Graphical abstract
Keywords: Healthcare, Disinfection, Real-time monitoring, SARS-CoV-2, Technology
Abstract
The COVID-19 pandemic is continuing, and the innovative and efficient contributions of the emerging modern technologies to the pandemic responses are too early and cannot be completely quantified at this moment. Digital technologies are not a final solution but are the tools that facilitate a quick and effective pandemic response. In accordance, mobile applications, robots and drones, social media platforms (such as search engines, Twitter, and Facebook), television, and associated technologies deployed in tackling the COVID-19 (SARS-CoV-2) outbreak are discussed adequately, emphasizing the current-state-of-art. A collective discussion on reported literature, press releases, and organizational claims are reviewed. This review addresses and highlights how these effective modern technological solutions can aid in healthcare (involving contact tracing, real-time isolation monitoring/screening, disinfection, quarantine enforcement, syndromic surveillance, and mental health), communication (involving remote assistance, information sharing, and communication support), logistics, tourism, and hospitality. The study discusses the benefits of these digital technologies in curtailing the pandemic and ‘how’ the different sectors adapted to these in a shorter period. Social media and television’s role in ensuring global connectivity and serving as a common platform to share authentic information among the general public were summarized. The World Health Organization and Governments’ role globally in-line with the prevention of propagation of false news, spreading awareness, and diminishing the severity of the COVID-19 was discussed. Furthermore, this collective review is helpful to investigators, health departments, Government organizations, and policymakers alike to facilitate a quick and effective pandemic response.
1. Introduction
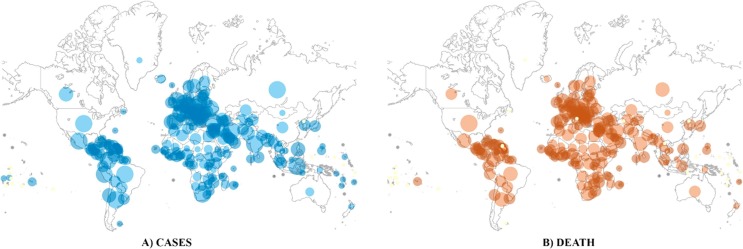
COVID-19 is an acute respiratory disease caused by the novel coronavirus SARS-CoV-2, which has created an unprecedented global health care crisis in modern medical history [1]. On January 30th, 2020 World Health Organization (WHO) announced COVID-19 as a Public Health Emergency of International Concern (PHEIC). Later on, within a span of fewer than 12 weeks after the first case was identified at Wuhan, China, WHO announced COVID-19 as a pandemic [2], [3]. Until now (i.e., as of March 16th, 2021), over 119 million infections and more than 2.6 million deaths have been confirmed globally after the first case was identified in December 2019 [4]. Fig. 1 shows the cumulative number of cases and deaths reported across the globe. The bigger (i.e., diameter) and darker bubbles indicate the severity of the outbreak in different regions across the world. However, the rapid exponentially increasing numbers of COVID-19 infections necessitates an urgently required enhancement of public health activities to elucidate and define the new virus’s epidemiology and characteristics [5]. Several public and private institutions worldwide are working together on finding an efficient way of lowering the impact of COVID-19 spread. During the Severe Acute Respiratory Syndrome (SARS) CoV1 and Ebola outbreak, different authorities used Mobile, GPS data, and other various electronic data to identify and monitor the clusters [6], [7], [8]. These outbreak responses to public health activities remain significant today, including tracking, immediate case detection, minimizing transmission to the communities, and robust public communication. It is essential to track the implementation and effect of such action on the rate of spreading and mortality.
Fig. 1.
Cumulative number of cases and deaths reported across the globe (as of March 16th, 2021) [9].
In the present situation of COVID-19, different countries use a range of digital tools to support public health initiatives. Several latest technologies, including mobile applications, robots, Artificial Intelligence (AI), drones, and other social media platforms, are found helpful in healthcare (i.e., in contact tracing, monitoring, thermal screening, sanitation, locomotion, and clinical conditions), logistics, surveillance, and awareness measures. Several public and private institutions worldwide are working together on finding an efficient way of lowering the impact of COVID-19 spreading. During the SARS CoV1, Hong Kong authorities used and analyzed various electronic data to identify and monitor the clusters [8]. Therefore, this review paper addresses the need to bring out the role of modern technologies into a single platform and discusses in detail ‘why’ and ‘how’ these technologies are used worldwide to fight against the surge in the pandemic outbreak.
Many aspects of life have changed with the technological transformation. Currently, 70% of the world population use mobile devices, out of which 65% use smartphones. Similarly, statistical studies show that around 4 billion people are active on social networking platforms [10], [11]. In this context, researchers concentrate on technical solutions to simplify the tracing and tracking processes more effectively. The use of GPS, Wi-Fi, or tower location to locate smartphones makes tracking purposes most ideal. Also, the built-in Bluetooth interface allows communication and proximity detection with nearby smartphones, making it suitable for automatic and accurate contact tracing [12], [13]. Such tracking applications automatically capture the user interaction data using the Bluetooth interface data that can then be applied to a potential source for the data analysis [14]. Apart from contact tracing, several mobile applications were developed to monitor and observe the infected people’s real-time condition for analyzing the health condition, effective and proper use of face masks, social distancing measures, and for providing mental health benefits [15].
As reported by the WHO, several potential COVID 19 vaccine developments are happening worldwide. Certain countries have also commenced the use of COVID-19 vaccines authorized by certain National Regulatory Authorities. However, none of these vaccines have received authorization from the WHO Emergency Use Listing/Prequalification (EUL/PQ) [16]. Therefore, avoiding direct interactions between people seems to be the only way to prevent the virus’s spread [17]. Similarly, the widespread of virus forced the governments to impose lockdowns, advise self-isolation, promote work from home policies, impose stringent social distancing requirements, and enact emergency health strategies, including extensive new technological infrastructure to treat and mass testing of the general public [18], [19]. Many countries have also used various drones for surveillance, thermal imaging, sanitization, and commercial deliveries in such a lockdown situation [15], [20]. However, it is not a permanent solution to sustain a full shutdown for the entire country. This necessitates rethinking and using robotic technology such as humanoids, robotic manipulators, drones, and independent systems to minimize and control the virus’s spread among the global population. Additionally, the impact of other platforms such as social media (search engines, Twitter, Facebook, LinkedIn, and others), television, Governmental initiatives (advertisements, signboards, and hoardings), and recreational applications played a significant role in spreading awareness against the pandemic outbreak.
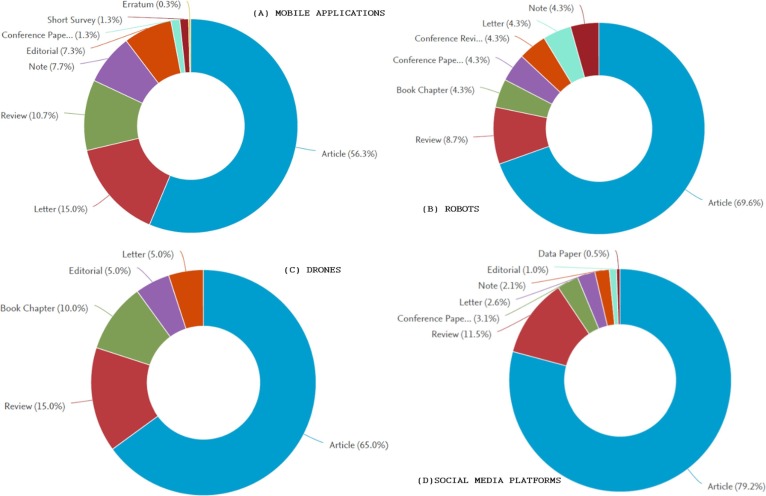
Fig. 2 shows the approximate numbers of articles by different categories (i.e., individual share) published in 2020, using the keywords ‘Mobile applications’ or ‘Robots’ or ‘Drones’ or ‘Social media platforms’ for COVID-19, and listed in the Scopus repository. Though the search outcome could differ with the use of different keywords, Fig. 2 illustrates the rise in technological dependence and the role of tackling the COVID-19. A cumulative total of 535 relevant articles were found in the categories mentioned above [21]. The share of review articles alone among the 535 articles was 60 (i.e., 11.2%). The data was retrieved from the Scopus database on October 12th, 2020.
Fig. 2.
Articles published in 2020 on different categories under mobile applications, robots, drones, and social media platforms for COVID-19 [21].
This review article’s primary objective is to discuss the latest and current-state-of-art modern technologies deployed in the fight against the novel coronavirus outbreak globally and their role in tackling the infectious disease. In the current scenario, with no possible cure or vaccine, the only remedy that the healthcare departments, Governments, and the general public alike can embrace is preventing the transmission of the pandemic with minimal risk at all costs. Therefore, this study provides critical and constructive discussions on the modern digital technologies (such as mobile applications, robots, and drones), social media platforms, television, the WHO, and various Governmental initiatives adopted towards curbing the pandemic. As the cumulative count of active infections is rising across the world, the discussions outlined in this study would benefit and widen the scientific community’s focus, help Governments and policymakers to utilize modern technologies to their full potential, and work towards vaccine/drug discovery.
The overview of the following sections is: Section 2 comprises of the role of various mobile applications developed globally; Section 3 discusses the aid of robots and drones; Section 4 deals with the contribution of social media platforms (search engines, Twitter, and Facebook), television, and other sources; Section 5 provides the details on the role of WHO and Governments worldwide, and Section 6 presents a concise summary of the study and authoritative future directions.
2. Mobile applications
Mobile applications (or apps) are integrated with other technologies to create solutions that facilitate combating the crisis and minimizing healthcare workers’ risk. Many apps were developed and proposed, some with the government’s aid for remote assistance like contact tracing, medical reporting, individual and regional risk assessment, isolation monitoring, information sharing, geofencing, border crossing registration, e-commerce, online learning, video conferencing, and health-related information sharing. Hospitals, universities, colleges, and other groups have also developed apps for tele-doctor service, self-health checking, monitoring, patient surveillance, pre-shift screening for employees, etc. Though these applications provide various utility functions, concerns were raised regarding the digital privacy of the user’s information. Also, during its initial stage of development, many apps required GPS and Bluetooth to be switched on the whole time, which drained the battery.
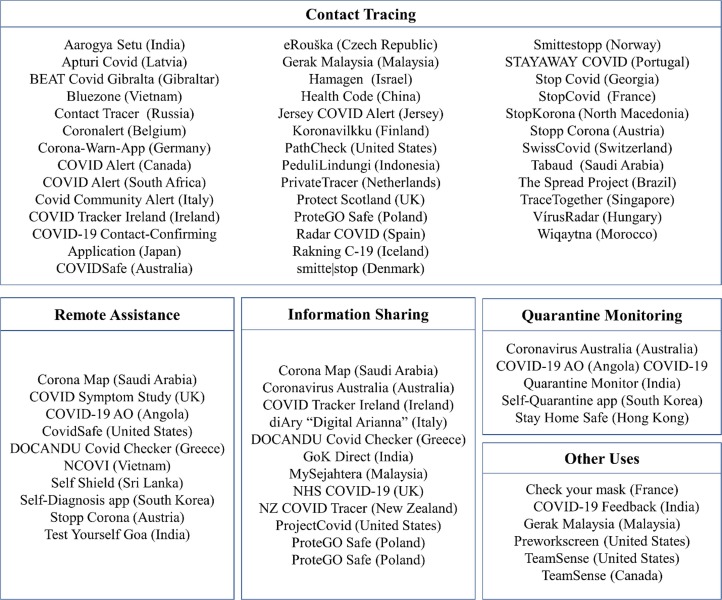
In this COVID-19 era, one of the frequently asked questions was, “Can mobile contact-tracing apps help lift lockdown?” [22]. This was because most of the apps launched for geofencing, contact tracing purposes remained unused, leading to its ineffectiveness. Although most of the apps and other integrated technology were not initially received well by the masses, it was later adopted on a large scale as people realized the applications’ predictive and preventive utilities [23]. This section discusses the various mobile applications developed worldwide to aid the fight against the COVID-19 pandemic. Fig. 3 represents an infographic outline of the different mobile applications launched globally and linked with COVID-19. For simplicity, the details in Fig. 3 were shortlisted to one application per country.
Fig. 3.
Infographic representation of various mobile applications deployed globally.
2.1. Contact tracing
Effective contact tracing is the preliminary step to tackle any pandemic in the initial stages before intensive testing and vaccination. An outbreak of ‘Nipah virus encephalitis’ in the Kerala state, India, was contained successfully because of an efficient contact tracing strategy carried out by the health department [24]. COVID-19 spread at an alarming rate, and it cannot be contained without adequate electronic health reporting and information management systems in place. According to the WHO, contact tracing should be done in three steps: contact identification, listing, and follow-up [25]. Many countries have developed applications to effectively record and monitor COVID-19 patients’ movements to track their primary and secondary contacts. GPS or Bluetooth network-based proximity detection was used to trace contacts and isolate them to contain the virus. Applications like ‘NOVID20′ in Austria, ‘OPEN CORONAVIRUS’ in Spain, ‘AROGYASETU’ in India, etc., which were developed for contact tracing, and proximity sensing helped to contain the virus to a large extent [26]. ‘Health Code’ developed by China makes it mandatory for users to scan codes wherever they go, be it offices, boarding a bus or train, and even housing complexes [27]. Both centralized and decentralized apps were developed globally, with the decentralized apps offering users a higher degree of privacy from the state or hackers for that matter [13]. The applications developed for contact tracing would be effective only if most of the population uses it, so countries like India have made it mandatory for its citizens [28].
2.2. Remote assistance, isolation monitoring, and syndromic surveillance
The major effort undertaken to decline the pandemic’s surge is by maintaining adequate social distancing and isolation to ensure that the virus does not spread. This situation demands monitoring patients from a distance, and all hospitals have adopted technological measures to ensure minimal contact between a patient and a health care professional [29]. Remote assistance includes video communication, audio call, instant messaging, and emergency call support for COVID-19 patients [30]. People who came in close contact with a COVID-19 patient and asymptomatic patients who do not need critical care life support systems are monitored remotely from the hospital at isolation centers. Patients may conduct self-assessment to check if their symptoms are related to COVID-19. Asymptomatic patients are asked to update their health data using a ‘sphygmomanometer’ for blood pressure, a thermometer for body temperature, an oximeter for heart-rate, and oxygen saturation levels on the application so that doctors can monitor them and assist them if necessary [31]. Self-Shield (Formerly COVID Shield) released by Commonwealth Centre for Digital Health (CWCDH) helps users regularly monitor their lung health. The app’s recording features analyze breathing sounds and related data to identify COVID-19 symptoms early [32]. This app was launched in Sri Lanka and also included features for managing quarantine and sharing information. The utility of the app will not be limited to COVID-19 alone but will be expanded further to assist people with various ailments for self-health checks.
2.3. Information sharing and communication support
The WHO declared the COVID-19 outbreak to be a Public Health Emergency of International Concern in end-January 2020 to bring about global coordination and support the nations where resources to fight the pandemic are lacking. The intent was to bring the world under a common platform to share information and guidelines to mitigate the virus. A common knowledge-sharing platform will help share research findings, news stories, or protocols to be followed, which was found useful in one corner of the world to the other [33]. This will ensure that people worldwide will have access to valid information and are not misinformed or propagandized during these testing times. If not curbed, fake news tends to be inflammatory and can provoke feelings of anxiety and depression among citizens, leading to panic buying, unnecessary fear, and panic [34]. Hence, proper monitoring of information is requisite.
A study conducted in Vietnam showed that people demand access to valid information related to ‘Updated information on disease and treatment,’ ‘Transmission mechanism and specific notices,’ and ‘Epidemiology of symptoms, treatment, and prevention’ [35]. Various governments and other organizations developed many applications in this context, one of the first among them being the GoK direct app by the Government of Kerala state in India to curb the spread of misinformation [36]. The application also contained toll-free helpline numbers for tele-assistance for fever clinic locating and ambulance services.
2.4. Quarantine enforcement
Many authorities across the world have launched applications to monitor the quarantined individuals. They use the network mapping facility in their smartphone to stamp their location and alert the authorities in case of any violations. China’s QR code scanning system, which was mandatory for citizens to move around, also served as a health certificate and travel pass. The mobile application’s color codes indicated the risk level of individuals and high-risk individuals (‘red’ color) were denied entry and required them to be isolated till their color code changed from ‘red’ to ‘green’ [15]. Similarly, the ‘Arogya Setu’ app launched by the Government of India enables users to self-assess individual risks to the virus. It gives a color code to each app user, depending on the exposure to the virus. The red color indicates that the user is COVID positive. ‘Orange’ and ‘yellow’ color indicates moderate exposure to an infected person. The ‘green’ color code means the user is safe and does not have to be isolated. Only people coded ‘green’ can enter premises that were opened after the lockdown [37]. The ‘Stay home safe’ app developed in Hong Kong for quarantine enforcement also uses the same concept and alerts the authorities if the user leaves the allotted quarantine center. The ‘Octopus mobile’ app, developed in Israel for quarantine monitoring and health crisis management, uses location tracking to keep individuals under isolation in check. The response center will receive a notification if the person leaves the geolocation of his home. Furthermore, his health will also be monitored periodically [38].
In India, the Karnataka state has developed and successfully implemented a quarantine monitoring app that keeps a close watch on people under home quarantine. The persons under home quarantine are compulsorily required to upload selfies every hour, tracked by the authorities. The photo or selfie contains the GPS coordinates, which will confirm the location of the person. Any violators will be moved to mass quarantine facilities [39]. India’s Tamil Nadu state has also launched an application to monitor those under home quarantine, known as ‘COVID-19 Quarantine monitor’. The app will alert the authorities if the user moves 500 m away from the prescribed location [40]. Apart from isolation monitoring, most of these applications also have features like a distress button and chat options to assist the user in case a need arises.
2.5. Mental health
The adverse psychological impacts along with the effect on physical health during a pandemic are a common cause of concern. Initial studies show that signs of anxiety and depression (16–28%) and self-reported stress (8%), along with disturbed sleep patterns, are common psychiatric problems associated with the pandemic. Though the introduction of measures like social distancing and lockdown is necessary, it can lead to isolation and decreased physical activity, which can have harmful mental health consequences [41]. Furthermore, many people face financial strain due to the loss of jobs or pay cuts, which can be emotionally taxing. The demand for mental health services and the burden on primary healthcare is at an all-time high, and telehealth sessions cannot cope with the demand. Mental health mobile apps are one way to deal with this situation and make mental health treatment accessible to all [42]. With the development of apps for mental health assistance, less severe trauma and mental health presentations can be dealt, and more acute cases can be dealt with at the clinics [43].
Health care people are the most traumatized and psychologically affected due to prolonged working hours to treat affected patients. Work strain and difficulties due to the pandemic have worsened the mental health amongst healthcare workers [44]. The University of North Carolina, along with Google Cloud, Alphabet, and One Mind, have teamed up to develop an application called’’ Heroes Health’ to attend to the mental health of frontline healthcare workers. The app provides weekly reports on symptom summary and information on the user’s mental health and even includes access to support resources if needed [45]. Some mobile applications previously developed and employed to assist military veterans in handling Post-Traumatic Stress Disorders (PTSD) were expanded to include frontline COVID-19 healthcare workers and recovered patients [46].
Another sub-category of the mental health applications is for recreational purposes. The world’s most famous ten English cognitive recreational applications reported millions of downloads after lockdown onset. The health care therapy online applications like Kara Connect® increased 16 times in their users after the lockdown [47]. The digital therapeutic mobile app BioBase® is familiar because of its ability to enhance mental health. The efficacy of BioBase® has been investigated for four weeks among university students and concluded that the BioBase® application significantly controlled anxiety and improved well-being [48]. This therapeutic pathway can also be followed to recover from mental problems such as depression caused due to the aftereffects of the COVID-19 pandemic. New York’s Counselling cell developed a set of clinical applications that can reduce anxiety, depression, sleeplessness and enhance recovery. Among their anxiety-reducing applications, headspace® is the widely used and essential therapeutic science-based clinically tested application [49]. It is a medication application, which can provide mindfulness and enhanced compassion within a minimum of 10 days of usage as per the developer’s statement. Another clinically tested therapeutic anxiety reduction application is the shine® [50]. It is also known as virus anxiety application, as it handles many topics, including; medications, xenophobia treatment, anxiety treatment, financial fear treatment, support for isolation, etc.
2.6. Other apps during COVID-19
Applications were developed for the self-screening of employees before the work shift. The employees can easily log in to the app and submit responses to a state-compliant symptom questionnaire, and the results will be updated on the company’s dashboard. Team sense in Canada and Pre-Work Screen in the US are examples of such applications being employed as employees across the world return to their workspaces [51], [52]. ‘Check Your Mask’ is another concept being developed to help individuals ensure the face mask’s correct position. The app analyses the mask’s position using a video selfie provided by the user and exploits Haar-like feature descriptors to detect key features of the face, and a decision-making algorithm is applied to validate the face mask [53]. Mobile applications were also employed to register and to provide permissions for border crossing across countries and states. One such example is the ‘Gerak Malaysia’ app used to track and record movement across states in Malaysia during the Movement Control Order (MCO) period. Various other applications also aim to improve the user’s motivation and self-confidence through community building, experience sharing, and sharing positive news related to fighting the pandemic, like new measures taken to curb the virus, recovery rate of patients, and so on.
2.7. Challenges with mobile applications
Presently, irrespective of the various utilities the mobile applications provide, there are many troubles with implementing such services. The primary concerns with privacy, data theft of the user’s information, and access to data produced by the mobile applications should be resolved by proposing a decentralized approach. Several European authorities raised their voice against the centralized system since it comes with individual privacy risks, a possibility of state surveillance, and third-party breaches. The decentralized approach enables to notify of at-risk contacts automatically without retaining any health or contact data. This means that the data is not accessible to anyone for research or other purposes.
The ethical usage of mobile applications should ensure the protection of voluntariness of every user. Each step of the digital contact tracing process, from owning a smartphone, downloading the application, allowing it to run in the background, reacting to alerts, and deciding to share contacts if tested positive, should be done voluntarily by the user itself for the application to be deemed truly voluntary [54]. Furthermore, the users should be free to uninstall the application at any time. But in many countries, such applications were made mandatory for people who wanted to move around public spaces such as malls, markets, etc. For example, even though the application is pro forma voluntary in China, people who wanted to access public areas had to have the application downloaded compulsorily. In France, when people refused to use contact applications, the government had to nudge the public to use them. With the pressure from the government and society, people felt compelled to download the application. As a solution to this, Morley et al. [55] suggest a framework for addressing the ethical concerns of contact tracing applications. This framework is intended to help designers evaluate the moral legitimacy of an application. The framework contains the following criteria, which should be answered positively. They are:
Is the use voluntary?
Is consent required to share the data?
Is the data kept private?
Can users erase the data?
Is the purpose defined?
Is it used for prevention only?
Is it equally available and accessible?
Is there an end of life process to decommission the contact tracing app?
The mobile applications can be deemed to be ethical only if these criteria are fulfilled. Therefore, similar frameworks are mandatory to ensure the legal bases of using mobile applications before it is employed for monitoring the contacts or outbreaks.
Initial media reports stressed that the contact tracing apps would be effective only at an adoption rate of more than 60%. However, studies show that even with a low adoption rate, the apps will help in reducing the number of COVID-19 cases and deaths [56]. Another issue with apps is that it might not work on older versions of smartphones, making them ineffective. False alarms also raise unnecessary concerns. For example, Bluetooth based proximity detection can cause over-reporting of interactions leading to unnecessary self-isolation and false-positive alarms. This decreases the app’s reliability, and users will start to ignore warnings, which could be true positive warnings [57]. Health apps might prove to be a vital tool in the modern era, but health professionals must continuously assess and monitor them to guide patients to use them most effectively. The study conducted by Kelly Hale et al. indicates that though the apps employ highly interactive intervention strategies, they cannot replace human factors such as empathy and understanding. The focus on incorporating emotion and cognitive strategy is significantly less since there is uncertainty over the apps’ effectiveness if it employs many strategies simultaneously [58].
3. Robots and drones
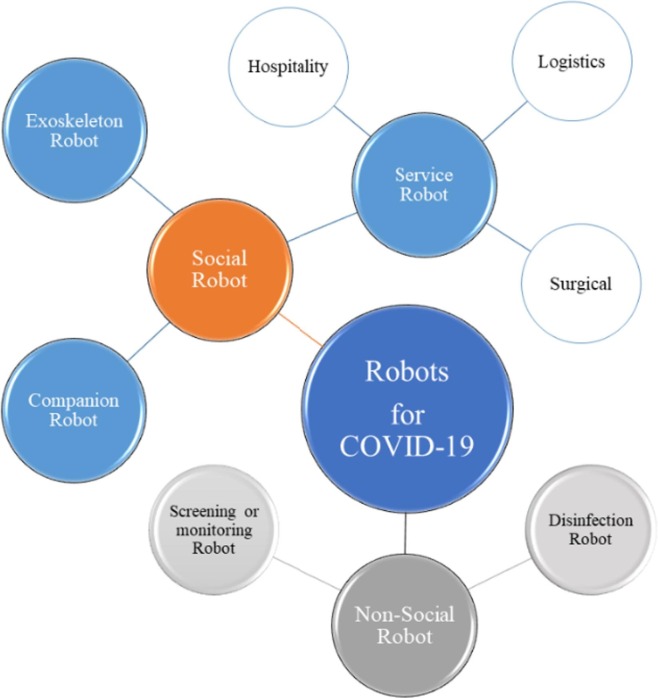
In the context of COVID-19, many countries have employed innovative strategies to counter the pandemic situation with robotics, drones, and artificial intelligence. Nowadays, common technologies include teleoperation, autonomous service robots, facial recognition, thermal scanning, and other intelligent systems to reduce, control, or diagnose the virus. Fig. 4 shows the major classification of robots based on the nature of applications. Robots in the COVID-19 situation can be classified under non-industrial robots, concentrating primarily on the service sector. These robots can be further classified into mobile and stationary robots based on their mobility; manually controlled, semi-autonomous, and autonomous robots depending upon their sensory feedbacks and intelligence level. Similarly, drones being robust and flexible were widely employed in preventing the surge in COVID-19 for screening and monitoring in travel sectors, healthcare, disinfection, and logistics. Therefore, this section justifies how robots and drones can solve the challenges being faced during the pandemic cause. Table 1 outlines the details of the commercially available robots and drones deployed worldwide to tackle the surge in the COVID-19 outbreak.
Fig. 4.
Schematic layout of different classification of robots based on applications.
Table 1.
Commercially available robots and drones deployed worldwide for COVID-19.
| Sl. No. | Robot name (Company) | Country of origin | Medical | Screening | Disinfection | Logistics | Companion | Hospitality | Others | Robot characteristics | Websites |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Greetbot (OrionStar) | China | √ | √ | √ | √ | Wheeled | https://www.vision-systems.com/ | |||
| 2 | Cruzr (Ubtech) | China | √ | √ | √ | √ | Wheeled | https://www.ubtrobot.com/products/cruzr?ls=en | |||
| 3 | Pepper (Softbank) | Japan | √ | √ | √ | √ | √ | √ | Wheeled | https://www.softbankrobotics.com/emea/en/pepper | |
| 4 | Whiz (Softbank) | Japan | √ | √ | Wheeled | https://www.meetwhiz.com/ | |||||
| 5 | Atlas (Boston Dynamics) | USA | √ | √ | √ | √ | Legged | https://www.bostondynamics.com/atlas | |||
| 6 | Sanbot (Qihan Technology) | China | √ | √ | √ | √ | Wheeled | http://en.sanbot.com/product/sanbot-nano/performance | |||
| 7 | Temi (Robotemi) | USA | √ | √ | √ | Wheeled | https://www.robotemi.com/ | ||||
| 8 | Nao (Softbank) | Japan | √ | √ | Wheeled | https://www.softbankrobotics.com/emea/en/nao | |||||
| 9 | Promobot (Promobot). | USA | √ | √ | √ | √ | Wheeled | https://promo-bot.ai/ | |||
| 10 | Mitra and Mitri (Invento Robotics) | India | √ | √ | √ | Wheeled | https://mitrarobot.com/ | ||||
| 11 | Mini Ada (Akin Robotics) | Turkey | √ | √ | √ | √ | Wheeled | https://www.akinrobotics.com/en/miniada3_pictures | |||
| 12 | AKINCI-4 (Akin Robotics) | Turkey | √ | √ | Legged | https://www.akinrobotics.com/en/akinsoft-humanoid-robot-akinci-4 | |||||
| 13 | ARAT-3.2 (Akin Robotics) | Turkey | √ | √ | Legged | https://www.akinrobotics.com/en/akinsoft-4-legged-robot-arat-3–2 | |||||
| 14 | C-Astra (Invento Robotics) | India | √ | √ | Omni-wheels | https://mitrarobot.com/covid/ | |||||
| 15 | Robo-C (Promobot) | USA | √ | √ | √ | Legged | https://promo-bot.ai/robots/robo-c/ | ||||
| 16 | AS-PNCR-2 (Akin Robotics) | Turkey | √ | √ | √ | Wheeled | https://www.akinrobotics.com/en/akinsoft-agricultural-robot-as-pncr-2 | ||||
| 17 | AtraxM (Polish Air Force) | Poland | √ | √ | Drone | https://www.airforce-technology.com/projects/atrax-vtol-unmanned-aerial-vehicle/ | |||||
| 18 | RoboDoc (Invento Robotics) | India | √ | √ | Wheeled | https://mitrarobot.com/covid/ | |||||
| 19 | Pudobot (Pudo Robotics) | China | √ | √ | √ | √ | Wheeled | https://pudurobotics.uk/ads | |||
| 20 | Robot Arm-3 (Akin Robotics) | Turkey | √ | √ | Stationary | https://www.akinrobotics.com/en/akinsoft-industrial-robot-arm-3 | |||||
| 21 | Ava (Ava Robotics) | USA | √ | √ | √ | √ | Wheeled | https://www.avarobotics.com/ | |||
| 22 | Moxi (Diligent robotics) | USA | √ | √ | √ | √ | √ | √ | √ | Wheeled | https://diligentrobots.com/moxi |
| 23 | DaVinci (Medtronic) | USA | √ | Robotic manipulator | https://www.medtronic.com/covidien/en-us/robotic-assisted-surgery/surgical-robotics.html | ||||||
| 24 | Disinfection robot (Siemens) | Germany | √ | √ | Track wheel | https://new.siemens.com/global/en/company/stories/industry/intelligentrobotics-siemens-aucma.html | |||||
| 25 | Model C (UVD Robots) | Denmark | √ | Omni wheels | https://www.uvd-robots.com/robots | ||||||
| 26 | LightStrike (Xenex Solutions) | USA | √ | √ | Wheeled | https://xenex.com/ | |||||
| 27 | GoBe (BlueOcean Robotics) | Denmark | √ | √ | Wheeled | https://www.gobe-robots.com/ | |||||
| 28 | PTR (BlueOcean Robotics) | Denmark | √ | √ | Stationary | https://www.ptr-robots.com/ | |||||
| 29 | Techman Vision (Uchimura Robotics) | Japan | √ | √ | Stationary | https://uchimurarobotics.com/ | |||||
| 30 | Mini U (Xiaoben Intelligence) | China | √ | √ | √ | Legged | http://www.uurobot.com/en/xiaoben.html | ||||
| 31 | Mink (Blue Ocean Robotics) | Denmark | √ | √ | Wheeled | https://www.blue-ocean-robotics.com/ | |||||
| 32 | Disinfecting Robot (Uchimura Robotics) | Japan | √ | Wheeled | https://uchimurarobotics.com/ | ||||||
| 33 | Pari 2.0 (Paaila Technology) | India | √ | √ | Legged | http://www.paailatechnology.com/robotics/pari2/ | |||||
| 34 | James (Zorabots) | Belgium | √ | √ | √ | √ | Wheeled | https://www.zorarobotics.be/robots/james | |||
| 35 | Sawyer (Zorabots) | Belgium | √ | √ | √ | Stationary | https://www.zorarobotics.be/robots/sawyer | ||||
| 36 | RP-VITA Telemedicine Robot (MedTech Boston) | USA | √ | √ | √ | √ | √ | √ | Wheeled | https://spectrum.ieee.org/automaton/robotics/medical-robots/irobot-and-intouch-health-announce-rpvita-telemedicine-robot | |
| 37 | Cutii (Careclever) | France | √ | √ | Wheeled | https://www.f6s.com/cutii | |||||
| 38 | Billy (Zorabots) | Belgium | √ | √ | Stationary | https://www.zorarobotics.be/robots/billy-billy | |||||
| 39 | Kiwibot (Kiwi Robotics) | Colombia | √ | √ | √ | Wheeled | https://www.kiwibot.com/ | ||||
| 40 | Starship (Starship Technologies) | USA | √ | √ | √ | Wheeled | https://robots.ieee.org/robots/starship/ | ||||
| 41 | RoboPony (Zhen Robotics) | China | √ | √ | √ | Wheeled | https://www.deccanchronicle.com/technology/gadgets/ | ||||
| 42 | R2 (Nuro Technology) | USA | √ | Wheeled | https://nuro.ai/product | ||||||
| 43 | Apollo 3 (Neolix Technologies) | China | √ | Wheeled | https://www.forbes.com/sites/ | ||||||
| 44 | Peanut (Keenon Robotics) | China | √ | √ | Wheeled | http://www.keenonrobot.com/EN/Product/pro2.html | |||||
| 45 | TUG (Aethon Robotics) | USA | √ | √ | √ | Wheeled | https://aethon.com/ | ||||
| 46 | Hospi (Panasonic) | Japan | √ | √ | Wheeled | https://news.panasonic.com/global/stories/2019/69861.html | |||||
| 47 | Run (Yunji Technology) | China | √ | √ | √ | √ | Wheeled | https://en.yunjichina.com | |||
| 48 | KARMI-Bot (Asimov Robotics) | India | √ | √ | √ | √ | Wheeled | https://www.livemint.com/news/india/kerala-govt-hospital-deploys-robot-to-serve-food-medicines-to-covid-19-patients-11587808212869.html | |||
| 49 | Amy (Pangolin Robotics) | China | √ | √ | √ | Wheeled | https://en.csjbot.com/content/12/1290.html | ||||
| 50 | Security Guard bot (CSJBOT) | China | √ | √ | Wheeled | https://en.csjbot.com/content/105/1301.html | |||||
| 51 | Mobile VendBot (CSJBOT) | China | √ | Wheeled | https://en.csjbot.com/content/11/1315.html | ||||||
| 52 | Snow (CSJBOT) | China | √ | √ | Wheeled | https://en.csjbot.com/content/12/1297.html | |||||
| 53 | Zafi (Propeller Technologies) | India | √ | √ | √ | √ | Wheeled | https://www.propellertechnologies.in/ | |||
| 54 | P3 (CSJBOT) | China | √ | √ | Wheeled | https://en.csjbot.com/content/106/1304.html | |||||
| 55 | Sona 2.5 (Club First robotic solutions) | India | √ | √ | Wheeled | https://clubfirst.org/product/sona-2–5-service-robot/ | |||||
| 56 | Sunbot (Siasun Robotics) | China | √ | √ | √ | √ | Wheeled | http://siasun.com/index.php?m=content&c=index&a=show&catid=108&id=447 | |||
| 57 | Spot (Boston Dynamics) | USA | √ | √ | √ | √ | √ | √ | √ | Legged | https://www.bostondynamics.com/spot |
| 58 | Dinsow (CT Asia Robotics) | China | √ | √ | √ | Wheeled | https://www.dinsow.com/about.html | ||||
| 59 | Handle (Boston Dynamics) | USA | √ | √ | Wheeled | https://www.bostondynamics.com/handle | |||||
| 60 | Aimbot (UBTech) | China | √ | √ | √ | Wheeled | https://www.ubtrobot.com/products/anti-epidemic-solution?ls=en | ||||
| 61 | K5 ASR (Knight Scope Robotics) | USA | √ | √ | √ | √ | Wheeled | https://www.knightscope.com/knightscope-k5 | |||
| 62 | O-R3 (Otsaw Technologies) | Singapore | √ | √ | √ | √ | Wheeled | https://otsaw.com/o-r3-security-robot/ | |||
| 63 | PGuard (Enova Robotics) | France | √ | √ | √ | Wheeled | http://enovarobotics.eu/ | ||||
| 64 | Camello (Otsaw Technologies) | Singapore | √ | √ | √ | √ | Wheeled | https://otsaw.com/camello/ | |||
| 65 | Veasense (Enova Robotics) | France | √ | √ | √ | √ | Wheeled | https://enovarobotics.eu/product/ | |||
| 66 | O-RX (Otsaw Technologies) | Singapore | √ | Wheeled | https://otsaw.com/o-rx-disinfection-robot/ | ||||||
| 67 | XR-1 (CloudMinds) | Japan | √ | √ | √ | √ | √ | Wheeled | https://www.en.cloudminds.com/ | ||
| 68 | ElliQ (Intuition Robotics) | USA | √ | √ | Stationary | https://elliq.com/ | |||||
| 69 | Dinsow (CT Asia Robotics). | Thailand | √ | √ | √ | √ | Wheeled | https://www.dinsow.com/ | |||
| 70 | Dasomi (Korea Herald Robotics solution) | Korea | √ | √ | √ | Wheeled | https://www.koreatimes.co.kr/www/tech/2019/06/133_268818.html | ||||
| 71 | Skyrocket (Google) | Australia | √ | Aerial | https://blog.werobotics.org/2020/04/25/cargo-drones-covid-19/ | ||||||
| 72 | Zipline (Zipline incorporations) | USA | √ | Aerial | https://blog.werobotics.org/2020/04/25/cargo-drones-covid-19/ | ||||||
| 73 | Corona Combat Drone (Indian Robotics Solution) | India | √ | Aerial | https://analyticsindiamag.com/this-indian-startup-is-fighting-covid-19-with-combat-drones/ | ||||||
| 74 | KC N901 (KC wearable technology) | China | √ | Wearable | https://kcwearable.com/ | ||||||
| 75 | T2 (Rokid) | China | √ | Wearable | https://www.rokid.com/en | ||||||
| 76 | M4000 (Vuzix) | USA | √ | Wearable | https://www.vuzix.com/ |
3.1. Robots in healthcare
The sudden outbreak of the coronavirus causes immense pressure and risk to all medical staff. The report shows that more than 30% of the diagnosed cases are healthcare workers as they come near infected patients [59]. In many parts of the world, the number of patients is alarmingly increasing, which forces facilities like the stadium, party halls, school/college auditoriums, etc., to be transformed into temporary hospitals to treat patients. This happens to create a shortage of available medical staff to treat patients. Robotics is the ideal solution to deal with these staffing shortages at hospitals and reduce the risk to frontline healthcare workers from getting affected by the coronavirus. The use of medical robots does not imply the complete replacement of doctors or nurses. However, this technology avoids the healthcare worker’s direct exposure to the patient through teleoperation/telepresence. Lanza et al. [60] proposed an intelligent medical care architecture into companion robots that can take sensible decisions for unhandled situations. The robot communicates the choice to the doctor at a distance for his/her permission. Telepresence involves an equipped mobile robot that brings a virtual interface of the patient with the doctor to perform diagnostic tests like checking temperature, taking blood samples, etc. Also, telepresence makes it possible for doctors/specialists under quarantine to treat patients adding a little extra slack to the overburdened system. Similarly, telepresence reduces the frequency of direct encounters for doctors and nurses from meeting COVID patients. Besides, these devices provide a platform for loved ones to visit patients under treatment or at quarantine remotely.
Even before the COVID outbreak, the Polish air force used drones for medical services. ‘AtraxM,’ a polish drone, was used to deliver necessary life-saving aids and first-aid kits [61]. The ‘Ava’ robot is one of the efficient telepresence robots seen in hospitals that combine autonomous mobility with a good quality video interface [62]. This robot is equipped with depth cameras and lidar sensors to navigate, avoiding obstacles along its path. Ava uses a video conferencing system partnered with Cisco Systems Inc. to ensure private conversations between the doctor and patient. Furthermore, this robot has a simple design, offers effortless assembly/disassembly, and easy cleanability. Diligent robotics introduced the ‘Moxi’ robot to perform non-care and non-value-related repetitive tasks in hospitals allowing the clinical staff to focus more on patients [63]. The fully autonomous Moxi robot consists of a robotic arm with a gripper for manipulation, performs logistical tasks like distribution of supplies and food to patients, sets up hospital rooms, and interacts with the surrounding environment. Circolo hospital in Italy introduced assistive robots named ‘Tommy’ for providing additional aid to doctors and nurses [64]. The robot consists of sophisticated tools to measure the patient’s vital statistics and enable continuous monitoring by the doctor. The robot can also measure the blood pressure and breathing capacity of patients. Fig. 5 shows the photographs of the selected robots and drones employed in the healthcare sector.
Fig. 5.
Photographs of (A) ATRAX, (B) AVA, (C) MOXI, and (D) TOMMY [64], [71], [72], [73].
The collection and transport of oropharyngeal swabs from patients to test for COVID-19 is another challenging task worldwide [65]. As a solution to this problem, the Chinese Academy of Sciences introduced drones to transport medical samples, significantly reducing human contacts [66]. This technology drastically reduces the risk factor, transportation time, and delivery expenditures by more than half. Similarly, Angurala et al. [67] developed a method to use drones and the Internet of Things (IoT) to collect samples and deliver medicines, ensuring zero contact between the medical staff and patients. Kimmig et al. [68] pointed out that performing surgeries during this epicenter of the pandemic is highly risky for both the surgical team and the patient subjected to surgery. Therefore, the author suggests robot-assisted surgery, especially for patients urgently needing complex oncological surgeries. Zemmar et al. [69] describe the benefits of utilizing AI, virtual, and augmented reality in surgical environments. The authors point out that this technique can improve the surgeon’s efficiency and enhance patient and doctor safety. Yang et al. [70] comment that the availability of 5G bandwidth and 4–8 K video streaming enables telemedicine and telecommuting possible and will mark how future organizations will function. In comparison to open surgeries, surgeries with the aid of robots reduce contamination with the body fluids due to no directly exposed medical staff. Few of the commercially available medical robots are Greetbot, Pepper, Sanbot, Promobot, Mitra, C-Astra, RoboDoc, Pudobot, Ava, Moxi, DaVinci, PTR robots, Techman vision, RP-Vita telemedicine robot, TUG, Karmi-Bot, Aimbot, Veasense, XR-1, Dinsow, Dasomi, etc., as shown in Table 1.
3.2. Real-time monitoring/screening
As mentioned previously, the highly contagious nature and non-existence of proper medication make it necessary to identify symptomatic/infectious persons within the community. It is also required to ensure that everyone follows the social distancing protocol and abides by government guidelines in public places. However, manual screening and monitoring of people is an unsafe, time-consuming, and hectic process. Therefore, in this state of a health crisis, robotic devices can be used to avoid the virus’s spread and enable efficient large-scale screening techniques. The digital health solutions involve real-time monitoring and evaluation of people to ensure law enforcement in public spaces. There are several methods to identify the concentration of the crowd in both indoor and outdoor scenes. This includes WiFi, tracking based on cellular connectivity, Bluetooth, Radio-frequency identification (RFID), etc. However, using WiFi or Bluetooth requires the person to be connected through a smartphone or smartwatch. Therefore, this technology is suitable to monitor a constrained space. China is one such country that promotes modern technologies and the first country to continuously introduce a satellite navigation system named ‘BeiDou’ to track COVID patients [72] continually.
Another low-cost method to screen high-risk environments includes the use of drones. Programming drones with appropriate sensors and AI enables it to gather relevant information to prioritize critical regions within a confined space [74]. Advancements in AI, Machine learning (ML), and image processing techniques make it possible to track, diagnose, and assist the concerned authorities in taking preventive measures. In India, the states Kerala and Gujarat are among the first to use drones for surveillance [75]. Generally, these aerial vehicles record the thermal images and their GPS location, which on further analysis identifies the symptomatic patients [76]. Sathyamoorthy et al. [77] developed a low-cost mobile robot named COVID robot that combines ‘Deep Reinforcement’ learning the model-based method to detect and warn pedestrians within the proximity of six feet from each other. The study also showcases the effectiveness of combining robot vision with CCTV (robot camera + CCTV) to identify pedestrians violating social distancing constraints.
Effective AI tools overcome the drawback of giving false positive or negative detection, especially at the early stages of COVID-19, as observed in the RT-PCR technique [78]. Some of the latest tools to screen the novel coronavirus disease include Convolutional Neural Networks (CNN) [79], Deep learning [80], IoT combined with ML [81], Big Data [82], etc. which rely mainly on the radiographic patterns seen in chest CT scans. For this reason, Hou et al. [83] introduced a deep learning model based on volumetric chest CT scan images for both COVID-19 and pneumonia patients. Rundo et al. [84] proposed a combination of AI and human intelligence to overcome the uncertainties with decision-making and diagnosing diseases. However, many challenges still exist, like distinguishing the COVID-19 from pneumonia since they both show very similar symptoms, data paucity, and initial investment. In addition to these limitations, other problems such as privacy and security issues and lack of transparency may lead to further complications [85]. These challenges create a massive gap between artificial intelligence implementation into the healthcare sectors [86]. Additionally, the introduction of complementary tools like receiver operating characteristic curve and specificity improves the diagnostic performance. Ye et al. [87] presented the ultrasound-based system to perform the ‘Cardiopulmonary Assessment’ on patients having COVID. The authors use a telerobotic ultrasound scanning device without sacrificing the information quality while performing the test. This methodology poses less threat to both patients and the examiner. Wang et al. [88] proposed an algorithm to identify people in public spaces with no mask using image processing techniques and CNN. Similarly, countries like China, the United Kingdom, Thailand, Italy, India, and the USA deploy drones for surveying, crowd management, and disease detection with the aid of loudspeakers, HD zoom lenses, floodlights, and thermal sensors [89].
Currently, there are several wearable devices available in the market that continuously measures body signals and pulses. These devices give bio-feedback based upon the measured values to warn and guide the user [90]. The Indian Robotics Solution (IRS) company developed a wearable helmet that describes individuals having elevated temperatures in public spaces. The device is called ‘Thermal Corona Combat Headgear’ (TCCH) [91]. Few other commercially available screening/monitoring robots are Cruz, Pepper, Atlas, Promobot, Mitri, Robo-C, AS-PNCR-2, AtraxM, Moxi, LightStrike robot, Mini U, Starship, Run, Spot, O-R3, etc., as shown in Table 1.
3.3. Disinfection
This subsection focuses on the applicability of robots to perform tedious routine tasks of disinfection to lower the risk of contact with bacteria, viruses, or other pathogens. Frequent disinfection and sanitizing of public places is the key safety measure to prevent COVID-19 spread. It is important to note that the disinfection robot is one of the most vital needs of the hour, aiming to protect public health by spraying disinfectants, emitting ultraviolet (UV) radiation [92], or sterilizing the virus exposed regions. Likewise, these robots also enable re-use masks or Personal Protective Equipment (PPE) at times of shortage. This technology can eliminate any form of human error and be a valuable tool to battle against infectious pathogens and harmful micro-organisms. Studies show that the use of unmanned aerial vehicles and unmanned grounded vehicles reduces the time needed for disinfection by 95% [93].
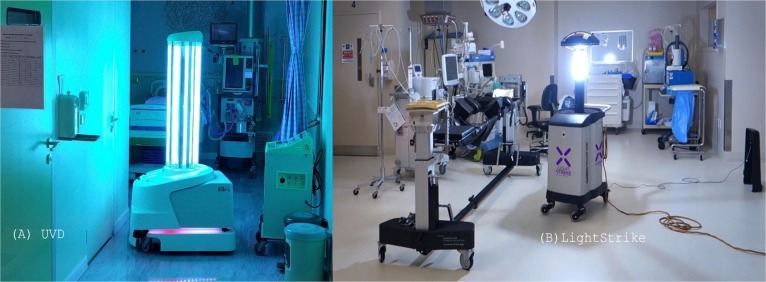
Siemens developed a very efficient disinfectant robot that uses hydrogen peroxide vapor and UV radiations to disinfect surfaces. The device reduces the direct exposure of humans to these contagious viruses and helps to decontaminate surfaces. This robot avoids the need for on-site refueling, as seen in certain moisturizer gun-based robots [94]. ‘UVD’ robots, a Denmark-based company, developed disinfectant robots that can emit short-wavelength and concentrated UV radiations. These radiations have enough energy to break the structure of any micro-organisms. This device offers a germicidal effect, which eliminates both airborne viruses and suspended aerosol particles. Similarly, the use of concentrated radiations makes it possible to disinfect hard-to-reach surfaces like the bed, staircase rail surfaces, corners, ventilators, exhaust fans, etc. [95]. The ‘LightStrike’ robots, developed by Xenex Disinfection Services LLC, use a broad-spectrum pulse xenon UV radiation to kill pathogens quickly and effectively eliminate Ebola and Anthrax viruses. This robot was first deployed at San Antonio International airport, the USA, to deactivate the SARS-CoV2 virus [92], [96]. Fig. 6 shows the photographs of the robots used for disinfection. Similarly, India successfully uses drones mounted with sanitizer to sanitize thickly populated slums and colonies in a short duration of time [97]. Similar to humans, animals/livestock are also prone to such deadly viruses. It may also turn out that these animals and their surroundings be another source of spreading the virus. However, manual disinfection is again very risky, laborious, and time-consuming. This mandates the need for intelligent disinfection techniques to be adopted for livestock breeding. For this reason, Feng and Wang [98] proposed a mobile robot consisting of a disinfectant spraying unit and a controller unit supporting remote operations. Other commercially available disinfection robots include Whiz, Mini Ada, ARAT-3.2, C-Astra, AS-PNCR-2, Model-C, LightStrike robot, James, Kiwibot, RoboPony, P3, Aimbot, PGaurd, Sterilization robot, etc., as shown in Table 1.
Fig. 6.
Photograph of (A) UVD robot, and (B) LightStrike robot [95], [96].
3.4. Companion robots
Recent studies show that loneliness and isolation due to coronavirus has created a global threat among people of all age groups [99]. Brooks et al. [100] performed a psychological study to understand the negative impact of quarantine on people. The study concludes that most people suffer from stress symptoms, confusion, anger, boredom, and fear during this period. The study also concludes that under extreme conditions, it may also lead to long-lasting effects. Henkel et al. [101] showcased that children below the age of puberty and people above 65 are the most vulnerable due to isolation. Companion robots mainly aim to keep patients under isolation or quarantine engaged by exchanging conversations and kill time sensibly. Developments in AI aim to equip the robot to understand the patient’s emotional feelings similar to humans and improve their mental state of mind. Other contagious diseases like chickenpox also provide room for such companion robots.
Adalgeirsson et al. [102] developed the ‘MeBot,’ which, in addition to sharing conversations, also expresses gestures and body poses. This expressive feedback makes the interaction more engaging and livelier. In addition to maintaining isolated patients, the elderly or disabled patients will require additional support to fulfill their basic needs. Again, the high risk of COVID-19 infections demands other alternatives to deal with these challenges. Therefore, using assistive robots makes it possible for senior citizens or the disabled to live independently, especially during quarantine or isolation [103]. The ‘BeamPro’ robot housed at Alexandra hospital, Singapore, is programmed to chat with patients under isolation [104], [105]. The robot can converse in four different languages with a relatively small response delay. In addition to this task, the ‘BeamPro’ robot makes it possible for the doctor to continuously inspect the patient in isolation and deliver the basic needs without a dedicated staff. DWI Dowellin, a Chinese based company, develops low-cost robocats and humanoids designed for children [106]. The robots are basically line-following robots that can sing, dance, and perform voice conversations. The ‘Pepper’ robot developed by Softbank robotics [107] is another common companion robot with 20 degrees of freedom (DOF) to make expressive movements while conversing. This robot is equipped with perception modules to recognize, interact, and speak 15 different languages. It can create an empathetic link with humans and develop intellectual skills. These social robots also instruct necessary exercising and relaxation tips to patients.
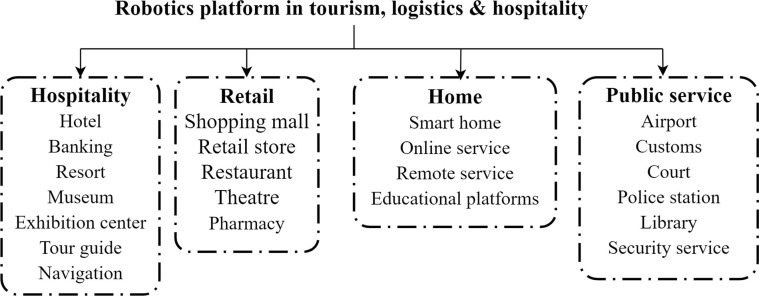
3.5. Tourism, logistics, and hospitality
The recent times show growing attention towards robots to perform interpersonal activities such as in tourism and hospitality. This may include providing the tourist with necessary directions and factual information, deliver food and other basic needs, cleaning, and also offer security service [108]. Even though most people restrain themselves from traveling, it is necessary to maintain the safekeeping of airports, railway stations, metro stations, etc., during this pandemic. This is achieved by employing robots to perform specific tasks like providing necessary information at the inquiry, enabling contactless e-ticketing facilities, security check, pick-and-place of luggage, and other routine services to enhance passengers’ security and safety. Few international airports that opted for robots to perform passenger assistance tasks are Munich airport, Incheon airport, Shenzhen airport, Amsterdam-Schiphol airport, Canadian airport, Dubai airport, Heathrow Airport, and Narita Airport, etc. Reports also estimate a Compound Annual Growth Rate (CAGR) growth of more than 15% in airport robot markets considering the current situation of the pandemic [109].
Similarly, the Indian railway implemented robots to screen passengers for coronavirus and cross-check for any government guidelines. This innovative step reduces the personnel burden and warns the passengers to maintain social distancing [110]. The idea of delivering commodities using robots/drones had begun much before the COVID pandemic outbreak. Ever since the COVID outbreak, the need for contactless delivery came to the forefront, with drones’ use most popular. Many e-commerce platforms like Alibaba [111] and Amazon [112] are moving towards complete contactless delivery of products to encourage people to stay at home and reduce all forms of human-to-human interactions. Furthermore, studies and trial runs are happening to automate logistics and deliveries using robots [113]. The ‘Nao’ robot developed by Softbank robotics is a miniature humanoid robot employed in companies, hospitals, hotels, etc., to welcome, give necessary information and entertain visitors [114]. The robot can recognize and speak in 25 different languages. The ‘Mitra’ Robot developed by Invento Robotics identifies guest-based face and voice recognition, consists of a built-in jukebox for entertainment, and collects analytics about visitors’ behavior and interactions [115]. Furthermore, the various sectors in which the robots are used for assistance in hospitality, retail, home, and public services, can be broadly classified, as shown in Fig. 7 .
Fig. 7.
Different sectors in which robots are utilized for assistance.
3.6. Limitations of AI and robotics
The major challenge of implementing robots is their high initial cost and expensive maintenance. Like the da Vinci surgical robot, many robots that assist doctors in performing surgeries are costly [116]. The high costs of robotic systems indirectly increase the patients’ treatment expenditures and limit their usage in many parts of the world. Currently, the high prices of robots are observed due to the complexities of sensing the surrounding environment and responding to external inputs from humans or other machines simultaneously. The key challenges with social robots are modeling the social dynamics and responding to social and moral norms in real-time. It is desired that social robots can input multiple modalities and combine them with predictive models to improve the dynamic nature of social interactions. Another issue with social bots is their ability to have one-to-one interactions only and their incapability of group interactions. Also, present-day robots cannot comprehend abnormal or suspicious activities during emergencies.
Robots are programmed with feedback loops to function in unstructured environments. However, the failure of any feedback sensors or put to work under non-ideal conditions may cause it to work abruptly. Any form of inconvenience experienced by the end-user due to robot malfunction can negatively affect service efficiency. The direct consequence of operation and complications with robotic systems is a severe issue, especially in the healthcare sector. In extreme situations, this may also lead to the patient’s tragic death. According to the study performed by the US Food and Drug Administration (FDA), unfortunate incidents have been prevalent, including fatalities, injuries, and robot malfunctioning. The study showed that from 2000 to 2013, there had been 144 casualties, 1391 injuries, and 8061 device malfunctioning cases reported by the use of robots during surgeries [117]. One solution to this problem is replacing rigid materials with softer lifelike materials to reduce the severity of accidents. Such robots, termed soft robots, can prevent potentially dangerous collisions when operating with humans or other similar environments [118].
As robots get increasingly involved with society, maintaining the user’s ethics and privacy becomes difficult. Advancements in AI for social and surveillance robots can be sources of ethical, legal, and social concerns that may lead to privacy risks. The ability of social robots to move around, monitor the surrounding environment, record interactions with robots, and register the daily routines of users creates reduced personal privacy. The consequences of robots getting hacked is another critical issue that fears the end-users of such robots. In this regard, the importance of security to avoid robots being externally or maliciously controlled needs to be taken care of before operation. Eduard et al. [119] explained that in addition to these concerns, continuous human-robot interactions might eventually lead to reduced human–human interactions. The author points out that there is a lack of research studying the change in people’s attitudes and mental health when interacting with robots over time. The authors conclude that it is equally important to educate the population on the correct usage of robotic technologies.
The disinfection and cleaning robots that have become popular in the recent past to fight the pandemic have the biggest challenge to perceive unstructured environments. This is because such robots are mainly designed and tested for controlled environments. Even though the UV disinfection robots can cover large spaces within a limited time, those objects and surfaces that are out of sight of the UV radiations are less effectively disinfected. Therefore, it requires the operators to run the device several times through multiple locations to complete the process in each space. Another critical consideration is the distance of the surface to be disinfected from the emitter. As the distance increases, the energy of the UV radiations drastically reduces, thereby reducing the overall disinfection efficiency and increasing the disinfection time. Additionally, for effective disinfection, enough energy must be supplied to kill the micro-organisms. Different organisms require different emission energies for them to be killed [120]. Therefore, it is necessary to decide the emission energy and delivery time of UV radiations, considering the room size and objects in space.
Samala et al. [121] observed that the implementation of robotics and AI into the tourism sector brings about an initial excitement for the guests. However, the lack of proper comprehension and response delays from robots changes peoples’ perception and interest over time. Many chatbots are designed to answer direct and straightforward queries that primarily work on keywords to answer questions. Ivanov et al. [122] point out that replacing humans with robots ruins the guest experience as they lack emotions and human-level interactions. According to the financial perspective, the investment involved in purchasing and maintaining a robot is more than hiring a human staff. It is also required to hire skilled people to operate the robot, which is an additional burden to the tourism sector, as they will demand a higher salary.
The reliability, consistency, adaptability, and service life of robots are the other significant challenges seen among users. Many of these challenges require innovation and collaborative researches to solve them. The several benefits of robots fighting the pandemic encourage the researchers to bring resulting solutions to transform the facet of our lives from medical care to hospitality. Some solutions include developing efficient and portable energy storage devices, newer materials with tunable properties, and improved fabrication strategies to lower robot building and handling costs. The currently available energy sources such as Lead-acid, Ni-metal hydride, and Li-ion batteries should be replaced with next-generation technologies such as fuel cells, non-conventional energy sources, or supercapacitors. Considering the security and privacy norms with companion, social, or surveillance robots, it is necessary to obtain informed consent before data collection for a stipulated time. Similarly, the level of autonomy of service bots should be kept within limits and not override human decisions when lives are at stake, especially in hospitals. It is advisable to employ robots in realistic scenarios with well-defined policy implications, as seen in Tokku Special Zone for Robotics in Japan [123].
3.7. Limitations of drones
Drones had emerged as a new method to fight the COVID-19 pandemic. Even though drones have a wide range of applications, their practical implementation still faces certain limitations. The common factors limiting the drone’s capability include weather, limited payload capacity, and autonomy. Drones can only be used to service a limited area with a package of limited size and weight [124]. Lower delivery speed compared to air freight carriers also cause hindrance to its practicality. The terrain upon which the drone has to be also operated matters, as it is not easy to handle a drone in hilly regions compared to plains. Access to remote or far away places from the operator’s location may be tedious or even impossible. High endurance and highly sophisticated unmanned aerial systems are deployed for military purposes like the Reaper, or Predator UAVs (Unmanned Aerial Vehicle) of the United States defense forces are very expensive than manned helicopters. Thus, the capabilities of UAVs are limited by their cost to an extent. Personal data can be collected with the aid of UAVs, which can lead to a privacy breach. It may violate the citizens’ fundamental right to protect their privacy. In the U.S.A, questions had been already raised by privacy advocates, demanding warrants for the use of drones for surveillance [125]. Even under certain circumstances, these UAV’s can cause a threat to airplanes similar to the one that a bird can cause [124]. AI has to be used extensively integrated into modern-day drones for the fight against Covid-19. It requires special training with Covid databases, and creating proper predictive models may also be difficult as it lacks historical data [15].
4. Social media, television, and others
Effective health communication is considered as one of the significant factors of the fight against the COVID-19 pandemic. Once the COVID-19 pandemic was initially reported from Wuhan City, China, much misinformation started to flow to the commoner through various communication platforms, majorly through social media. People began to post their hypothetical analysis about the origin, specifications, and nature of the virus, spreading methods, prevention methods, and even genetic details. In the initial stage, the official scientific community was also in a dilemma to examine these hypotheses as the available scientific evidence was not enough. Simultaneously, online media started to spread news like, ‘the COVID-19 is a bioweapon invented by China to defeat other countries, and a Canadian virology laboratory developed the COVID-19 virus for studies, and the Chinese researchers had stolen them from the laboratory, and they got expelled because of this reason. A lot of fake news, like the ones mentioned above were being spread and even spread now regarding the various aspects of COVID-19. In this section, the role of social media platforms (such as the search engines, Twitter, and Facebook), television, WHO, and governmental initiatives are discussed.
4.1. Social media
During the end-December 2019, the general public and researchers worldwide started to write on social media about their hypotheses against the virus pandemic spreading in Wuhan City, China. But even in the last week of December 2019, the number of cases was not that much stabilized. In the initial phases, social media ignored it as a laboratory-confirmed case and reclassified them as the patients were also diagnosed with other clinical conditions. After the instances increased and reached a higher level of 72,000 positive cases, China changed its measures to a countrywide lockdown. Criticisms were started in social media after the death of Dr. Li Wenliang from COVID-19, who was the first to get arrested first for posting critical concerns on social media [126].
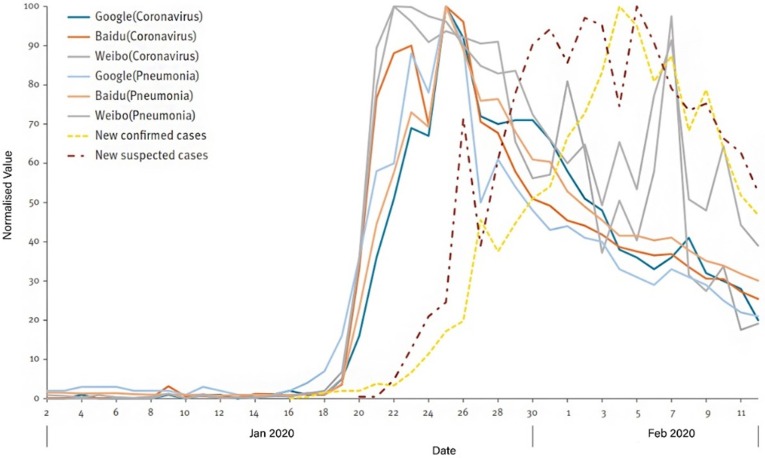
Researchers from China started retrospective analyses to forecast the possibility of the COVID-19 outbreak from social media posts and internet search data from January 2020 onwards [127]. Fig. 8 illustrates the daily trend data for search keywords ‘coronavirus’ and ‘pneumonia’ from various search engines in China for January and February 2020.
Fig. 8.
Daily search trends from various search engines in China for keywords coronavirus and pneumonia[127].
This investigation confirmed that a lag correlation exists between internet searches and daily lab-confirmed or suspected case numbers. The lag correlation showed an average of 10 days lag for lab-confirmed cases and seven days lag for suspected cases from the keyword searches. The possibilities of forecasting the spread using the search trends during epidemics were successfully established during previous influenza [128], Dengue [129], H1N1 influenza [130], Zika virus [131], Measles [132], and Middle-East Respiratory Syndrome [133].
Twitter is a widely used global platform for quick-short information sharing. The surveillance of trending tweets helped the authorities and policymakers arrive at decisions without many oppositions [134]. During the early stages of the COVID-19 pandemic, the first updates about the spreading were shared globally using tweets. A study conducted in the Middle-East has identified the topics with more tweeters from February 2nd to March 15th, 2020. Around 2.8 million tweets were identified with the keyword ‘corona,’ 2019-nCov’, and ‘COVID-19′ using twitter’s Application Programming Interface (API) and Python Tweepy library [135]. The study concluded that public health activities online and on the ground-level have increased to the next level during the early stages of this pandemic. The authorities were coming up with more disease surveillance by analyzing social media posts and fighting against false information.
Facebook is the next major social platform that has a direct impact on ordinary people. For example, in the last two decades, a movement named ‘anti-vaccination’ became popular among its users through groups, pages, and even profile posts. A study conducted by the Australian National University in 2017 collected and analyzed the depth of this movement among the users using various statistical models [136]. The study concluded that Facebook has a significant role in spreading such activities worldwide, even if most of the activists are from a small region of the world. An investigation of the outreach of posts made by public health organizations and their Facebook responses were reported with detailed information using the sentiment and emotion analysis of all COVID-19 related posts and comments.
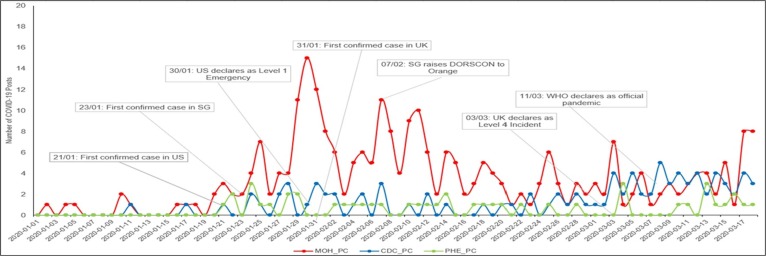
The data extraction from three public health authority pages; namely, the Ministry of Health (MOH) Singapore, Public Health England (PHE), and Centers for Disease Control and Prevention (CDC) of the United States during January 1st, 2020 to March 17th, 2020 for the analysis was done using the ‘Facepager’ tool [137]. The frequency of COVID-19 related posts done by these three public health authorities during the said period is shown in Fig. 9 . The investigation reported that among these three public health authorities, the MOH Singapore succeeded more in outreaching the information regarding pandemic COVID-19 than the others. As the COVID-19 situation has severe undesirable effects on the public’s mental health, a Facebook survey also reported the Taiwanese public’s mental health changes due to the COVID-19 related factors [138].
Fig. 9.
Frequency of COVID-19 posts done by the three public health authorities on Facebook [137].
The various impacts of the pandemic on public health were investigated with more importance to mental health. The descriptive analysis performed among 2031 respondents concluded that people with lower support from authorities were less stable with their mental health. Among them, sleep disturbances and suicidal thoughts were found to exist. The social distancing and the quarantine protocols also reduced mental health, as they become less social for a few weeks. In almost all countries, the public health department has taken counseling initiatives to the affected and ordinary people who are in trouble with the COVID-19 pandemic’s aftereffects.
4.2. Television
The medicine’s relationship with media in the COVID-19 pandemic situation has already undergone various investigations. The various official sources of information regarding the pandemic are updating continuously through the channels, enabling the public to get some authentic information for all related topics rather than the rumors spreading in social media. Due to the social distancing and the quarantine policies of prevention of COVID-19, the information through the television channels has become unavailable to some extent. The news channels followed a behavior that their statistics should go beyond the official counts. In order to make the public misbelieve that the channels give more accurate and early details than the government institutions. This behavior has made the channels provide unconfirmed spread data during the H1N1 pandemic lot before the official information [139]. In India, the need for credible health journalism to enhance communication possibilities between the health workers and journalists is having more importance in any pandemic situation, particularly during COVID-19 [140].
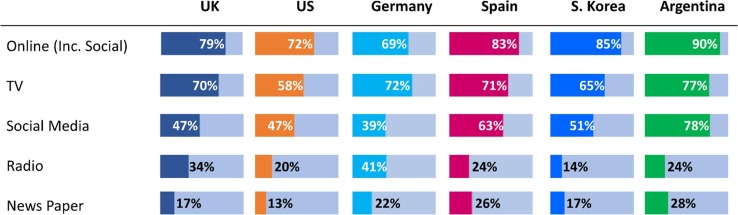
The responsibility of mass media is not getting fulfilled by spreading the news in a quick form. Still, they must give more importance to public health by conducting scientific reviews about passing information. In a detailed survey conducted by Oxford researchers, the role of different information-sharing platforms in fighting against the COVID-19 has been investigated with a sample space of people from six other countries [141]. The proportion of various sources used by the people for information gathering regarding COVID-19 is shown in Fig. 10 . The people from all these six countries showed that the people who rely on news media have higher authentic information about the people relying on other sources. Also, people from all six countries exhibited significant trust in WHO, other government authorities, doctors, scientists, and experts than the local politicians and public.
Fig. 10.
The proportion of various sources used by the people from six different countries to gather COVID-19 information [141]
4.3. Others
The widespread and non-controllable nature of COVID-19 has caused a shortage of necessities worldwide. Some of the essential mandatories include Personal Protective Equipment, such as face masks, shields, etc., especially for the healthcare workers. In this scenario, the utilization of 3-D printing technology plays a vital role in printing equipment at a relatively lower cost [142]. The 3-D printer can be used to fabricate low-cost disposable nasopharyngeal and oropharyngeal swab kits, respiration assisting gears, valves, etc. Another trend observed in industries includes transforming manually operated or semi-operated industries to complete automation [143]. This transformation reduces the direct human to human interactions and continues industrial procedures without the threat of the virus. Another threat is political leaders and celebrities who need special bodyguards or security while moving in public places. This problem can be solved using security robots equipped with modern technologies to maintain all possible crime risks under control [144].
4.4. Limitations of social media
Even though social media has played a vital role in sharing crucial official information regarding the prevention methods, institutional measures, and pandemic statistics, it has been reproached as the spreader of false news regarding the pandemic. Fake news is always fabricated information under circulation in social media, which contains misinformation that is not authentic.
Several investigations were reported, which predicts the various reasons for the spreading of false news. Human’ altruism’ was found as the most significant factor that enhances false news sharing [145]. This mentality enables them to share the information received by them with other persons in their concern, without inquiring about that news or subject's genuineness. The other attributes, unawareness, ignorance, attention-seeking, and political and demographical agendas, also play critical roles in false news sharing. One survey conducted among the primary and secondary students of Palestine reported the various potential negative impacts of social media in spreading the panic of the COVID-19 pandemic. Majority of them used Facebook to gather knowledge about the pandemic. The mental health and psychological and behavioral changes were analyzed, and around 78% of them were found adversely affected [146]. The female students were more panicked about the news of the pandemic.
Another survey analyzed the effects of misinformation being shared in the COVID-19 individual responses [147]. The average time shared by individuals on social media for the information gathering has been increased significantly due to the government policies of social distancing. The fake information spread about the pandemic has put individuals into psychological and mental distress or even into insomnia under worst conditions [148]. The study performed in a sample of 1078 young adults Iranians showed a result that was exactly in line with this general finding. The analysis also mentioned the importance of online campaigns to reduce people’s fear of COVID-19 and restore their psychological stability.
Meanwhile, the entire world is experiencing mental stress due to the misinformation being shared through social media. Some countries reported survey studies of COVID-19 humor campaigns conducted through social media to reduce mental stress. A survey reported in Jordan has coined the various effects of humor in peoples’ psychological well-being during the pandemic situation [149]. The study successfully demonstrated how humor could become a tool for mental relief in the COVID situation. Another investigation reported about the relationship between mental stress symptoms and social media usage during the pandemic situation confirmed their interdependency [150].
Through a detailed behavioral study of 4492 tweets posted during the pandemic time, investigators were able to identify successfully the interlinks between the fear developed through social media and the behavioral conditions such as loneliness [151]. Based on the criticisms aroused worldwide, most social media platforms have started their investigative measures to ensure the shared genuineness of the posts. They have begun to use artificial intelligence and machine learning-based algorithms for the processes of identification, assessment, warning, and denial of false spreading.
5. WHO and government initiatives
5.1. WHO
The conspiracy theories about the COVID-19 spread worldwide even more rapidly and efficiently than the actual virus because of previous scientific results' unavailability. After understanding the severity of the misinformation spreading worldwide, in the Munich Security Conference conducted in February 2020, the WHO Director-General Tedros Adhanom Ghebreyesus said, “We are not just fighting an epidemic: we are fighting an infodemic” [152]. In virtue of that situation, which started a campaign called ‘MythBusters’ and addressed around 30 prominent theories about COVID-19 spread worldwide [153]. Some of the posters developed by the ‘MythBusters’ team is illustrated in Fig. 11 . The team succeeded in finding misinformation and rumors widely spreading on social media platforms like Twitter, Facebook, TikTok, YouTube, Tencent, Pinterest, etc. After the WHO's initial warning, social media platforms started their filtration process to reduce the spreading of misinformation.
Fig. 11.
Some of the posters developed by the WHO ‘MythBusters’ team to fight misinformation [153].
To guide the public with authentic information, during the middle of 2020, WHO started a technical guidance page on their website [154]. They have included the official information under various categories like technical guidance publications, situation reports, media resources, public, technical guidance, travel advice, training exercises, strategy and planning, and COVID-19 supply chain system. Centers for disease control and prevention of the U.S department of health and human services have issued a public notice regarding the COVID-19 disease outbreak [155]. It provides authentic information regarding the do’s and don’ts the people should follow in spreading the information, public health authority messages, the behavior towards diseased, etc.
After numerous rigorous testing, many countries were come up with different types of vaccines. As they all have not got enough time to study the real-time aftereffects of the vaccine in the human body, the WHO has given Emergency Use Authorization (EUA) for only a few among the various types reported. The EUA license is supplied only based on three clinical test data phases and testing data regarding quality, safety, efficacy, and a risk management plan. Four major types of vaccines were reported from different biotech giants: Inactivated or weakened virus vaccines, protein-based vaccines, viral vector vaccines, and RNA or DNA vaccines [156].
Among the various, The Pfizer/BioNTech vaccine receives the WHO’s approval for emergency usage at first. Pfizer Inc. USA and BioNTech Germany, the globally known biotechnology companies, have combined their efforts to develop an mRNA-based vaccine for preventing the COVID-19 virus. The vaccine was reported safe to humans above 16 years of age and also needs to be taken in two shots with 21 days gap in between. The only challenge associated with the Pfizer/BioNTech vaccine is the ultra-cold chain requirement as it needs a low-temperature ambiance of −60 °C to −90 °C. This makes the logistics of the same challenging even after producing in bulk quantity [157]. The WHO’s EUA enables the countries to validate their vaccines and get approval for the supply to the others in need.
5.2. Governmental initiatives
Once after the COVID-19 pandemic onset, several hypotheses came up comparing the virus to a bioweapon, even though there is no evidence available with any country or agency to date. In virtue of the assumption of bioweapon, different countries were treated with fear at the beginning. But on the outset, the countries have gained enough fuel in all dimensions to defeat the pandemic. The primary step taken by them was to declare the nationwide lockdown. In India, the first lockdown was from March 25th, 2020, to April 14th, 2020. The second, third, and fourth phase lockdown phases were from April 15th, 2020 to May 3rd, 2020, May 4th, 2020 to May 17th, 2020, and May 18th, 2020 to May 31st, 2020. Likewise, almost all countries declared nationwide lockdown as the first measure to prevent the virus's spreading. Some of the institutional actions taken by different countries are reviewed here. Since China's first COVID-19 case was reported from Thailand, Malaysia has taken some stringent movement institutional control measures at first. Based on the hashtag of '#stay home,' the work from the home strategy was started. Many government and non-government organizations came up as front-liners as healthcare workers, volunteers, or even fundraisers. New hospitals, laboratories, and first-line treatment centers were set up with high bed capacity, and around 38 modern medical societies were set up by the Ministry of Health (MoH) [158]. A supporting package of RM 20.0 billion was issued in February 2020 as an immediate help, followed by a RM 250 billion package as a stimulus for the financial strategy and a 6-month moratorium period for all the loans. Along with the aids for the industrial sector, a package of RM 600 million was allocated for the MoH.
The United States is one of the most affected countries, even though the state administrations made appreciable efforts to reduce the impact from the very beginning itself. They have formulated policies in four different classes: measures for preventing the spreading, facility development, shift of administrative requirements, and statistical reporting of COVID-19 data. From the beginning of March 2020, around 14 states issued institutional restrictions to all public facilities. Among the various states, Arizona, North Carolina, Michigan, Connecticut, Minnesota, and Maryland were in the front line to set up the prevention measures [159]. They came across a rapidly updating policy strategy to overcome the current issues and account for the pandemic's changing scenario, and become more successful in implementing the policies. The next most affected area is the African continent. They lack the health care measures and facilities to administrate the treatment guidelines according to the standards. Even though the Malawi country in south-eastern Africa made some effective measures to prevent the spread of the virus, the people were only ready to comply with the measures if the expenses are low since their economic background is not that much. The government measures were initially concentrated to prevent the public gathering, stay at home, and washing hands campaigns. They found that people’s compliance with the standards improved once the cases increased and costs for measures were reduced [160].
The Asian country Mongolia, situated between China and Russia, made some early policy measures to forecast its severity. Policies were framed up in personal protection and prevention of spreading in the first stage, leading them to a complete shutdown. That includes the suspension of all activities, gatherings, and strict surveillance over the public [161]. The measures helped them to avoid a COVID-19 confirmed death until July 2020. In the Australian continent, the surge of COVID-19 positive cases was not as huge as the rest of the world. This flattening of the positive curve was made possible only by adopting strict health and social policies. The consumer organizations joined shoulder-to-shoulder with the health professional workers in framing such measures to make the policies ‘life-friendly’ [162]. The measures started with closing all the international and interstate borders, institutions, industries, and all public gatherings, followed by strict containment zone restrictions. In India, even the four phases of lockdowns were recorded to be effective. After the unlocking stages started and the international borders were opened, the positive case’s curve took a steep increase. The authorities found that the current control measures are not enough to prevent spreading. Based on the daily spread data, the researchers formulated new sophisticated mathematical models for forecasting, and the authorities started to frame the policies based on it [163]. To regain the country’s development, which was idle for the past few months, the lockdown declarations were restructured. Now, the locations with high symptomatic infection percentages are only needed to be declared as containment.
6. Summary and future directions
The unprecedented COVID-19 outbreak worldwide has burdened the healthcare sector in curbing the spread of infection, providing alternative remedies to fight the epidemiological traits, and the quest for possible vaccine/drug discovery. The cumulative records of infected individuals and mortality rates pointed out that even developed countries like the US, China, and Russia crumbled to tackle the spread and find a cure. An epidemic that was declared a pandemic within few weeks of its discovery is challenging even after ten months for the scientific community. With the discovery of a cure/vaccine at bay, the primary focus across the globe in the current scenario is to prevent the spread and reduce the mortality rate by adopting preventive measures such as the use of public face masks, handwashing, social distancing, isolation, lockdown/quarantine measures, and stricter surveillance of the general public.
This review conclusively showed that the nations that flattened the COVID-19 outbreak (in terms of active cases and mortality rate) had adopted wide use of digital technologies (such as mobile applications, robots, drones, social media platforms, television, and associated technologies) in the fight against the pandemic in policymaking and response. Countries worldwide have quickly deployed these technologies in the healthcare, communication, logistics, tourism, and hospitality sectors. It is also worth pointing out that COVID-19 has been a catalyst in highlighting the potential of digital technologies in various aspects and not limited to planning and control but to showcase their robustness and flexibility to be integrated with existing and developing technologies.
The notable merits of adoption of these digital technologies in minimizing the widespread of COVID-19 as reviewed from the literature considered in this study were:
-
(a)
Mobile applications introduced for contact tracing, remote assistance, isolation monitoring, syndromic surveillance, information sharing, and communication support, quarantine enforcement, mental health, and geofencing proved to be a great success in connecting the world on a single platform, and especially beneficial for the public in the remote locations of the world. These portable, freely available, and simple technology-aid to share relevant information from authentic sources like the WHO and health ministries with up-to-date statistics of the pandemic played a significant role in imparting awareness and educating the public worldwide.
-
(b)
Robots and drones were used as an excellent platform to minimize the risk or avoid direct contact between the healthcare/frontline officials and infected or suspected individuals. These technologies were deployed for primary diagnosis and screening tests, collect, transfer, and test oropharyngeal swab or other body fluid samples, disinfection, and provide physical and mental support to patients under quarantine or isolation, all by adhering to governmental protocols. Thereby speeding up the process and make available the healthcare/frontline workers to do other critical jobs.
-
(c)
Social media platforms and television had both positive and negative attributes in this pandemic era. In the initial phase of the pandemic, social media and television witnessed a surge in the number of allegations, controversies, and sharing of false information concerning COVID-19. However, after the interventions from the Governments and the WHO, these platforms were used to spread awareness, educate the public about the epidemiological traits and symptoms, information on lockdown/quarantine and social distancing norms, and to share the personal experience of recovered COVID-19 victims, thereby reduce the fear and urge the public to practice and adopt the preventive measures in day-to-day life.
-
(d)
The WHO and Governments played a crucial role across the globe to curtail the spread of COVID-19. With the limited information on the novel coronavirus, Governments and the WHO had to rely on strict and unconventional measures to prevent the person-to-person transmission by adopting lockdown with relaxation at various stages, enforcing stringent isolation/quarantine rules, travel restrictions, making mandatory measures such as the use of face masks, handwashing, maintaining personal hygiene, and social distancing norms. Though these regulations were criticized by the general public worldwide, studies have shown that the enforcement of such stringent rules drastically reduced transmission of COVID-19.
Although the digital technologies showed great promise in the fight against COVID-19, there are many allegations and end-user concerns related to data privacy, the associated agencies, and possible false positive and negative occurrences. Also, a major share of the apps introduced by Governments were made mandatory, and the public had no choice to opt-out of it. Enforcing international policies and regulations to ensure data protection, surveillance of spreading false information on social media platforms, and providing the flexibility of choice to the user would promote faith and the use of digital technology to its full potential. In regard to robots and drones, the major drawback associated with them is the frequency of charging required for the operation. Though it shows a great promise, intelligent power management algorithms, devising auxiliary unconventional power sources, multi-linguistic attributes, and flexibility in performing multiple complex tasks with ease would offer more reliability and acceptance. Governments and policymakers should also adopt relevant measures to promote emerging modern technological research and advancements, educate the younger generation to utilize these advancements for the greater good, and integrate them in combating similar epidemics or preparing for yet another pandemic.
CRediT authorship contribution statement
Mervin Joe Thomas: Formal analysis, Data curation, Writing - original draft. Vishnu Lal: Formal analysis, Data curation, Writing - original draft. Ajith Kurian Baby: Formal analysis, Data curation, Writing - original draft. Muhammad Rabeeh VP: Formal analysis, Data curation, Writing - original draft. Alosh James: Formal analysis, Data curation, Writing - original draft. Arun K. Raj: Conceptualization, Methodology, Formal analysis, Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G., Hu Y., Tao Z.W., Tian J.H., Pei Y.Y., Yuan M.L., Zhang Y.L., Dai F.H., Liu Y., Wang Q.M., Zheng J.J., Xu L., Holmes E.C., Zhang Y.Z. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danis K., Epaulard O., Bénet T., Gaymard A., Campoy S., Botelho-Nevers E., Bouscambert-Duchamp M., Spaccaferri G., Ader F., Mailles A., Boudalaa Z., Tolsma V., Berra J., Vaux S., Forestier E., Landelle C., Fougere E., Thabuis A., Berthelot P., Veil R., Levy-Bruhl D., Chidiac C., Lina B., Coignard B., Saura C. Cluster of Coronavirus Disease 2019 (COVID-19) in the French Alps. Clin. Infect. Dis. 2020;71(2020):825–832. doi: 10.1093/cid/ciaa424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.P.H. O’Neill, T. Ryan-Mosley, B. Johnson, A flood of coronavirus apps are tracking us. Now it’s time to keep track of them. | MIT Technology Review, (2020). https://www.technologyreview.com/2020/05/07/1000961/launching-mittr-covid-tracing-tracker/ (accessed October 11, 2020).
- 4.Weekly epidemiological update - 9 February 2021, (n.d.). https://www.who.int/publications/m/item/weekly-epidemiological-update---9-february-2021 (accessed March 15, 2021).
- 5.Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19 — studies needed. N. Engl. J. Med. 2020;382:1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 6.Wesolowski A., Buckee C.O., Bengtsson L., Wetter E., Lu X., Tatem A.J. Commentary: containing the ebola outbreak - the potential and challenge of mobile network data. PLoS Curr. 2014 doi: 10.1371/currents.outbreaks.0177e7fcf52217b8b634376e2f3efc5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quick J., Loman N.J., Duraffour S., Simpson J.T., Severi E., Cowley L., Bore J.A., Koundouno R., Dudas G., Mikhail A., Ouédraogo N., Afrough B., Bah A., Baum J.H.J., Becker-Ziaja B., Boettcher J.P., Cabeza-Cabrerizo M., Camino-Sánchez Á., Carter L.L., Doerrbecker J., Enkirch T., Garciá-Dorival I., Hetzelt N., Hinzmann J., Holm T., Kafetzopoulou L.E., Koropogui M., Kosgey A., Kuisma E., Logue C.H., Mazzarelli A., Meisel S., Mertens M., Michel J., Ngabo D., Nitzsche K., Pallasch E., Patrono L.V., Portmann J., Repits J.G., Rickett N.Y., Sachse A., Singethan K., Vitoriano I., Yemanaberhan R.L., Zekeng E.G., Racine T., Bello A., Sall A.A., Faye O., Faye O., Magassouba N., Williams C.V., Amburgey V., Winona L., Davis E., Gerlach J., Washington F., Monteil V., Jourdain M., Bererd M., Camara A., Somlare H., Camara A., Gerard M., Bado G., Baillet B., Delaune D., Nebie K.Y., Diarra A., Savane Y., Pallawo R.B., Gutierrez G.J., Milhano N., Roger I., Williams C.J., Yattara F., Lewandowski K., Taylor J., Rachwal P., Turner D.J., Pollakis G., Hiscox J.A., Matthews D.A., O’Shea M.K., Johnston A.M.D., Wilson D., Hutley E., Smit E., Di Caro A., Wolfel R., Stoecker K., Fleischmann E., Gabriel M., Weller S.A., Koivogui L., Diallo B., Keita S., Rambaut A., Formenty P., Gunther S., Carroll M.W. Real-time, portable genome sequencing for Ebola surveillance. Nature. 2016;530:228–232. doi: 10.1038/nature16996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leung G.M., Medley A.J., Ho L.M., Chau P., Wong I.O.L., Thach T.Q., Ghani A.C., Donnelly C.A., Fraser C., Riley S., Ferguson N.M., Anderson R.M., Tsang T., Leung P.Y., Wong V., Chan J.C.K., Tsui E., Lo S.V., Lam T.H. The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients. Ann. Intern. Med. 2004;141:662–673. doi: 10.7326/0003-4819-141-9-200411020-00006. [DOI] [PubMed] [Google Scholar]
- 9.WHO Coronavirus Disease (COVID-19) Dashboard, World Heal. Organ. (2020). https://covid19.who.int/table (accessed January 24, 2021).
- 10.App stores saw record 204 billion app downloads in 2019, consumer spend of $120 billion | TechCrunch, (n.d.). https://techcrunch.com/2020/01/15/app-stores-saw-record-204-billion-app-downloads-in-2019-consumer-spend-of-120-billion/ (accessed October 11, 2020).
- 11.The Mobile Economy 2020. GSM Association. 2020, (n.d.). https://www.gsma.com/mobileeconomy/wp-content/uploads/2020/03/GSMA_MobileEconomy2020_Global (accessed October 11, 2020).
- 12.Ram N., Gray D. Mass surveillance in the age of COVID-19. J. Law Biosci. 2020;7:1–17. doi: 10.1093/jlb/lsaa023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed N., Michelin R.A., Xue W., Ruj S., Malaney R., Kanhere S.S., Seneviratne A., Hu W., Janicke H., Jha S.K. A Survey of COVID-19 contact tracing apps. IEEE Access. 2020;8:134577–134601. doi: 10.1109/ACCESS.2020.3010226. [DOI] [Google Scholar]
- 14.Rowe F., Ngwenyama O., Richet J.L. Contact-tracing apps and alienation in the age of COVID-19. Eur. J. Inf. Syst. 2020;00:1–18. doi: 10.1080/0960085X.2020.1803155. [DOI] [Google Scholar]
- 15.Whitelaw S., Mamas M.A., Topol E., Van Spall H.G.C. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit. Heal. 2020;2:e435–e440. doi: 10.1016/S2589-7500(20)30142-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.COVID-19 vaccines, (n.d.). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed January 26, 2021).
- 17.Chen H., Xu W., Paris C., Reeson A., Li X. Social distance and SARS memory: impact on the public awareness of 2019 novel coronavirus (COVID-19) outbreak. MedRxiv. 2020;2020 doi: 10.1101/2020.03.11.20033688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lau H., Khosrawipour V., Kocbach P., Mikolajczyk A., Schubert J., Bania J., Khosrawipour T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 2020;27 doi: 10.1093/jtm/taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atalan A. Is the lockdown important to prevent the COVID-9 pandemic? Effects on psychology, environment and economy-perspective. Ann. Med. Surg. 2020;56:38–42. doi: 10.1016/j.amsu.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Urbaczewski A., Lee Y.J. Information Technology and the pandemic: a preliminary multinational analysis of the impact of mobile tracking technology on the COVID-19 contagion control. Eur. J. Inf. Syst. 2020;00:1–10. doi: 10.1080/0960085X.2020.1802358. [DOI] [Google Scholar]
- 21.Scopus, (n.d.). https://www.scopus.com/ (accessed October 12, 2020).
- 22.C. Stokel-Walker, Can mobile contact-tracing apps help lift lockdown?, BBC Futur. (2020). https://www.bbc.com/future/article/20200415-covid-19-could-bluetooth-contact-tracing-end-lockdown-early (accessed October 13, 2020).
- 23.Radanliev P., De Roure D., Walton R., Van Kleek M., Montalvo R.M., Santos O., Maddox L.T., Cannady S. COVID-19 what have we learned? The rise of social machines and connected devices in pandemic management following the concepts of predictive, preventive and personalized medicine. EPMA J. 2020;11:311–332. doi: 10.1007/s13167-020-00218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO, Nipah Virus Outbreak in Kerala, Surveill. Risk Assess. (2020) 1. https://www.who.int/southeastasia/outbreaks-and-emergencies/health-emergency-information-risk-assessment/surveillance-and-risk-assessment/nipah-virus-outbreak-in-kerala (accessed October 13, 2020).
- 25.R. Raskar, I. Schunemann, R. Barbar, K. Vilcans, J. Gray, P. Vepakomma, S. Kapa, A. Nuzzo, R. Gupta, A. Berke, D. Greenwood, C. Keegan, S. Kanaparti, R. Beaudry, D. Stansbury, B.B. Arcila, R. Kanaparti, V. Pamplona, F.M. Benedetti, A. Clough, R. Das, K. Jain, K. Louisy, G. Nadeau, V. Pamplona, S. Penrod, Y. Rajaee, A. Singh, G. Storm, J. Werner, Apps Gone Rogue: Maintaining Personal Privacy in an Epidemic, (2020). http://arxiv.org/abs/2003.08567.
- 26.Dar A.B., Lone A.H., Zahoor S., Khan A.A., Naaz R. Applicability of mobile contact tracing in fighting pandemic (COVID-19): issues, challenges and solutions. Comput. Sci. Rev. 2020;38 doi: 10.1016/j.cosrev.2020.100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coronavirus tracking apps: How are countries monitoring infections? | News | DW | 27.04.2020, (n.d.). https://www.dw.com/en/coronavirus-tracking-apps-how-are-countries-monitoring-infections/a-53254234 (accessed October 13, 2020).
- 28.Brooks L.L.Z., Johnston J. Use of mobile phone apps for contact tracing to control the COVID-19 pandemic a literature review. Jm. 2012:1–55. [Google Scholar]
- 29.Wright J.H., Caudill R. Remote treatment delivery in response to the COVID-19 Pandemic. Psychother. Psychosom. 2020;89:130–132. doi: 10.1159/000507376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Islam M.N., Islam I., Munim K.M., Islam A.K.M.N. A review on the mobile applications developed for COVID-19: an exploratory analysis. IEEE Access. 2020;8:145601–145610. doi: 10.1109/ACCESS.2020.3015102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taiwo O., Ezugwu A.E. Smart healthcare support for remote patient monitoring during covid-19 quarantine. Informatics Med. Unlocked. 2020;20 doi: 10.1016/j.imu.2020.100428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Commonwealth Centre for Digital Health (CWCDH) release COVID Shield app ~ ECHAlliance, (n.d.). https://echalliance.com/commonwealth-centre-for-digital-health-cwcdh-response-to-covid-19-pandemic-covid-shield/ (accessed October 13, 2020).
- 33.Information sharing during the coronavirus (coV) outbreak - The Nuffield Council on Bioethics, (n.d.). https://www.nuffieldbioethics.org/news/information-sharing-during-the-coronavirus-cov-outbreak (accessed October 13, 2020).
- 34.Liu P.L., Huang L.V. Digital disinformation about COVID-19 and the third-person effect: examining the channel differences and negative emotional outcomes, cyberpsychology. Behav. Soc. Netw. 2020;00:1–5. doi: 10.1089/cyber.2020.0363. [DOI] [PubMed] [Google Scholar]
- 35.Le H.T., Nguyen D.N., Beydoun A.S., Le X.T.T., Nguyen T.T., Pham Q.T., Ta N.T.K., Nguyen Q.T., Nguyen A.N., Hoang M.T., Vu L.G., Tran B.X., Latkin C.A., Ho C.S.H., Ho R.C.M. Demand for health information on COVID-19 among Vietnamese. Int. J. Environ. Res. Public Health. 2020;17:1–12. doi: 10.3390/ijerph17124377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kerala govt launches mobile app for details of COVID-19 | coronavirus infection in Kerala| coronavirus app| Gok Direct| mobile app for coronavirus, (n.d.). https://english.mathrubhumi.com/technology/tech-news/kerala-govt-launches-mobile-app-for-details-of-covid-19-1.4608234 (accessed October 13, 2020).
- 37.National Informatics Centre, Aarogya Setu, NIC - Gov. India. (2020). https://aarogyasetu.gov.in/ (accessed October 13, 2020).
- 38.Coronavirus Quarantine Monitoring Application & Health Crisis Management Platform, 2544. https://octopus-app.com/wp-content/uploads/2019/05/Octopus-Quarantine-app-and-Health-Crisis-Response-Platform.pdf (accessed October 13, 2020).
- 39.Quarantine watch: Karnataka uses apps to keep track of people under watch | Business Standard News, (n.d.). https://www.business-standard.com/article/technology/quarantine-watch-karnataka-uses-apps-to-keep-track-of-people-under-watch-120040201641_1.html (accessed October 13, 2020).
- 40.Coronavirus: TN tracks movements of home quarantine people through a mobile app | Deccan Herald, (n.d.). https://www.deccanherald.com/national/south/coronavirus-tn-tracks-movements-of-home-quarantine-people-through-a-mobile-app-817853.html (accessed October 13, 2020).
- 41.Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Azarang A., Pakyurek M., Giroux C., Nordahl T.E., Yellowlees P. Information technologies: an augmentation to post-traumatic stress disorder treatment among trauma survivors. Telemed. e-Health. 2019;25:263–271. doi: 10.1089/tmj.2018.0068. [DOI] [PubMed] [Google Scholar]
- 43.Marshall J.M., Dunstan D.A., Bartik W. The role of digital mental health resources to treat trauma symptoms in australia during COVID-19. Psychol. Trauma Theory, Res. Pract Policy. 2020;12:269–271. doi: 10.1037/tra0000627. [DOI] [PubMed] [Google Scholar]
- 44.Brahmi N., Singh P., Sohal M., Sawhney R.S. Psychological trauma among the healthcare professionals dealing with COVID-19. Asian J. Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.UNC ties up with Google to launch mental health app for front-line workers | FierceHealthcare, (n.d.). https://www.fiercehealthcare.com/tech/unc-ties-up-google-to-launch-mental-health-app-for-frontline-workers (accessed October 13, 2020).
- 46.Reyes A.T. A mindfulness mobile app for traumatized COVID-19 healthcare workers and recovered patients: a response to “the use of digital applications and COVID-19”. Community Ment. Health J. 2020;56:1204–1205. doi: 10.1007/s10597-020-00690-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Will digital mental health solutions thrive after Covid-19? - Medical Technology | Issue 30 | August 2020, (2020). https://medical-technology.nridigital.com/medical_technology_aug20/digital_mental_health_solutions (accessed October 13, 2020).
- 48.Ponzo S., Morelli D., Kawadler J.M., Hemmings N.R., Bird G., Plans D. Efficacy of the digital therapeutic mobile app biobase to reduce stress and improve mental well-being among university students: Randomized controlled trial. JMIR MHealth UHealth. 2020;8 doi: 10.2196/17767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.A NY state of mind - Headspace, (2020). https://www.headspace.com/ny (accessed October 13, 2020).
- 50.Care for Your Coronavirus Anxiety, (2020). https://www.virusanxiety.com/ (accessed October 13, 2020).
- 51.An Online COVID-19 Self-assessment System, (n.d.). https://preworkscreen.com/app (accessed October 13, 2020).
- 52.TeamSense - COVID-19 Symptom Screening for Employees, (2020). https://www.teamsense.com/ (accessed October 13, 2020).
- 53.Hammoudi K., Cabani A., Benhabiles H., Melkemi M. Validating the correct wearing of protection mask by taking a selfie: design of a mobile application “CheckYourMask” to limit the spread of COVID-19. C. - Comput. Model. Eng. Sci. 2020;124:1049–1059. doi: 10.32604/cmes.2020.011663. [DOI] [Google Scholar]
- 54.Dubov A., Shoptawb S. The value and ethics of using technology to contain the COVID-19 epidemic. Am. J. Bioeth. 2020;20:W7–W11. doi: 10.1080/15265161.2020.1764136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Morley J., Cowls J., Taddeo M., Floridi L. Ethical guidelines for SARS-CoV-2 digital tracking and tracing systems. SSRN Electron. J. 2020:1–6. doi: 10.2139/ssrn.3582550. [DOI] [Google Scholar]
- 56.Patrick Howell O’Neillarchive page, No, coronavirus apps don’t need 60% adoption to be effective | MIT Technology Review, MIT Technol. Rev. (2020). https://www.technologyreview.com/2020/06/05/1002775/covid-apps-effective-at-less-than-60-percent-download/ (accessed January 28, 2021).
- 57.Klar R., Lanzerath D. The ethics of COVID-19 tracking apps – challenges and voluntariness. Res. Ethics. 2020;16:1–9. doi: 10.1177/1747016120943622. [DOI] [Google Scholar]
- 58.Hale K., Capra S., Bauer J. A framework to assist health professionals in recommending high-quality apps for supporting chronic disease self-management: Illustrative assessment of type 2 diabetes apps. JMIR MHealth UHealth. 2015;3 doi: 10.2196/mhealth.4532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Keep health workers safe to keep patients safe: WHO, World Heal. Organ. (2020). https://www.who.int/news-room/detail/17-09-2020-keep-health-workers-safe-to-keep-patients-safe-who (accessed October 12, 2020).
- 60.Lanza F., Seidita V., Chella A. Agents and robots for collaborating and supporting physicians in healthcare scenarios. J. Biomed. Inform. 2020;108 doi: 10.1016/j.jbi.2020.103483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Konert A., Smereka J., Szarpak L. The use of drones in emergency medicine: practical and legal aspects. Emerg. Med. Int. 2019;2019:1–5. doi: 10.1155/2019/3589792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.E. Saffari, A. Meghdari, B. Vazirnezhad, M. Alemi, Ava (A social robot): Design and performance of a robotic hearing apparatus, Lect. Notes Comput. Sci. (Including Subser. Lect. Notes Artif. Intell. Lect. Notes Bioinformatics). 9388 LNCS (2015) 440–450. 10.1007/978-3-319-25554-5_44. [DOI]
- 63.Ackerman Evan. How Diligent’s Robots Are Making a Difference in Texas Hospitals. IEEE Spectr. 2020 https://spectrum.ieee.org/automaton/robotics/medical-robots/how-diligents-robots-are-making-a-difference-in-texas-hospitals (accessed October 12, 2020) [Google Scholar]
- 64.Angela Betsaida B, Robots can play a major role in COVID-19 battle, News Med. Life Sci. (2020). https://www.news-medical.net/news/20200402/Robots-can-play-a-major-role-in-COVID-19-battle.aspx (accessed October 12, 2020).
- 65.Petruzzi G., De Virgilio A., Pichi B., Mazzola F., Zocchi J., Mercante G., Spriano G., Pellini R. COVID-19: Nasal and oropharyngeal swab. Head Neck. 2020;42:1303–1304. doi: 10.1002/hed.26212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Junwei Yang, Timothy Reuter, 3 ways China is using drones to fight coronavirus, World Econ. Forum. (2020). https://www.weforum.org/agenda/2020/03/three-ways-china-is-using-drones-to-fight-coronavirus/ (accessed October 12, 2020).
- 67.Angurala M., Bala M., Bamber S.S., Kaur R., Singh P. An internet of things assisted drone based approach to reduce rapid spread of COVID-19. J. Saf. Sci. Resil. 2020;1:31–35. doi: 10.1016/j.jnlssr.2020.06.011. [DOI] [Google Scholar]
- 68.Kimmig R., Verheijen R.H.M., Rudnicki M. Robot assisted surgery during the COVID-19 pandemic, especially for gynecological cancer: a statement of the society of european robotic gynaecological surgery (SERGS) J. Gynecol. Oncol. 2020;31:1–7. doi: 10.3802/jgo.2020.31.e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zemmar A., Lozano A.M., Nelson B.J. The rise of robots in surgical environments during COVID-19. Nat. Mach. Intell. 2020;2:566–572. doi: 10.1038/s42256-020-00238-2. [DOI] [Google Scholar]
- 70.Yang G.Z., Nelson B.J., Murphy R.R., Choset H., Christensen H., Collins S.H., Dario P., Goldberg K., Ikuta K., Jacobstein N., Kragic D., Taylor R.H., McNutt M. Combating COVID-19-The role of robotics in managing public health and infectious diseases. Sci. Robot. 2020;5:1–3. doi: 10.1126/scirobotics.abb5589. [DOI] [PubMed] [Google Scholar]
- 71.Atrax VTOL Unmanned Aerial Vehicle-Airforce Technology, (2020). https://www.airforce-technology.com/projects/atrax-vtol-unmanned-aerial-vehicle/attachment/atrax-vtol-unmanned-aerial-vehicle2/ (accessed October 14, 2020).
- 72.Ava - ROBOTS: Your Guide to the World of Robotics, IEEE Spectr. (2018). https://robots.ieee.org/robots/ava/ (accessed October 12, 2020).
- 73.Moxi Robot, (n.d.). https://diligentrobots.com/moxi (accessed October 12, 2020).
- 74.Rosser J.C., Vignesh V., Terwilliger B.A., Parker B.C. Surgical and medical applications of drones: a comprehensive review. JSLS J. Soc. Laparoendosc. Surg. 2018;22 doi: 10.4293/JSLS.2018.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shilpa Nair Anand, COVID-19: Kerala Police uses drones to keep an eye on those who flout the lockdown, The Hindu. (2020). https://www.thehindu.com/society/kerala-polices-project-eagle-eye-uses-close-to-350-drones-to-track-those-flouting-the-rules-of-lockdown/article31331170.ece (accessed October 12, 2020).
- 76.Mohammed M.N., Hazairin N.A., Al-Zubaidi S., Sairah A.K., Mustapha S., Yusuf E. Toward a novel design for coronavirus detection and diagnosis system using iot based drone technology. Int. J. Psychosoc. Rehabil. 2020;24:2287–2295. doi: 10.37200/IJPR/V24I7/PR270220. [DOI] [Google Scholar]
- 77.A.J. Sathyamoorthy, U. Patel, Y.A. Savle, M. Paul, D. Manocha, COVID-Robot: Monitoring Social Distancing Constraints in Crowded Scenarios, ArXiv Prepr. (2020) 1–11. http://arxiv.org/abs/2008.06585. [DOI] [PMC free article] [PubMed]
- 78.T. Ai, Z. Yang, H. Hou, C. Zhan, C. Chen, W. Lv, Q. Tao, Z. Sun, L. Xia, Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases, Radiology. 296 (2020) E32–E40. 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed]
- 79.Uddin M.I., Shah S.A.A., Al-Khasawneh M.A. A novel deep convolutional neural network model to monitor people following guidelines to avoid COVID-19. J. Sensors. 2020;2020 doi: 10.1155/2020/8856801. [DOI] [Google Scholar]
- 80.C. Butt, J. Gill, D. Chun, B.A. Babu, Deep learning system to screen coronavirus disease 2019 pneumonia, Appl. Intell. 22 (2020) 1–7. 10.1007/s10489-020-01714-3. [DOI] [PMC free article] [PubMed]
- 81.Rehm G.B., Woo S.H., Chen X.L., Kuhn B.T., Cortes-Puch I., Anderson N.R., Adams J.Y., Chuah C.N. Leveraging IoTs and machine learning for patient diagnosis and ventilation management in the intensive care unit. IEEE Pervasive Comput. 2020;19:68–78. doi: 10.1109/MPRV.2020.2986767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA - J. Am. Med. Assoc. 2020;323:1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 83.Hou H., Lv W., Tao Q., Hospital T., Company J.T., Ai T., Hospital T., Wuhan T., Hospital T., Butt C., Gill J., Chun D., Babu B.A., Zhao J., Zhang Y., He X., Xie P. Artificial intelligence distinguishes COVID-19 from community acquired pneumonia on chest CT Lin. Radiology. 2020;296:1–5. doi: 10.1148/radiol.2020200905. [DOI] [PubMed] [Google Scholar]
- 84.Rundo L., Pirrone R., Vitabile S., Sala E., Gambino O. Recent advances of HCI in decision-making tasks for optimized clinical workflows and precision medicine. J. Biomed. Inform. 2020;108 doi: 10.1016/j.jbi.2020.103479. [DOI] [PubMed] [Google Scholar]
- 85.Topol E.J. High-performance medicine: the convergence of human and artificial intelligence. Nat. Med. 2019;25:44–56. doi: 10.1038/s41591-018-0300-7. [DOI] [PubMed] [Google Scholar]
- 86.Han C., Rundo L., Murao K., Nemoto T., Nakayama H. Bridging the gap between AI and healthcare sides: towards developing clinically relevant AI-powered diagnosis systems. IFIP Adv. Inf. Commun. Technol. 584 IFIP. 2020:320–333. doi: 10.1007/978-3-030-49186-4_27. [DOI] [Google Scholar]
- 87.Ye R., Zhou X., Shao F., Xiong L., Hong J., Huang H., Tong W., Wang J., Chen S., Cui A., Peng C., Zhao Y., Chen L. Feasibility of a 5G-based robot-assisted remote ultrasound system for cardiopulmonary assessment of patients with COVID-19. Chest. 2020:1–12. doi: 10.1016/j.chest.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang Z., Wang G., Huang B., Xiong Z., Hong Q., Wu H., Yi P., Jiang K., Wang N., Pei Y., Chen H., Miao Y., Huang Z., Liang J. Masked face recognition dataset and application. Electr. Eng. Syst. Sci. 2020;4:1–3. http://arxiv.org/abs/2003.09093 [Google Scholar]
- 89.Couch D.L., Robinson P., Komesaroff P.A. COVID-19—extending surveillance and the panopticon. J. Bioeth. Inq. 2020 doi: 10.1007/s11673-020-10036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tavakoli M., Carriere J., Torabi A. Robotics, smart wearable technologies, and autonomous intelligent systems for healthcare during the COVID-19 pandemic: an analysis of the state of the art and future vision. Adv. Intell. Syst. 2020;2:2000071. doi: 10.1002/aisy.202000071. [DOI] [Google Scholar]
- 91.Ananya Varma, Delhi police gets tech upgrade; “Thermal Corona Combat Head” can detect temp from 5-10m, Repub. World. (2020). https://www.republicworld.com/india-news/city-news/delhi-police-uses-thermal-corona-combat-headgear-to-screen-people.html (accessed October 12, 2020).
- 92.Pacharawan Chanprakon, T. Sae-oung, Treesukon, P. H, W. P, An Ultra-Violet sterilistaion robot for disinfection, IEEE Trans. Robot. Autom. Trans. Robot. 5 (2019) 44–47.
- 93.Allen Kim, Atlanta Falcons stadium using drones to sanitize arena, CNN. (2020). https://edition.cnn.com/2020/10/01/tech/drone-stadium-sanitize-spt-trnd/index.html (accessed October 12, 2020).
- 94.Intelligent robots help to fight viruses, Siemens. (2020). https://new.siemens.com/global/en/company/stories/industry/intelligentrobotics-siemens-aucma.html (accessed October 12, 2020).
- 95.UVD Robots®, Blue Ocean Robot. (2020). https://www.uvd-robots.com/ (accessed October 12, 2020).
- 96.Rich Stinson, Tonya Hope, San Antonio International is first airport in the world to purchase and deploy virus and bacteria defeating Xenex LightStrike robot, City San Antonio - Off. City Website. (2020) Accessed on October 12, 2020. https://www.sanantonio.gov/gpa/News/ArtMID/24373/ArticleID/19377/San-Antonio-International-is-first-airport-in-the-world-to-purchase-and-deploy-virus-and-bacteria-defeating-Xenex-LightStrike-robot (accessed October 12, 2020).
- 97.Indian Robotics Solution launches Corona Combat Drone to fight COVID-19, ETGovernment.Com. (2020). https://government.economictimes.indiatimes.com/news/technology/indian-robotics-solution-launches-corona-combat-drone-to-fight-covid-19/75077517 (accessed October 12, 2020).
- 98.Feng Q.C., Wang X. Design of disinfection robot for livestock breeding. Procedia Comput. Sci. 2020;166:310–314. doi: 10.1016/j.procs.2020.02.093. [DOI] [Google Scholar]
- 99.Odekerken-Schröder G., Mele C., Russo-Spena T., Mahr D., Ruggiero A. Mitigating loneliness with companion robots in the COVID-19 pandemic and beyond: an integrative framework and research agenda. J. Serv. Manag. 2020 doi: 10.1108/JOSM-05-2020-0148. [DOI] [Google Scholar]
- 100.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Henkel A.P., Čaić M., Blaurock M., Okan M. Robotic transformative service research: deploying social robots for consumer well-being during COVID-19 and beyond. J. Serv. Manag. 2020 doi: 10.1108/JOSM-05-2020-0145. [DOI] [Google Scholar]
- 102.S.O. Adalgeirsson, C. Breazeal, MeBot: A robotic platform for socially embodied presence, 5th ACM/IEEE Int. Conf. Human-Robot Interact. HRI 2010. (2010) 15–22. 10.1145/1734454.1734467. [DOI]
- 103.Flandorfer P. Population ageing and socially assistive robots for elderly persons: the importance of sociodemographic factors for user acceptance. Int. J. Popul. Res. 2012;2012:1–13. doi: 10.1155/2012/829835. [DOI] [Google Scholar]
- 104.Melendez-Fernandez F., Galindo C., Gonzalez-Jimenez J. A web-based solution for robotic telepresence. Int. J. Adv. Robot. Syst. 2017;14:1–19. doi: 10.1177/1729881417743738. [DOI] [Google Scholar]
- 105.NATASHA MEAH, Robot to deliver meals, medication to Covid-19 patients at Alexandra Hospital to reduce exposure of healthcare workers, TODAYonline. (2020). https://www.todayonline.com/singapore/robot-deliver-meals-medication-covid-19-patients-alexandra-hospital-reduce-exposure (accessed October 12, 2020).
- 106.Dwi Dowellin Neue Ankunft Kleine Mini Lustige Linie Follower Roboter Für Kinder, Alibaba.Com. (2020). https://german.alibaba.com/product-detail/dwi-dowellin-new-arrival-small-mini-funny-line-follower-robot-for-kids-62054131383.html (accessed October 12, 2020).
- 107.Pandey A.K., Gelin R. A mass-produced sociable humanoid robot: pepper: the first machine of its kind. IEEE Robot. Autom. Mag. 2018;25:40–48. doi: 10.1109/MRA.2018.2833157. [DOI] [Google Scholar]
- 108.Y. Shimosasa, J. Kanemoto, H. Horii, T. Ariki, F. K, A. Kimura, Security Service System with Autonomous Guard Robot Ii, in: 2000 26th Annu. Conf. IEEE Ind. Electron. Soc. IECON 2000, 2000, pp. 405–409. 10.1109/IECON.2000.973184. [DOI]
- 109.Airport Robots Market | 2020-2027, Mordor Intell. (2020). https://www.mordorintelligence.com/industry-reports/airport-robots-market (accessed October 12, 2020).
- 110.Amit Tripathi, Central Railways launches robotic “Captain Arjun” for screening of passengers for COVID-19 and surveillance in Pune, Zee News. (2020). https://zeenews.india.com/india/central-railways-launches-robotic-captain-arjun-for-screening-of-passengers-for-covid-19-and-surveillance-in-pune-2289625.html (accessed October 12, 2020).
- 111.Jiang H., Ren X. Comparative analysis of drones and riders in on-demand meal delivery based on prospect theory. Discret. Dyn. Nat. Soc. 2020;2020 doi: 10.1155/2020/9237689. [DOI] [Google Scholar]
- 112.Kellermann R., Biehle T., Fischer L. Drones for parcel and passenger transportation: a literature review. Transp. Res. Interdiscip. Perspect. 2020;4 doi: 10.1016/j.trip.2019.100088. [DOI] [Google Scholar]
- 113.Hilary George Parkin, Home delivery helped China manage coronavirus, but the US must catch up., Vox.Com. (2020). https://www.vox.com/the-goods/2020/3/25/21193817/home-delivery-china-coronavirus-us-alibaba-amazon (accessed October 12, 2020).
- 114.Assad-Uz-Zaman M., Islam M.R., Rahman M.H., Wang Y.C., McGonigle E. Kinect controlled NAO robot for telerehabilitation. J. Intell. Syst. 2020;30:224–239. doi: 10.1515/jisys-2019-0126. [DOI] [Google Scholar]
- 115.Mitra - Invento Robotics, (n.d.). https://mitrarobot.com/ (accessed October 12, 2020).
- 116.Crew B. Worth the cost? A closer look at the da Vinci robot’s impact on prostate cancer surgery. Nature. 2020;580:S5–S7. doi: 10.1038/d41586-020-01037-w. [DOI] [Google Scholar]
- 117.Alemzadeh H., Raman J., Leveson N., Kalbarczyk Z., Iyer R.K. Adverse events in robotic surgery: a retrospective study of 14 years of fda data. PLoS One. 2016;11 doi: 10.1371/journal.pone.0151470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.A. Balaji, J. Mithil, J.G. J, Design and analysis of universal gripper for robotics applications, in: IOP Conf. Ser. Mater. Sci. Eng., 2021. 10.1088/1757-899X/1012/1/012006. [DOI]
- 119.Fosch Villaronga E., Tamò-Larrieux A., Lutz C. Did I tell you my new therapist is a robot? Ethical, legal, and societal issues of healthcare and therapeutic robots. SSRN Electron. J. 2018 doi: 10.2139/ssrn.3267832. [DOI] [Google Scholar]
- 120.Germicidal UV Dose UV Irradiation Dosage Table, Am. Air Water Inc. (n.d.). https://www.americanairandwater.com/uv-facts/uv-dosage.htm (accessed January 14, 2021).
- 121.Samala N., Katkam B.S., Bellamkonda R.S., Rodriguez R.V. Impact of AI and robotics in the tourism sector: a critical insight. J. Tour. Futur. 2020 doi: 10.1108/JTF-07-2019-0065. [DOI] [Google Scholar]
- 122.S. Ivanov, F. Seyitoğlu, M. Markova, Hotel managers’ perceptions towards the use of robots: a mixed-methods approach, Springer Berlin Heidelberg, 2020. 10.1007/s40558-020-00187-x. [DOI]
- 123.Weng Y.H., Sugahara Y., Hashimoto K., Takanishi A. Intersection of “Tokku” special zone, robots, and the law: a case study on legal impacts to humanoid robots. Int. J. Soc. Robot. 2015;7:841–857. doi: 10.1007/s12369-015-0287-x. [DOI] [Google Scholar]
- 124.Euchi J. Do drones have a realistic place in a pandemic fight for delivering medical supplies in healthcare systems problems? Chinese J. Aeronaut. 2020 doi: 10.1016/j.cja.2020.06.006. [DOI] [Google Scholar]
- 125.G. McNeal, Drones and aerial surveillance: Considerations for legislatures, Brookings Proj. Civ. Robot. (2014). https://www.brookings.edu/research/drones-and-aerial-surveillance-considerations-for-legislatures/ (accessed January 15, 2021).
- 126.Sonja J.C.S., Rasmussen A. MD, MS, Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- Ann Oncol. 2020:19–21. [Google Scholar]
- 127.Li C., Chen L.J., Chen X., Zhang M., Pang C.P., Chen H. Retrospective analysis of the possibility of predicting the COVID-19 outbreak from Internet searches and social media data, China. Eurosurveillance. 2020;25(2020):1–5. doi: 10.2807/1560-7917.ES.2020.25.10.2000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Polgreen P.M., Chen Y., Pennock D.M., Nelson F.D. Using internet searches for influenza surveillance. Clin. Infect. Dis. 2008;47:1443–1448. doi: 10.1086/593098. [DOI] [PubMed] [Google Scholar]
- 129.C. de A. Marques-Toledo, C.M. Degener, L. Vinhal, G. Coelho, W. Meira, C.T. Codeço, M.M. Teixeira, Dengue prediction by the web: Tweets are a useful tool for estimating and forecasting Dengue at country and city level, PLoS Negl. Trop. Dis. 11 (2017) 1–20. 10.1371/journal.pntd.0005729. [DOI] [PMC free article] [PubMed]
- 130.N. Wilson, K. Mason, M. Tobias, M. Peacey, Q.S. Huang, M. Baker, Interpreting “ Google Flu Trends” Data for Pandemic H1N1 Infuenza: The New Zealand Experience, Rapid Commun. 14 (2009) 25–27. www.eurosurveillance.org. [PubMed]
- 131.Majumder M.S., Santillana M., Mekaru S.R., McGinnis D.P., Khan K., Brownstein J.S. Utilizing nontraditional data sources for near real-time estimation of transmission dynamics during the 2015–2016 Colombian zika virus disease outbreak. JMIR Public Heal. Surveill. 2016;2 doi: 10.2196/publichealth.5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Santangelo O.E., Provenzano S., Piazza D., Giordano D., Calamusa G., Firenze A. Digital epidemiology: assessment of measles infection through google trends mechanism in Italy. Ann. Di Ig. 2019;31:385–391. doi: 10.7416/ai.2019.2300. [DOI] [PubMed] [Google Scholar]
- 133.Shin S.Y., Seo D.W., An J., Kwak H., Kim S.H., Gwack J., Jo M.W. High correlation of Middle East respiratory syndrome spread with Google search and Twitter trends in Korea. Sci. Rep. 2016;6:1–7. doi: 10.1038/srep32920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Jordan S.E., Hovet S.E., Fung I.C.H., Liang H., Fu K.W., Tse Z.T.H. Using twitter for public health surveillance from monitoring and prediction to public response. Data. 2019;4:1–20. doi: 10.3390/data4010006. [DOI] [Google Scholar]
- 135.Abd-Alrazaq A., Alhuwail D., Househ M., Hai M., Shah Z. Top concerns of tweeters during the COVID-19 pandemic: a surveillance study. J. Med. Internet Res. 2020;22:1–9. doi: 10.2196/19016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Smith N., Graham T. Mapping the anti-vaccination movement on Facebook. Inf. Commun. Soc. 2019;22:1310–1327. doi: 10.1080/1369118X.2017.1418406. [DOI] [Google Scholar]
- 137.Raamkumar A.S., Tan S.G., Wee H.L. Measuring the outreach efforts of public health authorities and the public response on facebook during the COVID-19 pandemic in early 2020: cross-country comparison. J. Med. Internet Res. 2020;22 doi: 10.2196/19334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Li D.J., Ko N.Y., Chen Y.L., Wang P.W., Chang Y.P., Yen C.F., Lu W.H. Covid-19-related factors associated with sleep disturbance and suicidal thoughts among the taiwanese public: A facebook survey. Int. J. Environ. Res. Public Health. 2020;17:1–12. doi: 10.3390/ijerph17124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Reintjes R., Das E., Klemm C., Richardus J.H., Keßler V., Ahmad A. “Pandemic public health paradox”: Time series analysis of the 2009/10 influenza A/H1N1 epidemiology, media attention, risk perception and public reactions in 5 European countries. PLoS One. 2016;11:1–14. doi: 10.1371/journal.pone.0151258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sharma D.C., Pathak A., Chaurasia R.N., Joshi D., Singh R.K., Mishra V.N. Fighting infodemic: Need for robust health journalism in India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:1445–1447. doi: 10.1016/j.dsx.2020.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.R.K. Nielsen, R. Fletcher, N. Newman, J.S. Brennen, P.N. Howard, Navigating the “Infodemic”: How People in Six Countries Access and Rate News and Information about Coronavirus, Reuters Inst. Study Journal. 01 (2020) 1–34. https://bit.ly/2VZ4h9R%0Ahttps://reutersinstitute.politics.ox.ac.uk/sites/default/files/2020-04/Navigating the Coronavirus Infodemic FINAL.pdf%0Ahttps://reutersinstitute.politics.ox.ac.uk/infodemic-how-people-six-countries-access-and-rate-news-and-informa.
- 142.Tsikala Vafea M., Atalla E., Georgakas J., Shehadeh F., Mylona E.K., Kalligeros M., Mylonakis E. Emerging technologies for use in the study, diagnosis, and treatment of patients with COVID-19. Cell. Mol. Bioeng. 2020;13:249–257. doi: 10.1007/s12195-020-00629-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Motamedi S., Wang P., Zhang T., Chan C.Y. Acceptance of full driving automation: personally owned and shared-use concepts. Hum. Factors. 2020;62:288–309. doi: 10.1177/0018720819870658. [DOI] [PubMed] [Google Scholar]
- 144.Outdoor Security Robot_Security Series_Pangolin Robot, (2020). https://en.csjbot.com/content/105/1301.html (accessed October 12, 2020).
- 145.Apuke O.D., Omar B. Fake news and COVID-19: modelling the predictors of fake news sharing among social media users. Telemat. Informatics. 2021;56 doi: 10.1016/j.tele.2020.101475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Radwan E., Radwan A., Radwan W. The role of social media in spreading panic among primary and secondary school students during the COVID-19 pandemic: an online questionnaire study from the Gaza Strip. Palestine, Heliyon. 2020;6 doi: 10.1016/j.heliyon.2020.e05807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Barua Z., Barua S., Aktar S., Kabir N., Li M. Effects of misinformation on COVID-19 individual responses and recommendations for resilience of disastrous consequences of misinformation. Prog. Disaster Sci. 2020;8 doi: 10.1016/j.pdisas.2020.100119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Lin C.Y., Broström A., Griffiths M.D., Pakpour A.H. Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interv. 2020;21 doi: 10.1016/j.invent.2020.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Hussein A.T., Aljamili L.N. COVID-19 humor in Jordanian social media: A socio-semiotic approach. Heliyon. 2020;6 doi: 10.1016/j.heliyon.2020.e05696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Brailovskaia J., Cosci F., Mansueto G., Margraf J. The relationship between social media use, stress symptoms and burden caused by Coronavirus (Covid-19) in Germany and Italy: a cross-sectional and longitudinal investigation. J. Affect. Disord. Reports. 2021;3 doi: 10.1016/j.jadr.2020.100067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Koh J.X., Liew T.M. How loneliness is talked about in social media during COVID-19 pandemic: text mining of 4,492 Twitter feeds. J. Psychiatr. Res. 2020 doi: 10.1016/j.jpsychires.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.WHO Director Tedros Adhanom to address tech conference on coronavirus pandemic | News | DW | 20.05.2020, (2020). https://www.dw.com/en/who-director-tedros-adhanom-to-address-tech-conference-on-coronavirus-pandemic/a-53510711 (accessed October 13, 2020).
- 153.WHO-Coronavirus disease (COVID-19) advice for the public: Mythbusters, (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters (accessed October 13, 2020).
- 154.Technical guidance, (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance (accessed October 13, 2020).
- 155.Cerc, CS315829-A CERC in an Infectious Disease Outbreak, (2019) 315829.
- 156.WHO Team Coronavirus disease (COVID-19): Vaccines. World Heal. Organ. 2020;53 https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines (accessed March 22, 2021) [Google Scholar]
- 157.WHO TEAM, WHO issues its first emergency use validation for a COVID-19 vaccine and emphasizes need for equitable global access, World Heal. Organ. (n.d.). https://www.who.int/news/item/31-12-2020-who-issues-its-first-emergency-use-validation-for-a-covid-19-vaccine-and-emphasizes-need-for-equitable-global-access (accessed March 22, 2021).
- 158.Shah A.U.M., Safri S.N.A., Thevadas R., Noordin N.K., Rahman A.A., Sekawi Z., Ideris A., Sultan M.T.H. COVID-19 outbreak in Malaysia: actions taken by the Malaysian government. Int. J. Infect. Dis. 2020;97:108–116. doi: 10.1016/j.ijid.2020.05.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Chen A.T., Ryskina K.L., Jung H.Y. Long-term care, residential facilities, and COVID-19: an overview of federal and state policy responses. J. Am. Med. Dir. Assoc. 2020;21:1186–1190. doi: 10.1016/j.jamda.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kao K., Lust E., Dulani B., Ferree K.E., Harris A.S., Metheney E. The ABCs of Covid-19 prevention in Malawi: authority, benefits, and costs of compliance. World Dev. 2021;137 doi: 10.1016/j.worlddev.2020.105167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Erkhembayar R., Dickinson E., Badarch D., Narula I., Warburton D., Thomas G.N., Ochir C., Manaseki-Holland S. Early policy actions and emergency response to the COVID-19 pandemic in Mongolia: experiences and challenges. Lancet Glob. Heal. 2020;8:e1234–e1241. doi: 10.1016/S2214-109X(20)30295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Andrikopoulos S., Johnson G. The Australian response to the COVID-19 pandemic and diabetes – Lessons learned. Diabetes Res. Clin. Pract. 2020;165 doi: 10.1016/j.diabres.2020.108246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Sardar T., Nadim S.S., Rana S., Chattopadhyay J. Assessment of lockdown effect in some states and overall India: a predictive mathematical study on COVID-19 outbreak. Chaos, Solitons Fractals. 2020;139 doi: 10.1016/j.chaos.2020.110078. [DOI] [PMC free article] [PubMed] [Google Scholar]