Abstract
Patient: Female, 47-year-old
Final Diagnosis: Adenocarcinoma of the ovary
Symptoms: Pain
Medication: —
Clinical Procedure: Completely laparoscopic staging of ovarian cancer • laparoscopic morcellation of ovarian tumor
Specialty: Obstetrics and Gynecology
Objective:
Rare co-existance of disease or pathology
Background:
Advances in minimally invasive surgery are essential for the improvement of patient care, overall health care efficiency, and total cost reductions. Morcellation, the technique used in the present case, is often used to aid minimally invasive laparoscopic procedures, whereby larger tissue specimens are broken down and divided to be removed via smaller incisions. Morcellation has become controversial in the medical community owing to the risk of the procedure spreading an occult malignancy.
Case Report:
A 47-year-old woman with obesity presented with right-sided pelvic pain and suspicion of ovarian torsion. The patient experienced severe acute pain and was taken to the operating room for laparoscopy to remove the left-sided adnexal mass seen on imaging. During surgery, there was no evidence of torsion, and the mass was perfused. During removal of the entire tumor, blunt instruments were utilized for in-bag manual morcellation to avoid spillage of the contents of the bag, which were then sent for frozen section analysis, and a diagnosis of adenocarcinoma of the ovary was made. Once the tumor was removed, a board-certified gynecologic oncologist was consulted to assist with the remainder of the procedure. Following this, the ovarian cancer staging procedure was able to be completed laparoscopically.
Conclusions:
This technique of in-bag manual morcellation using blunt instruments allows laparoscopic procedures to be performed on large tissue specimens with potential malignancies without spreading cancerous tissue, overcoming the associated risks of dissemination of malignancy. This technique is therefore more beneficial to patients.
Keywords: Gynecologic Surgical Procedures; Laparoscopy; Ovarian Neoplasms; Surgical Procedures, Minimally Invasive
Background
Medical advancements in minimally invasive surgery, through the use of laparoscopic and robotic procedures, provide patients with an alternative to laparotomy that is often considered preferable owing to the added benefits to patients, including better cosmetic results, reduced risk of infection, reduced pain, faster recovery, and an overall improvement in quality, efficiency, and cost-effectiveness in patient care [1]. However, the removal of large tissue specimens that exceed the size of laparoscopic openings remains challenging. For this to be accomplished, removal of the intact mass is unlikely. Morcellation techniques have often been used to address this challenge but they carry an increased risk of intraperitoneal spillage. Care must be taken to avoid any dissemination, which, in cases of malignancy, can result in seeding of potentially malignant cells [2,3] and, in benign cases, can result in peritonitis [4] or similar adverse outcomes [5,6].
Morcellation is a technique utilized in minimally invasive procedures, in which tissue specimens are broken up into smaller pieces using electromechanical power or hand mechanical power so that the specimen can be removed via an incision that is smaller than the original specimen size. Although this can address the problem of removing large specimens, there is some controversy with this technique, specifically in performing power morcellation during laparoscopic surgery, because of the potential to spread cancerous tissue within the abdominal and pelvic area in patients with unsuspected malignancy [7,8]. Concern for disseminated malignant cells became especially apparent after a patient with presumed leiomyoma was found to have leiomyosarcoma that had disseminated throughout the abdomen due to the use of a power morcellator [8,9]. This prompted the United States Food and Drug Administration (FDA) to address these concerns through the release of a warning communication in 2014 containing new guidelines and contraindications for morcellation procedures, which has discouraged power morcellation in minimally invasive gynecological surgery [9]. In a study done on the impact of the 2014 FDA warning, it was found that power morcellation rates did decrease, most often in response to hospital mandates, and rates of laparotomy were increased, in spite of the clear benefits of minimally invasive surgery routes. Many of those surveyed in the study did not believe that the FDA warning resulted in improved patient outcomes [10].
Contrary to the FDA warning on power morcellation, studies have presented contained power morcellation systems [6,11] and contained manual morcellation techniques [8] as feasible procedures that could safely and effectively remove large specimens; both techniques allow for the preservation of the benefits minimally invasive surgery provides. In this case report, we present a surgical technique that was used to remove a 17-cm ovarian adenocarcinoma using a completely contained, in-bag manual morcellation. This was followed by laparoscopic completion of the staging procedure, which ultimately avoided the need for an open procedure. A previous version of this case was presented orally at the International Conference on Gynecology & Obstetrics, in Barcelona, Spain on October 3, 2017 [12].
Case Report
The patient was a 47-year-old woman who was nulligravid, had morbid obesity, and had a history of a 6-cm left-sided adnexal cystic mass, which was being followed with observation for over 2 years. In that time, there had been no significant changes in the size or character of the mass. The patient’s CA-125 levels were also tracked, and had remained within the normal reference range for a premenopausal woman.
Following vigorous exercise, the patient had an acute episode of pain in the lower pelvic region and called an ambulance upon onset of this pain. Once the ambulance arrived, the pain had largely resolved, and she declined further care at that time. Shortly thereafter, she presented in the emergency department complaining of severe lower abdominal and pelvic pain. A transvaginal ultrasound (Figure 1) and computed tomography scan (Figure 2) were ordered. The imaging results revealed a large complex adnexal mass on her left side. Pertinent laboratory results revealed a white blood cell count of 9.3×10e3/uL, hemoglobin level of 4.2 g/dL, hematocrit level of 41.2%, and platelet count of 260×10e3/uL. Follicle stimulating hormone and CA-125 levels remained pending at the time. Despite Doppler studies showing perfusion in the ovarian mass, the sudden increase in the intensity of the patient’s pain led to the presumed diagnosis of partial or intermittent ovarian torsion as the primary differential diagnosis. When considering the possibility of malignancy, it was reassuring that the left-sided mass had been followed and seen as stable, with a CA-125 level found to be within the normal reference range in the patient’s recent medical history, although malignancy could not be entirely ruled out of the differential diagnosis.
Figure 1.

Transvaginal ultrasound was subsequently performed to evaluate the mass. A left adnexal mass, measuring 14.0×13.4×16.7 cm, with thick, nodular septations was visualized.
Figure 2.
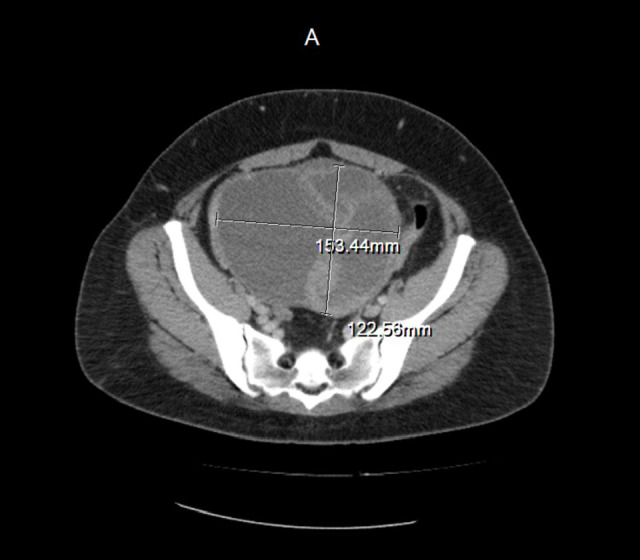
Computed tomography (scan, transverse plane). A centrally located mass measuring 15.3×12.3×16.7 cm with thick, irregular septations was visualized.
We determined that the patient needed urgent surgical intervention for a possible diagnosis of ovarian torsion. The procedure was begun by installing a Valtchev manipulator in the cervix to manipulate the uterus during the procedure. This device was inserted using a speculum. A small incision was made at the bottom of the umbilicus to gain access to the abdominal cavity, and a Veress needle was placed in the abdominal cavity. Following this, a saline needle “drop test”, “withdrawal test”, and “injection test” were then employed to ensure appropriate needle positioning. All of these tests showed the tip of the needle to be in the appropriate position in the abdominal cavity. The abdomen was then insufflated to 15 mmHg of pressure, and an 11-mm bladeless laparoscopic trocar was placed into the abdominal cavity through the same umbilical incision. Following this, 2 more laparoscopic trocar ports were placed, with the first placed midline and approximately 3 cm above the pubis symphysis and the second placed approximately 8 cm laterally to the right of that position. The abdominal cavity was then washed, and the washing fluid specimens were sent to the pathology department for analysis.
Findings within the abdomen were within normal limits, with the exception of the left ovary which showed no sign of torsion but was entirely replaced by a large 17-cm, smooth-surfaced white mass. The right fallopian tube was divided from its origin at the uterus using a LigaSure bipolar coagulation device, and the dissection followed down the outer edge of the fallopian tube, traversing the infundibulopelvic ligament to detach the left ovary. Using the umbilical port, a 15-mm Endocatch bag (Figure 3) was inserted into the abdominal cavity to scoop the detached mass with the aid of wavy graspers, without rupturing the mass. The mouth of the Endocatch bag was exteriorized prior to any rupture of the mass, thus minimizing the possibility of spillage of any cellular content of the mass in the abdominal cavity. Once the mouth of the bag was exteriorized, the mass was manually morcellated extensively, as it was removed through the 15-mm umbilical port (Figure 4). The mass was sent to the pathology department for frozen section analysis, and a diagnosis of adenocarcinoma of the ovary was made.
Figure 3.
An Endocatch bag was placed through a 15-mm trocar. The Endocatch bag is 23 cm in depth and used to maximize the potential of laparoscopic procedures by allowing for the safe and efficient removal of large masses.
Figure 4.

A balloon measuring approximately 17 cm in diameter was used to demonstrate our in-bag morcellation technique. Exteriorization of the bag opening was crucial to minimize the risk of mass rupture intra-abdominally.
Upon the finding of malignancy, a gynecological oncologist was consulted to assist with the remainder of the procedure, including ovarian cancer staging. All of these procedures were completed laparoscopically. The staging procedure included laparoscopic hysterectomy, biopsy of the bilateral pelvic and periaortic lymph nodes, complete omentectomy, and unilateral left salpingo-oophorectomy. Ultimately, the pelvic and paraaortic lymph nodes were negative for malignancy, and the final pathology report showed a FIGO stage I adenocarcinoma of the ovary. The cytology results showed the abdominal washing fluid was free of malignant cells. Outpatient observation was recommended, without chemotherapy. At the 21-month follow-up visit with the patient, there was no evidence of recurrence of the malignancy and no complications were reported.
Discussion
In the present case, the surgeons proceeded with the minimally invasive technique to remove the mass, with the assumption that the mass was most likely benign. Evidence for this included the patient’s negative CA-125 levels, the long period that the mass had been followed without an observed metastasis, and the large size of the mass. The patient’s severe pain warranted emergency surgical intervention, and although acute ovarian torsion was not seen during surgery, it cannot be known whether intermittent ovarian torsion was a cause of the patient’s pain. Although preoperative ultrasound studies were negative for torsion, in retrospect it must be considered that partial or intermittent ovarian torsion could have played a role in masking Doppler flow within the mass, which may have been increased in the presence of a malignancy. It is possible that the increased flow that would be expected in a malignant tumor may have been hidden because of possible torsion.
Although the FDA safety warning statements on morcellation have significantly decreased the application of minimally invasive surgery in the gynecological setting, there are still significant advantages of minimally invasive surgery over laparotomy to consider, including better surgical outcomes, shorter patient recovery time, and overall improvement of quality of life for patients who undergo such procedures [1,7]. Owing to the obvious benefits of minimally invasive surgery, it is imperative to continue to improve and overcome existing challenges that arise with minimally invasive techniques so that more patients can benefit from such procedures.
The contained morcellation technique, described in the present case, efficiently and effectively minimized the risks of dissemination, which are associated with power morcellation, by using gentle techniques to move the specimen to the retrieval bag and then exteriorizing the mouth of the bag prior to morcellation. This effectively created a closed system where there was no communication between the tissue and the abdominal cavity. At this point, manual morcellation was performed to remove all of the tissue through the small laparoscopic incision. The use of blunt instruments such as ring forceps decreased the chance of rupturing the containment bag and spilling the contents. Following removal of the ovarian tumor and confirmation of its malignancy, the ovarian cancer staging procedure, as documented by many other authors, was completed laparoscopically. Such an outcome in a procedure can make a large impact on potential treatment options for patients who are known to have cancer, as well as gynecological patients. Successful minimally invasive surgery techniques, which allow for reduction in recovery time and improved quality of life, can allow patients to go forward with the next steps in treatment, such as chemotherapy or radiation. These adjuvant therapies can, in theory, be started much sooner than in those patients who undergo open procedures.
Several contained morcellation techniques that support the method used in the present case have been proposed as feasible methods to address cell dissemination risks in laparoscopic large specimen removal [7,11,13–17]. Our method showed an additional advancement in gynecological minimally invasive surgery, namely the successful staging of a large ovarian malignancy. Although previous research on gynecological contained morcellation has focused on myomectomy or hysterectomy, in each study, the contained morcellation technique was found to be reliable, safe, and preferable to conventional laparotomy and laparoscopy techniques used in large mass removal because of the superior surgical outcomes obtained [13–17]. Even so, patients must be informed of the risk of potential unknown malignancies, and the possible impact and prognosis of those potential malignancies must be weighed against the substantial gains of minimally invasive surgery procedures prior to using morcellation techniques. Use of contained morcellation has also been described in surgical cases of splenomegaly and nephrectomy [18,19]. Further evaluation and comparison of using this technique for other large specimens of varied tissue types could be useful outside of the gynecological field.
The successful use of this contained manual morcellation method has the potential to promote further discussion on the return to more widespread use of minimally invasive surgery for gynecological cases involving large masses, even for those with potential malignancy. Further studies on contained morcellation would aid in a wider acceptance of the method, potentially leading to an increase in laparoscopic candidates and, ultimately, better outcomes for patients. To validate this contained morcellation technique, future studies with larger patient cohorts are needed and should focus on evaluating the safety and efficacy of this method in preventing dissemination of malignant cells and its accuracy in the staging of ovarian cancers. Additionally, further analyses of containment bag types, with regard to size, integrity, and leakage potential, would help avoid potential limitations of very large masses and further reduce the risk of microscopic leakage that may not be objectively seen.
Conclusions
The controversy surrounding power morcellation has resulted in a decrease in minimally invasive gynecologic procedures, despite increased benefits to the patient with the use of a proper technique. This method of contained, in-bag manual morcellation with the aid of forceps and other blunt instruments addresses this controversy by circumventing the risks commonly associated with morcellation. The use of a containment system with morcellation enables the laparoscopic removal and staging of large ovarian malignancies without the dissemination of cancerous tissue or the use of unnecessarily large incisions. The success of the present case marks a pivotal point in the progression of minimally invasive surgery, and we are hopeful that our contained morcellation technique will become better established in the setting of more invasive open techniques and more dangerous uncontained morcellation techniques. While this report is only of a single case, and future studies are needed, we are hopeful that the method presented here encourages the increased use of beneficial minimally invasive treatment methods for gynecological treatments as a whole.
Acknowledgments
The Marchand Institute for Minimally Invasive Surgery would like to acknowledge the efforts of all of the students, researchers, residents, and fellows at the institute who put their time and effort into these projects without compensation, only for the betterment of medicine. We firmly assure them that the future of medicine belongs to them.
Footnotes
Conflict of Interest
None.
References:
- 1.Goh SM, Yam J, Loh SF, et al. Minimal access approach to the management of large ovarian cysts. Surg Endosc. 2007;21(1):80–83. doi: 10.1007/s00464-005-0596-5. [DOI] [PubMed] [Google Scholar]
- 2.Park JY, Park SK, Kim DY, et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecol Oncol. 2011;122(2):255–59. doi: 10.1016/j.ygyno.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Tchartchian G, Bojahr B, Becker S, et al. Occult malignancy rate of 1498 hysterectomies or myomectomies with morcellation: A retrospective single-arm study. J Obstet Gynaecol India. 2019;69(Suppl.2):188–93. doi: 10.1007/s13224-018-1190-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kondo W, Bourdel N, Cotte B, et al. Does prevention of intraperitoneal spill-age when removing a dermoid cyst prevent granulomatous peritonitis? BJOG. 2010;117:1027–30. doi: 10.1111/j.1471-0528.2010.02580.x. [DOI] [PubMed] [Google Scholar]
- 5.Leren V, Langebrekke A, Qvigstad E. Parasitic leiomyomas after laparoscopic surgery with morcellation. Acta Obstet Gynecol Scand. 2012;91(10):1233–36. doi: 10.1111/j.1600-0412.2012.01453.x. [DOI] [PubMed] [Google Scholar]
- 6.Devassy R, Cezar C, Krentel H, et al. Feasibility of myomatous tissue extraction in laparoscopic surgery by contained in-bag morcellation: A retrospective single arm study. Int J Surg. 2019;62:22–27. doi: 10.1016/j.ijsu.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 7.Venturella R, Rocca ML, Lico D, et al. In-bag manual versus uncontained power morcellation for laparoscopic myomectomy: Randomized controlled trial. Fertil Steril. 2016;105(5):1369–76. doi: 10.1016/j.fertnstert.2015.12.133. [DOI] [PubMed] [Google Scholar]
- 8.Dotson S, Landa A, Ehrisman J, et al. Safety and feasibility of contained uterine morcellation in women undergoing laparoscopic hysterectomy. Gynecol Oncol Res Pract. 2018;5:8. doi: 10.1186/s40661-018-0065-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Food and Drug Administration Laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. 2014. [cited 2020 Nov 18]. http://wayback.archive-it.org/7993/20170722215731/, https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm393576.htm.
- 10.Lum DA, Sokol ER, Berek JS, et al. Impact of the 2014 Food and Drug Administration warnings against power morcellation. J Minim Invasive Gynecol. 2016;23(4):548–56. doi: 10.1016/j.jmig.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 11.Cohen SL, Einarsson JI, Wang KC, et al. Contained power morcellation within an insufflated isolation bag. Obstet Gynecol. 2014;124(3):491–97. doi: 10.1097/AOG.0000000000000421. [DOI] [PubMed] [Google Scholar]
- 12.Marchand GJ, Pile R. Successful complete laparoscopic staging of ovarian cancer in a patient with a 17cm malignant ovarian tumor. Presented at the 4th International Conference on Gynecology & Obstetrics; 2017 Oct 3; Barcelona, Spain. [Google Scholar]
- 13.Hong MK, Wei YC, Chu TY, et al. Safety and efficacy of contained manual morcellation during laparoscopic or robotic gynecological surgery. Int J Gynaecol Obstet. 2020;148(2):168–73. doi: 10.1002/ijgo.13062. [DOI] [PubMed] [Google Scholar]
- 14.Steller C, Cholkeri-Singh A, Sasaki K, et al. Power morcellation using a contained bag system. JSLS. 2017;21(1):e2016.00095. doi: 10.4293/JSLS.2016.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Demir RH, Marchand GJ. Effect of improved vaginal manipulator on laparoscopic sacrocolpopexy. J Minim Invasive Gynecol. 2012;19(6):S77. [Google Scholar]
- 16.Yang J, Song YJ, Na YJ, et al. Two-port myomectomy using bag-contained manual morcellation: A comparison with three-port myomectomy using power morcellation. Taiwan J Obstet Gynecol. 2019;58(3):423–27. doi: 10.1016/j.tjog.2019.01.029. [DOI] [PubMed] [Google Scholar]
- 17.Chang Y, Kay N, Huang MR, et al. laparoendoscopic single-site supracervical hysterectomy with manual morcellation: a retrospective study. J Minim Invasive Gynecol. 2018;25(6):1094–100. doi: 10.1016/j.jmig.2018.02.017. [DOI] [PubMed] [Google Scholar]
- 18.Greene AK, Hodin RA. Laparoscopic splenectomy for massive splenomegaly using a Lahey bag. Am J Surg. 2001;181(6):543–46. doi: 10.1016/s0002-9610(01)00632-8. [DOI] [PubMed] [Google Scholar]
- 19.Wu SD, Lesani OA, Zhao LC, et al. A multi-institutional study on the safety and efficacy of specimen morcellation after laparoscopic radical nephrectomy for clinical stage T1 or T2 renal cell carcinoma. J Endourol. 2009;23(9):1513–18. doi: 10.1089/end.2009.0387. [DOI] [PubMed] [Google Scholar]



