Abstract
Objective
To quantify and describe urologic adverse events and symptoms after vaccination with the Pfizer-BioNTech and Moderna COVID-19 vaccines.
Methods and Materials
We queried the FDA Vaccine Adverse Event Reporting System (VAERS) for all reported symptoms following the Pfizer-BioNTech and Moderna vaccines as of February 12th, 2021. All urologic symptoms were isolated and the reported adverse events associated with each symptom were reviewed.
Results
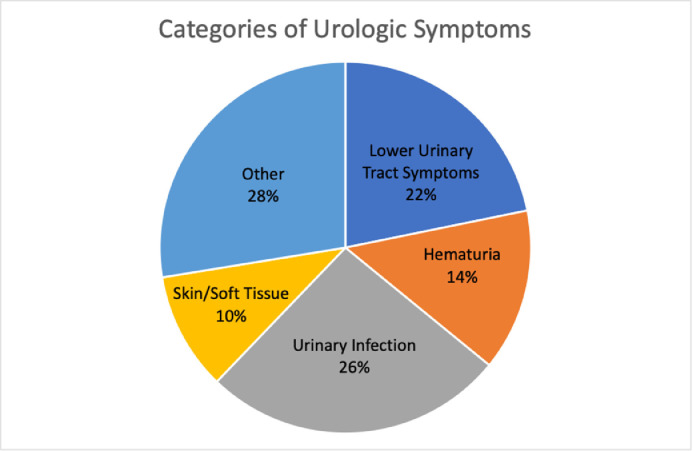
Out of 15,785 adverse event reports, only 0.7% (113) described urologic symptoms. A total of 156 urologic symptoms were described amongst the 113 adverse event reports. The Pfizer-BioNTech vaccine was responsible for 61% of these reports and the Moderna vaccine was responsible for 39%. These symptoms were grouped into five different categories: Lower Urinary Tract Symptoms (n = 34, 22%), Hematuria (n = 22, 14%), Urinary Infection (n = 41, 26%), Skin and/or Soft Tissue (n = 16, 10%), and Other (n = 43, 28%). The median age of the patients reporting urologic symptoms was 63 years (IQR 44-79, Range: 19-96) and 54% of the patients were female.
Conclusion
Urologic symptoms reported after COVID-19 vaccination are extremely rare. Given the common prevalence of many of these reported symptoms in the general population, there does not appear to be a correlation between vaccination and urologic symptoms, but as the vaccination criteria expands, further monitoring of the Vaccine Adverse Event Reporting System is needed.
Keywords: COVID19, vaccination, urologic symptoms, urologic side effects
The COVID-19 pandemic has had a dramatic impact on urologic providers and patients.1 Currently, large scale efforts are underway to vaccinate the majority of the population in an effort to achieve herd immunity. The United States Food and Drug Administration (FDA) issued Emergency Use Authorization for the Pfizer-BioNTech COVID-19 vaccine on December 11, 2020 and the Moderna COVID-19 vaccine on December 18, 2020.2 As of February 12th 2021, over 54 million doses have been administered to the United States population.3
While common and serious adverse events following vaccination have been widely reported and are carefully monitored, there is little known about potential organ-specific complications. 2 , 4 , 5 Given that the number of vaccinations will continue to dramatically increase in the following months, urologists should be aware of potential genitourinary side effects of the vaccine. In this study, we investigated the FDA Vaccine Adverse Event Reporting System (VAERS) to quantify and describe reported urologic symptoms following COVID-19 vaccination with the Pfizer-BioNTech and Moderna vaccines.
METHODS
The FDA VAERS is an early warning system that can detect potential issues with licensed vaccines by recording and analyzing adverse events following vaccinations.6 These adverse events can be submitted by health care professionals, vaccine manufacturers, and the public. Raw VAERS data can be directly downloaded or accessed through the CDC WONDER (Center for Disease Control and Prevention Wide-ranging OnLine Data for Epidemiologic Research) search tool (https://wonder.cdc.gov/vaers.html).
We first queried the CDC WONDER tool for all reported symptoms following the Pfizer-BioNTech and Moderna vaccines that have been processed as of February 12th, 2021. Each adverse event report can contain multiple symptoms related to the patient's clinical presentation or laboratory and imaging findings.
The list of unique symptoms was then reviewed separately by 2 physicians and all urology-specific symptoms were isolated. Nephrology-related side effects or symptoms (eg acute kidney injury, abnormal urine studies not related to infection or hematuria) were excluded from further analysis. Obstetrical and gynecologic symptoms were also excluded. Each urologic symptom was then queried through the CDC WONDER tool to obtain specific details about the related adverse event report. Patient demographics and adverse event description free text were reviewed and compiled. The vaccine manufacturer and the associated dose number was recorded. Non–specific complaints of pain including flank pain (n = 19), groin pain (n = 4), pelvic pain (n = 5), and suprapubic pain (n = 2) were also excluded as the event descriptions did not contain any urologic details. Urologic symptoms were then classified into relevant categories.
RESULTS
Our query generated a list of 15,785 adverse event reports with 73,867 symptoms. A total of 156 urologic symptoms were identified in the VAERS database following administration of the Pfizer-BioNTech or Moderna COVID19 vaccines. We organized the urologic symptoms into 5 different categories: Lower Urinary Tract Symptoms (n = 34, 22%), Hematuria (n = 22, 14%), Urinary Infection (n = 41, 26%), Skin and/or Soft Tissue (n = 16, 10%), and Other (n = 43, 28%). Figure 1 contains the individual symptoms and frequencies in each category. These symptoms came from 113 unique adverse event reports. The median age of the patients reporting urologic symptoms was 63 years (IQR 44-79, Range: 19-96). 54% of the reports were about female patients.
Figure 1.
Categories of urologic symptoms after vaccination (Color version of the figure is available online.)
Of the 113 adverse event reports, 44 (39%) were after the Moderna vaccine and 69 (61%) were after the Pfizer-BioNTech vaccine. There were 85 reports filed after the first vaccine dose and 8 filed after the second vaccine dose while 20 reports did not specify the dose number. Only 18% (20/113) of the adverse events reports described isolated urologic symptoms whereas the majority contained other organ-specific or constitutional symptoms in addition to urologic symptoms. Out of 15,785 total adverse event reports in the VAERS related to COVID vaccines, only 0.7% (113) described a urologic symptom. Urologic complaints made up 0.2% (156/73,867) of all the symptoms reported following vaccination.
DISCUSSION
To our knowledge, this is the first study to investigate urologic symptoms after COVID-19 vaccination as these details were not reported from the Pfizer-BioNTech and Moderna trial results.4 , 5 While the current literature suggests that there may be urologic manifestations of COVID-19 infections, our investigation of the VAERS finds that urologic symptoms reported after COVID-19 vaccination are rare.1 These results suggest that the Pfizer-BioNTech and Moderna vaccines are safe from a urologic standpoint and can provide reassurance and help counsel providers and patients, especially as vaccination efforts continue to grow.
The FDA VAERS is a passive reporting system designed to help monitor the safety of vaccines.6 It cannot determine causality but it can allow for earlier detection of unexpected or unusual patterns of adverse events or “safety signals”, leading to further safety investigation using the CDC Vaccine Safety Datalink (VSD) or the Clinical Immunization Safety Assessment (CISA) project.6
Because of the limitations with report submissions and event descriptions, we cannot create a direct connection between the vaccination and the symptom. For example, although we identified 22 reported symptoms related to hematuria, we do not often know the details of the patient's past medical history and cannot establish a causal link between vaccination and hematuria. In addition, many of the symptoms we identified are common in the general population. Thus, it is difficult to determine what is a true side effect. Nevertheless, some of these reported patient complaints, like lower urinary tract symptoms, could plausibly result from the immune response generated by the vaccine. Interestingly, 75% of the adverse events with urologic symptoms were reported after the first dose. This may represent a reporting bias as patients with severe symptoms after the first dose may have reported their side effects right away while those with milder symptoms after the first dose may have chosen not to report any side effects with either dose. Since the VAERS contains adverse events from voluntary reporters, it may not capture the entire spectrum or quantity of urologic side effects.
Other symptoms reported in the VAERS included laboratory and imaging findings that may not be related to the actual vaccination. For example, 3 adverse events reported a symptom of “Renal Cyst” because the patients were incidentally found to have renal cysts on abdominal imaging following vaccination. While these findings likely do not have any clinical implications, we chose to include them in this study to represent the entire spectrum of urologic symptoms reported in the VAERS.
Finally, it is also important to note that a narrow population of individuals has been vaccinated to date in the United States: healthcare workers, older individuals, and those with significant comorbidities. The patient demographics identified in our study correlate to the demographics of those who had been vaccinated. According to the CDC, in the first month of vaccination, 63% of the patients were women and 55% were 50 years old or older.7 As the vaccination criteria expands to a healthier, younger cohort, the types of reported adverse events may also change. In addition, vaccines with different mechanisms and dosing schedules will need to be carefully monitored.8 Further tracking of the VAERS database will help elucidate these questions.
Footnotes
Disclosures: None
References
- 1.Puliatti S, Eissa A, Eissa R, Amato M, Mazzone E, Dell’Oglio P, et al. COVID-19 and urology: a comprehensive review of the literature. BJU Int. 2020;125:E7–E14. doi: 10.1111/bju.15071. [DOI] [PubMed] [Google Scholar]
- 2.Gee J, Marquez P, Su J, Calvert G, Liu R, Myers T, et al. First month of COVID-19 vaccine safety monitoring — United States, december 14, 2020–january 13, 2021. MMWR Morb Mortal Wkly Rep. 2021 doi: 10.15585/mmwr.mm7008e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.“CDC COVID Data Tracker.”Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, covid.cdc.gov/covid-data-tracker/. Accessed February 15th, 2021.
- 4.Polack F, Thomas S, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the bnt162b2 mrna covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mrna-1273 sars-cov-2 vaccine. N Engl J Med. 2021;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaccine Adverse Event Reporting System (VAERS), U.S. Department of Health and Human Services. vaers.hhs.gov/. Accessed February 15th, 2021
- 7.Painter EM, Ussery EN, Patel A, Hughes M, Zell E, Moulia D, et al. Demographic characteristics of persons vaccinated during the first month of the COVID-19 vaccination program — United States, december 14, 2020–january 14, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:174–177. doi: 10.15585/mmwr.mm7005e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sadoff J, Le Gars M, Shukarev G, Heerwegh D, Truyers C, de Groot A, et al. Interim results of a phase 1-2a trial of ad26. Cov2. S covid-19 vaccine. N Engl J Med. 2021;384:1824–1835. doi: 10.1056/NEJMoa2034201. [DOI] [PMC free article] [PubMed] [Google Scholar]