Abstract
Background
Mental health symptoms are considered a public health concern by many professionals and are frequently impacted by factors related to occupation, employment opportunities, and economic stressors. This study investigated the relationship between economic stressors and mental health symptoms among Bangladeshi rehabilitation professionals.
Methods
We conducted a cross-sectional survey of 420 rehabilitation professionals between July 2020 and October 2020. Economic stressors were measured using Economic Hardship Questionnaire, Financial Threat Scale, and Financial Well-Being Scale. Mental health symptoms were measured using the Depression, Anxiety, and Stress Scale (DASS-21). Multivariable logistic regression analysis was performed to find associated factors on mental health problems after adjusting confounders.
Results
Among 420 rehabilitation professionals 62.1% were male, 38.6% were post-graduated and 75% were in practice. The overall prevalence of depression, anxiety, and stress was 51.0%, 58.6%, and 33.6%, respectively. The multivariable regression analysis indicated that without a high professional degree, lack of opportunity to practice, and loss of income were the associated factors for mental health symptoms. The modelling of the structural equation showed that financial threat is significantly associated with mental health symptoms.
Conclusion
During the era of COVID-19, a high prevalence of mental health symptoms was observed among rehabilitation professionals. To minimize the burden of mental health, we recommend that all rehabilitation organizations and the government come together to create equal opportunities to practice and enable individuals to obtain high professional degrees.
Keywords: Bangladesh, COVID-19, Depression, Anxiety, Stress, Economic stressors, Financial stress, Rehabilitation professionals
Bangladesh; COVID-19; Depression; Anxiety; Stress; Economic stressors; Financial stress; Rehabilitation professionals.
1. Introduction
Fifteen percent of the world population lives with chronic or residual disabilities around the globe [1]. World Health Organization and World Bank report estimated that the prevalence of disability in Bangladesh can be reached up to 31.9% [2]. A systematic analysis of the Global Burden of Diseases data suggested that 2.4 billion individuals, one in every three people in the world, need rehabilitation for disability at any point of their course of illness or injury [3]. The rehabilitation professionals (RP) include physical therapist (PT), occupational therapist (OT), speech and language therapists (SLT), prosthetic and orthotic practitioners, and PT/OT assistants are trained to service providers for a huge number of people with disability [1]. Despite the worldwide scarcity of RP, they are facing heterogeneity and negligence in the healthcare system [4, 5, 6]. Especially, in low- and middle-income countries like Bangladesh, the rehabilitation sector receives less attention from the governments, and professionals are offered limited employment opportunities [5].
In Bangladesh, the regulatory body for RP is yet to start working, thus the government does not register the RP. Information from professional organizations for the RP and published literature suggested that there are about 2000 RP has been graduated so far in Bangladesh giving one of the world's lowest rate of RP (i. e., ≤0.1) per 10,000 people [5, 7, 8]. Nonetheless, unlike other medical graduates, for example, physicians, dentists, and homoeopaths, the government does not offer an employment position to RP for the mainstream government healthcare system [9]. Only a few government projects recruit a limited number of RP as temporary contractual low-paid employees [10]. These heterogeneities may produce some major negative consequences; for example: (1) the healthcare system fails to meet rehabilitation service needs, (2) disabled patients get narrowest possible access to RP and, (3) RP do not get desired employments and professional recognition. Consequently, a large number of graduate RP left the profession, migrated to a developed country, and remained unemployed or adopted underemployment in Bangladesh [11].
Involuntary underemployment and/or unemployment (UUE) is associated with poor mental health [12, 13]. Multiple factors derived from the UUE situation, for example, economic anguish and joblessness, employment insecurity, continuous underlie feelings of failure, which severely may lead to common mental health symptoms such as depression, anxiety, and stress [14, 15]. And these mental health problems significantly reduce productivity and quality of life and responsible for most suicide casualties [16, 17, 18, 19, 20, 21]. Besides, a systematic review and meta-analysis concluded that vulnerability of suicidal behaviour can also be exacerbated by UUE induced stressful life outcomes such as financial threats [22].
An enormous financial threat to the world population has been imposed as an impact of the COVID-19 pandemic and predictably, the UUE groups are the worst victim. Very few researches examined the in-depth association between financial stress and mental health amid COVID-19. A study conducted during this pandemic found that financial constraint was the strongest and common risk factor for depression, anxiety, and insomnia in healthcare workers of Bangladesh [23]. Another study that determined the mental health impact of COVID-19 related lockdown among the Bangladeshi general population found that the unemployed, self-employed, and the private jobholders were in poor mental well-being, whereas, government jobholders showed much better mental adaptation with COVID-19 lockdown [24]. On the other hand, the studies that recently measured the mental health of healthcare workers amid the COVID-19 pandemic addressed only privileged working groups [25, 26]. However, less privileged healthcare workers such as RP are not yet addressed and there is a substantial gap in understanding the mental health status of underprivileged healthcare workers and/or the UUE population during the COVID-19 pandemic time. Therefore, this study examined the effect of economic stressors on mental health symptoms among Bangladeshi rehabilitation professionals during the COVID-19 pandemic.
2. Methodology
2.1. Subjects and procedure
A cross-sectional study was conducted among rehabilitation professionals in Bangladesh between 18 July and 18 October 2020. Seven hundred active members of Bangladesh Physiotherapy/Physical Therapy Association, Bangladesh Occupational Therapy Association, and Bangladesh Speech and Language Therapy Association were invited by email using digital directories strictly maintained by mentioned associations. 492 subjects filled and return the form giving a 70.3% response rate. However, we only included those RP who had completely filled the form, lived in Bangladesh permanently and did not leave the profession. Considering the inclusion and exclusion criteria, finally, we found 420 eligible data for analysis. Most of the participants were PT (n = 372) followed by OT (n = 34) and SLT (n = 14) that reflects the actual number of PT, OT, and SLT in Bangladesh.
2.2. Ethical approval
Ethical approval was taken from the Ethical Review Committee (ERC) of Uttara Adhunik Medical College and Hospital. Prospective observational trial registration has been obtained from the World Health Organization (WHO) endorsed Clinical Trial Registry- India (CTRI/2020/07/026633 [Registered on 17/07/2020]). The study has been conducted strictly following the STROBE guideline [27]. Before participating in the questionnaire, we obtained each participant's informed consent for participation and data collection through a digital form. The study designs, data presentations, and citations of this study comply with the standard Committee on Publication Ethics (COPE) guidelines [28]. Besides, we have read and understood the journal's policies, and we believe that neither the manuscript nor the study violates any of these.
2.3. Independent variables
Self-reported questionnaire composing a wide range of socio-demographic, occupational, and employment-related information, Economic Hardship Questionnaire (EHQ), Financial Threat Scale (FTS), Financial Well-Being Scale (FWBS), were used to collect data.
The socio-demographic variables included age, gender, marital status, exercise habit (30 minutes daily exercise-yes/no), smoking habit (yes, no and quitted), average hours of sleep per night, and hours of daily social media use questionnaire.
Occupational factors were comprised of education level, work experience in year, employer (i.e., hospital/private), service type (i.e., government/non-government). Participants were also reported their current economic condition by a binary response.
The Economic Hardship Questionnaire [29] comprising 10 items (e.g. During the last few years, did you or your family cut back on social activities and entertainment expenses?) with a four-point response scale (1–Never; 4–Very often) was used to evaluate Economic hardship. The EHQ weighs the financial hardships that persons and families experienced in the context of economic adversity. On this scale, higher scores reflect higher financial hardship. Like previous studies [30, 31], high levels of internal consistency were obtained (Cronbach's alpha 0.85) in this study.
The financial threat was evaluated using the Financial Threat Scale [32, 33] consisting of five items (e.g., “What is the likelihood you will have to declare bankruptcy to manage your debt?”) responded to on a five-point Likert scale from 1 (Not at all) to 5 (extremely uncertain). This scale assesses perceptions that persons feel towards their financial situation. In the previous study, a high level of internal constancy was found [30, 34]. Likewise, in this present study, we found a value of Cronbach's alpha as 0.92 which indicates excellent reliability.
For assessing Financial well-being, the Financial Well-Being Scale [35, 36], presenting eight statements (e.g. I am uncomfortable with the amount of debt I am in.) with a five-point Likert scale (1–Strongly disagree; 5–Strongly agree) was used. The FWBS measures wellbeing regarding financial status, where lower scores reflect higher levels of perceived financial wellbeing. High levels of internal consistency were found in previous studies [33, 34]. In the present study, Cronbach's alpha of 0.85 provides good reliability.
2.4. Measurement of depression, anxiety and stress
Depression Anxiety Stress scale 21- item version (DASS-21) [37] which is composed of 21 items (e.g. I felt that I had nothing to look forward to) was used to evaluate stress, anxiety, and depression. Seven items each compose the three dimensions of DASS-21 (i.e., depression, anxiety, and stress). Every item of the scale has a four-point response scale (0 = did not apply to me at all; 3 = applied to me very much, or most of the time-Almost always). Higher scores on each dimension reflect higher depression, anxiety, and stress respectively. The Cronbach's Alpha in this study for depression, anxiety, and stress was found as 0.90, 0.87, and 0.89, respectively that indicate excellent reliability.
The categorization of the DASS-21 score was made following the Pharr approach [13]. We categorized depression as normal 0–9, mild 10–13, moderate 14–20, severe 21–27, and extremely severe +28; anxiety as normal 0–7, mild 8–9, moderate 10–14, severe 15–19, and extremely severe +20, and stress as normal 0–14, mild 15–18, moderate 19–25, severe 26–33, and extremely severe +34.
2.5. Statistical analysis
SPSS version 22.0 and AMOS version 23.0 were used for data analysis. For univariate and multivariable analysis, moderate, severe, and very severe were combined to calculate scores of depression, anxiety, and stress on the DASS-21 [31,38]. In this study, sleeping time, social media using time, financial threat, financial well-being, and economic hardship were measured as continuous variables (note: continuous variables can take on an unlimited number of values between the lowest and highest points of measurement). For continuous variables, independent sample t-tests and Structural Equation Modeling (SEM) analysis were performed to examine the relationship between problematic and non-problematic scores of depression, anxiety, and stress. For categorical data, descriptive statistics (e.g., frequencies, percentages, and chi-squares/Fisher's Exact tests) were used. Multivariable logistic regression models were employed to identify the factors associated with mental health symptoms after adjusting the confounders. The results were interpreted with 95% confidence intervals and p-values. We consider a p-value less than or equal to 0.05 as significant. Furthermore, for SEM, root-mean-square residuals and standardized root-mean residuals lower than 0.08 and 0.05 indicate adequate and good fit respectively [39]. The comparative fit index and goodness of fit index higher than 0.90 and 0.95 indicate adequate and good fit respectively. The bootstrapping method with 95% bias-corrected confidence intervals and 5000 bootstrap samples was used to calculate the standardized beta coefficients between independent and outcome variables.
3. Results
3.1. Prevalence of depression, anxiety, and stress
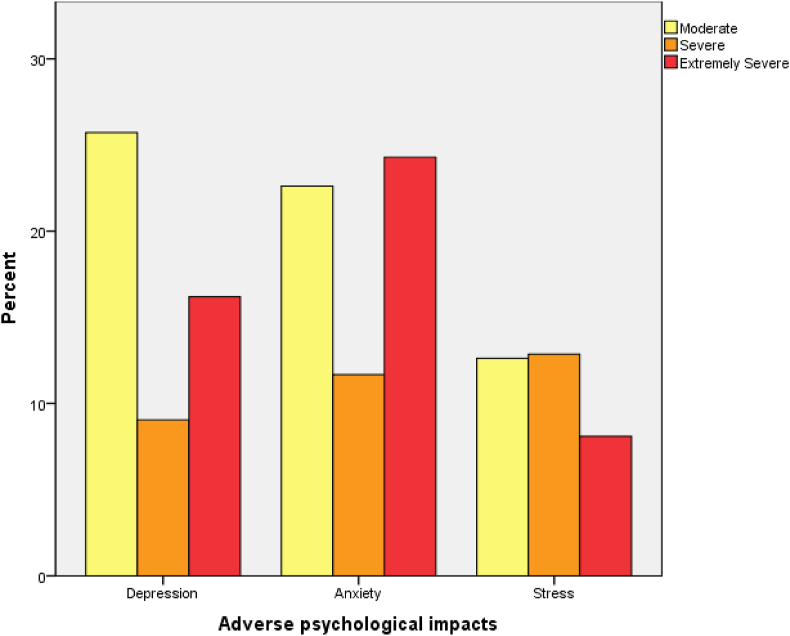
The overall prevalence of depression was 51.0%, however, 25.7%, 9.0%, and 16.2% RP were suffering from moderate, severe, and extremely severe types of depression, respectively. Regarding anxiety, the prevalence was 58.6%. The prevalence of moderate, severe, and extremely severe types of anxiety were 22.6%, 11.7%, and 24.3%, respectively. The prevalence of stress was 33.6% and the mild, moderate, severe and extremely severe types of stress were 12.6%, 12.9%, and 8.1%, respectively (Figure 1 presents details).
Figure 1.
Percent of participants experiencing adverse psychological impact, stratified by severity using DASS-21 (depression, anxiety and stress) (N = 420).
3.2. Socio-demographic variables on depression, anxiety, and stress
In this study, the percentage of male participants was higher than female (62.1% vs 37.9%). Most participants were from the 26–35 years age group (64%). The percentage of married-unmarried participants was almost equal. Only 36.9% of participants said that they performed regular 30 minutes exercises. A few RP were smokers (11.4%). However, we did not find a statistically significant association between any socio-demographic variables and depression, anxiety, and stress in this study (details in Table 1).
Table 1.
Univariate analysis: socio-demographic, profession and job-related variables and depression, anxiety, and stress levels.
| Variables | n (%) | Depression |
Anxiety |
Stress |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes; n (%) | X2 test value | p- value | Yes; n (%) | X2 test value | p-value | Yes; n (%) | X2 test value | p-value | ||
| Total | 420 (100%) | 214 (51.0) | 246 (58.6) | 198 (33.6) | ||||||
| Socio-demographic variables | ||||||||||
| Gender | 0.361 | 0.548 | 0.032 | 0.859 | 0.312 | 0.577 | ||||
| Female | 159 (37.9) | 84 (52.8) | 94 (59.1) | 56 (35.2) | ||||||
| Male | 261 (62.1) | 130 (49.8) | 152 (58.2) | 85 (32.6) | ||||||
| Age group | 2.160 | 0.340 | 0.666 | 0.717 | 1.996 | 0.369 | ||||
| ≥25 | 92 (21.9) | 53 (57.6) | 57 (62.0) | 30 (32.6) | ||||||
| 26–35 | 267 (63.6) | 132 (49.4) | 155 (58.1) | 95 (35.6) | ||||||
| ≥36 | 61 (14.5) | 29 (47.5) | 34 (55.7) | 16 (26.2) | ||||||
| Marital status | 1.317 | 0.251 | 0.309 | 0.578 | 0.027 | 0.868 | ||||
| Unmarried | 196 (46.7) | 94 (48.0) | 112 (57.1) | 65 (33.2) | ||||||
| Married | 224 (53.3) | 120 (53.6) | 134 (59.8) | 76 (33.9) | ||||||
| 30 minutes Exercise | 0.649 | 0.723 | 3.645 | 0.162 | 3.334 | 0.189 | ||||
| Yes | 155 (36.9) | 75 (48.4) | 82 (52.9) | 51 (32.9) | ||||||
| No | 229 (54.5) | 120 (52.4) | 140 (61.1) | 73 (31.9) | ||||||
| Stopped | 36 (8.6) | 19 (52.8) | 24 (66.7) | 17 (47.2) | ||||||
| Smoking | 1.318 | 0.517 | 0.081 | 0.960 | 0.100 | 0.951 | ||||
| Yes | 48 (11.4) | 28 (58.3) | 28 (58.3) | 17 (35.4) | ||||||
| No | 340 (81.0) | 171 (50.3) | 200 (58.8) | 113 (33.2) | ||||||
| Quitted | 32 (7.6) | 15 (46.9) | 18 (56.3) | 11 (34.4) | ||||||
| Profession-related variables | ||||||||||
| Education level | 12.375 | <0.001 | 3.270 | 0.071 | 9.325 | 0.002 | ||||
| Bachelor | 258 (61.4) | 149 (57.8) | 160 (62.0) | 101 (39.1) | ||||||
| Masters and above | 162 (38.6) | 65 (40.1) | 86 (53.1) | 40 (24.7) | ||||||
| Work experience | 4.483 | 0.214 | 2.949 | 0.400 | 5.694 | 0.113 | ||||
| <1 | 98 (23.3) | 53 (54.1) | 64 (65.3) | 36 (36.7) | ||||||
| 1–5 | 196 (46.7) | 106 (54.1) | 114 (58.2) | 73 (37.2) | ||||||
| 6–10 | 67 (16.0) | 27 (40.3) | 36 (53.7) | 19 (28.4) | ||||||
| >10 | 59 (14.0) | 28 (47.5) | 32 (54.2) | 13 (22.0) | ||||||
| Employment-related variables | ||||||||||
| Employer | 11.935 | 0.018 | 7.311 | 0.050 | 6.885 | 0.142 | ||||
| Medical college | 30 (7.1) | 11 (36.7) | 15 (50.0) | 8 (26.7) | ||||||
| Rehab institute | 91 (21.7) | 39 (42.9) | 45 (49.5) | 27 (29.7) | ||||||
| Hospital/clinic | 100 (23.8) | 49 (49.0) | 64 (64.0) | 30 (30.0) | ||||||
| Private chamber | 94 (22.4) | 48 (51.1) | 54 (57.4) | 30 (31.9) | ||||||
| Unemployed | 105 (25.0) | 67 (63.8) | 68 (64.8) | 46 (43.8) | ||||||
| Service type | 7.101 | 0.069 | 3.980 | 0.264 | 2.450 | 0.484 | ||||
| Government | 35 (8.3) | 15 (42.9) | 22 (62.9) | 11 (31.4) | ||||||
| Non-government | 196 (46.7) | 90 (45.9) | 105 (53.6) | 60 (30.6) | ||||||
| Self-employed | 85 (20.2) | 46 (54.1) | 55 (64.7) | 29 (34.1) | ||||||
| Others | 104 (24.8) | 63 (60.6) | 64 (61.5) | 41 (39.4) | ||||||
| Lost income source/employment | 20.485 | <0.001 | 5.868 | 0.015 | 12.690 | <0.001 | ||||
| Yes | 196 (46.7) | 123 (62.8) | 127 (64.8) | 83 (42.3) | ||||||
| No | 224 (53.3) | 91 (40.6) | 119 (53.1) | 58 (25.9) | ||||||
| Facing Economic constraints | 35.818 | <0.001 | 25.119 | <0.001 | 13.250 | <0.001 | ||||
| Yes | 322 (76.7) | 190 (59.0) | 210 (65.2) | 123 (38.2) | ||||||
| No | 98 (23.3) | 24 (24.5) | 36 (36.7) | 18 (18.4) | ||||||
| Adapt additional business | 4.666 | 0.031 | 1.255 | 0.263 | 0.047 | 0.908 | ||||
| Yes | 116 (27.6) | 69 (59.5) | 73 (62.9) | 38 (32.8) | ||||||
| No | 304 (72.4) | 145 (47.7) | 173 (56.9) | 103 (33.9) | ||||||
Bold faces are significant at 5% significance level.
3.3. Occupational factors on depression, anxiety, and stress
About two-thirds of the participants (61.4%) were bachelor degree holders and compare to the postgraduates, a significantly higher number of bachelor degree holders reported depression (X2 = 12.375, p < 0.001) and stress (X2 = 9.325, p = 0.002). On the other hand, about half of the participants (46.7%) have 1–5 years of professional work experience, however, those who have work experience of less than 1 year most frequently complained of depression and stress. Nonetheless, there was no statistically significant association between work experience and depression, anxiety, and stress (details in Table 1).
3.4. Employment opportunity on depression, anxiety, and stress
Among the sub-groups of the ‘employer’ group, the most participants were practicing at small hospital/clinic (23.8%) followed by at private chamber (22.4%), rehabilitation institute (21.7%), and medical college (7%). The remaining 25% of rehabilitation professionals were not in practice during the study period. The participants who were not in practice complained of depression (63.8%) and anxiety (64.8%) at higher rates. Statistically highly significant association were found between employer groups and depression (X2 = 11.935, p = 0.018), and anxiety (X2 = 7.311, p = 0.050). In this study, 46.7% of RP said that they have lost either their income source or employment due to the COVID-19 pandemic impact. In this case, those who lost their income source and/or employment reported significantly higher rate of depression (X2 = 20.485, p < 0.001) anxiety (X2 = 5.868, p = 0.015) and stress (X2 = 12.690, p < 0.001). Additionally, 76.7% RP said that they are facing economic constraints at this pandemic time and the sufferers complained in significantly higher rate of depression (X2 = 35.818, p= <0.001), anxiety (X2 = 25.11, p= <0.001) and stress (X2 = 13.250, p= <0.001). On the other hand, 27.6% of participants adopted additional business to compensate for the economic loss and a significantly higher number of them complained of depression (X2 = 4.666, p = 0.031) (details in Table 1).
3.5. Descriptive statistics: scores of depression, anxiety, and stress
Depressed participants had significantly higher score of financial threat (20.13 ± 4.37 vs. 15.82 ± 5.50, p= <0.001) and economic hardship (19.31 ± 4.25 vs. 16.18 ± 4.87, p < 0.001), however, a significantly lower score of economic wellbeing (09.41 ± 3.60 vs. 12.20 ± 4.37, p < 0.001). For anxious participants, there was a significantly higher score in financial threat (19.53 ± 4.69 vs. 15.85 ± 5.60, p < 0.001) and economic hardship (18.68 ± 4.47 vs. 16.51 ± 5.02, p < 0.001); significantly lower score in economic wellbeing (9.79 ± 3.74 vs. 12.16 ± 4.50, p < 0.001). Likewise, stressed participants had significantly higher score of financial threat (20.69 ± 4.31 vs. 16.65 ± 5.39, p < 0.001) and economic hardship (19.45 ± 4.49 vs. 16.93 ± 4.76, p < 0.001), however, significantly lower scores in economic wellbeing (8.88 ± 3.49 vs. 11.74 ± 4.25, p < 0.001) (details in Table 2).
Table 2.
Mean differences of the continuous variables with total sample according to depression, anxiety, and stress levels.
| Variables | Total (mean ± SD) | Depression (mean ± SD) |
Anxiety (mean ± SD) |
Stress (mean ± SD) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | p-value | No | Yes | p-value | No | Yes | p-value | ||
| Night sleeping time (h) | 7.00 ± 1.20 | 6.98 ± 1.10 | 7.01 ± 1.29 | 0.776 | 6.91 ± 1.13 | 7.06 ± 1.25 | 0.230 | 7.02 ± 1.13 | 6.95 ± 1.33 | 0.568 |
| Social media use (h) | 3.39 ± 2.37 | 3.18 ± 2.22 | 3.59 ± 2.49 | 0.080 | 3.26 ± 2.30 | 3.30 ± 2.37 | 0.506 | 3.37 ± 2.46 | 3.43 ± 2.20 | 0.830 |
| Financial threat | 18.01 ± 5.39 | 15.82 ± 5.50 | 20.13 ± 4.37 | <0.001 | 15.85 ± 5.60 | 19.53 ± 4.69 | <0.001 | 16.65 ± 5.39 | 20.69 ± 4.31 | <0.001 |
| Economic wellbeing | 10.78 ± 4.23 | 12.20 ± 4.37 | 09.41 ± 3.60 | <0.001 | 12.16 ± 4.50 | 9.79 ± 3.74 | <0.001 | 11.74 ± 4.25 | 8.88 ± 3.49 | <0.001 |
| Economic hardship | 17.78 ± 4.82 | 16.18 ± 4.87 | 19.31 ± 4.25 | <0.001 | 16.51 ± 5.02 | 18.68 ± 4.47 | <0.001 | 16.93 ± 4.76 | 19.45 ± 4.49 | <0.001 |
Bold faces are significant at 5% significance level.
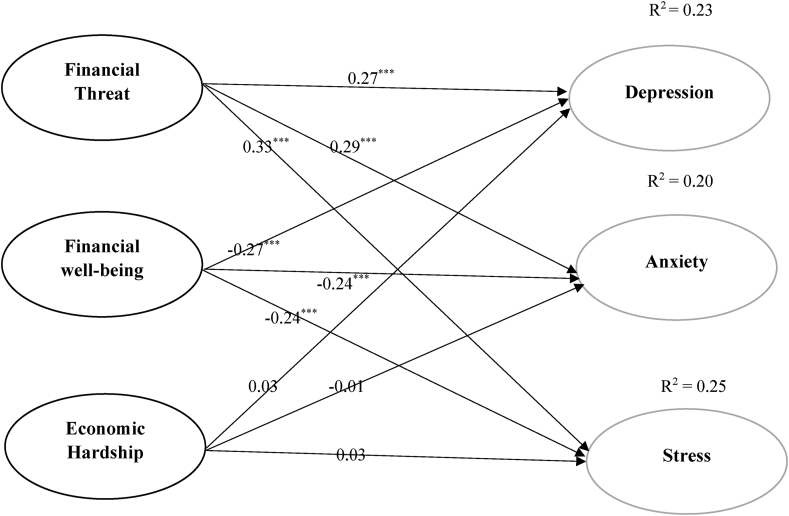
3.6. Relationships using the structural equation model
To examine the relationships of financial threat, economic wellbeing, and economic hardship with depression, anxiety, and stress after adjusting for daily sleep, and social media use durations; structural equation modelling was performed. Goodness of fit values indicated mostly good fit to the data in total sample ((χ2 = 1.539, df = 4, p = 0.820, χ2/df = 0.385, RMSEA = 0.00 [CI 90% (0.00, 0.05)], SRMR = 0.09, CFI = 1.00, GFI = 0.99).
The financial threat was positively associated with depression (β = 0.27, p < 0.001), anxiety (β = 0.29, p < 0.001), and stress (β = 0.33, p < 0.001). However, economic wellbeing was negatively associated with depression (β = -0.27, p < 0.001), anxiety (β = -0.24, p < 0.001) and stress (β = -0.24, p < 0.001). In this model, we did not find any association between economic hardship and depression, anxiety, and stress (details in Table 6 and Figure 2).
Table 6.
Standardized estimates of effects on depression, anxiety, and stress.
| Variables | Adjusted Effect | Standard Error |
|---|---|---|
| Financial Threat →Depression | 0.272∗∗∗ | 0.10 |
| Financial Threat →Anxiety | 0.294∗∗∗ | 0.09 |
| Financial Threat →Stress | 0.326∗∗∗ | 0.09 |
| Financial Well-being →Depression | -0.273∗∗∗ | 0.13 |
| Financial Well-being →Anxiety | -0.238∗∗∗ | 0.12 |
| Financial Well-being →Stress | -0.238∗∗∗ | 0.12 |
| Economic Hardship → Depression | 0.033 | 0.12 |
| Economic Hardship → Anxiety | -0.007 | 0.11 |
| Economic Hardship → Stress | 0.032 | 0.11 |
∗p < 05, ∗∗p < 01, ∗∗∗p < 001.
Figure 2.
Final model of the relationships among financial scales and DASS-21 subscales.
3.7. Multivariable analysis
Multivariable logistic regression suggested that factors related to education, employer, loss of income source/employment, and economic constraints were significantly associated with depression, anxiety, and stress. On the other hand, the structural equation model indicated that after adjusting for daily night sleeping time and social media using time, the financial threat is strongly positive, whereas, financial wellbeing is strongly negatively associated with depression, anxiety, and stress. Tables 3, 4, 5, and 6 show full results.
Table 3.
Logistic regression analysis of the variables with depression.
| Variables | Unadjusted Model |
Adjusted Model |
||||
|---|---|---|---|---|---|---|
| Odds Ratio (OR) | 95% confidence Interval (CI) | p-value | Adjusted Odds Ratio (AOR) | 95% confidence Interval (CI) | p-value | |
| Education | ||||||
| Masters or above | 0.541 | 0.345–.847 | 0.007 | 0.434 | 0.256–0.736 | 0.002 |
| Bachelor | Reference | Reference | ||||
| Employer | ||||||
| Medical college | 0.497 | 0.199–1.243 | 0.135 | 0.438 | 0.144–1.329 | 0.145 |
| Rehab institute | 0.798 | 0.416–1.531 | 0.497 | 0.623 | 0.240–1.619 | 0.332 |
| Hospital/Clinic | 0.709 | 0.381–1.319 | 0.277 | 0.632 | 0.258–1.550 | 0.317 |
| Private chamber | 0.622 | 0.335–1.155 | 0.133 | 0.513 | 0.236–1.112 | 0.091 |
| Unemployed | Reference | Reference | ||||
| Lost income source/employment | ||||||
| Yes | 1.546 | 0.976–2.448 | 0.063 | 1.588 | 0.988–2.552 | 0.050 |
| No | Reference | Reference | ||||
| Economic constrain | ||||||
| Yes | 3.428 | 1.920–6.119 | <0.001 | 3.415 | 1.869–6.240 | <0.001 |
| No | Reference | Reference | ||||
| Additional business | ||||||
| Yes | 1.235 | 0.768–1.985 | 0.384 | 1.221 | 0.774–2.005 | 0.390 |
| Reference | Reference | |||||
Table 4.
Logistic regression analysis of the variables with anxiety.
| Variables | Unadjusted Model |
Adjusted Model |
||||
|---|---|---|---|---|---|---|
| Odds Ratio (OR) | 95% confidence Interval (CI) | p-value | Adjusted Odds Ratio (AOR) | 95% confidence Interval (CI) | p-value | |
| Employer | ||||||
| Medical college | 0.543 | 0.270–1.500 | 0.213 | 0.500 | 0.202–1.722 | 0.134 |
| Rehab institute | 0.691 | 0.377–1.267 | 0.232 | 0.617 | 0.244–1.557 | 0.617 |
| Hospital/Clinic | 0.992 | 0.551–1.786 | 0.980 | 0.948 | 0.392–2.293 | 0.905 |
| Private chamber | 0.694 | 0.386–1.248 | 0.223 | 0.683 | 0.320–1.455 | 0.323 |
| Unemployed | Reference | Reference | ||||
| Lost income source/employment | ||||||
| Yes | 1.044 | 0.658–1.655 | 0.856 | 1.009 | 0.627–1.624 | 0.970 |
| No | Reference | Reference | ||||
| Economic constrain | ||||||
| Yes | 3.015 | 1.776–5.119 | <0.001 | 3.111 | 1.774–5.455 | <0.001 |
| No | Reference | Reference | ||||
Table 5.
Logistic regression analysis of the variables with stress.
| Variables | Unadjusted Model |
Adjusted Model |
||||
|---|---|---|---|---|---|---|
| Odds Ratio (OR) | 95% confidence Interval (CI) | p-value | Adjusted Odds Ratio (AOR) | 95% confidence Interval (CI) | p-value | |
| Education | ||||||
| Masters or above | 0.525 | 0.337–0.819 | 0.005 | 0.532 | 0.311–0.910 | 0.021 |
| Bachelor | Reference | Reference | ||||
| Lost income source/employment | ||||||
| Yes | 1.613 | 1.022–2.545 | 0.040 | 1.635 | 1.010–2.646 | 0.045 |
| No | Reference | Reference | ||||
| Economic constrain | ||||||
| Yes | 2.101 | 1.37–3.881 | 0.018 | 2.074 | 1.092–3.434 | 0.026 |
| No | Reference | Reference | ||||
4. Discussion
In this study, we found a high prevalence of depression, anxiety, and stress among RP in Bangladesh. A significant association between professional and employment-related factors was found with mental health symptoms. This study also revealed that a high number of RP in Bangladesh remain unemployed, additionally, to make the situation worst, about fifty per cent of total RP lost either their professional income source or employment during the COVID-19 pandemic. Factors related to employment and economic stress were the main predictors of the given mental health symptoms for RP in Bangladesh.
This is the first study evaluating mental health symptoms among rehabilitation professionals in Bangladesh. The solitary previous study measured the mental health of graduate health professionals in Bangladesh found that the prevalence rate of Depression, Anxiety, and Stress among medical doctors were 11.5% 11.0%, and 10.5%, respectively [40]. Unlike this low prevalence rate, we found the prevalence rate of Depression, Anxiety, and Stress 51.0 %, 58.6% and, 33.6%, respectively among Bangladeshi PR. The significantly higher prevalence rate of mental health symptoms among RP compared to the medical doctors clearly indicates the existence of underlying causes. A comparative study among RP and other medical graduates in Bangladesh using the same variables comprising profession, employment, and economic stress-related factors may help to understand the existing heterogeneity. Nonetheless, the prevalence rate of depression, anxiety, and stress among Bangladeshi unemployed graduates were 49.3%, 53.6%, and 28.3%, respectively [38], which was very similar to our findings. On the other hand, when we explored the prevalence rate of the graduate healthcare workers in Asia, available data suggested that the prevalence rate of depression, anxiety, and stress among Vietnamese nurses and Malaysian emergency medical officers were 13.2%/10.7%, 39.8%/28.6%, and 18.5%/7.9%, respectively [41, 42], which is much lower than the rates we found. Besides, a rapid systematic review of 59 studies conducted on the frontline and non-front line healthcare workers amid COVID-19 suggested that the median prevalence rate of depression, anxiety, and distress was 21%, 24%, and 37%, respectively. Another systematic review and meta-analysis of 55 studies (N = 189,159) unveiled that the mean prevalence of depression and anxiety among the population affected by COVID-19 was 15.9% and 15.15%, respectively. Evidence from these findings also suggested that the prevalence of mental health symptoms among Bangladeshi RP was remarkably higher. On the contrary, a study that measured mental health problems among undergraduate physiotherapy students in Pakistan found a similar prevalence rate (48.0% depression, 68.5% anxiety, and 53.2% stress) to Bangladeshi RP indicating poor mental health of RP in Asian countries. Further studies measuring mental health problems among rehabilitation professionals and students in other Asian countries and/or low- and middle-income countries are warranted.
When compared the prevalence rate we found with the UUE population over the world, available data suggested that the prevalence rate among Americans unemployed was- 29% depression, 31% anxiety, 28% stress [43]. In the Greek unemployed followed by the economic crisis in Greece, the rate was- 32.2% depression, 39.7% anxiety, 33% stress [44]. Prevalence rate of 51% depression, 35.5% anxiety in Spanish unemployed [45] and 39.5% depression in Korean graduate unemployed [46] along with 10.4% stress in Danish unemployed [47] and 69.4% stress among British graduate unemployed [48] were found. However, most of the prevalence rates were lower than the range we found among RP in Bangladesh.
On the other hand, analysis of professional factors and mental health symptoms revealed that RP with a higher professional degree in Bangladesh were in significantly better mental health states than the fresh graduate. It is well established that post-graduation helps in finding better employment and/or career path. Unsurprisingly, in Bangladesh, post-graduated candidates get privileges when recruited for the very limited number of secured full-time employments for RP [49]. Socio-economic conditions, scarcity of appropriate employment or income sources after completing graduation, and unavailability of post-graduate courses in cost-effective institutions may also put extra pressure on the mental health of fresh graduate RP in Bangladesh. In line with our findings, a study among Bangladeshi graduates has also suggested that the prevalence of depression, anxiety, and stress among appropriate employment seekers was very high [31].
Traditionally, in Bangladesh, the private and public medical college offers updated clinical and academic settings with well-paid stable employments for healthcare workers. In our study, we found only 7.1% of participants work in medical college settings, and predictably, the mental health of medical college employees was significantly better than unemployed and RP who work in small hospitals and clinics (which offer low-paid temporary jobs). Likewise, rehabilitation institute employees were in a better mental health state. It might be possible that in a specialized rehabilitation institute, RP gets a favourable working environment and desired wedges. However, in support of our findings, a systematic review and meta-analysis of 485 studies suggested that stable and well-paid employees suffer from fewer mental health problems [50].
A recent report from the International Labor Organization suggested that 55 million domestic workers were significantly affected by the COVID-19 pandemic till June 2020 [51]. Likewise, we found 62.8% RP either lost their employment or income source, and 59% currently facing economic constraints due to the impact of COVID-19. Unsurprisingly, a high number of them were suffering from mental health symptoms. In addition to this, we found, financial threats were strongly positive, and economic wellbeing was strongly negatively predicted mental health symptoms. Like previous studies, these economic factors help further explain the higher prevalence rates of mental health symptoms found in the present study as well as the fragile economic condition of Bangladeshi RP [30, 31].
This study suggested that a high number of RP remained out of practice and financially interrupted by the COVID-19 pandemic in Bangladesh. Furthermore, when we compared the mean scores of FTS and EHQ of the present study with a previous similar study conducted among graduate unemployed Bangladeshis [31], we found significantly higher FTS (18.01 vs. 15.90), and EHQ (17.78 vs. 16.58) mean scores indicating greater economic problems among rehabilitation professionals. As a result, this research indicates that these professionals require a holistic approach to reduce mental health symptoms. The burden of mental health could be minimized if equal opportunities for practice were provided in this occupational category. Stimulus programs may be provided to recovery practitioners to enable them to start their own practice, enabling them to become financially self-sufficient.
Limitations of cross-sectional study and methods bias of self-reported data collection must be admitted for this study. Furthermore, in this study, we did not take data regarding participant's health condition, substance abuse, the economic condition of participants' families that might confound mental health disorders. Despite these limitations, this study sets baseline evidence of employment situation, subjective economic condition, and their relation with mental health status among RP in Bangladesh.
Previous studies suggested that the prevalence of suicidality was higher among the UUE population and the high rates of mental sufferings are associated with up to 90% of the suicidality [21, 22, 52, 53]. Thus, further study is warranted concerning the suicidal behaviours among the RP in Bangladesh. The study that would measure mental health status and suicidality among RP students in Bangladesh are also required for early measurement and prevention. In addition, a further study among multiple professional groups is warranted to find a more generalized representation. Finally, when considering global implication, our study findings suggest that further similar studies among RP in other low- and middle-income countries are warranted.
5. Conclusion
COVID-19 pandemic offers unprecedented economic turmoil globally that resulted in a significant rise of unemployment and underemployment rate, consequently, economic threat. Along with the identification of other risk factors, our study explained the relation between economic stressors and mental health symptoms among a neglected professional group in Bangladesh. The findings could assist in recognizing people who are at risk of mental illness and encouraging the creation of an intervention program to minimize mental illness's burden.
Declarations
Author contribution statement
Mohammad Ali: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Zakir Uddin, Ahmed Hossain: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Jesus T.S., Landry M.D., Dussault G., Fronteira I. Human resources for health (and rehabilitation): six Rehab-Workforce Challenges for the century. Hum. Resour. Health. 2017 Dec 23;15(1):8. doi: 10.1186/s12960-017-0182-7. https://human-resources-health.biomedcentral.com/articles/10.1186/s12960-017-0182-7 [Internet] [cited 2020 Nov 7] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shakespeare T., Officer A. Editorial. Disabil. Rehabil. 2011 Jan 23;33(17–18):1491–1492. doi: 10.3109/09638288.2011.590392. http://www.tandfonline.com/doi/full/10.3109/09638288.2011.590392 [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 3.Cieza A., Causey K., Kamenov K., Hanson S.W., Chatterji S., Vos T. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020 Dec doi: 10.1016/S0140-6736(20)32340-0. [Internet] [cited 2020 Dec 13] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta N., Castillo-Laborde C., Landry M.D. Health-related rehabilitation services: assessing the global supply of and need for human resources. BMC Health Serv. Res. 2011 Dec 17;11(1):276. doi: 10.1186/1472-6963-11-276. https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-11-276 [Internet] [cited 2020 Nov 12] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jesus T.S., Koh G., Landry M., Ong P.-H., Lopes A.M.F., Green P.L. Finding the “right-size” physical Therapy workforce: international perspective across 4 countries. Phys. Ther. 2016 Oct 1;96(10):1597–1609. doi: 10.2522/ptj.20160014. https://academic.oup.com/ptj/article/96/10/1597/2870249 [Internet] [cited 2020 Nov 12] Available from: [DOI] [PubMed] [Google Scholar]
- 6.Taylor R., Zwisler A.-D., Uddin J. Global health-care systems must prioritise rehabilitation. Lancet. 2020 Dec doi: 10.1016/S0140-6736(20)32533-2. [Internet] [cited 2020 Dec 13] [DOI] [PubMed] [Google Scholar]
- 7.Chartered Society of Physiotherapy World confederation for physical Therapy. https://www.wcpt.org/node/25749 [Internet]. [cited 2020 Jun 7]. Available from:
- 8.WORLD federation of occupational therapists. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 1952;6(6):274–278. https://www.wfot.org/member-organisations/bangladesh-bangladesh-occupational-therapy-association [Internet] [cited 2020 Nov 18]; Available from: [PubMed] [Google Scholar]
- 9.Bangladesh public service commission-government of the People∖’s republic of Bangladesh. http://www.bpsc.gov.bd/ [Internet]. [cited 2021 Mar 2]. Available from:
- 10.Ministry of social welfare Bangladesh. Ministry of social welfare-government of the people’s republic of Bangladesh. 2015. https://msw.gov.bd/ [Internet]. [cited 2021 Mar 2]. Available from:
- 11.Mamin F.A., Hayes R. Physiotherapy in Bangladesh: inequality begets inequality. Front. Publ. Heal. 2018 Mar 23:6. doi: 10.3389/fpubh.2018.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dooley D., Prause J., Ham-Rowbottom K.A. Underemployment and depression: longitudinal relationships. J. Health Soc. Behav. 2000 Dec;41(4):421. http://www.jstor.org/stable/2676295?origin=crossref [Internet] [cited 2020 Nov 19] Available from: [PubMed] [Google Scholar]
- 13.Pharr J.R., Moonie S., Bungum T.J. The impact of unemployment on mental and physical health, access to health care and health risk behaviors. ISRN Publ. Health. 2012;2012:1–7. https://www.hindawi.com/archive/2012/483432/ [Internet] [cited 2020 Nov 19] Available from: [Google Scholar]
- 14.Bartelink V.H.M., Zay Ya K., Guldbrandsson K., Bremberg S. Unemployment among young people and mental health: a systematic review. Scand. J. Publ. Health. 2020 Jul 10;48(5):544–558. doi: 10.1177/1403494819852847. [Internet] [cited 2020 Nov 20] [DOI] [PubMed] [Google Scholar]
- 15.Meltzer H., Bebbington P., Brugha T., Jenkins R., McManus S., Stansfeld S. Job insecurity, socio-economic circumstances and depression. Psychol. Med. 2010 Aug 11;40(8):1401–1407. doi: 10.1017/S0033291709991802. https://www.cambridge.org/core/journals/psychological-medicine/article/job-insecurity-socioeconomic-circumstances-and-depression/12DFA33E6270D4F6154C0D49780E5E2E [Internet] [cited 2020 Nov 20] Available from: [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO) Mental health policy and service development team Publications produced or distributed by Nations for Mental Health. Ment. Heal. Policy Serv. Dev. 2000:6–9. http://www.who.int/mental_health [Internet] [cited 2020 Dec 19] Available from: [Google Scholar]
- 17.Olatunji B.O., Cisler J.M., Tolin D.F. Quality of life in the anxiety disorders: a meta-analytic review. Clin. Psychol. Rev. 2007 Jun 1;27(5):572–581. doi: 10.1016/j.cpr.2007.01.015. https://linkinghub.elsevier.com/retrieve/pii/S0272735807000360 [Internet] [cited 2020 Dec 19] Available from: [DOI] [PubMed] [Google Scholar]
- 18.Too L.S., Spittal M.J., Bugeja L., Reifels L., Butterworth P., Pirkis J. The association between mental disorders and suicide: a systematic review and meta-analysis of record linkage studies. J. Affect. Disord. 2019 Dec 1;259:302–313. doi: 10.1016/j.jad.2019.08.054. [Internet] [cited 2020 Nov 21] Available from: https://linkinghub.elsevier.com/retrieve/pii/S0165032719306202. [DOI] [PubMed] [Google Scholar]
- 19.Large M., Smith G., Sharma S., Nielssen O., Singh S.P. Systematic review and meta-analysis of the clinical factors associated with the suicide of psychiatric in-patients. Acta Psychiatr. Scand. 2011 Jul 1;124(1):18–19. doi: 10.1111/j.1600-0447.2010.01672.x. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1600-0447.2010.01672.x [Internet] [cited 2020 Nov 21] Available from: [DOI] [PubMed] [Google Scholar]
- 20.Harris E.C., Barraclough B. Suicide as an outcome for mental disorders. Br. J. Psychiatry. 1997 Mar 3;170(3):205–228. doi: 10.1192/bjp.170.3.205. https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/suicide-as-an-outcome-for-mental-disorders/1AAE5E8FEDA89A87A68EF082A783FEEE [Internet] [cited 2020 Nov 21] Available from: [DOI] [PubMed] [Google Scholar]
- 21.Bachmann S. Epidemiology of suicide and the psychiatric perspective. www.mdpi.com/journal/ijerph [cited 2020 Dec 19]; Available from: [DOI] [PMC free article] [PubMed]
- 22.Milner A., Page A., LaMontagne A.D. Long-term unemployment and suicide: a systematic review and meta-analysis. Baradaran H.R., editor. PloS One. 2013 Jan 16;8(1) doi: 10.1371/journal.pone.0051333. https://dx.plos.org/10.1371/journal.pone.0051333 [Internet] [cited 2020 Nov 21] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ali M., Uddin Z., Ahsan N.F., Haque M.Z., Bairagee M., Khan S.A. Prevalence and predictors of anxiety, depression, and insomnia among healthcare workers in dhaka city amid COVID-19 pandemic. Res Sq. 2020 Nov 10 [Internet] [cited 2020 Nov 21] [Google Scholar]
- 24.Ali M., GU Ahsan, Khan R., Khan H.R., Hossain A. Immediate impact of stay-at-home orders to control COVID-19 transmission on mental well-being in Bangladeshi adults: patterns, Explanations, and future directions. BMC Res. Notes. 2020 Dec 22;13(1):494. doi: 10.1186/s13104-020-05345-2. https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-020-05345-2 [Internet] [cited 2020 Oct 22]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S.Ø. Vol. 293. Elsevier Ireland Ltd; 2020. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review; p. 113441. (Psychiatry Research). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. 2020. Prevalence of Depression, Anxiety, and Insomnia Among Healthcare Workers during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. [cited 2020 Oct 18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vandenbroucke J.P., Von Elm E., Altman D.G., Gøtzsche P.C., Mulrow C.D., Pocock S.J. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4 doi: 10.1371/journal.pmed.0040297. http://www.epidem.com/ [Internet] [cited 2020 Mar 17] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.COPE . Publication on Ethics; 2020. Promoting Integrity in Scholarly Research and its Publication, Committee on Publication Ethics.https://publicationethics.org/ [Internet] [cited 2021 Feb 25]. Available from: [Google Scholar]
- 29.Lempers J.D., Clark-Lempers D., Simons R.L. Economic hardship, parenting, and distress in adolescence. Child Dev. 1989 Feb;60(1):25. doi: 10.1111/j.1467-8624.1989.tb02692.x. https://www.jstor.org/stable/1131068?origin=crossref [Internet] [cited 2020 Nov 25] Available from: [DOI] [PubMed] [Google Scholar]
- 30.Viseu J., Leal R., de Jesus S.N., Pinto P., Pechorro P., Greenglass E. Relationship between economic stress factors and stress, anxiety, and depression: moderating role of social support. Psychiatr. Res. 2018;268(July):102–107. doi: 10.1016/j.psychres.2018.07.008. [Internet] [DOI] [PubMed] [Google Scholar]
- 31.Mamun M.A., Akter S., Hossain I., Faisal M.T.H., Rahman M.A., Arefin A. Financial threat, hardship and distress predict depression, anxiety and stress among the unemployed youths: a Bangladeshi multi-city study. J. Affect. Disord. 2020 Nov 1;276:1149–1158. doi: 10.1016/j.jad.2020.06.075. https://linkinghub.elsevier.com/retrieve/pii/S0165032720324721 [Internet] [cited 2020 Dec 21] Available from: [DOI] [PubMed] [Google Scholar]
- 32.Marjanovic Z., Greenglass E.R., Fiksenbaum L., De Witte H., Garcia-Santos F., Buchwald P. Evaluation of the financial threat scale (FTS) in four European, non-student samples. J. Behav. Exp. Econ. 2015 Apr 1;55:72–80. [Google Scholar]
- 33.Marjanovic Z., Greenglass E.R., Fiksenbaum L., Bell C.M. Psychometric evaluation of the Financial Threat Scale (FTS) in the context of the great recession. J. Econ. Psychol. 2013 Jun 1;36:1–10. https://linkinghub.elsevier.com/retrieve/pii/S0167487013000299 [Internet] [cited 2020 Nov 25] Available from: [Google Scholar]
- 34.Jesus S.N., Leal A.R., Viseu J.N., Valle P., Matavelli R.D., Pereira J. Coping as a moderator of the influence of economic stressors on psychological health. Análise Psicol. 2016 Dec 12;34(4):365–376. http://publicacoes.ispa.pt/index.php/ap/article/view/1122 [Internet] [cited 2020 Nov 25] Available from: [Google Scholar]
- 35.Norvilitis J.M., Szablicki P.B., Wilson S.D. Factors influencing levels of credit-card debt in college Students1. J. Appl. Soc. Psychol. 2003 May 1;33(5):935–947. [Internet] [cited 2020 Nov 25] [Google Scholar]
- 36.Leal R., Viseu J., Jesus S.N., Paixão O., Greenglass E. 2014 July. Economic Stressors and Symptoms of Psychological Distress: Data from a Portuguese Sample; pp. 17–24. [Google Scholar]
- 37.Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 1995 Mar 1;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 38.Rafi M.A., Mamun M.A., Hsan K., Hossain M., Gozal D. Psychological implications of unemployment among Bangladesh civil service job seekers: a pilot study. Front. Psychiatr. 2019 Aug 12;10:578. doi: 10.3389/fpsyt.2019.00578. [Internet] [cited 2020 Nov 7]. Available from: https://www.frontiersin.org/article/10.3389/fpsyt.2019.00578/full. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu L.T., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 1999;6(1):1–55. https://www.tandfonline.com/doi/abs/10.1080/10705519909540118 [Internet] [cited 2020 Dec 11]. Available from: [Google Scholar]
- 40.Shibli Sadiq M., Mahjabin Morshed N., Rahman W., Chowdhury N.F., Yasir Arafat S.M., Mullick S.I. Depression, anxiety, stress among postgraduate medical residents: a cross sectional observation in Bangladesh. Iran. J. Psychiatry. 2019 Aug 6;141(3):192–197. [Internet] [cited 2020 Dec 12]. Available from: https://publish.kne-publishing.com/index.php/IJPS/article/view/1320. [PMC free article] [PubMed] [Google Scholar]
- 41.Tran T.T.T., Nguyen N.B., Luong M.A., Bui T.H.A., Phan T.D., Tran V.O. Stress, anxiety and depression in clinical nurses in Vietnam: a cross-sectional survey and cluster analysis. Int. J. Ment. Health Syst. 2019 Jan 3;(1):3–13. doi: 10.1186/s13033-018-0257-4. [Internet] [cited 2020 Dec 14] Available from: https://ijmhs.biomedcentral.com/articles/10.1186/s13033-018-0257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yahaya S.N. Prevalence and associated factors of stress, anxiety and depression among emergency medical officers in Malaysian hospitals. World J. Emerg. Med. 2018;9(3):178. doi: 10.5847/wjem.j.1920-8642.2018.03.003. www.wjem.com.cn [Internet] [cited 2020 Dec 14]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Howe G.W., Hornberger A.P., Weihs K., Moreno F., Neiderhiser J.M. Higher-order structure in the trajectories of depression and anxiety following sudden involuntary unemployment. J. Abnorm. Psychol. 2012;121(2):325–328. doi: 10.1037/a0026243. https://pmc/articles/PMC3621986/?report=abstract [Internet] [cited 2020 Dec 16]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kokaliari E. Quality of life, anxiety, depression, and stress among adults in Greece following the global financial crisis. Int. Soc. Work. 2018 May 28;61(3):410–424. [Internet] [cited 2020 Dec 16] [Google Scholar]
- 45.Navarro-Abal Y., Climent-Rodríguez J., López-López M., Gómez-Salgado J. Psychological coping with job loss. Empirical study to contribute to the development of unemployed people. Int. J. Environ. Res. Publ. Health. 2018 Aug 20;15(8):1787. doi: 10.3390/ijerph15081787. [Internet] [cited 2020 Dec 16] Available from: http://www.mdpi.com/1660-4601/15/8/1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lim A.Y., Lee S.-H., Jeon Y., Yoo R., Jung H.-Y. Job-seeking stress, mental health problems, and the role of perceived social support in university graduates in Korea. J. Kor. Med. Sci. 2018 May 7;33(19) doi: 10.3346/jkms.2018.33.e149. [Internet] [cited 2020 Dec 16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mæhlisen M.H., Pasgaard A.A., Mortensen R.N., Vardinghus-Nielsen H., Torp-Pedersen C., Bøggild H. Perceived stress as a risk factor of unemployment: a register-based cohort study. BMC Publ. Health. 2018 Jun 13;18(1):728. doi: 10.1186/s12889-018-5618-z. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5618-z [Internet] [cited 2020 Dec 16] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cassidy T., Wright L. Graduate employment status and health: a longitudinal analysis of the transition from student. Soc. Psychol. Educ. 2008 May 11;11(2):181–191. https://link.springer.com/article/10.1007/s11218-007-9043-x [Internet] [cited 2020 Dec 16] Available from: [Google Scholar]
- 49.The Daily Star. ePaper - the Daily Star _ Bangladesh Top News, Business, Sports, Entertainment, Politics, Technology, World, Lifestyle and Crime News. the daily star; 2020. https://epaper.thedailystar.net/ [Internet] [cited 2020 Dec 16];6. Available from: [Google Scholar]
- 50.Faragher E.B. The relationship between job satisfaction and health: a meta-analysis. Occup. Environ. Med. 2005 Feb 1;62(2):105–112. doi: 10.1136/oem.2002.006734. http://oem.bmj.com/cgi/doi/10.1136/oem.2002.006734 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Impact of the COVID-19 crisis on loss of jobs and hours among domestic workers. https://coronavirus.jhu.edu/ [Internet]. [cited 2020 Dec 18]. Available from:
- 52.Brådvik L. Suicide risk and mental disorders. Int. J. Environ. Res. Publ. Health. 2018;15 doi: 10.3390/ijerph15092028. www.mdpi.com/journal/ijerph [Internet] [cited 2021 Feb 26]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Milner A., Witt K., LaMontagne A.D., Niedhammer I. Vol. 75. Occupational and Environmental Medicine. BMJ Publishing Group; 2018. Psychosocial Job Stressors and Suicidality: A Meta-Analysis and Systematic Review.http://oem.bmj.com/ [Internet] [cited 2021 Feb 26]. p. 245–53. Available from: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.