Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has affected many countries negatively, particularly in terms of their health care and financial systems. Numerous countries have attempted to employ precautions to address this pandemic. This study was aimed at exploring and assessing the early precautionary actions taken by 175 countries on six continents to prevent the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Methods
An observational study utilizing available public data was conducted on the basis of data collected from December 31, 2019 until the end of April 2020 and then compared with data in January 2021. Several data were extracted, including information related to the date of the first reported case of SARS-CoV-2, total confirmed cases, total active cases and more. In addition, seven validated indicators were used to assess the countries’ preparedness and precautionary actions.
Results
A total of 175 countries were included in the study. The total COVID-19 infection rate increased exponentially and rapidly in North America and Europe from March to April. The application of precautions (indicators) varied between countries. School closures, quarantines and curfews were the most-applied indicators among all countries. As for the relationship between the indicators and their effects on the infection rate, Italy and Spain were the top countries in Europe and adopted all the indicators. Nevertheless, they faced high infection rates: 239,639 and 205,463 COVID-19 cases in Spain and Italy, respectively.
Conclusion
The precautionary actions might have played a role in limiting the spread of COVID-19 in several countries. However, many countries might not benefit from applying these indicators.
Keywords: Coronavirus disease 2019, COVID-19, Infection rate, Mortality rate, Pandemic, SARS-CoV-2, Precautionary actions
1. Introduction
During the last 20 years, there have been several epidemics associated with viruses, including SARS-associated coronavirus, H1N1 influenza and Middle East Respiratory Syndrome CoronaVirus (MERS-CoV), and all these epidemics have imposed a humanistic and economic burden on several countries (Cascella et al., 2020). The first cases of coronavirus disease 2019 (COVID-19) were reported to the World Health Organization (WHO) in December 31, 2019.
The WHO initially believed COVID-19 would be limited to China. However, given the increased number of cases and countries that have been affected, it was considered a high-level epidemic (Cascella et al., 2020). On March 11, the WHO declared COVID-19 a pandemic because it had spread to most countries, and millions of patients were affected by the disease worldwide (WHO, 2020a).
All data showed that even in countries with a well-developed public health system, COVID-19 imposes a considerable burden not only on health care but also at the country level. Countries such as Italy, Spain and the United States of America (USA), which are known to have good health care systems, have experienced huge numbers of cases and deaths. In particular, the USA and United Kingdom (UK) account for a large percentage of deaths worldwide (Worldometer, n.d.).
These countries’ death rates between March and April of 2020 ranged from 12.9% to 14.2%, which is considered high (CoronaTracker, n.d., Worldometer, n.d). These challenges make dealing with COVID-19 very difficult and could lead to huge burdens on the health care system.
The main difficult issues facing the health system in addressing COVID-19 include the fact that there was no available vaccine for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) until recently. However, there is still an issue with the supply chain, which will take longer to cover all countries. Furthermore, several medications were used in an off-label manner for COVID-19. There were hopes that hydroxychloroquine and chloroquine would be used to treat patients with COVID-19 following a study by Philippe Gautret and others (Gautret et al., 2020); however, several clinical trials found that these medications are ineffective for COVID-19 treatment (Abd-Elsalam et al., 2020, Axfors et al., 2020, Cavalcanti et al., 2020, Group, 2020, Mitjà et al., 2020).
Therefore, the first method of addressing COVID-19 is preventing the spread of the virus. SARS-CoV-2 is highly transmissible among humans, which might be one of the reasons for the rapid spread of the virus and its becoming a pandemic (Bernal-Delgado et al., 2018).
Several actions were taken at the source of the virus, the city of Wuhan in Hubei Province, China. These included isolation of any suspected or confirmed cases and their contacts, but the primary action taken was restriction of the mobility of the city’s residents (WHO, 2020a). These actions are believed to delay the spread of SARS-CoV-2 (Dong et al., 2020). Moreover, the best indicators that might prevent or delay the spread of SARS-CoV-2 were taken by some countries as precautions before any cases occurred (Alshammari et al., 2020).
Many countries took precautionary measures and actions aimed at reducing contact rates within the population and thereby reducing transmission of the virus. These actions included school and workplace closings, workforce reductions, public event cancelations, public transportation closures, public information campaigns, international travel restrictions and quarantines and curfews intended to limit the spread of the virus (Ferguson et al., 2020). It is thought that containment indicators for COVID-19 may only slow its spread and that the virus is now entering a stage of unprecedented threat in terms of its global impact (CEPI, n.d.). However, these indicators are likely to be implemented to varying degrees depending on the countries in question and their strategies (Imai et al., 2020). The major challenge is maintaining the precautions and interventions (Cauchemez et al., 2008). Therefore, this study is aimed at exploring the early precautionary activities and patterns of 175 countries from six continents worldwide intended to address and prevent the spread of COVID-19.
2. Methodology
2.1. Sample and data
An observational epidemiological study was conducted on the basis of data collected from all validated resources worldwide. The study included 175 countries from 6 continents worldwide (i.e., Asia, Africa, Europe, North America, Oceania and South America). In addition, it compared the numbers of infected cases in different countries with the current situation during January 2021 to yield knowledge on the importance of continuing with precautionary actions.
The study was conducted during the period from December 31, 2019 to the January 2021 All countries’ information was searched, selected manually by the research team and divided by continents. After collection, the data were double-checked by the research team (each member checked the other members).
The country list was obtained utilizing the data from the WHO official page on the novel SARS‑CoV‑2 (WHO, 2020b). For each selected country, specific data related to SARS‑CoV‑2 and its indicators were collected. This included information related to the date of the first reported case, total confirmed cases, total active or suspected cases, total serious cases, total recovered cases, total deaths and deaths per million people starting from the beginning of the virus’ spread to the end of March 2020. In addition to total confirmed cases and deaths per million people, data such as death rates and the numbers of confirmed, recovered and serious cases were also collected for April to compare the two months (April 2020 and January 2021).
2.2. Measures of variables
Validated indicators were used to assess the countries’ preparedness and precautionary actions. These indicators of government response included school closures (R1), workplace closures or workforce reductions (R2), public event cancelations (R3), public transport closures (R4), public information campaigns such as ones encouraging social distancing (R5), international travel restrictions (R6) and quarantines and curfews or movement reductions (R7) (Saez et al., 2020, Thomas et al., 2020).
Several sources were used to extract the countries’ data, including the University of Oxford, Worldometer COVID-19 data, KPMG International Cooperative, health ministries, UNESCO, the Government of the United Kingdom and each country’s U.S. embassy.
2.3. Data analysis
Descriptive statistics, including numbers and means, were used to compute government response indicators, infection cases, deaths, deaths per 1 million people and the percentage of increase in infections and deaths between March and April to obtain further insight into how countries’ actions affected the spread of COVID-19.
Data were exported to the Tableau software tool to support visual data analysis. The figures created present the total number of actions in countries grouped by continent, the total number of infections by continent, total deaths expressed as death rates in countries grouped by continent, the total infection increase rate between March and April by continent, a comparison of the number of indicators taken with the number of deaths by continent and the differences in infections in March and April by continent. For data analysis, we used IBM SPSS Statistics for Macintosh, Version 21.0.0.0, and Tableau Desktop, Version 2020.1.
3. Results
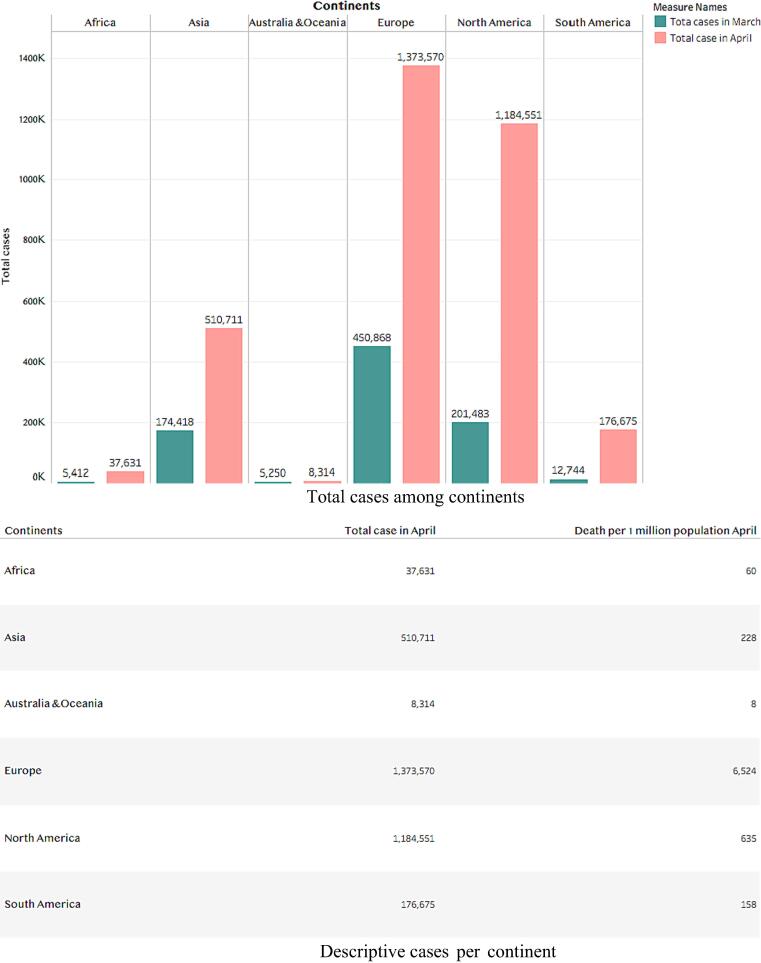
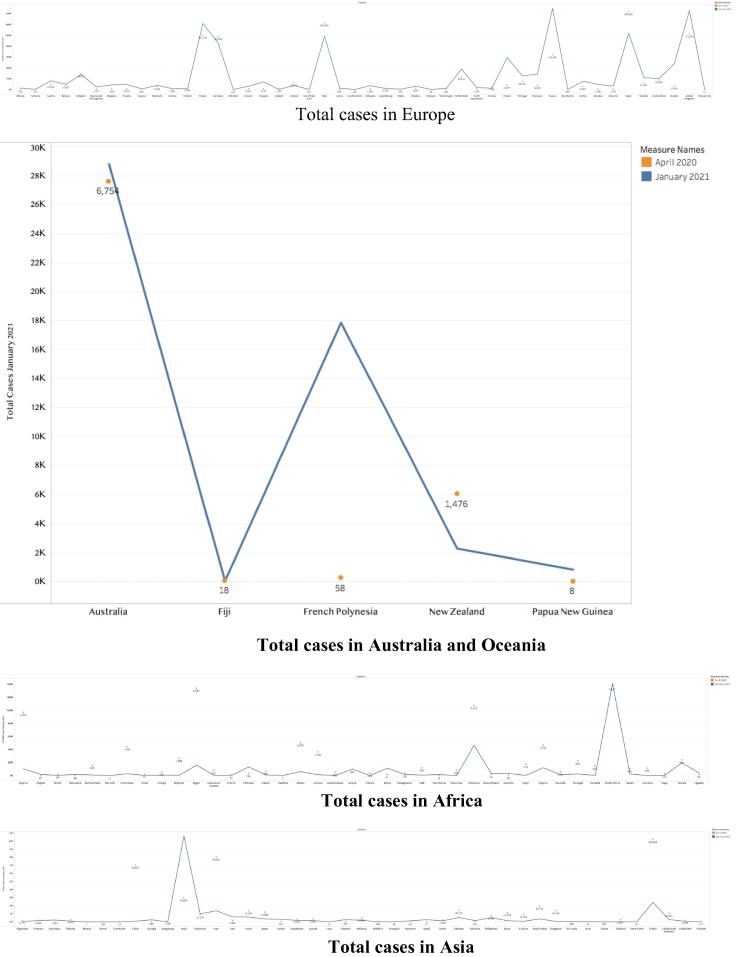
A total of 175 countries were included in the study. Of these, 42 were located in Africa, 43 were in Asia, 5 were in Oceania, 47 were in Europe, 26 were in North America and 12 were in South America. All included countries applied at least one of the precautionary indicators. Infection rates were highest in Europe, followed by in North America. Furthermore, Europe had the highest death rate at 6,524 deaths per million people, whereas Oceania had the lowest at 8 deaths per million people.
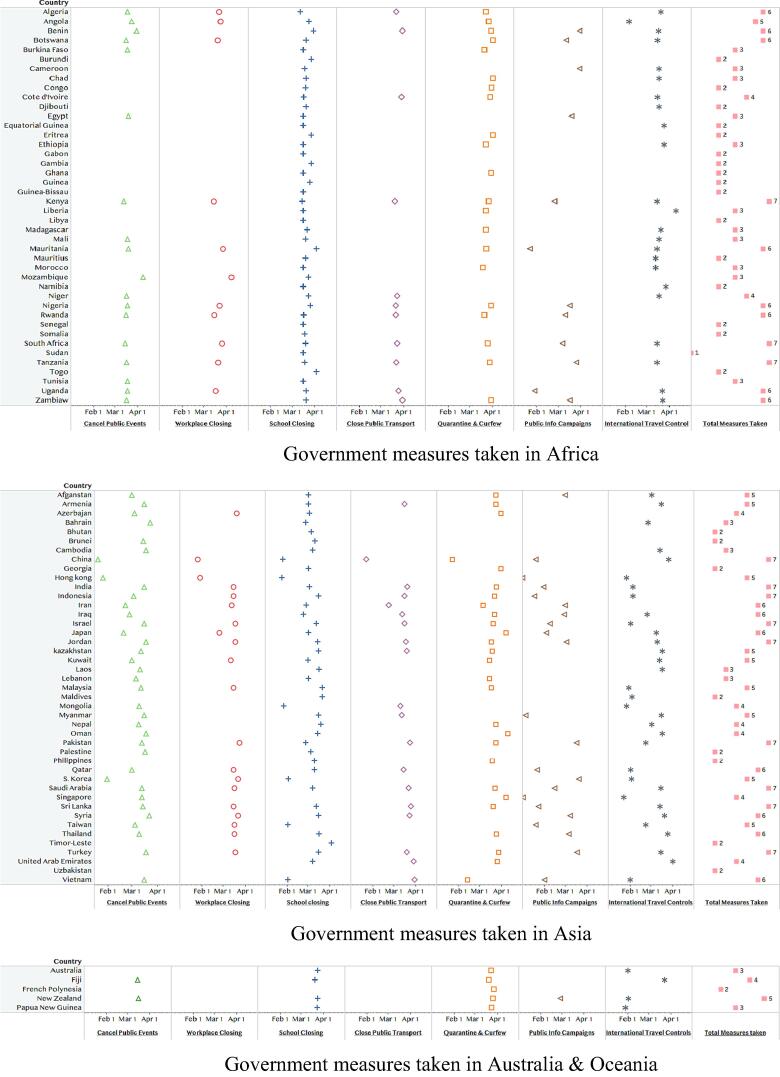
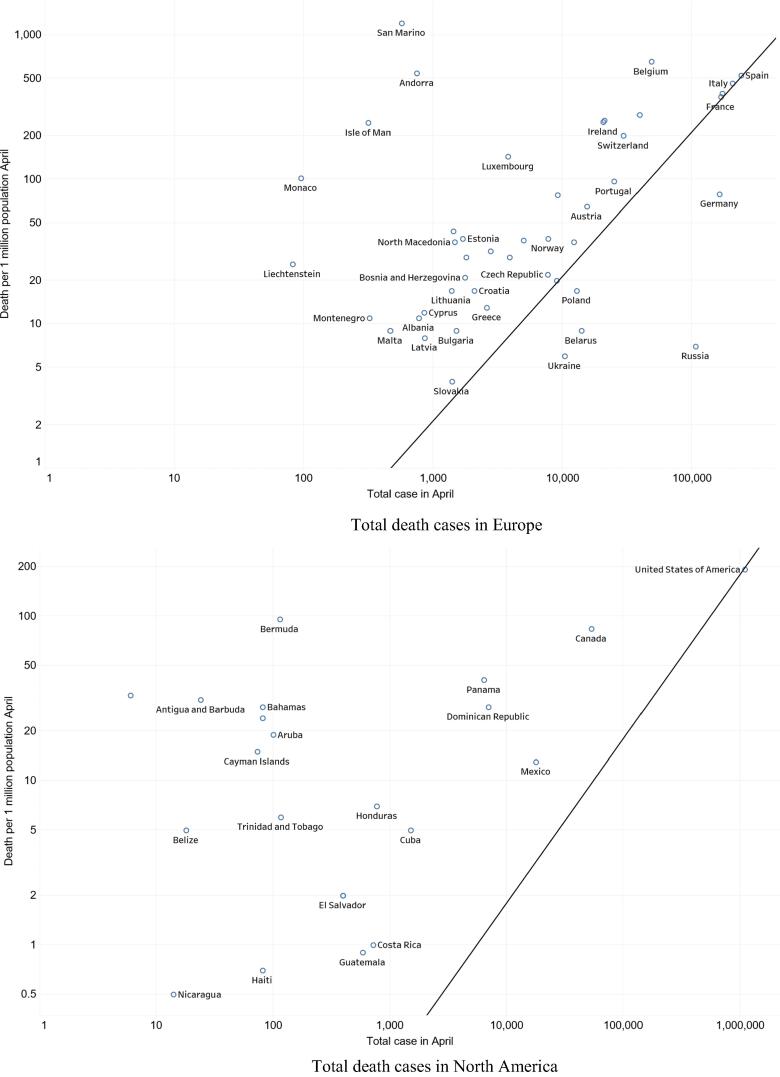
Worldwide, a maximum of 7 indicators were applied by governments. Figs. A present the total governmental indicators taken grouped by continent. Fig. A-1 presents the total governmental indicators taken in 42 countries in Africa. Among these, 16 countries applied only 2 standards, 11 applied 3 standards, 2 applied 4 standards, 1 applied 5 standards, 8 applied 6 standards and 3 applied 7 standards. One country (Somalia) applied only one standard. The countries that applied all 7 indicators were Kenya, South Arica and Tanzania. All 43 countries closed schools, and only 20 closed workplaces and canceled public events. In total, 19 countries closed public transportation and used public information campaigns, and 11 applied international travel restrictions as well as quarantines and curfews.
Fig. A.
Government measures (indicators) that were taken by 175 countries.
Fig. A-2 presents governmental indicators taken in Asia, where 43 countries applied precautionary indicators. Of these, 8 countries applied 2 indicators, 4 applied 3 indicators, 6 applied 4 indicators, 9 applied 5 indicators and 8 applied 6 indicators and eventually 7 indicators. Most countries closed schools, but only 23 closed workplaces. Furthermore, 36 countries canceled public events, and 19 closed their public transportation, 21 countries used public information campaigns, 33 imposed international travel restrictions and 27 applied quarantines and curfews.
Fig. A-3 shows the total governmental indicators taken in 5 countries in Oceania. Among these 5 countries, 1 applied 2 indicators, 2 applied 3 indicators, 1 applied 4 indicators and 1 applied 5 indicators. No countries applied 6 or 7 standards. Most countries closed schools, imposed international travel restrictions and established quarantines and curfews. Only New Zealand and Fiji canceled public events.
Fig. A-4 presents the total governmental indicators taken within 47 countries in Europe. Among these, 3 countries applied 1 indicator, 6 applied 2 indicators, 5 applied 3 indicators, 8 applied 4 indicators, 7 applied 5 indicators, 10 applied 6 indicators and 8 applied 7 indicators. Austria, Croatia, Hungary, Italy, Serbia, Spain, Switzerland and Ukraine applied all 7 indicators. Most countries closed schools and canceled public events, and almost half closed workplaces and used public information campaigns. Only 11 countries closed public transportation, whereas 36 imposed international travel restrictions and 30 established quarantines and curfews.
The governmental measures or indicators were a bit different in North America. Among 26 countries, 1 applied 1 indicator, 6 applied 2 indicators, 3 applied 3 indicators, 5 applied 4 indicators, 3 applied 5 indicators, 7 applied 6 indicators and 1 applied 7 indicators. Only Bermuda applied all the indicators. Most countries (24) closed schools, but only 13 closed workplaces and canceled public events. Only 5 countries closed public transportation, whereas 13 used public information campaigns; 18 countries imposed international travel restrictions and established quarantines and curfews. For further details, see (Fig. A-5).
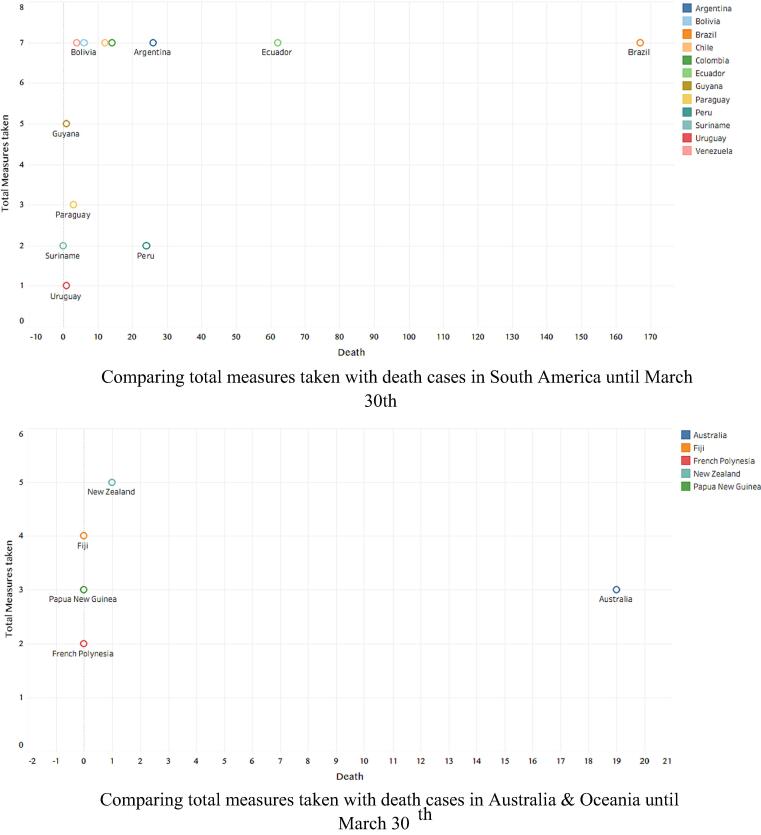
Fig. A-6 presents the total governmental indicators taken in 12 countries in South America. Among these, 1 country applied 1 indicator, 2 applied 2 indicators, 1 applied 3 indicators, 1 applied 5 indicators, 1 applied 6 indicators and 6 applied 7 indicators. Most countries (11) closed schools, and the majority (9) closed workplaces, imposed international travel restrictions and established quarantines and curfews. Seven countries closed public transportation and used public information campaigns, and 7 canceled public events.
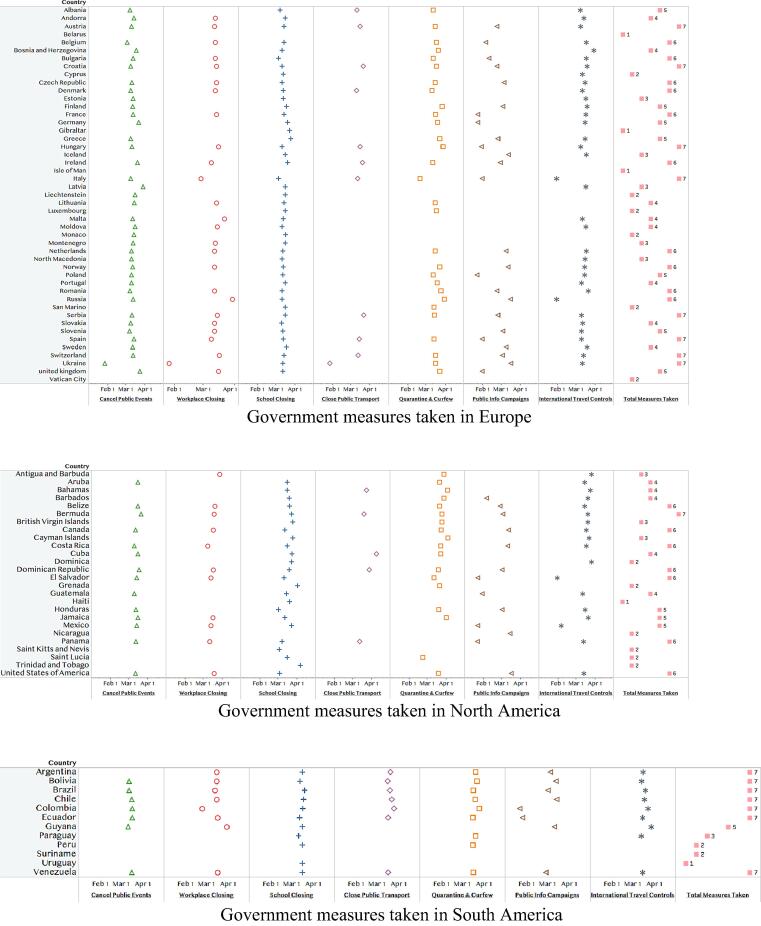
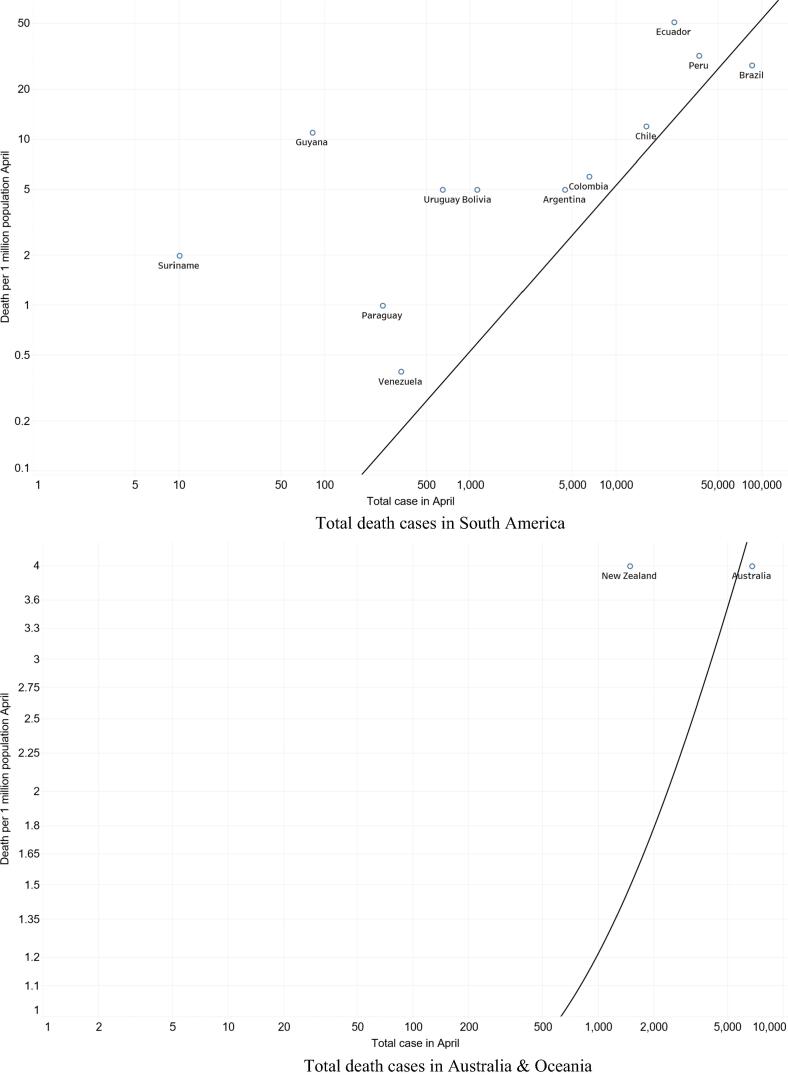
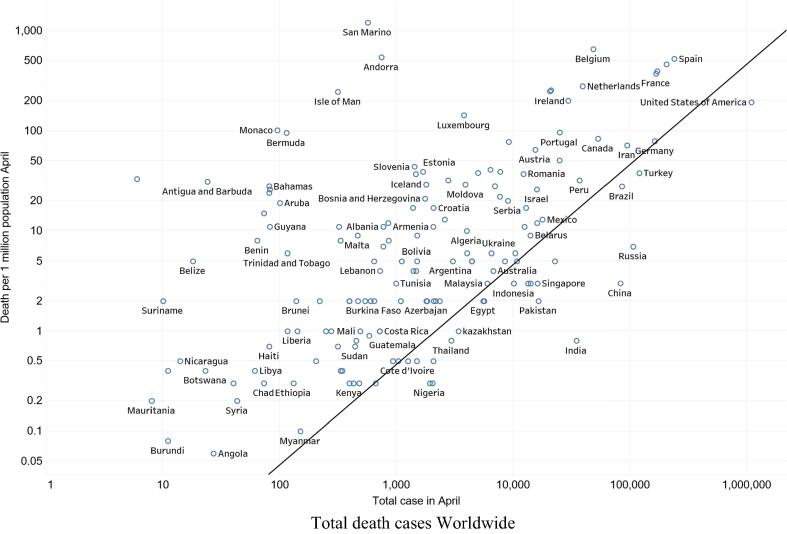
Another important factor was the total death rate in the studied countries. Figs. B show a plot chart of total deaths per million people versus total infections on 6 continents. Fig. B-1 shows a plot chart of total deaths per million people versus total infections in Africa during the period January 2020–April 2020. Algeria had the highest death rate at 10 deaths per million people and had 4,006 infections, followed by Benin, which had 8 deaths per million people and a total of 64 infections. Morocco had a death rate of 5 deaths per million people and a total of 4,423 infections.
Fig. B.
Number of total COVID-19 death cases in the 6 continents and worldwide.
In Asia, Iran had the highest death rate at 72 deaths per million people, with 94,640 infections. Turkey’s death rate was 38 deaths per million people, and the country had 120,000 infections, see (Fig. B-2).
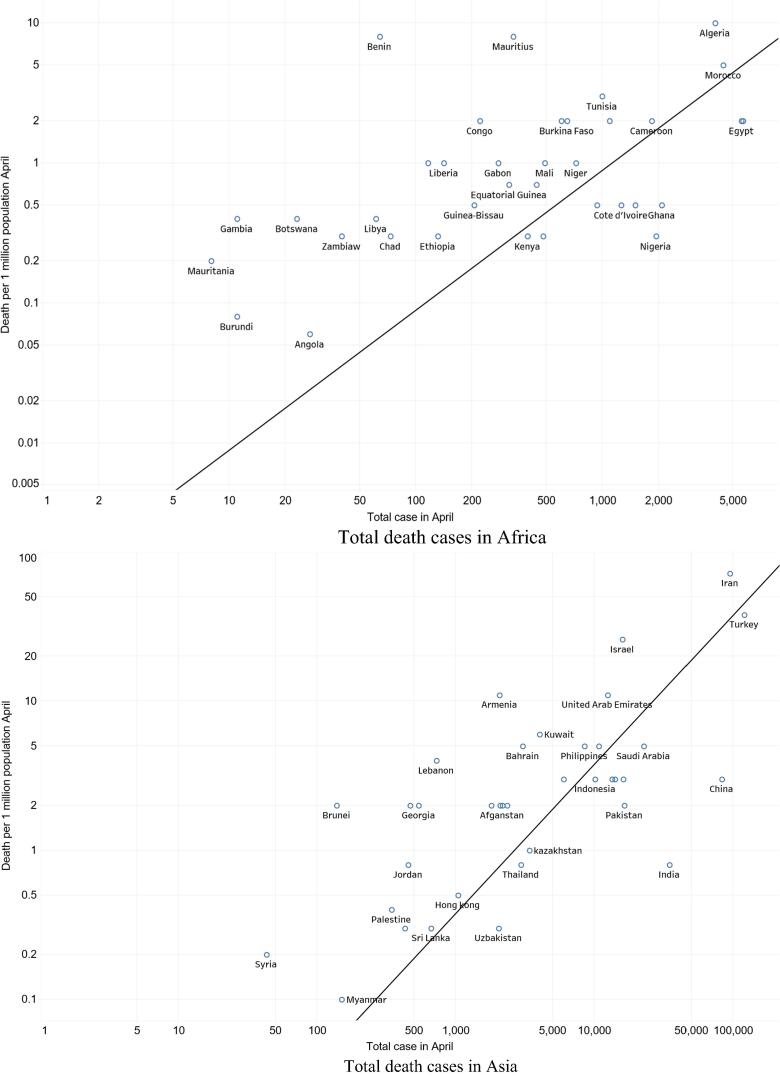
Fig. B-3 shows the death rate in Europe, where San Marino had the highest death rate at 1,208 deaths per million people as well as 569 infections. Belgium had a death rate of 655 deaths per million people, with 48,519 infections. Spain had the highest total infections and a death rate of 525 deaths per million people.
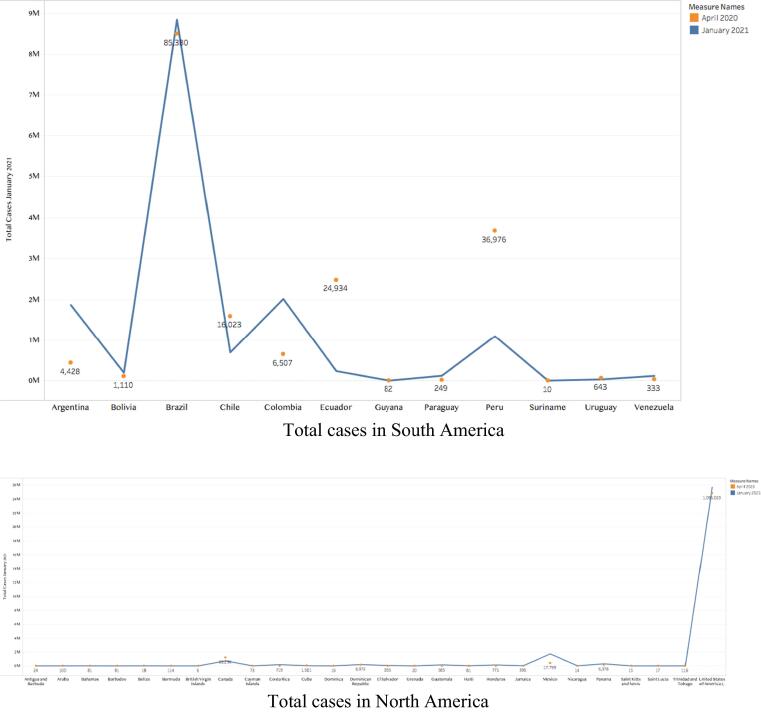
The USA had the highest death and infection rates in North America, with 193 deaths per million people and 1,095,023 infections. Bermuda was second with a death rate of 96 deaths per million people and 114 infections (Fig. B-4). In neighboring South America, death rates ranged from 0.4 to 51 deaths per million people. Ecuador’s death rate was the highest at 51 deaths per million people, and it had 24,934 infections. However, Brazil had the highest infection rate, with 85,380 cases and a death rate of 28 deaths per million people (Fig. B-5). In Oceania, Australia and New Zealand both had a death rate of 4 deaths per million people, with 6,754 cases in Australia and 1,476 cases in New Zealand. For further information, see (Fig. B-6).
As shown in Fig. B-7, worldwide, the death rate varied from 0.06 to 1,200 deaths per million people. Bhutan in Asia had the lowest death rate of 0 deaths per million people and had only 7 infections. In Europe, Vatican City had the lowest death rate at 0 deaths per million people, and it had only 11 infections.
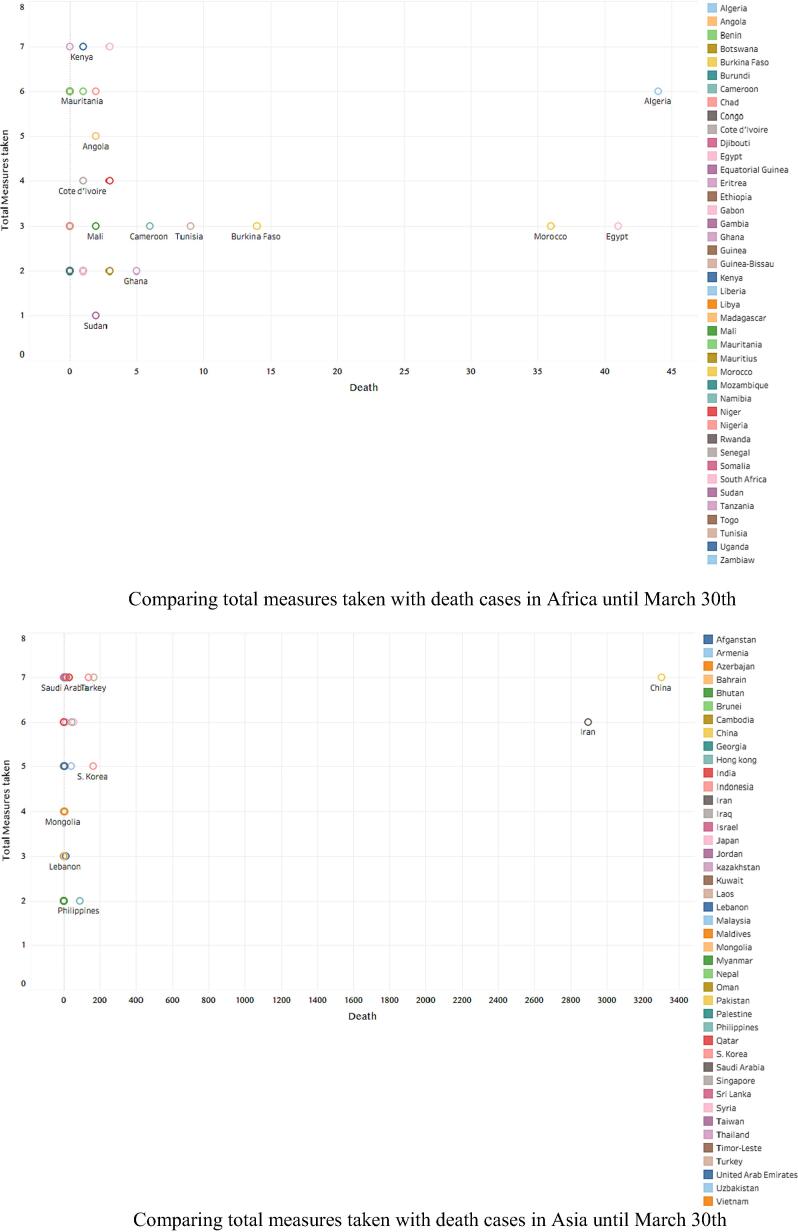
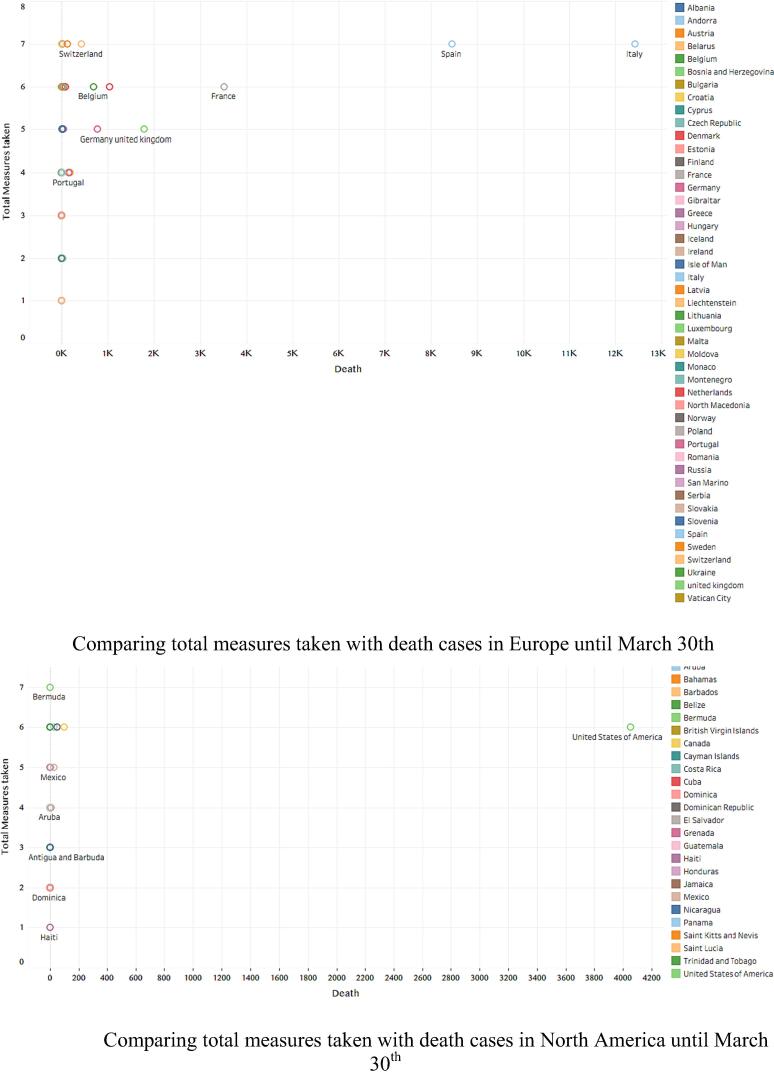
Figs. C compare countries and their total indicators taken using total infections between March and April 2020. In Africa, South Africa had the highest number of infections during March (1,353), followed by Algeria (716). These countries applied 7 and 6 indicators, respectively. However, by April, Egypt and Morocco had joined South Africa and Algeria due to a considerable increase in their numbers of infections. With 5,537 and 4,423 infections, respectively, and 3 indicators taken, both of the former countries had relatively similar numbers of infections compared to those of South Africa and Algeria (5,647 and 4,006, respectively). For further details, see (Fig. C-1).
Fig. C.
Comparison of number of death rate and total measures.
In Asia, China and Iran had the highest numbers of infections in March (81,518 and 44,605, respectively) and 7 and 6 indicators taken, respectively. However, by April, cases in Turkey (120,204), which applied 7 indicators, outnumbered those in China. For further details, see (Fig. C-2).
Fig. C-3 presents infections rates in Europe, where most counties showed an increase across both months. Spain and Italy adopted all 7 indicators but faced the highest infection rates. In North America, as Fig. C-4 shows, the USA, which applied 6 indicators, had the highest infection rate during March and April.
As Fig. C-5 shows, in South America, Brazil applied all 7 indicators and had the highest infection rate in March and April. However, Uruguay applied only 1 indicator and had the lowest number of infections on the continent.
In Australia and Oceania, as Fig. C-6 shows, a steady increase of infection cases occurred continent-wide. However, Australia had the highest infection rate and applied only 3 indicators.
In a comparison of the COVID-19 death rates among the continents, Europe and North America had the highest ones, whereas Oceania and Africa had the lowest ones (see Fig. D-2). In addition, the total COVID-19 infection rate increased exponentially and rapidly in North America and Europe from March to April (Fig. D-1).
Fig. D.
Total number of COVID-19 cases and death rate per million among the six continents.
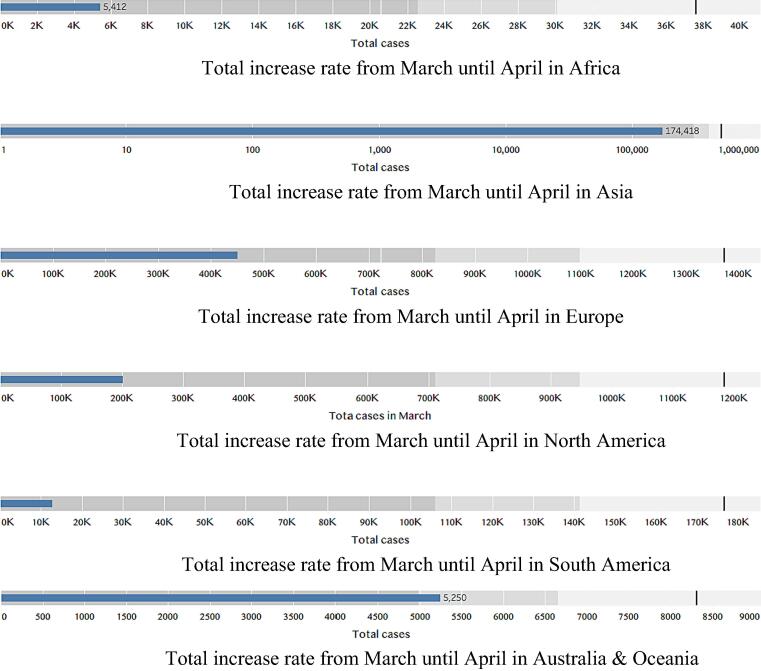
Figs. E present a stacked bar chart view that shows that the number of infections in Asia increased during the period March–April 2020. On March 30, the total number of infections in Asia was 175,130. By the end of April, this number had reached 510,711 reported cases (Fig. E-2). However, Africa’s rate of increase was greater than Asia’s. In total, 5,412 cases occurred in Africa, but the total number of infections had risen to 37,631 by the end of April 2020 (Fig. E-1). Countries in Oceania were not affected in both months, and their rate of increase was low, as the total number of cases was 5,250 at end of March and 8,314 at the end of April (Fig. E-6).
Fig. E.
Increase rate of COVID-19 cases from March to April 2020 among the six continents.
Between March and April 2020, the number of cases in Europe and North America increased by 6 and 3 times, respectively (Figs. E-3 and E-4). On March 30, the total number of infections in North America was 201,483, but by the end of April 2020, it had reached 1,184,551. Europe had 450,868 cases on March 30 and 1,373,570 cases by the end of April.
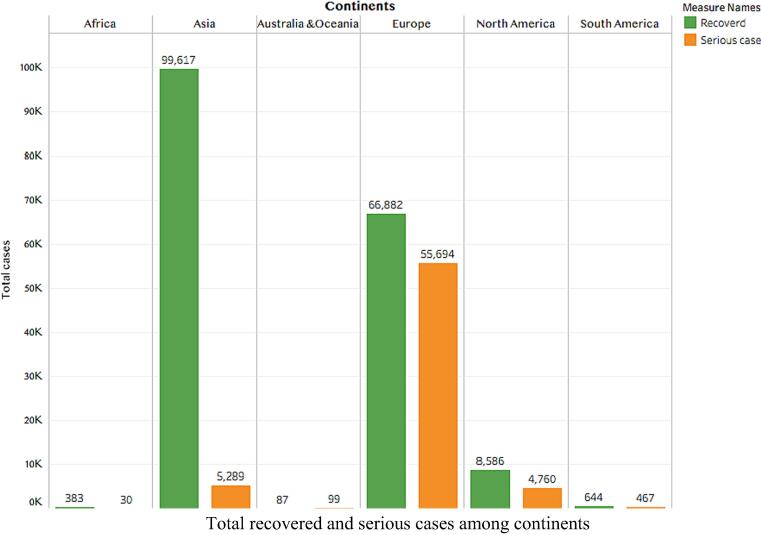
The highest rate of infection increase was observed in South America, where it increased by 13 times. The total number of infections was 12,744 at end of March, but this increased to 176,675 by the end of April 2020 (Fig. D-1). The recovered cases pattern was similar for all continents except Europe, as the number of serious cases was 55,694 there but far lower elsewhere (Fig. F).
Fig. F.
Total number of COVID-19 active, serious and recovered cases among the six continents.
In January 2021, the number of cases in Europe had slightly increased compared to in the April 2020 situation, except in some countries such as Russia, the United Kingdom and Ukraine (Fig. G-1). The Australian & Oceanian continent increases were also limited except for in French Polynesia, where there was a noticeable increase (Fig. G-2).
Fig. G.
Total number of COVID-19 cases among the six continents.
The infected cases in Africa reported in January 2021 were comparable to the number of cases registered last April (Fig. G-3).
There were no great increases in the rate of infection in Asia compared to the rate during the last April, except in India, where the number of cases increased by three times (Fig. G-4). We also noticed as much in the continent of South America, except in Brazil, where there was an increase in the number of infected cases (Fig. G-5).
In North America is January 2021, the infected cases were close to what were recorded the April before, except in the United States (Fig. G-6).
4. Discussion
On December 31, 2019, Chinese authorities alerted the WHO to an outbreak of SARS‑CoV‑2 in Wuhan City, Hubei Province, China. On March 11, 2020, the WHO announced that COVID-19 had become a pandemic. The rapid spread of COVID-19 worldwide has led to the creation and adoption of a wide range of responses in various countries to address outbreaks of the virus and reduce severe global socioeconomic disruption.
Recommended preventive indicators included hand washing, covering one’s mouth, maintaining distance between people and self-isolation for those who suspect they are infected. However, the governments differed widely in which measures they adopted and how quickly they implemented changes such as school or workplace closures, workforce reductions, public event cancelations, public transportation closures, public information campaigns, international travel restrictions (on travel to or from China or all travel) and curfews, resulting in the uneven spread of the virus.
In general, government responses have become more stringent over the course of the COVID-19 outbreak. However, responses have also varied among countries and this is consistent with an Working Paper Series conducted by University of Oxford. (Hale et al., 2020) This difference may owe to fear of economic repercussions, weak or strong resources and wars. Nevertheless, the countries with higher healthcare investments as a percentage of Gross Domestic Product (GDP) has mitigated the fatality rate of COVID-19 even when applied a shorter period of lockdown. (Coccia, 2021a, Karnon, 2020).
This study examined the actions taken by 175 countries on 6 continents. We aimed to cover most regions worldwide and investigate the patterns among these countries. Thus, there were no specific exclusion criteria for countries, but inclusion depended on the availability of and access to data. Although COVID-19 originated from China, the highest death rate was in Europe, not Asia (Yuan et al., 2020). This may have occurred for many reasons. The number of COVID-19 cases was high during the study period, and Europe’s elderly population is quite large; furthermore, most COVID-19 deaths occurred among elderly people due to weak immune systems (Rothan and Byrareddy, 2020, Wang et al., 2020) or due to environmental and social weaknesses. (Coccia, 2020) In addition, a lack of some important medical equipment—such as test kits, personal protective equipment, ventilators and available beds in intensive care units—in some countries, especially those with very high numbers of COVID-19 cases, might be another reason for the high death rate in Europe (Rubino et al., 2020). In contrast, Oceania had the lowest rate at 8 deaths per million people. This might be due to the distance between the continent’s islands, its low population and the early precautionary actions on the part of some of countries in Oceania, which limited the number of COVID-19 cases in those countries. New Zealand is a successful example of controlling the COVID-19 pandemic. The number of tests conducted indicates that testing was performed more than once (“COVID-19 – current cases in New Zealand, Ministry of Health – Manatū Hauora,” n.d.), and seven indicators were used to assess the country’s activities and preparedness to fight SARS-CoV-2. Only 15% of countries applied all 7 indicators, whereas the largest proportion applied only 2 indicators (22%). However, this pattern is different for Africa, South America and Oceania. Fewer indicators were applied by a couple of countries in Oceania. Thus, that continent had both the lowest rate of COVID-19 pandemic infection and the lowest average number of indicators. governmental indicators. This does not indicate that these indicators had no effect, however. These results could have occurred for several reasons: 1) applying some indicators such as quarantines and school closures early, 2) closing the country by preventing international travel to and from some countries and 3) Oceania’s location, which, unlike Europe’s, makes travel between countries difficult because of their sea borders (“COVID-19 – current cases in New Zealand, Ministry of Health – Manatū Hauora,” n.d.). These reasons could also be why the spread of SARS-CoV-2 was lowest in Oceania. When comparing cases at the end of March to those at the end of April, we found that the rate increase in Oceania was only 36%, compared to 74% worldwide. Similarly, the death rate increased by about the same percentage.
However, cases differed across other continents, where SARS-CoV-2 spread more when governments applied fewer indicators. This is clearly shown in data for continents such as South America, Africa and North America, where the rate of spread was higher than the worldwide rate. Asia and Europe were comparable, and the rate of spread on both continents was lower than the worldwide rate, possibly due to their extensive efforts in applying most indicators to limit the spread of SARS-CoV-2.
The spread of SARS CoV-2 among the studied countries might have been affected by the applied indicators; this was seen in various countries. In Oceania, the more indicators governments applied, the fewer COVID-19 cases they reported. For example, in New Zealand and Fiji, this trend continued for both months (i.e., March and April). Several other continents’ countries, such as Kenya, Saudi Arabia, Japan, Austria, Switzerland, Bermuda, Canada, Bolivia and Argentina, exhibited the same pattern. However, this was not always the case because some countries applied more indicators but still faced high numbers of infections, as in China, South Africa, Spain, Italy and the USA. This might have occurred because these indicators were not followed well, were applied late after many cases had already occurred or were not well recognized as being of considerable importance, especially during the early period of the pandemic, as in China (Aleta and Moreno, 2020, Sebastiani et al., 2020). This is consistent with a simulation study conducted in Wuhan, which found that if precautionary actions (social distancing in the general community and school and workplace closures) would be applied well, the pandemic would vanish by end of April; however, the countries are still suffering from it (Prem et al., 2020). A study by Atalan conducted on 49 countries found that lockdowns have reduced the number of COVID-19 infections, but cases in Italy and Spain were not affected by lockdowns, which consists with our study (Atalan, 2020).
In a comparison of the indicators or actions used by continents with the mortality rate at the end of the first month, in Africa, most countries that applied more indicators, such as Kenya, Mauritania, Angola and Cote d’Ivoire, had lower mortality rates. However, results were different in Algeria, which had a high mortality rate despite applying 6 of the 7 indicators. The only indicator Algeria did not apply was a public information campaign, which might indicate that educational materials and information about SARS-CoV-2 played a major role in counteracting this pandemic. Similarly, in Europe, Switzerland and Germany had low fatality rates, and both countries applied a high number of these indicators (Huber and Langen, 2020). However, countries such Spain and Italy applied high numbers of indicators but still had high mortality rates. This might be due to late application or lack of seriousness in applying these indicators by these countries (Liu et al., 2020, Saez et al., 2020). However, a longer period of lockdown does not significantly reduce the fatality rate. (Coccia, 2021a). In addition, as mentioned earlier, demographics and aging might have played roles in these countries (Rubino et al., 2020). These results are consistent with a study conducted by Coccia M et al., which found that a longer lockdown (>1 month) compared to a shorter one (maximum 15 days) is not associated with a reduction in COVID-19 cases (Coccia, 2021b). Furthermore, a study conducted in Italy found that these increases in cases might have owed to the air pollution and high population density in the affected cities (Coccia, 2021c, Coccia, 2021d). Nevertheless, a study by Tobias A conducted in Italy and Spain for a month found that there was a reduction in the number of cases after the lockdowns; however, the study was started in February where cases were already very high (Tobias A., 2020***). Moreover, another study that assessed the effect of non-pharmaceutical interventions on COVID-19 in Europe found that there was a reduction in the transmission of COVID-19, but the study lasted until May, at which point cases had started to decline (Flaxman et al., 2020). Brauner J. et al. conducted a study on 41 European countries and found that nonessential and high-risk business closures as well as stay-at-home orders had only a small to moderate effect on COVID-19 transmission, whereas closing educational institutions, limiting gatherings to 10 people or fewer and curtailing face-to-face businesses had a considerable effect on COVID-19 transmission (Brauner et al., 2021).
When the mortality rate was compared among countries worldwide, most countries with higher fatality rates were in Europe. The country with the highest rate was San Marino, followed by Belgium, Andorra, Spain, Italy, the UK, France and Sweden. This might be because of the massive number of COVID-19 cases that occurred earlier in Europe, as hospitals might not have been ready to deal with such a high number of cases (Rubino et al., 2020). Another explanation could be the aging population in these countries, especially considering that such individuals are part of the most-affected age group (Toshkov, Dimiter, 2020).
There were more serious COVID-19 cases in Europe than in comparable continents. This sharp increase in cases occurred mainly in Italy and Spain, possibly due to the unpreparedness of these countries’ health care systems, especially when faced with a huge number of cases. Also, the late action by these countries in applying restrictions might be a reason, taking into consideration the high number of cases before March. In addition, these countries’ populations contain more elderly people, and most of the people affected have been elderly; this could be another justification for such a high number of serious cases (Rubino et al., 2020, Toshkov et al., 2020). A study conducted in Italy and Spain found that when the lockdown was applied, the number of cases dropped in March and April compared to in February. This might be because cases were already very high in February (Tobías, 2020). Nevertheless, another study conducted in 50 countries found that rapid border closures and full lockdowns are not associated with reduction critical cases or mortality reduction (Chaudhry et al., 2020).
When total SARS-CoV-2 infection rates among continents for the months of March and April are compared, most countries continued to increase at the same rate for both months regardless of the number of governmental indicators taken. However, in Asia and Europe, Turkey and Spain had percentage increases higher than the average infection rate, overtaking China and Italy, which were considered the most-infected countries in Asia and Europe.
Several actions were taken at the source of the virus in Wuhan City, Hubei Province, China, including improved rates of diagnostic testing, immediate isolation of any suspected or confirmed cases and contacts and restriction of the mobility of the city’s residents (Kraemer et al., 2020). These actions are believed to have delayed the spread of SARS-CoV2 (Tian et al., 2020). This is consistent with a study by Perm et al. (2020).
Some countries such as Singapore, Hong Kong and Taiwan relied more on early precautions because of their belief that prevention was the only option without an available vaccine or drugs at that time. Singapore was among the first countries to apply a travel ban from China at that time. In addition, daily testing of up to 2,000 people was conducted to check for SARS-CoV-2, and employees were asked to work from home due to mandatory quarantines in the country. Similar actions were taken by Hong Kong, and most people believed in these actions because the country had been affected by SARS-CoV during the 2003–2004 pandemic (“What We Can Learn From Singapore, Taiwan and Hong Kong About Handling Coronavirus. Time. 2020,” n.d.).
Some indicators were reduced in countries in late April for a number of reasons. The outbreak of the pandemic affected educational systems worldwide, leading to the near-total closures of schools and universities and causing a destabilizing threat to the global economy. In addition, the increased global use of equipment to combat virus outbreaks caused food and supply shortages. The SARS-CoV-2 outbreak has had various impacts worldwide, especially in terms of disrupting factories and logistics operations (Fernandes, 2020).
The second wave of COVID-19 has shown the important of these precautionary actions as of Jan 25, 2021. The USA is now the country most affected by COVID-19 cases, surpassing 25 million total cases. As an example, the state of California had used these actions to limit the spread of COVID-19 (California governor REF).
The increase in the number of cases might owe to the reopening of schools and universities, especially in September, and variation in the application of the school closures procedure in different states.
This might be due to easing into and implementing procedures, especially wearing masks, returning to work completely in most states and partial restriction of flights.
Since the beginning of July, India has eased lockdown actions despite increased confirmed cases and deaths. At the end of January 2021, it had reached nearly 11 million cases with 111 deaths per million people. Furthermore, that Brazil has shown one of the worst responses to the pandemic is unequivocal. Brazil is among the three countries with the largest number of confirmed cases (more than 9 million as of Jan 25, 2021, according to the WHO), with high mortality and a high number of deaths, especially among health professionals and pregnant women (Moraes T, 2020, Takemoto et al., 2020).
At the end of December 2020, several European countries, including France, Germany, Italy, the Netherlands and Ireland, imposed travel restrictions on the United Kingdom over the new coronavirus variant identified there. Other countries such as Canada, Saudi Arabia and El Salvador also imposed travel restrictions.
In some continents—Asia and Africa—we found no increase in the infected cases. The reason may be the lack of reporting by the countries or of testing due to a state’s economic situation or the unavailability of a COVID-19 test; thus, the number of cases might have been decreased.
This study has several advantages. To our knowledge, it is the first study to evaluate these 7 indicators as precautionary actions on the part of 175 countries worldwide. In addition, our study involved important indicators that cover the most of the actions taken by countries. It also included data such as the numbers of infections, serious cases, recovered cases and deaths, the death rate per million people and the number of indicators applied by each country. The study’s limitations include that we lacked time series information (i.e., the number of infections or deaths for multiple time points) because some data were unavailable or difficult to acquire. In addition, it is difficult to judge and compare the countries because of the unavailability of several factors needed for this comparison and the emergence of the new coronavirus variant in some countries.
4.1. Recommendations
It is clear that the COVID-19 pandemic will continue over time for at least a year from now, and there is a hope that the availability of vaccines will help to end it; however, there is no solid evidence on that point. Therefore, precautionary actions might be considered the best methods to prevent the transmission of COVID-19, although the issue is still debatable. Educational (i.e., schools) and workplace closures (using online methods instead), border closure, social distancing and hand and face washing seem to be actions that can be recommended. Nevertheless, these recommendations might differ from one country to another.
5. Conclusion
Most studied countries exhibited the same pattern in terms of increasing numbers of COVID-19 cases. This study showed that the precautionary indicators taken by various countries might have played a role in limiting the spread of COVID-19. This might be seen clearly at the point when some countries stopped these precautionary actions, as they now have a second wave of COVID-19. However, some countries might not benefit from applying these indicators.
CRediT authorship contribution statement
TMA started the research idea. AFA, KAA and TMA have written the paper; TMA and AFA have supervised the research; FAA and GF have analyzed and interpreted the data; KAA, GF and FAA worked on data collection and prepared the manuscript. Each author listed on the manuscript has seen and approved the submission of the present version of the manuscript and takes full responsibility for the manuscript.
Footnotes
Peer review under responsibility of King Saud University.
References
- Abd-Elsalam S., Esmail E.S., Khalaf M., Abdo E.F., Medhat M.A., Abd El Ghafar M.S., Ahmed O.A., Soliman S., Serangawy G.N., Alboraie M. Hydroxychloroquine in the Treatment of COVID-19: A Multicenter Randomized Controlled Study. Am. J. Trop. Med. Hyg. 2020;103:1635–1639. doi: 10.4269/ajtmh.20-0873. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Aleta A., Moreno Y. Evaluation of the potential incidence of COVID-19 and effectiveness of containment measures in Spain: a data-driven approach. BMC Med. 2020;18:157. doi: 10.1186/s12916-020-01619-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshammari T.M., Altebainawi A.F., Alenzi K.A. Importance of early precautionary actions in avoiding the spread of COVID-19: Saudi Arabia as an Example. Saudi Pharm. J. 2020;28(7):898–902. doi: 10.1016/j.jsps.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atalan A. Is the lockdown important to prevent the COVID-19 pandemic? Effects on psychology, environment and economy-perspective. Ann. Med. Surg. 2020;56:38–42. doi: 10.1016/j.amsu.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axfors, C., Schmitt, A.M., Janiaud, P., van ’t Hooft, J., Abd-Elsalam, S., Abdo, E.F., Abella, B.S., Akram, J., Amaravadi, R.K., Angus, D.C., Arabi, Y.M., Azhar, S., Baden, L.R., Baker, A.W., Belkhir, L., Benfield, T., Berrevoets, M.A.H., Chen, C.-P., Chen, T.-C., Cheng, S.-H., Cheng, C.-Y., Chung, W.-S., Cohen, Y.Z., Cowan, L.N., Dalgard, O., de Almeida e Val, F.F., de Lacerda, M.V.G., de Melo, G.C., Derde, L., Dubee, V., Elfakir, A., Gordon, A.C., Hernandez-Cardenas, C.M., Hills, T., Hoepelman, A.I.M., Huang, Y.-W., Igau, B., Jin, R., Jurado-Camacho, F., Khan, K.S., Kremsner, P.G., Kreuels, B., Kuo, C.-Y., Le, T., Lin, Y.-C., Lin, W.-P., Lin, T.-H., Lyngbakken, M.N., McArthur, C., McVerry, B.J., Meza-Meneses, P., Monteiro, W.M., Morpeth, S.C., Mourad, A., Mulligan, M.J., Murthy, S., Naggie, S., Narayanasamy, S., Nichol, A., Novack, L.A., O’Brien, S.M., Okeke, N.L., Perez, L., Perez-Padilla, R., Perrin, L., Remigio-Luna, A., Rivera-Martinez, N.E., Rockhold, F.W., Rodriguez-Llamazares, S., Rolfe, R., Rosa, R., Røsjø, H., Sampaio, V.S., Seto, T.B., Shehzad, M., Soliman, S., Stout, J.E., Thirion-Romero, I., Troxel, A.B., Tseng, T.-Y., Turner, N.A., Ulrich, R.J., Walsh, S.R., Webb, S.A., Weehuizen, J.M., Velinova, M., Wong, H.-L., Wrenn, R., Zampieri, F.G., Zhong, W., Moher, D., Goodman, S.N., Ioannidis, J.P.A., Hemkens, L.G., 2020. Mortality outcomes with hydroxychloroquine and chloroquine in COVID-19: an international collaborative meta-analysis of randomized trials. medRxiv 2020.09.16.20194571. https://doi.org/10.1101/2020.09.16.20194571.
- Bernal-Delgado E., Garcia-Armesto S., Oliva J., Sanchez Martinez F.I., Repullo J.R., Pena-Longobardo L.M., Ridao-Lopez M., Hernandez-Quevedo C. Spain: Health System Review. Health Syst. Transit. 2018;20:1–179. [PubMed] [Google Scholar]
- Brauner J.M., Mindermann S., Sharma M., Johnston D., Salvatier J., Gavenčiak T., Stephenson A.B., Leech G., Altman G., Mikulik V., Norman A.J., Monrad J.T., Besiroglu T., Ge H., Hartwick M.A., Teh Y.W., Chindelevitch L., Gal Y., Kulveit J. Inferring the effectiveness of government interventions against COVID-19. Science. 2021;371(6531):eabd9338. doi: 10.1126/science:abd9338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascella, M., Rajnik, M., Cuomo, A., Dulebohn, S.C., Di Napoli, R., 2020. Features, Evaluation and Treatment Coronavirus (COVID-19). Treasure Island (FL). [PubMed]
- Cauchemez S., Valleron A.-J., Boëlle P.-Y., Flahault A., Ferguson N.M. Estimating the impact of school closure on influenza transmission from Sentinel data. Nature. 2008;452(7188):750–754. doi: 10.1038/nature06732. [DOI] [PubMed] [Google Scholar]
- Cavalcanti A.B., Zampieri F.G., Rosa R.G., Azevedo L.C.P., Veiga V.C., Avezum A., Damiani L.P., Marcadenti A., Kawano-Dourado L., Lisboa T., Junqueira D.L.M., de Barros e Silva P.G.M., Tramujas L., Abreu-Silva E.O., Laranjeira L.N., Soares A.T., Echenique L.S., Pereira A.J., Freitas F.G.R., Gebara O.C.E., Dantas V.C.S., Furtado R.H.M., Milan E.P., Golin N.A., Cardoso F.F., Maia I.S., Hoffmann Filho C.R., Kormann A.P.M., Amazonas R.B., Bocchi de Oliveira M.F., Serpa-Neto A., Falavigna M., Lopes R.D., Machado F.R., Berwanger O. Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19. N. Engl. J. Med. 2020;383(21):2041–2052. doi: 10.1056/NEJMoa2019014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CEPI, n.d. CEPI welcomes UK Government’s funding and highlights need for $2 billion to develop a vaccine against COVID-19 [WWW Document]. URL https://cepi.net/news_cepi/2-billion-required-to-develop-a-vaccine-against-the-covid-19-virus/ (accessed 6.15.20).
- Chaudhry R., Dranitsaris G., Mubashir T., Bartoszko J., Riazi S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. EClinicalMedicine. 2020;25:100464. doi: 10.1016/j.eclinm.2020.100464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. The relation between length of lockdown, numbers of infected people and deaths of Covid-19, and economic growth of countries: Lessons learned to cope with future pandemics similar to Covid-19 and to constrain the deterioration of economic system. Sci. Total Environ. 2021;775 doi: 10.1016/j.scitotenv.2021.145801. [DOI] [Google Scholar]
- Coccia, M., 2021b. National Lockdown to Cope with COVID-19 Pandemic: Effects (Contradictory) on Public Health and (Negative) on Economic System. Res. Sq. https://doi.org/10.21203/rs.3.rs-115665/v1
- Coccia M. Effects of the spread of COVID-19 on public health of polluted cities: results of the first wave for explaining the dejà vu in the second wave of COVID-19 pandemic and epidemics of future vital agents. Environ. Sci. Pollut. Res. 2021 doi: 10.1007/s11356-020-11662-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. How do low wind speeds and high levels of air pollution support the spread of COVID-19? Atmos. Pollut. Res. 2021;12:437–445. doi: 10.1016/j.apr.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. An index to quantify environmental risk of exposure to future epidemics of the COVID-19 and similar viral agents: Theory and practice. Environ. Res. 2020;191:110155. doi: 10.1016/j.envres.2020.11015510.37473/dac/10.1016/j.envres.2020.110155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CoronaTracker [WWW Document], n.d. URL https://www.coronatracker.com/country/united-kingdom/ (accessed 6.16.20).
- COVID-19 - current cases in New Zealand, Ministry of Health – Manatū Hauora [WWW Document], n.d. URL https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-current-situation/covid-19-current-cases (accessed 6.14.20).
- Dong L., Hu S., Gao J. Discovering drugs to treat coronavirus disease 2019 (COVID-19) Drug Discov. Ther. 2020;14(1):58–60. doi: 10.5582/ddt.2020.01012. [DOI] [PubMed] [Google Scholar]
- Ferguson, N., Laydon, D., Nedjati Gilani, G., Imai, N., Ainslie, K., Baguelin, M., Bhatia, S., Boonyasiri, A., Cucunuba Perez, Z., Cuomo-Dannenburg, G., 2020. Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand.
- Fernandes, N., 2020. Economic effects of coronavirus outbreak (COVID-19) on the world economy. Available SSRN 3557504.
- Flaxman S., Mishra S., Gandy A., Unwin H.J.T., Mellan T.A., Coupland H., Whittaker C., Zhu H., Berah T., Eaton J.W., Monod M., Ghani A.C., Donnelly C.A., Riley S., Vollmer M.A.C., Ferguson N.M., Okell L.C., Bhatt S. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- Gautret P., Lagier J.-C., Parola P., Hoang V.T., Meddeb L., Mailhe M., Doudier B., Courjon J., Giordanengo V., Vieira V.E., Tissot Dupont H., Honoré S., Colson P., Chabrière E., La Scola B., Rolain J.-M., Brouqui P., Raoult D. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents. 2020;56 doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group R.C. Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2020;383:2030–2040. doi: 10.1056/NEJMoa2022926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale, T., Angrist, N., Boby, T., Cameron-Blake, E., Hallas, L., Kira, B., Majumdar, S., Petherick, A., Phillips, T., Tatlow, H., Webster, S., 2020. Variation in Government Responses to COVID-19 [WWW Document]. Blavatnik Sch. Gov. URL https://www.bsg.ox.ac.uk/research/publications/variation-government-responses-covid-19 (accessed 3.10.21).
- Huber, M., Langen, H., 2020. The Impact of Response Measures on COVID-19-Related Hospitalization and Death Rates in Germany and Switzerland. arXiv Prepr. arXiv2005.11278. [DOI] [PMC free article] [PubMed]
- Imai N., Gaythorpe K.A.M., Abbott S., Bhatia S., van Elsland S., Prem K., Liu Y., Ferguson N.M. Adoption and impact of non-pharmaceutical interventions for COVID-19. Wellcome Open Res. 2020;5 doi: 10.12688/wellcomeopenres.15808.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karnon J. A Simple Decision Analysis of a Mandatory Lockdown Response to the COVID-19 Pandemic. Appl. Health Econ. Health Policy. 2020;18(3):329–331. doi: 10.1007/s40258-020-00581-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer M.U.G., Yang C.-H., Gutierrez B., Wu C.-H., Klein B., Pigott D.M., du Plessis L., Faria N.R., Li R., Hanage W.P., Brownstein J.S., Layan M., Vespignani A., Tian H., Dye C., Pybus O.G., Scarpino S.V. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science:abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitjà O., Corbacho-Monné M., Ubals M., Tebe C., Peñafiel J., Tobias A., Ballana E., Alemany A., Riera-Martí N., Pérez C.A., Suñer C., Laporte P., Admella P., Mitjà J., Clua M., Bertran L., Sarquella M., Gavilán S., Ara J., Argimon J.M., Casabona J., Cuatrecasas G., Cañadas P., Elizalde-Torrent A., Fabregat R., Farré M., Forcada A., Flores-Mateo G., Muntada E., Nadal N., Narejos S., Gil-Ortega A.N., Prat N., Puig J., Quiñones C., Reyes-Ureña J., Ramírez-Viaplana F., Ruiz L., Riveira-Muñoz E., Sierra A., Velasco C., Vivanco-Hidalgo R.M., Sentís A., G-Beiras C., Clotet B., Vall-Mayans M. Hydroxychloroquine for Early Treatment of Adults with Mild Covid-19: A Randomized-Controlled Trial. Clin. Infect. Dis. an Off. Publ. Infect. Dis. Soc. Am. 2020 doi: 10.1093/cid/ciaa1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moraes T, B.L., 2020. COVID-19: public policies and society’s responses. Quality information for refining public policies and saving lives. Policy briefing note 20. São Paulo: Rede de Pesquisa Solidária de Políticas Públicas e Sociedade (n.d.).
- Liu Peiyu, Sha He L.R. The effect of control measures on COVID-19 transmission in Italy: Comparison with Guangdong province in China. Res. Sq. 2020 doi: 10.21203/rs.3.rs-20412/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N., Jit M., Klepac P. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet. Public Heal. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubino S., Kelvin N., Bermejo-Martin J.F., Kelvin D. As COVID-19 cases, deaths and fatality rates surge in Italy, underlying causes require investigation. J. Infect. Dev. Ctries. 2020;14:265–267. doi: 10.3855/jidc.12734. [DOI] [PubMed] [Google Scholar]
- Saez M., Tobias A., Varga D., Barceló M.A. Effectiveness of the measures to flatten the epidemic curve of COVID-19. The case of Spain. Sci. Total Environ. 2020;727:138761. doi: 10.1016/j.scitotenv.2020.138761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebastiani G., Massa M., Riboli E. Covid-19 epidemic in Italy: evolution, projections and impact of government measures. Eur. J. Epidemiol. 2020;35(4):341–345. doi: 10.1007/s10654-020-00631-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takemoto Maira L.S., Menezes Mariane de O., Andreucci Carla B., Nakamura‐Pereira Marcos, Amorim Melania M.R., Katz Leila, Knobel Roxana. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2020;151(1):154–156. doi: 10.1002/ijgo.v151.110.1002/ijgo.13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, Sam Webster, Petherick, Anna, Phillips, Toby, B.K., n.d. Oxford COVID-19 Government Response Tracker, Blavatnik School of Government. 2020. [WWW Document]. URL https://covidtracker.bsg.ox.ac.uk/ (accessed 6.15.20).
- Tian, H., Liu, Y., Li, Y., Wu, C.-H., Chen, B., Kraemer, M.U.G., Li, B., Cai, J., Xu, B., Yang, Q., Wang, B., Yang, P., Cui, Y., Song, Y., Zheng, P., Wang, Q., Bjornstad, O.N., Yang, R., Grenfell, B., Pybus, O., Dye, C., 2020. The impact of transmission control measures during the first 50 days of the COVID-19 epidemic in China. medRxiv 2020.01.30.20019844. https://doi.org/10.1101/2020.01.30.20019844.
- Tobías A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci. Total Environ. 2020;725:138539. doi: 10.1016/j.scitotenv.2020.138539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toshkov Dimiter. Government Capacity, Societal Trust or Party Preferences? What Accounts for the Variety of National Policy Responses to the COVID-19 Pandemic in Europe? OSF Prepr. 2020 doi: 10.31219/osf.io/7chpu. [DOI] [Google Scholar]
- Wang Weier, Tang Jianming, Wei Fangqiang. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan. China. J. Med. Virol. 2020;92(4):441–447. doi: 10.1002/jmv.v92.410.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- What We Can Learn From Singapore, Taiwan and Hong Kong About Handling Coronavirus. Time. 2020 [WWW Document], n.d. URL https://time.com/5802293/coronavirus-COVID-19-singapore-hong-kong-taiwan/ (accessed 4.15.20).
- WHO, 2020a. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. [WWW Document]. URL https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 (accessed 3.26.20).
- WHO Alphabetical List of WHO Member States [WWW Document] 2020. https://www.who.int/choice/demography/by_country/en/ accessed 6.20.20.
- Worldometer, n.d. COVID-19 CORONAVIRUS PANDEMIC [WWW Document]. URL https://www.worldometers.info/coronavirus/ (accessed 6.15.20).
- Yuan J., Li M., Lv G., Lu Z.K. Monitoring transmissibility and mortality of COVID-19 in Europe. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2020;95:311–315. doi: 10.1016/j.ijid.2020.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]