Abstract
Introduction:
Food insecurity (FI) is the lack of consistent access to enough food for an active and healthy life. Community-based hunger relief programs often serve as emergency food sources for families with FI. However, these programs may not provide foods that diverse populations of people prefer. We sought to evaluate the dietary patterns and preferences of families living in food-insecure neighborhoods and utilizing a community-based hunger relief program, in order to improve the utilization of local nutritional programs.
Methods:
We examined the Help Our People Eat (HOPE) community-based mobile meal program. Free-listing interviews (n = 63) were conducted with English-(66%) and Spanish-speaking (34%) participants of the program. Participants were asked about FI risk, food preferences, and dietary behaviors at home.
Results:
The majority of participants (90%) had children in the household. About 60% reported not being able to afford the type of food they enjoyed. Most participants reported using stoves for cooking (80%). Participants overwhelmingly cooked with chicken, beef, and pork. The most common side dishes included potatoes, rice, and salad. Most participants reported no interest in cooking differently or learning new recipes.
Conclusions:
A common theme throughout interviews was that families prefer similar meals, but may prepare them differently based on the language spoken. Food preferences consisted of a high intake of carbohydrate-rich meals, perhaps because these foods may be cheaper and easier to access. Notably, new recipes and cooking methods were not a priority for these families, possibly due to the time and effort needed to learn them.
Key words: Food insecurity, dietary preferences, meal preparation, mobile meal program, culturally relevant food
Introduction
Food insecurity (FI) – the lack of consistent food for an active and healthy life – remains a major public health problem in the United States of America (USA) [1]. In 2018, 11.1% of US households, or over 35 million Americans were food insecure. Households with children are at higher risk of having FI: 13.9% of households with children were food insecure in 2018. Households with incomes near or below the federal poverty level and those headed by racial and ethnic minorities are also disproportionately vulnerable to FI [1–3]. While FI has decreased over the past decade, it remains problematic in North Carolina, which has the 10th highest prevalence in the USA [1]. Winston-Salem, a medium-sized city located in Forsyth County in the Piedmont region of Northwest North Carolina, has an even higher FI rate: 16% for all households and 21% for households with children [4]. In both children and adults, FI negatively affects mental and physical health; however, children are particularly vulnerable due to its adverse effects on growth, behavior, and development [5–8].
FI is linked with poor dietary quality, including fewer fruits and vegetables, and lower nutrient intake [7]. Federal nutrition programs, such as the National School Meals Program (NSMP) and the Supplemental Nutrition Program (SNAP), provide more consistent access to nutritious food, improve dietary quality, and reduce FI for low-income households with children [9–15]. However, approximately 26% of food-insecure households in Winston-Salem do not qualify for these federal nutrition programs; furthermore, NSMP is unavailable when school is not in session [4]. Therefore, community-based hunger relief programs, such as mobile meal programs, have grown to further address local unmet needs. These organizations allow meals to be served or delivered in settings beyond schools, such as recreation centers, churches, and camps [16].
Although many studies have examined the nutrition-related behaviors and dietary preferences of participants who receive food from governmental nutrition programs, such as NSMP and SNAP, these studies have shown mixed results on the nutritional quality of food children receive [17]. There is sparse research available on mobile and community-based approaches in providing healthy and nutritious foods to diverse, low-income populations [18, 19]. To address the question of how community-based organizations can tailor the provision of healthy foods that participants living in diverse communities prefer, we undertook this exploratory study with the aim of understanding the dietary patterns, food preferences, and meal preparation methods of families at high risk for FI.
Methods
Study Setting and Population
We conducted a qualitative study of adults who utilize the Help Our People Eat (HOPE) (www.hopews.org) mobile meal program and assessed their dietary patterns, food preferences, and meal preparation methods. Adult participants were recruited from community locations that receive HOPE’s food resources, including weekend meals and produce delivery services.
Using the principles of community engagement, this study was designed, executed, and analyzed in close collaboration with our community partner, HOPE of Winston-Salem, which was founded in 2013 [20]. Every weekend, HOPE’s mobile meal program delivers free meals to children and fresh produce to families at risk for hunger, with the expressed goal of bridging children between school meals provided during the week and weekends when access to nutritious food may decline. Typical lunches provided for children include a sandwich, fruit/yogurt, milk/water, and a healthy treat. The produce offered to families varies every week based on supplier food donations, but occasionally includes non-produce items such as bread. This program partners with the local food bank, a variety of community gardens, and several food pantries in the area. HOPE delivers approximately 1100 healthy meals and 1500 lbs of fresh produce per week to 28 neighborhood sites consisting of apartment complexes, schools, community centers, and churches. These community sites are targeted by the poverty level based on census tract data and the number of children eligible for school breakfast/lunch at the neighborhood school (Table 1) [21]. All 28 sites are located in neighborhoods where at least 25% of the population lives below 200% of the federal poverty level, and 12 of those sites are in neighborhoods where 70% or more lives below 200% of the federal poverty level. Food deserts are defined by the USDA as census tract areas that qualify as low-income communities with low access to a supermarket, meaning they are more than one mile away in an urban area [22]. Twenty-three of the 28 sites are located in census tracts that qualify as food deserts [23]. All of the sites are within the Winston-Salem, North Carolina city limits. All adults who spoke either English or Spanish and presented to one of the HOPE sites were eligible to participate in this study.
Table 1.
Population characteristics of the zip codes included in the study
| 27103 | 27105 | 27107 | |
| Male | 47% | 47.9% | 46.5% |
| Children (<18 years) | 23.7% | 25.5% | 21.2% |
| Race Hispanic/Latino White Black/African American |
14.6% 46.0% 34.8% |
5.5% 72.4% 23.1% |
12.3% 72.4% 13.3% |
| Percentage of adults (25 years of age and older) with a high school graduate/higher | 87.5% | 84% | 90.6% |
| Percentage of adults (25 years of age or older) with a bachelor’s degree or higher | 34.2% | 19.9% | 31.7% |
| Median household income | $44,311 | $40,375 | $49,407 |
| Percent of individuals who live below 100% of the federal poverty level | 21.7% | 12.7% | 14.2% |
Data were obtained from the United States Census Bureau (2019): https://www.census.gov/quickfacts/fact/table/kernersvilletownnorthcarolina,walkertowntownnorthcarolina,winstonsalemcitynorthcarolina/PST04521920.
Data Collection
Through a detailed review of the literature and consultation with outside experts, we developed a free-listing interview guide consisting of 11 open-ended questions (Table 2) designed to elicit the food preferences and dietary behaviors of both adults and children in each household. These questions were pilot tested on five parents of children at risk for FI at the Downtown Health Plaza (DHP) Clinic of Wake Forest Baptist Health. DHP is a safety-net clinic that provides care to approximately 14,000 children from the same neighborhoods served by HOPE. The data from these five participants were not included in the final analysis. To evaluate fresh produce preferences, we showed participants a picture chart of various fruits and vegetables that have previously been offered by HOPE, and asked them to choose five items they used the most and five items they used the least at home (Fig. 1).
Table 2.
Interview guide questions
| • What is your favorite meal to cook/have cooked for you at home? o Tell me how you cook that meal. What foods or ingredients were used? o Do you use a stove, oven, or microwave? |
| • Are you able to afford the types of foods you like to eat? |
| • What are some other meals that you cook/are cooked regularly at home (≥once/month)? |
| • What are your child’s likes /dislikes about the prepared meals from HOPE that he/she receives? How about the fruits/vegetables? Does your family use the fruits/vegetables to cook? |
| • What are new meals or recipes that you want to learn how to cook at home? What are some ways you want to cook differently at home? |
| • What is your child’s favorite meal to eat that you cook at home? |
Fig. 1.
This graphic was shown when participants were asked about five favorite and least favorite produce items.
Free-listing interviews were conducted between June and August 2019 by study team members (E.C., C.L.A., and K.M), who were all trained in qualitative interview techniques, using the guide. The technique of free listing involves asking open-ended questions to obtain a comprehensive and exhaustive list of items within a specific domain of interest, thus eliciting themes from all responses within a question. The purpose of free listing is to reduce the need for subsequent interviews [24, 25]. HOPE participants were approached at the time of meal and/or produce delivery along two different routes of the Sunday delivery program. Each route consisted of five–seven stops. Verbal consent was obtained prior to each interview in English or Spanish, dependent on the interviewee’s preferred language. Each interview was conducted in the participant’s preferred language (English or Spanish). Participants provided verbal responses while the interviewers recorded answers onto the interview guide, with each encounter lasting 5–10 min. Demographic information collected included primary language spoken at home, if there were children in the household, and FI risk (based on the response to the one question asking if participants were able to afford the types of food they enjoyed). To characterize the neighborhoods that participants were recruited from, we determined the percentage of males, households with children, race/ethnicity, and adults who graduated high school or had a bachelor’s degree, the median household income, and percent of individuals living below 100% of the federal poverty level in each zip code included based on data from the US Census Bureau (Table 1).
Analysis
All interviews were transcribed and de-identified; data were analyzed using Microsoft Excel (Redmond, WA, USA) (2016). All responses were initially reviewed by a group of five study team members, which included the HOPE community partner. Qualitative data were analyzed within the cultural domains of interest: food preferences and behaviors. Responses were then listed by categories of main and side dishes. Using the constant-comparison method and group discussion, a common coding scheme was developed using the first five interviews, and codes were modified iteratively as needed [26]. Each transcript was then coded independently by two members of the team based on the coding scheme. Through an iterative process, the team regularly reviewed codes, identified emerging themes, and resolved discrepancies through consensus. Interviews continued until thematic saturation was reached. This study was deemed exempt from human subjects research by the Wake Forest University Health Sciences Institutional Review Board.
Results
Study Population Demographics
We conducted a total of 63 interviews at 12 HOPE sites within 3 different zip codes, predominately located in East and Southeast Winston-Salem. Of all participants, 68% (n = 43) were primarily English-speaking, and 32% (n = 20) were Spanish-speaking. Ninety percent (n = 57) of participants had children in the household. Fifty-seven percent (n = 36) of all respondents reported not being able to afford the type of food they enjoyed (Table 3).
Table 3.
Study population characteristics
| n = 63 | N (%) | |
|---|---|---|
| Preferred language | English | 43 (68%) |
| Spanish | 20 (32%) | |
| Children in the household | Yes | 57 (90%) |
| No | 6 (10%) | |
| Able to afford the types of food they enjoyed | Yes | 24 (38%) |
| No | 36 (57%) |
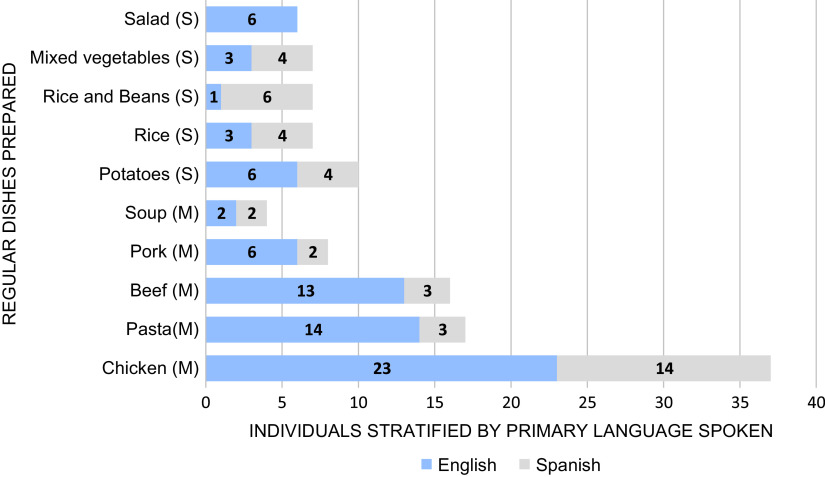
Families Preferred Chicken, Pasta, and Beef Dishes for Favorite Meals (Fig. 2)
Fig. 2.
Top five meal preferences of Spanish- and English-speaking households. M, main dish; S, side dish.
When asked to share their household’s favorite meal to cook at home, participants responded with main dishes consisting of chicken (n = 34), most often fried or baked, followed by pasta (n = 18), beef (n = 15), and pork (n = 5). Overall, the most popular side dishes were potatoes (n = 10), rice (n = 7), rice and beans (n = 7), mixed vegetables (n = 7), and salad (n = 6). Spanish-speaking participants preferred main dishes containing chicken (n = 14) (notably chicken mole), beef (n = 3), and pasta (n = 3), with a side dish of rice and beans (n = 6). Mole is a traditional Mexican sauce that is used for a variety of meat dishes including chicken, turkey, and enchiladas [27]. Similarly, English-speaking participants reported primarily eating chicken (n = 23), pasta (n = 14), and beef (n = 13), although the chicken was most commonly fried (n = 10) in this group. When asked about children’s favorite meals, adults mentioned chicken (n = 24), pasta (n = 14), and beef (n = 6). A popular answer among participants was that the children eat “everything” or “whatever is on their plates.”
Adults Preferred Vegetables While Children Favored Fruit
We asked participants about their preferences for produce (Fig. 3a–d). Adults reported favoring tomatoes (n = 30), onions (n = 27), and potatoes (n = 26). The least favorite produce were eggplants (n = 20), mushrooms (n = 17), and okra (n = 17). English-speaking participants preferred onions (n = 20), peppers (n = 17), tomatoes (n = 15), and potatoes (n = 15), while Spanish-speaking participants liked tomatoes (n = 15), potatoes (n = 11), strawberries (n = 10), and mentioned more fruit in general. Okra, eggplant, and mushrooms were similarly disliked by all. Overall, children enjoyed more fruit than adults, especially apples (n = 9), oranges (n = 9), and grapes (n = 8).
Fig. 3.
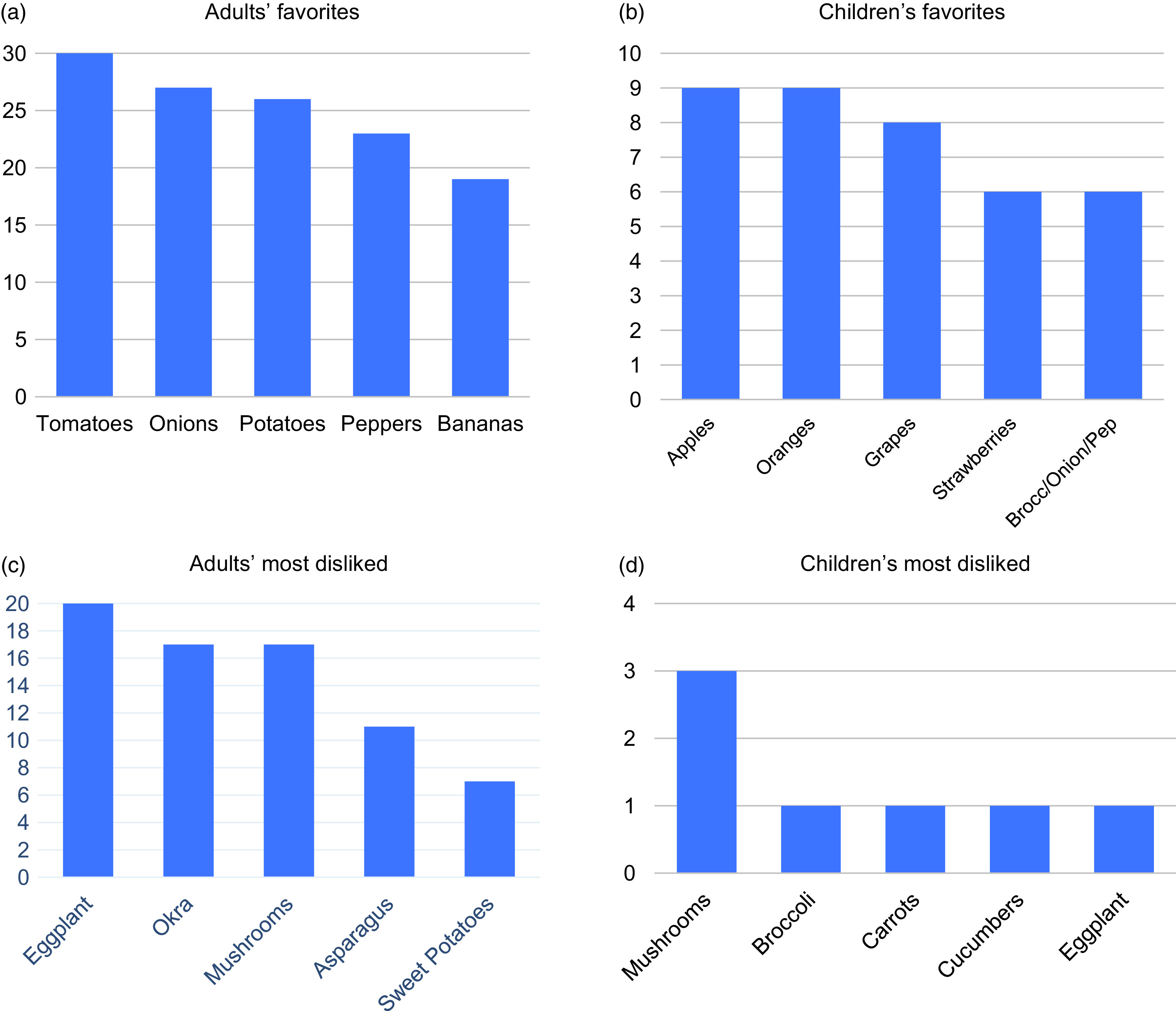
Most and least liked fresh produce preferences of participants interviewed. (N, number of respondents on y-axis, produce on x-axis). Answers stratified into adult and child preferences. Children’s preferences are primarily reported by adults. Note: Fig. 3(b) shows broccoli/onion/peppers as all preferred the same amount, consolidated in one bar.
Adults Primarily Used Stoves at Home and Were Not Interested in New Ways of Cooking
When asked which appliances were most used to prepare meals, participants mentioned: stove (n = 60), oven (n = 10), and microwave (n = 5). There were no differences in the methods used to cook between English- and Spanish-speaking participants. A few families stated that they did not own a microwave. Participants were asked if they would like to learn any new meals or recipes and many responded with “none” (n = 36), or “did not answer” (n = 2). Some specified with: “cook with less salt/oil,” “cook with fresh produce,” and “how to eat as a diabetic.” When asked about specific ways that participants wanted to cook differently, 95% (n = 60) answered with “not sure” (n = 1), “none” (n = 30), or “did not answer” (n = 29).
Discussion
In this study within a medium-sized southeastern city of 63 adults from diverse, low-income communities at high risk for FI, we found some dietary preferences in common: chicken, pasta, and beef were the most popular home-cooked dishes among adults and children alike. However, there were variations in preparation methods between English- and Spanish-speaking participants. Of all produce offered, adults enjoyed more vegetables, while reporting that children preferred more fruit. Lastly, families had little interest in learning new recipes or cooking methods at home and primarily used stoves.
Compared to individuals living in food-secure households, individuals living in food-insecure households have less healthy dietary patterns. Individuals in food-insecure households generally have a higher consumption of more palatable foods such as high-fat dairy and salty snacks, more red/processed meat, decreased frequency of fat-lowering behaviors, and less vegetable consumption [3, 7, 28, 29]. Our sample population had food preferences similar to what is described in the literature, with a high intake of calorie-dense foods and low consumption of vegetables. This could be because these foods, in comparison to fresh produce, may be cheaper, have longer shelf lives, provide more sustenance, and are easier to access within food deserts. Children have similar dietary patterns to adults in the same households, as seen in our study. Prior research has shown that children from food-insecure households have a higher likelihood of eating fast food, and can develop unhealthy eating patterns due to intermittent availability of food and increased stress levels [30–32]. While much of the food consumed was similar between English- and Spanish-speaking households, it was often prepared differently. Meat is typically held in high regard by many cultures, while other food items may have varying levels of significance [33]. It is important to understand the food preferences of particular groups of people, including culturally relevant foods (based on language, race/ethnicity, or religion, for example), so that community-based hunger relief programs, such as HOPE, can provide not only healthy, but culturally acceptable food.
Fresh produce preferences differed among adult and pediatric populations. We found that adults listed more vegetables, while children overwhelmingly liked fruit. This is consistent with literature showing that younger children rate fatty foods, sugary foods, and fruit the highest, and generally dislike vegetables [34, 35]. While the relationship of fruit and vegetable intake to weight has shown mixed results, various studies have shown an inverse association with intake and type II diabetes mellitus risk, visceral fat, liver fat, and insulin resistance in Hispanic/Latino children, thus making this a potentially important variable to evaluate in pediatric health [36, 37]. It has been shown that food preferences of parents, early introduction, and increased exposure of foods such as vegetables are important in increasing children’s preferences for such foods [38, 39]. Fruit and vegetable intake has also been directly correlated with its accessibility and availability at home, school, local markets, and the inclusion of children in cooking meals at home with their families [35, 40, 41]. In this manner, HOPE and other mobile meal programs may attempt to increase accessibility, availability, and visibility of fresh produce to encourage increased consumption by children and adults alike. Further research is needed to understand how community-based hunger relief programs can provide better access to fresh produce and encourage the intake of produce among food-insecure families.
One surprising finding in our study was that participants expressed little interest in learning new recipes or cooking methods. This may be due to financial constraints, time, and effort needed to learn to cook new recipes, and no guarantee that everyone in the household will eat a novel meal. In fact, one study showed that FI was associated with a lack of mealtime planning [42]. Other studies, such as Landers et al. [43], found that food-insecure families want to learn low-cost recipes such as soups based on canned stock or bouillon cubes, stir-fry, and one-dish skillet dinners that can be prepared in 30 min or less. Lack of supplies may also be a barrier to new methods of cooking, as literature has found that food-insecure households typically own fewer kitchen supplies than their food-secure counterparts [44]. The presence of food preparation supplies is associated with increased family meal frequency and child consumption of home-prepared dinners. Improving access to these supplies could be an important target in improving food-insecure families’ diets, as eating more family meals at home has been associated with the reduced caloric beverage and greater fruit and vegetable intake [45]. Literature shows that there may be areas of intervention such as teaching time-saving and cost-effective recipes, educating about meal planning, and providing more basic kitchen supplies to families. Further research is still needed to understand how families with limited budgets and time can eat healthier meals. Given the current literature and the results of our study, HOPE is encouraging local farmers to grow the produce that families reported they preferred and modifying the produce they provide to better address the needs of the families that utilize their services; furthermore, HOPE has made changes to the prepared meals in response to participant feedback such as ingredients in sandwiches and snacks. Additionally, a future development for HOPE is to begin offering cooking classes with recipes incorporating delivered produce that can generally be prepared within 30 min. Future studies and incentive programs could also consider distributing cooking utensils with related educational programming to encourage families to prepare more meals at home if they have successfully used the tools and successfully made a meal they enjoy.
There are several limitations to our study that should be acknowledged. First, although we tried to identify a diverse sample of adults from neighborhoods at high risk of FI, our small sample size may not be generalizable to other communities. Second, parents who agreed to participate in the study may not be representative of the populations in these neighborhoods due to selection bias. Third, because we were conducting interviews at the time participants were receiving services at HOPE, we limited the number of demographics collected for each participant to reduce the time of the interviews. We are unable to draw conclusions about differences in food preferences by demographics such as race/ethnicity. Lastly, due to stigma, we may have underestimated the risk of FI in participants when asking if they could afford the type of food they enjoyed, as they were asked verbally with other community members in proximity. Furthermore, we did not screen for FI using a validated instrument.
Conclusion
To more effectively address the unmet food needs of families at risk of FI who utilize community-based hunger relief programs, a greater understanding is needed regarding dietary and food preparation preferences. We found that families prefer similar meals, but may prepare them differently based on cultural practices among groups of people who speak English versus Spanish. Furthermore, there was little interest in learning new ways to prepare food. Taking into account that diverse, low-income communities often have limited resources, educational and food delivery interventions should be tailored to most effectively meet the needs of families.
Acknowledgments
Dr. Palakshappa is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number K23HL146902. Dr. Rachel Zimmer is supported by the Health Resources and Services Administration under Award Number K01HP33462. The funding sources did not have any role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the report; and in the decision to submit the article for publication. Portions of this study were presented at the 2020 Academic Pediatrics Association Region IV Meeting in Charlottesville, VA, USA. We would like to acknowledge the Wake Forest Clinical Translational Science Institute Program in Community Engagement and the Maya Angelou Center for Health Equity Integrated Special Populations Program, which is supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Award Number UL1TR001420. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
The authors have no conflicts of interest to declare.
References
- 1. Coleman-Jensen A, Rabbitt M, Gregory C, Singh A. Household Food Security in the United States in 2018. USDA, 2019.
- 2. Kreider B, Pepper J, Gundersen C. The economics of food insecurity in the United States. Applied Economic Perspective and Policy 2011; 33(3): 281–303. [Google Scholar]
- 3. Mello JA, Gans KM, Risica PM, Kirtania U, Strolla LO, Fournier L. How is food insecurity associated with dietary behaviors? An analysis with low-income, ethnically diverse participants in a nutrition intervention study. Journal of the American Dietetic Association 2010; 110(12): 1906–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Feeding America. Food insecurity in North Carolina, 2019.. (https://map.feedingamerica.org/county/2017/overall/north-carolina)
- 5. Seligman H, Larana B, Kushel M. Food insecurity is associated with chronic disease among low-income NHANES participants. Journal of Nutrition 2010; 140(2): 304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Berkowitz SA, Gao X, Tucker KL. Food-insecure dietary patterns are associated with poor longitudinal glycemic control in diabetes: results from the Boston Puerto Rican study. Diabetes Care 2014; 37(9): 2587–2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. American Journal of Clinical Nutrition 2014; 100(2): 684–692. [DOI] [PubMed] [Google Scholar]
- 8. Billimek J, Sorkin D. Food insecurity, processes of care, and self-reported medication underuse in patients with type 2 diabetes: results from the California health interview survey. Health Services Research 2012; 47(6): 2159–2168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huang J, Barnidge E. Low-income children’s participation in the national school lunch program and household food insufficiency. Social Science & Medicine 2016; 150: 8–14. [DOI] [PubMed] [Google Scholar]
- 10. Nalty CC, Sharkey JR, Dean WR. School-based nutrition programs are associated with reduced child food insecurity over time among Mexican-origin mother-child dyads in Texas Border Colonias. Journal of Nutrition 2013; 143(5): 708–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bartfeld JS, Ahn HM. The school breakfast program strengthens household food security among low-income households with elementary school children. Journal of Nutrition 2011; 141(3): 470–475. [DOI] [PubMed] [Google Scholar]
- 12. Nord M. How much does the supplemental nutrition assistance program alleviate food insecurity? Evidence from recent programme leavers. Public Health Nutrition 2012; 15(5): 811–817. [DOI] [PubMed] [Google Scholar]
- 13. Mabli J, Worthington J. Supplemental nutrition assistance program participation and child food security. Pediatrics 2014; 133(4): 610–619. [DOI] [PubMed] [Google Scholar]
- 14. Black MM, et al. WIC participation and attenuation of stress-related child health risks of household food insecurity and caregiver depressive symptoms. Archives of Pediatrics & Adolescent Medicine 2012; 166(5): 444–451. [DOI] [PubMed] [Google Scholar]
- 15. Metallinos-Katsaras E, Gorman KS, Wilde P, Kallio J. A longitudinal study of WIC participation on household food insecurity. Maternal and Child Health Journal 2011; 15(5): 627–633. [DOI] [PubMed] [Google Scholar]
- 16. Bruce JS, De La Cruz MM, Lundberg K, Vesom N, Aguayo J, Merrell SB. Combating child summer food insecurity: examination of a community-based mobile meal program. Journal of Community Health 2019; 44(5): 1009–1018. [DOI] [PubMed] [Google Scholar]
- 17. Simmet A, Depa J, Tinnemann P, Stroebele-Benschop N. The nutritional quality of food provided from food pantries: a systematic review of existing literature. Journal of the Academy of Nutrition and Dietetics 2017; 117(4): 577–588. [DOI] [PubMed] [Google Scholar]
- 18. Campbell E, Hudson H, Webb K, Crawford P. Food preferences of users of the emergency food system. Journal of Hunger & Environmental Nutrition 2011; 6(2): 179–187. [Google Scholar]
- 19. Greenwald HP, Zajfen V. Food insecurity and food resource utilization in an urban immigrant communtiy. Journal of Immigrant and Minority Health 2015; 19: 179–186. doi: 10.1007/s10903-015-0331-9. [DOI] [PubMed] [Google Scholar]
- 20. McCloskey DJ, et al. Principles of Community Engagement. Agency for Toxic Substances and Disease Registry, 2011. NIH Publication No. 11-7782. (https://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf)
- 21. United States Census Bureau. QuickFacts. U.S. Department of Commerce. 2019.. (https://www.census.gov/quickfacts/fact/table/kernersvilletownnorthcarolina,walkertowntownnorthcarolina,winstonsalemcitynorthcarolina/PST04521920)
- 22. NEMAC. Western North Carolina Vitality Index: Food Deserts, 2016.. (http://www.wncvitalityindex.org/food-security/food-deserts)
- 23. USDA. Food Access Research Atlas, 2019.. (https://www.ers.usda.gov/data-products/food-access-research-atlas/go-to-the-atlas.aspx)
- 24. Bernard HR, Gravlee CC. Handbook of Methods in Cultural Anthropology (pp 347–369). Lanham, MD: Rowman & Littlefield, 2015. [Google Scholar]
- 25. Weller SC, Romney AK. Systematic Data Collection (pp 9–16). Newbury Park, CA: Sage Publications, 1988. [Google Scholar]
- 26. Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Quality and Quantity 2002; 36(4): 391–409. [Google Scholar]
- 27. Fabricant F. Fare of the county; blending the flavors of Mexican history. New York Times, p. 16, 1982. (https://www.nytimes.com/1982/03/28/travel/fare-of-the-county-blending-the-flavors-of-mexican-history.html?emc=eta1)
- 28. Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. Journal of the Academy of Nutrition and Dietetics 2014; 114(12): 1943–1953. [DOI] [PubMed] [Google Scholar]
- 29. Kirkpatrick SI, Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. Journal of Nutrition 2008; 138(3): 604–612. [DOI] [PubMed] [Google Scholar]
- 30. Widome R, Neumark-Sztainer D, Hannan PJ, Haines J, Story M. Eating when there is not enough to eat: eating behaviors and perceptions of food among food-insecure youths. American Journal of Public Health 2009; 99(5): 822–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mark S, Lambert M, O’Loughlin J, Gray-Donald K. Household income, food insecurity, and nutrition in Canadian youth. Revue Canadienne de Sante Publique 2012; 103(2): 94–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Institute of Medicine (US). Hunger and Obesity: Understanding a Food Insecurity Paradigm: Workshop Summary. Washington, DC: National Academies Press, 2011. [PubMed] [Google Scholar]
- 33. Allen MW, Baines S. Manipulating the symbolic meaning of meat to encourage greater acceptance of fruits and vegetables and less proclivity for red and white meat. Appetite. 2002; 38(2): 118–130. [DOI] [PubMed] [Google Scholar]
- 34. Cooke LJ, Wardle J. Age and gender differences in children’s food preferences. British Journal of Nutrition 2005; 93(5): 741–746. [DOI] [PubMed] [Google Scholar]
- 35. Edwards JS, Hartwell HH. Fruit and vegetables—attitudes and knowledge of primary school children. Journal of Human Nutrition and Dietetics 2002; 15(5): 365–374. [DOI] [PubMed] [Google Scholar]
- 36. Cooper AJ, et al. A prospective study of the association between quantity and variety of fruit and vegetable intake and incident type 2 diabetes. Diabetes Care 2012; 35(6): 1293–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cook LT, O’Reilly GA, Goran M, Weigensberg MJ, Sprutijit-Metz D, Davis JN. Vegetable consumption is linked to decreased visceral and liver fat and improved insulin resistance in overweight Latino youth. Journal of the Academy of Nutrition and Dietetics 2014; 114(11): 1776–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Skinner JD, Carruth BR, Bounds W, Ziegler PJ. Children’s food preferences: a longitudinal analysis. Journal of the American Dietetic Association 2002; 102(11): 1638–1647, [DOI] [PubMed] [Google Scholar]
- 39. Fildes AF, van Jaarsveld C, Wardle J, Cooke L. Parent-administered exposure to increase children’s vegetable acceptance: a randomized controlled trial. Journal of the Academy of Nutrition and Dietetics 2014; 114(6): 881–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chu YL, Storey KE, Veugelers PJ. Involvement in meal preparation at home is associated with better diet quality among Canadian children. Journal of Nutrition Education and Behavior 2014; 46(40): 304–308. [DOI] [PubMed] [Google Scholar]
- 41. Bere E, Klepp K. Changes in accessibility and preferences predict children’s future fruit and vegetable intake. International Journal of Behavioral Nutrition and Physical Activity 2005; 2: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Fiese BH, Gundersen C, Koester B, Jones B. Family chaos and lack of mealtime planning is associated with food insecurity in low income households. Economics and Human Biology 2016; 21: 147–155. [DOI] [PubMed] [Google Scholar]
- 43. Landers P, Shults C. Pots, pan and kitchen equipment: do low-income clients have adequate tools for cooking? Journal of Extension 2008; 46(1): 1RIB4. [Google Scholar]
- 44. Oakley AR, Nikolaus CJ, Ellison B, Nichols-Richardon SM. Food insecurity and food preparation equipment in US households: exploratory results from a cross-sectional questionnaire. Journal of Human Nutrition and Dietetics 2019; 32(2): 143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Appelhans B, Waring M, Schneider K, Pagoto S. Food preparation supplies predict children’s family meal and home-prepared dinner consumption in low-income households. Appetite 2014; 76: 1–8. [DOI] [PubMed] [Google Scholar]