Abstract
Context:
Fertility preservation (FP) is necessary for cancer patients who develop infertility due to chemotherapy and radiotherapy. In Indonesia, many systematic steps and long-term continued actions must be taken to establish FP units since there has been an increasing incidence of cancer among people under 45 years old.
Aims:
This study aimed at a comprehensive evaluation on the awareness and practices of health-care providers (HCPs) toward FP.
Settings and Design:
This was a descriptive cross-sectional study.
Subjects and Methods:
A validated nationwide online survey was completed by 160 HCPs as a representative sample from 11 provinces in 2017 that provide medical care to cancer patients at hospitals or clinics.
Statistical Analysis Used:
Descriptive statistics, analysis of variance, logistic regression, and Pearson correlation tests were used for the statistical analysis.
Results:
Respondents were specialists (59.4%) and other HCPs (40.6%). Around 60% of the HCPs who performed cancer therapies already discussed the fertility issues with their patients. Meanwhile, the HCPs (60.7%) also tended not to consult and refer their patients to fertility experts (P < 0.05). However, those who discussed the risk of infertility with patients tended to consult with and refer them to a fertility consultant for further FP procedure as the follow-up for their discussions (odds ratio = 8.98, confidence interval 95%, P < 0.05).
Conclusions:
In Indonesia, FP awareness of the HCPs who performed cancer therapy was high. Nevertheless, attitudes to refer patients to fertility experts for possible FP management still need to be improved.
KEYWORDS: Attitude, awareness, fertility preservation, health-care providers
INTRODUCTION
The advanced management of cancer is known to increase the 5-year relative survival rate, however, it may cause the loss of fertility for young cancer survivors.[1,2] Hence, the American Society of Clinical Oncology (ASCO) in 2018 recommended that all cancer patients of reproductive age should be informed about the possibility of infertility, and attending physicians should discuss available fertility preservation (FP) options, as well as refer patients to reproductive specialists prior to cancer treatment.[3,4,5] Since the referral system for FP in Indonesia has not been well-established, this study aimed to evaluate the awareness and practices of both specialists and other health-care providers (HCPs) toward FP.[6]
SUBJECTS AND METHODS
This descriptive cross-sectional study was conducted in 2017 and data were collected using a nationwide online questionnaire survey, named “Oncologic Attention and Perception of Cancer Patients on the Preservation of Fertility Before Cancer Therapy,” distributed in 11 provinces in Indonesia including Aceh, Riau, West Java, Central Java, East Java, Jakarta, Bali, West Nusa Tenggara, South Kalimantan, South Sulawesi, and Jayapura. As a representative sample, these study sites are located from the most western parts until the most eastern islands of Indonesia reflecting the whole archipelago of Indonesia, including some islands recognized as the largest provinces with good quality of health care in Indonesia. Purposive sampling method was conducted to HCPs related to oncology, especially specialists who are members of the Indonesian specialists' associations, such as (1) Himpunan Onkologi Ginekologi Indonesia (HOGI) – gynaecologists; (2) Ikatan Dokter Anak Indonesia – Hematologi Onkologi (IDAI) – pediatrician; (3) Perhimpunan Hematologi Onkologi Medik Penyakit Dalam Indonesia (PERHOMPEDIN) – internists; (4) Perhimpunan Dokter Spesialis Bedah Onkologi (PERABOI) – specialists surgeon and (5) Perhimpunan Onkologi Radiasi Indonesia (PORI) - radiologists; and (6) other healthcare providers: midwives, nurses, general practitioners and embryologists.
The sample size was calculated using the formula below:
(Zc/p(1-p))/d2
Z = Standard normal variant (at 5% type of error or P < 0.05, which is 1.96)
P = expected proportion in population based on previous study
D = absolute error (5%)
Sample size = (1.962/0.15 [1 − 0.15])/0.052 = 148
The inclusion criteria were specialists, especially members of Indonesian specialists' associations, who agreed to be included in this research by completing the online questionnaire and willing to be interviewed, and clinicians and other HCPs who work in public hospitals since we aimed to compare the oncologists' and the other HCPs' knowledge and attitudes related to the FP issue. The work length experience was ignored.
This study had been approved by the Medical and Health Research Ethics Committee of the Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada No. KE/FK/0748/EC/2017 and had permission from the Department of Education and Research, Sardjito Hospital, Indonesia. Written informed consent was obtained from all participants before starting the study. The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
The respondents did not receive any direct supervision on completing the questionnaire. Therefore, the opportunity for literature searching to answer the questions regarding the knowledge of the specialists toward FP might have led to bias.
Data analysis was performed using SPSS version 20 (IBM Corp., Chicago, Illinois, USA) software package for quantitative and qualitative methods. Analyses included descriptive statistics, analysis of variance (ANOVA), logistic regression, and Pearson correlation tests. Statistical level of significance was set at P < 0.05 with 95% confidence interval (CI).
RESULTS
A total of 400 questionnaires were delivered and 160 were returned. Out of 160 respondents, 95 specialists and 65 other HCPs finished the survey questionnaires (response rate of 40%).
Demographic data
The average age of the other HCP respondents was 25–34 years old (40%, n = 26). Around 81.1% of the specialists and other HCPs are working on Java island (n = 77) and the rest of them (18.9%) are working outside of Java island (n = 18). Most of the respondents are between 35 and 44 years old (40%, n = 38). Most of them have never attended any FP seminars/workshops before the data were collected (77.5%, n = 124). The majority of the patients were women (53.7%, n = 51) between 36 and 44 years old (41.1%, n = 39). Complete data of the demographic characteristics are provided in Table 1.
Table 1.
Respondents’ demographic data
| Category | Specialist, n (%) | Other healthcare providers, n (%) |
|---|---|---|
| Total respondents (n=160) | 95 (59.4) | 65 (40.6) |
| Location of work | ||
| Java | 77 (81.1) | 48 (73.84) |
| Outside Java | 18 (18.9) | 17 (26.15) |
| Age | ||
| 18-34 | 14 (14.7) | 44 (67.7) |
| 35-54 | 74 (77.9) | 8 (12.3) |
| 55-64 | 4 (4.2) | |
| ≥65 | 3 (2.1) |
Awareness of respondents about the risk of infertility after cancer therapy
Most of respondents who prescribed chemotherapy have known about the moderate-to-high risk of gonadotoxicity involved in treatments with cisplatin and cyclophosphamide. Related to cyclophosphamide administration, oncologists have significantly more awareness compared to other HCPs regarding its high risk of gonadotoxicity (58.8% vs. 40.38%; ANOVA test, P < 0.05).
Data in Figure 1 show that most of the respondents are highly aware of what techniques of FP should be done in cancer patients with certain conditions as described in the questionnaire. These data also provide information that oocyte cryopreservation is the main (72.94%) FP technique known by the respondents followed by ovarian tissue cryopreservation 37.65% and embryo cryopreservation (23.35%), whereas testicle tissue cryopreservation, sperm cryopreservation, gonadal shielding, ovarian transposition, and GnRH agonist administration were unfamiliar for them.
Figure 1.
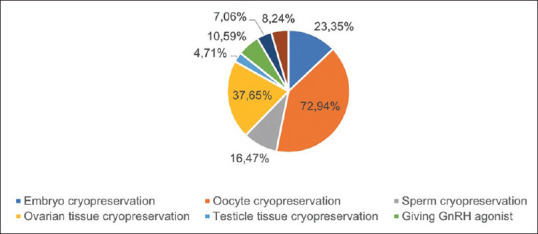
Fertility preservation techniques that are very familiar among respondents are oocyte cryopreservation 72.94%, followed by ovarian tissue cryopreservation 37.65%, embryo cryopreservation 23.35%, and sperm cryopreservation 16.47%. The four remaining methods were unfamiliar to the respondents
Attitude of respondents toward fertility preservation
The percentage of respondents who prescribe chemoradiotherapy and always or usually discuss the fertility issue to their patients was higher compared to respondents who rarely or never discuss it with their patients (60.70%; P < 0.05) [Figure 2]. Nevertheless, only a small proportion of the HCPs (39.30%) consult with and refer the patients to the fertility experts (P < 0.05). However, respondents who discussed the risk of infertility with their patients tended to consult fertility experts for more comprehensive management including FP options (odds ratio = 8.98, 95% CI; P > 0.05). In addition, written information regarding gonadotoxicity of the chemotherapeutic agents was seldomly (32.10%) given to the patients (ANOVA, P < 0.05).
Figure 2.
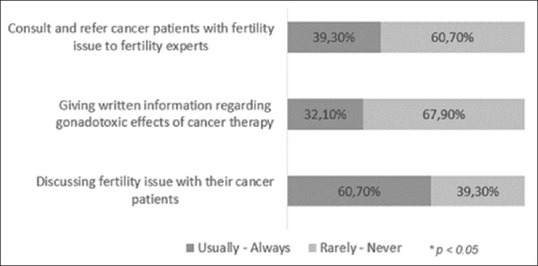
The majority (60.70%) of the respondent discuss fertility issue with their cancer patients, however only a few of them (39.30%) consult with and refer the patients to the fertility experts. Written information regarding gonadotoxicity of the chemotherapeutic agents was rarely (32.10%) given to the patients. (ANOVA, p< 0.05)
Most of the respondents agreed that the counseling on FP should be started for cancer patients in the reproductive age who plan to receive high-risk chemoradiotherapy, compared to that in an earlier age (i.e., the child and teenage groups) (84.55% vs. 30.88%: ANOVA test, P < 0.05).
Related to FP options, many reasons would be considered before specialists who prescribe chemoradiotherapy to offer FP techniques to their high-risk patients. Most of the specialists (38.82%) consider that age is the most important factor to be considered before discussing the FP issue with their cancer patients. In addition, around 10% of the specialists would start the discussion about fertility issues only if their patients have a good prognosis. Moreover, having extra time for discussion (1.18%) was not one of the main reasons considered by specialists to offer FP to their patients [Figure 3].
Figure 3.
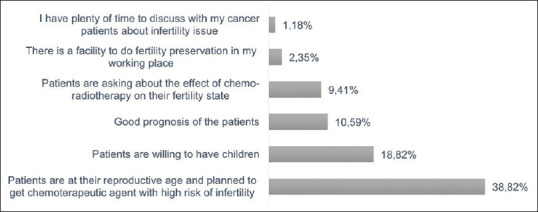
Some of the respondents (38.82%) considered to start offering fertility preservation only if the patients are in reproductive age, willing to have children and have good prognosis. Only a small percentage (1.18%) of them admitted that they only would offer FP if they have enough time for discussion
DISCUSSION
To date, the awareness regarding FP for cancer patients is increasing significantly. In Asia, Japan, Korea, and India have standard protocols and policies including a nationwide referral system for optimum FP application.[6] However, one study in China showed that most of oncologists never informed their patients about FP and only a few know correct methods and institutions for FP.[7,8] In Indonesia, FP options have been recently considered by reproductive HCPs; however, there have been no surveys addressing specialists' awareness and attitudes toward FP for cancer patients. This research is the first study in Indonesia that reports the findings of a nationwide survey of Indonesian specialists and other HCPs regarding their awareness and attitudes toward FP in cancer patients.
Fertility preservation awareness
Our findings indicate that most of the specialists have been aware of the risks regarding the gonadotoxic therapy. However, the other HCP respondents know regarding the risk of cyclophosphamide toward fertility. In addition, the results on the choice of FP options showed that most of the HCPs were well familiar with the oocyte cryopreservation, yet few of them know about ovarian tissue cryopreservation. In fact, ovarian tissue cryopreservation presently is the only FP method available for children.[9] Health care providers in Indonesia should be more aware of various options of FP since different cancer origins and treatment regimens carry different fertility risks and various options of FP based on cancer patients' conditions.[10] Specialists and other HCPs should know that the choices recommended in the guidelines include a wide variety of options that include sperm cryopreservation, hormonal gonadoprotection, testicular tissue cryopreservation, re-implantation or grafting which are recommended for male patients, as well as embryo cryopreservation, unfertilized oocyte cryopreservation, ovarian transposition, conservative gynecologic surgery, ovarian suppression, ovarian tissue cryopreservation, and transplantation which are recommended for adult women patients.[9] Our study showed that oocyte cryopreservation is the most known FP option by specialists and HCPs. This is a different result from another study in Indonesia that found GnRH agonist is the most known option for FP.[11] This discrepancy might be due to the different population samples of the study, because in the other study, the respondents were only obstetricians and gynecologists, and not various HCPs.
Fertility preservation attitude
This study found positive attitude toward FP in more than half of the respondents, especially specialists were already discussing the fertility issue related to the risk of chemotherapy to their patients, although they did not provide any written information. In addition, the more specialist and other HCPs discussed the risk of infertility after cancer therapy, the more likely they consulted with and referred their patients to the fertility experts for further FP management. Multiple studies in a review indicated that oncologists' knowledge barriers can inhibit a discussion about FP with a newly diagnosed cancer patient of childbearing age.[12] Two key knowledge barriers often faced by oncologists are knowledge of where to refer patients and knowledge of FP treatment options.[12] One study confirmed that close communication between oncology specialists and reproductive specialists is necessary to be encouraged in order to give early intervention and ensure future reproductive success.[10]
A systematic literature review by Vindrola-Padros et al.[13] reported across studies that five main factors influence HCPs' discussion of FP with young cancer patients: (1) HCPs' knowledge; (2) HCPs' sense of comfort; (3) patient factors (i.e., sexual maturity, prognosis, partnership status, and whether or not they initiate the conversation); (4) parent factors (i.e., HCPs' perceptions of the extent of their involvement); and (5) availability of educational materials.
However, in the current study, the age of the patients mostly influences the HCPs to offer the options of FP. The most preferred age to offer FP options would be adolescence and reproductive age. Suhag et al.[14] also emphasized to provide information about the risk of infertility and possible interventions to maintain the reproductive potential to these groups at the time of diagnosis. The reasons are because cancer-related infertility often comes as a surprise to young survivors, whereas a number of them still have a strong desire to have children in the future. In addition, a study in Jakarta asserted that reproductive functions are more influenced by biological age as shown by the decline of AMH serum levels in women between 34 and 35 years old.[14] Therefore, offering FP options to patients <35 years old would be very beneficial. However, in this study, most of the respondents still did not agree to offer FP options earlier to children and teenagers. This result was also inconsistent with the updated ASCO 2018 guidelines which recommend the option of ovarian tissue cryopreservation as a viable FP approach for children.[9]
In our study, the patient at the reproductive age is considered to be at the best time to start FP discussion. Another study in India produced a FP guideline for Asians in which the specialists must provide information about the risks of infertility and possible interventions to maintain the reproductive potential to all young adult patients and their parents at the time of diagnosis.[10] In addition, most of the guidelines in oncology and reproductive medicine also emphasize the importance of communicating FP options to young patients with cancer since a recent study found patient concerns about future fertility ranked second only to questions about mortality.[10]
It has been recommended in the ASCO clinical practice guidelines that the primary role of HCPs in FP is to be prepared to discuss infertility issues resulting from chemotherapy as soon as possible after cancer diagnosis and before any treatment is started.[9] Patients interested in fertility should also be referred, as well as those who are ambivalent or uncertain in FP including adults and children to reproductive specialists as soon as possible.[9] Although addressing potential fertility loss may be overwhelming for patients newly diagnosed with cancer and their families, multiple studies suggest that failure to confront the possibility can cause regret and distress to cancer survivors and significantly impact their quality of life.[13]
The information about FP is better delivered with both oral and written information. In addition, comprehensive cancer-specific fertility information for patients is also currently available online (e.g., from National Comprehensive Cancer Network-NCCN). Without the provision of written information, the quality of the information will vary and might not be standardized as the information available through NCCN. Moreover, accurate and up-to-date written information would help patients to better understand the issues involved and help them to make a more informed choice from the available options.[3]
The discussion about infertility issues is best done before the schedule for chemotherapy is formulated. Surprisingly, in a qualitative study, survivors of adolescent cancer were more likely to recall discussions of possible infertility not at diagnosis but after treatment had already begun. Several recent qualitative studies with adults and pediatricians suggest that several factors are responsible for this behavior, including lack of knowledge, uncertainty about the success of FP methods, and language/cultural barriers.[15] Recent studies in Japan and Indonesia found that physicians who had better knowledge scores and positive attitudes toward FP were more likely to discuss potential fertility issues with cancer patients.[11,16]
Our study showed that lack of awareness due to lack of knowledge highly influences HCPs' behavior to discuss FP and refer their patients to the fertility experts. It indicated that HCPs in Indonesia need training and thorough guidelines so that the FP discussion would be more appropriate. This conclusion was in line with the results of a study in India that stated the concept of early referral followed by FP in young cancer patients should be included in the teaching curriculum of oncology residents, and moreover, all countries should have clear-cut guidelines regarding FP and must enforce strict compliance.[6] For example, in Asia, Japan, Korea, India, and China have established their own society in the Organization for FP,6 whereas in Indonesia, initiatives to create FERTI-protect teams have been initiated and is an on-going process, but still, presently, the referral system has not been well established.[6] Ultimately, there is a need to establish accurate written information and offer current advice about FP options to the cancer patients as standard practice in Indonesia as outlined in ASCO clinical guidelines. There is a great need to establish a national oncofertility team and having universal protocols for the FP referral system is fundamental to meeting these needs.
CONCLUSIONS
In Indonesia, fertility preservation awareness of the healthcare providers who performed cancer therapy was high. Nevertheless, attitudes to refer patients to fertility experts for possible fertility preservation management still need to be improved.
Financial support and sponsorship
This research was funded by the Public Grant Funding (Hibah Dana Masyarakat), Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada 2017. This joint publication was funded and facilitated by the World Class Professor program of Directorate General of Higher Education, Ministry of Research, Technology and Higher Education, Indonesia, 2018.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Regina Arumsari who helped to distribute questionaire. Hindun Wildani Wahab who helped to distribute questionaire. Erik C. Hookom who provided professional proof reading services.
REFERENCES
- 1.Morgan S, Anderson RA, Gourley C, Wallace WH, Spears N. Cancer statistics. Hum Reprod Update. 2013;30:1–11. doi: 10.1093/humupd/dms022. [DOI] [PubMed] [Google Scholar]
- 2.King L, Quinn GP, Vadaparampil ST, Gwede CK, Miree CA, Wilson C, et al. Oncology nurses' perceptions of barriers to discussion of fertility preservation with patients with cancer. Clin J Oncol Nurs. 2008;12:467–76. doi: 10.1188/08.CJON.467-476. [DOI] [PubMed] [Google Scholar]
- 3.Adams E, Hill E, Watson E. Fertility preservation in cancer survivors: A national survey of oncologists' current knowledge, practice and attitudes. Br J Cancer. 2013;108:1602–15. doi: 10.1038/bjc.2013.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takeuchi E, Kato M, Wada S, Yoshida S, Shimizu C, Miyoshi Y. Physicians' practice of discussing fertility preservation with cancer patients and the associated attitudes and barriers. Support Care Cancer. 2017;25:1079–85. doi: 10.1007/s00520-016-3495-5. [DOI] [PubMed] [Google Scholar]
- 5.McDougall R. The ethics of fertility preservation for paediatric cancer patients: From offer to rebuttable presumption. Bioethics. 2015;29:639–45. doi: 10.1111/bioe.12190. [DOI] [PubMed] [Google Scholar]
- 6.Harzif AK, Santawi VP, Maidarti M, Wiweko B. Investigation of each society for fertility preservation in Asia. Front Endocrinol (Lausanne) 2019;10:151. doi: 10.3389/fendo.2019.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu L, Peterson B, Inhorn MC, Boehm JK, Patrizio P. Knowledge, attitudes, and intentions toward fertility awareness and oocyte cryopreservation among obstetrics and gynecology resident physicians. Hum Reprod. 2016;31:403–11. doi: 10.1093/humrep/dev308. [DOI] [PubMed] [Google Scholar]
- 8.Zhang H, Wang G, Jiang B, Cao M, Jiang Q, Yin L, et al. The knowledge, attitude, and self-reported behaviors of oncology physicians regarding fertility preservation in adult cancer patients. J Cancer Educ. 2020;35:1119–27. doi: 10.1007/s13187-019-01567-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36:1994–2001. doi: 10.1200/JCO.2018.78.1914. [DOI] [PubMed] [Google Scholar]
- 10.Revel A, Revel-Vilk S. Fertility preservation in young cancer patients. J Hum Reprod Sci. 2010;3:2–7. doi: 10.4103/0974-1208.63113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harfiz A, Iswaranti MM, Wiweko B. Knowledge and attitude of Indonesian obstetricians and gynecologists regarding fertility preservation in cancer patients. Adv Sci Lett. 2017;23:7. [Google Scholar]
- 12.Knapp CA, Quinn GP. Healthcare provider perspectives on fertility preservation for cancer patients. Cancer Treat Res. 2010;156:391–401. doi: 10.1007/978-1-4419-6518-9_30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vindrola-Padros C, Dyer KE, Cyrus J, Lubker IM. Healthcare professionals' views on discussing fertility preservation with young cancer patients: a mixed method systematic review of the literature. Psychooncology. 2017;26:4–14. doi: 10.1002/pon.4092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suhag V, Sunita BS, Sarin A, Singh AK, Dashottar S. Fertility preservation in young patients with cancer. South Asian J Cancer. 2015;4:134–9. doi: 10.4103/2278-330X.173175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiweko B, Prawesti DM, Hestiantoro A, Sumapraja K, Natadisastra M, Baziad A. Chronological age vs biological age: An age-related normogram for antral follicle count, FSH and anti-Mullerian hormone. J Assist Reprod Genet. 2013;30:1563–7. doi: 10.1007/s10815-013-0083-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shimizu C, Bando H, Kato T, Mizota Y, Yamamoto S, Fujiwara Y. Physicians' knowledge, attitude, and behavior regarding fertility issues for young breast cancer patients: A national survey for breast care specialists. Breast Cancer. 2013;20:230–40. doi: 10.1007/s12282-011-0328-8. [DOI] [PubMed] [Google Scholar]


