Abstract
Heat waves and Covid-19 overlap, as this pandemic continues into summer 2021. Using a narrative review, we identified overlapping risk groups and propose coping strategies. The high-risk groups for heat-related health problems as well as for high-risk COVID-19 groups overlap considerably (elderly with pre-existing health conditions). Health care facilities will again be challenged by Covid-19 during heat waves. Health care personnel are also at risk of developing heat related health problems during hot periods due to the use of personal protective equipment to shield themselves from SARS-CoV-2 and must therefore be protected from excessive heat periods. Some existing recommendations for heat health protection contradict recommendations for COVID-19 protection. This paper provides a preliminary overview of possible strategies and interventions to tackle these ambiguities. The existing recommendations for protection against heat-related illnesses need revisions to determine whether they include essential aspects of infection control and occupational safety and how they may be supplemented.
Keywords: Covid-19, Heat wave, Personal protection equipment, PPE, SARS-CoV-2, Summer, Heat related health problem, Health care personnel
Funding
Funded by the Federal Ministry for the Environment, Nature Conservation and Nuclear Safety (BMU) on the basis of a resolution of the German Bundestag (project number: 67DAS213).
1. Background
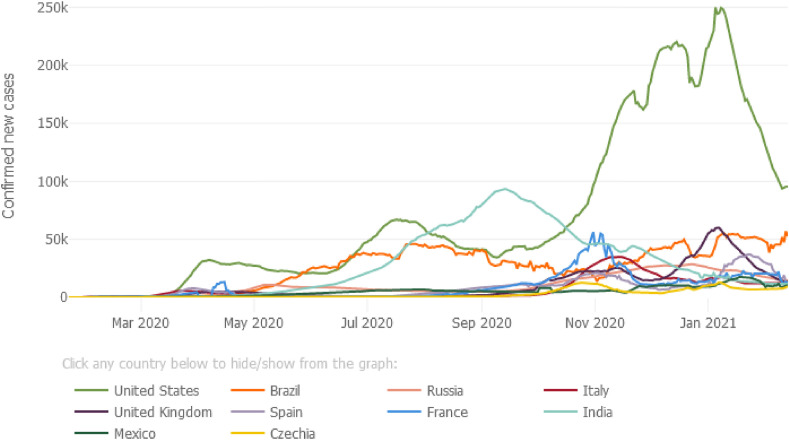
Since February 2020, COVID-19 cases have been reported globally. There is still an increase in daily new cases (see Fig. 1 ).
Fig. 1.
Daily confirmed new cases (7-day moving average). Outbreak evolution for the current 10 most affected countries, February 14, 2021(https://coronavirus.jhu.edu/data/new-cases).
COVID-19 not only poses extreme challenges to the healthcare system, the entire societies also experienced the implementation of substantial non-pharmaceutical interventions to contain and mitigate the spread and infection rates.
The pandemic will probably last for many more months, if not years (Barbarossa and Fuhrmann, 2020). Societies as a whole undergo long time broad non-pharmaceutical interventions (NPI), such as case isolation, tracking, home quarantine, social/physical distancing, closure of schools and care home facilities, to name but a few (Aleta et al., 2020; Kissler et al., 2020; Liu et al., 2020). General precautions such as hand washing, good respiratory hygiene, no shaking of hands etc. should be adhered to minimize transmissions (Kim et al., 2020). Second and third waves are occurring often in countries where NPI are less strict. In an outbreak lasting over a longer period, only strict implementation of NPIs can ensure that the healthcare systems will not become overwhelmed (Hellewell et al., 2020).
A further challenge for the healthcare system is to deal with more frequent and severe health effects caused by climate change. Compared to pre-industrial times, the global average temperature has risen by about 1.0 °C. In connection with this, hot days, heat waves and tropically warm nights are already occurring and will certainly continue to occur more frequently and for longer periods (IPCC 2014 et al., 2014). Hot periods and the thresholds when they become a risk can vary largely locally. Setting the specific threshold is part of a “heat health action plan”. In general, heat waves with tropically warm nights impose greater strain on the human organism, and they are particularly stressful for the old and chronically ill (Calleja-Agius et al., 2020; IPCC 2018. et al., 2019; van Schönthaler and von Andrian-Werburg, 2019).
Heat waves are the main cause of premature climate-change-related deaths, especially in the above-mentioned risk groups (Watts et al., 2018). Seventy-thousand deaths in Europe were claimed due to the heat wave in 2003 (Robine et al., 2008). Globally there is an upward trend of heat-related premature deaths (Watts et al., 2019). To combat this, the WHO, with experts from various fields, has drawn up recommendations for heat health action plans (Matthies et al., 2008) detailing the risks posed by heat and strategies to reduce heat related loss of work productivity, morbidity and mortality. Many Western countries already have adopted and implemented heat health action plans (Bittner et al., 2014; Casanueva et al., 2019). With the Covid-19 pandemic, it is necessary to adapt these plans to address the conflicting advice for protection against Covid-19 and for heat management (Daanen et al., 2020; Foster et al., 2020; Lee et al., 2020; Martinez et al., 2020; Morabito et al., 2020). Information addressing this issue was compiled and the first recommendations have been published on national and international levels (Global Heat Health Information Network (GHHIN), 2020).
There is a high risk of contracting SARS-CoV-2, especially for the elderly and the chronically-ill and people in need of care (Kim et al., 2020; Leclerc et al., 2020; Nachtigall et al., 2020; Pijls et al., 2021; Williamson et al., 2020; Wingert et al., 2020). These vulnerable groups are likewise at high risk of developing or dying prematurely from heat-related health problems (D'Ippoliti et al., 2010; Matthies et al., 2008; Semenza et al., 1996). It is to be feared that with a continuing COVID-19 pandemic and possible heat waves in the 2021 and beyond, these vulnerable groups will be at multiple risks. Hence, health systems need to prepare for heat events — in addition to managing COVID-19. Heat health action plans and recommendations may need modification in cases where they are restricted, unavailable or in contradiction due to COVID-19 measures and guidelines (Daanen et al., 2020; Martinez et al., 2020; Morabito et al., 2020). Additionally, prolonged heat can put an additional burden on health systems and emergency services that are already under pressure due to the COVID-19 pandemic.
1.1. Objectives
The concurrence of a biological (SARS-CoV-2) and a climate (heat) threat did occur in summer 2020 and will likely occur in summer 2021. Most national heat health action plans - developed over previous years - need amendments to accommodate for regulations and advice for protection against the new SARS-CoV-2. The speed at which this global pandemic has occurred adds considerable stress on policy makers as heat health action plans must be updated and amended immediately. It will be a new challenge for hospital managers, staff, medical and non-medical personnel in outpatient and inpatient care. Supplementing the heat health action plans with important points of infection control and occupational safety and health will minimize heat strain, as well as the transmission rates. This article aimed to identify the special challenges for:
-
•
Overlapping vulnerable populations.
-
•
Reducing heat strain for medical and non-medical personnel, especially when working with personal protective equipment (PPE).
-
•
Dealing with conflicting measures for heat protection and simultaneous infection control
2. Methods
For this paper, we chose a narrative review, since new findings on Covid-19 are reported on a daily basis and many of the publications included were only available as preprints and not as peer-reviewed articles. The following sources were used for the literature research:
-
•
Heat stress: Institutional reports from WHO (World Health Organization), GHHIN (Global Heat Health Information Network), CDC (Center for Disease Control), RKI (Robert Koch-Institute), and UBA (German Environmental Agency), and systematic reviews (PubMed listed) Search terms: “ Heat Stress Disorders/prevention and control"[MAJR], "COVID-19"[MeSH] AND "Health Personnel"[MAJR] AND "Hot Temperature"[MAJR]
-
•
COVID-19: Websites of (inter)national institutes and authorities, and the websites of John Hopkins University, CDC (Center for Disease Control), ECDC (European Centre for Disease Prevention and Control), EUROMOMO, medRxiv (Preprint Server), and PubMedSearch terms: “ Covid-19+AND + climate + change“
The results of the literature research were analysed by title and abstract screening. The “Munich” team developed the objectives for this paper, set up a Mendeley data bank, read the selected papers and condensed the information into the different tables and figures.1 The scientific advisory board, including relevant German agencies and stakeholders for this project peer-reviewed the first draft, including a videoconference.2
The Global Heat Health Information Network (GHHIN) is spearheaded by the WHO, the World Meteorological Organization Joint Office for Climate and Health (WMO), and the United States National Oceanic and Atmospheric Administration (NOAA). GHHIN organized an expert workshop on “hot but habitable” in Leiden/The Netherlands (March 9–13 in 2020) and was the driving force for the development of an information series on heat and COVID-19 (Global Heat Health Information Network (GHHIN), 2020).
The second, revised draft was sent out to an international team of experts,3 which was formed during this workshop on “hot but habitable” in Leiden at the Lorentz Center (https://www.lorentzcenter.nl/hot-but-habitable.html). Several of the workshop participants, including GHHIN members, published a paper: “COVID-19 and thermoregulation-related problems - practical recommendations” (Daanen et al., 2020). The GHHIN information series is the result of scientific collaboration of over 70 contributors and reviewers (see acknowledgement). Several authors are part of the GHHIN team and contributed to this paper as well as the information supplied on the GHHIN web pages (Global Heat Health Information Network (GHHIN), 2020). The international expert group commented and added to the draft, including additional references and materials.
3. Results
3.1. Overlapping vulnerable populations
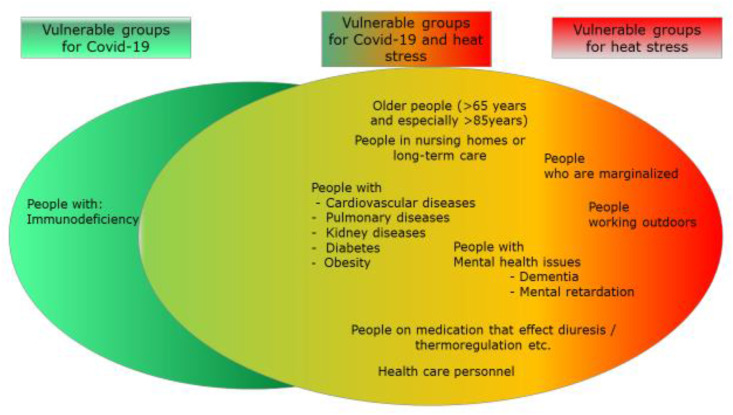
Population groups vulnerable to the effects of heat stress and those at higher risk for severe Covid-19 and mortality overlap largely. Variations in risk related to heat depend on the level of exposure to hot weather and heat waves and the ability to adapt.
Risk factors for heat-related mortality (Calleja-Agius et al., 2020; D'Ippoliti et al., 2010; Gosling et al., 2009; Kenny et al., 2010; Matthies et al., 2008; McGregor et al., 2015; Oudin Åström et al., 2015; Semenza et al., 1996; World Health Organization (WHO), 2011) include:
-
•
Age: Old (75–84 years) or very old (85+ years)
-
•
Pre-existing health conditions: Chronic respiratory-, heart- and kidney diseases, diabetes
-
•
People working outside, people taking certain medication etc.
Risk factors for COVID-19 related mortality (Kim et al., 2020; Nachtigall et al., 2020; Pijls et al., 2021; Williamson et al., 2020; Wingert et al., 2020) include:
-
•
Age/setting: older people (65+), especially very old people (85+), people in care institutions
-
•
Pre-existing health conditions: (poorly controlled) chronic lung-, kidney- or cardiovascular diseases, immune deficiency, obesity
The next Fig. 2 shows the intersection of vulnerable groups. Other factors such as cognitive impairment, dementia, need for assistance or social isolation and homelessness make it more difficult to care for the vulnerable groups (Matthies et al., 2008; Zielo and Matzarakis, 2018).
Fig. 2.
Vulnerable groups for heat stress and for COVID-19 and their intersection.
Although the vulnerable groups for heat-related mortality and COVID-19 mortality show overlap regarding age and pre-existing health conditions, sex does not seem to have a strong effect on heat related mortality. Elderly females might be more sensitive to heat mortality then males (van Steen et al., 2019), but there are studies showing that men might be more vulnerable (Alele et al., 2020). COVID-19 mortality is clearly higher in males (Kim et al., 2020; Li et al., 2020; Nachtigall et al., 2020; Pijls et al., 2021; Williamson et al., 2020; Wingert et al., 2020).
Reducing heat strain for medical and non-medical personnel, especially when working with PPE.
The above-mentioned risk groups are cared for or treated by outpatient nursing services, relatives caring for them or in inpatient nursing facilities and clinics, by health care and nursing staff, doctors as well as medical and non-medical assistant staff. COVID-19 clusters can be located in households, hospitals and inpatient care facilities and therefore put the vulnerable people at higher risk due to their exposure at these locations (Emmerton and Abdelhafiz, 2021; Leclerc et al., 2020). Medical and non-medical personnel are, thus, exposed to an increased risk of infection, depending on the measures taken for protection against infection (European Centre for Disease Prevention and Control (ECDC), 2020). Due to the spread of Covid-19, staff at risk of infection must wear personal protective equipment (PPE) and therefore increases the heat load (Tabah et al., 2020). PPE makes it more difficult to lose body heat, since the additional layers of clothing significantly reduce the evaporation of sweat and thus the resulting cooling effect (Jacklitsch et al., 2016). Working in protective clothing therefore reduces a person's endurance, cognitive performance and increases the risk for accidents (Dorman and Havenith, 2009; Jacklitsch et al., 2016; Luze et al., 2020; McLellan et al., 2013; Zhang et al., 2019). During hot spells, heat stress can occur in non-air-conditioned healthcare facilities. Medical and non-medical personnel develop heat-related health problems due to the wearing of protective equipment, which may ultimately affect the quality of care (Jegodka et al., 2021; Lee et al., 2020). There are existing recommendations to protect staff from heat stress and ensure their occupational health and safety exist on national and international levels (Jacklitsch et al., 2016). For the current situation, there are a few suggestions to protect employees who use PPE at elevated temperatures (Daanen et al., 2020; Foster et al., 2020; Lee et al., 2020; Luze et al., 2020; Morabito et al., 2020; Workplace Safety and Health Council, 2020) GHHIN has developed some recommendations (Global Heat Health Information Network (GHHIN), 2020). Since the global temperatures are increasing these recommendations will remain relevant also for future summers (with or without out COVID-19).
3.2. Dealing with conflicting measures for heat protection and simultaneous infection control
Employees must be protected against the effects of heat stress by appropriate protective measures (Kuklane et al., 2015; Workplace Safety and Health Council, 2020). Traditionally, employment standards have been created for those wearing PPE in the industrial, construction or agricultural sector, but to date there are no studies to support standards for the care sector that requires the use of PPE under heat stress (Cheung et al., 2016). For the safety of employees, it is essential to quickly develop feasible and validated safeguarding concepts. Some possible measures to make working during hot spells with PPE more bearable are listed in Table 1 .
Table 1.
Possible interventions for medical and non-medical personnel.
| Recommendations and options specifically for occupational health and safety for medical and non-medical personnel: |
|---|
| ➢Technical measures |
| •Air conditioning system (RLT) or mobile air conditioning units. Air-conditioning systems need to be well maintained, while adequate settings and filters need to be adopted. Setting climate control systems to low “cold” temperatures (below 70 F/ 21C) and “dry” low humidity settings (below 40%) should be avoided. Devices without adequate filters could spread SARS-CoV-2 (www.ghhin.org/heat-and-covid-19/ac-and-ventilation) (Chirico et al., 2020; Correia et al., 2020; Jay et al., 2015; Lu et al., 2020; Morawska and Cao, 2020; Pease et al., 2021). |
| •Passive, structural protection against solar radiation and avoidance of other heat sources (Matthies et al., 2008; Widerynski et al., 2016) |
| •Systematic and continuous recording of temperature/humidity in affected work areas, definition of threshold values (Jacklitsch et al., 2016; World Health Organization (WHO), 2011) |
| •Ventilating over night to use cooler air if possible (Matthies et al., 2008) |
| •In many places, electric fans may be more accessible; but may help transmit the virus indoors, and in very hot and dry environments these can increase heat stress; fans should be avoided if more people are in one room (www.ghhin.org/heat-and-covid-19/ac-and-ventilation(Jay et al., 2015; Morris et al., 2020) |
| ➢Organizational measures |
| •Awareness raising and training of personnel on heat and virus related health risks and prevention measures (Jacklitsch et al., 2016; Schoierer et al., 2019; Zielo and Matzarakis, 2018) |
| •Observance of heat warnings and implementation of respective prevention measures •(Matthies et al., 2008; Morabito et al., 2020; Singh et al., 2019) |
| •Establishing shorter work cycles in overheated rooms, more frequent breaks, changed shift patterns, better staff shift schedules (Jacklitsch et al., 2016) |
| •Planning/shifting longer activities with the need for infection control to times of day/building areas with lower temperature/solar radiation |
| •Taking organisational measures within the team, e.g. for early symptoms of heat stress ->stop working in the heat ->seek cooler premises and direct help (colleagues) |
| •Encouraging mindfulness of oneself and colleagues; fostering open communication of problems in the institution (www.ghhin.org/assets/technical-brief-COVID-and-Heat-final.pdf) |
| •Wearing adequate clothing under the protective equipment, if necessary, consider special clothing (cooling vests) in particularly stressful conditions (Bach et al., 2019; Daanen et al., 2020; Gao et al., 2018; Luze et al., 2020; Morris et al., 2020; Quinn et al., 2017; Teunissen et al., 2014; Watson et al., 2019) |
| •Consideration of the possible overlap of hot spells (increased need for personnel) with the summer holidays (less available personnel due to increased holiday volume) in the duty roster or holiday planning (consider heat warnings) |
| ➢Personal measures |
| •Heat acclimatization and aerobic conditioning to enhance heat tolerance (Alhadad et al., 2019; Douzi et al., 2020; Lee et al., 2008; Leyk, 2019; Morris et al., 2020) |
| •Start to work precooled (www.ghhin.org/heat-and-covid-19/PPE) (Alhadad et al., 2019; Daanen et al., 2020; Douzi et al., 2020; McLellan et al., 2013; Morris et al., 2020) |
| •Encourage staff to self-monitor their hydration; drinking unsweetened liquids/sports drinks/cold fluids/ice slushies before and during work; self-control of the body's own fluid balance (toilet); start work cooled and well hydrated (Foster et al., 2020; Lee et al, 2008, 2013, 2020; McLellan et al., 2013; Tan and Lee, 2015) |
3.3. Heat protection and infection control: Identification of conflicting measures
To protect against infection with SARS-CoV-2, general hygiene measures (washing hands, coughing and sneezing etiquette, and no shaking hands), social distancing and the wearing of simple mouth and nose protection are recommended by WHO and the respective national authorities to the population since spring 2020. This also applies to the high-risk groups listed (Fig. 2). In healthcare systems, physical and social proximity can at best be minimized to adhere to the “physical distancing” requirement. For the high-risk groups, technical, organizational and personal measures must be prepared to protect against excessive heat strain (Table 2 ) (Jacklitsch et al., 2016; Schoierer et al., 2019; Semenza et al., 1996; Zielo and Matzarakis, 2018). Measures to protect against SARS-CoV-2 are also shown in Table 2. These measures are partly conflicting (Daanen et al., 2020). The transmission of SARS-CoV-2 mainly takes place indoors (Kriegel et al., 2020; Leclerc et al., 2020). In the interior, all regulations for protection against infection must be observed in accordance with the respective specifications and regulations (European Centre for Disease Prevention and Control (ECDC), 2020).
Table 2.
Compatibility of recommendations for the two vulnerable groups for protection against heat versus protection against Covid-19.
| Compatibility of measures for the protection against the two different hazards | ||
|---|---|---|
| Protection against heat-related illnesses or mortality | Protection against Covid-19 | |
| Regular care – professional caretaker | X | Physical distancing (1–2 m) |
| Regular support – relatives, neighbourhood help/volunteers | X | Self-isolation/social distancing |
| Cool, breathable clothing | X | Face mask in all public buildings, shops, plastic facial screens, etc. |
| Visiting cooling centers, cool spaces outdoors to avoid staying in overheated homes | ? | Staying at home as much as possible |
| Using night cooling; windows closed during heat | ? | Airing rooms regularly |
| Avoid physical activity during hot hours | ? | Regular physical exercise to strengthen the immune system |
| Using social networks | ✓ | Using social networks e.g. for shopping |
| Adjustment of medication by the doctor | ✓ | Adjustment of medication by the doctor |
| Cooling through nursing measures (wraps, arm/foot baths etc.) | ✓ | Coughing and sneezing etiquette, hand washing |
| Adequate hydration | ✓ | Balanced diet |
| Shopping in cooler mornings | ✓ | Shopping not at peak hours |
| Protecting the windows against sunlight and avoiding additional heat sources (e.g. electrical appliances) | ✓ | |
| When going outside, protecting the body against the sun with a hat | ||
| Relocation of sitting/sleeping places to rooms with lower temperature/less sun exposure | ✓ | |
| Avoid hot places, overheated public transport | ✓ | Avoid crowded places, public transport |
| ✓ | Get pneumococcal vaccination | |
| ✓ | Get Covid-19 vaccination | |
The use of “cooler rooms” in care facilities, such as the house chapel, or group rooms on the cooler ground floor are reasonable. Such "cooler rooms" can be set up in the facilities for mobile patients, while respecting infection prevention regulations and depending on the spatial conditions.
The recommendation to move to shaded, “cooler outdoor areas” such as terraces, gardens or parks in hot weather makes sense from a heat protection point of view (Matthies et al., 2008; World Health Organization (WHO), 2011; Zielo and Matzarakis, 2018). In the view of the authors, this recommendation can be maintained, if the rules of physical distancing and general hygiene recommendations to reduce the risk of infection with SARS-CoV-2 are observed, and if the specific local conditions permit this.
“Cooling Centers" during the COVID 19 pandemic in combination with heat waves are now recommended by the Center for disease Control (CDC) as a safe alternative (Centers for Disease Control and Prevention, 2020).
The heat health action plans recommend that high-risk patients who live at home should receive direct daily care, while the Covid-19 hazard warns against direct social contact. An international expert group has developed on how best to manage heat stress and infection protection in tandem (Global Heat Health Information Network (GHHIN), 2020). As communities develop emergency action plans for managing the pandemic, public officials must also consider heat preparedness plans. Some channels for COVID-19 communications and heat protection exist:
-
•
World Health Organization (https://www.who.int/emergencies/diseases/novel-coronavirus-2019) Center for Disease Control (CDC) (www.cdc.gov/coronavirus/2019-ncov/faq.html)
-
•
Global Heat Health Information System (GHHIN) (www.ghhin.org/heat-and-covid-19)
-
•
Harvard University (www.hsph.harvard.edu/c-change/subtopics/coronavirus-and-heatwaves/)
-
•
High Council of Public Health (Haut Conseil de la santé publique - HCSP) (www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=817) (French)
-
•
German Environmental Agency (Umweltbundesamt - UBA) www.umweltbundesamt.de/coronaviren-umwelt) (German)
4. Discussion
Older adults (>60 years) and those with pre-existing health conditions are considered vulnerable for severe COVID-19 and heat-related illnesses. This common vulnerable group is highly volatile and is of particular challenge to the healthcare systems. COVID-19 related mortality in retirement and nursing home is very high in many high-income countries. One potential risk factor is that nursing personnel can acquire COVID-19 outside their workplace, and infect others later, especially when they are asymptomatic and/or not adequately monitored. To protect against this route of infection, health professionals must work under strict infection control measures. Medical and non-medical personnel are at risk of developing heat related health problems during hot summer periods due to the PPE required during this pandemic (Tabah et al., 2020). At present, a question arises whether the requirement of social distancing is not a contra-indication to the previously recommended protection measure against heat (Matthies and Menne, 2009). The recommendations to protect high-risk groups from COVID-19 and from heat stress and at times cancel out each other in parts. The authors consider it necessary to establish appropriate recommendations, based on the available materials (GHHIN, WHO and others) and adapting them to the local context. Heat health action plans can be a valuable source to be adapted (Daanen et al., 2020; Martinez et al., 2020; Mücke and Litvinovitch, 2020). At the same time it is important to communicate these combined risks from heat and COVID-19 to the vulnerable populations to increase their knowledge and risk perception, thereby incurring respective changes to their daily behaviours (Eady et al., 2020; Golechha and Panigrahy, 2020).
The COVID-19 pandemic already places a heavy burden on the healthcare systems, not even considering in detail the role of mutations, but for further planning, other possible stress factors must be taken into account. After extreme events, such as e.g. the earthquake in Croatia in March 2020 or the glacier break in India in January 2021, it was observed that compliance with personal protection against SARS-CoV-2 infection was difficult, as the usual assistance and rescue measures were complicated by the need for PPE to protect against infection. Not only heat, but also other environmental influences such as extreme weather events (forest fires, heavy precipitation, floods, and storms), major damage events or accidents (e.g. in a nuclear power plant or chemical plant, earthquakes) can lead to an additional burden on the overall healthcare system, concurrent to the COVID-19 pandemic.
5. Conclusion
It is currently assumed that potential heat waves and prolonged periods of heat in the summer months will place an additional burden on many healthcare systems, coinciding with the COVID-19 pandemic. The existing recommendations for protection against heat-related illnesses and mortality should therefore be reviewed on regional and local levels to determine whether they include important aspects of infection protection and occupational safety and how they should be supplemented accordingly. Adjusted heat health action plans need to be monitored throughout the summer periods and be evaluated for their effectiveness and lessons learnt.
Credit author statement
Conceptualization: Franziska Matthies-Wiesler, Stephan Bose-O’Reilly, Hein Daanen, Peter van den Hazel, Nicola Gerrett, Maud Maria Theresia Elisabeth Huynen, Jason Lee, Joy Shumake-Guillemot, Joris Adriaan Frank van Loenhout, Data curation: Stephan Bose-O’Reilly, Katharina Deering, Stefan Karrasch, Hanna Mertes, Julia Schoierer, Dennis Nowak, Franziska Matthies-Wiesler, Jason Lee, Nicola Gerrett, Maud Maria Theresia Elisabeth Huynen, Formal analysis: Stephan Bose-O’Reilly, Katharina Deering, Hanna Mertes, Nicola Gerrett, Maud Maria Theresia Elisabeth Huynen, Jason Lee, Funding acquisition: Stephan Bose-O’Reilly, Katharina Deering, Hanna Mertes, Julia Schoierer, Investigation: Stephan Bose-O’Reilly, Katharina Deering, Hanna Mertes, Nicola Gerrett, Maud Maria Theresia Elisabeth Huynen, Jason Lee, Methodology: Franziska Matthies-Wiesler, Stephan Bose-O’Reilly, Hein Daanen, Peter van den Hazel, Nicola Gerrett, Maud Maria Theresia Elisabeth Huynen, Jason Lee, Joy Shumake-Guillemot, Joris Adriaan Frank van Loenhout, Project administration: Julia Schoierer, Supervision: Stephan Bose-O’Reilly, Julia Schoierer, Validation: Stephan Bose-O’Reilly, Visualization: Stephan Bose-O’Reilly, Katharina Deering, Stefan Karrasch, Hanna Mertes, Julia Schoierer, Writing - original draft: Stephan Bose-O’Reilly, Katharina Deering, Stefan Karrasch, Hanna Mertes, Julia Schoierer, Dennis Nowak, Writing - review & editing: Stephan Bose-O’Reilly, Hein Daanen, Peter van den Hazel, Franziska Matthies-Wiesler, Nicola Gerrett, Maud Maria Theresia Elisabeth Huynen, Jason Lee, Joy Shumake-Guillemot, Joris Adriaan Frank van Loenhout.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The GHHIN information series is the result of scientific collaboration of over 70 contributors and reviewers, and is the scientific backbone of this paper (Global Heat Health Information Network (GHHIN), 2020). We would like very much to acknowledge their role, especially of the two board members, that joined the workshop in Leiden: Joy Shumake-Guillemot, as co-author, and Hunter Jones, on behalf of all other contributors and reviewers. The team from the University Hospital in Munich (SB, KD, SK, HM, JS, DN) received a grant from the German Ministry of Environment: Avoidance of heat-related diseases in times of increased infection protection of vulnerable groups -funded by the Federal Ministry for the Environment, Nature Conservation and Nuclear Safety (BMU) on the basis of a resolution of the German Bundestag (project number: 67DAS213).
Footnotes
Stephan Bose-O’Reilly, Katharina Deering, Stefan Karrasch, Hanna Mertes, Julia Schoierer, Dennis Nowak.
Dr. Matthias an der Heiden (Robert Koch Institute), Dr. Christian Berringer (German Ministry of Health), Johanna Grünewald (Cologne City Council), Dr. Andreas Hellmann (Doctor's Association - Pneumologist), Dr. Ralph Krolewski (Family Doctor's Association North Rhine), Prof. Dr. Caroline Herr (Bavarian Agency for Food Safety and Health), Prof. Andreas Matzarakis (Germany's National Meteorological Service), Dr. Hans-Guido Mücke (German Environmental Protection Agency), Dr. Peter Tinnemann (Academy of Public Health Services).
Hein Daanen, Peter van den Hazel, Stephan Bose-O’Reilly, Nicola Gerrett, Maud Maria Theresia Elisabeth Huynen, Jason Lee, Joy Shumake-Guillemot, Joris Adriaan Frank van Loenhout.
References
- Alele F., Malau-Aduli B., Malau-Aduli A., Crowe M. Systematic review of gender differences in the epidemiology and risk factors of exertional heat illness and heat tolerance in the armed forces. BMJ Open. 2020;10:1–10. doi: 10.1136/bmjopen-2019-031825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleta A., Martín-Corral D., Pastore y Piontti A., Ajelli M., Litvinova M., Chinazzi M., Dean N.E., Halloran M.E., Longini I.M., Merler S., Pentland A., Vespignani A., Moro E., Moreno Y. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nat. Hum. Behav. 2020;4:964–971. doi: 10.1038/s41562-020-0931-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhadad S.B., Tan P.M.S., Lee J.K.W. Efficacy of heat mitigation strategies on core temperature and endurance exercise: a meta-analysis. Front. Physiol. 2019;10 doi: 10.3389/fphys.2019.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bach A.J.E., Maley M.J., Minett G.M., Zietek S.A., Stewart K.L., Stewart I.B. An evaluation of personal cooling systems for reducing thermal strain whilst working in chemical/biological protective clothing. Front. Physiol. 2019;10 doi: 10.3389/fphys.2019.00424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbarossa M.V., Fuhrmann J. 2020. Germany's Next Shutdown—Possible Scenarios and Outcomes. Influenza Other Respi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bittner M.I., Matthies E.F., Dalbokova D., Menne B. Are European countries prepared for the next big heat-wave? Eur. J. Publ. Health. 2014;24:615–619. doi: 10.1093/eurpub/ckt121. [DOI] [PubMed] [Google Scholar]
- Calleja-Agius J., England K., Calleja N. The effect of global warming on mortality. Early Hum. Dev. 2020 doi: 10.1016/j.earlhumdev.2020.105222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanueva A., Burgstall A., Kotlarski S., Messeri A., Morabito M., Flouris A.D., Nybo L., Spirig C., Schwierz C. Overview of existing heat-health warning systems in Europe. Int. J. Environ. Res. Publ. Health. 2019;16 doi: 10.3390/ijerph16152657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2020. Covid and Cooling Centers. [Google Scholar]
- Cheung S.S., Lee J.K.W., Oksa J. Thermal stress, human performance, and physical employment standards. Appl. Physiol. Nutr. Metabol. 2016;41:S148–S164. doi: 10.1139/apnm-2015-0518. [DOI] [PubMed] [Google Scholar]
- Chirico F., Sacco A., Bragazzi N.L., Magnavita N. Can air-conditioning systems contribute to the spread of SARS/MERS/COVID-19 infection? Insights from a rapid review of the literature. Int. J. Environ. Res. Publ. Health. 2020;17:1–11. doi: 10.3390/ijerph17176052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correia G., Rodrigues L., Gameiro da Silva M., Gonçalves T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med. Hypotheses. 2020;141:109781. doi: 10.1016/j.mehy.2020.109781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daanen H., Bose-O’Reilly S., Brearley M., Flouris D.A., Gerrett N.M., Huynen M., Jones H.M., Lee J.K.W., Morris N., Norton I., Nybo L., Oppermann E., Shumake-Guillemot J., Van den Hazel P. COVID-19 and thermoregulation-related problems: practical recommendations. Temperature. 2020;8:1–11. doi: 10.1080/23328940.2020.1790971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorman L.E., Havenith G. The effects of protective clothing on energy consumption during different activities. Eur. J. Appl. Physiol. 2009;105:463–470. doi: 10.1007/s00421-008-0924-2. [DOI] [PubMed] [Google Scholar]
- Douzi W., Dupuy O., Theurot D., Smolander J., Dugué B. Per-cooling (Using cooling systems during physical exercise) enhances physical and cognitive performances in hot environments. a narrative review. Int. J. Environ. Res. Publ. Health. 2020 doi: 10.3390/ijerph17031031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D', Ippoliti D., Michelozzi P., Marino C., De'Donato F., Menne B., Katsouyanni K., Kirchmayer U., Analitis A., Medina-Ramon M., Paldy A., Atkinson R., Kovats S., Bisanti L., Schneider A., Lefranc A., Iniguez C., Perucci C.A. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Env. Heal. 2010 doi: 10.1186/1476-069X-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eady A., Dreyer B., Hey B., Riemer M., Wilson A. Reducing the risks of extreme heat for seniors: communicating risks and building resilience. Heal. Promot. Chronic Dis. Prev. Canada. 2020;40:215–224. doi: 10.24095/hpcdp.40.7/8.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmerton D., Abdelhafiz A.H. Care for older people with dementia during COVID-19 pandemic. SN Compr Clin Med. 2021 doi: 10.1007/s42399-020-00715-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC) 2020. Coronavirus Disease 2019 (COVID-19) in the EU/EEA and the UK– Ninth Update.www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-coronavirus-disease-2019-covid-19-pandemic-ninth-update [Google Scholar]
- Foster J., Hodder S.G., Goodwin J., Havenith G. Occupational heat stress and practical cooling solutions for healthcare and industry workers during the COVID-19 pandemic. Ann. Work Expo. Heal. 2020;64:915–922. doi: 10.1093/annweh/wxaa082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao C., Kuklane K., Östergren P.O., Kjellstrom T. Occupational heat stress assessment and protective strategies in the context of climate change. Int. J. Biometeorol. 2018;62:359–371. doi: 10.1007/s00484-017-1352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Heat Health Information Network (GHHIN) Protecting health from hot weather during the COVID-19 pandemic [WWW document]. URL. 2020. https://ghhin.org/wp-content/uploads/technical-brief-COVID-and-Heat-finalv2-1.pdf
- Golechha M., Panigrahy R.K. COVID-19 and heatwaves: a double whammy for Indian cities. Lancet Planet. Heal. 2020;4:e315–e316. doi: 10.1016/S2542-5196(20)30170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosling S.N., Lowe J.A., McGregor G.R., Pelling M., Malamud B.D. Associations between elevated atmospheric temperature and human mortality: a critical review of the literature. Climatic Change. 2009 doi: 10.1007/s10584-008-9441-x. [DOI] [Google Scholar]
- Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W., Munday J.D., Kucharski A.J., Edmunds W.J., Sun F., Flasche S., Quilty B.J., Davies N., Liu Y., Clifford S., Klepac P., Jit M., Diamond C., Gibbs H., van Zandvoort K., Funk S., Eggo R.M. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Heal. 2020;8:e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IPCC, Pachauri K., Meyer L.A., editors. Climate Change 2014: Synthesis Report. Contribution, Climate Change 2014: Synthesis Report. 2014. [Google Scholar]
- IPCC . In: Global Warming of 1.5°C an IPCC Special Report on the Impacts of Global Warming of 1.5°C above Pre-industrial Levels and Related Global Greenhouse Gas Emission Pathways. Masson-Delmotte V., Zhai P., Pörtner H.-O., Roberts D., Skea J., Shukla P.R., Pirani A., Moufouma-Okia W., Péan C., Pidcock R., Connors S., Matthews J.B.R., Chen Y., Zhou X., Gomis M.I., Lonnoy E., Maycock T., Tignor M., Waterfield T., editors. 2018. (The Context of Strengthening the Global Response to the Threat of Clima). [Google Scholar]
- Jacklitsch B., Williams W., Musolin K., Coca A., J-H K., Turner N. Occupational exposure to heat and hot environments: revised criteria 2016. U.S. Dep. Heal. Hum. Serv. Centers Dis. Control Prev. Natl. Inst. Occup. Saf. Heal. DHHS Publ. 2016 www.cdc.gov/niosh/docs/2016-106/pdfs/2016-106.pdf?id=10.26616/NIOSHPUB2016106 [Google Scholar]
- Jay O., Cramer M.N., Ravanelli N.M., Hodder S.G. Should electric fans be used during a heat wave? Appl. Ergon. 2015;46:137–143. doi: 10.1016/j.apergo.2014.07.013. [DOI] [PubMed] [Google Scholar]
- Jegodka Y., Lagally L., Mertes H., Deering K., Buchberger B., Reilly S.B. 2021. Hot Days and Covid-19 – Unusual Heat Stress for Nursing Professions in Germany. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny G.P., Yardley J., Brown C., Sigal R.J., Jay O. Heat stress in older individuals and patients with common chronic diseases. CMAJ (Can. Med. Assoc. J.) 2010;182:1053–1060. doi: 10.1503/cmaj.081050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim L., Garg S., O'Halloran A., Whitaker M., Pham H., Anderson E.J., Armistead I., Bennett N.M., Billing L., Como-Sabetti K., Hill M., Kim S., Monroe M.L., Muse A., Reingold A.L., Schaffner W., Sutton M., Talbot H.K. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the US coronavirus disease 2019 (COVID-19)-Associated hospitalization surveillance Network (COVID-NET) Clin. Infect. Dis. 2020;30329:1–9. doi: 10.1093/cid/ciaa1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;80:eabb5793. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriegel M., Buchholz U., Gastmeier P., Bischoff P., Abdelgawad I., Hartmann A. 2020. Predicted Infection Risk for Aerosol Transmission of Sars-COV-2. medRxiv. [DOI] [Google Scholar]
- Kuklane K., Lundgren K., Gao C., Löndahl J., Hornyanszky E.D., Östergren P.O., Becker P., Samuels M.C., Gooch P., Sternudd C., Albin M., Taj T., Malmqvist E., Swietlicki E., Olsson L., Persson K., Olsson J.A., Kjellstrom T. Ebola: improving the design of protective clothing for emergency workers allows them to better cope with heat stress and help to contain the epidemic. Ann. Occup. Hyg. 2015;59:258–261. doi: 10.1093/annhyg/mev003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leclerc Q.J., Fuller N.M., Knight L.E., Funk S., Knight G.M. What settings have been linked to SARS-CoV-2 transmission clusters? [version 2; peer review: 2 approved] Wellcome Open Res. 2020;5 doi: 10.12688/wellcomeopenres.15889.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.K.W., Shirreffs S.M., Maughan R.J. Cold drink ingestion improves exercise endurance capacity in the heat. Med. Sci. Sports Exerc. 2008;40:1637–1644. doi: 10.1249/MSS.0b013e318178465d. [DOI] [PubMed] [Google Scholar]
- Lee J.K.W., Yeo Z.W., Nio A.Q.X., Koh A.C.H., Teo Y.S., Goh L.F., Tan P.M.S., Byrne C. Cold drink attenuates heat strain during work-rest cycles. Int. J. Sports Med. 2013;34:1037–1042. doi: 10.1055/s-0033-1337906. [DOI] [PubMed] [Google Scholar]
- Lee J., Venugopal V., Latha P.K., Alhadad S.B., Leow C.H.W., De Goh N.Y., Tan E., Kjellstrom T., Morabito M., Lee J.K.W. Heat stress and thermal perception amongst healthcare workers during the covid-19 pandemic in India and Singapore. Int. J. Environ. Res. Publ. Health. 2020;17:1–12. doi: 10.3390/ijerph17218100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyk D. Health risks and interventions in exertional heat stress. Dtsch. Aerzteblatt Online. 2019 doi: 10.3238/arztebl.2019.0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L.Q., Huang T., Wang Y.Q., Wang Z.P., Liang Y., Huang T.B., Zhang H.Y., Sun W., Wang Y. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020;92:577–583. doi: 10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Morgenstern C., Kelly J., Lowe R., Jit M. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. medRxiv. 2020:1–12. doi: 10.1101/2020.08.11.20172643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu J., Gu J., Li K., Xu C., Su W., Lai Z., Zhou D., Yu C., Xu B., Yang Z. COVID-19 outbreak associated with air conditioning in restaurant, guangzhou, China, 2020. Emerg. Infect. Dis. J. 2020;26 doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luze H., Nischwitz S.P., Kotzbeck P., Fink J., Holzer J.C.J., Popp D., Kamolz L.-P. Personal protective equipment in the COVID-19 pandemic and the use of cooling-wear as alleviator of thermal stress. Wien Klin. Wochenschr. 2020 doi: 10.1007/s00508-020-01775-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez G.S., Linares C., De'Donato F., Diaz J. Protect the vulnerable from extreme heat during the COVID-19 pandemic. Environ. Res. 2020 doi: 10.1016/j.envres.2020.109684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthies F., Menne B. Prevention and management of health hazards related to heatwaves. Int. J. Circumpolar Health. 2009;68:8–22. doi: 10.3402/ijch.v68i1.18293. [DOI] [PubMed] [Google Scholar]
- Matthies F., Bickler G., Cardenosa Marin N., Hales S., World Health Organization (WHO) 2008. Heat - Health Action Plans. [Google Scholar]
- McGregor G.R., Bessemoulin P., Ebi K., Menne B., editors. Heatwaves and Health: Guidance on Warning-System Development 114. 2015. [Google Scholar]
- McLellan T.M., Daanen H.A.M., Cheung S.S. Encapsulated environment. Comp. Physiol. 2013;3:1363–1391. doi: 10.1002/cphy.c130002. [DOI] [PubMed] [Google Scholar]
- Morabito M., Messeri A., Crisci A., Pratali L., Bonafede M., Marinaccio A. Heat warning and public and workers' health at the time of COVID-19 pandemic. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.140347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris N.B., Jay O., Flouris A.D., Casanueva A., Gao C., Foster J., Havenith G., Nybo L. Sustainable solutions to mitigate occupational heat strain - an umbrella review of physiological effects and global health perspectives. Environ. Heal. 2020;19:1–24. doi: 10.1186/s12940-020-00641-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mücke H.G., Litvinovitch J.M. Heat extremes, public health impacts, and adaptation policy in Germany. Int. J. Environ. Res. Publ. Health. 2020;17:1–14. doi: 10.3390/ijerph17217862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nachtigall I., Lenga P., Jóźwiak K., Thürmann P., Meier-Hellmann A., Kuhlen R., Brederlau J., Bauer T., Tebbenjohanns J., Schwegmann K., Hauptmann M., Dengler J. Clinical course and factors associated with outcomes among 1904 patients hospitalized with COVID-19 in Germany: an observational study. Clin. Microbiol. Infect. 2020;26:1663–1669. doi: 10.1016/j.cmi.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oudin Åström D., Schifano P., Asta F., Lallo A., Michelozzi P., Rocklöv J., Forsberg B. The effect of heat waves on mortality in susceptible groups: a cohort study of a mediterranean and a northern European City. Environ. Heal. A Glob. Access Sci. Source. 2015;14:1–8. doi: 10.1186/s12940-015-0012-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pease L.F., Wang N., Salsbury T.I., Underhill R.M., Flaherty J.E., Vlachokostas A., Kulkarni G., James D.P. Investigation of potential aerosol transmission and infectivity of SARS-CoV-2 through central ventilation systems. Build. Environ. 2021 doi: 10.1016/j.buildenv.2021.107633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pijls B.G., Jolani S., Atherley A., Derckx R.T., Dijkstra J.I.R., Franssen G.H.L., Hendriks S., Richters A., Venemans-Jellema A., Zalpuri S., Zeegers M.P. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: a meta-analysis of 59 studies. BMJ Open. 2021;11:1–10. doi: 10.1136/bmjopen-2020-044640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn T., Kim J.H., Strauch A., Wu T., Powell J., Roberge R., Shaffer R., Coca A. Physiological evaluation of cooling devices in conjunction with personal protective ensembles recommended for use in west africa. Disaster med. Public Health Prep. 2017;11:573–579. doi: 10.1017/dmp.2016.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robine J.M., Cheung S.L.K., Le Roy S., Van Oyen H., Griffiths C., Michel J.P., Herrmann F.R. Death toll exceeded 70,000 in Europe during the summer of 2003. Comptes Rendus Biol. 2008;331:171–178. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- Schoierer J., Mertes H., Wershofen B., Bose-O’Reilly S. Trainingmodules on climate change, heat, and health for medical assistants and nurses in outpatient care. Bundesgesundheitsblatt - Gesundheitsforsch. - Gesundheitsschutz. 2019;62:620–628. doi: 10.1007/s00103-019-02942-w. [DOI] [PubMed] [Google Scholar]
- Semenza J.C., Rubin C.H., Falter K.H., Selanikio J.D., Flanders W.D., Howe H.L., Wilhelm J.L. Heat-related deaths during the July 1995 heat wave in Chicago. N. Engl. J. Med. 1996;335:84–90. doi: 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- Singh R., Arrighi J., Jjemba E., Strachan K., Spires M., Kadihasanoglu A. 2019. Heatwave Guide for Cities. [Google Scholar]
- Tabah A., Ramanan M., Laupland K.B., Buetti N., Cortegiani A., Mellinghoff J., Conway Morris A., Comporota L., Zappella N., Elhadi M., Povoa P., Amrein K., Vidal G., Derde L., Bassetti M., Francois G., Ssi yan kai N., De Waele J.J. Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): an international survey. J. Crit. Care. 2020;59:70–75. doi: 10.1016/j.jcrc.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan P.M.S., Lee J.K.W. The role of fluid temperature and form on endurance performance in the heat. Scand. J. Med. Sci. Sports. 2015;25:39–51. doi: 10.1111/sms.12366. [DOI] [PubMed] [Google Scholar]
- Teunissen L.P.J., Wang L.C., Chou S.N., Huang C., Jou G.T., Daanen H.A.M. Evaluation of two cooling systems under a firefighter coverall. Appl. Ergon. 2014;45:1433–1438. doi: 10.1016/j.apergo.2014.04.008. [DOI] [PubMed] [Google Scholar]
- van Schönthaler P.K., von Andrian-Werburg S. Umweltbundesamt; 2019. [Monitoring Report 2019 on the German Strategy for Adaptation to Climate Change - Report of the Interministerial Working Group on Adaptation Strategy of the Federal Government. [Google Scholar]
- van Steen Y., Ntarladima A.M., Grobbee R., Karssenberg D., Vaartjes I. Sex differences in mortality after heat waves: are elderly women at higher risk? Int. Arch. Occup. Environ. Health. 2019;92:37–48. doi: 10.1007/s00420-018-1360-1. [DOI] [PubMed] [Google Scholar]
- Watson C., Troynikov O., Lingard H. Design considerations for low-level risk personal protective clothing: a review. Ind. Health. 2019;57:306–325. doi: 10.2486/indhealth.2018-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts N., Amann M., Ayeb-Karlsson S., Belesova K., Bouley T., Boykoff M., Byass P., Cai W., Campbell-Lendrum D., Chambers J., Cox P.M., Daly M., Dasandi N., Davies M., Depledge M., Depoux A., Dominguez-Salas P., Drummond P., Ekins P., Flahault A., Frumkin H., Georgeson L., Ghanei M., Grace D., Graham H., Grojsman R., Haines A., Hamilton I., Hartinger S., Johnson A., Kelman I., Kiesewetter G., Kniveton D., Liang L., Lott M., Lowe R., Mace G., Odhiambo Sewe M., Maslin M., Mikhaylov S., Milner J., Latifi A.M., Moradi-Lakeh M., Morrissey K., Murray K., Neville T., Nilsson M., Oreszczyn T., Owfi F., Pencheon D., Pye S., Rabbaniha M., Robinson E., Rocklöv J., Schütte S., Shumake-Guillemot J., Steinbach R., Tabatabaei M., Wheeler N., Wilkinson P., Gong P., Montgomery H., Costello A. The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet. 2018;391:581–630. doi: 10.1016/S0140-6736(17)32464-9. [DOI] [PubMed] [Google Scholar]
- Watts N., Amann M., Arnell N., Ayeb-Karlsson S., Belesova K., Boykoff M., Byass P., Cai W., Campbell-Lendrum D., Capstick S., Chambers J., Dalin C., Daly M., Dasandi N., Davies M., Drummond P., Dubrow R., Ebi K.L., Eckelman M., Ekins P., Escobar L.E., Fernandez Montoya L., Georgeson L., Graham H., Haggar P., Hamilton I., Hartinger S., Hess J., Kelman I., Kiesewetter G., Kjellstrom T., Kniveton D., Lemke B., Liu Y., Lott M., Lowe R., Sewe M.O., Martinez-Urtaza J., Maslin M., McAllister L., McGushin A., Jankin Mikhaylov S., Milner J., Moradi-Lakeh M., Morrissey K., Murray K., Munzert S., Nilsson M., Neville T., Oreszczyn T., Owfi F., Pearman O., Pencheon D., Phung D., Pye S., Quinn R., Rabbaniha M., Robinson E., Rocklöv J., Semenza J.C., Sherman J., Shumake-Guillemot J., Tabatabaei M., Taylor J., Trinanes J., Wilkinson P., Costello A., Gong P., Montgomery H. The 2019 report of the Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394:1836–1878. doi: 10.1016/S0140-6736(19)32596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widerynski S., Schramm P., Conlon K., Noe R., Grossman E., Hawkins M., Nayak S., Roach M., Hilts A.S. 2016. The Use of Cooling Centers to Prevent Heat-Related Illness: Summary of Evidence and Strategies for Implementation Climate and Health Technical Report Series. [Google Scholar]
- Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E., Curtis H.J., Mehrkar A., Evans D., Inglesby P., Cockburn J., McDonald H.I., MacKenna B., Tomlinson L., Douglas I.J., Rentsch C.T., Mathur R., Wong A.Y.S., Grieve R., Harrison D., Forbes H., Schultze A., Croker R., Parry J., Hester F., Harper S., Perera R., Evans S.J.W., Smeeth L., Goldacre B. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingert A., Pillay J., Gates M., Guitard S., Rahman S., Beck A., Vandermeer B., Hartling L. Risk factors for severe outcomes of COVID-19: a rapid review. medRxiv. 2020 doi: 10.1136/bmjopen-2020-044684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Workplace Safety and Health Council . 2020. Managing Heat Stress in the Workplace. [Google Scholar]
- World Health Organization (WHO) 2011. Public Health Advice on Preventing Health Effects of Heat. [Google Scholar]
- Zhang F., de Dear R., Hancock P. Effects of moderate thermal environments on cognitive performance: a multidisciplinary review. Appl. Energy. 2019;236:760–777. doi: 10.1016/j.apenergy.2018.12.005. [DOI] [Google Scholar]
- Zielo B., Matzarakis A. Relevance of heat health actions plans for preventive public health in Germany. Gesundheitswesen. 2018;80:e34–e43. doi: 10.1055/s-0043-107874. [DOI] [PubMed] [Google Scholar]