Abstract
‘Post-acute coronavirus disease 2019 (COVID-19) syndrome’ is a new term that was coined to describe a constellation of persistent symptoms and new complications following recovery from COVID-19 initial illness. Identifying post-COVID-19 complications is crucial for early diagnosis and subsequent initiation of therapies to ensure more favorable outcomes. Severe COVID-19-related hemophagocytic lymphohistiocytosis (HLH) has been previously described during the acute phase of the infection. It is characterized by hyperinflammation, multi-organ involvement, and hemophagocytosis. We report the case of a 69-year-old woman who presented, two weeks after recovery from COVID-19, with hyperosmolar state and high inflammatory markers. Bone marrow aspirate, flow cytometry, extensive viral panel and total body scan were performed. Review of bone marrow aspirate smear showed hemophagocytosis. Flow cytometry, viral panel, and total body scan were normal. The diagnosis of post COVID-19-related HLH was made. Unfortunately, the patient died despite adequate treatment. To our knowledge, this is the first case establishing a high probability of COVID-19-related HLH given its occurrence two weeks following a documented biological and clinical recovery. Awareness and early recognition of HLH features following COVID-19 recovery should prompt timely initiation of therapy.
Keywords: COVID-19, SARS-CoV-2, Hemophagocytic lymphohistiocytosis, Post-acute Covid-19 syndrome, Hyperinflammatory syndrome, Late onset
Introduction
Immune activation accompanied by high levels of inflammatory cytokines has been frequently described in severe coronavirus disease 2019 (COVID-19) infection [1]. Hemophagocytic lymphohistiocytosis (HLH), characterized by hyperinflammation, multi-organ involvement and hemophagocytosis, has been reported during the acute phase of COVID-19 infection [2]. Here, we report a case of fatal HLH two weeks following recovery from COVID-19 infection.
Case report
A 69-year-old woman with non-insulin dependent diabetes mellitus, hypertension, dyslipidemia, and recent recovery from COVID-19 infection was brought to the emergency department for a five-day worsening altered mental status and anorexia with decreased food intake. She had been diagnosed with COVID-19 three weeks prior to this presentation and required hospitalization for one week. At the time, her nonenhanced chest CT showed ground-glass opacities with superimposed septal thickening in the left lower and middle lobes. She was treated with a methylprednisone course and low molecular weight heparin and was discharged home on prednisone taper after biological and clinical recovery. C-reactive protein (CRP) and procalcitonin were elevated during her acute illness but normalized upon discharge. SARS-CoV-2 antigen polymerase chain reaction (PCR) tests were performed at 6 days (8 days after discharge) and at 2 days (12 days after discharge) prior to her current presentation. Both were negative and were not repeated upon admission. Her diabetes was controlled with metformin/empagliflozin in addition to gliclazide. Her other medications included bisoprolol, amlodipine/telmisartan, atorvastatin, and fenofibrate.
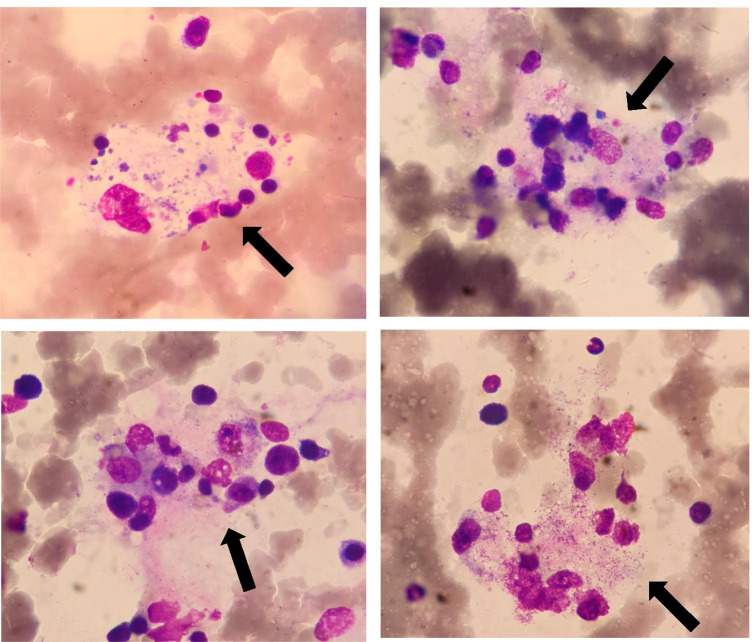
On admission, the patient’s vitals were: blood pressure of 130/60, heart rate at 124 bpm, respiratory rate of 18, oxygen saturation of 98%, and point of care glucose of 570 mg/dL. On physical exam, she had altered mental status, appeared dry with sunken eyes, dry mucosa, was cachectic and had an oral thrush. Table 1 indicates the main laboratory results for the first 4 days of admission. Her arterial blood gas showed metabolic acidosis with compensatory respiratory alkalosis. She was diagnosed with hyperosmolar hyperglycemic nonketotic syndrome. A CT-scan with contrast (chest, abdomen, and pelvis) was performed to identify a potential infectious source and was normal except for the presence of pulmonary sequelae thought to be related to COVID-19. Her urine and blood cultures were negative. She received 3 l of intravenous 0.9% normal saline and was started on insulin drip. The following day, her mental status improved, but she developed fever at 39 °C and was started on broad spectrum antibacterial and antifungal coverage with imipenem/cilastatin, teicoplanin and fluconazole. On day 2, as indicated in Table 1, her WBC count dropped significantly and her transaminases rose. She had an elevated ferritin of 10,510 ng/ml, LDH of 1927 u/l, fibrinogen of 4.54 g/l, D-dimers of 5.03 ug/ml, IL-6 of 104.6 pg/ml, CRP of 174 mg/dl, ESR of 91 mm and triglyceride of 2.85 mmol/. Positive direct Coombs 1 + and negative indirect Coombs with reticulocyte count of 18,528 mm3. Peripheral blood smear showed anisopoikilocytosis, elliptocytosis, schistocyte 0.5%, macrothrombocytosis and leukopenia. Given the concern for a central bone marrow process, a bone marrow aspiration was performed (see Fig. 1) showing prominent phagocytosis of hematopoietic elements. Flow cytometry showed absence of abnormal cells. Viral serology panel including EBV, CMV, HIV, PB19, HBV, and HCV was negative except for SARS-CoV-2 antibodies: IgM = 4.02 A.U/ml (< 1.1 A.U/ml) and IgG = 5.9 A.U/ml (< 1.1 A.U/ml). A purified protein derivative (PPD) skin test was negative. Subsequently, the diagnosis of HLH syndrome post-COVID-19 was made. She was started on dexamethasone 40 mg and etoposide 170 mg. On day 5, ferritin levels rose to 17,550 ng/ml while CRP, LDH, fibrinogen, and D-dimers decreased to 47 mg/l, 1369 u/l, 2.98 g/l, and 4.62 ug/ml, respectively. On day 6, her platelet count dropped significantly to 19,000/mm3. The patient’s mental status deteriorated along with the development of new right-sided hemiparesis and subsequent rapid loss of consciousness with anisocoria on exam. An intracranial bleed was suspected. The patient expired following cardiovascular arrest. An autopsy was not performed.
Table 1.
Main laboratory tests during the first five days of hospitalization
| Unit | Normal range | At arrival | D1 | D2 | D3 | D4 | |
|---|---|---|---|---|---|---|---|
| Hemoglobin | g/dl | 12–16 | 12.3 | 11.3 | 11.3 | 10.4 | 10.8 |
| White blood cells | 10*9/L | 4–9 | 4.7 | 1.8 | 0.6 | 0.7 | 2.4 |
| Neutrophils | % | 50–78 | 86.7 | 76.9 | 0 | 0 | 85 |
| Eosinophils | % | < 11 | 1.1 | 1.8 | 0 | 0 | 0 |
| Basophils | % | < 3 | 0.5 | 0.6 | 0 | 0 | 0 |
| Lymphocytes | % | 20–45 | 6 | 17.2 | 0 | 0 | 10 |
| Monocytes | % | < 10 | 5.7 | 3.5 | 0 | 0 | 5 |
| Platelets | 10*9/L | 150–400 | 162 | 130 | 94 | 95 | 104 |
| Urea | mmol/L | 2.5–7.5 | 15.5 | 13.2 | 8.4 | 7.2 | 7.6 |
| Creatinine | umol/L | 46–92 | 135 | 105 | 101 | 84 | 81 |
| Alanin transaminase (ALT) | u/L | < 35 | 261 | 385 | 679 | 571 | |
| Aspartate transaminase (AST) | u/L | 14–36 | 432 | 991 | 1760 | 1044 | |
| Blood osmolarity | mosmol/kg | 280–300 | 334 | ||||
| Lactate | mmol/L | 0.7–2.1 | 1 | ||||
| Blood ketones | 1 + | ||||||
| Troponin T | ng/L | < 14 | 26 | 27 | |||
| Interleukin-6 | pg/mL | 0–7 | 105 | ||||
| Triglyceride | mmol/L | < 1.69 | 2.85 | ||||
| Ferritin | ng/mL | 13–150 | 10,510 | 17,550 | |||
| Reticulocytes | 10*3 mm3 | 20–120 | 18.5 | ||||
| LDH | u/L | 120–246 | 1927 | 1369 | |||
| Fibrinogen | g/L | 2–4 | 4.54 | 2.98 | |||
| D-dimers | ug/mL | < 0.5 | 5.03 | 4.62 | |||
| CPK | u/L | 30–135 | 60 | ||||
| Procalcitonin | ug/L | < 0.1 | 1.1 | 0.18 | |||
| CRP | mg/L | < 3.5 | 174 | 47 | |||
| ESR | mm | 0–15 | 91 | ||||
| INR | 1.12 | ||||||
| aPTT | 28–36 | 32 |
Fig. 1.
Hematoxylin and eosin stain was used to examine the bone marrow aspirate sample. Prominent phagocytosis of hematopoietic elements (black arrows) with an increased number of activated macrophages is shown in the bone marrow, 1000 ×
Materials and methods
Bone marrow aspiration was performed and examination of the aspirates with hematoxylin–eosin staining under optical microscopy with 1000 × magnification. Flow cytometric immunophenotyping of CD-5, CD-7, CD-14, CD-19, CD-22, CD-33, and CD-34 was conducted on the bone marrow aspirate.
Results
Bone marrow smear was normal for the patient’s age and showed sufficient cell count without increase in lymphocytes or plasma cells, normal megakaryocytes, and no maturation cell arrest nor cell dysplasia. However, several images of hemophagocytosis were seen suggesting the diagnosis of hemophagocytic lymphohistiocytosis (see Fig. 1). Flow cytometric immunophenotyping showed no clonal expansion abnormalities.
Discussion
HLH is a life-threatening syndrome seen more frequently in infants than in children and adults [3]. HLH is characterized by hyperinflammation, multi-organ involvement, fever, and hemophagocytosis [4]. Persistent activation of macrophages, natural killers cells (NK), and cytotoxic T lymphocyte (CTLs) are the main causes of immune system dysregulation in HLH [5]. Two types of HLH have been described: primary and secondary. The primary (familial) type, occurring mostly in children, is caused by genetic defects of cytolytic pathways proteins whereas the secondary (acquired) type occurs particularly in adults and is mostly due to malignancies, infections, and autoimmune disorders. The most commonly described triggers are viral infections including Epstein–Barr virus (EBV), hepatitis A, B, and C, parvovirus B19, human immunodeficiency virus (HIV), adenovirus, and enterovirus [6, 7]. More recently, COVID-19 was identified as a trigger of HLH-like syndrome [1, 8]. During SARS-CoV-2 infection, the pathogenesis of hyperinflammation is believed to result from macrophage activation and modulation [9]. The probability of having HLH can be estimated by calculating the H-score that is based on nine criteria: presence of underlying immunosuppression, high temperature, hepatosplenomegaly, cytopenia, hypertriglyceridemia, hyperferritinemia, elevated AST, hypofibrinogenemia, and hemophagocytosis on bone marrow aspirates [10]. Our patient had a score of 205 on day 2 of her admission, corresponding to a very high probability of having the disease (88–93%).
Diagnostic criteria of HLH are based on the HLH-2004 study and include: fever > 38.5 °C, splenomegaly, cytopenia, hypertriglyceridemia > 265 mg/dl and/or hypofibrinogenemia < 150 mg/dl, hemophagocytosis in bone marrow, spleen, lymph node or liver, low or absent NK cell activity, ferritin > 500 ng/ml and elevated soluble CD25 (> 2SD). Five of eight criteria must be fulfilled to establish the diagnosis [11]. Our patient fulfilled four criteria: fever, cytopenia, hypofibrinogenemia, and hemophagocytosis. NK cell activity and soluble CD25 are not routinely performed in our local laboratory and could not be obtained. The patient’s triglyceride levels were below the diagnostic cut-off and this might be attributed to her being on both statin and fibrate. The absence of hepatosplenomegaly was reported in 85% of cases of HLH secondary to COVID-19 infection, suggesting that hepatosplenomegaly is less common in COVID-19-related HLH than in other HLH [2], which was the case of our patient. No autoimmune disease was identified in our patient and an extensive virus panel was negative except for SARS-CoV-2 antibodies. No obvious malignancy was detected on the total body scan nor on the bone marrow flow cytometry. By exclusion, these findings suggested a role of COVID-19 in HLH occurrence in this patient despite its event two weeks after COVID-19 recovery and two negative PCR tests. A latent and persistent subclinical inflammatory state secondary to COVID-19 virus could have led to this presentation.
Prilutskiy et al. have reported four cases of HLH associated with SARS-CoV-2 in patients whose clinical courses were dominated by acute respiratory distress syndrome and cytokine storm. Hyperferritinemia, hypertriglyceridemia, and high-grade fever were the most useful clinical parameters to identify HLH among their COVID-19 autopsy cohort [12]. Moreover, other published case reports postulated a hyperinflammatory state induced by COVID-19 with development of HLH during the acute phase of the infection [13–16]. Harris et al. identified a high incidence of lymphopenia, neutrophilic leukocytosis, and hemophagocytosis upon bone marrow examination on autopsy of expired patients with COVID-19 [17]. All these findings described in the literature support the burgeoning theory of COVID-19-related HLH. Recent studies showed that COVID-19 patients continued to have symptoms and complications related to COVID-19 even past the acute phase. Terms used to describe this phase included ‘long term COVID’, ‘post-COVID syndrome’, and ‘post-acute COVID-19 syndrome’ [18]. Most commonly described symptoms included fatigue, shortness of breath, cough, joint pain, chest pain, muscle pain, headache, fast or pounding heartbeat, loss of smell and/or taste, and memory problems. In addition to these symptoms, impairment of different organs has been described past the acute phase: myocarditis resulting from myocardial injury, pulmonary fibrosis from long-standing damage to the alveoli, increased thromboembolic risk with liver and kidney dysfunction from blood vessel injury, and a possible increase in the risk of developing Parkinson’s and Alzheimer’s disease [19]. A recently published cohort study from the USA showed that 27% of discharged COVID-19 patients were either readmitted or died by 60 days after discharge. Persistent COVID-19, sepsis, pneumonia, and heart failure were the most common causes of readmission [20]. Our case is unique and the first to describe HLH as a possible cause of death in “post-acute COVID-19 syndrome” phase.
Conclusion
Although more patients have been surviving after severe SARS-CoV-2 infection, data on outcomes after initial hospitalization are still limited. To our knowledge, this is the first case describing a high probability of HLH two weeks following COVID-19 biological and clinical recovery. In conclusion, awareness and early recognition of HLH features following COVID-19 recovery should prompt timely initiation of therapy. HLH can be an underreported cause of death during ‘post-acute COVID-19 syndrome’.
Acknowledgements
We would like to thank Prof. Philippe DeMoerloose and Dr Najib Nassani for helping us in reviewing and finalizing the manuscript.
Author contribution
All authors contributed to the writing and revision of the manuscript. EN, BMN and RM were responsible for the final version of the manuscript. All authors read and approved the final manuscript.
Data availability
Not applicable.
Code availability
Not applicable.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Saint Joseph University in Beirut. Informed consent was obtained from the relative (son) of the patient included in the study.
Consent for publication
Written informed consent for publication of clinical details was obtained from the relative (son) of the patient. A copy of the consent form is available for review by the Editor of this journal.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet Lond Engl. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Retamozo S, Brito-Zerón P, Sisó-Almirall A, Flores-Chávez A, Soto-Cárdenas M-J, Ramos-Casals M. Haemophagocytic syndrome and COVID-19. Clin Rheumatol. 2021 [cited 2021 Feb 5]; Available from: http://link.springer.com/10.1007/s10067-020-05569-4 [DOI] [PMC free article] [PubMed]
- 3.Filipovich A, McClain K, Grom A. Histiocytic disorders: recent insights into pathophysiology and practical guidelines. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant. 2010;16:S82–89. doi: 10.1016/j.bbmt.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 4.Lin C-I, Yu H-H, Lee J-H, Wang L-C, Lin Y-T, Yang Y-H, et al. Clinical analysis of macrophage activation syndrome in pediatric patients with autoimmune diseases. Clin Rheumatol. 2012;31:1223–1230. doi: 10.1007/s10067-012-1998-0. [DOI] [PubMed] [Google Scholar]
- 5.Al-Samkari H, Berliner N. Hemophagocytic lymphohistiocytosis. Annu Rev Pathol. 2018;13:27–49. doi: 10.1146/annurev-pathol-020117-043625. [DOI] [PubMed] [Google Scholar]
- 6.Ramos-Casals M, Brito-Zerón P, López-Guillermo A, Khamashta MA, Bosch X. Adult haemophagocytic syndrome. Lancet Lond Engl. 2014;383:1503–1516. doi: 10.1016/S0140-6736(13)61048-X. [DOI] [PubMed] [Google Scholar]
- 7.Tiab M, Mechinaud F, Harousseau JL. Haemophagocytic syndrome associated with infections. Baillieres Best Pract Res Clin Haematol. 2000;13:163–178. doi: 10.1053/beha.2000.0066. [DOI] [PubMed] [Google Scholar]
- 8.Ombrello MJ, Schulert GS. COVID-19 and cytokine storm syndrome: are there lessons from macrophage activation syndrome? Transl Res. 2021 [cited 2021 Apr 5]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7934701/ [DOI] [PMC free article] [PubMed]
- 9.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20:355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D, et al. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol Hoboken NJ. 2014;66:2613–2620. doi: 10.1002/art.38690. [DOI] [PubMed] [Google Scholar]
- 11.Henter J-I, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 12.Prilutskiy A, Kritselis M, Shevtsov A, Yambayev I, Vadlamudi C, Zhao Q, et al. SARS-CoV-2 Infection-associated hemophagocytic lymphohistiocytosis. Am J Clin Pathol. 2020;154:466–474. doi: 10.1093/ajcp/aqaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von der Thüsen JH, van Bommel J, Kros JM, Verdijk RM, Lopuhaä B, Lam KH, Dik WA, Miedema JR (2020) Case report: a fatal combination of hemophagocytic lymphohistiocytosis with extensive pulmonary microvascular damage in COVID-19 pneumonia. J Hematop 1–5. 10.1007/s12308-020-00423-7 [DOI] [PMC free article] [PubMed]
- 14.Lima R, Filho CC, Ferreira Filho CM, Vaisman M, Cossenza A, Rebello CP, et al. Hemophagocytic syndrome and COVID-19. Respir Med Case Rep. 2020;31:101162. doi: 10.1016/j.rmcr.2020.101162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tholin B, Hauge MT, Aukrust P, Fehrle L, Tvedt TH. Hemophagocytic lymphohistiocytosis in a patient with COVID-19 treated with tocilizumab: a case report. J Med Case Rep. 2020;14:187. doi: 10.1186/s13256-020-02503-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schnaubelt S, Tihanyi D, Strassl R, Schmidt R, Anders S, Laggner AN, et al. Hemophagocytic lymphohistiocytosis in COVID-19: case reports of a stepwise approach. Medicine (Baltimore) 2021;100:e25170. doi: 10.1097/MD.0000000000025170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris CK, Hung YP, Nielsen GP, Stone JR, Ferry JA (2021) Bone marrow and peripheral blood findings in patients infected by SARS-CoV-2. Am J Clin Pathol. 10.1093/ajcp/aqaa274 [DOI] [PMC free article] [PubMed]
- 18.Post COVID/Long COVID. [cited 2021 Feb 5]. Available from: https://www.idsociety.org/covid-19-real-time-learning-network/disease-manifestations--complications/post-covid-syndrome/
- 19.COVID-19 (coronavirus): Long-term effects - Mayo Clinic. [cited 2021 Feb 5]. Available from: https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-long-term-effects/art-20490351
- 20.Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA. 2021;325:304. doi: 10.1001/jama.2020.21465. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.