Abstract
Fibromyalgia has been increasing worldwide and is considered a public health problem. Nonpharmacological treatment through exercise and education is recommended for fibromyalgia management. In this sense, there is a need for interdisciplinary programs to promote health and improve symptoms in fibromyalgia. The purpose of this study was to verify the effectiveness of interdisciplinary health education programs for individuals with fibromyalgia. This is a systematic review that followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations and was registered at Prospective Register of Systematic Reviews (CRD4201913228). A search was conducted in the following databases: Scientific Electronic Library Online, Lilacs, Medical Literature Analysis and Retrieval System Online, Scopus, Web of Knowledge ISI, Physiotherapy Evidence Database, Excerpta Medica Database, Cumulative Index to Nursing and Allied Health Literature, Cochrane Library, and SPORTDiscus. The descriptors used were “Fibromyalgia” and “Health Education.” Clinical trials published between 1990 and 2019 were selected. The Jadad Quality Scale and the Cochrane Risk-of-Bias Tool were used to evaluate the risk of bias and the methodological quality of the clinical trials. The search found 2887 articles, and only two studies were included in the analysis. Both studies conducted the interventions through lectures and group activities. In particular, the topics most frequently approached at the interdisciplinary health education programs were general information about fibromyalgia, body practices, physical activities, and pharmacological approaches. An interdisciplinary health education program can improve pain and quality of life in people with fibromyalgia; however, evidence shows low methodological quality. This systematic review indicates that studies are of low quality, interfering with the effectiveness of interdisciplinary health education programs.
Keywords: Fibromyalgia, health education, health promotion, quality of life, rheumatic diseases
Introduction
There has been ample discussion on interventions to treat fibromyalgia (however, they are disciplinary and specific interventions),[1,2,3,4,5,6,7,8] a syndrome of complex multifactorial etiopathogenesis not totally known; characterized by widespread musculoskeletal pain and tenderness on palpation (tender points); frequently associated with fatigue, sleep disturbances, somatic and cognitive symptoms, and psychological disorders.[9]
The overall prevalence of fibromyalgia in the population ranges from 0.2% to 6.6%, and this syndrome affects mostly women.[10] In recent years, fibromyalgia has acquired greater significance and become a public health problem.[11] There are many reasons to justify this situation: prevalent growth in the adult population in general, insufficient knowledge of its cause and of the mechanisms that cause it, absence of symptom control, lack of a standardized care, and dissatisfaction of patients and professionals with the current therapeutic approaches.[12,13,14]
The most efficient strategy includes a combination of pharmacological[15] and nonpharmacological[16] interventions. Pharmacological support is an important complement, whereas nonpharmacological interventions focus on the process of adapting to and coping with fibromyalgia in day-to-day life.[17] For instance, physical exercise is beneficial to physical and functional abilities and fibromyalgia symptoms, whereas behavioral interventions can improve pain confrontation and reduce anxiety, which are the basis of fibromyalgia care management.[18]
The reviewed recommendations of the European League against Rheumatism for fibromyalgia management indicate that the initial strategy should focus on patient education and nonpharmacological interventions.[19] Health education is one of the main items to enable health promotion at primary health care (PHC) in Brazil.[20] It should prepare people to assume the control and responsibility over their own health and their territory health, as well as prepare them for empowerment, decision-making, participation, social control, and acting on the conditioning and determining factors of their health and quality of life.[21]
Due to the chronic nature of fibromyalgia, patients deal negatively with this syndrome and its consequences.[22] To tackle this problem, interdisciplinary care programs have been developed to promote the health of people with fibromyalgia.[23,24,25] These programs are directed to care optimization by means of instruction to patients provided by several professionals from different areas of knowledge, guiding them on how to control the pain and cope with the problems associated with their lifestyle.[26] These professionals interact to develop care praxis from the interdisciplinarity perspective, gathering people with different viewpoints and knowledge.[27] Thus, this systematic review of the literature aimed to assess the effectiveness of interdisciplinary health education programs for the treatment of fibromyalgia.
Materials and Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist.[28] The study was registered at the International Prospective Register of Systematic Reviews under no. CRD4201913228.
Search strategy
Eligibility criteria were as follows: (1) types of study – randomized or nonrandomized clinical trials; (2) type of participants – adults aged 18–59 years of both genders, classified with fibromyalgia according to the preliminary criteria of the American College of Rheumatology of 1990[29] or 2010;[3] (3) types of intervention – interdisciplinary health education program in at least one of the study groups; (4) types of outcome – biological, physical, nutritional, psychological, and social variables evaluated soon after the end of the intervention program; and (5) types of approach – programs developed in teams.
Exclusion criteria were as follows: update articles; articles of creation, validation, adaptation, translation, and feasibility of assessment tools; case reports; comments; comparative studies; database articles; editorials; case studies; prefaces; opinion articles; pilot studies; protocol registrations; ethnographies; guidelines; longitudinal studies; qualitative studies; reflection papers; abstracts; bibliographic reviews; critical reviews; integrative reviews; narrative reviews; systematic and meta-analysis reviews; case series; and cross-sectional studies. Studies conducted on children and adolescents; studies on interventions with health education associated with disciplinary approach; studies on other rheumatic disease treatments and integrative and complementary practices, disciplinary interventions, and individual health education interventions; and studies comparing the types of health education were also excluded from this survey.
A search was conducted in the following databases: Scientific Electronic Library Online, Literatura Latino-americana e do Caribe em Ciências da Saúde (LILACS), Medical Literature Analysis and Retrieval System Online, Scopus, Web of Knowledge ISI, Physiotherapy Evidence Database, Excerpta Medica Database, Cumulative Index to Nursing and Allied Health Literature, Cochrane Library, and SPORTDiscus (last access: March 19, 2019).
The following descriptors in Health Science (DeCS) and Medical Subject Headings (MeSH) were used: in Portuguese, “Fibromialgia” and “Educação em Saúde;” in English, “Fibromyalgia” and “Health Education;” and in Spanish “Fibromialgia” and “Educación em Salud.” At DeCS and MeSH, the Boolean operators “OR” and “AND” were used to create combined search topics.
Clinical trials published in Portuguese, English, and Spanish between 1990 and 2019 were searched. The search was limited to records published as of 1990, when the classification criteria of the American College of Rheumatology for fibromyalgia were published for the first time.[29]
Study selection
Two independent reviewers (MDA and FCNRL) selected the articles by title and abstract. The studies that met the eligibility criteria were analyzed and evaluated. After reading the selected studies in full, the reviewers verified whether there was any conflict between them. In case of disagreement between the reviewers, resolution was reached by consensus. When no consensus was achieved, a third reviewer was responsible for the decision.
Risk-of-bias assessment
The Jadad quality scale is a tool developed to evaluate the methodological quality of clinical trials that aims at decreasing the bias, that is, their internal validity. There are two response options in the scale items: yes or no. It comprises five items to be analyzed whose sum may result from 0 to 5 points. Its classification ranges from <3 points (high risk of bias) to ≥3 points (low risk of bias).[30]
The Cochrane Risk-of-Bias tool is used to evaluate the risk of bias and the methodological quality of clinical trials in a systematic review.[31] According to this tool, different domains associated with risk of bias are independently evaluated for each study: random sequence generation; allocation concealment; masking (blinding) of participants and team; masking (blinding) at outcome evaluation; outcome incomplete data; outcome selective reporting; and other sources of bias (potential biases). For each of these domains, the risk of bias is evaluated and classified as high, low, or unclear.
Analysis
Descriptive statistical analysis and the data extracted from the studies were cataloged as follows: first author/year of publication, country of origin, type of study, participants' characteristics (gender, age, and population), variables assessed and tools used for collection, activities performed at the educational interdisciplinary interventions and control groups, follow-up, baseline, and results.
Results
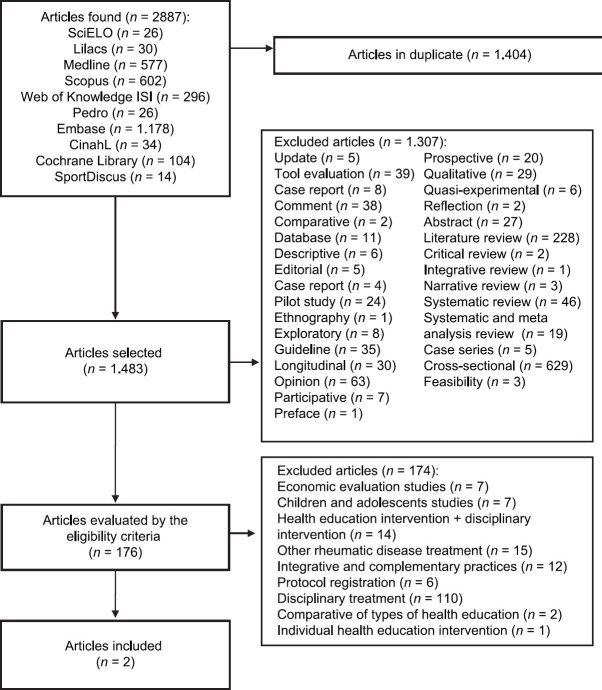
The search found 2887 articles, and two studies were selected for the present review after application of the exclusion criteria [Figure 1]. The first study found was that of Bosch Romero et al.[32] where after an interdisciplinary educational intervention, some dimensions of the quality of life of the instrument used related to pain improved, which suggests that health education for people with fibromyalgia changes their perception of quality of life and reduces pain. In addition, this type of activity increases understanding of the disease and reduces dependence on health services. The second study by Pereira Pernambuco et al.[33] after an intervention of 44 patients divided them into an experimental and a control group; the intragroup and intergroup analyses revealed that the treatment induced significant increases in chemochemical levels, highlighting that the intervention can promote the health of individuals with fibromyalgia. One study was conducted in Brazil and the other in Spain. There was no consistency regarding the analyzed variables and the evaluation tools [Table 1]. Table 2 shows the results obtained after evaluation of the studies regarding methodological quality using the Jadad Quality Scale and risk of bias using the Cochrane Risk-of-Bias Tool. The evidence quality showed that one study presented low risk of bias and the other presented high risk of bias. Regarding the finding of low methodological quality, double-blinding was the least satisfying criterion.
Figure 1.
Article selection flowchart
Table 1.
Comparison between the selected studies
| Author/year | Country of origin | Type of study | Age and gender of participants | Variables assessed (evaluation tool) | Interdisciplinary activities in health education | Control group | Follow- up | Baseline (Preintervention) | Outcomes (Postintervention) |
|---|---|---|---|---|---|---|---|---|---|
| Romero et al.[32] | Spain | RCCT | Participants SG: 32 Participants CG: 33 Age SG: 52.3±9.1 Age CG: 54.6±6.6 Gender: Female |
Quality of Life (Nottingham Health Profile) Psychic discomfort (Mini International Neuropsychiatric Interview) |
Number of meetings: 4 Duration: 1 h Frequency: Once a week Type of approach: Lectures and group activities Program content General information about the syndrome. Pharmacological treatments and physical-rehabilitative measures Physical exercise and behavioral hygiene Relaxation techniques |
No intervention performed | 1 month | Quality of Life SG Energy (M: 63.3) Emotion (M: 61.6) Pain (M: 85.0) Mobility (M: 45.6) Sleep (M: 68.0) Social isolation (M: 34.0) Quality of Life CG: Energy (M: 61.6) Emotion (M: 41.6) Pain (M: 78.7) Mobility (M: 38.7) Sleep (M: 61.0) Social Isolation (M: 11.0) Psychic Discomfort SG and CG: Not informed |
Quality of Life SG Energy (M: 58.3) Emotion (M: 61.6) Pain (M: 75.0) Mobility (M: 43.1) Sleep (M: 62.0) Social Isolation (M: 29.0) Quality of Life CG: Energy (M: 61.6) Emotion (M: 47.2) Pain (M: 86.8) Mobility (M: 45.0) Sleep (M: 64.0) Social Isolation (M: 15.0) Psychic Discomfort SG and CG: Not informed |
| Pernambuco et al.[33] | Brazil | RCCT | Participants SG: 21 Participants CG: 23 Age SG: 51.43±11.26 Age CG: 48.26±11.03 Gender: Female |
Cytokine levels (blood sample) Cortisol levels (saliva samples) Fibromyalgia impact (Fibromyalgia impact questionnaire - FIQ) |
No meetings: 9 Duration: 2 h Frequency: Once a week (with a 15-day interval between the 6th and 7th meetings) Type of approach content: Lectures and informal talks Program Therapeutic contact/workshop of senses Mental preparation Physical preparation Stress and individuality Symptoms Nutrition Chronicity consequence Types of treatment Activities to remember what has been learned |
No intervention performed | Not informed | Score FIQ SG (95% CI=−39.16) Cortisol levels SG (95% CI=0.18) Cytokines SG IL2 (95% CI=−1.39) IL4 (95% CI=0.14) IL6 (95% CI=−0.68) IL10 (95% CI=−0.08) TNF (95% CI=−0.38) IL17 (95% CI=−2.34) AC/CI ratio (95% CI=0.01) Score FIQ CG (95% CI=−4.57) Cortisol levels CG (95% CI=−1.40) Cytokines CG IL2 CG (95% CI=−1.58) IL4 CG (95% CI=−1.44) IL6 CG (95% CI=−4.80) IL10 CG (95% CI=−0.55) TNF CG (95% CI=−0.90) IL17 (95% CI=−4.68) AC/CI ratio (95% CI=−0.11) |
Score FIQ SG (95% CI=−21.56) Cortisol levels SG (95% CI=1.78) Cytokines SG IL2 (95% CI=0.27) IL4 (95% CI=1.39) IL6 (95% CI=−3.25) IL10 (95% CI=0.43) TNF (95% CI=0.46) IL17 (95% CI=3.19) AC/CI (95% CI=0.13) Score FIQ CG (95% CI=9.81) Cortisol levels CG (95% CI=0.74) Cytokines CG IL2 (95% CI=0.43) IL4 (95% CI=0.15) IL6 (95% CI=2.60) IL10 (95% CI=0.10) TNF (95% CI=0.28) IL17 (95% CI=6.75) AC/CI ratio (95% CI=0.47) |
RCCT=Randomized controlled clinical trial, SG=Study Group, CG=Control Group, M=Mean; FIQ=Fibromyalgia Impact Questionnaire
Table 2.
Assessment of the methodological quality and risk of bias of the studies using the Jadad Quality Score and the Cochrane Risk-of-Bias Tool
| Study quality evaluation Author (year) | Is it randomized? | Is it double blind? | Is there abandonment description? | Is the randomization method described? | Is the concealment method described? | Total Score |
|---|---|---|---|---|---|---|
| Romero et al.[32] | 1 | 0 | 1 | 0 | 0 | 2 |
| Pernambuco et al.[33] | 1 | 0 | 1 | 1 | 1 | 4 |
| Risk-of-bias assessment | Romero et al.[32] | Pernambuco et al.[33] | ||||
| Random sequence generation | ✓ | ✓ | ||||
| Allocation concealment | ✓ | ✓ | ||||
| Masking (blinding) of participants and team | ✗ | ✗ | ||||
| Masking (blinding) at outcome evaluation | ✗ | ✗ | ||||
| Outcome incomplete data | ✗ | ✓ | ||||
| Outcome selective reporting | ⓤ | ⓤ | ||||
| Other sources of bias | ✗ | ✗ | ||||
Low risk of bias: ✓, High risk of bias: ✗, Unclear risk of bias: ⓤ
Discussion
The studies included in this systematic review estimated the effect of interdisciplinary health education interventions for individuals with fibromyalgia compared with control groups.[32,33] It was observed that one interdisciplinary health education program improved pain and quality of life in individuals with fibromyalgia.
The interdisciplinary health education program proposed by Bosch Romero et al.[32] improved pain, and according to these authors, it consequently improved the quality of life. However, pain was the only one domain of the Nottingham Health Profile, and the others were energy, emotional reactions, physical mobility, sleep, and social isolation, and the combination of these dimensions was responsible for the quality of life of individuals. In contrast, the study by Pereira Pernambuco et al.[33] suggested that, from the results obtained, it can be said that health education may induce subjective and objective changes (immunological and neuroendocrine), which explains, at least partially, the improvement in the health status of individuals with fibromyalgia.
Both studies conducted the interventions through lectures and group activities. In particular, the topics most frequently approached at the interdisciplinary health education programs were general information about fibromyalgia, body practices, physical activities, and pharmacological approaches. Regarding intervention duration, a difference was observed between the two studies. Intervention varied from 4 (28 days)[32] to 11 weeks (77 days).[33] The literature suggests that program attendance time be, at least, 102 days – the time necessary for daily habit formation.[34]
One month after intervention, Bosch Romero et al.[32] evaluated the participants to verify the maintenance of the obtained results, whereas Pereira Pernambuco et al.[33] only analyzed pre- and post-intervention results. Currently, there is an increasing demand for the evaluation and monitoring of policies and social programs in which nongovernmental organizations are increasingly identifying the need to include methodologies to assess and monitor the results and impacts of the implemented programs. Assessment approaches are an important tool for research legitimacy in health education; however, there is still little conclusive evidence regarding several actions in health education. Thus, there is a need to stimulate the development of more efficient ways to evaluate programs, mainly the sustainability of these actions. In general, both studies provided meaningful benefits in some of the variables assessed (reduction of pain[32] and immunological and neuroendocrine changes,[33] but using different tools.
Health professionals and public policymakers should consider the costs and effectiveness of interdisciplinary health education programs for individuals with fibromyalgia. Although educational approaches are widely used at the practice and prevention of other health problems, the current evidence on interdisciplinary health education groups in fibromyalgia still needs to be clearer. Such evidence is essential for health professionals to know the best way to approach health education in individuals with fibromyalgia and be able to include it in PHC.
In this context, the need for other studies with higher quality, designed to establish sufficient and strong evidence for the adequate management of fibromyalgia symptoms, is evident. However, the conclusions of this review show a series of studies with low evidence and with some limitations. Therefore, comprehensive and well-planned assessments and interdisciplinary interventions in health education are needed for individuals with fibromyalgia.
Currently, the research group responsible for this review is conducting an important randomized clinical trial addressing the development of a protocol for an interdisciplinary health promotion program for individuals with fibromyalgia. Thus, the researchers may soon provide new, high-quality information on this theme. This study is expected to contribute to a better comprehension of the effectiveness of this intervention.
The present study's limitation was the limited number of studies analyzed in the scientific literature on educational interventions that promote health in people with fibromyalgia through the trial-clinical method. However, our article sought to use the articles that are considered to be the best levels of scientific evidence in order to find the answer to the proposed objective.
Conclusion
An interdisciplinary health education program can improve pain and quality of life in people with fibromyalgia; however, evidence shows low methodological quality. Researchers should consider the results of this systematic review when suggesting new interdisciplinary health education programs for people with fibromyalgia. It is important that health professionals should be trained and prepared to apply educational interventions for people with fibromyalgia and disseminate this possibility of care in every health network. New studies are suggested to strengthen the interdisciplinary educational actions that promote the health of people with fibromyalgia, as it is a topic that has shown great importance and has been indicated by many professionals, however studies have not been carried out with these important characteristics. Therefore, it is important to carry out studies that develop, apply, and evaluate educational health promotion interventions for individuals with fibromyalgia in PHC worldwide.
Financial support and sponsorship
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to acknowledge Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES).
References
- 1.Glasgow A, Stone TM, Kingsley JD. Resistance exercise training on disease impact, pain catastrophizing and autonomic modulation in women with fibromyalgia. Int J Exerc Sci. 2017;10:1184–95. doi: 10.70252/LAZD6794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Assunção Júnior JC, de Almeida Silva HJ, da Silva JFC, da Silva Cruz R, de Almeida Lins CA, de Souza MC. Zumba dancing can improve the pain and functional capacity in women with fibromyalgia. [Last accessed on 2020 Sep 13];J Bodyw Mov Ther. 2018 22:455–9. doi: 10.1016/j.jbmt.2017.09.022. Available from: https://doi.org/10.1016/j.jbmt. 2017.09.022 . [DOI] [PubMed] [Google Scholar]
- 3.Lazaridou A, Buliteanu A, Dorado K, Schreiber K. The effects of yoga on pain, fatigue, and catastrophizing in fibromyalgia. [Last accessed on 2020 Sep 13];J Pain. 2018 19:30–1. Available from: https://doi.org/10.1016/j.jpain.2017.12.075 . [Google Scholar]
- 4.Castro Sánchez AM, García López H, Fernández Sánchez M, Pérez Mármol JM, Aguilar-Ferrándiz ME, Luque Suárez A, et al. Improvement in clinical outcomes after dry needling versus myofascial release on pain pressure thresholds, quality of life, fatigue, pain intensity, quality of sleep, anxiety, and depression in patients with fibromyalgia syndrome. [Accessed on: 13 Sep. 2020];Disabil Rehabil. 2019 41:2235–46. doi: 10.1080/09638288.2018.1461259. Available from: https://doi.org/10.1080/096382 88.2018.1461259 . Ernberg M, Christidis N, Ghafouri B, Bileviciute-Ljungar I, Löfgren M, Bjersing J, et al. Plasma cytokine levels in fibromyalgia and their response to 15 weeks of progressive resistance exercise or relaxation therapy. Mediators Inflamm 2018;2018:1-14. Available from: https://doi.org/10.1155/2018/3985154. [Last accessed on 2020 Sep 13] [DOI] [PubMed] [Google Scholar]
- 5.Fioravanti A, Manica P, Bortolotti R, Cevenini G, Tenti S, Paolazzi G. Is balneotherapy effective for fibromyalgia? Results from a 6-month double-blind randomized clinical trial. [Last accessed on 2020 Sep 13];Clin Rheumatol. 2018 37:2203–12. doi: 10.1007/s10067-018-4117-z. Available from: https://doi.org/10.1007/s10067-018-4117-z . [DOI] [PubMed] [Google Scholar]
- 6.Mist SD, Jones KD. Randomized controlled trial of acupuncture for women with fibromyalgia: Group acupuncture with traditional Chinese medicine diagnosis-based point Selection. [Last accessed on 2020 Sep 13];Pain Med. 2018 19:1862–71. doi: 10.1093/pm/pnx322. Available from: https://doi.org/10.1093/pm/pn×322 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang C, Schmid CH, Fielding RA, Harvey WF, Reid KF, Price LL, et al. Effect of tai chi versus aerobic exercise for fibromyalgia: Comparative effectiveness randomized controlled trial. [Last accessed on 2020 Sep 13];BMJ. 2018 360:k851. doi: 10.1136/bmj.k851. Available from: https://doi.org/10.1136/bmj.k851 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. [Last accessed on 2020 Sep 13];Arthritis Care Res (Hoboken) 2010 62:600–10. doi: 10.1002/acr.20140. Available from: https://doi.org/10.1002/acr0.20140. A . [DOI] [PubMed] [Google Scholar]
- 9.Marques AP, Santo AD, Berssaneti AA, Matsutani LA, Yuan SL. A prevalência de fibromialgia: Atualização da revisão de literatura. [Last accessed on 2020 Sep 13];Rev Bras Reumatol. 2017 57:356–63. doi: 10.1016/j.rbre.2017.01.005. Available from: http://dx.doi.org/10.1016/j.rbre. 20170.01.005 . [DOI] [PubMed] [Google Scholar]
- 10.Brandão PM, Jr, Besset VL. Dor crônica: Um problema de saúde pública, uma questão para a psicanálise. Polêm!ca. 2015;15:25–41. Available from: https://doi.org/10.12957/polemica. 2015.19359 . [Google Scholar]
- 11.Ruiz Pérez I, Ubago Linares MC, Bermejo Pérez MJ, Plazaola Castaño J, Olry de Labry-Lima A, Hernández Torres E. Differences in sociodemographic, clinical, psychosocial and health care characteristics between men and women diagnosed with fibromyalgia. [Last accessed on 2020 Sep 13];Rev Clin Esp. 2007 207:433–9. doi: 10.1157/13109832. Available from: https://doi.org/10.1157/13109832 . [DOI] [PubMed] [Google Scholar]
- 12.Sicras-Mainar A, Rejas J, Navarro R, Blanca M, Morcillo A, Larios R, et al. Treating patients with fibromyalgia in primary care settings under routine medical practice: A claim database cost and burden of illness study. [Last accessed on 2020 Sep 13];Arthritis Res Ther. 2009 11:R54. doi: 10.1186/ar2673. Available from: https://doi.org/10.1186/ar2673 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgs JB. Fibromyalgia in primary care. [Last accessed on 2020 Sep 13];Prim Care. 2018 45:325–41. doi: 10.1016/j.pop.2018.02.008. Available from: https://doi.org/10.1016/j.pop.2018.02.008 . [DOI] [PubMed] [Google Scholar]
- 14.Rowe CA, Sirois FM, Toussaint L, Kohls N, Nöfer E, Offenbächer M, et al. Health beliefs, attitudes, and health-related quality of life in persons with fibromyalgia: Mediating role of treatment adherence. [Last accessed on 2020 Sep 13];Psychol Health Med. 2019 24:962–77. doi: 10.1080/13548506.2019.1576913. Available from: https://doi.org/10.1080/13548506.2019.1576913 . [DOI] [PubMed] [Google Scholar]
- 15.Conversano C, Poli A, Ciacchini R, Hitchcott P, Bazzichi L, Gemignani A. A psychoeducational intervention is a treatment for fibromyalgia syndrome. Clin Exp Rheumatol. 2019;37(Suppl 116):98–104.4. [PubMed] [Google Scholar]
- 16.Oliveira JO, Jr, Almeida MB. The current treatment of fibromyalgia. [Last accessed on 2020 Sep 13];Br J Pain. 2018 1:255–62. Available from: https://doiorg/105935/2595-011820180049 . [Google Scholar]
- 17.Sosa-Reina MD, Nunez-Nagy S, Gallego-Izquierdo T, Pecos-Martín D, Monserrat J, Álvarez-Mon M. Effectiveness of therapeutic exercise in fibromyalgia syndrome: A systematic review and meta-analysis of randomized clinical trials. [Last accessed on 2020 Sep 13];Biomed Res Int. 2017 17(1):1–14. doi: 10.1155/2017/2356346. Available from: https://doi.org/10.1155/2017/2356346 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Fluß E, et al. EULAR revised recommendations for the management of fibromyalgia. [Last accessed on 2020 Sep 13];Ann Rheum Dis. 2017 76:318–28. doi: 10.1136/annrheumdis-2016-209724. Available from: https://doi.org/10.1136/annrheumdis-2016-209724 . [DOI] [PubMed] [Google Scholar]
- 19.Carneiro AC, de Souza V, Godinho LK, de Faria IC, Silva KL, Gazzinelli MF. Health promotion education in the context of primary care. [Last accessed on 2020 Sep 13];Rev Panam Salud Publica. 2012 31:115–20. doi: 10.1590/s1020-49892012000200004. Available from: https://doi.org/10.1590/s1020-49892012000200004 . [DOI] [PubMed] [Google Scholar]
- 20.Candeias NM. Conceitos de educação e de promoção em saúde: Mudanças individuais e mudanças da saúde no contexto da atenção primária. [Last accessed on 2020 Sep 13];Rev Panam Salud Publica. 2012 31:115–20. Available from: https://doi.org/10.1590/S0034-89101997000200016 . [Google Scholar]
- 21.Rolls C, Prior Y. Non-pharmacological interventions for people with fibromyalgia: A systematic review. [Last accessed on 2020 Sep 13];Rheumatol. 2018 57:164–5. Available form: https://doi.org/10.1093/rheumatology/key075.509 . [Google Scholar]
- 22.Ablin J, Fitzcharles MA, Buskila D, Shir Y, Sommer C, Häuser W. Treatment of fibromyalgia syndrome: recommendations of recent evidence-based interdisciplinary guidelines with special emphasis on complementary and alternative therapies. [Last accessed on 2020 Sep 13];Evid Based Complement Alternat Med. 2013 13(1):1–7. doi: 10.1155/2013/485272. Available from: https://doi.org/10.1155/2013/485272 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giusti EM, Castelnuovo G, Molinari E. Differences in multidisciplinary and interdisciplinary treatment programs for fibromyalgia: A mapping review. [Last accessed on 2020 Sep 13];Pain Res Manag. 2017 17(1):1–19. doi: 10.1155/2017/7261468. Available from: https://doi.org/10.1155/2017/7261468 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Montesó-Curto P, García-Martinez M, Romaguera S, Mateu ML, Cubí-Guillén MT, Sarrió-Colas L, et al. Problems and solutions for patients with fibromyalgia: Building new helping relationships. [Last accessed on 2020 Sep 13];J Adv Nurs. 2018 74:339–49. doi: 10.1111/jan.13412. Available from: https://doi.org/10.1111/jan.13412 . [DOI] [PubMed] [Google Scholar]
- 25.Marques AP, Matsutani LA, Ferreira EA, Mendonça LL. A fisioterapia no tratamento de pacientes com fibromialgia: Uma revisão da literatura. Rev Bras Reumatol. 2002;42:42–8. [Google Scholar]
- 26.Miranda NA, Berardinelli LM, Sabóia VM, Brito ID, Santos RD. Interdisciplinary care praxis in groups of people living with fibromyalgia. [Last accessed on 2020 Sep 13];Rev Bras Enferm. 2016 69:1115–23. doi: 10.1590/0034-7167-2016-0279. Available from: https://doi.org/10.1590/0034-7167-2016-0279 . [DOI] [PubMed] [Google Scholar]
- 27.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. [Last accessed on 2020 Sep 13];Syst Rev. 2015 4:1. doi: 10.1186/2046-4053-4-1. Available from: https://doi.org/10.1136/bmj.g7647 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. [Last accessed on 2020 Sep 13];Arthritis Rheum. 1990 33:160–72. doi: 10.1002/art.1780330203. Available from: https://doi.org/10.1002/art. 1780330203 . [DOI] [PubMed] [Google Scholar]
- 29.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? [Last accessed on 2020 Sep 13];Control Clin Trials. 1996 17:1–2. doi: 10.1016/0197-2456(95)00134-4. Available from: https://doi.org/10.1016/0197-2456 (95) 00134-4 . [DOI] [PubMed] [Google Scholar]
- 30.Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Versão 5.1.0. United Kingdom: The Cochrane Collaboration; 2011. Available from: https://handbook-5-1.cochrane.org . Updated March 2011. [Google Scholar]
- 31.Bosch Romero E, Sáenz Moya N, Valls Esteve M, Viñolas Valer S. Study of quality of life of patients with fibromyalgia: Impact of a health education programme. [Last accessed on 2020 Sep 13];Aten Primaria. 2002 30:16–21. doi: 10.1016/S0212-6567(02)78958-0. Available from: https://doi.org/10.1016/s0212-6567 (02) 78958-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pereira Pernambuco A, de Souza Cota Carvalho L, Pereira Leite Schetino L, Cunha Polese J, de Souza Viana R, d' Ávila Reis D. Effects of a health education program on cytokines and cortisol levels in fibromyalgia patients: A randomized controlled trial. [Accessed on: 13 Sep. 2020];Adv Rheumatol. 2018 58:21. doi: 10.1186/s42358-018-0022-z. Available from: https://doi.org/10.1186/s42358-018-0022-z . [DOI] [PubMed] [Google Scholar]
- 33.Lally P, Van Jaarsveld CH, Potts HW, Wardle J. How are habits formed: Modelling habit formation in the real world. [Accessed on: 13 Sep. 2020];Eur Jn Soc Psychol. 2010 40:998–1009. Available from: https://doi.org/10.1002/ejsp. 674 . [Google Scholar]
- 34.Boland L, Légaré F, Carley M, Graham ID, O'Connor AM, Lawson ML, et al. Evaluation of a shared decision making educational program: The Ottawa Decision Support Tutorial. [Accessed on: 13 Sep. 2020];Patient Educ Couns. 2019 102:324–31. doi: 10.1016/j.pec.2018.09.008. Available from: https://doi.org/10.1016/j.pec. 2018.09.008 . [DOI] [PubMed] [Google Scholar]