Abstract
Aims
There is compelling evidence for gradient effects of household income on school readiness. Potential mechanisms are described, yet the growth curve trajectory of maternal mental health in a child's early life has not been thoroughly investigated. We aimed to examine the relationships between household incomes, maternal mental health trajectories from antenatal to the postnatal period, and school readiness.
Methods
Prospective data from 505 mother–child dyads in a birth cohort in Singapore were used, including household income, repeated measures of maternal mental health from pregnancy to 2-years postpartum, and a range of child behavioural, socio-emotional and cognitive outcomes from 2 to 6 years of age. Antenatal mental health and its trajectory were tested as mediators in the latent growth curve models.
Results
Household income was a robust predictor of antenatal maternal mental health and all child outcomes. Between children from the bottom and top household income quartiles, four dimensions of school readiness skills differed by a range of 0.52 (95% Cl: 0.23, 0.67) to 1.21 s.d. (95% CI: 1.02, 1.40). Thirty-eight percent of pregnant mothers in this cohort were found to have perinatal depressive and anxiety symptoms in the subclinical and clinical ranges. Poorer school readiness skills were found in children of these mothers when compared to those of mothers with little or no symptoms. After adjustment of unmeasured confounding on the indirect effect, antenatal maternal mental health provided a robust mediating path between household income and multiple school readiness outcomes (χ2 126.05, df 63, p < 0.001; RMSEA = 0.031, CFI = 0.980, SRMR = 0.034).
Conclusions
Pregnant mothers with mental health symptoms, particularly those from economically-challenged households, are potential targets for intervention to level the playing field of their children.
Key words: Household income, maternal mental health, perinatal mood, school readiness
Background
Socioeconomic status (SES) has profound effects on the capacity and achievement of children, including cognitive, social–emotional and brain development (Hackman et al., 2010; Shonkoff et al., 2012; Piccolo et al., 2016; Sheridan and McLaughlin, 2016). SES-related contextual factors are also salient risks for suboptimal maternal mood (Petterson and Albers, 2001; Kiernan and Huerta, 2008; Allen et al., 2014). While prior studies have largely focused on demonstrating the negative sequelae of low SES, recent studies use a life course approach to study the familial transmission of disadvantage and to describe potential explanatory pathways (Cents et al., 2013; Pearson et al., 2013).
Maternal mental health has been proposed as a candidate pathway contributing to SES disparity in multiple child developmental outcomes, yet studies confirming this hypothesis are lacking. There is, however, plentiful and compelling evidence for the association between maternal mental health and developmental competencies of the offspring (Cents et al., 2013; Pearson et al., 2013; O'Donnell and Meaney, 2017; Meaney, 2018). Recently, our own group and others have shown that the experience of maternal depression and anxiety not only ‘gets under the skin’ of children, but that discernible differences are already evident in the brains of newborn infants after antenatal exposure as a foetus (Qiu et al., 2013; Noble et al., 2015; Rifkin-Graboi et al., 2015; Lebel et al., 2016; Shen et al., 2016; Wen et al., 2017).
During pregnancy, 10–15% of women report depression and anxiety symptoms above clinical cut-offs, while up to 30% have high, but often subclinical, levels of symptoms (Meaney, 2018). Perinatal mental health studies often focus on women meeting criteria for a clinical disorder, which may miss the latter group of women. Mothers with high symptom counts, although not at clinical levels, transmit increased risks related to psychological outcomes to the next generation when compared to mothers without symptoms (Weinberg et al., 2001; Tietz et al., 2014; Meaney, 2018). Consequently, studying depressive and anxiety symptoms instead of clinical diagnoses enables the understanding of whether child outcomes vary based on different degrees of maternal symptoms.
During the perinatal period, depressive and anxiety symptoms covary and are hard to isolate independently (Lancaster et al., 2010; Verreault et al., 2014). For example, depressive symptoms at the second trimester are correlates of high anxiety levels at the third trimester, which in turn predict depressive symptoms in the postnatal period (Skouteris et al., 2009). As perinatal maternal symptoms vary in timing, severity and duration, it is best studied using trajectories across time (Dennis et al., 2017). Prior studies generally examine either antenatal or postnatal period while controlling for the other, which do not fully capture the dynamic processes across time points (Goodman and Tully, 2009; Pearson et al., 2013). Hence, this present study incorporates maternal depressive and anxiety symptom trajectories from the antenatal to postnatal period to represent a whole experience for the child using latent growth curve models (LGCMs).
As school readiness constitutes a critical skill set for shaping children's long-term life successes and health, our group seeks to understand whether maternal mental health trajectory forms an underlying pathway explaining why children are differentially affected by poverty. School readiness is a multifaceted concept that encompasses skill sets needed for preparation into school and wider ecological systems (High, 2008; Moreno, 2013; Scharf, 2016). By this definition, school readiness skills stretch beyond general knowledge and pre-academic skills, such as literacy and early mathematics, and include additional dimensions (e.g. behavioural and socio-emotional, cognitive and executive functions) (Welsh et al., 2010; Blair and Raver, 2015; Perry et al., 2018). Four dimensions of school readiness skills are the outcomes in this study and are captured from 2 to 6 years of age.
Mediators of the income-school readiness gap, especially measurable and modifiable ones, are potential leverage points that may inform interventions. In this study, we targeted perinatal maternal mental health as a promising mediator based on our group's neuroimaging and neurophysiological findings (Qiu et al., 2013; Rifkin-Graboi et al., 2015; Wen et al., 2017). We hypothesised that antenatal maternal mental health and its trajectory from pregnancy to 2-years postpartum, both attenuated the effects of household income on child school readiness.
Methods
Participants
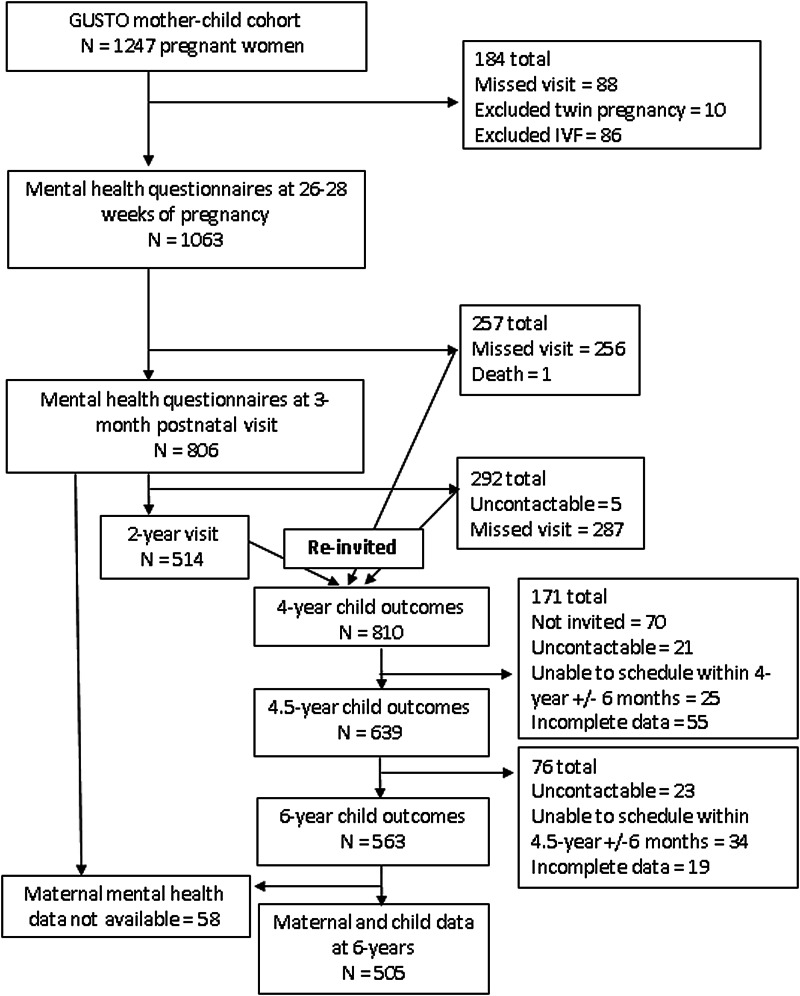
Data were obtained from the Growing Up in Singapore towards Healthy Outcomes (GUSTO) longitudinal birth cohort study (Soh et al., 2014). The cohort consisted of 1247 mother–child dyads who were representative of the multi-ethnic population in Singapore. Pregnant women were recruited in their first trimester in 2009 to 2010 from two public hospitals in Singapore. Women with preterm infants (<37 weeks' gestation), twin pregnancy or conception via in vitro fertilisation techniques were excluded from this study. Participants were followed through and beyond delivery and their children were seen for neurocognitive testing regularly either in participants' home or at our neurodevelopmental research centre (Fig. 1). At 4 years of age, we re-invited families who missed a prior postnatal visit to keep their enrolment active. As our cohort consisted of many study domains, at 4.5 years, we prioritised our invitation to families who had attended the most postnatal visits between 6-months and 4-years to match our laboratory capacity, reduce the time burden, and allow for the most complete set of data for analysis. Not all our instruments produced age-equivalent scores; therefore, participants who could not be scheduled within 6 months of the designated visit time were not included in the analyses.
Fig. 1.
Study flow diagram.
Exposures
Household income
Household income obtained during pregnancy was in four groups (<S$2000, $2000–4000, $4000–6000 and >$6000/month; S$1 = US$0.73 = £0.57). There is currently no official poverty line or income-to-needs index in Singapore. However, an absolute household monthly income of ~S$2000 is often used to represent those who satisfy the household income criterion for a governmental financial subsidy (Donaldson et al., 2013). Hence, based on the context of this birth cohort, the decision was made to use an income cut-off <S$2000 v. ⩾$2000 per month in inferential statistics to allow for real-world relevance.
Maternal mood
The following two measures were administered between 26 and 28 weeks of pregnancy and also at 3- and 24-months postpartum. Edinburgh Postnatal Depression Scale (EPDS). The EPDS is a widely-used questionnaire that assesses the presence and severity of depressive symptoms (Cox et al., 1987). Initially, it was developed for postnatal depression and was subsequently validated for depression during pregnancy (Murray and Cox, 1990). Although the cut-off of ‘above 12’ (i.e. 13 or more) is used to screen for clinical depression in a general population, the cut-off during pregnancy is ‘above 14’ (i.e. 15 or more) (Matthey et al., 2006). It is important to note that this tool also elicits anxiety symptoms (e.g. I have been anxious or worried for no good reason, I have felt scared or panicky). State-Trait Anxiety Inventory (STAI). The STAI is a well-validated measure of state and trait anxiety used in perinatal studies to assess maternal mood (Spielberger, 2010). We used state anxiety to represent temporal mood fluctuations during pregnancy. As STAI does not have an established cut-off for subclinical symptoms, we first determined the extent, in standard deviations, to which the EPDS subclinical cut-off range (EPDS 9–14) was above the cohort mean for depressive symptoms, then we applied the same calculations to determine a cut-off range for anxiety symptoms.
Four dimensions of school readiness
The following seven assessments measured different dimensions of school readiness, namely behavioural and socio-emotional, pre-academic, fluid reasoning and working memory, a component of executive functions. These were the same assessments that were validated against the cohort's school-age data (unpublished) and were previously used by other longitudinal cohorts as a school readiness panel (O'Donnell et al., 2014). As English is the medium used in education in Singapore, tools administered to children were in English. Child Behaviour Checklist, Preschool (CBCL) at age 2. The CBCL is a validated questionnaire for behavioural and socio-emotional problems in children ages 1.5–5, is widely used in mental health services, and validated in Singapore (Achenbach and Rescorla, 2000; Woo et al., 2007). We used the internalising and externalising raw scores, as recommended by the Achenbach manual, to capture two spectrums of behavioural difficulties (Achenbach and Rescorla, 2000). Lollipop Test. The Lollipop is a measure of general knowledge and comprises four subtests: colours and shapes, numbers, letters and spatial recognition (Chew, 1981). The Lollipop has been demonstrated to have good reliability and predicts performance in fourth grade (Chew, 1981). Number Knowledge Test (NKT). The NKT consists of questions testing numerical concepts and counting skills of the child. The NKT has good validity and is representative of numeracy in kindergarten (Griffin, 2002). Peabody Picture Vocabulary Test, 4th Edition (PPVT-IV). The PPVT-IV is a reliable instrument measuring receptive vocabulary in individuals from ages 2.5 to 90, with reliability and validity coefficients above 0.90 (Naglieri and Pfeiffer, 1983). Comprehensive Test of Phonological Processing (CTOPP). The CTOPP is a measure of phonological processing abilities, which are crucial for reading and achievement, and has internal and test-retest reliability coefficients above 0.80 (Wagner et al., 2013). Kaufman Brief Intelligence Test, Second Edition (KBIT-2) at age 4.5. The non-verbal score of the KBIT-2 is a measure of fluid reasoning (i.e. problem-solving and identifying patterns) for individuals ages 4–90 and has a correlation coefficient of 0.88 (95% CI: 0.74–0.95) with the matrix reasoning score of the Wechsler Intelligence Scale for Children, Fourth Edition (Kaufman and Kaufman, 2004). Cambridge Neuropsychological Test Automated Battery (CANTAB) Spatial Working Memory (SWM) at age 6. The CANTAB is a well-validated, computerised battery that covers a range of executive function tasks (Luciana and Nelson, 2002). The SWM in the CANTAB tests children's ability to retain spatial information mentally. We used the number of total errors (i.e. the sum of between and within errors) from the 4, 6 and 8 box SWM tasks as the outcome (Fried et al., 2015).
Statistical analysis
To compare characteristics of children from various household income groups, we conducted a one-way analysis of variance (ANOVA) with 3000-iteration bootstrapping and Chi-square for the trend test with an odds ratio on the interval and categorical variables, respectively. We then determined the school readiness gap between children from the bottom and the top household income groups using mean differences in standard deviations (Z-scores). We also utilised one-way ANOVA and post-hoc Tukey to compare the child outcomes between groups of mothers with (1) clinical levels, (2) high, but subclinical levels and (3) little or no antenatal depressive or anxiety disturbances. Descriptive analyses were completed using IBM SPSS version 22.0 (Armonk, NY: IBM Corp).
Since both questionnaires (i.e. STAI and EPDS) collectively measured different facets of mental health and at the same time contained overlapping items, we first tested whether depressive and anxiety symptoms, as manifest variables, were representative of one or two mental health constructs (see online Supplementary text). Similar to an exploratory bi-factor analysis completed by our group previously, depressive symptoms (loadings 0.84–0.93) and anxiety symptoms (0.80–0.87) both contributed comparably to one general mental health construct (see online Supplementary Fig. S1) (Phua et al., 2017). Hence, we created a single mental health trajectory using latent constructs at three time points: antenatal mental health (26–28 weeks' gestation), Time 1 (postnatal 3 months) and Time 2 (postnatal 24 months).
Next, we examined the linear trajectory of maternal mental health from these time points and its relation with child outcomes. LGCMs were most suited in this case to capture an individual's mood trajectory and inter-individual differences in these trajectories. Finally, we added household income as an exposure and school readiness skills as outcomes into the LGCMs to understand the contribution of antenatal maternal mental health (intercept) and its linear trajectory (slope) as potential mediators. As the indirect paths through two covarying latent mediators could be sensitive to omitted confounders, we conducted correlated augmented model sensitivity analysis (CAMSA), which used correlations between residuals, termed confounder correlations, to model the effects of the omitted confounders (Tofighi et al., 2019). These models were completed using Mplus 8 (Los Angeles, CA: Muthén & Muthén). P-values were provided in multiple degrees of freedom tests, including LGCMs. For all other analyses, bootstrap confidence intervals were presented.
Missing data
Prior to analysis, we estimated that the minimum sample size needed for our final LGCM to detect an effect (Cohen's d of 0.25) was 306. A post-hoc Monte Carlo simulation was also conducted with our sample size to understand whether the observed and expected Chi-square tests of model fit were comparable at α = 0.05 and to ensure that β was >0.80. Our post-hoc Monte Carlo simulation with a sample size of 505 resulted in powers, as expressed in % significant coefficients, of 0.84–1.00. Given that the indicator was categorical, we utilised robust maximum likelihood (MLR) estimation to account for 49 children who attended the 6-year-old visit but missed the 2-year-old visit.
Ethics approval
The study was approved by the Singapore National Healthcare Group and SingHealth Group Institutional Review Boards. All mothers gave informed consent at recruitment and after each amendment, and all children, who turned 7 years in 2017, assented to the study.
Results
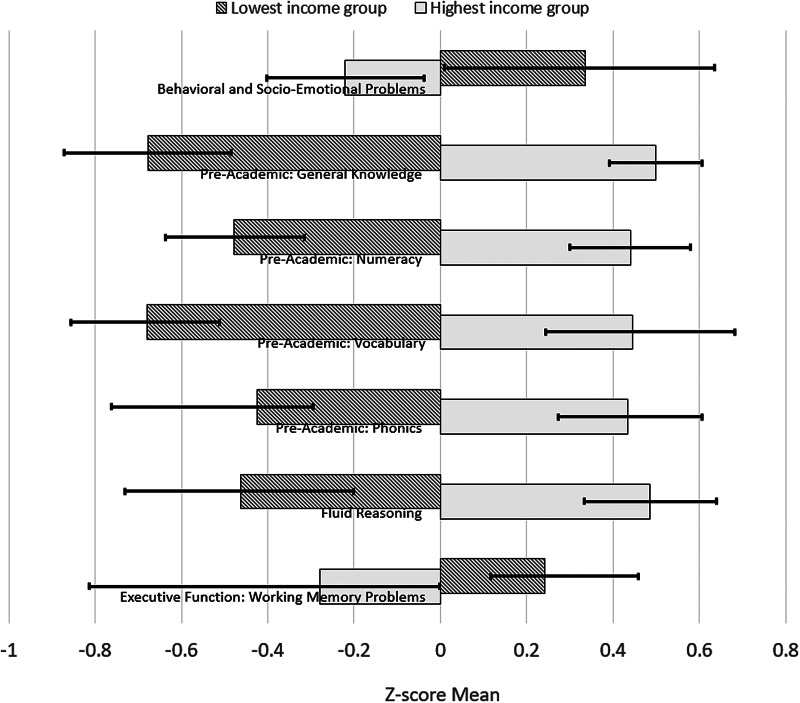
Table 1 shows the demographic characteristics of the cohort. Sixteen percent of the mothers reported a household income <S$2000/month (US$1470/month or £1133/month). Between household income groups, notable gradients were found in maternal mental health and child outcomes. Following the format of the Programme for International Student Assessment (PISA), Fig. 2 shows the Z-score mean differences in child outcomes between the top and the bottom household income groups (Organisation for Economic Co-operation Development, 2012). We found that the poverty-related gaps were 0.60 s.d. (95% Cl: 0.28–0.92) in the behavioural and socio-emotional dimension, 0.86 (95% Cl: 0.64, 1.07) to 1.21 s.d. (95% CI: 1.02, 1.40) in major pre-academics (i.e. general knowledge, numeracy, vocabulary and phonics), 0.95 s.d. (95% CI: 0.66, 1.23) in fluid reasoning and 0.52 (95% Cl: 0.23, 0.67) in working memory.
Table 1.
Demographics and characteristics of the cohort (by household income level)
| Cohort N = 1076 | <S$2000 n = 177 | S$2000–$3999 n = 338 | S$4000–$5999 n = 271 | >S$6000 n = 290 | OR (95% CI) ⩾ S$2000 relative to < S$2000 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||
| Maternal education | |||||||||||
| High school and below (Ref) | 353 | 32.1 | 114 | 66.3 | 151 | 45.8 | 59 | 22.3 | 12 | 4.4 | NA |
| Post high school | 398 | 36.2 | 50 | 29.1 | 146 | 44.2 | 121 | 45.8 | 62 | 22.5 | (2.65, 5.27) 3.74 |
| University | 348 | 31.7 | 8 | 4.7 | 33 | 10.0 | 84 | 31.8 | 201 | 73.1 | (13.03, 55.83) 26.97 |
| Male (Ref) | 537 | 52.7 | 78 | 48.1 | 168 | 52.0 | 133 | 52.2 | 158 | 56.6 | (0.59, 1.13) 0.81 |
| Breastfeeding >3months | 582 | 54.1 | 51 | 28.8 | 143 | 42.3 | 160 | 59.0 | 228 | 78.6 | (2.54, 5.56) 3.76 |
| Smoke exposure (cotinine level and/or reported) | 160 | 14.9 | 51 | 28.8 | 68 | 20.1 | 37 | 13.7 | 9 | 3.1 | (0.24, 0.51) 0.35 |
| Mean | s.d. | Mean | s.d. | Mean | s.d. | Mean | s.d. | Mean | s.d. | p | |
| Maternal | |||||||||||
| Age at delivery | 31.41 | 5.10 | 29.67 | 6.14 | 30.72 | 5.35 | 31.32 | 4.69 | 31.41 | 5.10 | <0.001 |
| Parity (antenatal) | 0.84 | 0.95 | 1.14 | 1.07 | 0.96 | 1.05 | 0.74 | 0.88 | 0.65 | 0.79 | <0.001 |
| Gestational age | 38.78 | 1.44 | 38.62 | 1.44 | 38.75 | 1.43 | 38.61 | 1.28 | 39.04 | 1.56 | 0.002 |
| Antenatal | |||||||||||
| Depression score (EPDS) | 7.45 | 4.46 | 8.81 | 5.03 | 8.06 | 4.27 | 7.21 | 4.45 | 6.01 | 3.89 | <0.001 |
| State-anxiety score (STAI-S) | 34.72 | 9.79 | 38.83 | 10.01 | 36.71 | 9.50 | 33.34 | 9.17 | 31.27 | 9.15 | <0.001 |
| Total anxiety score (Total STAI) | 71.26 | 17.89 | 78.72 | 18.55 | 74.77 | 17.09 | 69.03 | 16.39 | 65.01 | 16.92 | <0.001 |
| Postnatal 3-month | |||||||||||
| Depression score (EPDS) | 6.48 | 4.76 | 7.74 | 4.90 | 7.24 | 5.14 | 6.17 | 4.47 | 5.26 | 4.29 | <0.001 |
| State-anxiety score (STAI-S) | 34.17 | 10.28 | 37.51 | 10.05 | 35.45 | 10.55 | 33.52 | 10.07 | 31.37 | 9.58 | <0.001 |
| Total anxiety score (Total STAI) | 70.54 | 19.34 | 76.69 | 18.65 | 72.87 | 20.10 | 69.33 | 18.66 | 65.23 | 18.39 | <0.001 |
| Cohort | <S$2000 (Ref.) | S$2000–$3999 | S$4000–$5999 | >S$6000 | |||||||
| Mean | s.d. | Mean | s.d. | Mean | s.d. | Mean | s.d. | Mean | s.d. | ||
| Postnatal 24-month | |||||||||||
| Depression score (EPDS) | 6.60 | 4.97 | 8.15 | 4.65 | 7.42 | 5.18 | 6.10 | 5.19 | 5.71 | 4.75 | 0.004 |
| State-anxiety score (STAI-S) | 34.73 | 10.00 | 37.95 | 9.10 | 36.29 | 9.93 | 34.41 | 10.09 | 32.25 | 10.24 | <0.001 |
| Total anxiety score (Total STAI) | 70.97 | 19.55 | 77.22 | 17.17 | 74.19 | 19.08 | 70.52 | 20.35 | 66.03 | 20.05 | <0.001 |
| Child | |||||||||||
| Birthweight | 3.12 | 0.45 | 3.06 | 0.44 | 3.08 | 0.44 | 3.09 | 0.46 | 3.17 | 0.45 | 0.047 |
| Four dimensions of school readiness | |||||||||||
| (1) Behavioural and social–emotional at 2 years, Z-score | |||||||||||
| Internalising | 0.00 | 1.00 | 0.559 | 1.22 | 0.11 | 1.09 | −0.10 | 0.83 | −0.32 | 0.79 | <0.001 |
| Externalising | 0.00 | 1.00 | 0.350 | 1.11 | 0.11 | 1.01 | −0.06 | 0.92 | −0.20 | 0.96 | 0.004 |
| 2) Pre-academic skills at 4 years, Z-score | |||||||||||
| Lollipop | 0.00 | 1.00 | −0.61 | 0.99 | −0.28 | 0.99 | 0.10 | 0.90 | 0.46 | 0.81 | <0.001 |
| NKT | 0.00 | 1.00 | −0.53 | 0.88 | −0.28 | 0.87 | 0.04 | 0.84 | 0.44 | 1.08 | <0.001 |
| PPVT | 0.00 | 1.00 | −0.66 | 0.81 | −0.34 | 0.82 | 0.20 | 0.97 | 0.43 | 1.02 | <0.001 |
| CTOPP | 0.00 | 1.00 | −0.42 | 0.69 | −0.27 | 0.67 | 0.05 | 0.93 | 0.43 | 1.25 | <0.001 |
| 3) Fluid reasoning at 4.5 years, Z-score | 0.00 | 1.00 | −0.46 | 1.07 | −0.25 | 0.92 | 0.06 | 0.94 | 0.46 | 0.93 | <0.001 |
| 4) Executive function (working memory) at 6 years | |||||||||||
| SWM total errors | 75.16 | 14.46 | 76.52 | 12.79 | 77.72 | 15.37 | 74.60 | 14.62 | 71.93 | 13.56 | 0.010 |
Fig. 2.
Differences in children's outcomes between the top and bottom household income groups. Whiskers represent 95% bias-corrected confidence interval of the Z-score mean.
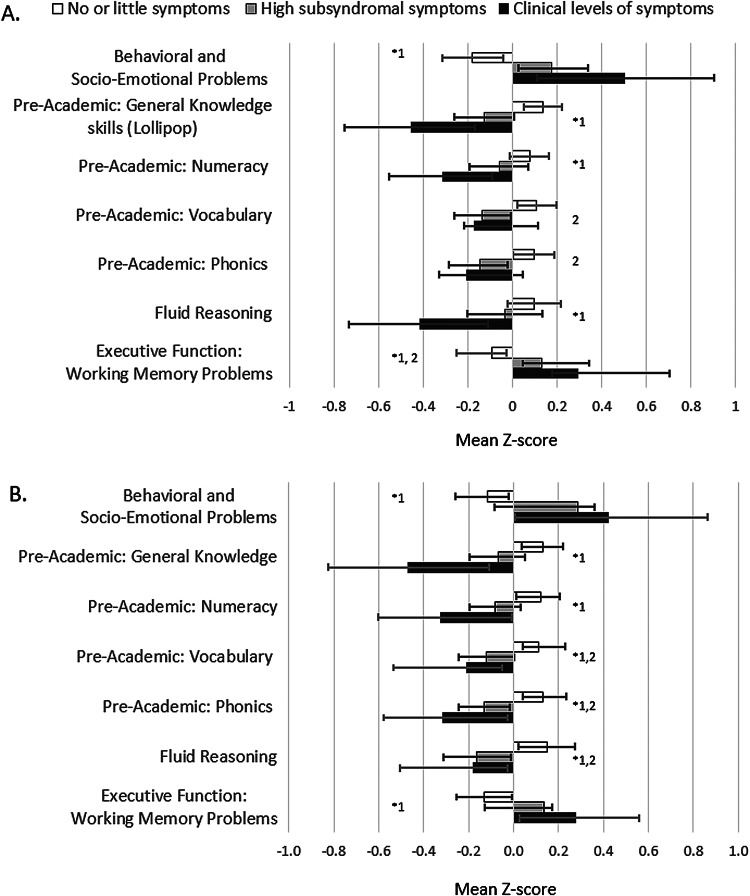
Of the 7.3 and 6.5% of mothers reporting clinical levels of depressive and anxiety symptoms, respectively, at least 78.6% reported both types of symptoms. Another 30.9 and 31.4% were in the highest, subclinical depressive and anxiety (>0.35 and >1.50 s.d. above the mean of EPDS and STAI) levels of symptoms, respectively. There was a depressive symptom gradient seen in most of the child outcomes, except for vocabulary and phonics; however, the state anxiety gradient was present for all outcomes (Fig. 3).
Fig. 3.
Child outcomes by gradients of (A) maternal depressive and (B) anxiety symptoms. ANOVA *p < 0.05 and Post-hoc Tukey p < 0.05 1no vs. clinical, 2no vs. high.
Our initial step in building an LGCM was to utilise different Latent State models to determine whether the latent maternal mental health constructs from the two depression and anxiety scales at three time points were valid and to understand the residual structure of the models (see online Supplementary text, online Supplementary Figs S1, S2 and S3). Online Supplementary Table S1 (see online Supplementary material) shows the improvements in the fit indices with each new model. The evaluation of model fit was based on the Chi-square statistic, comparative fit index (CFI), root mean square error of approximation (RMSEA), standardised root mean square residual (SRMR) and Akaike information criteria (AIC). It is important to note that a non-significant result in the Chi-square statistic of latent models is known to be difficult to achieve in large samples. The most parsimonious model with CFI >0.95, RMSEA <0.05 and SRMR 0.05 was selected.
From our initial LGCM (see online Supplementary Fig. S4), we found that pregnant women in this cohort varied substantially in their antenatal mental health (VarINTERCEPT = 12.13, Z = 11.54, p < 0.001) and in their intra-individual change of mental health over time (VarSLOPE = 1.13, Z = 3.21, p = 0.001). However, as a group, a general pattern emerged in that the mean change in mental health over time was small and negative (MSLOPE = −0.21, Z = −3.60, p < 0.001), indicating that mothers reported an overall improved mental health from antenatal to the postnatal period. The negative correlation of −0.167 in online Supplementary Fig. S4 (see online Supplementary material) between the intercept and the slope indicated that mothers with poorer antenatal mental health symptoms tended to show fewer improvements over time when compared to mothers with more optimal antenatal mental health.
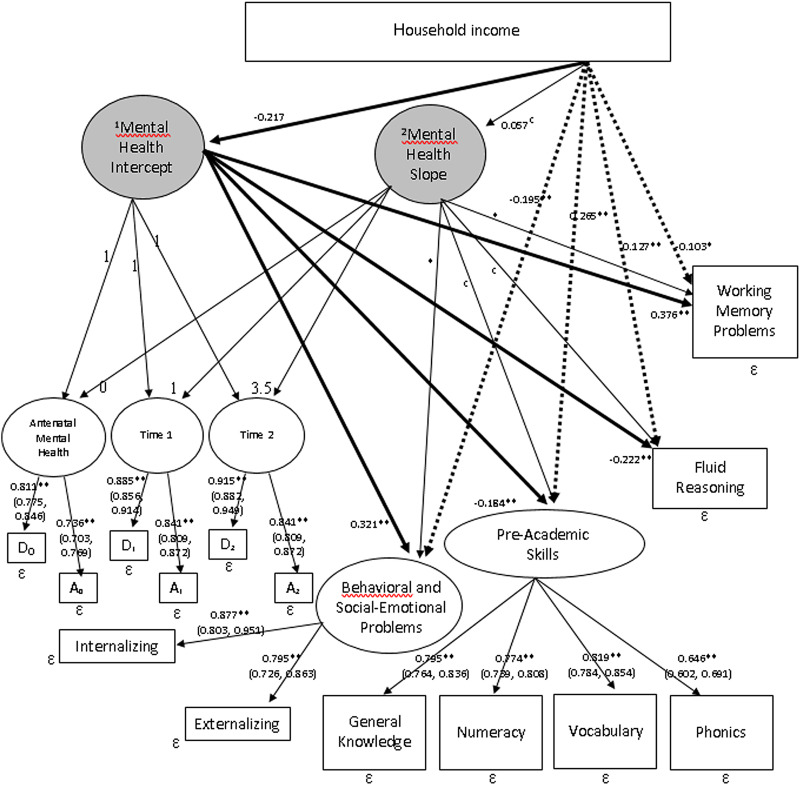
We next sought to understand whether household income influenced mental health trajectories and child outcomes, and subsequently whether antenatal maternal mental health provided an indirect path to predict child outcomes. Figure 4 shows our final latent growth curve mediation model (LGCMM). The higher the household income, the better the antenatal maternal mental health (β = −0.217, p < 0.001) and all four dimensions of school readiness skills (Table 2 direct path coefficients). Furthermore, antenatal maternal mental health mediated at least a quarter of the total effects of household income on the offspring's behavioural and social–emotional skills at 2 years as well as fluid reasoning at 4.5 years, 13.2% of the total effects on pre-academic skills at 4 years and 44.2% of the total effects on working memory at 6 years (Table 2).
Fig. 4.
LGCMM with predictor and outcomes. Rectangular: observed variable; oval: latent variable; *p < 0.05; **p < 0.01; 95% CIs are shown in parentheses; 1Latent variable derived from the two depressive and anxiety symptom measures during pregnancy (time intercept = 0); 2Trajectory of the latent mental health variables from pregnancy, to postnatal 3-months and 24-months. Solid lines represent indirect paths and dashed lines represent direct paths to the outcomes.
Table 2.
Path estimates of the direct effects and indirect effects via the mental health intercept mediator (i)
| Paths from household income to | Direct | Indirect to i | Indirect from i | p (x to y via i) | % of indirect/total |
|---|---|---|---|---|---|
| Behavioural and social–emotional problems | −0.195 (−0.289, −0.102) | −0.217 (−0.283, −0.150) | 0.321 (0.221, 0.421) | <0.001 | 26.4 |
| Pre-academic skills | 0.265 (0.200, 0.327) | −0.184 (−0.269, −0.095) | 0.007 | 13.2 | |
| Fluid reasoning | 0.127 (0.048, 0.203) | −0.222 (−0.312, −0.135) | 0.001 | 27.5 | |
| Working memory problems | −0.103 (−0.201, −0.013) | 0.376 (0.309, 0.465) | <0.001 | 44.2 |
No indirect effects found via the mental health slope mediator; total effects = sum of direct effect and indirect effect (product of indirect to i and indirect from i).
Maternal symptom trajectory provided paths to behavioural and social–emotional as well as working memory problems in this study; however, these changes over time were not predicted by household income and could not provide a complete indirect path to these two outcomes. A correlated augmented model designed to quantify the unmeasured confounder bias in models with intercept and slope mediators was therefore not required. Instead, sensitivity plots with 95% Cl were produced to understand the extent to which the unmeasured confounders could reverse the mediation results of the LGCMM (Imai et al., 2010; VanderWeele, 2016; VanderWeele and Tchetgen Tchetgen, 2017). We plotted our indirect effects against a range of hypothetical sensitivity parameters, also called rho (see online Supplementary Fig. S5). The plots indicated that the indirect paths to the four school readiness dimensions would be trustworthy until the sensitivity parameters were 0.70, 0.40, 0.43 and 0.64, respectively, which were highly implausible given the actual coefficients listed in Fig. 4. Hence, the sensitivity analyses indicated that antenatal mental health was a robust mediator between household income and school readiness, even when unmeasured confounders were accounted for.
Comment
Principal findings
This longitudinal birth cohort uniquely explored the intergenerational transmission of income disparity in school readiness by delineating the role of maternal mental health symptoms in the foetal and postnatal milieu. Consistent with prior literature, lower household income predicted higher antenatal mental health problems and poorer readiness for school in the offspring (Petterson and Albers, 2001; Kiernan and Huerta, 2008; Allen et al., 2014; Meaney, 2018). While the effect of household income on a diverse variety of child outcomes could not be disputed, this study supported accumulating evidence that subclinical maternal depressive and anxiety symptoms, not only clinical disorders, adversely influenced children's capabilities in a graded fashion. Our two critical findings were that almost 40% of women reported high antenatal mental health symptoms and these symptoms independently explained 13–44% of the income-school readiness gap.
Strengths of the study
LGCMs are considered a powerful approach to test for intra-individual changes over time and inter-individual differences in trajectories across time (Hertzog and Nesselroade, 1987; Curran and Hussong, 2003). In this study, while the mean mental health trajectory showed slight improvements over time, trajectories differed based on each mother's mental health in pregnancy; mothers with worse symptoms during pregnancy improved less in mood over time, when compared to those with better symptoms during pregnancy. Recent data demonstrated that earlier onset of mental health symptoms during pregnancy was a characteristic of pregnant women with moderate and severe anxiety, depression, whereas later onset (i.e. third trimester) tended to be milder (Putnam et al., 2017). Furthermore, predictors of severe pregnancy depression and anxiety, such as low self-esteem, poor perceived support, adverse life experiences and a history of child abuse, could potentially predispose women to parental styles characterised by low care and high control, impaired mother–infant bonding, as well as other psychiatric conditions (Leigh and Milgrom, 2008; Grant et al., 2012; Huizink et al., 2017). Thus, high severity of mental health symptoms during pregnancy likely warrants effective treatment before a cascade of downstream complications incur.
The use of symptom scale measures of depression and anxiety allowed us to compare mothers with subthreshold and clinical levels of symptoms of mothers. The association between high, subsyndromal levels of symptoms and child outcomes implied that the risk for worse child outcomes was not limited to women with clinical levels of symptoms. Rather, maternal mental health variations have negative effects on the outcomes of the next generation in a dose–response fashion. This study adds to the literature by suggesting that there are other considerable consequences to the offspring of mothers with varying levels of mental health symptoms, not only in behavioural and socio-emotional functions, but also multiple components of school readiness. This finding is of considerable public health significance as a large percentage of women face subclinical levels of affective symptoms during pregnancy.
Limitations of the data
Although the LGCMM allowed us to examine in-depth maternal mental health trajectories from the antenatal to the postnatal period, the sample size was not large enough to test more than one mediating pathway between household income and child outcomes, as well as potential effects of other confounders. The pertinent confounders in our multi-ethnic population included parenting styles and quality, roles of father, social and family values, such as cultural expectations and incremental beliefs. To address this, we conducted sensitivity analyses to account for unmeasured confounder bias. Another limitation was that we were unable to explore the bidirectional effects of the child on maternal symptoms; however, the mother's mental health trajectory over time in the growth curve analyses likely captured the complex interplay between the child and the mother. Finally, the child behavioural and social–emotional rating scales were completed by mothers and there were previous studies showing a small association between higher maternal depression and parental tendency to over-report child behavioural problems while others did not find a ‘depressed mother reporter bias’ (Fergusson et al., 1993; Boyle and Pickles, 1997). Therefore, when the mother was the only source of information on the child, the association between maternal mental health and child outcomes could be stronger than in reality. In this cohort, we collected information on the child's behaviours from the fathers and our ongoing study will explore the differences between maternal and paternal reports.
Interpretation
Similar to other studies, we confirmed stronger effects of antenatal maternal mental health on the child compared to perinatal mental health variations across time (Evans et al., 2001, 2012; Matthey et al., 2006; Monk et al., 2013; Qiu et al., 2013; Glover, 2014; O'Donnell et al., 2014; Rifkin-Graboi et al., 2015; Sandman et al., 2015; Lebel et al., 2016; Meaney, 2018). The apparent influence of antenatal maternal mental health on child outcomes suggests that maternal mental health alters the in utero environment with an impact on the foetus' brain development. This pathway may thus serve as a mechanism underlying socio-economic disparities in cognition and achievement. Our group previously used neonatal neuroimaging to demonstrate a link between antenatal maternal affective symptoms and the development of infant brain structures (Qiu et al., 2013; Rifkin-Graboi et al., 2015; Wen et al., 2017). In these studies, antenatal maternal symptoms of depression and anxiety were associated with the hippocampal growth and connectivity of the amygdala with the insula (Qiu et al., 2013; Wen et al., 2017).
Conclusions
This study aims to elucidate the contribution of maternal mental health to income disparities of school readiness outcomes. While this study suggests the antenatal period as a potential time for maternal intervention, there is important evidence for the reversibility of the effects of poorer maternal mental health through postnatal intervention (Weissman et al., 2015; Handley et al., 2017; Meaney, 2018). The brain plasticity of children also allows for sensitivity to interventions in early childhood (Cicchetti et al., 2000; Shaw et al., 2009; Shonkoff et al., 2012; Noble et al., 2015). Hence, maternal mental health, whether antenatal or postnatal, may be a salient prevention focus moving forward. This study provides justifications for the need to embed universal mental health screens at the first obstetric appointment, offer low-resource therapeutic approaches for women with subthreshold depression and anxiety symptoms (e.g. web-based programs), and consider population-level prevention through improving the mental health literacy of women during early childbearing ages (Ashford et al., 2016; Khanlari et al., 2019). A novel, pre-emptive strategies to improve mother's mental health through a life-course development approach may be indispensable for optimising the achievement, cognition and behaviours of the next generation.
Acknowledgements
We thank Dr Dimple Rajgor for her assistance in editing, formatting, and in submitting the manuscript for publication. The GUSTO study group includes Allan Sheppard, Amutha Chinnadurai, Anne Goh, Anne Rifkin-Graboi, Anqi Qiu, Arijit Biswas, Bee Wah Lee, Boon Long Quah, Borys Shuter, Chai Kiat Chng, Cheryl Ngo, Choon Looi Bong, Christiani Jeyakumar Henry, Claudia Chi, Cornelia Chee, Daniel Goh, Doris Fok, E Shyong Tai, Elaine Tham, Elaine Quah, Evelyn Loo, Fabian Yap, Falk Mueller-Riemenschneider, George Yeo, Heng Hao Tan, Hugo van Bever, Iliana Magiati, Inez Wong, Ivy Lau, Izzuddin Bin Mohd Aris, Jeevesh Kapur, Jenny Richmond, Jerry Chan, Joanna Holbrook, Joanne Yoong, Joao Ferreira., Jonathan Choo, Jonathan Bernard, Joshua Gooley, Keith Godfrey, Kenneth Kwek, Kok Hian Tan, Krishnamoorthy Niduvaje, Kuan Jin Lee, Leher Singh, Lieng Hsi Ling, Lin Lin Su, Ling-Wei Chen, Marielle Fortier, Mark Hanson, Mary Chong, Mary Rauff, Mei Chien Chua, Melvin Khee-Shing Leow, Mya Thway Tint, Neerja Karnani, Ngee Lek, Oon Hoe Teoh, P. C. Wong, Paulin Tay Straughan, Pratibha Agarwal, Queenie Ling Jun Li, Rob M. van Dam, Salome A. Rebello, Seang-Mei Saw, See Ling Loy, S. Sendhil Velan, Seng Bin Ang, Shang Chee Chong, Sharon Ng, Shiao-Yng Chan, Shu-E Soh, Sok Bee Lim, Stella Tsotsi, Stephen Hsu, Sue Anne Toh, Swee Chye Quek, Victor Samuel Rajadurai, Walter Stunkel, Wayne Cutfield, Wee Meng Han, Wei Wei Pang, Yin Bun Cheung, Yiong Huak Chan and Yung Seng Lee.
Financial support
This research is funded by the Singapore Ministry of Health's National Medical Research Council and Singapore National Research Foundation under their Translational and Clinical Research (TCR) Flagship Program (NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014) and the Ministry of Health's Health Services Research Grant (HSR–NIG 011/2015).
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S204579602000102X.
click here to view supplementary material
Data
The cohort investigators are in the process of moving towards an open cohort. In the interim, data can be shared upon request. Requests can be emailed to the corresponding author, Dr Evelyn Law at, evelyn_law@nuhs.edu.sg
Conflict of interest
C.Y.S. is part of the Epigen Academic Consortium and has received academic research funding from Abbot Nutrition, Nestec and Danone, outside of this submitted work. All other authors report no conflicts of interest or financial relationships.
References
- Achenbach TM and Rescorla LA (2000) Manual for the ASEBA Preschool Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Allen J, Balfour R, Bell R and Marmot M (2014) Social determinants of mental health. International Review of Psychiatry 26, 392–407. [DOI] [PubMed] [Google Scholar]
- Ashford MT, Olander EK and Ayers S (2016) Computer- or web-based interventions for perinatal mental health: a systematic review. Journal of Affective Disorders 197, 134–146. [DOI] [PubMed] [Google Scholar]
- Blair C and Raver CC (2015) School readiness and self-regulation: a developmental psychobiological approach. Annual Review of Psychology 66, 711–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle MH and Pickles AR (1997) Influence of maternal depressive symptoms on ratings of childhood behavior. Journal of Abnormal Child Psychology 25, 399–412. [DOI] [PubMed] [Google Scholar]
- Cents R, Diamantopoulou S, Hudziak J, Jaddoe V, Hofman A, Verhulst F, Lambregtse-van den Berg M and Tiemeier H (2013) Trajectories of maternal depressive symptoms predict child problem behaviour: the generation R study. Psychological Medicine 43, 13–25. [DOI] [PubMed] [Google Scholar]
- Chew AL (1981) The Lollipop Test, A Diagnostic Screening Test of School Readiness. Atlanta, GA: Humanics. [Google Scholar]
- Cicchetti D, Rogosch FA and Toth SL (2000) The efficacy of toddler-parent psychotherapy for fostering cognitive development in offspring of depressed mothers. Journal of Abnormal Child Psychology 28, 135–148. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM and Sagovsky R (1987) Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry 150, 782–786. [DOI] [PubMed] [Google Scholar]
- Curran P and Hussong A (2003) The use of latent trajectory models in psychopathology research. Journal of Abnormal Psychology 112, 526–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis CL, Falah-Hassani K and Shiri R (2017) Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. The British Journal of Psychiatry 210, 315–323. [DOI] [PubMed] [Google Scholar]
- Donaldson JA, Loh J, Mudaliar S, Md Kadir M, Wu B and Yeoh LK (2013) Measuring poverty in Singapore: frameworks for consideration. Social Space 6, 58–66. [Google Scholar]
- Evans J, Heron J, Francomb H, Oke S and Golding J (2001) Cohort study of depressed mood during pregnancy and after childbirth. BMJ 323, 257–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J, Melotti R, Heron J, Ramchandani P, Wiles N, Murray L and Stein A (2012) The timing of maternal depressive symptoms and child cognitive development: a longitudinal study. Journal of Child Psychology and Psychiatry 53, 632–640. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Lynskey MT and Horwood LJ (1993) The effect of maternal depression on maternal ratings of child behavior. Journal of Abnormal Child Psychology 21, 245–269. [DOI] [PubMed] [Google Scholar]
- Fried R, Hirshfeld-Becker D, Petty C, Batchelder H and Biederman J (2015) How informative is the CANTAB to assess executive functioning in children with ADHD? A controlled study. Journal of Attention Disorders 19, 468–475. [DOI] [PubMed] [Google Scholar]
- Glover V (2014) Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Practice & Research Clinical Obstetrics & Gynaecology 28, 25–35. [DOI] [PubMed] [Google Scholar]
- Goodman SH and Tully EC (2009) Recurrence of depression during pregnancy: psychosocial and personal functioning correlates. Depression and Anxiety 26, 557–567. [DOI] [PubMed] [Google Scholar]
- Grant K-A, Bautovich A, McMahon C, Reilly N, Leader L and Austin M-P (2012) Parental care and control during childhood: associations with maternal perinatal mood disturbance and parenting stress. Archives of Women's Mental Health 15, 297–305. [DOI] [PubMed] [Google Scholar]
- Griffin S (2002) The development of math competence in the preschool and early school years: cognitive foundations and instructional strategies. In Roher JM (ed.), Mathematical cognition. Greenwich, CT: Information Age Publishing, Inc. [Google Scholar]
- Hackman D, Farah M and Meaney M (2010) Socioeconomic status and the brain: mechanistic insights from human and animal research. Nature Reviews. Neuroscience 11, 651–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handley ED, Michl-Petzing LC, Rogosch FA, Cicchetti D and Toth SL (2017) Developmental cascade effects of interpersonal psychotherapy for depressed mothers: longitudinal associations with toddler attachment, temperament, and maternal parenting efficacy. Development and Psychopathology 29, 601–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertzog C and Nesselroade J (1987) Beyond autoregressive models: some implications of the trait-state distinction for the structural modeling of developmental change. Child Development 58, 93–109. [PubMed] [Google Scholar]
- High PC (2008) School readiness. Pediatrics 121, e1008–e1015. [DOI] [PubMed] [Google Scholar]
- Huizink AC, Menting B, De Moor MHM, Verhage ML, Kunseler FC, Schuengel C and Oosterman M (2017) From prenatal anxiety to parenting stress: a longitudinal study. Archives of Women's Mental Health 20, 663–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai K, Keele L and Tingley D (2010) A general approach to causal mediation analysis. Psychological Methods 15, 309–334. [DOI] [PubMed] [Google Scholar]
- Kaufman A and Kaufman N (2004) Kaufman Brief Intelligence Test, 2nd Edn. Bloomington, MN: Pearson Inc. [Google Scholar]
- Khanlari S, Barnett Am B, Ogbo FA and Eastwood J (2019) Re-examination of perinatal mental health policy frameworks for women signalling distress on the Edinburgh Postnatal Depression Scale (EPDS) completed during their antenatal booking-in consultation: a call for population health intervention. BMC Pregnancy and Childbirth 19, 221–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiernan KE and Huerta MC (2008) Economic deprivation, maternal depression, parenting and children's cognitive and emotional development in early childhood 1. The British Journal of Sociology 59, 783–806. [DOI] [PubMed] [Google Scholar]
- Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM and Davis MM (2010) Risk factors for depressive symptoms during pregnancy: a systematic review. American Journal of Obstetrics and Gynecology 202, 5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel C, Walton M, Letourneau N, Giesbrecht GF, Kaplan BJ and Dewey D (2016) Prepartum and postpartum maternal depressive symptoms are related to children's brain structure in preschool. Biological Psychiatry 80, 859–868. [DOI] [PubMed] [Google Scholar]
- Leigh B and Milgrom J (2008) Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry 8, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luciana M and Nelson CA (2002) Assessment of neuropsychological function through use of the Cambridge neuropsychological testing automated battery: performance in 4- to 12-year-old children. Developmental Neuropsychology 22, 595–624. [DOI] [PubMed] [Google Scholar]
- Matthey S, Henshaw C, Elliott S and Barnett B (2006) Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale – implications for clinical and research practice. Archives of Women's Mental Health 9, 309–315. [DOI] [PubMed] [Google Scholar]
- Meaney MJ (2018) Perinatal maternal depressive symptoms as an issue for population health. American Journal of Psychiatry 175, 1084–1093. [DOI] [PubMed] [Google Scholar]
- Monk C, Georgieff MK and Osterholm EA (2013) Research review: maternal prenatal distress and poor nutrition – mutually influencing risk factors affecting infant neurocognitive development. Journal of Child Psychology and Psychiatry 54, 115–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno MA (2013) School readiness. JAMA Paediatrics 167, 784. [DOI] [PubMed] [Google Scholar]
- Murray D and Cox JL (1990) Screening for depression during pregnancy with the Edinburgh Depression Scale (EPDS). Journal of Reproductive and Infant Psychology 8, 99–107. [Google Scholar]
- Naglieri JA and Pfeiffer SI (1983) Stability, concurrent and predictive validity of the PPVT-R. Journal of Clinical Psychology 39, 965–967. [DOI] [PubMed] [Google Scholar]
- Noble K, Houston S, Brito N, Bartsch H, Kan E, Kuperman J, Akshoomoff N, Amaral D, Bloss C and Libiger O (2015) Family income, parental education and brain structure in children and adolescents. Nature Neuroscience 18, 773–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell K and Meaney M (2017) Fetal origins of mental health: the developmental origins of health and disease hypothesis. The American Journal of Psychiatry 174, 319–328. [DOI] [PubMed] [Google Scholar]
- O'Donnell K, Glover V, Barker E and O'Connor T (2014) The persisting effect of maternal mood in pregnancy on childhood psychopathology. Development and Psychopathology 26, 393–403. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation Development, (OECD) (2012) Equity and Quality in Education: Supporting Disadvantaged Students and Schools, Figure II.2.3. Paris, France: OECD Publishing. Available at 10.1787/9789264130852-en.pdf accessible at, https://www.oecd.org/education/school/50293148.pdf (17 Jan 2020). [DOI] [Google Scholar]
- Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, O'Connor TG and Stein A (2013) Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry 70, 1312–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry RE, Braren SH and Blair C, Family Life Project Key I (2018) Socioeconomic risk and school readiness: longitudinal mediation through children's social competence and executive function. Frontiers in Psychology 9, 1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petterson SM and Albers AB (2001) Effects of poverty and maternal depression on early child development. Child Development 72, 1794–1813. [DOI] [PubMed] [Google Scholar]
- Phua DY, Kee M, Koh DXP, Rifkin-Graboi A, Daniels M, Chen H, Chong YS, Broekman BFP, Magiati I, Karnani N, Pluess M and Meaney MJ, Growing Up In Singapore Towards Healthy Outcomes Study G (2017) Positive maternal mental health during pregnancy associated with specific forms of adaptive development in early childhood: evidence from a longitudinal study. Development and Psychopathology 29, 1573–1587. [DOI] [PubMed] [Google Scholar]
- Piccolo LR, Merz EC, He X, Sowell ER and Noble KG (2016) Age-related differences in cortical thickness vary by socioeconomic status. PLoS One 11, e0162511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam KT, Wilcox M, Robertson-Blackmore E, Sharkey K, Bergink V, Munk-Olsen T, Deligiannidis KM, Payne J, Altemus M, Newport J, Apter G, Devouche E, Viktorin A, Magnusson P, Penninx B, Buist A, Bilszta J, O'Hara M, Stuart S, Brock R, Roza S, Tiemeier H, Guille C, Epperson CN, Kim D, Schmidt P, Martinez P, Di Florio A, Wisner KL, Stowe Z, Jones I, Sullivan PF, Rubinow D, Wildenhaus K and Meltzer-Brody S (2017) Clinical phenotypes of perinatal depression and time of symptom onset: analysis of data from an international consortium. The Lancet Psychiatry 4, 477–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu A, Rifkin-Graboi A, Chen H, Chong Y, Kwek K, Gluckman P, Fortier M and Meaney M (2013) Maternal anxiety and infants' hippocampal development: timing matters. Translational Psychiatry 3, e306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rifkin-Graboi A, Meaney MJ, Chen H, Bai J, Hameed WBR, Tint MT, Broekman BF, Chong Y-S, Gluckman PD and Fortier MV (2015) Antenatal maternal anxiety predicts variations in neural structures implicated in anxiety disorders in newborns. Journal of the American Academy of Child & Adolescent Psychiatry 54, 313–321, e2. [DOI] [PubMed] [Google Scholar]
- Sandman CA, Buss C, Head K and Davis EP (2015) Fetal exposure to maternal depressive symptoms is associated with cortical thickness in late childhood. Biological Psychiatry 77, 324–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf RJ (2016) School readiness. Paediatrics in Review 37, 501–503. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN and Gardner F (2009) Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology 21, 417–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen H, Magnusson C, Rai D, Lundberg M, Le-Scherban F, Dalman C and Lee BK (2016) Associations of parental depression with child school performance at age 16 years in Sweden. JAMA Psychiatry 73, 239–246. [DOI] [PubMed] [Google Scholar]
- Sheridan MA and McLaughlin KA (2016) Neurobiological models of the impact of adversity on education. Current Opinion in Behavioral Sciences 10, 108–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, Pascoe J and Wood DL, Child CoPAo, Health F, Committee on Early Childhood A, Care D (2012) The lifelong effects of early childhood adversity and toxic stress. Pediatrics 129, e232–e246. [DOI] [PubMed] [Google Scholar]
- Skouteris H, Wertheim EH, Rallis S, Milgrom J and Paxton SJ (2009) Depression and anxiety through pregnancy and the early postpartum: an examination of prospective relationships. Journal of Affective Disorders 113, 303–308. [DOI] [PubMed] [Google Scholar]
- Soh S, Tint M, Gluckman P, Godfrey K, Rifkin-Graboi A, Chan Y, Stünkel W, Holbrook J, Kwek K and Chong Y (2014) Cohort profile: growing up in Singapore towards healthy outcomes (GUSTO) birth cohort study. International Journal of Epidemiology 43, 1401–1409. [DOI] [PubMed] [Google Scholar]
- Spielberger CD (2010) State-trait anxiety inventory. In Weiner IB and Craighead WE (eds), The Corsini Encyclopedia of Psychology. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Tietz A, Zietlow A-L and Reck C (2014) Maternal bonding in mothers with postpartum anxiety disorder: the crucial role of subclinical depressive symptoms and maternal avoidance behaviour. Archives of Women's Mental Health 17, 433–442. [DOI] [PubMed] [Google Scholar]
- Tofighi D, Hsiao YY, Kruger ES, MacKinnon DP, Van Horn ML and Witkiewitz KA (2019) Sensitivity analysis of the no-omitted confounder assumption in latent growth curve mediation models. Structural Equation Modeling 26, 94–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ (2016) Mediation analysis: a practitioner's guide. Annual Review of Public Health 37, 17–32. [DOI] [PubMed] [Google Scholar]
- VanderWeele TJ and Tchetgen Tchetgen EJ (2017) Mediation analysis with time varying exposures and mediators. Journal of the Royal Statistical Society: Series B (Statistical Methodology) 79, 917–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verreault N, Da Costa D, Marchand A, Ireland K, Dritsa M and Khalifé S (2014) Rates and risk factors associated with depressive symptoms during pregnancy and with postpartum onset. Journal of Psychosomatic Obstetrics & Gynecology 35, 84–91. [DOI] [PubMed] [Google Scholar]
- Wagner RK, Torgesen JK, Rashotte CA and Pearson NA (2013) CTOPP-2: Comprehensive Test of Phonological Processing, 2nd Edn. Austin, TX: Pro-Ed. [Google Scholar]
- Weinberg MK, Tronick EZ, Beeghly M, Olson KL, Kernan H and Riley JM (2001) Subsyndromal depressive symptoms and major depression in postpartum women. American Journal of Orthopsychiatry 71, 87–97. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Pilowsky DJ, Poh E, Batten LA, Hernandez M, Flament MF, Stewart JA, McGrath P and Blier P (2015) Treatment of maternal depression in a medication clinical trial and its effect on children. American Journal of Psychiatry 172, 450–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh JA, Nix RL, Blair C, Bierman KL and Nelson KE (2010) The development of cognitive skills and gains in academic school readiness for children from low-income families. Journal of Educational Psychology 102, 43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen D, Poh J, Ni S, Chong Y, Chen H, Kwek K, Shek L, Gluckman P, Fortier M and Meaney M (2017) Influences of prenatal and postnatal maternal depression on amygdala volume and microstructure in young children. Translational Psychiatry 7, e1103–e1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo B, Ng T, Fung D, Chan Y, Lee Y, Koh J and Cai Y (2007) Emotional and behavioural problems in Singaporean children based on parent, teacher and child reports. Singapore Medical Journal 48, 1100–1106. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S204579602000102X.
click here to view supplementary material
Data Availability Statement
The cohort investigators are in the process of moving towards an open cohort. In the interim, data can be shared upon request. Requests can be emailed to the corresponding author, Dr Evelyn Law at, evelyn_law@nuhs.edu.sg