Abstract
BACKGROUND:
Amidst corona virus disease-2019 (COVID-19) pandemic, disruption to the usual ways of life can lead to anxiety and feeling of being unsafe, which may be associated with self-medication. The study was planned to investigate the prevalence of anxiety and self-medication during COVID-19 pandemic.
MATERIALS AND METHODS:
In this cross-sectional study, data were collected through an anonymous online survey with questionnaire consisting of four sections: demographic data of the participants, validated COVID-19 Anxiety Inventory Items, Self-rating Anxiety Scale, and self-medication practices during COVID-19 pandemic. The data were organized and analyzed using Windows Microsoft excel and SPSS software (Version 21). Descriptive statistics were calculated for all patient characteristics and survey responses. Analytical analysis included relationship between various parameters using Chi-square test.
RESULTS:
A total of 1100 responses were received. Approximately half of the participants were worried about getting severely ill. Majority reported reduced social contact (71.3%, n = 784) and also communicated that the pandemic has influenced their use of safety measures (86.5%, n = 951). The prevalence of mild-to-moderate, moderate-to severe, and extremely severe anxiety cases were 23.1%, 4.7%, and 0.54%, respectively. One-fourth of the responders reported self-medication, out of which 60% were found to be anxious. Nonsteroidal anti-inflammatory drugs were most commonly used.
CONCLUSIONS:
Rising to the present challenge will require integration across different sectors with the immediate aim of getting people safely through the pandemic. As the world focuses on containing and delaying the spread of the COVID-19, with burdened health-care systems, we should not miss out on people with anxiety disorders and self-medication problem, which may worsen with the pandemic.
Keywords: Anxiety, corona virus disease-2019, pandemic, self-medication, Self-Rating Anxiety Scale
Introduction
Corona virus disease-2019 (COVID-19) has become a global health emergency requiring countries to rapidly change their public health policies with the goals to restrict the transmission of infection, provide early treatment, convey key information, and reduce economic and social impacts. India witnessed the greatest confinement experiment in history to minimize the spread of infection and flatten the COVID-19 curve. A 14-h voluntary curfew was initially observed on March 22, 2020, which was followed up with lockdowns in 75 districts with COVID-19 cases. A 21-day nationwide lockdown was announced on March 24 till April 14, which was later extended till May 17th. The need for social support is paramount in times of adverse situations such as the current pandemic, severing this can threaten an individual's sense of connectedness and may take a considerable toll on mental health.[1] Anxiety and complacency are commonly observed effects of pandemic. Increased use of masks and sanitizers resulting in exhaustion of resources in the market at the onset of coronavirus pandemic highlights the existence of anxiety in the population.[2] There is a documented link between anxiety and self-medication. Self-medication is a regular occurrence in individuals who suffer from anxiety disorders.[3] The course of novel COVID-19 is changing incessantly. In this scenario, where anxiety is a common manifestation, it is crucial to how it is affecting the tendency to self-medicate. There is no study in Indian context that relates anxiety with self-medication; more so exploring this association in the current pandemic is paramount. It is essential to study how people are reacting to the ongoing disaster. Hence, this study was planned to determine the prevalence of self-rated anxiety and self-medication during COVID-19 pandemic in general population.
Materials and Methods
The present cross-sectional study was conducted after obtaining clearance from the Institutional Ethical Committee. The exponential nondiscriminative snowball sampling method was used for data collection. The participation in the survey was entirely voluntary in nature; filling of online form was considered as their consent. The identification information of participants was not recorded anywhere on the questionnaire to maintain confidentiality and anonymity. Participants were general public from middle and high socioeconomic status (SES). Inclusion criteria include age >18 years and family income >50,000/month. Individuals with a history of any psychiatric illness were also excluded from the study. The SES was determined as per Modified Kuppuswamy's classification updated for 2019.[4] Participants were asked to fill a prevalidated questionnaire using a web platform (Google forms). The link of the questionnaire was made available to the participants through social media (WhatsApp) and mail. Participants were encouraged to forward the survey to as many people as possible. The data were collected from 1 May through May10, 2020.
The questionnaire was divided into four sections. The first section included demographic data of the participants such as sex, age, marital status, family setup, education level, and monthly income. The Section 2 contained six validated COVID-19 Anxiety Inventory Items; each item was rated on a scale of 0–4, where 0 has the least and 4 the maximum value. The items were modified from the scale used by Wheaton et al.[5] after taking inputs from psychiatrists experienced in evaluating and treating individuals with anxiety disorders. Items were designed based on clinical observations to assess participants' concerns about the spread of COVID-19, perceived likelihood of contracting the disease, perceived severity of infection, avoidance of certain places and people, and adopting safety behaviors. The items with Cronbach's alpha >0.7 were included in the inventory. Participants rated their agreement with each item on a 5-point scale ranging from 0 (“very little”) to 4 (“very much”).
Section 3 evaluated the subjective feeling of anxiety using Self-Rating Anxiety Scale (SAS). SAS consists of 20-item Likert scales; each item determines intensity of psychological and physiological symptoms experienced by the participants. The participants rated each item as per their experience within the past week, using a 4-point scale ranging from 1 (none, or a little of the time) to 4 (most, or all of the time). The scores were reversed for items 5, 9, 13, 17, and 19, which depict positive experience. The total raw scores range from 20 to 80. The raw score is to be converted to an “SAS Anxiety Index.” The SAS Anxiety index is calculated by dividing the raw score by 80 and then multiplying it by 100.[6]
The clinical interpretation of one's level of anxiety is as follows:[7]
20–44 = Normal range
45–59 = Mild-to-moderate anxiety level
60–74 = Marked-to-severe anxiety level
75–80 = Extreme anxiety level.
The fourth section evaluated the self-medication practice during the COVID-19 pandemic and included questions about the common medicines they had taken during the lockdown period, for what ailment and whether they have been previously or not.
The data were organized and analyzed using Windows Microsoft excel (2018) and SPSS software (Version 21, IBM Corp., Armonk, NY, USA). Descriptive analysis (means with standard deviation and percentage frequencies) was calculated for all patient characteristics and survey responses. The inferential analysis of the relationship between gender, age, and anxiety was done using the Chi-square test. The significance between self-medication and other variables such as gender, family type, and anxiety was calculated using Chi-square test. The level of significance was kept at <0.05.
Results
A total of 1100 responses were received within the stipulated time. Table 1 shows the demographic characteristics of the participants.
Table 1.
Demographic characteristics of the participants
| Demographic parameter | Categories | Percentage |
|---|---|---|
| Gender | Male | 51 |
| Female | 48.2 | |
| Prefer not to say | 0.2 | |
| Age group | 20- 30 | 24.1 |
| 30.1- 40 | 28.5 | |
| 40.1- 50 | 33.3 | |
| 50.1- 60 | 9.6 | |
| >60 | 4.4 | |
| Occupation | Professional | 65.81 |
| Homemaker | 12.3 | |
| Self-employed | 13 | |
| Retired | 3 | |
| Student | 5.9 | |
| Marital status | Married | 67.5 |
| Unmarried | 26.9 | |
| Divorced | 1.9 | |
| Other | 3.7 | |
| Family set up | Nuclear | 67.8 |
| Joint | 30.7 | |
| Extended | 1.5 | |
| Socioeconomic status | Upper | 21.4 |
| Upper middle | 22.5 | |
| Lower middle | 56.1 |
Corona virus disease-2019 anxiety inventory
The mean score of COVID-19 anxiety inventory items is given in Table 2. Only 14% of participants reported being worried that they could become infected with COVID-19. Around 44.2% of the participants were paranoid with the thought that they would be severely ill. Among the participants, 71.3% had reduced social contact, and they were of the opinion that COVID-19 influenced their decisions to be around people and in around. About 83% of participants communicated the COVID-19 pandemic had influenced their travel plans. Majority (86.5%) of the participants reported that the pandemic has influenced their use of safety measures.
Table 2.
COVID-19 anxiety inventory
| number | Items | Mean score (SD) |
|---|---|---|
| 1 | To what extent are you concerned about COVID-19? | 3.23 (0.89) |
| 2 | How likely is it that you could become infected with COVID-19? | 2.24 (1.11) |
| 3 | If you did become infected with COVID-19, to what extent are you concerned that you will be severely ill? | 2.41 (0.96) |
| 4 | To what extent has the threat of COVID-19 influenced your decision to be around people? | 3.02 (0.97) |
| 5 | To what extent has the threat of COVID-19 influenced your travel plans? | 3.45 (0.99) |
| 6 | To what extent has the threat of COVID-19 influenced your use of safety behaviors? | 3.45 (0.88) |
Items rated from 0 to 4. SD=Standard deviation
Self-rating Anxiety Scale
The responses to the items and mean score are shown in Table 3.
Table 3.
Self-rating Anxiety Scale
| Item number | Items | Mean score (SD) |
|---|---|---|
| 1 | I feel more nervous and anxious than usual | 1.94 (0.90) |
| 2 | I feel afraid for no reason at all | 1.68 (0.86) |
| 3 | I get upset easily or feel panicky | 1.77 (0.88) |
| 4 | I feel like I’m falling apart and going to pieces | 1.48 (0.79) |
| 5 | I feel that everything is all right and nothing bad will happen | 2.61 (1.00) |
| 6 | My arms and legs shake and tremble | 1.14 (0.42) |
| 7 | I am bothered by headaches neck and back pain | 1.57 (0.82) |
| 8 | I feel weak and get tired easily | 1.64 (0.85) |
| 9 | I feel calm and can sit still easily | 2.33 (1.10) |
| 10 | I can feel my heart beating fast | 1.37 (0.61) |
| 11 | I am bothered by dizzy spells | 1.31 (0.62) |
| 12 | I have fainting spells or feel like it | 1.15 (0.44) |
| 13 | I can breathe in and out easily | 1.59 (0.99) |
| 14 | I get feelings of numbness and tingling in my fingers and toes | 1.25 (0.53) |
| 15 | I am bothered by stomach aches or indigestion | 1.50 (0.77) |
| 16 | I have to empty my bladder often | 1.54 (0.74) |
| 17 | My hands are usually dry and warm | 2.98 (1.11) |
| 18 | My face gets hot and blushes | 1.31 (0.58) |
| 19 | I fall asleep easily and get a good night’s rest | 2.20 (1.04) |
| 20 | I have nightmares | 1.53 (0.83) |
The items were rated on a 4-point scale ranging from 1 (none, or a little of the time) to 4 (most, or all of the time). The scores were reversed for items 5, 9, 13, 17 and 19, which depict positive experience. SD=Standard deviation
Mild-to-moderate, moderate-to–severe, and extremely severe anxiety were observed to be 254, 52, and 6 individuals, respectively. The prevalence of mild-to-moderate, moderate-to–severe, and extremely severe anxiety cases were 23.1%, 4.7%, and 0.54%, respectively. The mean SAS Index was 42.17 ± 9.19. In terms of physiological responses, 5.3% of people felt weak and tired easily, 2.5% of people often had to urinate, and 4.8% of people suffered from head, neck, and back pain. In terms of emotional responses, 8.9% of people were more nervous and anxious than usual, 5.9% of people were afraid for no reason, and 6.1% of people were easily upset or panicked. In terms of behavioral responses, only 3.8% of people thought that they are falling apart and going to pieces. 13.9% of people had problems falling asleep and 5.2% had nightmares. In the description of positive statements, 86% of people slept well through the night; 89.2% found it easy to breathe; 79.4% of people were calm and at ease; and 54.7% of people often had dry and warm hands and feet.
Single-factor Chi-square test results showed that the anxiety ratio was higher for females than for males (χ2= 14.44, P = 0.00014). No significant difference in anxiety ratio was observed in population above and below 50 years of age group (χ2= 0.0038, P = 0.95). There was no significant difference in the prevalence of anxiety in married individuals as compared to unmarried (χ2= 0.15, P = 0.69).
Self-medication
Around 25% of responders (n = 266) had taken medicine without consultation, out of these 56.6% were taking it for the first time. The drug groups used for self-medication most commonly are shown in Figure 1. The demographic profile of participants who self-medicated is shown in Table 4.
Figure 1.
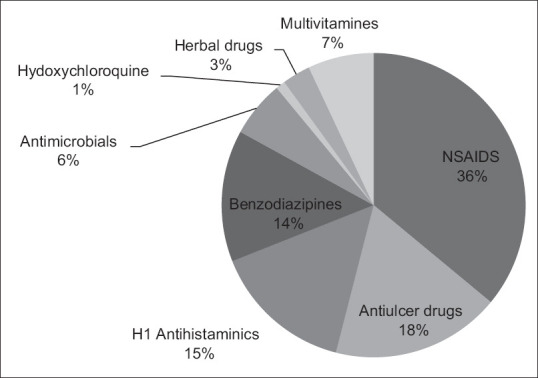
The most commonly used drug groups for self-medication
Table 4.
Demographic characteristics of participants who self-medicated
| Demographic characteristics | Categories | n (%) | χ2 | P |
|---|---|---|---|---|
| Gender | Male | 46 (17) | 159.5 | <0.00001 |
| Female | 220 (83) | |||
| Marital status | Married | 232 (87) | 61.9 | <0.00001 |
| Unmarried/divorced/others | 34 (33) | |||
| Family setup | Nuclear | 176 (66) | 0.44 | 0.51 |
| Joint/extended | 90 (34) | |||
| SAS index | >45 | 160 (60) | 22.8 | <0.00001 |
| <45 | 106 (40) |
P<0.05 was taken as the level of significance. The proportion of participants who reported self-medication differed significantly by gender, marital status, family setup and anxiety (SAS) index. SAS=Self-rating Anxiety Scale
The drugs were taken primarily for symptoms such as headache, pain abdomen, ghabrahat, and inability to sleep.
Discussion
COVID-19 pandemic presents a new, unexpected, and tremendous challenge for the population globally; hence, the psychosocial response to an event of such a magnitude will be complex. The contextual factors surrounding COVID-19, such as the effortlessness of transmission, lack of immunity among global populations, delayed testing, inadequate medical equipment, uncertainty of the pandemic course, and the level of anxiety within people, all coalesce to create increasing pressure on health and welfare systems.[8] The novel coronavirus necessitates people around the world to take immediate actions to minimize their risk for infection and the spread of the virus; the guidelines for the same have been provided by the concerned authorities.[9] A combination of anxiety, uncertainty, social isolation, and economic problems (due to limitations on daily life and social activities for an unknown period of time) may adversely affect the mental well-being and physical health of a given population.
Different studies from other countries have shown that in an early phase of the severe acute respiratory syndrome in COVID, a range of psychiatric morbidities had occurred, including persistent depression, anxiety, panic attacks, psychotic symptoms, and even suicide.[10,11] The present study thus explored the psychological experience of general population and its link with use of medication during this COVID-19 pandemic in Indian context. Literature search did not retrieve any significant data on the association of self-medication with anxiety during COVID-19 outbreak.
A study by Wang et al. found that age and gender are associated with anxiety.[12] They observed increased risk of anxiety in individuals above 40 years old and reported females to have a higher risk of anxiety than males. The present study did not report any age-associated difference in anxiety status. Similarly, no difference was observed in the anxiety level of married and unmarried people. However, females were found to be more anxious than males. Contrary to our findings, other studies have shown that married people experienced increased financial and home stresses and felt more apprehensive during the pandemic.[11]
COVID-19 pandemic is making the population nervous and pushing them into a state of high hassle. The physiological, psychological, and behavioral changes during pandemic state produce corresponding responses. Usually, the physiological response of stress state is manifested as changes of the autonomic nervous system and endocrine system. The manifestations of which include increased heartbeat, rise in blood pressure, increased blood sugar, appetite disorder, dyspepsia, sleep disorder, headache, body pain, and endocrine disorders. The emotional response caused by stress can result in a negative emotional state such as depression, anxiety, panic, disappointment, or fear. The behavioral changes caused by stress can result in frequent anger, forced behavior (excessive disinfection and repeated hand washing), crying easily, smoking, and alcohol abuse.
A study done by Roy et al.[2] in Indian population reported frequent use of sanitizers, hand wash, and masks during the past 1 week. This indicates the increasing concern of participants toward personal hygienic measures to avoid COVID-19 infection. Similar to this, the present study also showed that majority of participants were concerned about the infection. Roy et al. reported about 72% of participants to be worried of getting infected themselves and about their close ones getting infected during the ongoing pandemic.[2] Contrary to this, only 14% of participants reported being worried that they could become infected with COVID-19. This difference can be due to the time difference in the conduction both the studies. Similar to our study, another study from USA showed a small percentage of people getting worried and believing that they would definitely or probably get the coronavirus.[9] Chakraborty and Chatterjee[13] reported more than half of the responders to be worried about the ongoing pandemic. Studies from other countries have also reported moderate-to-severe psychological impact among the respondents.[11,14]
The fear and uncertainty, which has risen with the pandemic, can result in many people turning to self-medicate with drugs and alcohol to ease the stress. It is a known fact that isolation and loneliness have an overwhelming effect on drug or alcohol addiction. “Any anxiety disorder” had an odds ratio of 1.7 of being diagnosed with a substance use disorder, as compared with individuals without an anxiety disorder.[3] The comorbidity of substance use disorders and anxiety disorders has been clearly established in several nationally representative studies.[3,15,16] In the United States, prescriptions for antidepressant, anti-anxiety, and anti-insomnia drugs were reported to increase by 21% from mid-February after COVID-19 was declared a pandemic[17]
In the present study, 24.2% of respondents had taken medicine without prescription. Among them, approximately 1% were taking hydroxychloroquine prophylaxis. According to Chakraborty and Chatterjee, 19.9% of the respondents were taking hydroxychloroquine as a prophylaxis for COVID-19, out of which around 10.8% were taking the drug without any doctor's advice.[13] Self-medication with NSAIDs was highest in our study, similar to the findings by other authors from India and abroad.[18,19] NSAIDs are usually the most commonly used medicines by community, as they are easily available over-the-counter and people keep analgesics at home for symptomatic relief of pain.
In the current scenario, with nationwide lockdown and fear of getting infected, people find self-medication more convenient. Further, self-care, inconvenience of visiting a doctor, lack of health services can increase the incidence of self-medication. Self-medication with these drugs can pose problems. In addition, use of antipyretics and analgesics in viral influenza has shown to increase mortality in animals[20] and has shown to cause suppression of serum antibodies and prolongation of viral shedding in humans.[21]
In our study, self-medication was significantly more in respondents who were anxious. Self-medication behavior has been found to be significantly associated with an increased likelihood of suicidal ideation as well as suicide attempts.[3] This is a major concern and needs attention. Social media platforms can be useful for creating mental health awareness.[22] Sessions of meditation and mindfulness may be helpful in reducing anxiety.[23]
Limitations
Strength of the study is the sample size keeping in mind the short time duration. The current study is limited by self-reported bias. In addition, oversampling a particular network of peers can lead to bias.
Conclusions
Proper use of over-the-counter medications for managing simple ailments of common occurrence in general population also needs to be monitored. As the pandemic unfolds, the society should be cautious against ignoring the shocking traumatization it has caused, and for dealing with such issues, psychosocial crisis prevention and intervention models should be urgently developed by the stakeholders. Rising to the present challenge will require integration across different sectors with the immediate aim of getting people safely through the pandemic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Usher K, Bhullar N, Jackson D. Life in the pandemic: Social isolation and mental health. J Clin Nurs. 2020;29:2756–7. doi: 10.1111/jocn.15290. [DOI] [PubMed] [Google Scholar]
- 2.Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083. doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolton J, Cox B, Clara I, Sareen J. Use of alcohol and drugs to self-medicate anxiety disorders in a nationally representative sample. J Nerv Ment Dis. 2006;194:818–25. doi: 10.1097/01.nmd.0000244481.63148.98. [DOI] [PubMed] [Google Scholar]
- 4.Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh's scale updated for 2019. J Family Med Prim Care. 2019;8:1846–9. doi: 10.4103/jfmpc.jfmpc_288_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wheaton MG, Abramowitz JS, Berman NC, Fabricant LE, Olatunji BO. Psychological Predictors of Anxiety in Response to the H1N1 (Swine Flu) Pandemic. Cogn Ther Res. 2012;36:210–18. [Google Scholar]
- 6.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–9. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 7.Kuvačić G, Fratini P, Padulo J, Antonio DI, De Giorgio A. Effectiveness of yoga and educational intervention on disability, anxiety, depression, and pain in people with CLBP: A randomized controlled trial. Complement Ther Clin Pract. 2018;31:262–7. doi: 10.1016/j.ctcp.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. How Coronavirus Spreads. 2020. [Last accessed on 2020 Jun19]. Available from: https://wwwcdcgov/coronavirus/2019-ncov/prepare/transmissionhtml .
- 9.Panahi S, Ashrafi-Rizi H, Panahi M. Exposure to coronavirus (COVID-19) using narrative and simulated experience approaches: A commentary. J Educ Health Promot. 2020;9:135. doi: 10.4103/jehp.jehp_267_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–9. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Zoghby SM, Soltan EM, Salama HM. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J Community Health. 2020;45:689–95. doi: 10.1007/s10900-020-00853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2020;30:1–10. doi: 10.1080/13548506.2020.1746817. doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- 13.Chakraborty K, Chatterjee M. Psychological impact of COVID19 pandemic on general population in West Bengal: A cross-sectional study. Indian J Psychiatry. 2020;62:266–72. doi: 10.4103/psychiatry.IndianJPsychiatry_276_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning province, China: A cross-sectional study. Int J Environ Res Public Health. 2020;17:2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–8. [PubMed] [Google Scholar]
- 17.America's State of Mind: Use of Mental Health Medications Increasing with Spread of Coronavirus. [Last assessed on 2020 Jun 19]. Available from: https://www.express-scripts.com/corporate/americas-state-of-mindreport .
- 18.Auta A, Banwat SB, Sariem CN, Shalkur D, Nasara B, Atuluku MO. Medicines in pharmacy students' residence and self-medication practices. J Young Pharm. 2012;4:119–23. doi: 10.4103/0975-1483.96627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tesfamariam S, Anand IS, Kaleab G, Berhane S, Woldai B, Habte E, et al. Self-medication with over the counter drugs, prevalence of risky practice and its associated factors in pharmacy outlets of Asmara, Eritrea. BMC Public Health. 2019;19:159. doi: 10.1186/s12889-019-6470-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eyers S, Weatherall M, Shirtcliffe P, Perrin K, Beasley R. The effect on mortality of antipyretics in the treatment of influenza infection: Systematic review and meta-analysis. J R Soc Med. 2010;103:403–11. doi: 10.1258/jrsm.2010.090441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Graham NM, Burrell CJ, Douglas RM, Debelle P, Davies L. Adverse effects of aspirin, acetaminophen, and ibuprofen on immune function, viral shedding, and clinical status in rhinovirus-infected volunteers. J Infect Dis. 1990;162:1277–82. doi: 10.1093/infdis/162.6.1277. [DOI] [PubMed] [Google Scholar]
- 22.Latha K, Meena KS, Pravitha MR, Dasgupta M, Chaturvedi SK. Effective use of social media platforms for promotion of mental health awareness. J Educ Health Promot. 2020;9:124. doi: 10.4103/jehp.jehp_90_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nasiri Z, Alavi M, Ghazavi Z, Rabiei K. The effectiveness of mindfulness-based intervention on perceived stress and perception of disease in patients with acute coronary syndrome. J Educ Health Promot. 2020;9:130. doi: 10.4103/jehp.jehp_660_19. [DOI] [PMC free article] [PubMed] [Google Scholar]


