Abstract
Emphysematous cystitis is a rare disorder that is usually associated with immunosuppression, poorly controlled diabetes mellitus, and other risk factors such as previous urinary tract infection and/or recent instrumentation of the urinary tract. The case of an 89-year-old woman with emphysematous cystitis who had no evidence of immunodeficiency or other risk factors except for advanced age is reported. A review of the literature on emphysematous cystitis in immunocompetent, nondiabetic individuals is presented.
Keywords: diabetes, emphysematous cystitis, nonimmunocompromised hosts
Emphysematous cystitis is an uncommon infection that occurs mostly in diabetics and immunocompromised patients. It is uncommon in immunocompetent, nondiabetic patients. We describe a case of emphysematous cystitis in an elderly, nondiabetic, nonimmunocompromised patient. We also summarize the available literature regarding data on immunocompetent patients with emphysematous cystitis.
Case Presentation
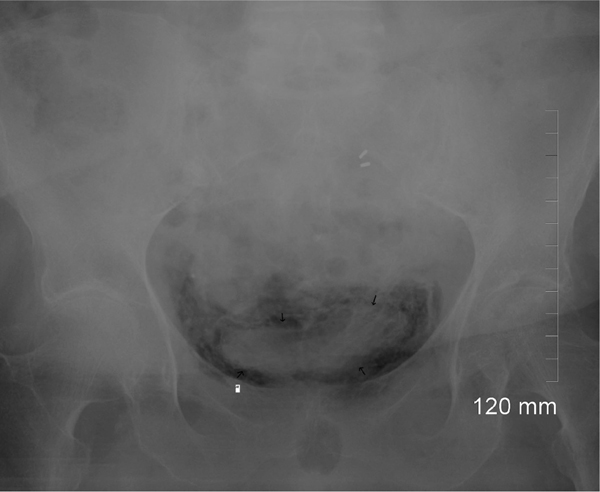
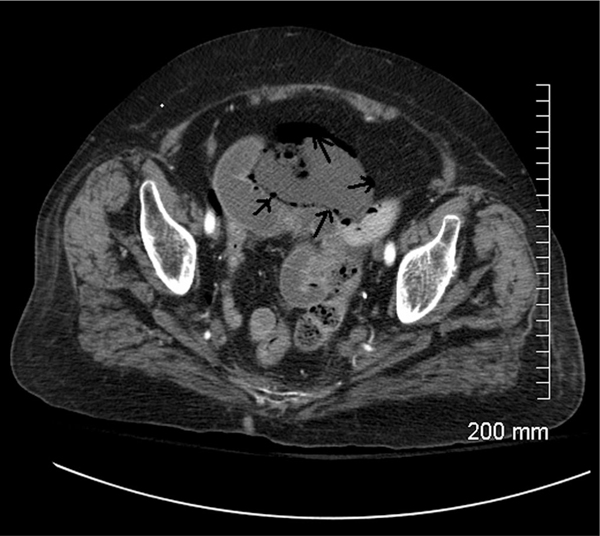
An 89-year-old woman presented to the hospital after a mechanical fall while walking. Her past medical history was significant for chronic obstructive pulmonary disease, osteoarthritis and hypertension. On further questioning, she had mild abdominal discomfort and chronic back pain. On physical examination, she was afebrile with a temperature of 98.6°F and was hemodynamically stable with suprapubic tenderness. Initial pertinent laboratory data included a white cell count of 19.5 × 109/L with 92.2% polymorphonuclear cells, a random blood glucose of 110 mg/dL, with normal renal and liver functions and serum electrolytes. A urinalysis revealed pyuria and bacteriuria, whereas a urine culture which was obtained after initiation of antibiotic therapy was negative. An x-ray of the spine and pelvis did not reveal any fractures. A plain abdominal x-ray showed air within the wall of urinary bladder (Fig. 1). A computed tomography of the abdomen and pelvis revealed air in the bladder wall, suggestive of emphysematous cystitis (Fig. 2) and confirmed the absence of any fractures. The patient received three doses of intravenous ciprofloxacin, and she developed delirium which was thought to be caused by ciprofloxacin. Since the patient reported a known allergy to penicillin she received intravenous aztreonam for 5 more days to finish a 7-day course of antibiotic treatment. She responded with improvement of her abdominal discomfort and a decline in her white cell count. Her hospital course was complicated by the development of atrial fibrillation, but she recovered and was discharged to a rehabilitation facility. A repeat abdominal x-ray film which was performed one month after the patient was discharged showed resolution of the air within the wall of the urinary bladder.
Fig. 1.
A plain abdominal x-ray showing air within the wall of the urinary bladder (arrows).
Fig. 2.
A computed tomography of the abdomen and pelvis revealing air in the bladder wall (arrows).
Discussion
Definition and Risk Factors
Emphysematous cystitis is a complication of urinary tract infection, characterized by the spontaneous appearance of gas within the bladder wall or in the bladder. Emphysematous cystitis is a relatively uncommon condition, usually seen in patients who are either diabetic or have other immunosuppressive diseases.1 The major risk factors for the disease include old age and female sex, diabetes mellitus, urinary tract outlet obstruction of any degree or cause (benign prostatic hypertrophy, urethral stricture, neurogenic bladder), structural abnormalities of the bladder, or indwelling urinary catheters and chronic urinary tract infection.1–3 It has also been reported with other pre-existing conditions such as alcoholism,4 undernutrition5 or a disabled general medical condition.1 Other risk factors for emphysematous cystitis include hemorrhagic cystitis, alcoholic liver disease,6 broad spectrum antibiotics, penetrating injury to the bladder, instrumentation including cystoscopy, vesicorec or vesicovaginal fistula, and the presence of vesical diverticula.1,7 In a recent review of 135 cases of emphysematous cystitis, 90/135 patients were diabetic (66.6%).8 Grupper et al1 reviewed 53 reported cases of emphysematous cystitis, and 69.8% were found to be diabetic (37/53) and 30.2% (16/53) were nondiabetic. Four of the diabetic patients and four of the nondiabetic patients had other immunosuppressive conditions such as alcohol abuse (4 cases), malnutrition (2 cases), immunosuppressive therapy (2 cases), solid cancer (1 case), and hematologic malignancy (3 cases). Twelve of the nondiabetic patients were nonimmunocompromised. The most common urinary tract pathologies reported were neurogenic bladder (5 cases), and a history of recurrent urinary tract infection (4 cases). Bailey et al7 found that diabetes occurred in 15/19 (80%) of a series of cases with emphysematous cystitis. Other conditions that have been associated with emphysematous cystitis include end stage renal disease cystic fibrosis,9,10 renal transplantation, renal infarction, and systemic lupus erythematosus.11 Use of immunosuppressive agents such as cyclophosphamide12,13 and corticosteroids has also been associated with emphysematous cystitis.13
Methods
However, emphysematous cystitis in nondiabetic immunocompetent patients is rare. Of the 53 cases of emphysematous cystitis described in the most recent review about this clinical entity, 12 (22.6%) had neither immunosuppressive comorbidity nor diabetes,1 but no further details on these patients were provided by the authors.1 Although emphysematous cystitis has been reviewed in other reports,1,3 cases of emphysematous cystitis in nondiabetic and nonimmunocompromised patients have not been reviewed before in the literature. All cases included in our literature review were found using a PubMed search (1970-January 2009) of the English language medical literature applying the terms “emphysematous cystitis” or “cystitis emphysematosa.” The references cited in these articles were examined to identify additional reports. Cases in which patients were immunocompetent and nondiabetic but had other immunosuppressive conditions which have been associated with emphysematous cystitis, including alcohol abuse4,6 or malnutrition,3,14 were excluded from our review. Old age was not used as exclusion criterion.
Results
We identified 15 cases of emphysematous cystitis described in nondiabetic, immunocompetent patients (Table).5,10,15–27 In 3 cases, the patients described were immunocompetent but had known risk factors that were associated with emphysematous cystitis such as neurogenic bladder,18 enterovesical fistula,21 and urinary obstruction.26 Thus, 12 cases were included in our final analysis.5,10,15–17,19,20 In one case,10 a nondiabetic patient had cystic fibrosis, which had been previously associated with emphysematous cystitis, but only in the context of coexisting diabetes mellitus.9,10 The mean age of the nondiabetic, nonimmunocompromised patients with emphysematous cystitis was 57 ± 22 years (range, 21–90 yr). The majority of patients were female (7/12, 58.3%). Five cases (41.7%) were described in America,10,20,22,24,27 4 (33.4%) in Asia,5,19,23,25 and 3 cases (25%) were described in Europe.15–17 Abdominal pain was the most common symptom and was noticed in 9/12 (75%) of cases. Escherichia coli was the most common pathogen that was isolated in 7/10 (70%) cases. No culture data was reported in one case20 and urine culture was negative in another case.24 Details on the antibiotic therapy were available only in 5 cases (41.7%) (Table).5,17,19,23,24 All patients except for one16 survived and recovered.
Table.
Cases of emphysematous cystitis in non-diabetic immunocompetent patients
| Author Year | Country | Patient Age | Patient Sex | Patient Characteristics | Symptoms | Pathogen | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Beri 200810 | USA | 21 | F | Cystic fibrosis, non diabetic | Productive cough, fever, cramping, lower abdominal pain | Mixed organisms | Antibiotics (NR) for 14 days | Recovered |
| Lakhal 200815 | France | 55 | M | Aortic valve replacement | Pelvic pain | Enterobacter cloacae | Data not reported | Recovered |
| Leclerq 200816 | Belgium | 77 | F | Non diabetic | Confusion, hypertdermia and abdominal pain | E coli | Intravenous antibiotics (NR) and bladder catheterization | Died |
| Thomas 200617 | Ireland | 80 | M | Non diabetic, Ulcerative colitis | Pyrexia, abdominal pain, and haematuria | E coli | Gentamicin and piperacillin/tazobactam then cefuroxime | Recovered |
| Ahmad M 200419 | India | 36 | M | Non diabetic | Fever, vomiting, dysuria, oliguria and left flank pain of four days duration |
Aspergillus fumigatus | Patient had refused any surgical intervention. He was treated successfully with liposomal amphotericin B and 5-flucytosin | Recovered |
| Al-Assiri 200420 | Canada | 58 | M | Non diabetic with acute pancreatitis | Epigastric pain, nausea, vomiting and symptoms of acute pancreatitis. Incidental finding on CT of abdomen |
No culture data reported | Antibiotics (NR) | Recovered |
| Ebe 20035 | Japan | 27 | F | Eating disorder and schizophrenia | Severe weight loss and psychotic symptoms | E coli | Piperacillin initially, followed by ceftazidime | Recovered |
| O’Connor LA 200122 | USA | 90 | F | Nursing home resident, hypertension | Abdominal pain and distention | E coli | Foley catdeter was placed and intravenous antibiotics (NR) (7 days) | Recovered |
| Mimata 200023 | Japan | 56 | F | Non diabetic. Brain contusion might have induced temporal bladder dysfunction | Lower abdominal pain, dysurea 7 days after admission |
E coli | Antibiotics for 7days (cefotiam IV) | Recovered |
| Weddle 199824 | USA | 76 | F | Non diabetic, hypertension | Abdominal pain, diarrhea | Negative culture | Bladder irrigation, intravenous antibiotic therapy with cefazolin, gentamicin, and metronidazole then oral ofloxacin and metronidazole | Recovered |
| Lee G 199825 | Korea | 67 | F | Non diabetic, history of pulmonary tuberculosis and gallstones | Abdominal pain, flank pain | E coli | Antibiotics | Recovered |
| Davidson 199527 | USA | 45 | M | Immunocompetent, hypospadias | Painless gross hematuria | E coli | Antibiotics | Recovered |
Abbreviations: NR: Not reported; F: female; M: male; CT, computed tomography.
Pathogenesis
The pathogenesis, clinical manifestations and treatment of emphysematous cystitis have been reviewed elsewhere.1 It is postulated that emphysematous cystitis occurs due to the fermentation of glucose or albumin by gas-forming organisms within the wall of the urinary bladder. In nondiabetic patients, impaired host response associated with impaired vascular supply has been implicated in the pathogenesis of emphysematous renal disease.
Clinical Manifestations
The clinical features are inconclusive. Common presenting features include abdominal and flank pain, tenderness, pneumaturia, and other common symptoms of urinary tract infection including hematuria, dysuria, frequency, and fever. Abdominal pain is the most common symptom of emphysematous cystitis, occurring in up to 80% of cases.1,3 However, the classic symptoms of acute cystitis (dysuria, urinary frequency, and urinary urgency) occurred in only about one-half of patients.1,3 A history of pneumaturia is highly suggestive but is rarely offered by the patient.
Diagnosis
The radiologic findings provide the most reliable diagnostic clues. Demonstration of intramural gas in the wall of the urinary bladder is the basis for the radiologic diagnosis of emphysematous cystitis. Diagnosis can be made on a plain x-ray film of the abdomen and typical imaging shows a curvilinear area of radiolucency delineating the bladder wall. Plain abdominal x-ray is sensitive, however, it lacks specificity. Abdominal computed tomography is the most useful imaging tool when symptoms do not easily lead to diagnosis and can reveal air bubbles within the lumen or the wall of the urinary bladder. There is no adequate evidence about the use of magnetic resonance imaging for the diagnosis of emphysematous cystitis. Laboratory testing usually reveals pyuria and hematuria with positive urine cultures. In a recent review of cases of emphysematous cystitis, urine cultures were positive for Escherichia coli in 57.4% of cases and Klebsiella pneumoniae in 21.3%.1 Other organisms reportedly associated with emphysematous cystitis include Enterobacter aerogenes, Proteus mirabilis, Staphylococcus aureus, streptococci, Clostridium perfringens, and Candida albicans.1,3 Polymicrobial infection was occasionally seen. Bacteremia was present in approximately one-half of cases.1,3
Treatment
Emphysematous cystitis can usually be treated with medical therapy alone. Treatment in most cases includes antibiotic therapy for the urinary tract infection and adequate bladder drainage with bladder catheterization. However, bladder irrigation may be needed if the patient cannot adequately void or blood clots are present. Surgical intervention is appropriate only in cases with urinary tract obstruction, stone, or other anatomic abnormality and for complications like peritonitis, pneumoperitoneum, and perivesical abscess formation. Treatment duration depends on the clinical response, but antibiotics are necessary during a mean of 7–10 days.1–3 In the majority of the described cases, the duration of treatment is usually extended to 7 days to avoid the development of complications and recurrence. The prognosis is generally good with the majority of cases resolving within four days of therapy1 except in those patients who exhibit systemic organic dysfunction. Delayed diagnosis may lead to unfavorable outcomes including overwhelming infection, extension to the ureters and the renal parenchyma, bladder rupture, and death.1,3
Conclusion
We describe a case of emphysematous cystitis in a nondiabetic, nonimmunocompromised elderly patient and we summarize the pertinent literature for the first time. The only risk factors for emphysematous cystitis in our patient were old age and female sex. Emphysematous cystitis can present asymptomatically. In such instances the diagnosis should be suspected based on imaging findings. Physicians should be aware of the potential lack of typical symptoms and the association of this clinical entity with nonimmunocompromised individuals. Aggressive pursuance of imaging studies should guide the early diagnosis. Rapid appropriate intervention by an alert physician in these difficult cases will lead to a better patient outcome.
Morning at the Window.
They are rattling breakfast plates in basement kitchens,
And along the trampled edges of the street I am aware of the damp souls of housemaids Sprouting despondently at area gates.
The brown waves of fog toss up to me
Twisted faces from the bottom of the street,
And tear from a passer-by with muddy skirts An aimless smile that hovers in the air And vanishes along the level of the roofs.
—T.S. Eliot
Key Points.
Emphysematous cystitis is an uncommon infection tdat occurs mostly in diabetics.
Emphysematous cystitis can present asymptomatically. In such instances, tde diagnosis should be suspected based on imaging findings.
Physicians should be aware of tde potential lack of typical symptoms and tde possible presentation of tdis clinical entity in nonimmunocompromised individuals.
Rapid, appropriate intervention by an alert physician in tdese difficult cases will lead to a better patient outcome.
References
- 1.Grupper M, Kravtsov A, Potasman I. Emphysematous cystitis: illustrative case report and review of the literature. Medicine (Baltimore) 2007; 86:47–53. [DOI] [PubMed] [Google Scholar]
- 2.Greene MH. Emphysematous cystitis due to Clostridium perfringens and Candida albicans in two patients with hematologic malignant conditions. Cancer 1992;70:2658–2663. [DOI] [PubMed] [Google Scholar]
- 3.Quint HJ, Drach GW, Rappaport WD, Hoffmann CJ. Emphysematous cystitis: a review of the spectrum of disease. J Urol 1992;147:134–137. [DOI] [PubMed] [Google Scholar]
- 4.O’Connor P, Davies M, Feely J. Emphysematous cystitis–another alcohol-related problem? Ir Med J 1987;80:420–421. [PubMed] [Google Scholar]
- 5.Ebe T, Oshima H, Takeda N, Matsumoto T. Emphysematous cystitis developed in a patient with an eating disorder and schizophrenia. J Infect 2003;47:260–261. [DOI] [PubMed] [Google Scholar]
- 6.Becker TM, Holmes KK. An alcoholic woman with air in the bladder wall. Hosp Pract (Off Ed) 1985;20:34F, 34H. [DOI] [PubMed] [Google Scholar]
- 7.Bailey H Cystitis emphysematosa; 19 cases with intraluminal and interstitial collections of gas. Am J Roentgenol Radium Ther Nucl Med 1961;86:850–862. [PubMed] [Google Scholar]
- 8.Thomas AA, Lane BR, Thomas AZ, Remer EM, Campbell SC, Shoskes DA. Emphysematous cystitis: a review of 135 cases. BJU Int 2007;100: 17–20. [DOI] [PubMed] [Google Scholar]
- 9.Upadhyay D, Jain M. Emphysematous cystitis and renal stones in cystic fibrosis. JAMA 2004;292:1953–1954. [DOI] [PubMed] [Google Scholar]
- 10.Beri A, Dwamena F. A Case of Emphysematous Cystitis in Cystic Fibrosis. South Med J 2009;102:89–90. [DOI] [PubMed] [Google Scholar]
- 11.Granel B, Serratrice J, Juhan V et al. Lupus cystitis: a possible additive risk factor for emphysematous cystitis in diabetes mellitus: discussion about one case. Lupus 2000;9:72–73. [DOI] [PubMed] [Google Scholar]
- 12.Galloway NT. Gas gangrene of the bladder complicating cyclophosphamide cystitis. Br J Urol 1984;56:100–101. [DOI] [PubMed] [Google Scholar]
- 13.Abuzarad H, Gadallah MF, Rabb H, Vermess M, Ramirez G. Emphysematous cystitis: possible side-effect of cyclophosphamide therapy. Clin Nephrol 1998;50:394–396. [PubMed] [Google Scholar]
- 14.Dinkel HP, Lourens S, Brehmer U, Pfammatter R, Triller J, Vock P. Emphysematous cystitis in a patient presenting with paradoxical arterial embolism and intestinal mycobacteriosis without evidence of diabetes. Eur Radiol 2001;11:246–249. [DOI] [PubMed] [Google Scholar]
- 15.Lakhal K, Paubelle E. Emphysematous cystitis. Lancet 2008;372:1184. [DOI] [PubMed] [Google Scholar]
- 16.Leclercq P, Hanssen M, Borgoens P, Bruyere PJ, Lancellotti P. Emphysematous cystitis. CMAJ 2008;178:836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas AA, Long RM, Creagh TA, Patchett S. Emphysematous cystitis in an elderly patient with ulcerative colitis. Ir Med J 2006;99:56–57. [PubMed] [Google Scholar]
- 18.Karashima E, Ejima J, Nakamura H, Koike A, Kaneko T, Ohmura I. Emphysematous cystitis with venous bubbles. Intern Med 2005;44:590–592. [DOI] [PubMed] [Google Scholar]
- 19.Ahmad M Emphysematous pyelonephritis due to Aspergillus fumigatus: a case report. J Nephrol 2004;17:446–448. [PubMed] [Google Scholar]
- 20.Al-Assiri M, Chan P. Incidental discovery of emphysematous cystitis with rapid resolution in a patient presenting with acute pancreatitis. Scientific World Journal 2004:881–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Forestier D, Valero S, Paccalin M. A case of emphysematous cystitis. Gerontology 2004;50:259. [DOI] [PubMed] [Google Scholar]
- 22.O’Connor LA, De GJ. Emphysematous cystitis: a radiographic diagnosis. Am J Emerg Med 2001;19:211–213. [DOI] [PubMed] [Google Scholar]
- 23.Mimata H, Tasaki Y, Nomura Y. Emphysematous cystitis following brain contusion. Urol Int 2000;64:165–166. [DOI] [PubMed] [Google Scholar]
- 24.Weddle J, Brunton B, Rittenhouse DR. An unusual presentation of emphysematous cystitis. Am J Emerg Med 1998;16:664–666. [DOI] [PubMed] [Google Scholar]
- 25.Lee G, Choi PS, Woo DS, Park HC, Kim HJ, Lee YH. Emphysematous cystitis. J Korean Med Sci 1998;13:215–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fernandes LP, Sajwany MJ, Derweesh A. Emphysematous pyelonephritis and cystitis associated with bilateral pelviureteric junction obstruction: a case report. J Pediatr Surg 1998;33:739–740. [DOI] [PubMed] [Google Scholar]
- 27.Davidson J, Pollack CV Jr. Emphysematous cystitis presenting as painless gross hematuria. J Emerg Med 1995;13:317–320. [DOI] [PubMed] [Google Scholar]