Abstract
Background
The COVID-19 pandemic has affected patients with ST-segment elevation myocardial infarction (STEMI) requiring primary percutaneous coronary intervention (PCI) worldwide. In this review we examine the global effect of the COVID-19 pandemic on incidence of STEMI admissions, and relationship between the pandemic and door to balloon time (D2B), all-cause mortality, and other secondary STEMI outcomes.
Methods
We performed a systematic review and meta-analysis to primarily compare D2B time and in-hospital mortality of STEMI patients who underwent primary PCI during and before the pandemic. Subgroup analyses were performed to investigate the influence of geographical region and income status of a country on STEMI care. An online database search included studies that compared the aforementioned outcomes of STEMI patients during and before the pandemic.
Results
In total, 32 articles were analyzed. Overall, 19,140 and 68,662 STEMI patients underwent primary PCI during and before the pandemic, respectively. Significant delay in D2B was observed during the pandemic (weighted mean difference, 8.10 minutes; 95% confidence interval [CI], 3.90-12.30 minutes; P = 0.0002; I2 = 90%). In-hospital mortality was higher during the pandemic (odds ratio [OR], 1.27; 95% CI, 1.09-1.49; P = 0.002; I2 = 36%), however this varied with factors such as geographical location and income status of a country. Subgroup analysis showed that low–middle-income countries observed a higher rate of mortality during the pandemic (OR, 1.52; 95% CI, 1.13-2.05; P = 0.006), with a similar but insignificant trend seen among the high income countries (OR, 1.17; 95% CI, 0.95-1.44; P = 0.13).
Conclusions
The COVID-19 pandemic is associated with worse STEMI performance metrics and clinical outcome, particularly in the Eastern low–middle-income status countries. Better strategies are needed to address these global trends in STEMI care during the pandemic.
RÉSUMÉ
Introduction
Dans le monde entier, la pandémie de COVID-19 a nui aux patients atteints d'infarctus du myocarde avec élévation du segment ST (STEMI) qui avaient besoin d'une intervention coronarienne percutanée (ICP) primaire. Dans cette revue, nous examinons les répercussions de la pandémie de COVID-19 à l’échelle mondiale sur le nombre d'admissions en raison de STEMI, et la relation entre la pandémie et le délai de prise en charge médicale aux urgences (D2B, de l'anglais door to balloon time), la mortalité toutes causes confondues et les autres critères secondaires liés au STEMI.
Méthodes
Nous avons réalisé une revue systématique et une méta-analyse principalement pour comparer le D2B et la mortalité intrahospitalière des patients atteints d'un STEMI qui avaient subi une ICP primaire durant et avant la pandémie. Nous avons réalisé des analyses en sous-groupes pour examiner l'influence de la région géographique et du revenu des pays sur les soins aux patients atteints d'un STEMI. La consultation en ligne de bases de données consistait à trouver des études qui portaient sur la comparaison des critères liés au STEMI ci-dessus mentionnés durant et avant la pandémie.
Résultats
Au total, nous avons analysé 32 articles. Dans l'ensemble, 19 140 et 68 662 patients atteints d'un STEMI avaient subi une ICP primaire durant et avant la pandémie, et ce, de façon respective. Nous avons observé un D2B important durant la pandémie (différence moyenne pondérée, 8,10 minutes; intervalle de confiance [IC] à 95 %, 3,90-12,30 minutes; P = 0,0002; I2 = 90 %). La mortalité intrahospitalière était plus élevée durant la pandémie (ratio d'incidence approché [RIA], 1,27; IC à 95 %, 1,09-1,49; P = 0,002; I2 = 36 %). Toutefois, elle variait en fonction de facteurs tels que la région géographique et le revenu des pays. L'analyse en sous-groupes a montré que les pays à revenu faible ou intermédiaire avaient un taux plus élevé de mortalité durant la pandémie (RIA, 1,52; IC à 95 %, 1,13-2,05; P = 0,006), ainsi qu'une tendance similaire, mais non significative dans les pays à revenu élevé (RIA, 1,17; IC à 95 %, 0,95-1,44; P = 0,13).
Conclusions
La pandémie de COVID-19 est associée à des indicateurs de performance et des issues cliniques liées aux STEMI qui sont pires, particulièrement dans les pays de l'Est à revenu faible ou intermédiaire. De meilleures stratégies sont nécessaires pour remédier à ces tendances mondiales dans les soins aux patients atteints d'un STEMI durant la pandémie.
The COVID-19 pandemic has overwhelmed all levels of medical services in many countries with a substantial strain on health care personnel and medical resources.1 An integrated network of emergency medical services, emergency departments (EDs), referring hospitals, and percutaneous coronary intervention (PCI)-capable hospitals is vital in ST-segment elevation myocardial infarction (STEMI) care to ensure timely reperfusion for patients with STEMI, especially during the pandemic.2 Although primary PCI is the standard reperfusion strategy during the pandemic as recommended by major guidelines,3 performing such high-risk procedures on patients with confirmed or unknown COVID-19 status will put health care workers and other patients at risk of transmission. However, strict infection control measures might potentially delay treatment.4 Hence, treatment strategies for STEMI patients have differed across countries5, 6, 7, 8, 9, 10 in an attempt to strike a balance between optimal STEMI care and safety of the community.2 The global effect of such strategies on STEMI outcome is still unknown.
Multiple observational studies have reported varying degrees of reduction in STEMI presentations and delay in PCI treatment across the globe.11, 12, 13, 14, 15 However, most of these studies were small, and on the basis of the experience of a single centre or involved registry data from the Western developed world. Thus, we sought to perform a systematic review and meta-analysis on such a heterogeneous group of studies to examine the incidence of STEMI admissions during the COVID-19 pandemic compared with before the pandemic, the relationship between the pandemic and door to balloon time (D2B), mortality, and other important secondary STEMI outcomes, as well as the effect of geographical and economic differences on these outcomes.
Methods
Data sources and searches
The Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines were used in the synthesis of this review.16 The protocol of this review was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42020219776). An electronic database search of Medline and Embase was performed on February 28, 2021 using keywords and terms synonymous with COVID-19, ST-elevation myocardial infarction, STEMI, percutaneous coronary intervention, and PCI. Additionally, references from included studies and pertinent review articles were searched to identify other potential studies that met the selection criteria. The search was limited to articles written in the English language. An example of the search strategy is shown in Supplemental Appendix S1.
Study selection
Article sieving was performed by 2 authors (V.X.Y.T. and R.R.Y.H.) working independently with any discrepancies being resolved by achieving consensus with a third and senior author (N.W.S.C.). Inter-rater agreement was quantified through the use of the Cohen kappa statistic coefficient, k, with standard agreement definition being used to quantify degrees of agreement.17 In this review we primarily focus on comparing the D2B and mortality rates of STEMI patients before and during the pandemic. The inclusion criteria were that of: (1) cohort studies that compared the outcome of patients treated during and before the COVID-19 pandemic; (2) studies involving patients who presenting with STEMI; and (3) studies in which all patients underwent coronary angiography with the intent for PCI as the treatment strategy of choice. Studies that reported on either D2B or mortality were included. However, studies were excluded when they included patients with nonspecific diagnosis at presentation, patients with non-STEMI, or if they failed to make a comparison between patients treated during and before the COVID-19 pandemic.
Outcomes and data extraction
Data from included studies were extracted by the same independent pair of authors (V.X.Y.T. and R.R.Y.H.) using a standardized protocol and reporting form. Disagreements were resolved by obtaining the consensus with a senior author. The following information was extracted: study characteristics (study name, authors, publication year, country of origin, sample size, and the pandemic and pre-pandemic periods as defined by the individual studies), study sample characteristics (mean age, sex, and major comorbidities), and primary and secondary outcomes as detailed in the following paragraphs.
The primary outcome for medical service efficiency was D2B, and the primary treatment outcome was all-cause mortality. D2B was defined as the length of time during which the patient with STEMI arrived at the hospital to either needle entry, balloon inflation, or other device deployment.18 If a study reported multiple time points, the time from hospital arrival to balloon inflation was used for our analysis. A summary of the definitions of D2B by individual studies is shown in Supplemental Table S1.
Secondary outcomes included onset to door time (O2D), left ventricular ejection fraction (LVEF), cardiogenic shock, procedural success, length of hospital and intensive care unit (ICU) stay, and major adverse cardiac events (MACE). MACE was defined as a combination of all-cause mortality, repeat revascularization, stroke, heart failure, nonfatal reinfarction, stent thrombosis, or major bleeding.19 O2D time was defined as the time between the onset of symptoms and arrival at the ED of a PCI-capable hospital.20, 21, 22, 23, 24 Study and patient demographic characteristics, procedural outcomes (D2B, post-PCI Thrombolysis In Myocardial Infarction [TIMI] flow grade), and complications data were extracted from included studies. When the mean and SD were not available, estimation of mean and SD was performed using the methods described by Wan et al.25 using the study sample size, median, range, and/or interquartile range.
Statistical analysis
Pairwise meta-analysis was performed to synthesize observational data for binary and continuous outcomes. Odds ratios (ORs) were used to compare binary outcome data, and weighted mean differences (WMDs) were used to compare continuous outcome data. In the analysis of OR and WMD, the Mantel-Haenszel and inverse variance models were used to pool the results, respectively. Heterogeneity scores were measured using the I 2 statistic and Cochran Q test, with 40% or P < 0.10, respectively, indicative of substantial heterogeneity.26 Random effects were used in all analysis regardless of heterogeneity. All analyses were performed using Review Manager (RevMan) version 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) and Stata version 16.1 (StataCorp; College Station, TX); and statistical significance was considered at a P value ≤ 0.05. Subgroup analyses were conducted on the basis of geography (Eastern and Western centres) and country level-income (high income vs low–middle-income). Western centres included studies from Europe, whereas Eastern centres included studies from the Middle East and Asia. The countries were stratified into 2 groups—high and low–middle-income—using the gross national income per capita valued annually in US dollars according to the World Bank classification of countries by income, which has been a widely accepted classification tool since 1989.27 A pictorial representation of this classification of included studies is shown in Supplemental Figure S1. When there were sufficient studies reporting a given outcome (n > 10), publication bias was assessed using Egger regression and the Harbord test for continuous and binary outcomes, respectively.
Risk of bias and quality assessment
There were methodological challenges in studying the effect of pandemic on the prognosis of STEMI patients that conventional risk of bias tools, such as Risk Of Bias In Non-randomised Studies - of Interventions (ROBINS-I), would have been suboptimal in the evaluation of COVID-19 era studies because of the presence of collider bias.28 In a systematic review Iwakami et al. described the suitability of the Quality In Prognosis Studies (QUIPS)29 in the bias assessment of included studies that compared the prognosis of retrospectively replicated cohorts.30 The QUIPS tool evaluates the risk of bias of studies using 6 domains, namely, study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, and statistical analysis. Quality assessment of included articles was performed using the Newcastle-Ottawa Scale (NOS), which allows for grading of each article on cohort selection, as well as the adequacy of outcomes measured.31 Two authors (R.R.Y.H. and V.X.Y.T.) performed concurrent independent bias evaluation of the studies.
Results
Summary of included studies
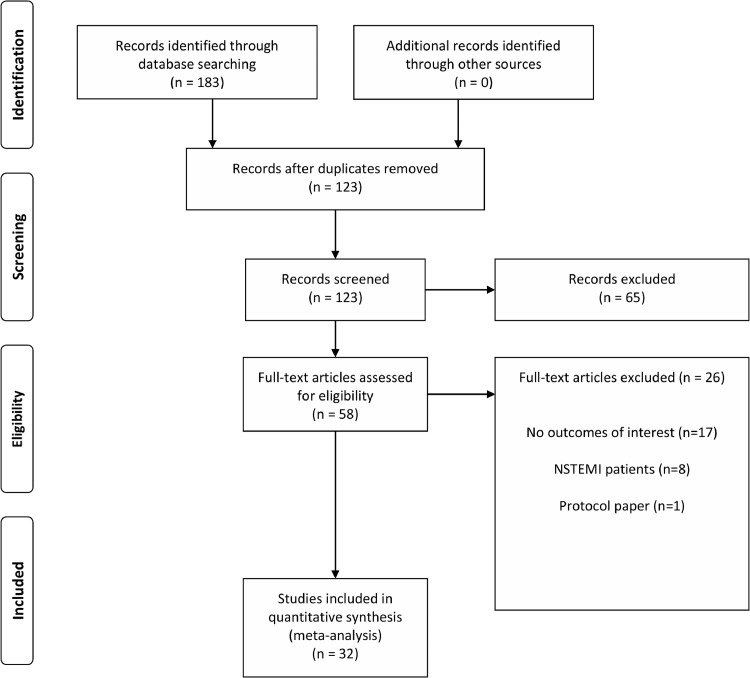
A flow diagram of the literature search and related screening process is shown in Figure 1 . A total of 32 studies met our inclusion criteria. Four studies each originated from China,4 , 24 , 32 , 33 Italy,20 , 34, 35, 36 and North America,37, 38, 39, 40 3 each from France41, 42, 43 and Turkey,44, 45, 46 2 from the United Kingdom,47 , 48 and 1 each from Austria,49 Belgium,50 Egypt,51 Iran,52 Israel,53 Japan,54 Pakistan,55 Poland,56 Singapore,23 Spain,57 and Switzerland.58 One study was a multicentred cohort study of various databases belonging to different European countries.59 All studies were retrospective in study design. In total, 20,492 and 70,217 patients underwent primary PCI for STEMI during and before the pandemic, respectively. A summary of the characteristics of included articles is shown in Supplemental Table S2. Several studies reported the proportion of patients who presented with out-of-hospital cardiac arrest (OHCA) and cardiogenic shock on arrival. In all 3 studies that reported on OHCA, the proportion of patients who presented with OHCA was observed to be greater during compared with before the pandemic.23 , 42 , 59 Seven studies reported on the proportion of patients who presented with cardiogenic shock, of which 5 of the studies showed a greater proportion of patients who presented with cardiogenic shock during compared with before the pandemic.20 , 42 , 43 , 48 , 59 A summary of the results is shown in Supplemental Table S3.
Figure 1.
Flow chart of study selection. NSTEMI, non-ST-elevation myocardial infarction.
Primary outcomes
D2B
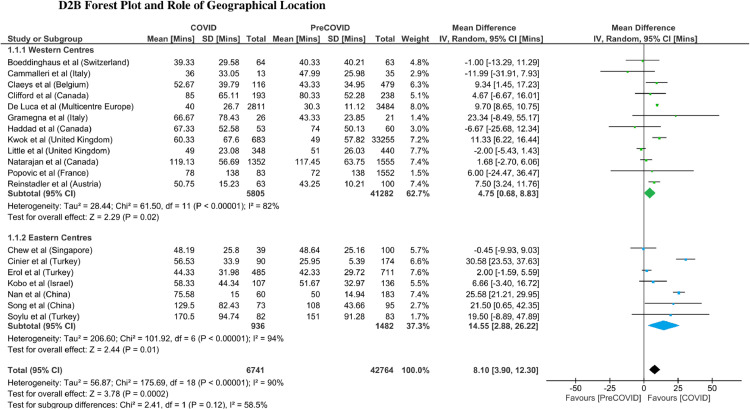
Nineteen studies reported D2B at their respective institutions. D2B was significantly longer during, compared with before the pandemic (n = 49,505; WMD, 8.10 minutes; 95% confidence interval [CI], 3.90-12.30 minutes; P = 0.0002). Because study heterogeneity of the overall D2B comparison was considerable (I 2 = 90%), subgroup analyses were performed to further investigate heterogeneity. D2B was observed to be significantly longer during the pandemic in the Western (n = 47,087; WMD, 4.75 minutes; 95% CI, 0.68-8.83 minutes; P = 0.02) and Eastern (n = 2418; WMD, 14.55 minutes; 95% CI, 2.88-26.22 minutes; P = 0.01) countries; without any overall difference between both subgroups (P = 0.12; Fig. 2 ). Further subgroup analysis of high-income and low–middle-income countries showed a trend toward longer average D2B in low–middle-income countries (n = 2036; WMD, 19.64 minutes; 95% CI, 4.61-34.68 minutes; P = 0.01) compared with high-income countries (n = 47,469; WMD, 4.52 minutes; 95% CI, 0.80-8.25 minutes; P = 0.02). However, there was no significant difference between the subgroups (P = 0.06). Egger regression analysis did not identify any significant publication bias (P = 0.512).
Figure 2.
Door to balloon time forest plot and subgroup analysis on the basis of geographical location.
Mortality
In-hospital mortality after primary PCI was reported by 26 studies, with significantly lower mortality rates before, compared with during the pandemic (n = 85,367; OR = 1.27; 95% CI, 1.09-1.49; P = 0.002). The overall mortality rates were 5.43% (1023/18,854) during the pandemic and 4.62% (3070/66,513) before the pandemic. There was no significant publication bias among these studies, which was assessed using the Harbord test (P = 0.462). Study heterogeneity for the overall comparison of in-hospital mortality rates was moderate (I 2 = 36%). Hence, subgroup analyses were undertaken as a means to further investigate potential sources of heterogeneity.
Subgroup analyses showed a significantly increased intrapandemic mortality rate among the Eastern countries, compared with that of the prepandemic period (n = 31,066; OR, 1.41; 95% CI, 1.09-1.83; P = 0.01). There was an observable increase in mortality among the Western countries intrapandemically compared with the prepandemic period, although this did not reach statistical significance (n = 54,301; OR, 1.19; 95% CI, 0.95-1.49; P = 0.13; Fig. 3 ). Mortality rates were 4.90% (636/12,969) and 4.07% (737/18,097) during and before the pandemic, respectively, for centres based in the Eastern countries, and 6.58% (387/5885) and 4.82% (2333/48,416) during and before the pandemic, respectively, for centres based in the Western countries. There was no significant difference in mortality rates between the 2 geographical regions (P = 0.34).
Figure 3.
Mortality rate forest plot and subgroup analysis in terms of study geographical location.
Additional subgroup analyses of high income compared with low–middle-income countries showed a significantly increased rate of mortality among the low–middle-income countries during, compared with before the pandemic (n = 30,098; OR, 1.52; 95% CI, 1.13-2.05; P = 0.006). Conversely there was an observable increase in mortality among the high-income countries intrapandemically compared with the prepandemic period, although this did not reach statistical significance (n = 55,269; OR, 1.17; 95% CI, 0.95-1.44; P = 0.13; Fig. 4 ). There was no significant difference in mortality rates between the high- and low–middle-income countries (P = 0.16).
Figure 4.
Mortality rate forest plot and subgroup analysis in terms of country income status.
On further analysis of the subgroup of Eastern countries, Eastern low–middle-income countries in particular observed a significantly higher mortality rate during the COVID-19 pandemic (n = 30,098; OR, 1.52; 95% CI, 1.13-2.05; P = 0.006). However, the Eastern high-income countries did not experience significantly different mortality rates between the time periods during and before the pandemic (n = 968; OR, 1.01; 95% CI, 0.55-1.87; P = 0.98). The differences in mortality according to the income status of the Eastern countries was not significant (P = 0.24).
Secondary outcomes
O2D
Nine studies reported the delay in O2D. The COVID-19 pandemic was associated with patients having a significantly longer O2D, compared with patients who presented before the pandemic (n = 37,331; WMD, 38.22 minutes; 95% CI, 12.67-63.77 minutes; P = 0.003).
Left ventricular systolic function and cardiogenic shock
Considering the 8 studies that reported LVEF of the patients on discharge, patients who underwent PCI during the pandemic had worse LVEF compared with those treated before the pandemic (n = 1040; WMD, 4.20%; 95% CI, 1.19%-7.21%; P = 0.006). Post-PCI cardiogenic shock was reported in 12 studies, with no significant difference in the incidence between the 2 study periods (n = 63,024; OR, 1.03; 95% CI, 0.86-1.23; P = 0.75).
Procedural characteristics
Post-PCI TIMI grading was used by 13 studies to measure the success of reperfusion with TIMI grade < 3 indicative of suboptimal reperfusion. Patients admitted during the pandemic were more likely to experience suboptimal reperfusion after PCI, compared with those admitted before the pandemic (n = 44,165; OR, 1.60; 95% CI, 1.17-2.21; P = 0.004).
In-hospital and ICU length of stay
STEMI patients who underwent PCI during the pandemic had longer duration of ICU stay (n = 423; WMD, 0.70 days; 95% CI, 0.40-0.99 days; P < 0.00001). However, the overall length of hospital stay was similar in patients admitted during and before the pandemic (n = 43,467; WMD, 0.24 days; 95% CI, −0.46 to 0.93 days; P = 0.51).
MACE
There was an increased risk of MACE during the pandemic, compared with the prepandemic period (n = 65,436; OR, 1.54; 95% CI, 1.18-2.00; P = 0.001).
Discussion
To our knowledge, this meta-analysis is the first to show that the delays caused by the COVID-19 pandemic in STEMI care could be associated with an increased mortality rate, especially among the low–middle-income countries. There was a significant increase in D2B and the mortality rate during, compared with before the pandemic. The increase in D2B was observed regardless of the geographical location or country income status. However, after adjusting for relevant variables, the mortality rate during the pandemic was significantly increased only among the Eastern low–middle-income countries.
During the pandemic, there was a global reduction in STEMI admissions compared with before the pandemic.58 Of the 32 included studies, 21 made a time-matched comparison of the number of STEMI admissions between the study periods. All 21 studies reported decreased STEMI admissions to the respective institutes during compared with before the pandemic (Supplemental Table S2). Among studies that reported clinical presentations, there was a higher proportion of patients with more severe clinical presentations (cardiogenic shock and OHCA) during compared with before the pandemic.20 , 24 , 32 , 34 , 42 , 43 , 48 , 59 Patients admitted during the pandemic had less favourable procedural outcomes with a higher proportion of them with post-PCI TIMI < 3 grading, and worse clinical outcomes as evident by higher incidences of MACE, lower LVEF on discharge, and longer ICU stay compared with those admitted before the pandemic.
The prothrombotic milieu of the COVID-19 virus infection, with the potential increased tendency of plaque rupture has led to an anticipated increase in patients presenting with acute coronary syndromes.60, 61, 62 Paradoxically, there was a global reduction of STEMI-related hospitalizations in the usually high-volume centres irrespective of geographically location.15 , 63, 64, 65 It has been postulated that this reduction could be attributed to fewer patients seeking help for STEMI-related symptoms because of fear of COVID-19 exposure or reduced access to medical services as a result of the overwhelmed health services. Such adverse health-seeking behaviour was not limited to geographical regions with higher COVID-19 burden or death toll. De Luca and colleagues reported significant heterogeneity in primary PCI volume across different European centres, which was unrelated to the number of COVID-19 cases or COVID-19-related deaths.59 As a result, increased mortality and morbidity due to prolonged total ischemic time and associated adverse consequences has been observed in multiple studies.4 , 20 , 21 , 24 , 32 , 36 , 44 , 53 , 57 , 59
The American College of Cardiology and Society for Cardiovascular Angiography and Interventions still advocate PCI as the main reperfusion strategy for STEMI patients during the pandemic with the same general D2B targets.2 However, our study showed a significant increase in D2B during the pandemic regardless of the geographical location or income status of a country. Among the reasons for delay detailed in several studies include: (1) an overwhelmed ED; (2) ever-changing STEMI pathways for COVID-19 testing before transfer to the catheterization laboratory; (3) stringent infection control measures; (4) late presentation outside of therapeutic window for PCI; and (5) limited availability of personnel protective equipment.58 , 60 , 66 It has also been suggested that the largest component of delay in D2B was in the ED, because it serves as the gatekeeper to screen for COVID-19 risk factors and implement safe transfers to the catheterization laboratory.23
Moreover, the significant delay in O2D observed during the pandemic is also alarming. Several studies postulated that the reasons for delay in O2D were related to the fear of COVID-19 exposure in hospitals, ill-informed altruistic behaviour not to overburden the hospital system, or social distancing measures.11, 12, 13, 14, 15 , 67 Additionally, it remains plausible that the more severe disease state at presentation among patients observed during the pandemic could also partly be related to delayed presentation and/or treatment, potentially translating to poorer long-term outcomes. This is consistent with our findings of the universally higher incidence of MACE and worse left ventricular systolic dysfunction.
The advent of such barriers to timely reperfusion could be a plausible explanation for the increase in in-hospital mortality rates, with delayed O2D and D2B potentially resulting in the failure to meet the limited window of time available for reperfusion to be effective in reversing the pathophysiology of ischemic cardiomyocyte death. Previous observational studies have suggested that small incremental improvements in D2B did not affect in-hospital mortality.68 During the pandemic, there was, on average, an 8-minute delay in D2B. Apart from the prolonged total ischemic time contributed by increased O2D (contributed by a complex interplay of patient and emergency medical services-related delays), other pandemic-specific factors might contribute to the increased in-hospital mortality rates. It is intuitive to speculate that these pandemic-specific factors include the more severe clinical presentations, associated effects of social distancing such as more sedentary lifestyle, avoidance of angiotensin-converting enzyme inhibitors and angiotensin receptor blocker use because of the initial alarming concern that these agents might increase susceptibility to COVID-19 infection,56 and the overwhelmed support services in STEMI care such as respiratory therapy, and allied health care services including cardiac rehabilitation. As the pandemic continues to evolve, and with the increasing availability of the COVID-19 vaccine,69 , 70 only time will tell the true long-term effects of the pandemic on cardiovascular diseases and economic burden on the health care system. For now, strategies to address health care system delays will help to reduce the total ischemic time.63 Experience in the pandemic should serve as an important lesson to all levels of the health care system such that infection control measures might be more organized in dealing with future pandemics, and at the same time maintain the efficiency of time-sensitive acute medical services such as primary PCI and STEMI care.
The findings of our study are in stark contrast to a recent review, which only included studies published before August 2020 and showed no differences in short-term mortality before and during the pandemic among patients who underwent primary PCI for STEMI.71 Global response to the pandemic is rapidly changing, and potentially diverging in terms of the pace at which certain countries mount the learning curve of adapting to the pandemic. As such, although early studies might have shown a global homogeneity in keeping intrapandemic mortality rates comparable with that of the prepandemic level, our latest cumulative evidence suggests a potential increase in overall short-term mortality rates among the Eastern countries and countries of lower-income status during the pandemic. Through serial subgroup analyses adjusted for geographical location, income status, and subsequently both of these variables, we observed that Eastern countries with a low–middle-income status faced the highest increased rate of mortality during the COVID-19 pandemic. Conversely, the increase in mortality rates between the 2 study periods among the Western or high-income countries was not statistically significant. This raises immediate concern on the challenges faced by the low–middle-income countries during the pandemic and might suggest that countries lacking advanced infrastructure to surmount the barriers to timely reperfusion are unable to cope with the effects of COVID-19 pandemic on STEMI care.
Strengths and limitations
This meta-analysis on the global effect of the COVID-19 pandemic on STEMI care raises relevant and immediate questions on strategies for subsequent increases in infection rates or, in a broader context, on future outbreaks. Recent evidence suggests a rebound increase in STEMI admissions reverting back to the usual 2019 levels a few months into the pandemic.23 , 66 These factors might exacerbate the strain on the health care system with longer-lasting prognostic and economic effects. With the evidence from this study suggesting that the strain on the health care system mainly affecting countries of low–middle-income, a strong call to action can be made to greater optimize the pace at which such countries mount the response curve of adapting to the barriers to achieving timely reperfusion for STEMI patients. In general, all acute medical services especially the time-sensitive ones are likely to be adversely affected in one way or another. Lessons from previous and current outbreaks must be learned so that the world communities could be better prepared as the COVID-19 pandemic continues to escalate and also for future outbreaks.
Although the findings are relevant to the COVID-19 pandemic, our study has several limitations. First, although the differences in outcome between the 2 study periods were statistically significant, they should be interpreted with caution because the reporting of outcomes from different studies might vary. Furthermore, some subgroup analyses included relatively small sample sizes that might be underpowered to detect any clinically meaningful differences. Second, because of the clinical context, all studies included in this analysis were retrospective studies. Moreover, D2B definitions might vary among the studies but they are considered clinically and prognostically relevant to the respective health systems. In addition, measures were taken to standardize the definition of D2B for this analysis by using the time from hospital arrival to balloon inflation if multiple time points were reported. In addition, our global estimates might be subjected to publication bias because studies included were limited to those published in English, and only certain health care organizations had the capability to collect and publish data. Finally, only short-term outcomes are available at the current phase of the COVID-19 pandemic. Longer-term studies are vitally important especially that current data indicate poorer short-term outcomes among STEMI patients who undergo primary PCI, which in turn, could adversely affect the long-term outcomes of these patients. Interventions to mitigate delays and improve STEMI care efficiency during the pandemic should be evaluated.
Conclusion
The COVID-19 pandemic is associated with worse STEMI performance metrics and clinical outcomes worldwide with worse clinical status at presentation, D2B delay irrespective of geographic location or income status of a country, as well as less favourable post-PCI outcomes despite a reduction in STEMI admissions. Mortality rates, although unaffected in high-income countries, significantly increased during the COVID-19 pandemic in low–middle-income countries. Better strategies are needed to address these global trends in STEMI care especially among the communities at risk.
Funding Sources
None.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 1457 for disclosure information.
To access the supplementary material accompanying this article, visit the online version of the Canadian Journal of Cardiology at www.onlinecjc.ca and at doi:10.1016/j.cjca.2021.04.003.
Appendix. Supplementary materials
References
- 1.Ow ZGW, Cheong CK, Chin YH, Chin BZ. A look at the global impact of SARS CoV-2 on orthopedic services. J Clin Orthop Trauma. 2021;12:33–39. doi: 10.1016/j.jcot.2020.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahmud E, Dauerman HL, Welt FGP, et al. Management of acute myocardial infarction during the COVID-19 pandemic: a position statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP) J Am Coll Cardiol. 2020;76:1375–1384. doi: 10.1016/j.jacc.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2017;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 4.Xiang D, Xiang X, Zhang W, et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. 2020;76:1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sadeghipour P, Talasaz AH, Eslami V, et al. Management of ST-segment-elevation myocardial infarction during the coronavirus disease 2019 (COVID-19) outbreak: Iranian “247” National Committee's position paper on primary percutaneous coronary intervention. Catheter Cardiovasc Interv. 2021;97:E346–E351. doi: 10.1002/ccd.28889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xiang D, Huo Y, Ge J. Expert consensus on operating procedures at chest pain centers in China during the coronavirus infectious disease-19 epidemic. Cardiol Plus. 2020;5:21–32. doi: 10.4103/cp.cp_5_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahmud E, Dauerman HL, Welt FGP, et al. Management of acute myocardial infarction during the COVID-19 pandemic: a consensus statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP) Catheter Cardiovasc Interv. 2020;96:336–345. doi: 10.1002/ccd.28946. [DOI] [PubMed] [Google Scholar]
- 8.Scotto di Uccio F, Valente S, Colivicchi F, et al. ANMCO position paper: Network Organization for the Treatment of Acute Coronary Syndrome Patients during the Emergency COVID-19 Pandemic. Eur Heart J Suppl. 2020;22(suppl G):G223–G227. doi: 10.1093/eurheartj/suaa111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zaman S, MacIsaac AI, Jennings GL, et al. Cardiovascular disease and COVID-19: Australian and New Zealand consensus statement. Med J Aust. 2020;213:182–187. doi: 10.5694/mja2.50714. [DOI] [PubMed] [Google Scholar]
- 10.Szerlip M, Anwaruddin S, Aronow HD, et al. Considerations for cardiac catheterization laboratory procedures during the COVID-19 pandemic perspectives from the Society for Cardiovascular Angiography and Interventions Emerging Leader Mentorship (SCAI ELM) members and graduates. Catheter Cardiovasc Interv. 2020;96:586–597. doi: 10.1002/ccd.28887. [DOI] [PubMed] [Google Scholar]
- 11.De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41:2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roffi M, Guagliumi G, Ibanez B. The obstacle course of reperfusion for ST-segment-elevation myocardial infarction in the COVID-19 pandemic. Circulation. 2020;141:1951–1953. doi: 10.1161/CIRCULATIONAHA.120.047523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Piccolo R, Bruzzese D, Mauro C, et al. Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID-19 outbreak. Circulation. 2020;141:2035–2037. doi: 10.1161/CIRCULATIONAHA.120.047457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tam CF, Cheung KS, Lam S, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong. China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-Segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of Observational Studies in Epidemiology. A proposal for reporting. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 17.Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005;85:257–268. [PubMed] [Google Scholar]
- 18.Foo CY, Bonsu KO, Nallamothu BK, et al. Coronary intervention door-to-balloon time and outcomes in ST-elevation myocardial infarction: a meta-analysis. Heart. 2018;104:1362–1369. doi: 10.1136/heartjnl-2017-312517. [DOI] [PubMed] [Google Scholar]
- 19.Poudel I, Tejpal C, Rashid H, Jahan N. Major adverse cardiovascular events: an inevitable outcome of ST-elevation myocardial infarction? A literature review. Cureus. 2019;11:e5280. doi: 10.7759/cureus.5280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gramegna M, Baldetti L, Beneduce A, et al. ST-segment-elevation myocardial infarction during COVID-19 pandemic: insights from a regional public service healthcare hub. Circ Cardiovasc Interv. 2020;13 doi: 10.1161/CIRCINTERVENTIONS.120.009413. [DOI] [PubMed] [Google Scholar]
- 21.Kwok CS, Gale CP, Kinnaird T, et al. Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart. 2020;106:1805–1811. doi: 10.1136/heartjnl-2020-317650. [DOI] [PubMed] [Google Scholar]
- 22.Little C, Jabbour R, Kotecha T, et al. TCT CONNECT-221 primary PCI for STEMI during the COVID-19 pandemic in London: a systematic analysis of pathway activation and outcomes. J Am Coll Cardiol. 2020;76:B96. [Google Scholar]
- 23.Chew NW, Sia CH, Wee HL, et al. Impact of the COVID-19 pandemic on door-to-balloon time for primary percutaneous coronary intervention- results from the Singapore Western STEMI Network. Circ J. 2021;85:139–149. doi: 10.1253/circj.CJ-20-0800. [DOI] [PubMed] [Google Scholar]
- 24.Nan J, Meng S, Hu H, et al. Comparison of clinical outcomes in patients with ST elevation myocardial infarction with percutaneous coronary intervention and the use of a telemedicine app before and after the COVID-19 pandemic at a center in Beijing, China, from August 2019 to March 2020. Med Sci Monit. 2020;26 doi: 10.12659/MSM.927061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sabawoon W. Differences by country-level income in COVID-19 cases, deaths, case-fatality rates, and rates per million population in the first five months of the pandemic. Available at: https://www.medrxiv.org/content/10.1101/2020.07.13.20153064v1. Accessed March 15, 2021.
- 28.Griffith GJ, Morris TT, Tudball MJ, et al. Collider bias undermines our understanding of COVID-19 disease risk and severity. Nat Commun. 2020;11:5749. doi: 10.1038/s41467-020-19478-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grooten WJA, Tseli E, Äng BO, et al. Elaborating on the assessment of the risk of bias in prognostic studies in pain rehabilitation using QUIPS—aspects of interrater agreement. Diagn Progn Res. 2019;3:5. doi: 10.1186/s41512-019-0050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iwakami N, Nagai T, Furukawa TA, et al. Optimal sampling in derivation studies was associated with improved discrimination in external validation for heart failure prognostic models. J Clin Epidemiol. 2020;121:71–80. doi: 10.1016/j.jclinepi.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 31.Wells G, Shea B, O Connell DL, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed March 20, 2021.
- 32.Song C, Liu S, Yin D, et al. Impact of public health emergency response to COVID-19 on management and outcome for STEMI patients in Beijing—a single-center historic control study. Curr Probl Cardiol. 2021;46 doi: 10.1016/j.cpcardiol.2020.100693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang B, Xu C, Liu H, et al. In-hospital management and outcomes of acute myocardial infarction before and during the coronavirus disease 2019 pandemic. J Cardiovasc Pharmacol. 2020;76:540–548. doi: 10.1097/FJC.0000000000000909. [DOI] [PubMed] [Google Scholar]
- 34.Cammalleri V, Muscoli S, Benedetto D, et al. Who has seen patients with ST-segment-elevation myocardial infarction? First results from Italian real-world coronavirus disease 2019. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.017126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fileti L, Vecchio S, Moretti C, et al. Impact of the COVID-19 pandemic on coronary invasive procedures at two Italian high-volume referral centers. J Cardiovasc Med (Hagerstown) 2020;21:869–873. doi: 10.2459/JCM.0000000000001101. [DOI] [PubMed] [Google Scholar]
- 36.Tomasoni D, Adamo M, Italia L, et al. Impact of COVID-2019 outbreak on prevalence, clinical presentation and outcomes of ST-elevation myocardial infarction. J Cardiovasc Med (Hagerstown) 2020;21:874–881. doi: 10.2459/JCM.0000000000001098. [DOI] [PubMed] [Google Scholar]
- 37.Clifford CR, Le May M, Chow A, et al. Delays in ST-elevation myocardial infarction care during the COVID-19 lockdown: an observational study. CJC Open 2020;3:565-73. [DOI] [PMC free article] [PubMed]
- 38.Haddad K, Potter BJ, Matteau A, Gobeil F, Mansour S. Implications of COVID-19 on time-sensitive STEMI care: a report from a North American epicenter. Cardiovasc Revasc Med 2021;30:33–7. [DOI] [PMC free article] [PubMed]
- 39.Hannan EL, Wu Y, Cozzens K, et al. Percutaneous coronary intervention for ST-elevation myocardial infarction before and during COVID in New York. Am J Cardiol. 2021;142:25–34. doi: 10.1016/j.amjcard.2020.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Natarajan MK, Wijeysundera HC, Oakes G, et al. Early observations during the COVID-19 pandemic in cardiac catheterization procedures for ST-elevation myocardial infarction across Ontario. CJC Open. 2020;2:678–683. doi: 10.1016/j.cjco.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hauguel-Moreau M, Pillière R, Prati G, et al. Impact of coronavirus disease 2019 outbreak on acute coronary syndrome admissions: four weeks to reverse the trend. J Thromb Thrombolysis. 2021;51:31–32. doi: 10.1007/s11239-020-02201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Popovic B, Varlot J, Metzdorf PA, et al. Changes in characteristics and management among patients with ST-elevation myocardial infarction due to COVID-19 infection. Catheter Cardiovasc Interv. 2021;97:E319–E326. doi: 10.1002/ccd.29114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rangé G, Hakim R, Beygui F, et al. Incidence, delays, and outcomes of STEMI during COVID-19 outbreak: analysis from the France PCI registry. J Am Coll Emerg Physicians Open. 2020;1:1168–1176. doi: 10.1002/emp2.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Çinier G, Hayıroğlu M, Pay L, et al. Effect of the COVID-19 pandemic on access to primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Turk Kardiyol Dern Ars. 2020;48:640–645. doi: 10.5543/tkda.2020.95845. [DOI] [PubMed] [Google Scholar]
- 45.Soylu K, Coksevim M, Yanık A, Bugra Cerik I, Aksan G. Effect of Covid-19 pandemic process on STEMI patients timeline. Int J Clin Pract. 2021;75:e14005. doi: 10.1111/ijcp.14005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Erol MK, Kayikcioglu M, Kilickap M, et al. Treatment delays and in-hospital outcomes in acute myocardial infarction during the COVID-19 pandemic: a nationwide study. Anatol J Cardiol. 2020;24:334–342. doi: 10.14744/AnatolJCardiol.2020.98607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kwok CS, Gale CP, Curzen N, et al. Impact of the COVID-19 pandemic on percutaneous coronary intervention in England: insights from the British Cardiovascular Intervention Society PCI database cohort. Circ Cardiovasc Interv. 2020;13 doi: 10.1161/CIRCINTERVENTIONS.120.009654. [DOI] [PubMed] [Google Scholar]
- 48.Little CD, Kotecha T, Candilio L, et al. COVID-19 pandemic and STEMI: pathway activation and outcomes from the pan-London heart attack group. Open Heart. 2020;7 doi: 10.1136/openhrt-2020-001432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reinstadler SJ, Reindl M, Lechner I, et al. Effect of the COVID-19 pandemic on treatment delays in patients with st-segment elevation myocardial infarction. J Clin Med. 2020;9:1–10. doi: 10.3390/jcm9072183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Claeys MJ, Argacha JF, Collart P, et al. Impact of COVID-19-related public containment measures on the ST elevation myocardial infarction epidemic in Belgium: a nationwide, serial, cross-sectional study [e-pub ahead of print]. Acta Cardiol doi:10.1080/00015385.2020.1796035, accessed September 4, 2021. [DOI] [PubMed]
- 51.Ayad S, Shenouda R, Henein M. The impact of covid-19 on in-hospital outcomes of ST-segment elevation myocardial infarction patients. J Clin Med. 2021;10:1–7. doi: 10.3390/jcm10020278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salarifar M, Ghavami M, Poorhosseini H, et al. The impact of a dedicated coronavirus disease 2019 primary angioplasty protocol on time components related to ST-segment elevation myocardial infarction management in a 24/7 primary percutaneous coronary intervention–capable hospital. Kardiol Pol. 2020;78:1227–1234. doi: 10.33963/KP.15607. [DOI] [PubMed] [Google Scholar]
- 53.Kobo O, Efraim R, Saada M, et al. The impact of lockdown enforcement during the SARSCoV-2 pandemic on the timing of presentation and early outcomes of patients with ST-elevation myocardial infarction. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kitahara S, Fujino M, Honda S, et al. COVID-19 pandemic is associated with mechanical complications in patients with ST-elevation myocardial infarction. Open Heart. 2021;8 doi: 10.1136/openhrt-2020-001497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mengal N, Saghir T, Hassan Rizvi SN, et al. Acute ST-elevation myocardial infarction before and during the COVID-19 pandemic: what is the clinically significant difference? Cureus. 2020;12:e10523. doi: 10.7759/cureus.10523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Siudak Z, Grygier M, Wojakowski W, et al. Clinical and procedural characteristics of COVID-19 patients treated with percutaneous coronary interventions. Catheter Cardiovasc Interv. 2020;96:E568–E575. doi: 10.1002/ccd.29134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rodríguez-Leor O, Cid-Álvarez B, Pérez de Prado A, et al. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev Esp Cardiol (Engl Ed) 2020;73:994–1002. doi: 10.1016/j.rec.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tanner R, MacDaragh Ryan P, Caplice NM. COVID-19-where have all the STEMIs gone? Can J Cardiol. 2020;36:1161. doi: 10.1016/j.cjca.2020.04.032. e9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.De Luca G, Verdoia M, Cercek M, et al. Impact of COVID-19 Pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76:2321–2330. doi: 10.1016/j.jacc.2020.09.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 61.Madjid M, Vela D, Khalili-Tabrizi H, Casscells SW, Litovsky S. Systemic infections cause exaggerated local inflammation in atherosclerotic coronary arteries: clues to the triggering effect of acute infections on acute coronary syndromes. Tex Heart Inst J. 2007;34:11–18. [PMC free article] [PubMed] [Google Scholar]
- 62.Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alrawashdeh A, Nehme Z, Williams B, Stub D. Emergency medical service delays in ST-elevation myocardial infarction: a meta-analysis. Heart. 2020;106:365. doi: 10.1136/heartjnl-2019-315034. [DOI] [PubMed] [Google Scholar]
- 64.Mafham MM, Spata E, Goldacre R, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Solomon MD, McNulty EJ, Rana JS, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 66.Garcia S, Stanberry L, Schmidt C, et al. Impact of COVID-19 pandemic on STEMI care: an expanded analysis from the United States. Catheter Cardiovasc Interv 2021;98:217–22. [DOI] [PMC free article] [PubMed]
- 67.Trabattoni D, Montorsi P, Merlino L. Late STEMI and NSTEMI patients’ emergency calling in COVID-19 outbreak. Can J Cardiol. 2020;36:1161. doi: 10.1016/j.cjca.2020.05.003. e1167-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Menees DS, Peterson ED, Wang Y, et al. Door-to-balloon time and mortality among patients undergoing primary PCI. N Engl J Med. 2013;369:901–909. doi: 10.1056/NEJMoa1208200. [DOI] [PubMed] [Google Scholar]
- 69.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jackson LA, Anderson EJ, Rouphael NG, et al. An mRNA vaccine against SARS-CoV-2 - preliminary report. N Engl J Med. 2020;383:1920–1931. doi: 10.1056/NEJMoa2022483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rattka M, Dreyhaupt J, Winsauer C, et al. Effect of the COVID-19 pandemic on mortality of patients with STEMI: a systematic review and meta-analysis. Heart. 2021;107:482. doi: 10.1136/heartjnl-2020-318360. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.