Abstract
BACKGROUND:
Musculoskeletal pain is highly prevalent among office workers and causes high costs to the public health system. Strategies including education and exercise are recommended, with major benefits when conducted by physical therapists in the occupational environment. However, the required investment is uncommon among companies. This study aimed to evaluate the efficacy of a multimodal physiotherapy intervention to relieve musculoskeletal pain in office workers.
MATERIALS AND METHODS:
The study employed a single group study with a pre-post study design and was conducted at Universidad San Jorge in 2018. Outcome variables were: workplace ergonomics (INSHT Guide), existence and severity of musculoskeletal disorders (Nordic Musculoskeletal Questionnaire), musculoskeletal pain intensity (Numeric Rating Scale), and Clinical Global Impression Scale. Office workers in a university setting (n = 24, 19 females) were assessed at baseline, after 4 weeks of in-person sessions and following 3 weeks of autonomous performance. The physiotherapy program included education, ergonomic supervision, self-treatment, strengthening, and stretching exercises. A repeated-measures ANOVA or Friedman test (with post hoc comparisons) and Chi-squared test were used to compare the study variables.
RESULTS:
At baseline, cervical spine (54%), shoulder (42%), and lumbar regions (37.5%) were the most symptomatic regions according to the Nordic Musculoskeletal Questionnaire. Even if the proportion of symptomatic areas did not decrease significantly after the intervention, a great reduction of musculoskeletal pain intensity was observed after the program in the cervical (P < 0.001), lower back (P = 0.005), shoulder (P = 0.006) regions, and in the overall pain level (P < 0.001).
CONCLUSIONS:
These results support that a multimodal physiotherapy program can relieve work-related musculoskeletal pain in office workers and serve as a basis for future controlled trials.
Keywords: Musculoskeletal diseases, musculoskeletal pain, office workers, physiotherapy
Introduction
Musculoskeletal pain is the greatest cause of disability in developed countries, representing a public health problem with great economic repercussions.[1] The proliferation of office-based work contributes to the global rise in the prevalence of work-related musculoskeletal disorders.[2] European countries show the highest prevalence, with around 50% of office workers suffering neck and upper limb pain and over 30% displaying low back pain.[3,4,5]
Office workers are those who use a data-display screen at work for >4 h daily or 20 h weekly.[6] They are recognized as a population at risk of developing musculoskeletal disorders involving pain and disability in the long term.[3,7] Work-related musculoskeletal disorders in office workers have shown to be associated with occupational features such as the maintenance of static positions for excessive time periods or inappropriate postural and ergonomic hygiene, as well as the work environment and poor workstation design.[7,8] Furthermore, a sedentary lifestyle and low levels of physical activity are associated with higher levels of musculoskeletal pain and disability.[9]
Occupational medicine recommends resolving or alleviate musculoskeletal symptoms quickly and effectively once occurring to reduce workers' disability and sick leaves.[10] However, strategies cannot be limited to solve the episodic symptomatic exacerbations, but also proper preventive actions are necessary to avoid chronicity and recurrent events of musculoskeletal pain.
Industrial physical therapists increase the effectiveness of the prevention and management of musculoskeletal disorders by helping preventive services to carry out more individualized ergonomics for the workstations and providing considerable advantages in injury prognosis and recovery thanks to their direct therapeutic intervention.[11,12] The development of fitness programs at the workplace, designed and led by physical therapists, seems to offer considerable benefits. These programs include physical exercise before and during the workday, helping to improve workers' body awareness and physical attitude, while at the same time promoting more effective coping mechanisms to take on their workload.[11,12,13,14]
The main objective of this study was to assess the effectiveness of a multimodal physiotherapy program to relieve musculoskeletal pain in volunteer office workers. In addition, the ergonomic conditions of the workstations and the level of workers' satisfaction with the program were evaluated to propose future actions.
Materials and Methods
Study design
A longitudinal pre-post study was carried out during the months of March, April, and May 2018 in a population made up of office workers at the Universidad San Jorge (Zaragoza, Spain). The University Ethics Committee approved the study (reference: USJ: 008-18/19), which was carried out with respect to the agreements of the Declaration of Helsinki.
Participants
Participants were recruited voluntarily from the university setting through internal announcements. Inclusion criteria included: working with data display screens for >4 h daily or >20 h weekly, being an active worker at the university for >1 year and providing informed written consent. Exclusion criteria were: receiving physiotherapy treatment 1 month before the beginning of the study, any history of recent surgery, peripheral or central nervous system neurological disease, having suffered any kind of mental health disorder during the past 3 years, including anxiety and depression. To receive or implement any physiotherapy treatment during the study period or not complete, at least 80% of the in-person sessions were considered withdrawal criteria.
An estimated pilot study sample size for matched pairs was conducted using G*Power (version 3.1.9.2, Dusseldorf, Germany). The calculations were based on a standard deviation (SD) of 2.7 points in the pain NRS in office workers,[15] and a within-group difference of 2 points, which is considered the clinically important difference for the pain NRS.[16] Twenty-three subjects were estimated to obtain an alpha level of 0.05, a desired power of 80%, a Cohen's d of 0.7, and accounting for a 20% rate of possible dropouts.
Outcomes
In the initial assessment, carried out in the workplace, the socio-demographic data were recorded and a technician from the prevention department carried out the assessment of the workstations design and the participants' ergonomics, based on the technical guide of the Spanish National Institute of Safety and Health at Work (INSHT) that assesses working conditions of computer workers.[6]
Every clinical outcome was measured before intervention (pre-intervention), after the in-person phase of the physical therapy and education program, lasting 4 weeks (post-intervention) and finally, on completion of the autonomous follow-up phase lasting 3 weeks (follow-up), as presented in Table 1.
Table 1.
Assessment and physiotherapy intervention
| Assessment 1 (preintervention) | |
|---|---|
| One theoretical group session (week 1) | Health education |
| Work-related musculoskeletal diseases, pain and contributing factors (20’) | |
| Postural hygiene and healthy habits at the workstation (20’) | |
| Participants questions (10’) | |
| Individual workplace ergonomics supervision (week 1) | Workplace ergonomic |
| Adjustments of equipment and workers’ use (15’) | |
| Four practical group sessions (weeks 1 to 4) | Therapeutic exercises and pain education |
| Session 1 (week 1) | |
| Breathing exercises (10’) | |
| Body awareness in static positions and dynamic activities (10’) | |
| Activation-relaxation techniques for the cervical and oculomotor muscles (15’) | |
| Self-stretching of cervical and upper extremity muscles (levator scapulae, upper trapezius, pectoralis major, medial and lateral epicondyle muscles) (15’) | |
| Educational support about participants’ pains, beliefs and coping strategies during the exercises | |
| Session 2 (week 2) | |
| Breathing exercises (5’) | |
| Body awareness in static positions and dynamic activities (5’) | |
| Activation-relaxation techniques for the cervical and oculomotor muscles (5’) | |
| Self-stretching of cervical and upper extremity muscles: levator scapulae, upper trapezius, pectoralis major, medial and lateral epicondyle muscles (10’) | |
| Spinal motor control exercises (15’) | |
| Self-stretching of pelvic and lower extremity muscles: iliopsoas, hip external rotators, rectus femoris, and hamstrings (15’) | |
| Educational support about participants’ pains, beliefs, and coping strategies during the exercises | |
| Session 3 (week 3) | |
| Activation-relaxation techniques for the cervical and oculomotor muscles (5’) | |
| Self-stretching of cervical and upper extremity muscles: levator scapulae, upper trapezius, pectoralis major, medial and lateral epicondyle muscles (5’) | |
| Spinal motor control exercises (10’) | |
| Self-stretching of pelvic and lower extremity muscles: iliopsoas, hip external rotators, rectus femoris, and hamstrings (10’) | |
| Strengthening exercises of abdominal and pelvic floor muscles (15’) | |
| Myofascial release of tender points using the 3-tool (10’) | |
| Educational support about participants’ pains, beliefs and coping strategies during the exercises | |
| Session 4 (week 4) | |
| Breathing exercises (5’) | |
| Body awareness in static positions and dynamic activities (5’) | |
| Activation-relaxation techniques for the cervical and oculomotor muscles (5’) | |
| Self-stretching of cervical and upper extremity muscles: levator scapulae, upper trapezius, pectoralis major, medial and lateral epicondyle muscles (5’) | |
| Spinal motor control exercises (5’) | |
| Self-stretching of pelvic and lower extremity muscles: iliopsoas, hip external rotators, rectus femoris, and hamstrings (5’) | |
| Strengthening exercises for abdominal and pelvic floor muscles (10’) | |
| Myofascial release of tender points using the 3-tool (10’) | |
| Educational support about participants’ pains, beliefs and coping strategies during the exercises | |
| Assessment 2 (postintervention) | |
| Follow up phase (weeks 5- 7) | Therapeutic exercises and workplace ergonomics |
| Autonomous performance by workers with audiovisual support | |
| Weekly supervision by the physical therapist in the workplace | |
| Assessment 3 (Follow-up) | |
Standardized Nordic Musculoskeletal Questionnaire
The existence and severity of musculoskeletal disorders were assessed through the Standardized Nordic Musculoskeletal Questionnaire, which is divided into two parts. The general part consists of 27 questions with a dichotomous response (Yes/No) about musculoskeletal symptoms both during the past 12 months and the past 7 days. All these questions refer to 5 body regions: neck, shoulders, low back, elbows/forearms, wrists/hands, including a corporal diagram seen from behind. The specific part of the questionnaire delves into the analysis of symptoms in the lumbar, neck, and shoulder regions with a dichotomous response (Yes/No) and with the timing of the problem. In addition, it presents a specific question about the treatment received (Yes/No).[17,18,19]
Numeric Rating Scale
Pain intensity during the past 7 days, using a 0–10 Numeric Rating Scale (NRS: 0 “no pain” and 10 “worst imaginable pain”) was quantified for each body region and overall (both mean and maximum). The NRS is a unidimensional measure of pain intensity in adults and has high sensitivity as a simple and reproducible representation of pain severity.[20]
Level of physical activity
The level of regular physical activity was assessed using the International Physical Activity Questionnaire, short-form (IPAQ-SF), which considers three ranges according to the frequency and duration of physical activity during the last week: high (= 8.0 metabolic equivalent [METs]), moderate (=4.0 METs), and low level (=3.3 METs).[21] Differently than the other outcomes, IPAQ-SF was measured just before the intervention.
Clinical Global Impression
Self-perception of health state was quantified through the Clinical Global Impression (CGI). It comprises the CGI-Severity scale, assessing the severity of pathology (1 = normal to 7 = among the most extremely ill patients) and the CGI-Improvement scale to measure the change from the start of the treatment (1 = “very much improved” to 7 = “very much worse”).[22]
Ad-hoc satisfaction questionnaire
Finally, participants were asked to complete a Likert-like “ad hoc” questionnaire (1 = “completely disagree” to 5 = “completely agree”) to evaluate the education received, as well as the usefulness and level of personal satisfaction with the program, both globally and regarding every specific intervention modality.
Intervention
The intervention began with a theoretical education session on work-related musculoskeletal pain and contributing factors, accompanied by ergonomics and healthy habits to be adopted at the workplace. Then, the subjects were supervised on an individual basis in their workstations, where they were monitored in the ergonomic adaptations and requested to apply the knowledge they had learned.
Then, workers started the in-person physiotherapy program, comprising four group sessions (1 per week) of 60 min duration, led by a physical therapist [Table 1]. Participants received: exercises on body awareness in different work and daily life activities, conducted to prevent musculoskeletal fatigue and discomfort; guided breathing exercises to alleviate mental fatigue, pain and stress at work; self-stretching of the muscle groups especially taxed by the computer work; exercises on the activation and relaxation of the cervical and ocular-motor muscles; motor control exercises to balance deep and superficial spine muscles, as well as abdominal and pelvic floor muscle strengthening.[12,13,14] In addition, they were introduced to the autonomous use of the 3-tool instrument for musculoskeletal pain self-treatment through myofascial release.[23] All the contents practiced were accompanied by pain education, addressing negative beliefs influencing the onset of pain and learning active strategies to cope with stress and pain during the working day.[24] Workers were encouraged to complement the in-person sessions by performing the learned exercises every day. The guided exercise and education program was carried out in two groups so as to include all of the participants without affecting the quality of the intervention.
After concluding the first 4 weeks, participants were asked to continue performing the program independently in their workstations, on a daily basis. They received support from videos for this purpose. The autonomous follow-up phase lasted for 3 weeks, with individual supervision once a week by the physiotherapist.
The full program, including assessments, in-person intervention and latter autonomous phase, which extended over 7 consecutive weeks, was carried out during the working hours and in the working facilities.
Statistical analysis
Statistical analysis was carried out with the SPSS 24.0 version (IBM Corporation, Armonk, NY, USA) and the SigmaPlot 11.0 version application (Systat Software, Canada). For the descriptive analysis, the mean and SD or the median and interquartile range and numbers (percentages) were used. In order to determine the normality of the quantitative variables, the Shapiro–Wilk test was used. Based on these results, a repeated-measures ANOVA or Friedman test was used to compare the study variables, along with multiple post hoc comparisons (Bonferroni or Dunn-Sidak) when necessary. To analyze the results concerning the presence of pain in the different areas before and after the intervention, a comparison of proportions was conducted using the Chi-squared test.
Pearson or Spearman correlations were carried out to analyze the relationship between physical activity level and musculoskeletal pain. The strength of correlations was interpreted as low (0.00–0.25), fair (0.25–0.50), moderate to good (0.50–0.75), and good to excellent (>0.75).[25]
Statistical analysis was carried out at a confidence level of 95% and a statistical significance of P < 0.05 for all comparisons.
Results
A total of 29 participants were accepted for this study, of whom 5 were excluded because their work schedule or load were not compatible with the program sessions. The basal characteristics of the 24 workers who completed the study are shown in Table 2 (40 years of age ± 7.9; with 79% being female). The highest percentage (41.7%) was individuals with a moderate level of physical activity (1145 METs/min/week), followed by 33.3% with a low level (1065 METs/min/week) and 25% with a high regular physical activity level (4582 METs/min/week). On average, they declared to spend 8.6 h per day sitting, being the participants with low levels of physical activity who reported more time sitting (9.6 h ± 1.5). Neither gender nor physical activity nor sitting time was associated with any of the studied musculoskeletal pain features (P > 0.05).
Table 2.
Description of the sample (n=24)
| Characteristics | Category | Percentage |
|---|---|---|
| Gender | Male | 21 |
| Female | 79 | |
| Age (years) | <30 | 8.3 |
| 31- 35 | 20.8 | |
| 36- 40 | 29.2 | |
| 41- 45 | 29.2 | |
| 46- 50 | 0 | |
| 51- 55 | 4.2 | |
| >55 | 8.3 | |
| Time with the company (years) | 1- 3 | 25 |
| 4- 6 | 8 | |
| 7- 9 | 25 | |
| >10 | 42 | |
| Department | Corporate development | 17 |
| Finance | 8 | |
| Personnel management | 8 | |
| Research and company | 4 | |
| Quality control unit | 13 | |
| Academic organization | 8 | |
| Institute of technology | 4 | |
| Infrastructures | 4 | |
| Information systems | 13 | |
| Institute of languages | 8 | |
| Library | 4 | |
| General secretariat | 4 | |
| IPAQ | High physical activity | 25 |
| Moderate physical activity | 41.7 | |
| Low physical activity | 33.3 |
IPAQ: International physical activity questionnaire, short version
During the assessment of the workstations, corrections were necessary for a large percentage of the studied workers regarding equipment use, workplace furniture and humidity values, as summarized in Table 3. All the deficiencies related to the use of equipment by workers were corrected in the first intervention session and supervised throughout the program.
Table 3.
Initial assessment of the workstations based on the INSHT guidebook
| Analysis of workstations | Correct stations (%) | Stations requiring correction (%) |
|---|---|---|
| Equipment and furniture | ||
| The screen distance is correct | 71 | 29 |
| The screen height is correct | 37.5 | 62.5 |
| The keyboard is appropriate in terms of regulation and size | 21 | 79 |
| The mouse adapts correctly | 92 | 8 |
| The work table is appropriate in terms of size | 100 | 0 |
| The work table is appropriate in terms of stability | 100 | 0 |
| The work table height may be adjusted | 0 | 100 |
| The chair height may be adjusted | 67 | 33 |
| The chair has all of the regulation elements in proper functioning | 37.5 | 62.5 |
| The seat back can recline | 92 | 8 |
| The seat offers support for the entire back | 25 | 75 |
| The seat has an extension for lower back support | 100 | 0 |
| The seat has armrests | 0 | 100 |
| If there are armrests, they allow you to approach the table | - | - |
| The general state of the chair (tapestry, plastics, regulators) is appropriate | 8 | 92 |
| A mat is needed | 42 | 58 |
| A footrest is needed | 92 | 8 |
| A stand is needed | 4 | 96 |
| Work environment | ||
| The station dimensions permit changes in posture and freedom of movement | 83 | 17 |
| Lighting | ||
| The light available in the workstation is sufficient | 100 | 0 |
| There is the possibility of a direct glare (visual disturbances caused by strong light) due to the orientation of the station | 100 | 0 |
| Reflections are avoided (caused by light sources or other bright elements around the screen, keyboard or work surface) | 100 | 0 |
| Noise | ||
| The noise level allows for appropriate working | 100 | 0 |
| Humidity | ||
| The humidity of the environment is appropriate | 21 | 79 |
Concerning the existence of musculoskeletal pain at baseline, assessed through the Nordic Musculoskeletal Questionnaire, 70.8% of the office workers presented musculoskeletal pain during the past year, with the most prevalent being those of the cervical, lower back, and shoulder areas. However, only 42% of the participants had received any therapeutic attention to relieve their symptoms [Table 4].
Table 4.
Musculoskeletal symptomology and treatment received during the past 12 months according to the Nordic Musculoskeletal Questionnaire
| Location | No (%) | Yes (%) | Time of discomfort (%) | Treatment received | |
|---|---|---|---|---|---|
| No (%) | Yes (%) | ||||
| Neck | 33 | 67 | 1: 21 | 58 | 42 |
| 2: 4 | |||||
| 3: 25 | |||||
| 4: 17 | |||||
| Shoulder | 41.7 | 58,3 | 1: 20.8 | 62.5 | 37.5 |
| 2: 0 | |||||
| 3: 16.7 | |||||
| 4: 20.8 | |||||
| Lower back | 33 | 67 | 1: 21 | 71 | 29 |
| 2: 21 | |||||
| 3: 17 | |||||
| 4: 8 | |||||
| Elbow/Forearm | 75 | 25 | 1: 4 | 92 | 8 |
| 2: 17 | |||||
| 3: 4 | |||||
| 4: 0 | |||||
| Wrist/Hand | 79 | 21 | 1: 8 | 100 | 0 |
| 2: 13 | |||||
| 3: 0 | |||||
| 4: 0 | |||||
*1: 1-7 days *2: 8-30 days *3: more than 30 days, but not every day *4: every day.
In relation to the dichotomous variable that establishes the presence or lack of musculoskeletal pain in each body area over the past 7 days, complete symptoms relief was observed at the cervical and shoulder regions after completing all the program in a proportion of participants (16% and 9%, respectively) and complete low back pain relief was achieved by 12.5% of the workers after the first part of the intervention. However, the post hoc analysis revealed no statistical significance (P > 0.05) for the cited improvements when comparing the baseline, post in-person intervention (week 4) and follow-up (week 7) assessments [Figure 1].
Figure 1.
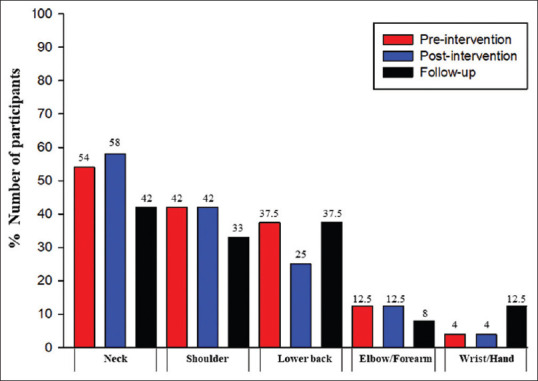
Presence of musculoskeletal pain according to the Nordic Musculoskeletal Questionnaire (past 7 days)
Regarding the intervention effects, the level of pain for the cervical, shoulder, and lower back regions was reduced after completing the entire program, as compared to the initial assessment. These improvements, which reached a pain reduction over 50%, were significant for the neck (P = 0.001), shoulder (P = 0.006) and low back area (P = 0.005), the latter displaying this decrease already after the in-person intervention (P = 0.001) [Table 5].
Table 5.
Level of pain in the distinct body areas during the last 7 days according to the Numeric Rating Scale (0- 10)
| Location | Mean (SD) | Percentage of improvement | P | ||||
|---|---|---|---|---|---|---|---|
| Pre | Post | FU | Post-pre | FU-pre | Post-pre | FU-pre | |
| Neck | 4.59 (3.66) | 3.40 (3.26) | 2.09 (2.80) | 25.92 | 54.46 | 0.107 | 0.001** |
| Shoulder | 3.50 (3.60) | 3.08 (3.23) | 1.74 (2.78) | 12.00 | 49.71 | 0.900 | 0.006* |
| Lower back | 3.83 (3.38) | 1.08 (2.20) | 1.74 (2.50) | 71.80 | 54.56 | 0.001** | 0.005* |
| Elbow/forearm | 1.33 (2.93) | 0.58 (1.61) | 0.52 (1.38) | 56.39 | 60.90 | 0.186 | 0.186 |
| Wrist/hand | 0.92 (2.20) | 0.54 (0.57) | 0.58 (0.68) | 41.30 | 36.95 | 0.063 | 0.063 |
SD=Standard deviation, PRE=Pre-intervention, POST=Postintervention, FU=Follow-up. Using Friedman test. *For P < 0.05; **for P < 0.001
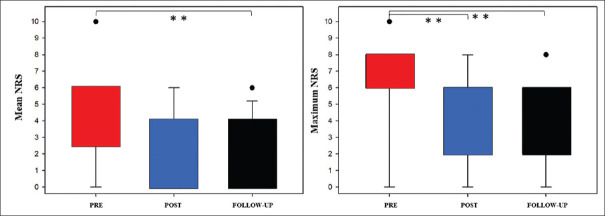
Analyzing changes in the average overall pain intensity, there were significant differences (P < 0.05) between preintervention (4.00 ± 2.43) and follow-up assessment (2.26 ± 1.84). Furthermore, the maximum overall pain intensity decreased significantly after the in-person intervention of the program (4.00 ± 2.83) as compared to the baseline values (6.10 ± 2.73), and maintained this significant reduction in the follow-up assessment, immediately after concluding the autonomous phase (3.22 ± 2.40) (P < 0.05) [Figure 2]. On the other hand, there was no statistical relevance with respect to the CGI comparisons (P > 0.05) between preintervention (2.67 ± 1.58), postintervention (2.17 ± 1.37), and follow-up (2.04 ± 1.22).
Figure 2.
Overall mean and maximum pain intensity (0–10 NRS). PRE: Preintervention. POST: Post-intervention. Using repeated measures ANOVA. **P < 0.001
With regards to the subjective assessment of the program by workers [Annexure 1], all of the approaches learned and applied during the program were considered to be useful, with the “ergonomics and education on healthy habits at the workstation” and “stretching exercises” obtaining the highest scores regarding usefulness (4.5/5), and being the most frequently applied in an autonomous manner during the follow-up period. Finally, workers gave scores over 4.5/5 for personal satisfaction and compliance with their expectations, expressing their desire to participate in future initiatives in this line.
Discussion
The proposed physical therapy program has reached a clinically relevant decrease of musculoskeletal pain intensity in office workers, even some of them displaying a complete pain relief. Our findings contribute to previous evidence highlighting the importance of the company physical therapist and the promotion of healthy activities carried out in the work facilities and taking place during the workday.[26]
Regarding the multimodal design of our intervention and its effectiveness, similar results to ours were obtained by a clinical trial conducted on office workers, where the combination of supervised ergonomic corrections and specific exercises succeeded to decrease pain intensity in the cervical, lower back and shoulder regions as compared to subjects receiving no type of action.[14] Furthermore, they also found that workers placed considerable importance on the follow-up of the postural hygiene and equipment use, revealing their personal commitment to this aspect of their own occupational health, which is in line with our findings obtained through the subjective assessment scale. Nevertheless, incorrect ergonomics is considered just one of the factors contributing to office workers' musculoskeletal pain.[12,27,28] Novoa Castro et al.[29] noted the importance of preventive exercises and stretching as essential elements to prevent and address work-related musculoskeletal disorders in office workers. At the same time, recent studies have extended the existing evidence with regard to the specific benefits of stretching,[30,31] while the systematic review and meta-analysis by Chen et al.[12] of interventions carried out in the workplace to improve cervical pain in office workers concluded that, although most of the actions were effective, strengthening exercises directed at the cervical area and shoulders were the most effective on pain relief. The occupational fitness part of our program included both muscle strengthening and stretching exercises, concluding effective results in the decrease of the overall musculoskeletal pain intensity and especially in the more affected areas. Besides, including pain education is essential to transform beliefs and behaviors regarding work-related musculoskeletal pain.[32,33,34] The recent research by Palsson et al.,[35] reviewing the effectiveness of educational programs to prevent and/or manage musculoskeletal pain in an occupational setting, concluded beneficial outcomes for these interventions. Other studies highlighted the need to prevent and manage all the important contributors; hence multimodal programs as the proposed in this pilot intervention are recommended, rather than different specific and isolated initiatives.[36,37]
Concerning our sample, despite the lack of official data about work-related musculoskeletal disorders in the target population, some epidemiological studies found rates of 30%–35% of Spanish office workers displaying cervical and low back pain, respectively.[5,38] Our findings overcome these results, with >60% of workers having presented musculoskeletal pain during the last year in the cited anatomical regions. On the other hand, the basal characteristics of our sample regarding physical activity were similar to those found in office workers from other universities.[39,40] Public health determines that office workers with sedentary and stressful labor activity are a population in which inactivity generates considerable risk, specifically regarding musculoskeletal disorders.[39,40,41,42] Therefore, it is suggested that companies invest in promoting health and wellbeing activities related to physical exercise, which workers can carry out during their workday.[13,43,44]
The qualitative study by Cooper and Barton,[40] using focus groups, allowed for the identification of the main barriers existing for the implementation of workplace programs, which was a lack of time for overloaded workers and a lack of corporate investment in health care. With this in mind, our program was designed to address work-related musculoskeletal pain as efficiently as possible, to ensure definitive learnings and early autonomy by the workers. These were achieved in a short intervention, thanks to our novel design presenting two main strengths. First, the program was focused on progressive learning, combining in-person guidance, audiovisual support, and individual supervision at the workplace. Second, a careful selection of therapeutic exercises and education was made to cover all the potential factors involved in musculoskeletal pain.
Assuming our study limitations, the lack of a control group and the small sample size do not allow us to generalize our findings. Secondarily, a psychological assessment would indicate profiles of workers who most significantly profited the intervention. Our study results, however, show that the proposed intervention extended their benefits in terms of pain relief and perception of usefulness and personal satisfaction to the majority of participants. Thus, the proposed intervention could be considered a feasible and cost-effective strategy to manage work-related musculoskeletal pain among the target population.
Conclusion
The results of this study support the foundations for the development of occupational physiotherapy programs in companies with office workers. Future research is warranted assessing the effectiveness of the piloted multimodal intervention in a randomized controlled trial, including a larger sample of computer workers and controlling for psychological individual and work features.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Leticia García-Gil, Ángel Vivancos-García, and Marta Hijazo-Alcaire for their collaboration from the Prevention Department of Mutua de Accidentes de Trabajo de Zaragoza and Universidad San Jorge.
Appendix
Annexure 1.
Program utility and worker satisfaction, ad-hoc questionnaire
| Questions about program | Subjective worker assessment (1- 5) (%) | Mean (SD) | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| With regards to the program in general | ||||||
| The overall program was appropriate | 0 | 0 | 0 | 42 | 54 | 4.57 (0.51) |
| The program content and structure were appropriate | 0 | 0 | 4 | 42 | 50 | 4.48 (0.59) |
| I feel that I will be able to apply the knowledge acquired in the future | 0 | 0 | 8 | 21 | 67 | 4.61 (0.65) |
| The professionalism of the physical therapist was appropriate | 0 | 0 | 0 | 17 | 79 | 4.83 (0.39) |
| The ability to communicate and transmit content was appropriate | 0 | 0 | 4 | 17 | 75 | 4.74 (0.54) |
| Program utility | ||||||
| With regards to the education received in the area of health | ||||||
| I have increased my knowledge in the area of health | 0 | 4 | 17 | 33 | 42 | 4.17 (0.89) |
| I believe that the following activities or tools may be useful for me in the future with regards to my health conditions and my workstation | ||||||
| Ergonomics and healthy habits at the workplace | 0 | 0 | 0 | 46 | 50 | 4.52 (0.51) |
| Exercises on body awareness, spine motor control and strengthening | 0 | 0 | 17 | 33 | 46 | 4.30 (0.76) |
| Stretching exercises | 0 | 0 | 4 | 38 | 54 | 4.52 (0.59) |
| Self-treatment with 3Tool | 8 | 17 | 17 | 38 | 17 | 3.39 (1.23) |
| With regards to the knowledge applied from the completion of the in-person program until the subsequent review in the workstation (follow-up) | ||||||
| I have carried out autonomously the following activities or guidelines during the follow-up period: | ||||||
| Ergonomics and healthy habits at the workplace | 4 | 8 | 8 | 17 | 58 | 4.22 (1.20) |
| Exercises on body awareness, spine motor control and strengthening | 25 | 13 | 21 | 17 | 21 | 2.96 (1.52) |
| Stretching exercises | 4 | 13 | 38 | 21 | 21 | 3.43 (1.12) |
| Self-treatment with 3-tool | 46 | 17 | 29 | 4 | 0 | 1.91 (0.99) |
| With regards to the assessment of your participation in the physiotherapy program | ||||||
| I have obtained personal satisfaction from participating in this program | 0 | 0 | 4 | 29 | 63 | 4.61 (0.58) |
| The program has complied with my expectations | 0 | 0 | 4 | 29 | 63 | 4.61 (0.58) |
| I would like to participate in this type of initiatives in the future | 0 | 0 | 0 | 21 | 75 | 4.78 (0.42) |
SD=Standard deviation. 1 = "completely disagree to 5 = “completely agree”
References
- 1.Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: Systematic review. Br J Sports Med. 2020;54:79–86. doi: 10.1136/bjsports-2018-099878. [DOI] [PubMed] [Google Scholar]
- 2.Aas RW, Tuntland H, Holte KA, Røe C, Lund T, Marklund S, et al. Workplace interventions for neck pain in workers. Cochrane Database Syst Rev. 2011;2011(4):CD008160. doi: 10.1002/14651858.CD008160.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoe VC, Urquhart DM, Kelsall HL, Zamri EN, Sim MR. Ergonomic interventions for preventing work-related musculoskeletal disorders of the upper limb and neck among office workers. Cochrane Database Syst Rev. 2018;10(10):CD008570. doi: 10.1002/14651858.CD008570.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vargas-Prada S, Serra C, Martínez JM, Ntani G, Delclos GL, Palmer KT, et al. Psychological and culturally-influenced risk factors for the incidence and persistence of low back pain and associated disability in Spanish workers: Findings from the CUPID study. Occup Environ Med. 2013;70:57–62. doi: 10.1136/oemed-2011-100637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campos-Fumero A, Delclos GL, Douphrate DI, Felknor SA, Vargas-Prada S, Serra C, et al. Low back pain among office workers in three Spanish-speaking countries: Findings from the CUPID study. Inj Prev. 2017;23:158–64. doi: 10.1136/injuryprev-2016-042091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spanish National Institute of Safety and Health at Work (INSHT). Ministry of Labour and Immigration of Spain. Evaluation and Prevention of Risks Related to the Use of Equipment with Display Screens. 2006. [Last accessed on 2020 Jul 22]. Available from: https://www.insst.es/documents/94886/509319/DTE_PVD-guiaTecnica.pdf/09375e8b-1de6-4793-9d07-c06f0dc16f1c .
- 7.Celik S, Celik K, Dirimese E, Taşdemir N, Arik T, Büyükkara İ. Determination of pain in musculoskeletal system reported by office workers and the pain risk factors. Int J Occup Med Environ Health. 2018;31:91–111. doi: 10.13075/ijomeh.1896.00901. [DOI] [PubMed] [Google Scholar]
- 8.Rodrigues MS, Leite RDV, Lelis CM, Chaves TC. Differences in ergonomic and workstation factors between computer office workers with and without reported musculoskeletal pain. Work. 2017;57:563–72. doi: 10.3233/WOR-172582. [DOI] [PubMed] [Google Scholar]
- 9.Hong S, Shin D. Relationship between pain intensity, disability, exercise time and computer usage time and depression in office workers with non-specific chronic low back pain. Med Hypotheses. 2020;137:109562. doi: 10.1016/j.mehy.2020.109562. [DOI] [PubMed] [Google Scholar]
- 10.Kim D. Effect of musculoskeletal pain of care workers on job satisfaction. J Phys Ther Sci. 2018;30:164–8. doi: 10.1589/jpts.30.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prall J, Ross M. The management of work-related musculoskeletal injuries in an occupational health setting: The role of the physical therapist. J Exerc Rehabil. 2019;15:193–9. doi: 10.12965/jer.1836636.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen X, Coombes BK, Sjøgaard G, Jun D, O'Leary S, Johnston V. Workplace-based interventions for neck pain in office workers: Systematic review and meta-analysis. Phys Ther. 2018;98:40–62. doi: 10.1093/ptj/pzx101. [DOI] [PubMed] [Google Scholar]
- 13.Moreira-Silva I, Santos R, Abreu S, Mota J. The effect of a physical activity program on decreasing physical disability indicated by musculoskeletal pain and related symptoms among workers: A pilot study. Int J Occup Saf Ergon. 2014;20:55–64. doi: 10.1080/10803548.2014.11077028. [DOI] [PubMed] [Google Scholar]
- 14.Shariat A, Cleland JA, Danaee M, Kargarfard M, Sangelaji B, Tamrin SB. Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: A randomized controlled trial. Braz J Phys Ther. 2018;22:144–53. doi: 10.1016/j.bjpt.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Besharati A, Daneshmandi H, Zareh K, Fakherpour A, Zoaktafi M. Work-related musculoskeletal problems and associated factors among office workers. Int J Occup Saf Ergon. 2020;26:632–8. doi: 10.1080/10803548.2018.1501238. [DOI] [PubMed] [Google Scholar]
- 16.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–58. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 17.Gómez-Rodríguez R, Díaz-Pulido B, Gutiérrez-Ortega C, Sánchez-Sánchez B, Torres-Lacomba M. Cultural adaptation and psychometric validation of the standardised nordic questionnaire spanish version in musicians. Int J Environ Res Public Health. 2020;17:653. doi: 10.3390/ijerph17020653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–7. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 19.Pugh JD, Gelder L, Williams AM, Twigg DE, Wilkinson AM, Blazevich AJ. Validity and reliability of an online extended version of the Nordic Musculoskeletal Questionnaire (NMQ-E2) to measure nurses' fitness. J Clin Nurs. 2015;24:3550–63. doi: 10.1111/jocn.12971. [DOI] [PubMed] [Google Scholar]
- 20.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short- Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S240–52. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 21.Martínez-González MA, López-Fontana C, Varo JJ, Sánchez-Villegas A, Martinez JA. Validation of the Spanish version of the physical activity questionnaire used in the Nurses' Health Study and the Health Professionals' Follow-up Study. Public Health Nutr. 2005;8:920–7. doi: 10.1079/phn2005745. [DOI] [PubMed] [Google Scholar]
- 22.Busner J, Targum SD. The clinical global impressions scale: Applying a research tool in clinical practice. Psychiatry (Edgmont) 2007;4:28–37. [PMC free article] [PubMed] [Google Scholar]
- 23.Mayoral del Moral O, Romay Barrero H. Conservative physical therapy in myofascial pain syndrome. Revista Iberoamericana de Fisioterapia y Kinesiologí. 2005;8:11–6. [Google Scholar]
- 24.Bernaards CM, Bosmans JE, Hildebrandt VH, van Tulder MW, Heymans MW. The cost-effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on recovery from neck and upper limb symptoms and pain reduction in computer workers. Occup Environ Med. 2011;68:265–72. doi: 10.1136/oem.2008.045450. [DOI] [PubMed] [Google Scholar]
- 25.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River New York: Prentice Hall Health; 2009. [Google Scholar]
- 26.Ahlstrom L, Hagberg M, Dellve L. Workplace rehabilitation and supportive conditions at work: A prospective study. J Occup Rehabil. 2013;23:248–60. doi: 10.1007/s10926-012-9391-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buckle PW, Devereux JJ. The nature of work-related neck and upper limb musculoskeletal disorders. Appl Ergon. 2002;33:207–17. doi: 10.1016/s0003-6870(02)00014-5. [DOI] [PubMed] [Google Scholar]
- 28.Piñeda A. Ergonomic screens handle for visualization data in office work. J Technol. 2014;13:7–18. [Google Scholar]
- 29.Novoa Castro B, Pérez Fernández MR, Torrecilla Serrano F, Novoa Castro R. Physiotherapist of company, a challenge for the physiotherapy in Spain. Fisioterapia. 2017;29:26–35. [Google Scholar]
- 30.Marangoni AH. Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcomes. Work. 2010;36:27–37. doi: 10.3233/WOR-2010-1004. [DOI] [PubMed] [Google Scholar]
- 31.van den Heuvel SG, de Looze MP, Hildebrandt VH, Thé KH. Effects of software programs stimulating regular breaks and exercises on work-related neck and upper-limb disorders. Scand J Work Environ Health. 2003;29:106–16. doi: 10.5271/sjweh.712. [DOI] [PubMed] [Google Scholar]
- 32.Ree E, Lie SA, Eriksen HR, Malterud K, Indahl A, Samdal O, et al. Reduction in sick leave by a workplace educational low back pain intervention: A cluster randomized controlled trial. Scand J Public Health. 2016;44:571–9. doi: 10.1177/1403494816653854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tang SK, Tse MM, Leung SF, Fotis T. Acute and chronic musculoskeletal pain situations among the working population and their pain education needs: An exploratory study. Fam Pract. 2020:1–8. doi: 10.1093/fampra/cmaa013. [DOI] [PubMed] [Google Scholar]
- 34.Tegner H, Frederiksen P, Esbensen BA, Juhl C. Neurophysiological pain education for patients with chronic low back pain: A systematic review and meta-analysis. Clin J Pain. 2018;34:778–86. doi: 10.1097/AJP.0000000000000594. [DOI] [PubMed] [Google Scholar]
- 35.Palsson TS, Boudreau S, Høgh M, Herrero P, Bellosta-Lopez P, Domenech-Garcia V, et al. Education as a strategy for managing occupational-related musculoskeletal pain: A scoping review. BMJ Open. 2020;10:e032668. doi: 10.1136/bmjopen-2019-032668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract. 2016;32:332–55. doi: 10.1080/09593985.2016.1194646. [DOI] [PubMed] [Google Scholar]
- 37.Malfliet A, Kregel J, Meeus M, Roussel N, Danneels L, Cagnie B, et al. Blended-learning pain neuroscience education for people with chronic spinal pain: Randomized controlled multicenter trial. Phys Ther. 2018;98:357–68. doi: 10.1093/ptj/pzx092. [DOI] [PubMed] [Google Scholar]
- 38.Campos-Fumero A, Delclos GL, Douphrate DI, Felknor SA, Vargas-Prada S, Serra C, et al. Upper extremity musculoskeletal pain among office workers in three Spanish-speaking countries: Findings from the CUPID study. Occup Environ Med. 2016;73:394–400. doi: 10.1136/oemed-2015-103327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arslan SS, Alemdaroğlu İ, Karaduman AA, Yilmaz ÖT. The effects of physical activity on sleep quality, job satisfaction, and quality of life in office workers. Work. 2019;63:3–7. doi: 10.3233/WOR-192902. [DOI] [PubMed] [Google Scholar]
- 40.Cooper K, Barton GC. An exploration of physical activity and wellbeing in university employees. Perspect Public Health. 2016;136:152–60. doi: 10.1177/1757913915593103. [DOI] [PubMed] [Google Scholar]
- 41.López Bueno R, Casajús Mallén JA, Garatachea Vallejo N. Physical activity as a tool to reduce disease-related work absenteeism in sedentary employees: A systematic review. Rev Esp Salud Publica. 2018;92:e201810071. [PMC free article] [PubMed] [Google Scholar]
- 42.Escalante Y. Physical activity, exercise and fitness in the field of public health. Rev Esp Salud Publica. 2011;85:325–8. doi: 10.1590/S1135-57272011000400001. [DOI] [PubMed] [Google Scholar]
- 43.Gram B, Holtermann A, Bültmann U, Sjøgaard G, Søgaard K. Does an exercise intervention improving aerobic capacity among construction workers also improve musculoskeletal pain, work ability, productivity, perceived physical exertion, and sick leave.: A randomized controlled trial? J Occup Environ Med. 2012;54:1520–6. doi: 10.1097/JOM.0b013e318266484a. [DOI] [PubMed] [Google Scholar]
- 44.Pérez ML, Yélamos F, Rodríguez MA. Intervention through a physical exercise program at the company. Medicina y Seguridad del Trabajo. 2015;61:240. [Google Scholar]