Abstract
BACKGROUND:
Irritable bowel syndrome (IBS) is one of the most common gastrointestinal diseases, and obsessive–compulsive disorder (OCD) is one of the main causes of this disease. The present study was aimed to investigate the prevalence of OCD in patients with IBS.
MATERIALS AND METHODS:
The present research is a cross-sectional survey study. The research sample included 120 patients with IBS who referred to Imam Reza Hospital and gastrointestinal clinics in Kermanshah (Iran) in the 3 months of April, May, July in 2019 that were selected using the census sampling method, and demographic information, clinical and medical records were collected. Data analysis was performed using frequency, percentage, and Chi-square.
RESULTS:
Among the patients who were studied, 58 of them (48.3%) were women and 62 (51.7%) were men, the results showed that the prevalence of OCD in patients with IBS was 14.96 and the symptoms of washing, checking, skepticism and slowness-repetition had the highest prevalence, respectively. These symptoms were more common in women than in men. There was also a significant relation between OCD prevalence in patients with IBS and with female gender, age-range 30–21 years, single, and history of OCD in the patient's immediate family and close relatives (P < 0.05), but there was no significant relationship between OCD prevalence in patients with IBS and level of education, occupation, income status, and place of residence
CONCLUSION:
Due to the high prevalence of OCD in patients with IBS, the interaction of gastroenterologists and psychiatrists to treat irritable bowel syndrome is very important.
Keywords: Irritable bowel syndrome, obsessive-compulsive disorder, patients, prevalence
Introduction
Irritable bowel syndrome (IBS) is one of the most common gastrointestinal diseases which is characterized by chronic abdominal pain and irritated bowel changes without any recognizable organ disorders.[1,2] The disease is considered a functional disorder that is diagnosed using symptom-based criteria, and a person's quality of life and health are affected by this chronic disease.[1,2] Research has shown that IBS is seen among 14%–25% of the general population.[3] The disease is so prevalent around the world that affects 11.2% of people of all ages, but young people are more affected than people over the age of 50. According to the World Gastroenterology Organization, the prevalence rate is higher among women than men.[1,2,4,5] Women make up 80% of the population of patients with severe IBS.[6] Its prevalence in the United States and Europe is approximately 5%–10%,[7] and in Iran, it is 6%.[8] Although the cause of IBS is not fully specified,[9] it has several causes, one of which is psychological factors that play an important role in the etiology and exacerbation of IBS symptoms.[10] According to recent studies, patients with IBS have a history of psychological conditions such as obsessive–compulsive disorder (OCD) throughout their lives, In fact, this disorder has been mentioned as the underlying cause of IBS, so that there is a coherent relationship between these two diseases.[11,12]
A brain-intestinal interaction in IBS plays an important role, and disorders related to psychological factors are possible factors affecting brain-intestinal activity.[13] OCD is the fourth most common psychiatric illness, which appears with recurrent obsessive thoughts and repetitive behaviors.[14] In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the American Psychiatric Association (APA), OCD is a collection of mental and behavioral patterns in which the patient, in almost all aspects of life, thinks about the order, perfectionism, personal and interpersonal control, and in the meantime, flexibility, theoretical openness, and saving time and energy become unimportant. This condition starts before adulthood and exists in different conditions. Thought and practical obsessions are the two main characteristics of OCD, each of which may appear alone or with the other.[15] The prevalence lifetime of this disorder in the general population is relatively constant and is about 2%–3%, and in patients who are referred to psychiatric clinics and offices has been reported up to 10%.[16] OCD, as one of the most common mental disorders, causes severe impairment in interpersonal, social, occupational relationships, committing suicide, and reduces the quality of life, which annually increases the economic and social costs in society.[17,18] The results of studies by Lee et al.,[19] Alhan and Okan,[20] Fond et al.,[21] Chou et al.[22] showed that there is a relationship between IBS and anxiety disorder.
Because IBS is one of the most common gastrointestinal disorders it has many effects on the health and economic system and paying attention to the importance and role of psychological factors such as OCD, as one of the factors causing and exacerbating IBS symptoms and the simultaneous incidence of physical and mental illnesses and the high prevalence of this disease, recognizing and examining the pathology of this disorder and discovering the cognitive factors involved in this disorder and its effectiveness on IBS is essential for the psychological therapies used. Because so far, no research has been conducted to evaluate the prevalence of disorders and obsessions in patients with IBS. Therefore, the current study was conducted in 2019 to investigate the prevalence of OCD in patients with IBS in Kermanshah (Iran).
Methods
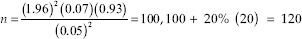
The present research is a cross-sectional survey study. The statistical population of this study was all patients with IBS who referred to Imam Reza Hospital and gastroenterology clinics in Kermanshah (Iran) in the 3 months of April, May July 2019, who were selected using the census sampling method. The sample size required for this study, considering the prevalence of 7% for OCD among the patients with IBS obtained from a study conducted by Burke et al.[23] in 1994, with 95% reliability and 5% accuracy, according to the type of the study, using the following formula, 100 people were calculated, including a 20% (20 people) drop, the final sample size was determined to be 120 people, who were selected by available sampling method and from the study population.
The criteria for entering into the study included all men and women with IBS, IBS diagnosis by a gastroenterologist based on positive Roman II criteria, and danger symptoms rejection (anal bleeding, weight loss, persistent diarrhea, persistent dilatation, anemia, and fever) and the exiting criteria were dissatisfaction with participation in the study, use of drugs affecting the gastrointestinal system, having other diseases that cause symptoms similar to IBS, in the case of acute and severe IBS symptoms that made it difficult or almost impossible for the patient to participate in the present study, the incompleteness of the questionnaire and major psychiatric disorders.
The diagnosis of OCD was made based on DSM-5 diagnostic criteria by a trained physician and a Maudsley Obsessive-Compulsive questionnaire.
The study method was conducted in such a way that the researchers, after obtaining the necessary permission and coordinating with the relevant authorities, were present among the study community and after a full explanation on how to carry out the plan and obtain written consent from patients, based on inclusion criteria and exclusion of the study, eligible individuals entered the study. These individuals were initially evaluated by the demographic variables questionnaire, the IBS (Rome-II) diagnostic criteria checklist, the DSM-5 criteria-based diagnostic interview, and the Maudsley Obsessive-Compulsive questionnaire, and their information was collected.
The information was collected through a specialist, interview, and questionnaires and entered into the SPSS-21 statistical software (IBM Corp: Armonk, NY, USA).
To diagnose IBS, based on the mentioned criterion (Rome-II), there must be two or three of the following symptoms for at least 3 months in a year consecutively or intermittently.
Having abdominal pain or discomfort with at least two of the following characteristics: 1 - Relieving pain by defecating. 2 - The onset of symptoms with changes in the number of bowel movements. 3 - The onset of symptoms with changes in the shape of the stool
Symptoms that generally support the diagnosis of IBS: 1 - The number of abnormal bowel movements (more than three times a day or <3 times a week). 2 - Abnormal stool shape (bulky, hard or loose, watery stool). 3 - Abnormal passage of feces (excretion by pressure and force, urgency in excretion or feeling of incomplete excretion). 4 - Mucus excretion. 5-Flatulence or abdominal distention.
The Maudsley OCD questionnaire was introduced in 1977 by Hodgson and Rachman. The questionnaire consists of 30 items that are answered with yes or no, and the total score of the Maudsley is between zero and 30, which includes four sub-components of checking, washing, slowness-repetition, and skepticism-doubt. The questionnaire is designed in a way that an obsessive person answers exactly half of the questions positively and the other half negatively. The score of the answers that match the answer key is one, and the score of the answers that do not match the answer key is zero. The general cutoff point for this questionnaire is 11 and more, which means that the OCD is significant, and the cutoff point for checking obsession is 6, washing 7, slowness-repetition 5, and skepticism-5.[14] Hodgson and Rachman reported the Cronbach's alpha coefficient of 0.70 for checking, 0.80 for washing, 0.70 for slowness-repetition 0.70 skepticism. This questionnaire has good test-retest reliability and internal validity. The test-retest correlation is 0.80 and internal validity is 0.7–0.80.[24] In Iran, Safaralizadeh et al. found the reliability coefficient of the whole test as 0.84 and its convergent validity with the Yale-Brown compulsive obsession scale as 0.87.[14]
The medical research and ethical committee of Kermanshah University of medical sciences, Kermanshah, Iran; approved the study (registration No. IR KUMS.REC.1398.081 at the date of April 24, 2019; grant number 9800087), which was performed by the ethical principles laid down in the seventh and current edition (2013) of the Declaration of Helsinki. All participants were volunteers who signed written informed consent.
At first, the information about the patients was collected and recorded. Frequency and percentage were used to describe the data. To assess the relationship between the prevalence of OCD in patients with IBS and classified variables, the Chi-square test was used. The data were entered into the software and analyzed by the relevant statistical methods. All analyses were performed using SPSS-21 statistical software. The significance level was also considered to be 0.05.
Results
The results showed that the prevalence of OCD among female patients was (15.51), checking (4.14), washing (5.43), slowness-repetition (3.01), and skepticism (3.41) and among the male patients, the prevalence of OCD was (14.43), checking (3.46), washing (5.25), slowness-repetition (2.64), and skepticism (3.26). In general, the prevalence of OCD in patients with IBS was 14.96, and the types of washing, checking, skepticism, and slowness-repetition had the highest prevalence, respectively [Table 1].
Table 1.
Prevalence of obsessive-compulsive disorder and its types in patients irritable bowel syndrome
| Prevalence | OCD, n (%) | Checking, n (%) | Washing/cleaning, n (%) | Slowness, n (%) | Doubting, n (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Female (n=58) | 9 (15.51) | 49 (84.49) | 2 (4.14) | 56 (95.86) | 3 (5.43) | 55 (94.57) | 2 (3.01) | 56 (96.99) | 2 (3.41) | 56 (96.49) |
| Male (n=62) | 9 (14.43) | 53 (85.57) | 2 (3.46) | 60 (96.54 | 3 (5.25) | 59 (94.75) | 2 (2.64) | 60 (97.36) | 2 (3.26) | 60 (96.74) |
| Total (n=120) | 18 (14.96) | 102 (85.04) | 5 (3.79) | 115 (96.21) | 6 (5.34) | 114 (94.64) | 3 (2.82) | 117 (97.18) | 4 (3.33) | 116 (96.67) |
OCD=Obsessive–compulsive disorder
In Table 2, the prevalence of OCD by age, gender, marital, education, occupation. Income, residence, and history of OCD in the family are shown in Table 2.
Table 2.
The prevalence of obsessive-compulsive disorder is based on demographic information in patients with irritable bowel syndrome
| Variable | Level | n (%) | χ2 | P |
|---|---|---|---|---|
| Age (year) | <20 | 19 (15.8) | 108.48 | 0.03 |
| 21-30 | 44 (36.7) | |||
| 31-40 | 23 (19.2) | |||
| 41-50 | 22 (18.3) | |||
| >50 | 12 (10.0) | |||
| Gender | Female | 58 (48.3) | 32.20 | 0.04 |
| Male | 62 (51.7) | |||
| Marital | Single | 64 (53.3) | ||
| Married | 50 (41.6) | 136.40 | 0.02 | |
| Divorced | 3 (2.5) | |||
| Widow | 3 (2.5) | |||
| Education | Illiterate | 3 (2.5) | ||
| Primary and high school | 17 (14.2) | 146.88 | 0.48 | |
| Diploma and high diploma | 30 (27.0) | |||
| >Bachelor | 70 (58.3) | |||
| Occupation | Housewife | 15 (12.5) | 126.60 | 0.88 |
| Student | 35 (29.2) | |||
| Employed | 62 (51.7) | |||
| Unemployed | 8 (6.7) | |||
| Income (monthly) | Low | 82 (68.3) | 91.52 | 0.82 |
| Middle | 30 (25.0) | |||
| High | 8 (6.7) | |||
| Residence | City | 114 (95.0) | 11.98 | 0.94 |
| Village | 6 (5.0) | |||
| History of OCD in the family | Yes | 39 (32.5) | 37.56 | 0.0.1 |
| No | 81 (67.5) |
OCD=Obsessive–compulsive disorder
Most of the patients, 44 people, were in the age group of 21–30 (36.7) and the lowest number of patients, 12 people, was in the age group of over 50 (10.0). There was a significant relationship between the prevalence of OCD in patients with IBS and age (P < 0.05), which had the highest prevalence among patients under 20 and 21–30 years old. In terms of marital status, most patients, 64 people (53.3%), were single, and the results showed that there was a significant relationship between OCD prevalence in patients with IBS and marital status (P < 0.05).
In terms of education level, 3 people (2.5%) were illiterate, 17 people (14.2%) had primary and secondary education, 30 people (27%) had high school diploma and A.A, 70 (58.3%) had bachelor's degree and higher. On the other hand, the majority of patients, 62 of them, were employed (51.7%) and 8 patients were unemployed (6.7%), who had the lowest frequency. Also, in terms of economic status, 82 patients (68.3%) had low income, 30 patients (25%) had average income and 8 patients (6.7%) had a high income. The majority of patients, 114 of them (95%), were urban residents and 6 (5%) were rural residents. The results showed that there was no significant relationship between the prevalence of OCD in patients with IBS and the level of education, occupation, income status, and place of residence (P < 0.05).
Furthermore, 39 patients (32.5%) had a history of OCD in the immediate family and close relatives, and 81 patients (67.5%) had no history of OCD and the results showed that there was a significant relationship between the prevalence of OCD in patients with IBS with a history of OCD in the family and close relatives of the patient at the level of (P < 0.05) [Table 2].
Discussion
The results of the present study showed that OCD was common in patients with IBS. However, the results of the research done by Lee et al.,[19] Alehan and Okan,[20] Fond et al.[21], Cho et al.[22], which showed that there is a relationship between IBS and anxiety disorder, were consistent. To elaborate on this finding, it can be stated that although IBS is a common gastrointestinal disease, it is associated with psychiatric disorders. Because the brain and intestines form a two-way relation between the autonomic nervous system and the hypothalamic-pituitary-adrenal axis; as a result, patients with psychiatric disorders develop IBS.[22]
In the DSM-5, IBS is listed in the category of psychological factors affecting medical diseases, that this factor also indicates the role of psychological factors in this syndrome, they play an important role in the course and clinical consequences of IBS.[25] The correlation of psychological disorders in patients with IBS has detrimental effects on the patients; and as the psychological factors aggravate, the symptoms of IBS exacerbate as well; as a result, it is associated with personal suffering, impaired social functioning, and decreased adherence to treatment, low quality of life[21,26,27,28] and increased risk of suicidal behaviors.[29]
The results also showed a significant relationship between the prevalence of OCD in patients with IBS and gender, and the prevalence of OCD is higher in female patients with IBS. The results of this finding are consistent with the study of Khosravi and Naseri,[30] who showed in their research that there is a relationship between OCD and gender. Epidemiological studies to investigate gender ratios among subjects with OCD showed a higher prevalence of this disorder in women.[31] In this regard, it can be said that like many disorders, in OCD, biological factors in interaction with other cases have an effective role that should be considered. For example, studies of gender differences in genetic capacity have shown that genetic aspects can have a significant impact on the manifestation of this disorder in women. As a result, the cause of the difference in prevalence in women's physiology and the type of responsibility they have can be considered.[30]
The results also showed a relationship between the prevalence of OCD in patients with IBS and age and its prevalence is higher in patients in the range of 21–-30 years. The results of this finding were consistent with the research done by Salehi et al.[31], who showed in their research the highest frequency at the onset of OCD was in the age group of 21–30, and the study done by Caraveo-Anduaga and Colmenar's,[32] who showed in their study that OCD is more common between the ages of 18 and 34. The prevalence of OCD is usually gradual, and most often appears in early adolescence or early adulthood and after a stressful event.[33]
So that the average age of onset is 19.5 years and in 25% of cases, it starts at 14 years old. It is not common to start after age 35, but it does happen occasionally. Some people have a periodic course and a small minority have a period of deterioration. The chances of normal recovery without treatment are very low in adults. Starting in childhood or adolescence can lead to lifelong OCD.[15]
On the other hand, the research finding showed that there is a significant relationship between the prevalence of OCD in patients with IBS and marital status, and most of the patients were single. In OCD epidemiological studies, the prevalence of this disorder in single people has been reported to be higher than in married people, and the important factor for remaining single is the obsession, which interferes with their interpersonal relationships.[14]
The results showed a significant relationship between the prevalence of OCD in patients with IBS and a history of OCD in the family and close relatives of the patient. However, there was no significant relationship between the prevalence of OCD and education level, job, income status, and place of residence. OCD is one of the most common mental disorders that affect all aspects of life, and due to the high prevalence of this disorder, which in addition to being considered as the underlying causes of IBS, in the long run, it also has devastating effects on interpersonal and social relationships.
Some studies have suggested that OCD is inherited and reports that a percentage of parents have patients with the disorder. Approximately 40% of people with OCD have a relative relationship with OCD.[34]
The results of Karimi et al.[35] study showed that 62.7% of people with OCD had a history of the disease in the maternal or paternal family, of which 18% had a history of OCD in the paternal family and 44.7% in the maternal family. 35% had no family history of OCD.
In OCD, family history, especially the mother's family, and the likelihood of developing OCD in families with the disorder is higher than a person without a family history.[34]
The limitation of the present study was that the samples only included patients with IBS in Kermanshah; therefore, generalizing the findings to patients in other geographical areas must be done carefully. This research was done by correlation method, based on which it was not possible to explain relationships; therefore, caution should be exercised in interpreting the results.
Conclusion
The findings of this study indicate a high prevalence of OCD in patients with IBS and there is a significant relationship between the prevalence of OCD and gender, age, marital status, and history of OCD in close relatives of patients with IBS. Therefore, considering the psychological issues and nonpharmacological treatments of these patients, considering the psychological etiology of this syndrome, combined with pharmacological treatments, can both reduce the symptoms and improve the patients with IBS and reduce the treatment costs of this disease. Be very effective. Therefore, in these patients, treatment of psychological problems is recommended along with the treatment of their disease.
It is suggested that in order to use combination therapies and make them more effective on patients with IBS, there should be close cooperation between gastroenterologists, psychiatrists and psychologists, and treatments should be performed as a team.
Financial support and sponsorship
Vice Chancellor for Research Affairs, Kermanshah university of Medical sciences, Kermanshah, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We also extend our thanks to clinical research development center of Imam Khomeini and Mohammad Kermanshahi and Farabi Hospitals affiliated to Kermanshah University of Medical Sciences for their kind support. (Grant number: 980087).
References
- 1.Muir JG, Varney JE, Ajamian M, Gibson PR. Gluten-free and low-FODMAP sourdoughs for patients with coeliac disease and irritable bowel syndrome: A clinical perspective. Int J Food Microbiol. 2019;290:237–46. doi: 10.1016/j.ijfoodmicro.2018.10.016. [DOI] [PubMed] [Google Scholar]
- 2.Cifre S, Gozalbo M, Ortiz V, Soriano JM, Merino JF, Trelis M. Blastocystis subtypes and their association with irritable bowel syndrome. J Medi Hypotheses. 2018;116:4–9. doi: 10.1016/j.mehy.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Afshar H, BagherianSararoodi R, Foroozandeh N, Khorramian N, Daghaghzadeh H, Merati MR, Adibi P. The relationship between Illness perception and symptom severity in patients with Irritable bowel syndrome. J Isfahan Med Sch. 2011;29:526–36. [Google Scholar]
- 4.Lacy BE, Mearin F, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel disorders. Gastroenterology. 2016;150:1393–407. doi: 10.1053/j.gastro.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 5.Quigley EM, Fried M, Gwee KA, Khalif I, Hungin AP, Lindberg G, et al. World gastroenterology organisation global guidelines irritable bowel syndrome: A global perspective update September 2015. J Clin Gastroenterol. 2016;50:704–13. doi: 10.1097/MCG.0000000000000653. [DOI] [PubMed] [Google Scholar]
- 6.Faeli A, Mohammadifar MA, Azizpour M, Dabiri R. Comparison of personality traits and quality of life between patients with irritable bowel syndrome and normal indiv iduals. J Clini Psycho. 2017;9:1–10. [Google Scholar]
- 7.Singh R, Salem A, Nanavati J, Mullin GE. The role of diet in the treatment of irritable bowel syndrome: A systematic review. Gastroenterol Clin North Am. 2018;47:107–37. doi: 10.1016/j.gtc.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Dibajnia P, Moghadasin M, KeykhayeFarzaneh MM. The Study of the relationship between psychological disorders with Irritable bowel syndrome. Pajouhandeh J. 2012;18:30–3. [Google Scholar]
- 9.Grundmann O, Yoon SL. Irritable bowel syndrome: Epidemiology, diagnosis and treatment: An update for health-care practitioners. J Gastroenterol Hepatol. 2010;25:691–9. doi: 10.1111/j.1440-1746.2009.06120.x. [DOI] [PubMed] [Google Scholar]
- 10.Posserud I, Svedlund J, Wallin J, Simrén M. Hypervigilance in irritable bowel syndrome compared with organic gastrointestinal disease. J Psychosom Res. 2009;66:399–405. doi: 10.1016/j.jpsychores.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 11.Gros DF, Antony MM, McCabe RE, Swinson RP. Frequency and severity of the symptoms of irritable bowel syndrome across the anxiety disorders and depression. J Anxiety Disord. 2009;23:290–6. doi: 10.1016/j.janxdis.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Masand PS, Keuthen NJ, Gupta S, Virk S, Yu-Siao B, Kaplan D. Prevalence of irritable bowel syndrome in obsessive-compulsive disorder. CNS Spectr. 2006;11:21–5. doi: 10.1017/s1092852900024123. [DOI] [PubMed] [Google Scholar]
- 13.Mahvi-Shirazi M, Fathi-Ashtiani A, Rasoolzadeh-Tabatabaei SK, Amini M. Comparison of mental health the mental health levels of patients suffering from irritable bowel synsrome, and inflammatory bowel disease, and healthy people. J of Resea in Psychologl Healt. 2008;2:75–83. [Google Scholar]
- 14.Safaralizadeh F, Hashemloo L, Bagheriyeh F, Motearefi H. The prevalence obsessive-compulsive disorder in students in Khoy University in 2013. Iran J Psychi Nurs. 2014;2:13–21. [Google Scholar]
- 15.American Psychiatric Association. Diagnoostic and Statistical Manual of Mental Disorder. In: Rezaee F, et al., editors. 5th Ed-DSM-5. American Psychiatric Publishing; 2013. Tehran: Arjmand Publication; 2015. [Google Scholar]
- 16.Sadock BJ, Sadock VA, Ruiz P. Synopsis of psychiatry. In: Rezaee F, editor. Behavioral Sciences/Clinical Psychiatry. Tehran: Arjmand Publication; 2015. [Google Scholar]
- 17.Brown LA, Wakschal E, Russman-Block S, Boisseau CL, Mancebo MC, Eisen JL, et al. Directionality of change in obsessive compulsive disorder (OCD) and suicidal ideation over six years in a naturalistic clinical sample. J Affect Disord. 2019;245:841–7. doi: 10.1016/j.jad.2018.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rachid F. Transcranial direct current stimulation for the treatment of obsessive-compulsive disorder? A qualitative review of safety and efficacy. Psychiatry Res. 2019;271:259–64. doi: 10.1016/j.psychres.2018.11.033. [DOI] [PubMed] [Google Scholar]
- 19.Lee C, Doo E, Choi JM, Jang SH, Ryu HS, Lee JY, et al. The increased level of depression and anxiety in irritable bowel syndrome patients compared with healthy controls: Systematic review and meta-analysis. J Neurogastroenterol Motil. 2017;23:349–62. doi: 10.5056/jnm16220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alhan C, Okan A. Irritable bowel syndrome, depression, and anxiety. East J Med. 2017;22:125–9. [Google Scholar]
- 21.Fond G, Loundou A, Hamdani N, Boukouaci W, Dargel A, Oliveira J, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): A systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. 2014;264:651–60. doi: 10.1007/s00406-014-0502-z. [DOI] [PubMed] [Google Scholar]
- 22.Cho HS, Park JM, Lim CH, Cho YK, Lee IS, Kim SW, et al. Anxiety, depression and quality of life in patients with irritable bowel syndrome. Gut Liver. 2011;5:29–36. doi: 10.5009/gnl.2011.5.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burke PM, Kocoshis S, Neigut D, Sauer J, Chandra R, Orenstein D. Maternal psychiatric disorders in pediatric inflammatory bowel disease and cystic fibrosis. Child Psychiatry Hum Dev. 1994;25:45–52. doi: 10.1007/BF02251099. [DOI] [PubMed] [Google Scholar]
- 24.Rachman S. A cognitive theory of compulsive checking. Behav Res Ther. 2002;40(6):625–639. doi: 10.1016/s0005-7967(01)00028-6. [DOI] [PubMed] [Google Scholar]
- 25.Kellner R. Psychosomatic syndromes, somatization and somatoform disorders. Psychother Psychosom. 1994;61:4–24. doi: 10.1159/000288868. [DOI] [PubMed] [Google Scholar]
- 26.Barbara G, Cremon C, Stanghellini V. Inflammatory bowel disease and irritable bowel syndrome: Similarities and differences. Curr Opin Gastroenterol. 2014;30:352–8. doi: 10.1097/MOG.0000000000000070. [DOI] [PubMed] [Google Scholar]
- 27.Graff LA, Walker JR, Bernstein CN. Depression and anxiety in inflammatory bowel disease: A review of comorbidity and management. Inflamm Bowel Dis. 2009;15:1105–18. doi: 10.1002/ibd.20873. [DOI] [PubMed] [Google Scholar]
- 28.Prasko J, Jelenova D, Mihal V. Psychological aspects and psychotherapy of inflammatory bowel diseases and irritable bowel syndrome in children. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2010;154:307–14. doi: 10.5507/bp.2010.046. [DOI] [PubMed] [Google Scholar]
- 29.Gradus JL, Qin P, Lincoln AK, Miller M, Lawler E, Sørensen HT, et al. Inflammatory bowel disease and completed suicide in Danish adults. Inflamm Bowel Dis. 2010;16:2158–61. doi: 10.1002/ibd.21298. [DOI] [PubMed] [Google Scholar]
- 30.Yoldascan E, Ozenli Y, Kutlu O, Topal K, Bozkurt AI. Prevalence of obsessive-compulsive disorder in Turkish university students and assessment of associated factors. BMC Psychiatry. 2009;9:40. doi: 10.1186/1471-244X-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salehi S, Mousavi AM, Sarichloo ME, Ghafelebashi H. Examined demographic characteristics and signs of obsessive-compulsive disorder. Quarterly J Sabzevar Univ Med Sci. 2014;21:343–51. [Google Scholar]
- 32.Caraveo Anduaga JJ, Colmena] s BE. The epidemiology of obsessive-compulsive disorder in Mexico City. Salud Mental. 2004;27:1–6. [Google Scholar]
- 33.Subramaniam M, Abdin E, Vaingankar JA, Chong SA. Obsessive-compulsive disorder: Prevalence, correlates, help-seeking and quality of life in a multiracial Asian population. Soc Psychiatry Psychiatr Epidemiol. 2012;47:2035–43. doi: 10.1007/s00127-012-0507-8. [DOI] [PubMed] [Google Scholar]
- 34.Rajeziesfahani S. Comparing the Efficacy of Meta-Cognitive and Cognitive-Behavioral Therapy on Patients Suffering from Obsessive-Compulsive Disorder. Ph.D Thesis Clinical Psychology, Shahed University Faculty of Humanity Science. 2015 [Google Scholar]
- 35.Maroufi A, Zarei M, Gharibi F. Evaluation of imprinting pattern in patients with obsessive-compulsive disorder in Sanandaj. Sci J Kurdistan Univ Med Sci. 2014;19(1):21–29. [Google Scholar]


