsychosocial health and wellbeing globally. Pre-pandemic studies suggest a high prevalence of common mental disorders, including anxiety and depression in South Asian countries, which may aggravate during this pandemic. This systematic meta-analytic review was conducted to estimate the pooled prevalence of anxiety and depression in South Asian countries during the COVID-19 pandemic.
Method
We systematically searched for cross-sectional studies on eight major bibliographic databases and additional sources up to October 12, 2020, that reported the prevalence of anxiety or depression in any of the eight South Asian countries. A random-effects model was used to calculate the pooled proportion of anxiety and depression.
Results
A total of 35 studies representing 41,402 participants were included in this review. The pooled prevalence of anxiety in 31 studies with a pooled sample of 28,877 was 41.3% (95% confidence interval [CI]: 34.7–48.1, I2 = 99.18%). Moreover, the pooled prevalence of depression was 34.1% (95% CI: 28.9–39.4, I2 = 99%) among 37,437 participants in 28 studies. Among the South Asian countries, India had a higher number of studies, whereas Bangladesh and Pakistan had a higher pooled prevalence of anxiety and depression. No studies were identified from Afghanistan, Bhutan, and Maldives. Studies in this review had high heterogeneity, high publication bias confirmed by Egger's test, and varying prevalence rates across sub-groups.
Conclusion
South Asian countries have high prevalence rates of anxiety and depression, suggesting a heavy psychosocial burden during this pandemic. Clinical and public mental health interventions should be prioritized alongside improving the social determinants of mental health in these countries. Lastly, a low number of studies with high heterogeneity requires further research exploring the psychosocial epidemiology during COVID-19, which may inform better mental health policymaking and practice in South Asia.
Keywords: COVID-19, Mental health, Anxiety, Depression, South Asia, Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, Sri Lanka, Psychiatry, Epidemiology
COVID-19; Mental health; Anxiety; Depression; South Asia; Afghanistan; Bangladesh; Bhutan; India; Maldives; Nepal; Pakistan; Sri Lanka; Psychiatry; Epidemiology.
1. Introduction
Novel coronavirus disease 2019 (COVID-19) is an acute respiratory illness caused by a newly discovered SARS-CoV-2 virus that emerged in December, 2019 [1,2]. The rapid spread of this disease critically impacted health and wellbeing globally, which was declared as a pandemic by the World Health Organization (WHO) on March 11, 2020 [3]. The sudden outburst of this highly infectious disease presented an unprecedented burden on mortality and morbidity across global nations [1]. In addition, healthcare systems and economies have been struggling to overcome the challenges imposed by this pandemic. To slow down the spread of this relatively unknown virus, countries have implemented several strategies such as quarantine, social distancing, stay at home orders, lockdowns, and border closures [4, 5]. While the clinical care practitioners and public health experts have been focusing on containing the spread of the virus, the COVID-19 pandemic and related quarantine measures have taken a heavy toll on people's mental health and wellbeing [6, 7, 8, 9].
Several studies conducted on people's mental health during lockdown or isolation reported restriction of movement showed that when people are restricted to a certain kind of environment, their mental health is adversely affected [10, 11, 12, 13]. Historically, quarantine has been related to psychological outcomes such as anxiety, depression, panic, irritability, somatic disorder, and insomnia [14]. These measures, as well as the fear and uncertainty related to the disease especially perceived susceptibility, treatment and control measures, exposure to misinformation in media regarding COVID-19, social isolation and loneliness, and economic hardships, have contributed to the adverse impact on the mental health of the population [9, 15]. Previous studies also suggest that the emergency health crisis has a debilitating effect on the mental health of the general population [16, 17, 18]. For example, reports of depression, anxiety, panic attacks, as well as suicidal ideation increased during the SARS and Ebola outbreak [19], where the reported rates of depression in the general population varied between 3% and 73.10% [20].
Recent studies have similarly shown that COVID-19 has affected mental health outcomes such as anxiety, depression, and post-traumatic stress symptoms [6, 7, 9]. Studies conducted in China in the early phase of COVID-19 found that the pandemic-affected individuals had a wide range of adverse psychological impacts of COVID-19 [21, 22, 23, 24, 25]. A recent meta-analysis by Salari et al., reported that the prevalence of stress 29.6%, the prevalence of anxiety 31.9%, and the prevalence of depression 33.7% globally [6]. Health professionals, older adults, and those with preexisting psychological disorders, especially vulnerable to these poor mental health outcomes [7, 9]. The growing psychosocial burden associated with COVID-19 pandemic is reported in recent systematic reviews highlighting evidence that has been synthesized from primary studies globally [26, 27].
Developing countries, especially countries in South Asia, are already struggling to combat the high mortality and morbidity rates caused by COVID-19 due to a highly dense population and low-resource settings [28]. In such situations, the mental health service takes a backseat even though there has been an increase in the demand for mental health services [29, 30]. Despite substantial evidence, there has been negligence in identifying people with mental health illnesses who have been impacted by the pandemic, especially in resource-poor countries [31, 32]. This is manifested in the lack of mental health service availability in developing countries during this outbreak. According to the World Health Organization, 80% of the developed countries are offering mental health services using telemedicine and teletherapy, whereas less than 50% of the developing countries are providing such services during the pandemic [33].
In South Asia, pre-pandemic studies suggest a high burden of mental health disorders in this region with limited access to mental health services [34, 35, 36, 37]. Previous systematic reviews of the prevalence of mental health disorder in South Asian countries suggest high prevalence rates for mental disorders, including depression, anxiety, mood disorders, suicidal behavior and self-harm, schizophrenia, substance use disorders, and other mental health problems [38, 39]. However, there is a lack of synthesized evidence on the regional and country-level estimates on the burden of common mental disorders such as anxiety and depression during the pandemic, where 150–200 million people in this region were suffering from mental disorders prior to COVID-19 pandemic [40].
We aimed to address this knowledge gap and conducted a quantitative systematic review to estimate the pooled prevalence of anxiety and depression in South Asia during COVID-19. The evidence synthesized in this review will provide an overview of the prevalence of depression and anxiety, which may inform better decision-making and future research on mental health in South Asia.
2. Methodology
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [41].
2.1. Data sources and search strategy
We conducted a comprehensive literature search in Medline, Embase, American Psychological Association (APA) PsycInfo, Academic Search Ultimate, Health Source Nursing/Academic Edition, Health Policy Reference Center, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Web of Science databases using the search query provided in Table 1. In each database, those keywords were searched using Boolean operators within the titles, abstracts, keywords, and subject headings (for example, MeSH terms). As this review aimed to focus on COVID-19, the search timeframe was set between 2019 and 2020. The preliminary search was conducted on August 16, 2020, and updated on October 12, 2020. In addition, we searched Google Scholar and reached out to mental health researchers in South Asia to identify relevant articles. Lastly, we also searched the bibliographies references of relevant articles to find additional studies that may fit this review.
Table 1.
Search strategy used in this systematic review and meta-analysis.
| Search query | Search topic | Search keywords (titles, abstracts, and subject headings) with Boolean operators |
|---|---|---|
| 1 | Exposure/Context | “Coronavirus” OR “COVID-19” OR “SARS-CoV-2” OR “2019-nCoV” |
| 2 | Outcome of interest | “Depression” OR “Depressive symptoms” OR “Depressive disorder∗” OR “Anxiety” OR “Social Anxiety” or “Social Phobia” OR “Anxiety disorder∗” |
| 3 | Epidemiological phenomenon | “Prevalence” OR “Incidence” OR "rate∗" OR "ratio∗" OR “Epidemiolog∗” OR “risk factor∗” OR “relative risk” OR “odds ratio” OR “risk ratio” OR “disease burden” |
| 4 | Population of interest | “Afghan∗” OR “Bangladesh∗” OR “Bhutan∗” OR “India∗” OR “Maldiv∗” OR “Nepal∗” OR “Pakistan∗” OR “Sri Lanka∗” OR “South Asia∗” |
| Final search query | Intersection of four topics | 1 AND 2 AND 3 AND 4 |
2.2. Selection criteria
We included studies if they met the following criteria:
-
a)
cross-sectional by design,
-
b)
reported the prevalence of depression or anxiety during COVID-19,
-
c)
measured depression or anxiety using any validated measurement tools or scales,
-
d)
included participants from any of the eight South Asian countries, and
-
e)
published as peer-reviewed articles in the English language.
We excluded articles that did not meet any of these primary criteria. Also, we considered original articles, short communications, and research letters that reported the methodology of the respective studies. Therefore, review articles or commentaries that did not present empirical findings with methodology were excluded from this review. Moreover, we excluded preprints that were not published as peer-reviewed journal articles. Also, we excluded studies that included people with pre-existing mental disorders or specialized population groups (for example, prison population), or focused on South Asian participants living abroad. Such studies were excluded as they may not reflect the burden of depression or anxiety during COVID-19 among people living in the South Asian region.
2.3. Study selection
Two authors independently reviewed the titles and abstracts of the retrieved studies. At the end of the primary screening, conflicts in terms of eligibility of any citation were addressed through discussion with a third author. Citations that appeared to be eligible were selected for the full-text evaluation. Further, full-text articles meeting all criteria of this review were retained for data extraction and subsequent analyses.
2.4. Data extraction
A data extraction form was prepared in Microsoft Excel to extract and record data-fields from the finally recruited articles. Data on the following variables were extracted: author information, year of publication, study design, response rate, recruitment strategy, sampling method, sample size and socio-demographic characteristics, assessment tools with cut-off values, and the prevalence of anxiety or depression in the respective study. Two authors independently extracted data from each article. Two separate datasets were reviewed and evaluated to unify addressing potential inconsistencies by another author at the end of the data extraction process.
2.5. Quality assessment of the reviewed studies
In this review, we used a modified version of the Newcastle-Ottawa Quality Assessment Scale adapted for cross-sectional studies, which has been used in similar meta-analyses previously [7, 42]. This scale assessed the quality of cross-sectional studies in the following domains:
-
1)
representativeness of the study (whether the study included all eligible participants or used random sampling approaches ensuring the representativeness of the study population),
-
2)
justified sample size (provided justification for the chosen sample size through theoretical and statistical measures),
-
3)
response rate (equal or more than 80%),
-
4)
used validated measurement tools with appropriate cut-offs,
-
5)
reported adequate statistics for the study findings.
A positive response in each domain could receive 1 point; thus, the total score could range from 0 to 5 on this modified scale. Studies receiving equal or more than 3 points were graded to have a low risk of bias, whereas studies with less than 3 points were regarded to have a high risk of bias according to this scale.
2.6. Statistical analyses
We performed meta-analyses using Open Meta Analyst [43] and StatsDirect [44] software packages. First, we transformed the proportion values from individual studies using the Freeman-Tukey double arcsine method for prevalence pooling, which prevented the variance instability for prevalence values near 0% or 100% [45]. Moreover, this method suppressed the confidence intervals (CI) from extending beyond 0% and 100%. Further, we used a generic inverse-variance method with a random-effects model to calculate the pooled prevalence from multiple studies [46]. The random-effects model aims to generalize the findings assuming that the studies are random samples from a larger population [47]. The Cochrane's Q-test was used to assess heterogeneity at the significance level of p < .1. Also, we used the I2 statistics to categorize heterogeneity as low (25%–50%), moderate (51%–75%), and high (above 75%) [48].
2.7. Subgroup analyses
Subgroup analyses are helpful to assess between-group variations of the prevalence as well as examine potential sources of heterogeneity across studies. We performed subgroup analyses by country, gender, populations, quality of the studies, measurement scale, and severity of depression and anxiety.
2.8. Meta-regression
We conducted meta-regression analyses to evaluate the correlations between the study level covariates and the pooled prevalence estimates. We used the mean age, quality of the studies, and the percentage of female participants in meta-regression models. In this meta-analytic review, factors were included in multivariate meta-regression analyses if they were significant at p < .2 level in univariate models.
2.9. Sensitivity analyses
Sensitivity analyses were performed in this meta-analysis to assess the influence of individual studies on the pooled prevalence estimates or heterogeneity. We excluded each study and calculated the pooled prevalence and I2 statistics for the rest of the studies.
2.10. Evaluation of the publication bias
We visually inspected the funnel plots and conducted Egger's regression tests to evaluate the publication bias that may exist and affect the generalizability of the study findings. A p value less than 0.1 was considered as an indication of publication bias in Egger's test.
3. Results
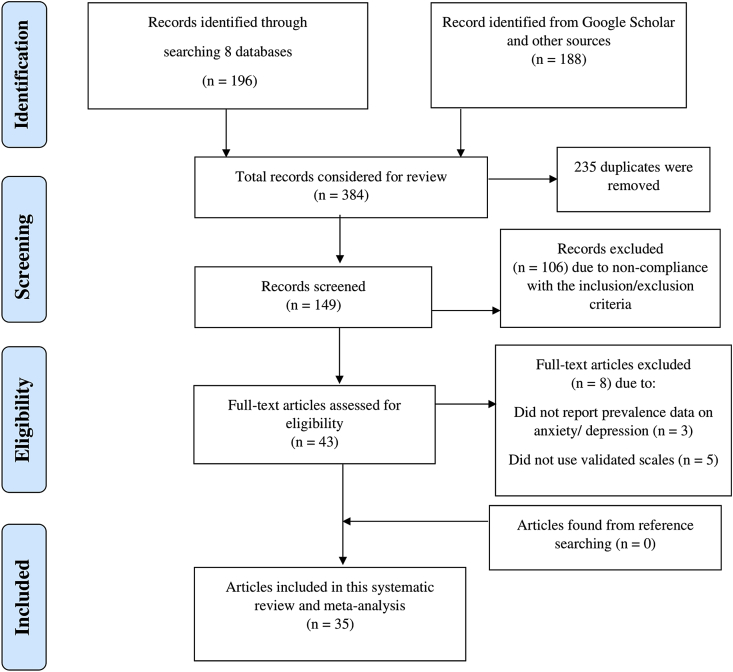
A PRISMA flowchart detailing the literature review process is illustrated in Figure 1. We found a total of 384 citations from selected databases and additional sources. After excluding 235 duplicates, we examined the titles and abstracts of 149 citations using the pre-determined eligibility criteria. At the end of the preliminary screening process, 43 citations were selected for full-text evaluation. Eight articles were excluded that did not meet all criteria. Finally, the remaining 35 articles representing 41,402 participants were retained in this meta-analytic review [49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83].
Figure 1.
Flow diagram of the literature retrieval process.
3.1. Characteristics of the included studies
An overview of the included studies is provided in Table 2. The highest number of studies were conducted in India (n = 19), followed by Bangladesh (n = 7), Pakistan (n = 5), Nepal (n = 3), and Sri Lanka (n = 1). No studies were identified from Afghanistan, Bhutan, and the Maldives. Among the included studies, the sample size ranged from 41 to 10,178. Most studies recruited young adult participants with a mean age of the participants ranging from 25.75 to 42.5 years. The median percentage of female participants was 45.4% among the included studies. Moreover, most studies (n = 29) used online platforms, including email and social media sites, to recruit participants and conduct surveys. Response rates ranged from 33.5% to 97.4% across individual studies. Most studies (n = 18) in this review recruited healthcare providers as study participants. Two studies recruited patients, and the remaining 15 studies consisted of general population with different demographic and socioeconomic conditions.
Table 2.
Characteristics of the studies included in this meta-analytic review.
| Authors and publication year | Country | Study design; response rate | Recruitment strategy; sampling method | Sample size and characteristics | Mean age with SD | Female (%) | Education and occupation | Assessment scale/tools and cut-off values | Prevalence of anxiety/depression |
|---|---|---|---|---|---|---|---|---|---|
| Ahmad et al. (2020) [49] | India | Cross-sectional; NR | Online; random | 392; general population | 30.3 (±9.28) | 47.2 | Graduate and above 91.9; student 41.3%, Service holders 43.2% | GAD-7 (>10) | Anxiety: 25.3% |
| Ahmed et al. (2020) [50] | Bangladesh | Cross-sectional; NR | Online; NR | 500; general population | 25.95 | 32.3 | Student 65.3%, service holders 25% | DASS-21 (Anxiety >4, Depression >5) | Anxiety: 39.8%; Depression: 43% |
| Amin et al. (2020) [61] | Pakistan | Cross-sectional; NR | Online; NR | 389; healthcare providers | 35 (Median) | 48.33 | Physician trainees 74.3%, post-graduate qualification 25.7%; front-line physicians | SRQ- 20 (>8) | Anxiety/depression: 43% |
| Banna et al. (2020) [72] | Bangladesh | Cross-sectional; NR | Online; convenience sampling | 1427; general population | 25.75 | 28.5 | Undergraduate 59% and graduate 28.3%; students 43.7%, Service holders 42.2% | DASS-21 (Anxiety >6, Depression >9) | Anxiety: 57.9%; Depression: 33.7% |
| Chatterjee et al. (2020) [78] | India | Cross-sectional; NR | Online; NR | 152; healthcare providers | 42.05 (±12.19) | 21.7 | Post-graduate 63.2% and graduate 34.2%; Government doctor 66.4%, Non-government doctors 33.6% | DASS-21 | Anxiety: 39.5%; Depression: 34.9% |
| Chew et al. (2020)a [80] | India | Cross-sectional; 33.5% | NR | 384; healthcare provider | 27.7 | 65.4 | physicians 21.95, nurses 43.5%, other non-medical staff 10.8%. | DASS-21 (Anxiety >7, Depression >9) | Anxiety/depression 0.8% |
| Chew et al. (2020)b [79] | India | Cross-sectional; 90.6% | NR | 426; healthcare provider | 29 | 64.3 | Mostly physicians and Nurses | DASS-21 (Anxiety >7, Depression >9) | Anxiety: 17.1%; Depression: 12.4% |
| Desai et al. (2020) [81] | India | Cross-sectional; NR | Online; snowball sampling | 1537; general population | 77.7% below 30 years | 50 | Undergraduate 61.9%; students 67.5%, working professionals 32.5% | GAD-7 (Anxiety >5); PHQ-9 (Depression >5) | Anxiety: 41.5%; Depression 47% |
| Grover et al. (2020) [82] | India | Cross-sectional; 90.05% | Online; NR | 1685; general population | 41.26 | 36.3 | Graduate and above 93.8%; healthcare worker 47.1%, Service holder 11.4%, Businessperson 10%, Student 0.6% | GAD-7 (Anxiety ≥5); PHQ-9 (Depression ≥10) | Anxiety: 38.2%; Depression 10.5% |
| Gupta AK et al. (2020) [83] | Nepal | Cross-sectional; NR | Online; snowball sampling | 150; healthcare providers | 29.5 | 52.7 | Graduate and above 52%; nursing staff 31.3 %, faculty members 24.7 % | GAD-7 (Anxiety ≥5); PHQ-9 (Depression ≥10) | Anxiety: 34%; Depression: 10% |
| Gupta S. et al. (2020)a [52] | India | Cross-sectional; 79.44% | Online; Quota sampling | 1124; healthcare providers | Mostly 20–35 years | 36.1 | Undergraduate degree 39.1%, graduate and above 59.5%; Doctors 66.6%, Nurses 18.4, paramedics 12%. | HADS (>7) | Anxiety: 37.2%; Depression 31.4% |
| Gupta S. et al. (2020)b [51] | India | Cross-sectional; 85.7% | Online; NR | 749; healthcare providers | Mostly 20–35 years | 25.8 | Undergraduate 24.6%, graduate and above 75.4%; Physicians 100% | HADS (>7) | Anxiety: 35.2%; Depression: 28.2% |
| Hasan et al. (2020) [53] | Pakistan | Cross-sectional; NR | Online; NR | 151; healthcare providers | 29 (±7.28) | 56.3 | Undergraduate degree 76.2% postgraduate degree 23.8%; Physicians 100% | GAD-7 (≥5) | Anxiety: 63.58% |
| Hossain et al. (2020) [54] | Bangladesh | Cross-sectional; NR | Online; NR | 880; general population | 26.3 (±7.2) | 30 | Undergraduate 34.1%, graduate and above 34.8%; Students 56%, Service holder 31% | GAD-7 (≥10) | Anxiety: 49.1% |
| Imran et al. (2020)a [56] | Pakistan | Cross-sectional; NR | Online; NR | 337; healthcare providers | 30.4 (±6.7) | 53 | Physicians 79%, nurses and paramedical staff 20% | GAD-7 (Anxiety >7), PHQ-9 (Depression ≥10) | Anxiety 36.2%; Depression 30% |
| Imran et al. (2020)b [55] | Pakistan | Cross-sectional; 88.6% | Online; NR | 10178; healthcare providers | 31.5 | 56.7 | Postgraduate trainees 100% | GAD-7 (Anxiety >5), PHQ-9 (Depression ≥8) | Anxiety: 22.6%; Depression: 26.4% |
| Islam et al. (2020)a [57] | Bangladesh | Cross-sectional; NR | Online; snowball sampling | 476; general population | Mostly 21–24 years | 32.8 | University student 100% | GAD-7 (Anxiety ≥5), PHQ-9 (Depression ≥5) | Anxiety: 81.7%; Depression: 82.4% |
| Islam et al. (2020)b [58] | Bangladesh | Cross-sectional; 97.4% | Online; NR | 1311; general population | 23.54 | 39.6 | Undergraduate degree 68.6%; students 81.6% | GAD-7 (≥10) | Anxiety: 37.3% |
| Jain et al. (2020) [59] | India | Cross-sectional; NR | Online; NR | 512; healthcare providers | Mostly <35 years | 44.3 | Anesthesiology residents 68.4%, consultants 31.6% | GAD-7 (≥5) | Anxiety: 74.2% |
| Khanal et al. (2020) [62] | Nepal | Cross-sectional; NR | Online; NR | 475; healthcare providers | 28.20 (±5.80) | 52.6 | Undergraduate 58.3%, graduate and above 21.9%; Nurses 35.2, Doctors 33.9% | HADS (>7) | Anxiety: 41.9%; Depression 37.5% |
| Khanna et al. (2020) [60] | India | Cross-sectional; NR | Online; NR | 2355; healthcare providers | 42.5 | 43.3 | Ophthalmology resident 15.2%, government doctor 12.8%, private practitioner 52.1%, Non-government doctor 19.9%. | PHQ-9 (≥5) | Depression: 32.6% |
| Mamun et al. (2020) [63] | Bangladesh | Cross-sectional; 91.52% | Online; NR | 10067; general population | 29.9 (±9.6) | 43.9 | Tertiary education 80.8%; 58.4% students, 25.7% employed,3.6% unemployed | PHQ-9 (≥10) | Depression: 33.3% |
| Mani et al. (2020) [64] | India | Cross-sectional; NR | Online; snowball sampling | 618; general population | NR | 43 | Graduate and above 67%; student 31%, healthcare worker 20%, service holder 21.9%, Businessperson 3.5% | GAD-7 (≥5) | Anxiety: 19.4% |
| Nisha S. et al. (2020) [65] | India | Cross-sectional; NR | N/R; convenience sampling | 359; general population | Mostly 18–21 years | 49.6 | Medical Students 100% | GAD-7 (Anxiety ≥5); CES-D (Depression ≥5) | Anxiety: 75.5%; Depression: 74.6% |
| Patabendige et al. (2020) [66] | Sri Lanka | Cross-sectional; NR | In-person; quota sampling | 257; pregnant participants | 29.2 (±5.8) | 100 | N/R | HADS (≥8) | Anxiety 17.5%; Depression: 19.5% |
| Reddy et al. (2020) [67] | India | Cross-sectional; NR | Online; respondent-driven sampling | 891; general population | Mostly 21–40 years | 47 | Graduate and above 94%; 34% students, employed 53%, others 8% | DASS-21 | Anxiety: 15%; Depression: 22% |
| Sandesh et al. (2020) [68] | Pakistan | Cross-sectional; NR | Online; NR | 112; healthcare providers | N/R | N/R | N/R | DASS-21 | Anxiety: 85.7%; Depression: 72.3% |
| Sebastian et al. (2020) [69] | India | Cross-sectional; NR | online | 1257; general population | 29.3 | 54.4 | Students 39%, employed 33.1%, unemployed 13.1% | PHQ-4 (Depression ≥3, Anxiety ≥9) | Anxiety: 20%, Depression: 18% |
| Sharma et al. (2020) [70] | India | Cross-sectional; NR | Landline | 62; Patients | 34.05 | 25.8 | Student-33.9%, Businessman- 17.7%, Housewife- 16.1%, Daily wage worker- 12.9% | CES-D (≥10) | Depression: 62.9% |
| Shrestha et al. (2020) [71] | Nepal | Cross-sectional; NR | N/R; convenience sampling | 101; healthcare providers | N/R | 57.4 | Doctors 59.4%, Nurses 40.6% | GAD-7 | Anxiety: 73.3% |
| Sil et al. (2020) [73] | India | Cross-sectional; NR | Online; snowball sampling | 41; healthcare providers | Mostly 26–30 years | 41.5 | Frontline dermatologists 100%. Postgraduate trainee 51.22% senior resident 29.27%, consultant 19.51% | PHQ-9 | Depression: 26.82% |
| Suryavanshi et al. (2020) [74] | India | Cross-sectional; NR | Online; snowball sampling | 197; healthcare providers | Mostly <30 years | 51.27 | 24% nurses, 34% physicians, 29% residents/interns and 13% others. | PHQ-9 (Depression: ≥5), GAD (Anxiety: ≥5) | Anxiety: 50%; Depression: 47% |
| Verma et al. (2020) [75] | India | Cross-sectional; 93.9% | Online; convenience sampling | 354; general population | Mostly 18–25 years | 48.3 | Graduate and above 91.8%; employed 39.5%, unemployed 60.5% | DASS-21 (Anxiety >7, Depression >9) | Anxiety: 27.96%; Depression: 25.14% |
| Wilson et al. (2020) [76] | India | Cross-sectional; NR | Online; NR | 350; healthcare providers | 30.21 | 46.6 | 84.3% doctors, 15.7% nurses. | GAD-7 (Anxiety ≥5, PHQ-9 (Depression ≥10) | Anxiety: 66.29%; Depression: 49.43% |
| Zubayer et al. (2020) [77] | Bangladesh | Cross-sectional; NR | Online; NR | 1146; general population | 26.38 | 40.8 | Graduate and above 78.5%; student 58.6%, housewife 3.9%, govt./private employee 16.6%, doctor/health worker 12.7%, and unemployed 8.2%. | DASS-21 (Anxiety ≥10, Depression ≥14) | Anxiety 46%; Depression 47.2% |
Note: NR: Not reported, GAD-7: Generalized Anxiety Disorder 7-item, DASS-21: Depression, Anxiety and Stress Scale - 21 Items, HADS: Hospital Anxiety and Depression Scale, PHQ-4: Patient Health Questionnaire-4, PHQ-9: Patient Health Questionnaire (PHQ)-9, SRQ-20: Self Reporting Questionnaire 20-items, CES-D: Center for Epidemiologic Studies Depression Scale.
In the Newcastle-Ottawa Quality Assessment, 24 studies were identified to have a high risk of bias, whereas 11 studies had a low risk of bias with a quality score of 3 and above (Supplementary file A). The prevalence rates of anxiety and depression were calculated using separate meta-analyses, including meta-regression, sub-group estimates, sensitivity analyses, and assessments of publication bias.
3.2. Prevalence of anxiety during COVID-19 in South Asia
3.2.1. Pooled prevalence of anxiety
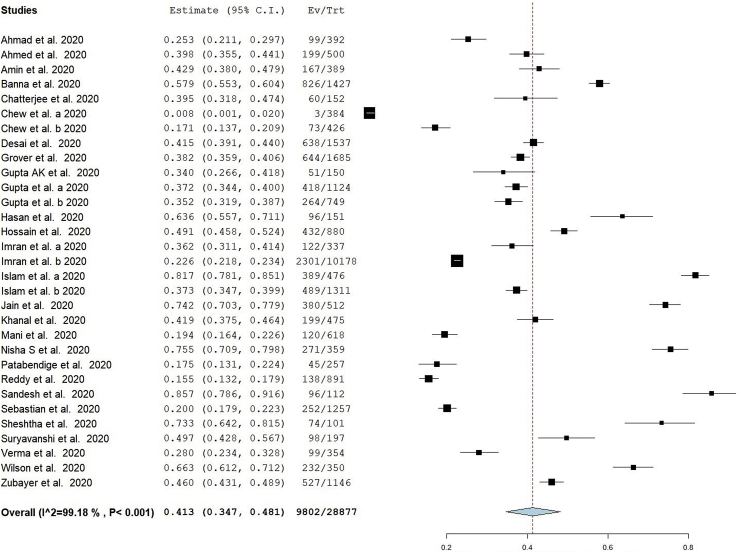
A total of 31 studies reported the prevalence of anxiety during COVID-19 in different samples from South Asian countries [49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 61, 62, 64, 65, 66, 67, 68, 69, 71, 72, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83]. These studies used different scales to measure anxiety in respective samples, including the Generalized Anxiety Disorder 7-item (GAD-7) scale (n = 16), Depression, Anxiety and Stress Scale - 21 Items (DASS-21) scales (n = 9), Hospital Anxiety and Depression Scale (HADS) (n = 4), Patient Health Questionnaire-4 (PHQ-4) (n = 1), and Self Reporting Questionnaire 20-items (SRQ-20) scale (n = 1). These scales were used with different cut-off values to determine the overall prevalence as well as the severity of anxiety. In random-effects model, the pooled prevalence of anxiety was 41.3% (95% CI: 34.7–48.1, I2 = 99.18%) among 28877 participants in 31 studies (Figure 2).
Figure 2.
Forest plot of the pooled prevalence of anxiety.
3.2.2. Meta-regression and subgroup analyses
The pooled prevalence of anxiety was significantly associated with the percentage of female participants in respective studies (p = .04) (Supplementary file B). Moreover, there was no correlation between the pooled prevalence and mean age of the participants (p = .98) or the quality score of the studies (p = .47). The subgroup analyses revealed different prevalence estimates in pooled samples (Table 3). The pooled prevalence of anxiety was higher (46.49%, 95% CI: 36.99–56.6, I2 = 98.5%) among female participants compared to the male participants (41.13%, 95% CI: 32.99–49.51, I2 = 98.6%).
Table 3.
Subgroup analyses of the prevalence of anxiety and depression.
| Groups | Subgroups | Anxiety | Depression |
|---|---|---|---|
| Gender | Female | 46.49%, 95% CI: 36.55–56.6 | 37.8%, 96% CI: 31.7–44.1 |
| I2 = 98.5% | I2 = 97.8% | ||
| Male | 41.13%, 95% CI: 32.99–49.51 | 36.7%, 95% CI: 29.97–43.6 | |
| I2 = 98.6% | I2 = 98.6% | ||
| Country | Bangladesh | 52.3%, 95% CI: 41–63.6 | 48.2%, 95% CI: 34.8–61.8 |
| I2 = 98.67% | I2 = 99.3% | ||
| India | 34.7%, 95% CI: 25.4–44.7 | 30.7%, 95% CI: 22.3–39.8 | |
| I2 = 99.13% | I2 = 99.05% | ||
| Nepal | 49.6%, 95% CI: 30.6–68.7 | 20.9%, 95% CI: 1.2–55.3 | |
| I2 = 95.45% | I2 = 98.42% | ||
| Pakistan | 50.4%, 95% CI: 30.5–70.2 | 41.6%, 95% CI: 27.5–56.4 | |
| I2 = 99% | I2 = 97.92% | ||
| Population Groups | General population | 40.7%, 95% CI: 31.6–50.1 | 39%, 95% CI: 29–49.5 |
| I2 = 99.15% | I2 = 99.44% | ||
| Healthcare providers | 43.6%, 95% CI: 33.1–54.5 | 29.9%, 95% CI: 23.9–36.2 | |
| I2 = 99.15% | I2 = 98.12% | ||
| Scales | GAD-7 (Anxiety), PHQ-9 (Depression) | 49.2%, 95% CI: 39.1–59.3 | 34.7%, 95% CI: 27.1–42.7 |
| I2 = 99.34% | I2 = 99.31% | ||
| DASS-21 | 34.2%, 95% CI: 19.2–51 | 29.8%, 95% CI: 18.3–42.7 | |
| I2 = 99.35% | I2 = 98.95% | ||
| HADS | 32.8%, 95% CI: 25.1–41 | 29.2%, 95% CI: 23.6–35.1 | |
| I2 = 94.39% | I2 = 89.89% | ||
| Risk of bias | Studies with low risk of bias | 36%, 95% CI: 20.4–53.2 | 23.8%, 95% CI: 14.6–34.5 |
| I2 = 99.26% | I2 = 99% | ||
| Studies with high risk of bias | 43.9%, 95% CI: 36.4–51.6 | 38.5%, 95% CI: 31.6–45.7 | |
| I2 = 99.19% | I2 = 99.05% | ||
| Severity | Mild | 27.24%, 95% CI: 19.38–35.89 | 25.11%, 95% CI: 17.72–33.29 |
| I2 = 99.3% | I2 = 99.3% | ||
| Moderate | 14.68%, 95% CI: 12.3–17.22 | 13.91%, 95% CI: 11.13–16.95 | |
| I2 = 94.7% | I2 = 96.6% | ||
| Severe | 9.94%, 95% CI: 7.09–13.2 | 11.97%, 95% CI: 8.29–16.2 | |
| I2 = 97.6% | I2 = 98.5% |
Among the South Asian countries reporting the prevalence of anxiety, Bangladesh had the highest prevalence (52.3%, 95% CI: 41–63.6, I2 = 98.67%) followed by Pakistan (50.4%, 95% CI: 30.5–70.2, I2 = 99%), Nepal (49.6%, 95% CI: 30.6–68.7, I2 = 95.45%), and India (34.7%, 95% CI: 25.4–44.7, I2 = 99.13%). Moreover, the pooled prevalence of anxiety among the healthcare providers was 43.6% (95% CI: 33.1–54.5, I2 = 99.15%), whereas general population had a prevalence of 40.7% (95% CI: 31.6–50.1, I2 = 99.15).
Furthermore, the prevalence of anxiety varied across samples that were assessed using different scales. The prevalence of anxiety was higher (49.2%, 95% CI: 39.1–59.3, I2 = 99.34%) in GAD-7 scale compared to samples that were assessed by DASS-21 (34.2%, 95% CI: 19.2–51, I2 = 99.35%) and HADS (32.8%, 95% CI: 25.1–41, I2 = 94.39%) scales. Also, studies with high risk of bias according to the Newcastle-Ottawa Quality Assessment has a higher prevalence (43.9%, 95% CI: 36.4–51.6, I2 = 99.19%) compared to studies with low risk of bias (36%, 95% CI: 20.4–53.2, I2 = 99.26%).
The prevalence of anxiety varied across subgroups based on the severity of symptoms among the participants. The prevalence was highest for mild anxiety (27.24%, 95% CI: 19.38–35.89, I2 = 99.3%) followed by moderate (14.68%, 95% CI: 12.3–17.22, I2 = 94.7%) and severe anxiety (9.94%, 95% CI: 7.09–13.2, I2 = 97.6%).
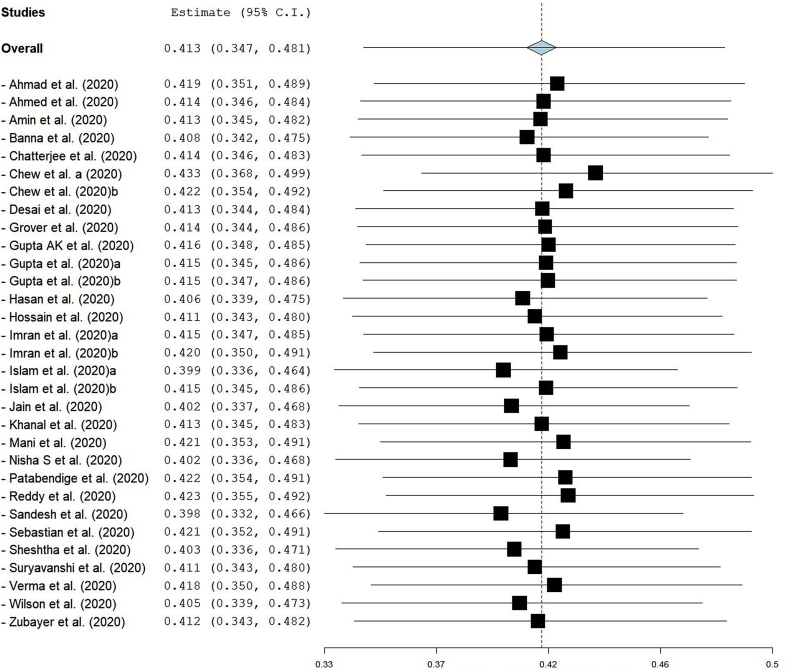
3.2.3. Sensitivity analysis and publication bias
In the sensitivity analysis, the lowest prevalence (39.8%, 95% CI: 33.2–46.6) was observed after excluding the study by Sandesh and colleagues [68], whereas the highest prevalence (43.3%, 95% CI: 36.8–49.9) was found after excluding a study by Chew and colleagues [80]. The exclusion of each study one-by-one from the meta-analytic model did not change the pooled prevalence of anxiety substantially (Figure 3). The visual inspection of the funnel plot revealed high publication bias (Supplementary file D), which was confirmed by Egger's test (p = .0002).
Figure 3.
Sensitivity analysis (leave one out) for studies reporting anxiety prevalence.
3.3. Prevalence of depression during COVID-19 in South Asia
3.3.1. Pooled prevalence of depression
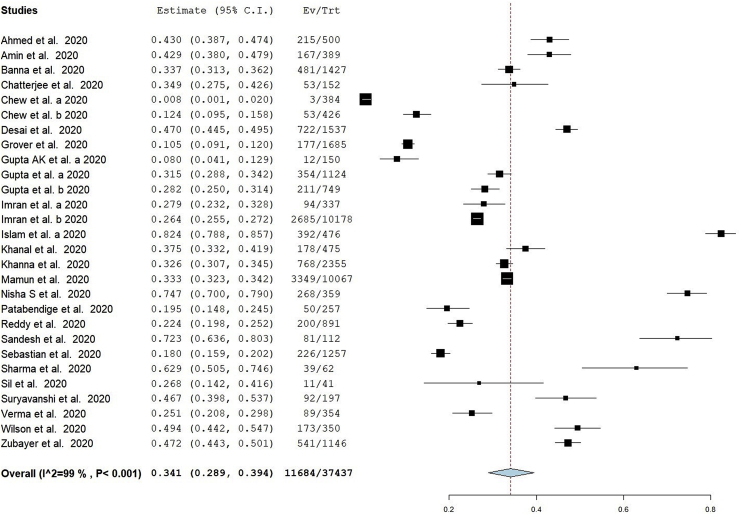
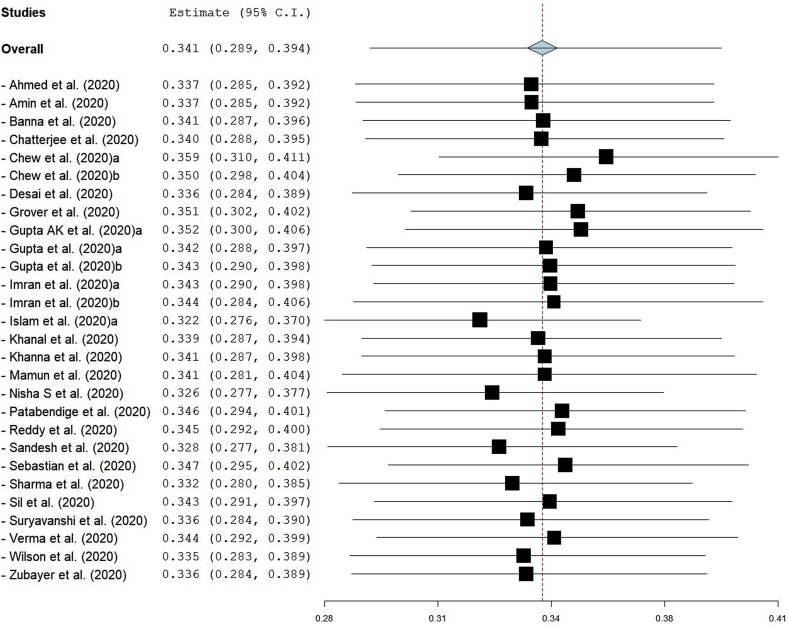
Twenty-eight studies reported the prevalence of depression during COVID-19 in different samples from South Asian countries [50, 51, 52, 55, 56, 57, 60, 61, 62, 63, 65, 66, 67, 68, 69, 70, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83]. The Patient Health Questionnaire (PHQ)-9 was the most frequently used instrument (n = 11), followed by Depression, Anxiety and Stress Scale - 21 Items (DASS-21) scales (n = 9), Hospital Anxiety and Depression Scale (HADS) (n = 4), Center for Epidemiologic Studies Depression Scale (CES-D) (n = 2), Patient Health Questionnaire-4 (PHQ-4) (n = 1), and Self Reporting Questionnaire 20-items (SRQ-20) scale (n = 1). These scales had different constructs measuring overall depression and the severity of the symptoms using multiple cut-off values. The pooled prevalence of depression was 34.1% (95% CI: 28.9–39.4, I2 = 99%) among 37437 participants in 28 studies (Figure 4).
Figure 4.
Forest plot of the pooled prevalence of depression.
3.3.2. Meta-regression and subgroup analyses
In meta-regression analyses, the prevalence of depression was not significantly associated with the mean age of the participants (p = .784) and the quality scores of the studies (p = .48) (Supplementary file C). However, the percentage of female participants was significantly associated (p = .03) with the prevalence of depression. Moreover, gender was not a significant moderator according to the subgroup analyses (Table 3). The prevalence was similar among male (36.7%, 95% CI: 29.97–43.6, I2 = 98.6%) and female (37.8%, 95% CI: 31.7–44.1, I2 = 97.8%) participants during COVID-19.
At the country level, Bangladesh had the highest prevalence of depression (48.2%, 95% CI: 34.8–61.8, I2 = 99.3%), followed by Pakistan (41.6%, 95% CI: 27.5–56.4, I2 = 97.92%), India (30.7%, 95% CI: 22.3–39.8, I2 = 99.05%), and Nepal (20.9%, 95% CI: 1.2–55.3, I2 = 98.42%). The prevalence of depression was higher in general population (39%, 95% CI: 29–49.5, I2 = 99.44%) compared to the healthcare providers (29.9%, 95% CI: 23.9–36.2, I2 = 98.12%).
The prevalence of depression varied across commonly used scales. For example, studies with GAD-7 had a higher prevalence (34.7%, 95% CI: 27.1–42.7, I2 = 99.31%), whereas studies with DASS-21 and HADS had similar prevalence (29.8%, 95% CI: 18.3–42.7, I2 = 98.95% vs 29.2%, 95% CI: 23.6–35.1, I2 = 89.89%). Moreover, studies with a high risk of bias had a higher pooled prevalence (38.5%, 95% CI: 31.6–45.7, I2 = 99.05%) compared to studies with a low risk of bias (23.8%, 95% CI: 14.6–34.5, I2 = 99%).
The pooled prevalence was calculated for subgroups based on the severity of depressive symptoms. The prevalence of mild depression was 25.11% (95% CI: 17.72–33.29, I2 = 99.3%), whereas the prevalence of moderate and severe depression was 13.91% (95% CI: 11.13–16.95, I2 = 96.6%) and 11.97% (95% CI: 8.29–16.2, I2 = 98.5%).
3.3.3. Sensitivity analysis and publication bias
We excluded each study one-by-one from the meta-analytic model in the sensitivity analysis. The findings showed no significant changes in the pooled prevalence of depression (Figure 5). The lowest prevalence was observed after excluding a study by Islam and colleagues (32.2%, 95% CI: 27.6–37)57, whereas the highest prevalence was found after excluding a study by Chew and colleagues (35.9%, 95% CI: 31–41.1)80. Furthermore, a high publication bias was observed in the visual assessment of the funnel plot (Supplementary file D)), which was validated by Egger's test results, indicating a significant publication bias (p = .05).
Figure 5.
Sensitivity analysis (leave one out) for studies reporting depression prevalence.
4. Discussion
4.1. Overview and interpretation of the synthesized findings
To the best of our knowledge, this is the first quantitative synthesis of the epidemiological burden of anxiety and depression during the COVID-19 pandemic in South Asian region with country-level estimates. We systematically identified 35 cross-sectional studies and quantitatively evaluated the pooled prevalence in the collective sample alongside estimating the prevalence rates in different sub-groups and populations in this region. The overall prevalence of anxiety and depression was 41.3% and 34.1%, respectively. Moreover, women had a higher prevalence of both disorders (anxiety 46.49%, depression 37.8%) compared to men (anxiety 41.13%, depression 36.7%). The percentage of female percentage was significantly associated with the prevalence of anxiety and depression in this review.
Bangladesh (anxiety 52.3%, depression 48.2%) and Pakistan (anxiety 50.4%, depression 41.6%) had higher prevalence rates compared to other South Asian countries. Furthermore, the prevalence estimates varied among the healthcare providers and general population, studies with different measurement instruments, and subgroups with varying severity of anxiety and depression. Specifically, the prevalence of severe symptoms was critically high (anxiety 9.94%, depression 11.97%) among samples included in this review. The I2 statistics of the pooled estimates ranged from 89.89% to 99.44%, indicating high heterogeneity and inconsistency among studies included in this review. Also, meta-analytic models for anxiety and depression indicated high publication bias. These findings, alongside a high prevalence of those disorders during this pandemic, require a critical assessment of the evidence from multiple perspectives.
During the early months of COVID-19 pandemic, the scientific literature on the psychosocial challenges associated with pandemic was limited compared to the infectious diseases literature [84]. Moreover, a major proportion of the literature was published from China and many western countries that were initially affected by this pandemic [9, 42, 84]. Compared to those regions, studies from South Asia as well as the global south has been limited in number and may not have explored how this pandemic has impacted psychosocial wellbeing in these populations [7, 8, 9]. Therefore, the findings of the available literature may not reflect the accurate burden of anxiety and depression during this pandemic in the South Asian population.
Another perspective on evidence-based mental health may inform that this review only emphasized on cross-sectional evidence that may not inform the psychological impacts that can be attributable to this pandemic alone. As there is a scarcity of cohort studies focusing on mental health problems in South Asia, the available syntheses of previous research reported in epidemiological reviews can offer meaningful insights. An umbrella review of reviews identified 15 reviews that reported a high burden of anxiety and depression in South Asian countries [39]. Moreover, a meta-analytic review found that the prevalence of anxiety, depressive symptoms were 25.8% and 26.8%, respectively [38]. These syntheses of the previous research highlight that anxiety and depression have been highly prevalent in South Asia, which may have aggravated amid the COVID-19 pandemic due to the continued fear of infection, loss of socioeconomic opportunities, impaired the psychosocial processes, and lack of access to mental health resources and services [50, 61, 75].
COVID-19 pandemic has become a major concern for global mental health, which is evident in a growing body of literature examining how this pandemic has impacted mental health and wellbeing in different contexts and populations [6, 7, 8, 42]. The findings of the current review can be compared with the existing reviews that synthesized empirical evidence in other geographic regions and population groups. For example, a meta-analysis of 13 studies reported that the prevalence of anxiety and depression in healthcare providers was 23.2% and 22.8%, respectively. However, this review did not report any studies from South Asian countries. Another meta-analysis of 17 studies assessed mental health problems in general population during COVID-19 and found the prevalence of anxiety and depression as 31.9% and 33.7%, respectively [6]. Our findings are similar to recent systematic reviews that reported an elevated burden of anxiety and depression in pandemic-affected populations groups suggesting a global crisis of mental health problems associated with this pandemic [26, 27]. Furthermore, studies from South East Asian countries suggest a varying prevalence of mental health problems when compared to the current review. Evidence from Vietnam and Philippines inform that the prevalence of mental health problems may range from 3.4% to 28.8% [85, 86]. The variations of psychosocial burden of this pandemic requires a consideration of spatial attributes of mental health problems as well as psychosocial dynamics in different phases of the pandemic in respective contexts [87, 88]. Our review found a comparatively higher prevalence through a quantitative synthesis of 35 studies with samples representing healthcare providers as well as the general population in South Asia, which necessitates further research to elucidate the psychosocial impacts of COVID-19 in South Asian countries.
4.2. Implications for future research
As this review synthesized evidence from cross-sectional studies with any sample size, future research should emphasize on longitudinal studies involving large samples that may provide more generalizable evidence on mental health among South Asian populations. Moreover, 29 out of the 35 included studies deployed an online approach for recruiting study participants and collecting data. Moreover, South Asian countries have a profound digital divide [89, 90]; therefore, people who do not use digital devices or services may not be able to participate in surveys that are administered through internet. Furthermore, rural and marginalized communities may have limited access to digital resources that may systematically exclude them from online participation [91]. Therefore, the current studies may not have included a mass proportion of the general public in respective contexts. Future research should engage different population groups using multipronged sampling and recruitment strategies, ensuring social distancing and infection prevention [9], which may offer the safety of the participants as well as improve the representativeness of those studies.
The use of different scales and cut-off values may impact prevalence estimates [7], which informs the need for using validated scales with uniform cut-off values across populations. It is essential to re-evaluate the items and latent constructs in each scale so that common scales with high reliability and validity can be widely used. Nonetheless, back calculations of different scales or sub-scales can be done if the primarily collected data are publicly available for re-analyses. Psychiatric epidemiological research should adhere to data sharing policies that promote transparency and the use of uniform measures across studies. Such measures are likely to provide better estimations of the epidemiological burden of anxiety and depression at the population level.
In this review, most studies recruited participants with varying educational and occupational levels. However, limited sociodemographic data may not show how people of different levels of education or income may experience psychosocial stressors during this pandemic. For example, a higher prevalence of anxiety among the healthcare providers may reflect the occupational challenges and lived experiences of the fear of COVID-19, whereas unemployed people with education may have altered levels of depression [8, 9, 42]. As COVID-19 has impacted socioeconomic activities in most contexts, such disruptions are likely to affect mental health and wellbeing among the affected occupational groups [92]. In future research, participant-level data with temporal variations in psychosocial measures should be recorded to assess how anxiety and depression may have manifested in different subgroups within the South Asian population.
The existing studies and their syntheses show a high prevalence of anxiety and depression among women in South Asia. Future studies with better participation of women are critical to examine the psychological issues and their determinants that may be associated with gender norms and roles within the context of South Asian countries. Women in these countries have limited autonomy, empowerment, participation in socioeconomic activities, and access to mental health services and resources [93]. It is not clear how preventive measures such as quarantine or lockdown may have affected women's mental health in South Asia. Moreover, gender-based violence is highly prevalent in South Asian countries [94, 95]. Previous research has shown tremendous impacts of oppression and violence on women's psychosocial health [93, 95, 96]. Recent reports suggest a growing burden of domestic violence, which is likely to affect the mental health and wellbeing among South Asian women [97]. Future research should investigate such issues that may not only explore the risk factors of depression and anxiety, but also examine social epidemiology of gender-based violence that may affect immediate and long-term mental health outcomes among women.
This review did not limit the age of the study participants; however, limited evidence on the children or older adults suggests a critical research gap during this pandemic. This gap can be attributable to the sampling strategies (e.g., convenient sampling) and recruitment methods (e.g., circulating survey link through social media) that are likely to engage the young participants rather than children and older adults. Further research is needed to examine mental health status in different age groups that may allow a comparative analysis of psychosocial impacts of this pandemic in respective populations [98, 99]. Moreover, online surveys may engage informal and family caregivers who may facilitate the participation of the children or older adults they live with, which may address the current knowledge gaps on those individuals.
While most studies in this review focused on the general population and healthcare providers, there is a lack of evidence on the prevalence of anxiety and depression among COVID-19 patients and their family caregivers. A study conducted among COVID-19 patients in North India found 62.9% prevalence of depression, suggesting a higher psychological burden in this population [70]. Prospective studies in South Asian countries should focus on these individuals, who may have experienced severe psychosocial distress and adverse mental health conditions during this pandemic.
People with chronic conditions are likely to have adverse health outcomes during COVID-19, which may increase psychological distress and deteriorated mental health outcomes in this pandemic [6, 9]. Also, people with chronic mental disorders may have been disproportionately affected during this pandemic who may have lost access to care and other services [100]. Moreover, coexisting mental disorders among the same individuals may affect the overall health and quality of living [74, 82, 101, 102]. Future research should pay special attentions to investigate anxiety, depression, and other mental health problems among those vulnerable individuals and populations.
Media use and quality of media contents may affect the mental health of individuals and populations amid this pandemic [15]. Misinformation and disinformation from available media sources may create psychological distress, whereas the lack of access to reliable sources may leave individuals with uncertainties regarding this pandemic [103]. Moreover, people confined at home or those with altered work style from home may have been exposed to excessive digital media time or screen use behavior that may influence their mental health [104, 105]. Further research is needed to clarify how the type, duration, contents, and quality of media use can influence anxiety, depression, and other mental health outcomes in South Asian populations.
It is necessary to investigate the social determinants of mental health in South Asia and their trajectories during and after this pandemic. An altered psychosocial state may impact intrapersonal, interpersonal, and community-based psychological processes and outcomes in the population level [57, 75]. Moreover, systematic oppression and repression in socioeconomically marginalized individuals may adversely influence the biopsychosocial processes, resulting in a higher burden of depression and other mental health problems. The high prevalence of anxiety and depression in this review informs the need for extensive research on such determinants among South Asian populations, which may facilitate preventive measures addressing those underlying disparities.
Implementation research is a neglected domain in the realm of global mental health. In the context of South Asia, little is known about how mental health policies, programs, and other population-level measures are developed, implemented, and evaluated [35, 106]. Nonetheless, the scope of mental health services within the current pandemic preparedness plans is yet to be examined. Policy researchers should complement epidemiological investigations through assessing the relevance of evidence-based public mental health interventions in the context of South Asia. Moreover, implementation research outcomes should be widely communicated to foster timely decision-making and setting priorities for future research and actions.
South Asian countries have a comparative lack of empirical research on mental health problems despite having a large proportion of the global population [39, 40, 107]. This was revalidated by the low number of empirical studies in the current review. Moreover, most studies were from India, Bangladesh, and Pakistan, with fewer studies from Nepal and Sri Lanka. No study was identified from Afghanistan, Bhutan, and Maldives, highlighting a research disparity in this region. Moreover, studies from one country may not recruit nationally representative samples, which may affect the generalizability of the subgroup estimates. These research gaps within and between the South Asian countries can be attributable to several issues such as a lack of research funding, inadequate institutional capacities, a low demand of scientific evidence among the key decision-makers, and other context-specific factors in respective health systems [39, 40]. It is necessary to address these challenges through engaging institutional stakeholders and empowering them to use research data for mental health policymaking. Stewardship approaches should be adopted by the healthcare leadership to strengthen country-level and regional research capacities and collaborations, which may improve the knowledge base amid this pandemic as well as advance mental health policymaking and practice.
4.3. Implications for mental health policymaking and practice
The current evidence suggests a high prevalence of anxiety and depression in South Asian countries, which requires increasing availability of and accessibility to mental health services. Such measures are critical to diagnose anxiety and depression in high-risk populations and deliver psychiatric and psychological therapies to the affected individuals. However, South Asian countries have a serious scarcity of mental health professionals according to the pre-pandemic estimates [35, 40, 106], which may aggravate during this pandemic as many healthcare organizations are prioritizing infection prevention and in-patient services for physical health problems. This growing gap should be acknowledged and addressed using contextually appropriate actions that may improve access to mental health services alongside pandemic control in respective populations. Potential strategies to improve mental health services during this pandemic may include task-shifting of mental health services through capacity building, initiating telepsychiatric care services, incentivizing healthcare providers and organizations for facilitating mental health services, and strengthening mental health systems for delivering mental health in the target populations [9, 14, 92, 108, 109].
This review suggests a relatively higher burden of anxiety and depression among marginalized populations groups such as women and occupational groups with higher psychological distress such as healthcare providers. It is essential to adopt targeted interventions for high-risk groups. Some of these interventions may be delivered in workplaces or organizations, whereas mass media interventions or self-management resources can be delivered in a more generalized manner targeting a broader audience [9, 92]. Such efforts should promote early diagnosis and referral to specialized care for individuals with advanced symptoms. Moreover, stigma to mental health problems is a critical psychosocial challenge in South Asia [40, 106]. Socio-culturally appropriate media campaigns should be organized to sensitize the general population, address stigma, and encourage them to participate in mental health programs.
In recent years, digital mental health has emerged as a promising approach to improve access to mental health services using digital devices and internet-based technologies [110]. Such interventions may facilitate self-management and patient-provider communication in mental health practice. However, the evidence on the effectiveness of such interventions during this pandemic is not well known [111]. Previous research suggests a lack of digital mental health interventions in South Asian countries [90], therefore, conceptualizing and delivering such interventions during this pandemic would involve expert opinions and the evidence available from other contexts. Moreover, evidence-based interventions such as internet-delivered cognitive behavioral therapy can be clinically effective as well as cost-effective [112, 113], which should be considered from expanding digital mental health services in this region. These initiatives should engage patients, caregivers, and mental healthcare providers to incorporate their perspectives, needs, and recommendations to optimize future digital interventions in the realm of mental health.
Primary care and community-based health facilities play a vital role in delivering preventive and therapeutic health services in South Asian countries [114, 115, 116]. However, the current capacity of such community-level facilities to deliver mental health services during this pandemic may not be adequate to address the continued burden of mental disorders among the communities they serve [35, 106]. Mental health policymakers and practitioners may need to assess the preparedness of these facilities and explore potential opportunities to strengthen community-based, low-cost, evidence-based, and sustainable mental health services during COVID-19 pandemic.
The current evidence suggests the need for accurate information and measures for preventing COVID-19 pandemic [15, 54, 117], which may address psychosocial distress among individuals and populations. Online and mass media health communication interventions should be developed in cooperation with media stakeholders and public health agencies ensuring effective risk communication during this pandemic. Moreover, healthcare providers should be equipped with protective equipment and psychoeducational resources that may address mental health problems due to occupational stressors [118, 119, 120].
Health and socioeconomic consequences of the COVID-19 pandemic may have disrupted public mental health programs in South Asian countries, which is a major challenge for providing mental health during this crisis as well as restoring the program activities for achieving program goals and targets. For example, India has National Mental Health Program and District Mental Health program that target population mental health, whereas multicomponent programs such as Rashtriya Kishor Swasthya Karyakram (RKSK) aims to improve mental health and wellbeing in adolescents alongside overall health promotion [35]. Since the institutional points of care such as the schools or community outreach events may not remain operational during this pandemic, those mental health programs may not be delivered to the target populations as they have been planned previously. These programs require careful attention and proactive efforts to revitalize the same. Moreover, restoring public mental health programs should be consistent with infection control measures and prevention policies in respective contexts.
Strengthening mental health services and programs may require resources that are often facilitated through the provisions of mental health policies in respective countries. However, South Asian countries have policy-level gaps in terms of coordinated mental health service delivery that are well documented [40, 106]. Moreover, local and national mental health policies may not have scopes for mobilizing resources in complex situations and public health emergencies. Two major approaches can be recommended in this regard. First, revisiting the current policies and leveraging available resources to facilitate mental health services. Second, adopting stand-alone mental health programs for addressing mental health problems during and after this pandemic that may complement the existing policies and programs. Devising policy alternatives can be a lengthy process, which is a common obstacle for decision-making during public health emergencies. A rapid evidence synthesis should be conducted, and all stakeholders should be informed regarding the available strategies that can be enacted, minimizing the potential misuse of resources and maximizing mental health actions.
Lastly, COVID-19 has deeply impacted every aspects of human lives and widened health disparities across contexts, which necessitates a holistic approach to address the psychosocial and environmental determinants of mental disorders [9, 49, 57]. Most of the South Asian countries have a high burden of social diseases such as poverty, unemployment, illiteracy, gender inequity, interpersonal violence, political unrest, systematic exclusion of minorities from socioeconomic opportunities, and many other issues that may adversely affect mental health and wellbeing across population groups [29, 39, 40, 93]. Such problems are likely to accelerate amid the changing socioeconomic landscape during the COVID-19 pandemic and increase the psychosocial stressors resulting in a growing burden of mental health problems. The coexistence of and interactions between multiple biophysical and psychosocial problems are suggestive of a syndemic [121], which may have long term population health consequences in this region. The policymakers and other key stakeholders must acknowledge and address these complex problems to improve public mental health in South Asian countries. In addition, public institutions and regulatory authorities should reach a consensus to develop mental health resilience through multipronged social efforts at the population level. Furthermore, collaborative decision-making may empower communities and institutions to adopt evidence-based, integrated, and timely measures that are necessary to alleviate the psychosocial burden of COVID-19 in South Asia.
4.4. Limitations of this review
This meta-analytic review has several limitations. First, a high publication bias indicates that some studies might not have been included in the current review. We focused on peer-reviewed journal sources; therefore, preprints and non-indexed journal articles were beyond the scope of this review. Although this measure ensured a better quality of our review by including peer-reviewed evidence only, this might have excluded some studies that could provide further epidemiological insights on anxiety and depression. Also, peer-reviewed articles indexed in databased that we did not use in this review could remain beyond the scope of our review. Despite in inclusive search of literature, this issue appears to be a limitation of our review. Second, the use of study-level data may lead to less accurate estimates compared to analyzing participant-level data. Most studies did not include an open data sharing approach that limited the opportunity to examine intra-study and inter-study variations in meta-analyses. Third, we included studies that used validated scales, whereas a more accurate evaluation of mental health would require clinical assessments and advanced diagnostic tests such as functional neuroimaging [122, 123]. Future research may adopt stronger methodological approaches integrating better estimations of mental health problems across populations. Last, we did not find enough data to construct and use multiple variables in additional sub-group analyses and meta-regression that could explain the potential sources of heterogeneity across studies. Moreover, such data could provide further insights on variances in population groups that would inform policymaking and clinical care for high-risk groups. We encourage future researchers to use uniform measurement instruments, recruit samples that represent the populations of interest, adopt liberal data sharing approaches, and improve the knowledge base through a more rigorous synthesis of evidence.
5. Conclusion
COVID-19 pandemic has adversely affected psychosocial health and wellbeing globally. This review synthesized the quantitative evidence on the prevalence of anxiety and depression in South Asia during this pandemic. The results inform a high burden of anxiety and depression in this region, necessitating the adoption of multilevel mental health interventions alleviating psychosocial burden of COVID-19. Moreover, high heterogeneity among studies and marked knowledge gaps on psychosocial epidemiology in South Asian countries inform the need for further research, which may facilitate evidence-based mental health promotion in this region during and after this pandemic.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.World Health Organization. Coronavirus Disease (COVID-19). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 2.Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Available at: https://www.cdc.gov/coronavirus/2019-ncov/cdcresponse/about-COVID-19.html.
- 3.World Health Organization . 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. [Google Scholar]
- 4.Chaudhry R., Dranitsaris G., Mubashir T., Bartoszko J., Riazi S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. E Clin. Med. 2020;25 doi: 10.1016/j.eclinm.2020.100464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tabari P., Amini M., Moghadami M., Moosavi M. International public health responses to COVID-19 outbreak: a rapid review. Iran. J. Med. Sci. 2020;45(3):157–169. doi: 10.30476/ijms.2020.85810.1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salari N., Hosseinian-Far A., Jalali R. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16(1):57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deng J., Zhou F., Hou W. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann. N. Y. Acad. Sci. October 2020 doi: 10.1111/nyas.14506. nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2020 doi: 10.1016/j.ijchp.2020.07.007. xxx---xxx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hossain M.M., Tasnim S., Sultana A. Epidemiology of mental health problems in COVID-19: a review. F1000Research. 2020;9:636. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh S., Roy D., Sinha K., Parveen S., Sharma G., Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatr. Res. 2020;293:113429. doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amerio A., Brambilla A., Morganti A. COVID-19 lockdown: housing built environment’s effects on mental health. Int. J. Environ. Res. Publ. Health. 2020;17(16):5973. doi: 10.3390/ijerph17165973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webb L. COVID-19 lockdown: a perfect storm for older people’s mental health. J. Psychiatr. Ment. Health Nurs. June 2020 doi: 10.1111/jpm.12644. jpm.12644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rossi R., Socci V., Talevi D. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatr. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hossain M.M., Sultana A., Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol. Health. 2020;42 doi: 10.4178/epih.e2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tasnim S., Hossain M., Mazumder H. Impact of rumors and misinformation on COVID-19 in social media. J. Prev. Med. Publ. Heal. 2020;53(3):171–174. doi: 10.3961/jpmph.20.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chong M.Y., Wang W.C., Hsieh W.C. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185(AUG):127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- 17.Wu P., Fang Y., Guan Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatr. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yip P.S.F., Cheung Y.T., Chau P.H., Law Y.W. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. 2010;31(2):86–92. doi: 10.1027/0227-5910/a000015. [DOI] [PubMed] [Google Scholar]
- 19.Chew Q.H., Wei K.C., Vasoo S., Chua H.C., Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singap. Med. J. 2020;61(7):350–356. doi: 10.11622/smedj.2020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.da Silva D.A.R., Weyll Pimentel R.F., das Merces M.C. Covid-19 and the pandemic of fear: reflections on mental health. Rev. Saude Publica. 2020;54 doi: 10.11606/s1518-8787.2020054002486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chi X., Becker B., Yu Q. Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the coronavirus disease (COVID-19) pandemic. Front. Psychiatr. 2020;11:1. doi: 10.3389/fpsyt.2020.00803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chi X., Becker B., Yu Q. Persistence and remission of depressive symptoms and psycho-social correlates in Chinese early adolescents. BMC Psychiatr. 2020;20(1):406. doi: 10.1186/s12888-020-02808-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tasnim S., Rahman M., Pawar P. Epidemiology of sleep disorders during COVID-19 pandemic: a systematic scoping review Authors. medRxiv. October 2020;2020 [Google Scholar]
- 26.Santabárbara J., Bueno-Notivol J., Lipnicki D.M. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: a rapid systematic review (on published articles in Medline) with meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Santabárbara J., Lasheras I., Lipnicki D.M. Prevalence of anxiety in the COVID-19 pandemic: an updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;109 doi: 10.1016/j.pnpbp.2020.110207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bhutta Z.A., Basnyat B., Saha S., Laxminarayan R. Covid-19 risks and response in South Asia. BMJ. 2020;368 doi: 10.1136/bmj.m1190. [DOI] [PubMed] [Google Scholar]
- 29.Roy A., Singh A.K., Mishra S., Chinnadurai A., Mitra A., Bakshi O. Mental health implications of COVID-19 pandemic and its response in India. Int. J. Soc. Psychiatr. 2020 doi: 10.1177/0020764020950769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern. Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 31.Rahman A., Naslund J.A., Betancourt T.S. The NIMH global mental health research community and COVID-19. The Lancet Psychiatry. 2020;7(10):834–836. doi: 10.1016/S2215-0366(20)30347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kar S.K., Yasir Arafat S.M., Kabir R., Sharma P., Saxena S.K. Coronavirus Disease 2019 (COVID-19) Nature Publishing Group; 2020. Coping with mental health challenges during COVID-19; pp. 199–213. [Google Scholar]
- 33.World Health Organization. COVID-19 Disrupting Mental Health Services in Most Countries, WHO survey. Available at: https://www.who.int/news/item/05-10-2020-covid-19-disrupting-mental-health-services-in-most-countries-who-survey.
- 34.Mubbashar M.H., Saeed K. Development of mental health services in Pakistan. East. Mediterr. Health J. 2001;7(3):392–396. [PubMed] [Google Scholar]
- 35.Hossain M., Purohit N. Improving child and adolescent mental health in India: status, services, policies, and way forward. Indian J. Psychiatr. 2019;61(4):415–419. doi: 10.4103/psychiatry.IndianJPsychiatry_217_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Desai N.G., Tiwari S.C., Nambi S. Urban mental health services in India : how complete or incomplete? Indian J. Psychiatr. 2004;46(3):195–212. [PMC free article] [PubMed] [Google Scholar]
- 37.Hossain M.M., Hasan M.T., Sultana A., Faizah F. New mental health act in Bangladesh: unfinished agendas. The Lancet Psychiatry. 2019;6(1):e1. doi: 10.1016/S2215-0366(18)30472-3. [DOI] [PubMed] [Google Scholar]
- 38.Naveed S., Waqas A., Chaudhary A.M.D. Prevalence of common mental disorders in South Asia: a systematic review and meta-regression analysis. Front. Psychiatr. 2020;11:899. doi: 10.3389/fpsyt.2020.573150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hossain M.M., Purohit N., Sultana A., Ma P., Mckyer L.J., Ahmed U. Prevalence of mental disorders in South Asia: an umbrella review of systematic reviews and meta-analyses. Asian J. Psychiatr. 2020 doi: 10.1016/j.ajp.2020.102041. [DOI] [PubMed] [Google Scholar]
- 40.Trivedi J.K., Goel D., Kallivayalil R.A., Isaac M., Shrestha D.M., Gambheera H.C. Regional cooperation in South Asia in the field of mental health. World Psychiatr. 2007;6(1):57–59. [PMC free article] [PubMed] [Google Scholar]
- 41.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339 doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wallace B.C., Dahabreh I.J., Trikalinos T.A., Lau J., Trow P., Schmid C.H. Closing the gap between methodologists and end-users: R as a computational back-end. J. Stat. Software. 2012;49(1):1–15. [Google Scholar]
- 44.Freemantle N. StatsDirect–statistical software for medical research in the 21st century. BMJ. 2000;321(7275):1536. [Google Scholar]
- 45.Barendregt J.J., Doi S.A., Lee Y.Y., Norman R.E., Vos T. Meta-analysis of prevalence. J. Epidemiol. Community Health. 2013;67(11):974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- 46.DerSimonian R., Laird N. Meta-analysis in clinical trials. Contr. Clin. Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 47.Cheung M.W.L., Ho R.C.M., Lim Y., Mak A. Conducting a meta-analysis: basics and good practices. Int. J. Rheum. Dis. 2012;15(2):129–135. doi: 10.1111/j.1756-185X.2012.01712.x. [DOI] [PubMed] [Google Scholar]
- 48.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ahmad A., Rahman I., Agarwal M. Early psychosocial predictors of mental health among Indians during coronavirus disease 2019 outbreak. J. Health Sci. 2020;10(2):147–156. [Google Scholar]
- 50.Ahmed O., Ahmed M.Z., Alim S.M.A.H.M., Khan M.D.A.U., Jobe M.C. COVID-19 outbreak in Bangladesh and associated psychological problems: an online survey. Death Stud. 2020:1–10. doi: 10.1080/07481187.2020.1818884. [DOI] [PubMed] [Google Scholar]
- 51.Gupta S., Kohli K., Padmakumari P. Psychological health among armed forces doctors during COVID-19 pandemic in India. Indian J. Psychol. Med. 2020;42(4):374–378. doi: 10.1177/0253717620934037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gupta S., Prasad A.S., Dixit P.K., Padmakumari P., Gupta S., Abhisheka K. Survey of prevalence of anxiety and depressive symptoms among 1124 healthcare workers during the coronavirus disease 2019 pandemic across India. Med. J. Armed Forces India. 2020;(xxxx) doi: 10.1016/j.mjafi.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hasan S.R., Hamid Z., Jawaid M.T., Ali R.K. Anxiety among doctors during COVID-19 pandemic in secondary and tertiary care hospitals. Pak. J. Med. Sci. 2020;36(6):1360–1365. doi: 10.12669/pjms.36.6.3113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hossain T., Ahammed B., Chanda S.K., Jahan N., Ela M.Z., Islam N. Social and electronic media exposure and generalized anxiety disorder among people during COVID-19 outbreak in Bangladesh: a preliminary observation. PloS One. 2020;15(9 September):1–13. doi: 10.1371/journal.pone.0238974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Imran N., Masood H.M.U., Ayub M., Gondal K.M. Psychological impact of COVID-19 pandemic on postgraduate trainees: a cross-sectional survey. Postgrad. Med. 2020 doi: 10.1136/postgradmedj-2020-138364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Imran N., Hashmi A.M., Masud K. The toll it takes: mental health burden and associated factors during COVID-19 outbreak among healthcare workers in Lahore, Pakistan. Ann King Edward Med. Univ. 2020;26(2):317–323. [Google Scholar]
- 57.Akhtarul Islam M., Barna S.D., Raihan H., Nafiul Alam Khan M., Tanvir Hossain M. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PloS One. 2020;15(8 August):1–12. doi: 10.1371/journal.pone.0238162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Islam M.S., Ferdous M.Z., Potenza M.N. Panic and generalized anxiety during the COVID-19 pandemic among Bangladeshi people: an online pilot survey early in the outbreak. J. Affect. Disord. 2020;276(July):30–37. doi: 10.1016/j.jad.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jain A., Singariya G., Kamal M., Kumar M., Jain A., Solanki R. COVID-19 pandemic: psychological impact on anaesthesiologists. Indian J. Anaesth. 2020;64(9) doi: 10.4103/ija.IJA_697_20. 774-774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Khanna R., Honavar S., Metla A., Bhattacharya A., Maulik P. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian J. Ophthalmol. 2020;68(6):994. doi: 10.4103/ijo.IJO_1458_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Amin F., Sharif S., Saeed R., Durrani N., Jilani D. COVID-19 pandemic- knowledge, perception, anxiety and depression among frontline doctors of Pakistan. BMC Psychiatr. 2020;20(1):459. doi: 10.1186/s12888-020-02864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khanal P., Devkota N., Dahal M., Paudel K., Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob. Health. 2020;16(1):89. doi: 10.1186/s12992-020-00621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mamun M.A., Sakib N., Gozal D. The COVID-19 pandemic and serious psychological consequences in Bangladesh: a population-based nationwide study. J. Affect. Disord. October 2020 doi: 10.1016/j.jad.2020.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mani V.E., Sarkar Z., Gutti N.B. A study of the impact of the COVID-19 pandemic on anxiety levels of young adults in India. J. Evol. Med. Dent. Sci. 2020;9(31):2233–2238. [Google Scholar]
- 65.Nihmath Nisha S., Francis Y.M., Balaji K., Raghunath G., Kumaresan M. A survey on anxiety and depression level among South Indian medical students during the COVID 19 pandemic. Int. J. Res. Pharm. Sci. 2020;11(Special Issue 1):779–786. [Google Scholar]
- 66.Patabendige M., Gamage M.M., Weerasinghe M., Jayawardane A. Psychological impact of the COVID-19 pandemic among pregnant women in Sri Lanka. Int. J. Gynecol. Obstet. 2020;151(1):150–153. doi: 10.1002/ijgo.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Reddy V.V., Revanth Karri S., Jezreel T., Afeen S., Khairkar P. Psychosocial impact of COVID-19 lockdown on mental wellbeing among 11 states of India: a Markov modeling approach. J. Psychiatry. Psychiatr. Disord. 2020;4(4):158–174. [Google Scholar]
- 68.Sandesh R., Shahid W., Dev K. Impact of COVID-19 on the mental health of healthcare professionals in Pakistan. Cureus. 2020;12(7):3–7. doi: 10.7759/cureus.8974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sebastian J., Anand A., Vakkalaganti Rajesh R., Lucca J.M., Joseph R. Impact of covid-19 pandemic on psychological responses of the general population in India: a nationwide survey. Int. J. Pharmacol. Res. 2020;12:2349–2357. COVIDWHO. [Google Scholar]
- 70.Sharma S., Bansal R., Parashar P., Ahmad S., Kumar A., Kumar A. Stress and depression among people admitted in a COVID 19 quarantine centre of North India. Subharti J. Interdiscip. Res. 2020;3 [Google Scholar]
- 71.Shrestha S.L. Prevalence of psychological effect of COVID-19 on medical professionals in a tertiary care center. J. Nepal Med. Assoc. JNMA. 2020;58(228):550–553. doi: 10.31729/jnma.5087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Banna MH Al, Sayeed A., Kundu S. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. Int. J. Environ. Health Res. 2020:1–12. doi: 10.1080/09603123.2020.1802409. [DOI] [PubMed] [Google Scholar]
- 73.Sil A., Das A., Jaiswal S. Mental health assessment of frontline COVID-19 dermatologists: a Pan-Indian multicentric cross-sectional study. Dermatol. Ther. 2020;(June):8–9. doi: 10.1111/dth.13884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Suryavanshi N., Kadam A., Dhumal G. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav. 2020;(July):1–12. doi: 10.1002/brb3.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Verma S., Mishra A. Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int. J. Soc. Psychiatr. 2020;66(8):756–762. doi: 10.1177/0020764020934508. [DOI] [PubMed] [Google Scholar]
- 76.Wilson W., Raj J.P., Rao S. Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: a nationwide observational study. Indian J. Psychol. Med. 2020;42(4):353–358. doi: 10.1177/0253717620933992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zubayer A Al, Rahman M.E., Islam M.B. Psychological states of Bangladeshi people four months after the COVID-19 pandemic: an online survey. Heliyon. 2020;6(9) doi: 10.1016/j.heliyon.2020.e05057. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 78.Chatterjee S., Bhattacharyya R., Bhattacharyya S., Gupta S., Das S., Banerjee B. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian J. Psychiatr. 2020;62(3):257. doi: 10.4103/psychiatry.IndianJPsychiatry_333_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chew N.W.S., Lee G.K.H., Tan B.Y.Q. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88(April):559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chew N.W.S., Ngiam J.N., Tan B.Y.-Q. Asian-Pacific perspective on the psychological well-being of healthcare workers during the evolution of the COVID-19 pandemic. BJ Psych. Open. 2020;6(6):e116. doi: 10.1192/bjo.2020.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Desai M.Z.J.H., Khan A.R., Kulkarni R., Hegde B. The psychological impact of COVID-19 and the subsequent social isolation on the general population of Karnataka, India. J. Ideas Heal. 2020;3(Special1):190–195. [Google Scholar]
- 82.Grover S., Sahoo S., Mehra A. Psychological impact of COVID-19 lockdown: an online survey from India. Indian J. Psychiatr. 2020;62(4):354. doi: 10.4103/psychiatry.IndianJPsychiatry_427_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gupta A.K., Mehra A., Niraula A. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID-19 pandemic. Asian J. Psychiatr. 2020;54(January) doi: 10.1016/j.ajp.2020.102260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hossain M.M. Current status of global research on novel coronavirus disease (COVID-19): a bibliometric analysis and knowledge mapping. F1000Research. 2020;9:374. [Google Scholar]
- 85.Le H.T., Lai A.J.X., Sun J. Anxiety and depression among people under the nationwide partial lockdown in Vietnam. Front. Publ. Heal. 2020;8:589359. doi: 10.3389/fpubh.2020.589359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tee M.L., Tee C.A., Anlacan J.P. Psychological impact of COVID-19 pandemic in the Philippines. J. Affect. Disord. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ahasan R., Alam M.S., Chakraborty T., Hossain M.M. Applications of GIS and geospatial analyses in COVID-19 research: a systematic review. F1000Research. 2020;9:1379. doi: 10.12688/f1000research.27544.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ahasan R., Hossain M.M. Leveraging GIS and spatial analysis for informed decision-making in COVID-19 pandemic. Heal Policy Technol. 2020 doi: 10.1016/j.hlpt.2020.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhou Y., Singh N., Kaushik P.D. The digital divide in rural South Asia: survey evidence from Bangladesh, Nepal and Sri Lanka. IIMB Manag. Rev. 2011;23(1):15–29. [Google Scholar]
- 90.Hossain M.M., Tasnim S., Sharma R. Digital interventions for people living with non-communicable diseases in India: a systematic review of intervention studies and recommendations for future research and development. Digit Heal. 2019;5 doi: 10.1177/2055207619896153. 205520761989615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tran B.X., Phan H.T., Thi Nguyen T.P. Reaching further by village health collaborators: the informal health taskforce of Vietnam for COVID-19 responses. J. Glob Health. 2020;10(1) doi: 10.7189/jogh.10.010354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Holmes E.A., O’Connor R.C., Perry V.H. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Niaz U., Hassan S. Culture and mental health of women in South-East Asia. World Psychiatr. 2006;5(2):118–120. [PMC free article] [PubMed] [Google Scholar]
- 94.Hossain M.M., Sultana A., Das A. Gender-based violence among Rohingya refugees in Bangladesh: a public health challenge. Indian J. Med. Ethics. 2018 doi: 10.20529/IJME.2018.045. [DOI] [PubMed] [Google Scholar]
- 95.Jejeebhoy S.J., Santhya K.G., Acharya R. Violence against women in South Asia: the need for the active engagement of the health sector. Global Publ. Health. 2014;9(6):678–690. doi: 10.1080/17441692.2014.916736. [DOI] [PubMed] [Google Scholar]
- 96.Keynejad R.C., Hanlon C., Howard L.M. Psychological interventions for common mental disorders in women experiencing intimate partner violence in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet Psychiatry. 2020;7(2):173–190. doi: 10.1016/S2215-0366(19)30510-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.vora M., Malathesh B.C., Das S., Chatterjee S.S. COVID-19 and domestic violence against women. Asian J. Psychiatr. 2020;53:102227. doi: 10.1016/j.ajp.2020.102227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sharma R., Hossain M.M., Pawar P., Sharma S. Air pollution and geriatric mental health: perspectives on the COVID-19 pandemic. Int. Psychogeriatr. 2020:1–2. doi: 10.1017/S1041610220001428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mazumder H., Hossain M.M., Das A. Geriatric care during public health emergencies: lessons learned from novel corona virus disease (COVID-19) pandemic. J. Gerontol. Soc. Work. 2020;63(4):257–258. doi: 10.1080/01634372.2020.1746723. [DOI] [PubMed] [Google Scholar]
- 100.Hao F., Tan W., Jiang L. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bhalla I.P., Stefanovics E.A., Rosenheck R.A. Mental health multimorbidity and poor quality of life in patients with schizophrenia. Schizophr. Res. 2018;201:39–45. doi: 10.1016/j.schres.2018.04.035. [DOI] [PubMed] [Google Scholar]
- 102.Hossain M.M., Khan N., Sultana A. Prevalence of comorbid psychiatric disorders among people with autism spectrum disorder: an umbrella review of systematic reviews and meta-analyses. Psychiatr. Res. 2020;287 doi: 10.1016/j.psychres.2020.112922. [DOI] [PubMed] [Google Scholar]
- 103.Tran B.X., Dang A.K., Thai P.K. Coverage of health information by different sources in communities: implication for COVID-19 epidemic response. Int. J. Environ. Res. Publ. Health. 2020;17(10):3577. doi: 10.3390/ijerph17103577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Smith L., Jacob L., Trott M. The association between screen time and mental health during COVID-19: a cross sectional study. Psychiatr. Res. 2020;292:113333. doi: 10.1016/j.psychres.2020.113333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sultana A., Tasnim S., Bhattacharya S., Hossain M.M., Purohit N. Digital screen time during COVID-19 pandemic: a public health concern. SocArXiv. 2020 [Google Scholar]
- 106.Shidhaye R., Sikander S., Jordans M., De Silva P., Chatterjee S. Mental Health in South Asia: Ethics, Resources, Programs and Legislation. Springer; Dordrecht: 2015. Mental health programs and policies in South Asia: initiatives and obstacles; pp. 95–111. [Google Scholar]
- 107.Hossain M.M., Sultana A., Tasnim S. Prevalence of mental disorders among people who are homeless: an umbrella review. Int. J. Soc. Psychiatr. 2020;66(6):528–541. doi: 10.1177/0020764020924689. [DOI] [PubMed] [Google Scholar]
- 108.Xiang Y.T., Yang Y., Li W. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Torous J., Myrick K.J., Rauseo-Ricupero N., Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. J. Med. Internet Res. 2020;22(3) doi: 10.2196/18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Soron T.R., Shariful Islam S.M., Ahmed H.U., Ahmed S.I. The hope and hype of telepsychiatry during the COVID-19 pandemic. The Lancet Psychiatry. 2020;7(8):e50. doi: 10.1016/S2215-0366(20)30260-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang M.W.B., Ho R.C.M. Moodle: the cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technol. Health Care. 2017;25(1):163–165. doi: 10.3233/THC-161261. [DOI] [PubMed] [Google Scholar]
- 113.Soh H.L., Ho R.C., Ho C.S., Tam W.W. Efficacy of digital cognitive behavioural therapy for insomnia: a meta-analysis of randomised controlled trials. Sleep Med. 2020;75:315–325. doi: 10.1016/j.sleep.2020.08.020. [DOI] [PubMed] [Google Scholar]
- 114.Hossain M., Sultana A., Munzur-E-Murshid Revitalising general practice in Bangladesh: complementing ’the Bangladesh paradox. Br. J. Gen. Pract. 2018;68(675):482. doi: 10.3399/bjgp18X699173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sultana A., Bhattacharya S., Hossain M.M. COVID-19 and primary care: a critical need for strengthening emergency preparedness across health systems. SocArXiv. 2020 doi: 10.4103/jfmpc.jfmpc_1874_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bhattacharya S., Juyal R., Hossain M., Singh A. Non-communicable diseases viewed as “collateral damage” of our decisions: fixing accountabilities and finding sloutions in primary care settings. J. Fam. Med. Prim. Care. 2020;9(5):2176. doi: 10.4103/jfmpc.jfmpc_202_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bhattacharya S., Sharma N., Hoedebecke K., Hossain M., Gökdemir Ö., Singh A. Harnessing the potential of uploading health educational materials on medical institutions’ social media for controlling emerging and re-emerging disease outbreaks. J. Educ. Health Promot. 2020;9(1):213. doi: 10.4103/jehp.jehp_215_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bhattacharya S., Singh A., Hossain M. Health system strengthening through Massive Open Online Courses (MOOCs) during the COVID-19 pandemic: an analysis from the available evidence. J. Educ. Health Promot. 2020;9(1):195. doi: 10.4103/jehp.jehp_377_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sultana A., Sharma R., Hossain M.M., Bhattacharya S., Purohit N. Burnout among healthcare providers during COVID-19: challenges and evidence-based interventions. Indian J. Med. Ethics. 2020:1–4. doi: 10.20529/IJME.2020.73. [DOI] [PubMed] [Google Scholar]
- 120.Bhattacharya S., Hossain M.M., Singh A. Addressing the shortage of personal protective equipment during the COVID-19 pandemic in India-A public health perspective. AIMS Publ. Heal. 2020;7(2):223–227. doi: 10.3934/publichealth.2020019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gravlee C.C. Systemic racism, chronic health inequities, and COVID-19: a syndemic in the making? Am. J. Hum. Biol. 2020;32(5) doi: 10.1002/ajhb.23482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Husain S.F., Yu R., Tang T.B. Validating a functional near-infrared spectroscopy diagnostic paradigm for Major Depressive Disorder. Sci. Rep. 2020;10(1):1–9. doi: 10.1038/s41598-020-66784-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ho C.S.H., Lim L.J.H., Lim A.Q. Diagnostic and predictive applications of functional near-infrared spectroscopy for major depressive disorder: a systematic review. Front. Psychiatr. 2020;11:1. doi: 10.3389/fpsyt.2020.00378. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supplementary material/referenced in article.