Abstract
Background
Numerous reports have described methods for repairing full-thickness upper eyelid defects using lower eyelid tissue. To avoid sacrificing the lower eyelid and thereby prevent lower eyelid sagging or dysfunction, we used innervated orbicularis oculi myocutaneous flaps harvested from the upper eyelid for upper eyelid reconstruction.
Methods
We modified a method reported by Moschella and Cordova for repairing full-thickness upper eyelid defects using innervated bipedicled orbicularis oculi myocutaneous flaps mobilized from the upper eyelid and labial mucosal grafts. First, we avoided the use of a Fricke flap, which is used in the original method to repair the myocutaneous flap donor site, since it can cause asymmetry of the eyebrows on both sides. Second, reconstruction of the double-fold eyelid was performed with buried sutures in the myocutaneous flap in secondary surgery, since the double eyelid fold of the original method is not necessary or is too wide for Asian people. Functional and cosmetic outcomes were assessed by six evaluators using postoperative photographs.
Results
Six patients with malignant upper eyelid tumours underwent repair of upper eyelid defects by our modified method. Donor sites of the myocutaneous flaps were repaired with a medial forehead flap in one patient with Merkel cell carcinoma, a lateral orbital flap in one patient with sebaceous carcinoma, and a two-stage skin graft in two patients with sebaceous carcinoma and basal cell carcinoma, respectively. The two remaining patients (one with sebaceous carcinoma and the other with basal cell carcinoma) required no donor site repair. Functional and cosmetic outcomes were good or excellent in most cases.
Conclusion
Our modified method for repairing full-thickness upper eyelid defects using innervated orbicularis oculi myocutaneous flaps resulted in optimal eyelid function and support, with morphologically satisfactory results including bilateral symmetry. This method provides a useful alternative to conventional methods of upper eyelid reconstruction.
Key words: Upper eyelid reconstruction, Full-thickness eyelid defect, Orbicularis oculi muscle, Bipedicled myocutaneous flap, Eyelid tumour, Innervated myocutaneous flap
Introduction
Numerous reports have described methods for reconstructing full-thickness upper eyelid defects, which are often challenging to repair.1,2 As the eyelid has a unique and complex structure, tissue harvested from the lower eyelid is considered ideal for upper eyelid reconstruction. While methods that use lower eyelid tissue to reconstruct upper eyelid defects have achieved satisfactory results,1,3 there are a number of issues with those procedures: 1) reconstruction requires a two-stage operation, and the eye must remain closed for two to three weeks, and 2) the sacrificed lower eyelid often develops lower eyelid deformities, such as sagging and flattening, as well as mild dysfunction of the orbicularis oculi muscle.
Since the upper eyelid should be in contact with the globe during eyelid movement, it must stretch horizontally when raised. In a full upward gaze, this may be in the range of 30 to 40%, or more, of the horizontal length of the upper eyelid margin.1 Optimal muscle tone of the orbicularis oculi muscle is required to keep the upper eyelid in contact with the globe. A smooth mucosal or conjunctival inner lining is also required to protect the cornea. To address these issues, we used an innervated (functional) orbicularis oculi myocutaneous flap harvested from the upper eyelid to repair the defect, and a full-thickness labial mucosal graft to reconstruct the inner lining.
Innervated (functional) orbicularis oculi myocutaneous flaps have been reported to be useful.4., 5., 6., 7. Moschella and Cordova first reported a method in which innervated bipedicled orbicularis oculi myocutaneous flaps mobilized from the upper eyelid were used to reconstruct upper eyelid defects. Patrinely et al. also used bipedicled orbicularis oculi myocutaneous flaps mobilized from the upper eyelid, using a skin graft to repair the donor site and a tarsoconjunctival graft to repair the posterior lamella.7
The original method described by Moschella and Cordova used a Fricke flap,8 which is harvested from the forehead area just above the eyebrow, to repair the donor site of the bipedicled myocutaneous flap. Using a Fricke flap often results in asymmetry of the eyebrows on both sides. Moreover, the flap provides a rather thick-skinned and suboptimal colour/texture eyelid compared with flaps from the lateral orbital area or cheek. In the method described herein, we made two modifications to the original method. First, we avoided using a Fricke flap, and optimal methods were selected according to the condition of each patient to repair the donor site of the myocutaneous flap.
Second, reconstruction of the eyelid fold was performed not at the upper edge of the bipedicled myocutaneous flap as in the original method, but in the flap secondarily in patients with double-fold eyelids, since the double eyelid fold made in the original method is not necessary or is too wide for Asian people. Moreover, secondary surgery provides a more precise double eyelid fold without tissue oedema.
Patients and methods
Operative technique
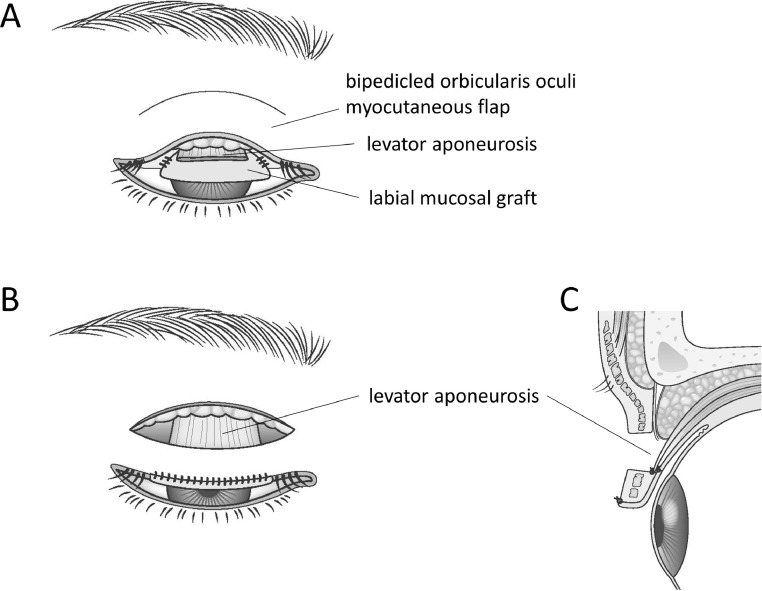
The operative technique of the modified method is as follows (Figure 1):
-
1.
The upper eyelid tumour is widely resected. If the levator aponeurosis is excised during surgery, the excised end is marked with sutures.(Figure 3B).
-
2.
A full-thickness mucosal graft is harvested from the lower lip. The lower lip defect is covered with artificial dermis (IntegraⓇ Bilayer Wound Matrix, Integra Life Sciences Corporation, Plainsboro, NJ) using 6–0 Vicryl sutures. The harvested graft is sufficient in size to fill the conjunctival defect under moderate tension, except that the lid margin is longer by 3 mm. The graft is then sutured to the conjunctival defect with 7–0 Vicryl sutures, leaving the lid margin 3 mm in excess of the defect (Figure 1A, 3D).
-
3.
An orbicularis oculi myocutaneous flap is elevated from the remaining upper eyelid (preseptal or orbital part of the eyelid). If elevated as a bipedicled flap, the vertical width of the flap is approximately 8 mm. The flap contains full-thickness orbicularis oculi muscle fibres, which maintain continuity at both ends of the bipedicled flap (muscle-ring continuity) and are innervated by temporal branches of the facial nerve (Figure 1A). When the defect is small, the orbicularis oculi muscle and skin covering it are only elevated from the tarsus and the orbital septum in the same manner and mobilized downward to the lid margin while maintaining continuity with the upper part of the eyelid with no tension.
-
4.
The flap is mobilized downward to the lid margin (Figure 1B). If necessary, small pieces of wedge-shaped surplus skin at both sides are cut and discarded. The marked stump of the levator aponeurosis is then dissected, spread horizontally, and sutured to the upper edge of the bipedicled myocutaneous flap at the point proximal to the labial mucosal graft layer with 7–0 Vicryl sutures. The stump is carefully sutured to a sufficiently deep portion of the upper edge of the flap to avoid the formation of an eyelid fold at this location (Figure 1C). Sutures are adjusted so that the lid margin is naturally curved when the eyelid is raised. Care is taken not to excessively advance the levator aponeurosis, as this can cause eyelid retraction. If the remaining aponeurosis is too short, a small fascia graft between the stump of the aponeurosis and the bipedicled myocutaneous flap may be necessary. If the defect is small enough and the aponeurosis is intact, this procedure is not necessary. The lower edge of the mucosal graft, 3 mm in excess at the lid margin, is sutured to the lower edge of the flap skin. The lower edge of the flap must be covered securely with the everted mucosal graft to protect the cornea (Figure 1B,C).
-
5.
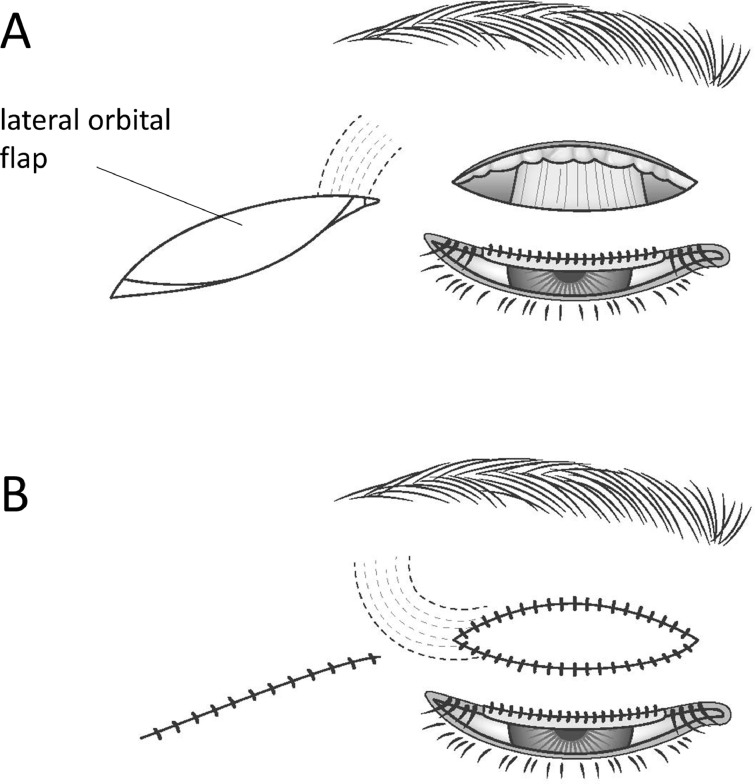
If necessary, the myocutaneous flap donor site is repaired with a flap or a skin graft other than a Fricke flap. The first choice for repairing the donor site is a lateral orbital flap9 (Fig. 2A,B,3C,E). When this is not available, other method such as a median forehead flap or a secondary skin graft is used based on the patient's condition (Table 1).
-
6.
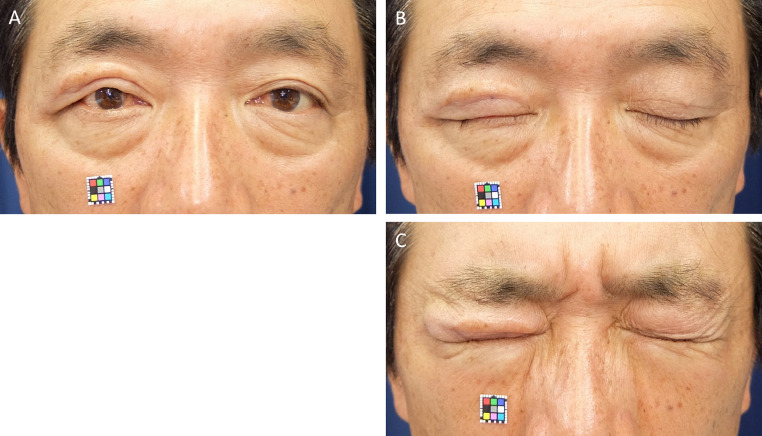
If the patient has double-fold eyelids, eyelid fold reconstruction surgery is performed several months after the initial surgery. The eyelid fold is created in the (bipedicled) orbicularis oculi myocutaneous flap to resemble the contralateral eyelid using 6–0 nylon buried sutures (Figure 4B).
Figure 1.
Schema. A: After the upper eyelid tumour is widely resected, a mucosal graft is harvested from the lower lip and sutured to the conjunctival defect. At the lid margin, a small excess length (3 mm) of graft is retained. B: An orbicularis oculi myocutaneous flap is mobilized downward to the lid margin. The stump of the aponeurosis of the levator muscle is sutured to the upper edge of the flap. The stump is carefully sutured to a sufficiently deep portion of the upper edge of the flap to avoid the formation of an eyelid fold at this location. Sutures are adjusted so that the lid margin is naturally curved when the eyelid is raised. The lower edge of the mucosal graft is sutured to the lower edge of the flap skin. The lower edge of the flap must be securely covered with the mucosal graft. C: Profile view of Figure. B.
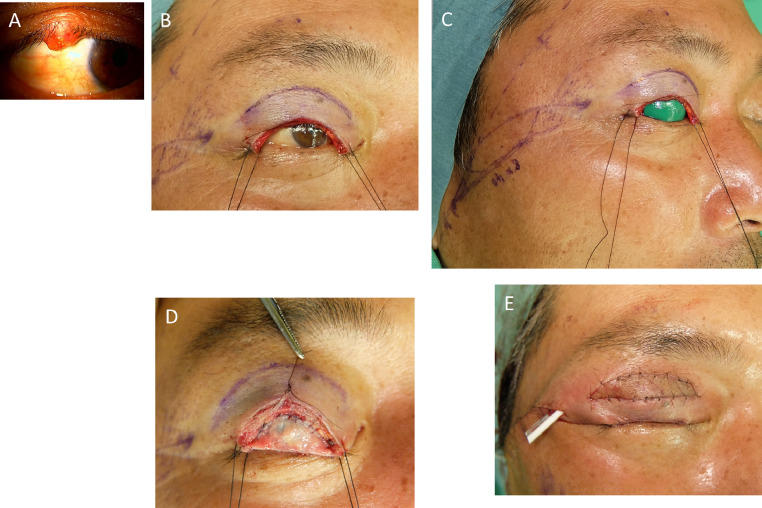
Figure 3.
Case involving a 55-year-old man (Patient 5). A: Sebaceous carcinoma on the right upper eyelid margin of the patient. B: The tumour is resected with a 7-mm margin. The stump of the levator aponeurosis is marked with 6–0 nylon suture. C: A lateral orbital flap is designed. D: The mucosal graft is sutured to the conjunctival defect with 7–0 Vicryl sutures. At the lid margin, a small excess (3 mm) is retained. Forceps are used to hold the 6–0 nylon suture marking the stump of the levator aponeurosis. E: The donor site of the bipedicled orbicularis oculi myocutaneous flap is repaired with the lateral orbital flap.
Figure 2.
Schema for Patient 5. A: A lateral orbital flap is designed. B: The donor site of the bipedicled orbicularis oculi myocutaneous flap is repaired with a lateral orbital flap.
Table 1.
Patient characteristics.
| Patient no. | Age/sex | diagnosis | tumour size height × width (mm) | Defect size height × width (mm) | Method of donor site repair | Follow-up period (years) | Oncological results | Functional results | Cosmetic results |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 58/F | MCC | 10 × 8 | 18 × 28 | Median forehead flap | 11 | Metastasis in deep parotid gland | Good | Fair |
| 2 | 81/M | SC | 6 × 9 | 10 × 19 | None | 1 | No recurrence | Excellent | Good |
| 3 | 76/M | BCC | 8 × 7.5 | 10 × 13.5 | Two-stage skin graft | 5.5 | No recurrence | Excellent | Excellent |
| 4 | 85/F | SC | 12 × 12 | 15 × 22 | Two-stage skin graft | 5 | No recurrence | Excellent | Good |
| 5 | 55/M | SC | 6 × 8 | 11 × 22 | Lateral orbital flap | 3 | No recurrence | Excellent | Excellent |
| 6 | 77/F | BCC | 7 × 7 | 9 × 13 | None | 1 | No recurrence | Excellent | Excellent |
MCC: Merkel cell carcinoma; SC: sebaceous carcinoma; BCC: basal cell carcinoma.
Figure 4.
Three years after the surgery (Patient 5). A: The eyelid appearance and function remain in excellent condition. B: In the bipedicled orbicularis oculi myocutaneous flap, a double eyelid fold has been secondarily created using 6–0 nylon buried sutures. C: When the eyelids are firmly closed, the reconstructed eyelid shows strong contracture of the orbicularis oculi muscle, which is .similar to that of the contralateral eyelid.
Patients
We performed upper eyelid reconstruction using the modified method in six patients with malignant upper eyelid tumours. Three patients had sebaceous carcinoma, two had basal cell carcinoma, and one had Merkel cell carcinoma. The donor sites of the orbicularis oculi myocutaneous flaps were repaired using a median forehead flap in the patient with Merkel cell carcinoma, a lateral orbital flap in one patient with sebaceous carcinoma, and a two-stage skin graft in two patients (one with basal cell carcinoma and the other with sebaceous carcinoma). The two remaining patients required no donor site repair (Table 1).
In Patient 1, since Merkel cell carcinoma is a highly malignant tumour, we avoided using a flap harvested from the area downstream of the lymph flow and instead used a median forehead flap.
In Patient 3, we could not use a lateral orbital flap since the patient's lateral orbital area had already been reconstructed with skin grafts to repair multiple haemangiomas. In Patient 2, donor site repair was performed with a skin graft, since the patient was in poor condition and desired a less invasive procedure. For Patients 2 and 3, a two-stage skin graft with an aesthetic skin graft technique10 was used to avoid suboptimal cosmetic outcomes (Table 1). All patients underwent complete tumour resection as confirmed by frozen section monitoring of the cutaneous, subcutaneous, and conjunctival margins.
All clinical information was collected after the patients provided written informed consent, and the study was approved by the institutional review board of the National Hospital Organization, Osaka National Hospital (IRB No: 20,074).
All patients provided informed consent, including for having their faces shown in the figures.
Assessment scores
Functional and cosmetic outcomes were assessed using postoperative photographs by six evaluators (one secretary, one clerk, two surgical trainees, one plastic surgeon, and one ophthalmologist). The postoperative photographs were taken at more than one year after the surgery. Given the importance of bilateral symmetry and optimal eyelid closure in eyelid reconstruction, these factors were scored on a scale of 0–3 points. Total scores were calculated, and functional and cosmetic outcomes were assessed as excellent, good, fair, or poor according to the mean total score amongst the six evaluators (Tables 2 and 3).
Table 2.
Photograph-based functional evaluation scores.
| Status | No asymmetry | Mild asymmetry | Moderate asymmetry | Severe asymmetry |
|---|---|---|---|---|
| 1) Eyelid opened | 3 | 2 | 1 | 0 |
| 2) Eyelid gently closed | 3 | 2 | 1 | 0 |
| 3) Eyelid firmly closed | 3 | 2 | 1 | 0 |
Total score (TS) was calculated as the sum of 1), 2), and 3).
Poor, 0 ≤ mean TS < 2.25; Fair, 2.25 ≤ mean TS < 4.5; Good, 4.5≤ mean TS < 6.75; Excellent, 6.75 ≤ mean TS ≤ 9.
Table 3.
Photograph-based cosmetic evaluation scores.
| Features | Excellent | Good | Fair | Poor |
|---|---|---|---|---|
| 1) Eyelid colour match | 3 | 2 | 1 | 0 |
| 2)Eyelid texture match | 3 | 2 | 1 | 0 |
| 3)Bilateral symmetry | 3 | 2 | 1 | 0 |
Total score (TS) was calculated as the sum of 1), 2), and 3).
Poor, 0 ≤ mean TS < 2.25; Fair, 2.25 ≤ mean TS < 4.5; Good, 4.5 ≤ mean TS < 6.75; Excellent, 6.75 ≤ mean TS ≤9.
Results
Case report
A representative case (Patient 5; Table 1) is presented below.
A 55-year-old man with sebaceous carcinoma on the right upper eyelid margin was referred to our hospital by an ophthalmologist (Figure 3A). The tumour was resected with a 7 mm margin, which is wider than usual, since pagetoid spread was observed in the epidermis of a biopsy specimen. The defect was reconstructed with a bipedicled orbicularis oculi myocutaneous flap and a labial mucosal graft. The donor site of the bipedicled myocutaneous flap was repaired with a lateral orbital flap (Figures 2A,B,3B-E). Seven months after the surgery, a double eyelid fold was created in the bipedicled myocutaneous flap with 6–0 nylon buried sutures(Figure 4B). Three years after the initial surgery, the eyelid appearance and function remained in excellent condition (Figures 4A,B), and when the eyelids are firmly closed, the reconstructed eyelid shows strong contracture of the orbicularis oculi muscle, which is .similar to that of the contralateral eyelid.(Figure 4C). The patient had no recurrence and remains in good health.
Functional and cosmetic outcomes
The results of the six patients who underwent upper eyelid defect reconstruction with this modified method (innervated orbicularis oculi myocutaneous flaps and labial mucosal grafts) are summarized in Table 1. Although labial mucosal grafts were used to reconstruct the inner lining, no in-turning of the eyelid due to shrinkage of the mucosal graft was observed in any of the patients.
Only one patient (Patient 1) showed reduced orbicularis oculi muscle function due to sacrifice of facial nerve branches during the wide resection of a metastatic lesion in the deep parotid gland eight months after the initial surgery. The other five patients demonstrated complete recovery of eyelid function; when their eyelids were firmly closed, orbicularis oculi muscle contracture was clearly observed in the reconstructed eyelid, as in the contralateral eyelid (Figure 4C). All but one patient (who was assessed as ‘good’) were assessed as ‘excellent’ in terms of functional outcome.
In all but one patient (Patient 1) with Merkel cell carcinoma, who suffered from left facial palsy (Table 2), the lower eyelid was intact with a perfectly symmetrical appearance and function. Additionally, the reconstructed eyelids had a very natural appearance in these patients. The patient with Merkel cell carcinoma who underwent donor site repair with a median forehead flap had a suboptimal cosmetic outcome due to the use of a thick-skinned forehead flap. The remaining five patients showed excellent or good morphological results (Table 3). The labial donor sites, which were covered with artificial dermis, were re-epithelialized by two to three weeks postoperatively with no deformity.
Discussion
In this report, we describe a modified version of a method described by Moschella and Cordova, which uses a innervated (functional) bipedicled orbicularis oculi myocutaneous flap harvested from the upper eyelid itself to repair full-thickness upper eyelid defects, and a full-thickness labial mucosal graft to reconstruct the inner lining.4 By introducing two modifications (i.e., avoiding Fricke flaps to repair the donor site and reconstructing double-fold eyelids in secondary surgeries), our method improved the cosmetic appearance of the face, including eyebrow symmetry and achieved a more natural double-fold eyelid (or single-fold eyelid) for Asian people.
A smooth mucosal or conjunctival inner lining is necessary to protect the cornea. A number of techniques have been described for the repair of the inner lining.7,11,12 Tarsoconjunctival grafts from the normal upper eyelid can be used to achieve satisfactory results for upper eyelid reconstruction but can compromise outcomes for the donor eyelid (e.g., cicatricial entropion, upper eyelid retraction) .7,13
Since the muscle fibres included in an orbicularis oculi myocutaneous flap maintain good muscle tone, which stabilizes the lid margin, some have suggested that cartilaginous solid tissues are not necessary for eyelid support.14,15 We used mucosal grafts from the lower lip as described by Moschella and Cordova. These grafts are smoother and more flexible than grafts from other tissues used to reconstruct the lining. Although some reports showed that the mucosal grafts used in eyelid reconstruction shrink substantially in the postoperative period,16 we observed no in-turning of the eyelid due to shrinkage of the mucosal graft in our patients. We suspect that the good muscle tone of the orbicularis oculi muscle flap may have prevented shrinkage of the mucosal graft.
For donor site repair, we avoided using a Fricke flap and instead used other methods to repair the donor site, such as a median forehead flap,a lateral orbital flap, and second-stage skin grafts, according to the condition of each patient (Table 1). Flaps harvested from the forehead produce a thick-skinned eyelid with suboptimal colour/texture match.17 On the other hand, lateral orbital flaps have a better colour/texture match than flaps from the forehead. Moreover, they leave almost invisible donor site scars and do not result in eyebrow asymmetry, as is observed with Fricke flaps.8,9 In our view, lateral orbital flaps are optimal for repairing the donor site of the bipedicled orbicularis oculi myocutaneous flap. In the present study, when the lateral orbital flap was not available, we used other methods as shown in Table 1.
Since our method requires the skin and orbicularis oculi muscle below the eyebrow to be more than 8 mm wide in the vertical direction, it cannot be used in patients who have a defect in that area, such as a total defect of the upper eyelid or a large defect in the vertical direction.
Since our method does not sacrifice the lower eyelid, there is no damage to its appearance or function. Moreover, there is no need to keep the eye closed for several weeks. The use of myocutaneous flaps that include innervated (functional) orbicularis oculi muscle also achieves good muscle tone of the upper eyelid, which keeps the lid in close contact with the globe without cartilaginous solid support and optimal eyelid closure. The modified method can be applied to patients with single-fold eyelids or narrow double-fold eyelids, and optimal outcomes can be obtained by selecting an appropriate method to repair the donor site of the bipedicled orbicularis oculi myocutaneous flap according to each patient's condition.
In conclusion, good to excellent outcomes, both functionally and morphologically, can be achieved with this method in most patients. The method offers a useful, simple, and less invasive alternative to other methods of conventional upper eyelid reconstruction.
Role of the funding source
None.
Ethical approval
The study was approved by the institutional review board of the National Hospital Organization, Osaka National Hospital (IRB No: 20,074).
Declaration of Competing Interest
None.
References
- 1.Mustarde J.C. Churchill Livingstone; New York: 1991. Repair and Reconstruction in the Orbital Region; pp. 125–296. [Google Scholar]
- 2.Spinelli H.M., Jelks G.W. Periocular reconstruction: a systematic approach. Plast Reconstr Surg. 1993;91:1017–1023. [PubMed] [Google Scholar]
- 3.Cutler N.L., Beard C. A method for partial and total upper lid reconstruction. Am J Ophthalmol. 1955;39:1–7. doi: 10.1016/0002-9394(55)92646-5. [DOI] [PubMed] [Google Scholar]
- 4.Moschella F.1., Cordova A. Upper eyelid reconstruction with mucosa-lined bipedicled myocutaneous flaps. Br J Plast Surg. 1995;48:294–299. doi: 10.1016/0007-1226(95)90067-5. [DOI] [PubMed] [Google Scholar]
- 5.Fujiwara M. Upper eyelid reconstruction with a hard palate mucosa-lined bipedicled myocutaneous flap. J Craniofac Surg. 2006;17:1011–1015. doi: 10.1097/01.scs.0000229553.20200.d5. [DOI] [PubMed] [Google Scholar]
- 6.Kadowaki M., Katsuno M. Takagi. Reconstruction of subtotal full-thickness upper eyelid defect using a bipedicle skin-orbicularis oculi muscle flap and lateral orbital flap. Skin Surg. 2010;19:133–136. [Google Scholar]
- 7.Patrinely J.R., O'Neal K.D., Kersten R.C., Soparkar C.N. Total upper eyelid reconstruction with mucosalized tarsal graft and overlying bipedicle flap. Arch Ophthalmol. 1999;117:1655–1661. doi: 10.1001/archopht.117.12.1655. [DOI] [PubMed] [Google Scholar]
- 8.Fricke J.C.G. Perthes & Besser; Hamburg: 1829. Building Neurer Augen linder (Blephalroplastik) [Google Scholar]
- 9.Ogawa. Y. Socket reconstruction by lateral orbital flap. Jpn J Plast Reconstr Surg. 1998;41:125–129. [Google Scholar]
- 10.Yoshitatsu S., Takagi T. A new tie-over method improves cosmetic results. Dermatol Surg. 2002;28:542–543. doi: 10.1046/j.1524-4725.2002.22043.x. [DOI] [PubMed] [Google Scholar]
- 11.Cohen M.S., Shorr N. Eyelid reconstruction with hard palate mucosa grafts. Ophthal Plast Reconstr Surg. 1992;8:183–195. doi: 10.1097/00002341-199209000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Hughes W.L. Reconstructive Surgery of the Eyelids. 2nd ed. St Lois. Mo: CV Mosby Co; 1954. Upper eyelid reconstruction; pp. 92–96. [Google Scholar]
- 13.Hawes M.J., Jamell G.A. Complications of transconjunctival grafts. Opthal Plast Reconstr Surg. 1996;12:45–50. doi: 10.1097/00002341-199603000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Goldstein M.H. Orbiting the orbicularis"–restoration of muscle-ring continuity with myocutaneous flaps. Plast Reconstr Surg. 1983;72:294–301. doi: 10.1097/00006534-198309000-00003. [DOI] [PubMed] [Google Scholar]
- 15.van der Meulen J.C. Reconstruction of the medial half of the lower eyelid using a "switch" split-lid procedure. Plast Reconstr Surg. 1991;88:718–722. doi: 10.1097/00006534-199110000-00027. [DOI] [PubMed] [Google Scholar]
- 16.Leone C.R., Jr. Mucous membrane grafting for cicatricial entropion. Ophthalmic Surg. 1974;5:24–28. [PubMed] [Google Scholar]
- 17.Breier F., Meissl G., Diem F. Functional reconstruction of the upper eyelid after excision of squamous cell carcinoma in xeroderma pigmentosum. Plast Reconstr Surg. 1997;99:1730–1733. [PubMed] [Google Scholar]