Abstract
Background
Out-of-hospital cardiac arrest (OHCA) accounts for a substantial proportion of sudden cardiac events globally, with hundreds of thousands of cases reported annually in the United States. The mortality rate of patients who suffer OHCA remains high despite extensive utilization of resources.
Objectives
We aim to describe the current landscape of OHCA during the COVID-19 pandemic and provide an overview of the logistical challenges and resuscitation protocols amongst emergency medical service (EMS) personnel.
Discussion
Recent studies in Italy, New York City, and France characterized a significant increase in OHCA incidence in conjunction with the arrival of the 2019 coronavirus disease (COVID-19) pandemic. The presence of the pandemic challenged existing protocols for field resuscitation of cardiac arrest patients as the pandemic necessitated prioritization of EMS personnel and other healthcare providers' safety through stringent personal protective equipment (PPE) requirements. Studies also characterized difficulties encountered by the first responder system during COVID-19, such as dispatcher overload, increased response times, and adherence to PPE requirements, superimposed on PPE shortages. The lack of guidance by governmental agencies and specialty organizations to provide unified safety protocols for resuscitation led to the development of different resuscitative protocols globally.
Conclusions
The ongoing COVID-19 pandemic modified the approach of first responders to OHCA. With the rise in OCHA during the pandemic in several geographic regions and the risks of disease transmission with superimposed equipment shortages, novel noninvasive, adjunct tools, such as point of care ultrasound, warrant consideration. Further prehospital studies should be considered to optimize OHCA and resource management while minimizing risk to personnel.
Keywords: OHCA, Out-of-hospital cardiac arrest, COVID-19, Cardiopulmonary resuscitation, POCUS
1. Introduction
Out-of-hospital cardiac arrest (OHCA) is defined as a cessation of cardiac mechanical activity occurring outside of the hospital setting, confirmed by absence of signs of circulation [1]. Approximately 326,000 OHCA events occur per year in the United States, making sudden cardiac arrests (SCAs) one of the leading causes of death [2]. OHCA is also common internationally, though incidence varies according to region [3]. In the last year, there has been a rise in OHCA, postulated to be connected to COVID-19 related-illness, the inability of patients to seek care for preventative care or general medical illness, and a reluctance to seek care because of COVID transmission in the hospital setting [[4], [5], [6], [7]]. The risk of transmission of the SARS-CoV-2 virus to first responders performing cardiopulmonary resuscitation (CPR) creates a dilemma in how best to manage CPR in the pandemic. In addition to standard resuscitative maneuvers, emergency medical service personnel (EMS) perform endotracheal intubation, an aerosol generating procedure capable of transmitting viral particles [8]. We aim to provide a narrative review describing the changes in OHCA characteristics in several areas associated with the pandemic and review the logistical challenges and exposure risks to first responders managing prehospital sudden cardiac events during COVID-19. We also review the use of point of care ultrasound (POCUS) as a noninvasive tool to evaluate cardiac arrest and propose its use as a diagnostic tool in OCHA as a way to diminish COVID exposure to prehospital personnel.
2. Methods
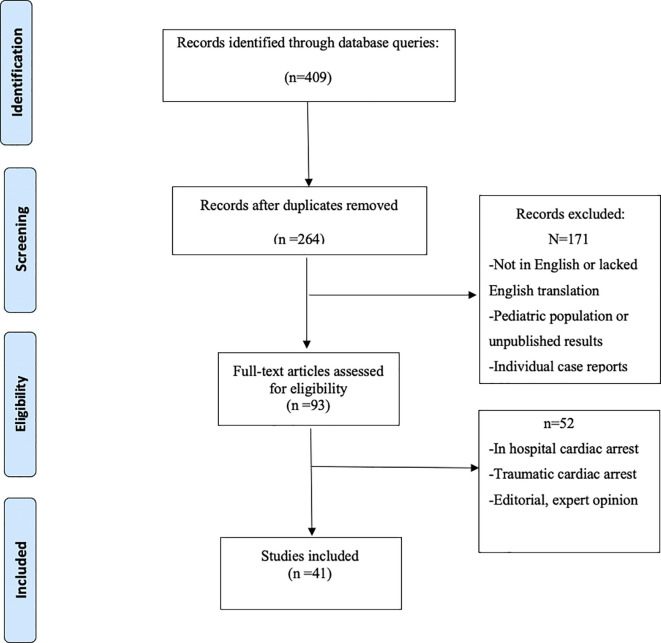
Searches using PubMed, Google Scholar, medRxiv, and SCOPUS for articles using a combination of the keywords “COVID-19,” “SARS-CoV-2,” and “OHCA”, “out-of-hospital cardiac arrest”, “cardiopulmonary resuscitation”, “CPR”, “emergency medical services”, and “bystander CPR” were performed. Studies comprised systematic reviews, case reports, case-studies, observational studies, retrospective and prospective studies, letters, perspectives, commentaries, and clinical guidelines. References of all included studies were also reviewed to identify additional sources. Only studies in English (including translated studies) were included. The initial literature search identified 409 articles, of which 145 were deemed duplicates across the search systems. Of the remaining 93 pieces, 52 articles were focused on traumatic cardiac arrest, in-hospital cardiac arrest, editorial, expert opinion or reported preliminary results. This produced a total of 41 articles included in our final review. Key points from these articles were identified and organized according to changes in OHCA incidence, impacts of emergency medical service response to OHCA events. A summary of the search algorithm is available in Fig. 1 .
Fig. 1.
Study query, inclusion, and exclusion criteria.
3. Results
3.1. Incidence of out-of hospital cardiac arrests during COVID-19
There is not one specific trend in OHCA that could be associated with the COVID-19 pandemic. Several studies showed an increase in OHCA, while other studies reported a drop or no changes in OCHA incidence (Table 1 ).
Table 1.
Change in Incidence of out-of hospital cardiac arrest events during COVID-19.
| City or region | Reported change in OHCA incidencea | Studied time interval | Statistically significant? | Source |
|---|---|---|---|---|
| Lombardy, Italy | +52% (Regional mean) +169%, Lodi +106%, Cremona +31%, Pavia +12%, Mantova |
February 21, 2020–April 20, 2020 | Yes | [4] |
| New York City, USA | +199% | March 1, 2020–April 25, 2020 | Yes | [5] |
| New York City, USA | +223% | March 20, 2020–April 22, 2020 | Yes | [6] |
| Paris, France | +99%b | March 16, 2020–April 26, 2020 | Yes | [7] |
| Padua, Italy | -2.9% | March 1, 2020–April 30, 2020 | No | [10] |
| King County, Washington, USA | -0.3% | January 1, 2020–April 15, 2020 | No | [11] |
| Munich, Germany | -6.9% | January 1, 2020–August 31, 2020 | No | [12] |
| Western Pennsylvania, USA | -1.8%c | March 1, 2020–May 25, 2020 | No | [13] |
Standard of comparison is 2019 OHCA incidence in a given region, unless otherwise noted.
Standard of comparison was mean OHCA incidence in Paris, France during 3–16–4-26 from 2012 to 2019.
Standard of comparison was mean OHCA incidence from January 2016 to February 2020.
Lombardy, Italy, New York City, USA, and Paris, France, are areas that saw large increases in COVID-19 transmission early in the pandemic. These areas also demonstrated an increased incidence of OHCA during their respective peak COVID periods, when compared to similar time frames in previous years [[4], [5], [6]]. In the Northern Italian region of Lombardy, a 52% increase in OHCA incidence was observed in the two month period following its first recorded COVID-19 case (February 21th to April 20th) compared to the same time frame in 2019 [4]. The OHCA curve in this region closely mirrored the COVID pandemic curve, with a high percentage of OHCA patients either having confirmed COVID or a COVID-like illness. Likewise in New York City, from March 1st to April 25th, the incidence rate of OHCA within city limits tripled from the same time interval in 2019 [5]. Of the excess OHCA events in this time period, 90% resulted in out-of-hospital deaths. A similar study by Mountantonakis et al. in New York City from March 20th to April 22th also reported an increase in OHCA events of 223% from 2019 [6]. Authors hypothesized that the observed increases were multifactorial, with challenges in accessing and seeking care as possible root causes. An observational study in Paris, France showed a doubling in the incidence of OHCAs from March 16th to April 26th when compared to the same timeframe from nine previous years [7]. This study noted that a greater proportion (90.2%) of OHCAs occurred in the home setting compared to previous years (76.8%) and also demonstrated an increase in OHCA mortality after multivariate regression analysis. A meta-analysis utilizing data from New York, Lombardy, and Paris studies by Singh et al. showed a nearly two-fold increase in odds ratio of OHCA during the first half of 2020 in comparison to 2019 [9].
Other studies showed no appreciable change in OHCA associated with the COVID-19 pandemic. Padua, Italy saw no significant changes in OHCA incidence during the peak pandemic period compared to 2019 or previous years [10]. A study from Washington State from January to April 2020 also found no change in OHCA (incident rate ratio of 0.997 for OHCA events between 2019 and 2020 [95% CI 0.989–1.016. p = .72]) [11]. A study by Huber et al. of the urban regions surrounding Munich, Germany likewise demonstrated no appreciable change in OHCA incidence between 2020 and the mean incidence from 2017 to 2019 [12]. A review of OHCA data by Elmer et al. from rural areas of Pennsylvania compared OHCA incidence from January 2016 to February 2020 to the time period of March 1st to May 25th, 2020 and found no significant change in the incidence of OHCA [13].
3.2. Risks and logistics for OHCA during COVID-19
There was not widely accepted, international guidance and processes for resuscitation of OHCA during the pandemic, as there remains an ongoing debate as to the level of risk of exposure for first responders. The World Health Organization recognizes CPR as an aerosol-generating procedure (AGP) [14,15]. With that understanding, most published guidance favored the safety of EMS personnel in the form of required PPE (gloves, eye protection, and surgical masks) or delayed resuscitation until PPE was acquired and donned. These recommendations were reinforced with reports early in the pandemic from experiences related to in-hospital resuscitation. The Centers for Disease Control and Prevention (CDC) published a report about a group of healthcare personnel without proper PPE exposed to a hospitalized, COVID-19 patient in California early on in the pandemic. Of 121 exposed healthcare personnel, 43 became symptomatic, with three testing positive for COVID [16]. The authors recommended the use of a N95 or higher-level respirators as necessary to protect frontline workers performing AGP.
Many National Resuscitation Councils, including those of Australia, New Zealand, the United Kingdom, and the United States, recommended a conservative approach to CPR [17]. These conservative measures included rescue breathing with a bag-mask device with a filter and tight seal [18]. The Australian College of Emergency Medicine, recognizing that many first responders may not have access to all appropriate PPE for COVID-19, strongly recommended that first responders don at least gloves, eye protection, and a surgical mask before initiating chest compressions [17]. Health agencies, such as the American Heart Association (AHA), English National Health Service (NHS), and Belgian Resuscitation Council, released guidance that promoted first responder safety by limiting resuscitative efforts until first responders donned PPE [[19], [20], [21], [22]]. The International Liaison on Resuscitation (ILCoR) published more liberal guidance suggesting that lay rescuers consider chest compressions and public access defibrillation, initiation of rescue breaths (and chest compressions when appropriate) for infants and children, and for healthcare workers to consider defibrillation prior to donning PPE where perceived benefit outweighed potential risks [23]. The Department of Health and Social Care (DHSC) in England indicated that emergency medical service (EMS) personnel should carry out CPR while waiting for further support, without necessitating proper donning of PPE, as chest compressions and defibrillation were not deemed to be AGPs [20,22]. DHSC guidance indicated that delayed resuscitation led to avoidable fatalities. This was acknowledged in a systematic review by Couper et al. stating that CPR delayed by a few minutes reduced the likelihood of patient survival. They also conceded that providing CPR to a COVID-probable or positive patient without PPE placed healthcare workers at risk [24]. The systematic review also pointed out that amongst the published studies, none resolved the debate of whether chest compressions and defibrillation generated aerosols. Sayre et al. argued that while approximately one healthcare worker per 10,000 may die due to viral transmission from CPR on a COVID-19 patient, roughly 300 lives per 10,000 with OHCA would be saved as a result of CPR [11]. They suggested that bystander CPR should only be delayed for proper PPE donning in regions of particularly high COVID-19 incidence. Even in cases where chest compressions were associated with viral transmission, the exposure to other airway maneuvers during resuscitation made it difficult to isolate chest compressions as the solitary cause of transmission.
In addition to policy challenges and changes governing resuscitation during COVID-19, the pandemic created unique stressors to the response systems to OHCA and non-OHCA events, including changes in response time, bystander CPR and assistance, decrease in resuscitation attempts and the utilization of specific termination of resuscitation protocols. Some of these impacts are detailed in Table 2 . Studies noted an increase in time for EMS response as a result of COVID phone screening questions (COVID status and symptomology), increased dispatcher workload, and delays in EMS departure due to the need for PPE donning [7]. However, the transit time from EMS departure to arrival at the scene generally decreased due to a reduction in vehicle traffic. In Paris, BLS teams were limited to one person per patient to reduce exposure and to increase distribution of first responders [25].
Table 2.
Consequences of COVID-19 on EMS response to OHCA events.
| Consequence on EMS Response | Additional Notes | Source |
|---|---|---|
| Increased EMS response time as a result of: -COVID-19 phone screening questions -Increased dispatcher workload -Delays in departure due to PPE requirement for personnel |
Delays in ambulance departure mostly attributed to need for PPE; ambulance sanitization and increased number of trips are also factors | [7,26] |
| Fewer resuscitative maneuvers attempted by EMS personnel per OHCA incident | Reduction from 52% to 39% of OHCA events led to resuscitative efforts noted in Padua, Italy | [10] |
| Need for PPE prior to initiation of resuscitation | Consists of gloves, goggles, and surgical mask Delayed CPR can lead to reduced likelihood of patient survival |
[[17], [18], [19], [20], [21], [22]] |
| BLS and CPR training for EMS personnel on hold | Put on hold due to need for close quarters training and practice with mouth-to-mouth resuscitation | [44] |
| Decreased incidence of bystander CPR for OHCA events | Additive effects of bystander reluctance, as well as guidance requiring PPE prior to CPR initiation | [26,35] |
| Inaccessible public AED stations | Closure of locations as a result of lockdowns | [25] |
| Limited EMS personnel per incident response | Reducing potential exposure while increasing first responder distribution | [25] |
| Varied rates of resuscitative termination | Decentralization of EMS oversight in urban areas | [36] |
OHCA; out of hospital cardiac arrest, EMS; emergency medical service, PPE; personal protective equipment, CPR; cardiopulmonary resuscitation, BLS; basic life support, AED; automated external defibrillator.
There were reductions in bystander CPR in many of the studied geographic regions. While not an official part of any EMS system, bystander CPR is relied upon intervention that plays a crucial role in OHCA survival. In Italy, Baldi et al. found EMS response times actually increased with median arrival time increased by three minutes, and a 15.6% drop in incidence of bystander CPR during OHCA events [26]. Of these, COVID-positive patients represented 77.4% of the excess OHCA calls. Lockdowns, as a result of COVID-19, led to unique circumstances for EMS personnel. Jost et al. noted that “laypeople” who would ordinarily help with CPR were no longer available to support EMS efforts and emergency response teams [25]. Many automatic external defibrillators (AED) stations were inaccessible with the closure of most public places.
The majority of studies that looked at OHCA noted a drop in resuscitation attempts during the COVID-19 pandemic as well as the invoking of specific termination of resuscitation (TOR) protocols in several cities. In Padua, Italy, 39% of EMS events during the peak of the pandemic led to resuscitation attempts compared to 52% for similar time frame in 2019 [10]. Likewise in New York City, 89% of OHCA cases experienced termination of resuscitation during the pandemic period compared to 74% during the equivalent period in 2019 [5]. In Spain, the total number of country-wide resuscitation attempts dropped during the pandemic from February 1st to April 30th, when compared to similar time periods from two previous years (2017 and 2018) [27]. Los Angeles County and New York City governing councils released statements prohibiting the transport of OHCA patients with potential COVID infection without return of spontaneous circulation [28,29]. In both cases, this specific guidance was released in an effort to minimize exposure risk for first responders. Because of the decentralized nature of EMS oversight in Los Angeles County, there may have been further variability in the rates of TOR [30].
4. Discussion
In several studies and cities, there appears to be a strong correlation between the number of COVID-19 cases and OHCA events. The strongest correlation was demonstrated in Lombardy, Italy with a COVID pandemic curve and OHCA event curve that closely mirrored one other [4]. Landi and De Servi proposed several different hypotheses that contributed to the rise in the incidence of OHCA which included a combination of healthcare reorganization, lockdown measures, and reductions in hospital visits and admissions for cardiovascular events such as myocardial infarction, heart failure, and dysrhythmias [31]. In the Paris study, Marijon et al. proposed the rise in OHCA deaths were likely linked to the difficulties in accessing medical care, reluctance and fear of visiting the emergency department (ED) or medical offices, increased psychological stress, and scaled back non-essential medical services, interventions (such as elective surgeries), and consultations in Paris during the pandemic [7]. Similarly, authors from Munich, Germany hypothesized that regions reporting a high incidence of COVID-19 positivity during peak pandemic periods saw a decrease in non-COVID related hospital visits likely due to public fears of contracting COVID-19 [12]. This may explain why regions such as Lombardy [4], New York City [5,6], and Paris [7] experienced significant increases in OHCA incidence, while other regions with lower COVID-19 incidence such as rural areas of Pennsylvania, USA [14] (2 cases per thousand residents) saw no changes in OHCA incidence. Expanding on this hypothesis, Scquizzato et al. postulated that delays to hospital care may be associated with increased incidence of acute hypoxemic respiratory failure (evolves into cardiac arrest) as well as an increase in the presence of non-shockable rhythms during CPR [32]. Delays in care, related to the pandemic, which led to cardiac arrest, especially amongst patients with preexisting conditions, warrants further exploration. A report in England demonstrated that acute myocardial infarction (AMI)-related hospitalizations dropped substantially during their peak pandemic period, coinciding with an increased incidence of OHCA [33]. These authors also noted that patients with AMI who were hospitalized after OHCA faced increased delays to reperfusion, less frequently received invasive coronary angiography, and were less likely to receive patient care from a specialist.
Hospital reorganization in response to COVID-19 demands may have negatively impacted patients with preexisting heart and heart-related conditions. These findings suggest that OHCA spikes are associated with both hesitancy in visiting hospitals as well as reprioritized hospital resources in favor of COVID-19 positive patients. As more data becomes available, larger comparisons and trends of COVID-19 and OHCA cases/events can be better evaluated to determine if a broader relationship exists.
The presence of the COVID-19 pandemic altered how OHCA events were managed by the emergency response systems. In Padua, Italy resuscitative maneuvers were attempted in 39% of OHCA cases during the pandemic period in 2020 compared to 52% in the equivalent time period from 2019 [10]. Similar findings were reported in Paris, France [7] as well as a more recent study from Spain, where a reduction in resuscitation events was reported and found to be independent of levels of local community transmission, particularly in the weeks immediately following their national shutdown [13]. These findings could be related to due to a variety of factors, including fear of disease transmission, limited resources at accepting hospitals, and data suggesting particularly poor prognosis in COVID patients with cardiac arrest. Additionally, delays in EMS response times likely lead to prolonged downtimes, making resuscitative efforts less successful.
The reluctance of bystanders to perform CPR and limited access to public AEDs probably contributed to OHCA mortality in local communities during the pandemic. Reluctance by lay-people to perform CPR was already problematic prior to the pandemic [34]. The aversion to performing CPR was only exacerbated [25] in the setting of a virus transmitted through aerosols. Baldi et al. demonstrated that rates of lay-person CPR decreased in Italy [35], in line with other studies. The reluctance to perform CPR was further complicated by guidance from national resuscitative councils in Australia, New Zealand, United Kingdom, and the United States, mandating PPE be donned prior to initiating resuscitative maneuvers [17]. The reduction in lay-person resuscitation combined with delays in EMS initiating resuscitation, favors the safety of the responders, but comes at the expense of positive OHCA patient outcomes.
In addressing pre-hospital OHCA response, the use of point-of-care ultrasound (POCUS) is intriguing but unproven as of now. A few studies have shown that POCUS has predictive value in OHCA outcomes such as in-ED mortality and survival to ED admission [[36], [37], [38], [39]]. There are, however, many barriers to implementation, such as mechanical US device failure, deferred US use for purposes of other interventions, and logistics of transferring US devices between EMS vehicles [40]. Nonetheless, several other studies have shown that limited training time for EMS personnel can lead to proficient evaluation of patients with cardiac standstill [[41], [42], [43]]. Implementation of POCUS in pre-hospital settings may be feasible, but much more research and field data during COVID-19 is needed.
As the pandemic evolves, so may the characteristics of OHCA and prehospital care, particularly as additional data becomes available to inform best practices and EMS protocols. Most importantly, we must learn from our experiences. For instance, the onset of mass vaccinations has the potential to change case-by-case resuscitation protocols in the near future, depending on the vaccination history of the patient. This will need to be continually monitored as we continue our response to this pandemic.
4.1. Limitations
There are notable limitations in the literature review for OHCA and the use of POCUS in OHCA. Although the findings in our review suggest a relationship between COVID-19 and an increase in OHCA incidence, the retrospective nature of this study does not allow causation as a conclusion. There are also several noted studies that demonstrated lower OHCA incidence during peak pandemic periods, which contradicts other noted trends. Variable regional COVID-19 incidence rates were explored as potential causes for the difference in OHCA rates. Additionally, our search algorithm excluded studies that were not written or translated in English, which may have led to exclusion of other data sets. This review looked at emergency response across many discrete regions of the globe (which reached peak pandemic periods at different time points) and have variations in their EMS systems. Findings in one city or region may not be generalizable to other locales. Additionally, our findings are only relevant to regions with well-established EMS systems; we cannot generalize findings to regions without such systems. Further studies with OHCA-specific patient populations are necessary. Although there are studies published about the use of POCUS in OHCA events, there has yet to be literature published about this topic during the COVID-19 pandemic. As a result, the potential for true translational practice to COVID patients remains speculative and unknown. Many of the studies in this review were published early in the pandemic and current trends and practices likely changed as the pandemic evolved.
5. Conclusions
The ongoing COVID-19 pandemic altered the approach of first responders to OHCAs. Given its rise in incidence in several regions, impact on provider response, and conservative trending guidance on the use of PPE during resuscitative attempts, novel approaches such as POCUS deserve attention and further prehospital studies to evaluate OHCA patients while maintaining provider safety. Additionally, prehospital protocols must be continuously refined based on the most up to date data and consensus guidelines, during this rapidly evolving pandemic.
Financial support
This is a non-funded study, with no compensation or honoraria for conducting the study.
Declaration of Competing Interest
The authors do not have a financial interest or relationship to disclose regarding this research project.
References
- 1.McNally B., Robb R., Mehta M., et al. Out-of-hospital cardiac arrest surveillance --- cardiac arrest registry to enhance survival (CARES), United States, October 1, 2005--December 31, 2010. MMWR Surveill Summ. 2011;60(8):1–19. [PubMed] [Google Scholar]
- 2.Milan M., Perman S.M. Out of hospital cardiac arrest: a current review of the literature that informed the 2015 American Heart Association guidelines update. Curr Emerg Hosp Med Rep. 2016;4(4):164–171. doi: 10.1007/s40138-016-0118-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berdowski J., Berg R.A., Tijssen J.G., et al. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Baldi E., Sechi G.M., Mare C., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41(32):3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lai P.H., Lancet E.A., Weiden M.D., et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;5(10):1154–1163. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mountantonakis S.E., Saleh M., Coleman K., et al. Out-of-hospital cardiac arrest and acute coronary syndrome hospitalizations during the COVID-19 surge. J Am Coll Cardiol. 2020;76(10):1271–1273. doi: 10.1016/j.jacc.2020.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5(8):e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4) doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh S., Fong H.K., Mercedes B.R., Serwat A., Malik F.A., Desai R. COVID-19 and out-of-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2020;156:164–166. doi: 10.1016/j.resuscitation.2020.08.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paoli A., Brischigliaro L., Scquizzato T., Favaretto A., Spagna A. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the Province of Padua, Northeast Italy. Resuscitation. 2020;154:47–49. doi: 10.1016/j.resuscitation.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sayre M.R., Barnard L.M., Counts C.R., et al. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications for bystander CPR. Circulation. 2020;142(5):507–509. doi: 10.1161/CIRCULATIONAHA.120.048951. [DOI] [PubMed] [Google Scholar]
- 12.Huber B.C., Brunner S., Schlichtiger J., Kanz K.G., Bogner-Flatz V. Out-of-hospital cardiac arrest incidence during COVID-19 pandemic in southern Germany. Resuscitation. 2020;157:121–122. doi: 10.1016/j.resuscitation.2020.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elmer J., Okubo M., Guyette F.X., Martin-Gill C. Indirect effects of COVID-19 on OHCA in a low prevalence region. Resuscitation. 2020;156:282–283. doi: 10.1016/j.resuscitation.2020.08.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harding H., Broom A., Broom J. Aerosol-generating procedures and infective risk to healthcare workers from SARS-CoV-2: the limits of the evidence. J Hosp Infect. 2020;105(4):717–725. doi: 10.1016/j.jhin.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization Transmission of SARS-CoV-2: implications for infection prevention precautions. 2020. https://www.who.int/publications-detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations Retrieved October 31. from.
- 16.Heinzerling A., Stuckey M.J., Scheuer T., et al. Transmission of COVID-19 to health care personnel during exposures to a hospitalized patient — Solano County, California, February 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):472–476. doi: 10.15585/mmwr.mm6915e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craig S., Cubitt M., Jaison A., et al. Management of adult cardiac arrest in the COVID-19 era: consensus statement from the Australasian College for Emergency Medicine. Med J Aust. 2020;213(3):126–133. doi: 10.5694/mja2.50699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Edelson D.P., Sasson C., Chan P.S., et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020;141(25):e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coronavirus (COVID-19) Resources for CPR Training. 2020. https://cpr.heart.org/en/resources/coronavirus-covid19-resources-for-cpr-training Retrieved August 14. from.
- 20.Cappuccio F.P. Confusion over CPR in patients with covid-19. BMJ. 2020;369:m1805. doi: 10.1136/bmj.m1805. [DOI] [PubMed] [Google Scholar]
- 21.DeFilippis E.M., Ranard L.S., Berg D.D. Cardiopulmonary resuscitation during the COVID-19 pandemic: a view from trainees on the front line. Circulation. 2020;141(23):1833–1835. doi: 10.1161/CIRCULATIONAHA.120.047260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahase E., Kmietowicz Z. Covid-19: doctors are told not to perform CPR on patients in cardiac arrest. BMJ. 2020;368:m1282. doi: 10.1136/bmj.m1282. [DOI] [PubMed] [Google Scholar]
- 23.Perkins G.D., Morley P.T., Nolan J.P., et al. International liaison committee on resuscitation: COVID-19 consensus on science, treatment recommendations and task force insights. Resuscitation. 2020;151:145–147. doi: 10.1016/j.resuscitation.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Couper K., Taylor-Phillips S., Grove A., et al. COVID-19 in cardiac arrest and infection risk to rescuers: a systematic review. Resuscitation. 2020;151:59–66. doi: 10.1016/j.resuscitation.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jost D., Derkenne C., Kedzierewicz R., et al. The need to adapt the rescue chain for out-of-hospital cardiac arrest during the COVID-19 pandemic: experience from the Paris fire brigade basic life support and advanced life support teams. Resuscitation. 2020;153:56–57. doi: 10.1016/j.resuscitation.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baldi E., Sechi G.M., Mare C., et al. Out-of-hospital cardiac arrest during the covid-19 outbreak in Italy. N Engl J Med. 2020;383(5):496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosell Ortiz F., Fernández del Valle P., Knox E.C., et al. Influence of the Covid-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation. 2020;157:230–240. doi: 10.1016/j.resuscitation.2020.09.037. S0300–9572(20)30505–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schenker J., Diglio M. Regional Emergency Medical Services Council of New York City, Inc; New York: 2020. Temporary Cardiac Arrest Standards for Disaster Response.http://www.nycremsco.org/wp-content/uploads/2020/02/2020-08-REMAC-Advisory-Temporary-Cardiac-Arrest-Standards-for-Disaster-Response-1.pdf Report no: 2020–08. [Accessed 7 March 2021] [Google Scholar]
- 29.Gausche-Hill M. Emergency Medical Services Agency, Los Angeles County; Los Angeles: 2020 Apr 9. Out-of-Hospital Cardiac Arrest (OHCA) Care During The COVID-19 Crisis.http://file.lacounty.gov/SDSInter/dhs/1071072_COVID-19OHCA2020-04-09Memo.pdf [Accessed 7 March 2021] [Google Scholar]
- 30.O’Connell F., Sweetser P., Quan T., Pourmand A. Application of termination of resuscitation rules during the COVID-19 pandemic by emergency medical service. Am J Emerg Med. 2020;42:254–255. doi: 10.1016/j.ajem.2020.06.029. S0735–6757(20)30517–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Landi A., De Servi S. Temporal trends in out-of-hospital cardiac arrest during the COVID-19 outbreak. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.07.045. S0735–6757(20)30640–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scquizzato T., Landoni G., Paoli A., et al. Effects of COVID-19 pandemic on out-of-hospital cardiac arrests: a systematic review. Resuscitation. 2020;157:241–247. doi: 10.1016/j.resuscitation.2020.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rashid Hons M., Gale Hons C.P., Curzen Hons N., et al. Impact of coronavirus disease 2019 pandemic on the incidence and management of out-of-hospital cardiac arrest in patients presenting with acute myocardial infarction in England. J Am Heart Assoc. 2020;9(22) doi: 10.1161/JAHA.120.018379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baldi E., Bertaia D., Savastano S. Mouth-to-mouth: an obstacle to cardiopulmonary resuscitation for lay-rescuers. Resuscitation. 2014;85(12):e195–e196. doi: 10.1016/j.resuscitation.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Baldi E., Sechi G.M., Mare C., et al. Treatment of out-of-hospital cardiac arrest in the COVID-19 era: a 100 days experience from the Lombardy region. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0241028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aichinger G., Zechner P.M., Prause G., et al. Cardiac movement identified on prehospital echocardiography predicts outcome in cardiac arrest patients. Prehosp Emerg Care. 2012;16(2):251–255. doi: 10.3109/10903127.2011.640414. [DOI] [PubMed] [Google Scholar]
- 37.Blaivas M., Fox J.C. Outcome in cardiac arrest patients found to have cardiac standstill on the bedside emergency department echocardiogram. Acad Emerg Med. 2001;8(6):616–621. doi: 10.1111/j.1553-2712.2001.tb00174.x. [DOI] [PubMed] [Google Scholar]
- 38.Gaspari R., Weekes A., Adhikari S., et al. Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation. 2016;109:33–39. doi: 10.1016/j.resuscitation.2016.09.018. [DOI] [PubMed] [Google Scholar]
- 39.Kedan I., Ciozda W., Palatinus J.A., Palatinus H.N., Kimchi A. Prognostic value of point-of-care ultrasound during cardiac arrest: a systematic review. Cardiovasc Ultrasound. 2020;18(1):1. doi: 10.1186/s12947-020-0185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fitzgibbon J.B., Lovallo E., Escajeda J., Radomski M.A., Martin-Gill C. Feasibility of out-of-hospital cardiac arrest ultrasound by EMS physicians. Prehosp Emerg Care. 2019;23(3):297–303. doi: 10.1080/10903127.2018.1518505. [DOI] [PubMed] [Google Scholar]
- 41.Chin E.J., Chan C.H., Mortazavi R., et al. A pilot study examining the viability of a Prehospital Assessment with UltraSound for Emergencies (PAUSE) protocol. J Emerg Med. 2013;44(1):142–149. doi: 10.1016/j.jemermed.2012.02.032. [DOI] [PubMed] [Google Scholar]
- 42.Breitkreutz R., Price S., Steiger H.V., Seeger F.H., Ilper H., Ackermann H., et al. Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: a prospective trial. Resuscitation. 2010;81(11):1527–1533. doi: 10.1016/j.resuscitation.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 43.Krogh C.L., Steinmetz J., Rudolph S.S., et al. Effect of ultrasound training of physicians working in the prehospital setting. Scand J Trauma Resusc Emerg Med. 2016;24:99. doi: 10.1186/s13049-016-0289-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baldi E., Contri E., Savastano S., Cortegiani A. The challenge of laypeople cardio-pulmonary resuscitation training during and after COVID-19 pandemic. Resuscitation. 2020;152:3–4. doi: 10.1016/j.resuscitation.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]