Abstract
Background:
Social rhythmicity refers to the regularity with which one engages in social and lifestyle activities. Social rhythms have important implications for health and well-being including the prevention and treatment of mental health disorders. Existing research on social rhythmicity has focused on the link with bipolar disorder and, to a lesser extent, with depression. However, it is unclear how social rhythms are tied to anxiety disorders or what might mediate this association. Sleep shows potential as an underlying link, particularly sleep behaviors and sleep thoughts.
Methods:
The current study used a sample of 3,284 adults to examine the role of sleep thoughts and behaviors as mediators of the association between social rhythms and mental health symptoms of depression and anxiety.
Results:
Parallel mediation models revealed that greater social rhythmicity is directly associated with fewer depressive and anxiety symptoms, and that healthier sleep behaviors and thoughts mediate this association.
Limitations:
This study used cross-sectional data and was limited in racial and ethnic diversity.
Conclusions:
The findings highlight the critical role lifestyle regularity plays in depressive and anxious symptom pathology in a large sample of adults across the lifespan. Results also highlight the complementary roles for both sleep behaviors and thoughts by demonstrating their concurrent links between regularity and mental health. Future work is needed to further disentangle the association of these constructs with mental health.
Keywords: Sleep, social rhythmicity, lifestyle regularity, depression, anxiety
Introduction
Anxiety disorders are consistently found to be the most common mental illness worldwide (Kessler et al., 2009) and are highly comorbid with depression, the leading cause of disability worldwide (World Health Organization, 2018). An estimated 19.1% of U.S. adults had an anxiety disorder in 2017, and an estimated 7.1% of adults in the U.S. had at least one major depressive episode (National Institute of Mental Health, 2017). Given the high prevalence of anxiety and depression, there remains a need to better understand the etiology of anxiety and depressive symptomatology in order to contribute to effective prevention and treatment efforts.
Social and Circadian Rhythms
Social rhythmicity refers to the regularity with which one engages in social and lifestyle activities. Such activities include the timing of meals, bedtimes, and social interactions (Bullock et al., 2011). In humans, these rhythms can be endogenously determined and self-sustaining, but are also influenced and synchronized by exogenous factors (or external cues) such as light, temperature, or social interactions known as “zeitgeibers” (Schimitt et al., 2010). Theoretical models, such as Ehler’s (1988) social zeitgeber theory, have been put forth to explain the link between these social and biological rhythms.
According to the social zeitgeber theory (see Figure 1), changes in mood arise as a consequence of life events that disturb social zeitgebers which, in turn, derail social and biological rhythms (Ehlers, 1988). These changes in social zeitgebers can result in a disruption of social rhythms (e.g., bedtimes, socialization, and mealtimes; Ashman et al., 1999), which could subsequently impact biological rhythms (e.g. poor sleep). Finally, changes in mood are theorized to result from the disruption of biological rhythms (Boland et al., 2012). In other words, life events may disturb social zeitgebers, impacting social rhythms, which then, consequently, disrupt biological rhythms, potentially leading to poor mood symptoms.
Figure 1.
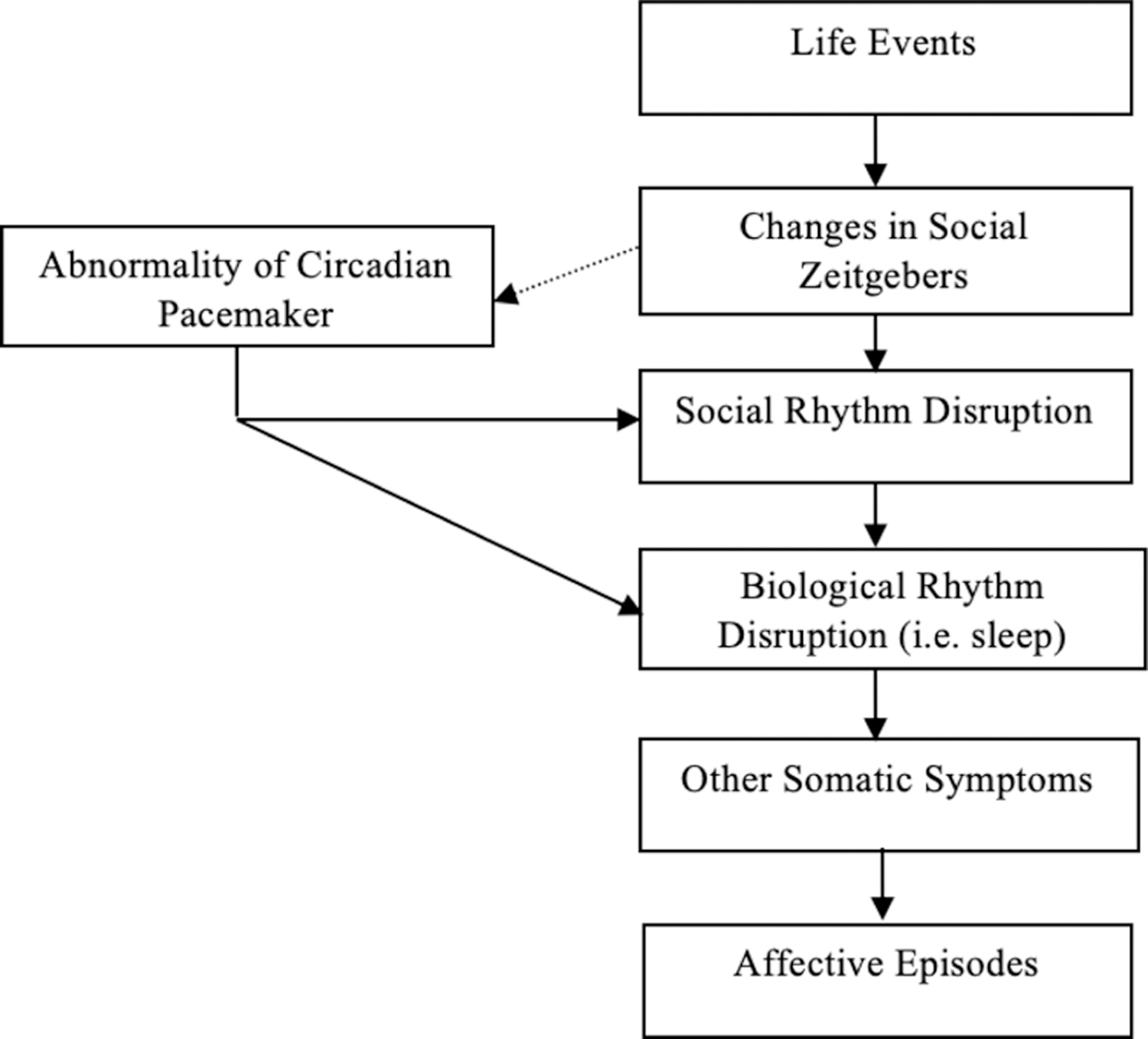
A model of the Social Zeitgeber Theory (Grandin et al., 2006).
Social Rhythmicity and Mental Health
The bulk of the literature on social rhythmicity has focused on clinical disorders with a primary focus on bipolar disorder (Ashman et al., 1999; Boland et al., 2012; Bullock et al., 2011; Ehlers, 1988; Grandin et al., 2006; Margraf et al., 2016; Monk et al., 1991). However, social rhythmicity has also been tied to depression. Individuals diagnosed with depression display significant disturbances in their biological rhythms, particularly in their sleep-wake cycles and in their neuroendocrine systems (Ashman et al., 1999; Boland et al., 2012; Brown et al., 1996; Ehlers, 1988; Grandin et al., 2006).
Conversely, less is known about the link between social rhythmicity and anxiety. Existing research suggests that similar to individuals diagnosed with depression, individuals diagnosed with anxiety disorders also exhibit irregular social rhythms (Margraf et al., 2016; Shear et al., 1994). Shear and colleagues (1994) suggested that individuals with anxiety disorders might have a heightened sensitivity to events that disrupt social rhythms, and that lower regularity in daily routine may contribute to feelings of unpredictability and uncontrollability that is characteristic of these disorders. In addition to the smaller body of research examining social rhythmicity and anxiety, little is known about the association between social rhythmicity and sub-clinical symptoms of anxiety and depression.
Sleep and Mental Health
In addition to the importance of social rhythm regularity for mental health, sleep disruption is highly comorbid with many, if not most, psychiatric disorders and subclinical symptoms (American Psychiatric Association, 2013; Benca et al., 1992; Harvey et al., 2011). Sleep disruption has been linked to the development, progression, and maintenance of anxiety and mood symptoms (Neckelmann et al., 2007). Our understanding of the role of sleep disturbance in both depression and anxiety has yielded important insights into the development, maintenance, and treatment of these disorders. Although the association between sleep disturbance and both anxiety and depression is well demonstrated, less is known about the relative importance of thoughts versus behaviors focused on sleep. To date, no known studies have investigated sleep behaviors (e.g. sleep health) and sleep thoughts (e.g. sleep self-efficacy) as predictors of mental health symptoms or as potential links between social rhythmicity and mental health symptoms. As such, the current study aims to examine the importance and role of sleep thoughts and behaviors as mediators of the association between social rhythms and depressive and anxiety symptoms. As these factors are salient and modifiable, they could be targeted to potentially intervene with depressive and anxiety symptoms. The current study seeks to investigate these associations in individuals reporting symptoms of anxiety and depression.
In summary, the present study had two aims: (1) to examine the association between social rhythmicity and depressive and anxiety symptoms, and (2) to investigate sleep health and sleep self-efficacy as mediators of the social rhythmicity and depressive and anxiety symptoms associations in adults. It was hypothesized that greater social rhythmicity (i.e., higher regularity) would be associated with fewer symptoms of depression and anxiety after adjusting for select covariates, and that both sleep health and sleep self-efficacy would emerge as links between social rhythmicity and depressive and anxiety symptoms
Method
Participants
The present study was a secondary analysis of data from the Investigating Sleep Longitudinally Across Normal Development (ISLAND) study (see Ravyts et al., 2019 for previous report using this data). In order to be eligible, participants had to be 18 years or older. The sample consisted of 3,284 participants (49% female) aged 18+. Inclusion and exclusion criteria were minimal and solely pertained to age and gender to ensure a relatively equal number of men and women living in the United States across the lifespan were recruited. A description of methods pertinent to the present study are provided here.
Procedure
The study was approved by the Institutional Review Board at Virginia Commonwealth University (IRB# HM20008543). Participants were recruited through Amazon’s Mechanical Turk (MTurk) and instructed to open a Qualtrics link to access the survey if they wished to participate. Upon clicking on the link, participants were informed about the purpose of the study and gave consent. In order to participate, access to a computer, tablet, or phone was required. Participants then completed a series of behavioral and psychological measures through self-report questionnaires, and received $0.25 for participating. Research examining data collected via MTurk has shown that compensation amounts do not affect the quality of data collected, and that the data obtained are as reliable as those obtained via traditional methods (Buhrmester et al., 2011).
The study lasted approximately 25–45 minutes. Two validity checks were integrated to address threats to validity associated with online data collection: (a) an instructional manipulation check which asked participants to respond to an item with a specific response and (b) a consistency check which compared participants’ responses to a question about their age at the beginning of the survey to a question about their birthdate at the end of the survey. Only participants who passed the instructional validity check and the consistency check were included in the present study (N = 3,284).
Measures
The Brief Social Rhythm Scale (BSRS):
Participants completed a 10-item self-report questionnaire that assesses the regularity with which they engage in basic daily activities during the weekdays and weekend. The BSRS is a shorter version of the Social Rhythm Metric (SRM; (Monk et al., 1991), a daily monitoring diary designed to assess social rhythms. Participants were asked to rate the general regularity of each activity (i.e., eating and meeting other people) in their lives in general using a scale ranging from 1 (very regularly) to 6 (very irregularly), with high mean scores indicating high irregularity. This measure can be administered at a single time point, rather than requiring a week of daily data to score. Summary scores are the average across all 10 items (ranging from 10 – 60). The original version of this scale, the SRM, has shown good test-retest reliability and construct validity, as well as adequate criterion validity for adults (Monk et al., 1991, 2002; Monk et al., 2003). Cronbach’s α in this sample was .85, suggesting good reliability within the sample.
RU Sated Scale:
Participants completed a 6-item self-report questionnaire (Buysse, 2014) that is used to assess six key dimensions of sleep health (RegUlarity, Satisfaction with sleep, Alertness during waking hours, Timing of sleep, Efficiency, and Duration). Participants indicated the frequency with which they experience or engage in each of the 6 sleep-wake behaviors in general. Individual items are scored on a scale from 1 (rarely/never) to 3 (usually/always). Item scores are totaled. A total score of “6” represents poor sleep health, and a score of “18” represents good sleep health. Preliminary evidence suggests that the scale is a valid and reliable measure for the assessment of sleep health indicators (Becker et al., 2018; Ravyts et al., 2019). Within the current sample, Cronbach’s α was lower (.64), suggesting suboptimal internal consistency.
Self-Efficacy of Sleep Scale (SES):
Participants completed a 9-item scale used to assess the sense of self-efficacy one has in regard to sleep (Lacks, 1987). On this measure, they were asked to indicate their beliefs about their level of confidence related to different aspects of sleep on a 5-point scale. Response options ranged from 1 (not confident at all) to 5 (very confident). The sum of confidence ratings provides an overall score of sleep self-efficacy that can range from 9 to 45, with higher scores reflecting more confidence. A previous study which used this measure with adults (aged 18+) demonstrated strong internal reliability (α = .85) as well as good concurrent validity and test-retest reliability (Bluestein et al., 2010). Cronbach’s α in the current sample was also good (.88).
Generalized Anxiety Disorder Scale (2 Items; GAD-2):
The GAD-2 is a short screening tool for generalized anxiety disorder that consists of the first two questions of the original GAD-7 scale (Spitzer et al., 2006). Response options were “not at all,” “several days,” “more than half the days,” and “nearly every day,” scored as 0, 1, 2, and 3, respectively. A total sum score was derived by adding the responses and was used in analyses. A score of 3 points is the preferred cut-off for identifying probable cases of GAD and in which further diagnostic evaluation is warranted. The original measure demonstrated excellent internal reliability (α = .92), as well as good criterion, construct, and procedural validity in a sample of adults aged 18+ (Spitzer et al., 2006). The internal reliability in the current sample was also good (α = .87).
Patient Health Questionnaire (2 items; PHQ-2):
The PHQ-2 consists of the first two questions of the PHQ-9—the depression module from the full PHQ (Spitzer et al., 1999). There were four response options ranging from not at all to nearly every day. A PHQ-2 score ranges from 0 to 6 and a total score was used in analyses by adding the responses. A score of 3 is the cut-off point when screening for depression with scores of 3 or greater indicating a likelihood that major depression is present. There is strong evidence for the reliability and validity (i.e. construct and criterion) of both the PHQ-9 and PHQ-2 (Kroenke et al., 2003). In the current sample, Cronbach’s α was .85.
Data Analyses
To assess all hypotheses, SPSS PROCESS macro (Hayes, 2013) was used to run two regressions and two parallel mediation models via a non-parametric, bias-corrected bootstrapping procedure that provided an empirical approximation of the sampling distribution of the product of the estimated coefficients in the indirect paths using 5,000 resamples from the dataset. Specifically, parallel mediation models were used to assess whether sleep health (M1) and sleep self-efficacy (M2) mediate the association between social rhythmicity (X) and anxiety and depressive symptoms (Y). In addition, the direct effect of: 1) social rhythmicity (X) predicting anxiety and depressive symptoms (Y; c’1); 2) the direct effect of social rhythmicity (X) predicting sleep health (M1) and sleep self-efficacy (M2; a1, a2); and 3) the direct effects of sleep health (M1) and sleep self-efficacy (M2) predicting anxiety and depressive symptoms (Y; b1, b2) were assessed. All models controlled for selected covariates of age and gender given known associations between an individual’s age and gender and social rhythmicity, sleep behaviors and mental health (Alvaro et al., 2013; Harvey, 2002; Monk et al., 2002; National Institute of Mental Health, 2017; World Health Organization, 2018).
Results
Descriptive and correlational results
On average, participants were 43.48 years old (SD = 16.68), primarily White (80.1%) and employed (61.9%), with over 50% of participants having a 4-year Bachelor’s degree or greater (Table 1). Pearson correlations were conducted to examine bivariate associations between all main variables of interest (i.e., social rhythmicity, sleep health, sleep self-efficacy, anxiety symptoms, depressive symptoms) and all covariates as presented in Table 2.
Table 1.
Participant Sociodemographic and Health Characteristics (M, SD)
| Variable | N | Percentage (%) |
|---|---|---|
| Age (43.48, 16.68) | ||
| 18 − 44 years | 1799 | 54.8 |
| 45 − 64 years | 978 | 29.8 |
| 65+ years | 507 | 15.4 |
| Gender | ||
| Male | 1479 | 45.0 |
| Female | 1594 | 48.5 |
| Other | 211 | 6.4 |
| Race | ||
| White/Caucasian | 2652 | 80.8 |
| Black/African American | 263 | 8.0 |
| Hispanic/Latino | 216 | 6.6 |
| Asian American | 208 | 6.3 |
| Native American/Pacific Islander | 67 | 2.1 |
| Employment Status | ||
| Employed for wages | 2034 | 61.9 |
| Unable to work or disabled | 111 | 3.4 |
| Unemployed | 266 | 8.1 |
| Retired | 459 | 13.9 |
| Student | 281 | 8.6 |
| Homemaker | 212 | 6.5 |
| Education | ||
| Doctorate Degree | 147 | 4.5 |
| Master’s Degree | 372 | 11.3 |
| 4-Year Bachelor Degree | 1171 | 35.7 |
| 2-Year Associate Degree | 387 | 11.8 |
| Some college | 853 | 26.0 |
| GED or high school equivalent | 96 | 2.9 |
| High school | 238 | 7.2 |
| Less than high school | 20 | 0.6 |
Note. More than one option may be endorsed for categories of race and employment status.
Table 2.
Pearson Correlation Coefficients among Social Rhythmicity, Sleep Health, Sleep Self-Efficacy, PHQ, and GAD
| Variable | M (SD) | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| 1. Social Rhythmicity | 28.72 (9.91) | - | ||||
| 2. Sleep Health | 7.59 (2.69) | −.406 | - | |||
| 3. Sleep Self-Efficacy | 29.32 (8.13) | −.365 | .617 | - | ||
| 4. PHQ | 1.59 (1.74) | .331 | −.397 | −.482 | - | |
| 5. GAD | 1.73 (1.86) | .283 | −.366 | −.490 | .730 | - |
Note. All data are significant at the p < .001 level
The direct associations between social rhythmicity, depressive symptoms, and anxiety symptoms
Accounting for covariates of age and gender, social rhythmicity was a significant predictor of both depressive symptoms (b = 0.050, SE = 0.003, p < 0.001) and anxiety symptoms (b = 0.045, SE = 0.003, p < 0.001). Higher irregularity predicted more symptoms. The overall models for depressive symptoms, F(5, 3278) = 178.973, p < .001, R2 = 0.214, and anxiety symptoms were significant, F(5, 3278) = 179.161, p < .001, R2 = 0.215. Results from the regression models for both outcomes are presented in Table 3.
Table 3.
Direct effect of Social Rhythmicity on Depressive and Anxiety Symptoms.
| Depressive Symptoms (Y) | Anxiety Symptoms (Y) | |||
|---|---|---|---|---|
| Coefficient (SE) | 0.95% CI | Coefficient (SE) | 0.95% CI | |
| Social Rhythmicity (X) | 0.055*** (0.003) | 0.049, 0.061 | 0.049*** (0.003) | 0.043, 0.055 |
| Age (U1) | −0.018*** (0.002) | −0.022, −0.015 | −0.023*** (0.002) | −0.027, −0.020 |
| Gender (U2) | 0.283*** (0.047) | 0.192, 0.374 | 0.420*** (0.050) | 0.322, 0.518 |
| R2 = 0.154 | R2 = 0.149 | |||
| F(2, 3280) = 198.288, p < .001 | F(2, 3280) = 191.496, p < .001 | |||
Note. U1 and U2 specify covariates.
p < .05,
p < .01,
p < .001.
The mediating roles of sleep health and sleep self-efficacy
For the model examining depressive symptoms, the direct association between social rhythmicity and sleep health and sleep self-efficacy was investigated (Table 4). After controlling for selected covariates, social rhythmicity was significantly associated with sleep health 95% CIs [−0.110, −0.092] and sleep self-efficacy [−0.300, −0.244]. Similarly, both sleep health [−0.079, − 0.027] and sleep self-efficacy [−0.071, −0.054] were significantly associated with depressive symptoms. Sleep health and sleep self-efficacy were then investigated as indirect pathways linking social rhythmicity to symptoms of depression. Both sleep health [0.005, 0.011] and sleep self-efficacy [0.019, 0.026] were found to be significant mediators of the social rhythmicity and depressive symptoms association. Greater social rhythmicity predicted better sleep health and sleep self-efficacy, which in turn, predicted fewer depressive symptoms.
Table 4.
Parallel Mediation Models Examining Depressive Symptoms.
| Sleep Health (M1) | Sleep Self-Efficacy (M2) | Depressive Symptoms (Y) | ||||
|---|---|---|---|---|---|---|
| Coefficient (SE) | 0.95% CI | Coefficient (SE) | 0.95% CI | Coefficient (SE) | 0.95% CI | |
| Social Rhythmicity (X) | −0.107*** (0.004) | −0.116, −0.099 | −0.288*** (0.013) | −0.314, −0.262 | 0.027*** (0.003) | 0.022, 0.033 |
| Sleep Health (M1) | -- | -- | -- | -- | −0.066*** (0.013) | −0.090, −0.041 |
| Sleep Self-Efficacy (M2) | -- | -- | -- | -- | –0.072*** (0.004) | –0.080, −0.064 |
| Age (U1) | 0.019*** (0.003) | 0.014, 0.024 | 0.047*** (0.008) | 0.032, 0.063 | −0.014*** (0.002) | −0.017, −0.011 |
| Gender (U2) | −0.223* (0.071) | −0.362, −0.085 | −1.636*** (0.217) | −2.062, −1.210 | 0.150*** (0.043) | 0.066, 0.235 |
|
R2 = 0.154 F(3, 3280) = 198.288, p < .001 |
||||||
Note. M1 and M2 indicate mediators. U1 and U2 specify covariates.
p < .05,
p < .01,
p < .001.
The direct association between social rhythmicity and sleep health and sleep self-efficacy was investigated in the model examining anxiety symptoms (Table 5). After controlling for selected covariates, social rhythmicity was significantly associated with sleep health 95% CIs [−0.112, −0.093] and sleep self-efficacy [−0.304, −0.247]. Similarly, both sleep health [−0.060, −0.004] and sleep self-efficacy [−0.088, −0.070] were significantly associated with anxiety symptoms. Social rhythmicity was linked to anxiety symptoms via sleep health [0.002, 0.009] and sleep self-efficacy [0.024, 0.032] as significant mediators. Once again, greater sleep health and sleep self-efficacy were associated with fewer anxiety symptoms, and significantly mediated the social rhythmicity − anxiety symptoms relation.
Table 5.
Parallel Mediation Models Examining Anxiety Symptoms.
| Sleep Health (M1) | Sleep Self-Efficacy (M2) | Depressive Symptoms (Y) | ||||
|---|---|---|---|---|---|---|
| Coefficient (SE) | 0.95% CI | Coefficient (SE) | 0.95% CI | Coefficient (SE) | 0.95% CI | |
| Social Rhythmicity (X) | −0.107*** (0.004) | −0.116, −0.099 | −0.288*** (0.013) | −0.314, −0.262 | 0.020*** (0.003) | 0.014, 0.027 |
| Sleep Health (M1) | -- | -- | -- | -- | −0.038* (0.013) | −0.064, −0.012 |
| Sleep Self-Efficacy (M2) | -- | -- | -- | -- | −0.087*** (0.004) | −0.096, −0.079 |
| Age (U1) | 0.019*** (0.003) | 0.014, 0.024 | 0.047*** (0.008) | 0.032, 0.063 | −0.019*** (0.002) | −0.022, − 0.015 |
| Gender (U2) | −0.223* (0.071) | −0.362, −0.085 | −1.636*** (0.217) | −2.062, −1.210 | 0.269*** (0.046) | 0.178, 0.359 |
| R2 = 0.149 | ||||||
| F(3, 3280) = 191.496, p < .001 | ||||||
Note. M1 and M2 indicate mediators. U1 and U2 specify covariates.
p < .05,
p < .01,
p < .001.
Discussion
The purpose of the present study was to characterize the associations between social rhythmicity, sleep health, sleep self-efficacy, and mental health in individuals reporting depressive and anxiety symptoms. Importantly, the association between sleep and mental health and social rhythmicity is likely bidirectional. Poorer mental health likely leads to poorer sleep thoughts and behaviors as well as greater social irregularity. However, the focus in the current study was to explore one particular direction of these associations with social rhythmicity predicting mental health symptoms and sleep thoughts and behaviors serving as links between this association. This study found cross-sectional evidence that social rhythmicity is directly associated with depressive and anxiety symptoms, and that sleep behaviors and thoughts mediate this association.
The findings from the current study add to the literature supporting the important associations of regularity and sleep with symptoms of depression and extend our understanding to symptoms of anxiety. The first aim of the study highlighted the links between lifestyle irregularity and anxiety and depressive symptoms. These findings align with previous studies that report associations between social rhythmicity and depression (Brown et al., 1996; Monk et al., 1991), as well as anxiety (Margraf et al., 2016; Shear et al., 1994). As previously mentioned, there is a much smaller body of literature that has linked social rhythmicity to anxiety. The current study’s findings add to the body of research in both of these areas and suggest that social rhythmicity is tied to anxiety and depressive mental health functioning in a continuum of individuals ranging from no symptomatology to severe.
Beyond tying social rhythmicity to mental health outcomes, a major aim of this study was to try to understand how social rhythmicity might be associated with mental health. Building on a common thread among existing research on social rhythmicity and mental health outcomes that recognizes the importance of sleep (i.e. the Social Zeitgeber Theory), the current study found further support for the importance of sleep by examining unique facets of sleep. Specifically, we examined sleep behaviors (sleep health) and sleep thoughts (sleep self-efficacy) as potential underlying processes within the social rhythmicity and mental health associations. Though an abundance of research has illustrated associations between sleep dysfunction with both depression and anxiety symptoms, much less is known about how the constructs of sleep health and sleep self-efficacy may also be associated with these mental health symptoms. Individual components of sleep health (i.e. sleep duration) have been tied to both depression and anxiety symptomology (Alvaro et al., 2013; Benca et al., 1992), as well as to social rhythms (Monk et al., 2003). In addition, sleep self-efficacy has been examined in relation to insomnia severity, health status, and insomnia treatment acceptability for behavioral approaches (Bluestein et al., 2010, 2011; Rutledge et al., 2013). However, sleep self-efficacy has not been examined in relation to mental health symptoms or social rhythmicity and no studies to date have examined sleep health and sleep self-efficacy as mediators.
Our finding that sleep health and sleep self-efficacy cross-sectionally link social rhythmicity and mental health symptoms is notable for several reasons. First, the examination of sleep health in relation to social rhythmicity or mental health outcomes is a novel addition to the literature. As mentioned above, the six characteristics of sleep health proposed by Buysse (2014) have each been studied separately quite heavily, with clear associations with physical, mental, and neurobehavioral health. For instance, sleep satisfaction/quality and efficiency (two of the dimensions of sleep health) have been previously linked to depressive symptoms (Baglioni et al., 2011). However, the construct of sleep health in its entirety has been studied minimally in relation to mental health symptoms. Our finding suggests that overall, the combination of the six dimensions of sleep health—regularity, satisfaction with sleep, alertness during waking hours, timing of sleep, sleep efficiency, and sleep duration—are linked to both social rhythm regularity and mental health symptoms. Sleep health indicates how well an individual is doing holistically in terms of their sleep practices. The expansion of our understanding of the sleep-mental health association to include sleep health has significant implications for future research. Further research with clinical samples could extend the understanding of the sleep—mood association by exploring sleep health as a protective factor within this population.
Second, our findings highlight the importance of both sleep behaviors and thoughts by demonstrating their ties to mental health, as well as their link between regularity and mental health. Though these are two entirely distinct constructs of sleep, they appear to be complementing each other by operating in a similar manner and relating similarly to depressive and anxiety symptoms. Additionally, the fact that both of these constructs remained significant when entered in parallel in the model suggests there is a unique role for each aspect of sleep in the rhythmicity—mental health association. The notion that thoughts and behaviors are tied to mental health is not new. For instance, it is widely acknowledged that cognitive processes play an essential role in the development, maintenance, and treatment of various disorders, from depression and anxiety disorders to insomnia (Harvey, 2002; Hiller et al., 2015). Similarly, behavioral activation, which aims to increase engagement in adaptive activities, is a popular evidence-based treatment for depression. As an example, these two pieces are collectively highlighted and acknowledged through the widely-used Cognitive-Behavior Therapy (CBT), which places equal importance on the roles of thoughts and behaviors as agents of change. However, this is the first study to find that lifestyle regularity is linked to mental health via sleep behaviors and thoughts, as well as the first to examine both of these constructs together. The findings suggest that how we think and behave in regards to sleep are underlying mechanisms in this association, which sheds light on the connection between each of these constructs. In addition to existing research which suggests social rhythmicity can predict better health outcomes (Boland et al., 2012; Shen et al., 2008), our findings suggest that regular daily activities are tied to fewer depressive and anxiety symptoms by facilitating healthy sleep behaviors and thoughts. For example, perhaps by maintaining a regular sleep/wake schedule and starting work at the same time, it is easier to obtain sufficient regular sleep (behaviors) and avoid catastrophizing and engaging in safety behaviors as the result of a poor night’s sleep (thoughts). Although the cross-sectional study design precludes making assumptions about causality and directionality, the mediation results stress the need to extend our understanding of sleep to include sleep-related behaviors and thoughts, as they are both playing significant roles in relation to social rhythms and mental health. An investigation into how social rhythmicity may contribute to healthy sleep behaviors and thoughts, is also warranted.
Implications
The associations between social rhythmicity, sleep health, sleep self-efficacy, and mental health symptoms have potentially important implications for treatment development and implementation. As previous researchers have pointed to the bidirectional nature of these relationships, treatment of either problems has the potential to impact the other. For example, interventions such as progressive muscle relaxation and guided imagery are empirically supported methods to reduce arousal and are often employed for both heightened mood and anxiety symptoms, as well as sleep disruptions (Coles et al., 2015). Research on the transdiagnostic role of mental processes, such as recurrent negative thinking and selective attention, suggest that there are likely underlying factors that contribute to regularity, sleep, and mental health symptomatology (Harvey et al., 2004). As such, future research is needed to understand the overlap between these variables. Furthermore, specific therapies that target regularity such as Interpersonal and Social Rhythm Therapy (IPSRT; Frank et al., 1997) may have a broader impact on sleep and mental health functioning. Furthering our understanding of the factors that contribute to depression and anxiety will allow us to improve our interventions.
Limitations and Strengths
There are several limitations in the current study which must be addressed. First is related to the cross-sectional nature of the data. We were unable to assess causality or directionality of the associations of interest by the current analyses. Longitudinal investigations are a critical next step for future research to identify the unique and complimentary contributions of these constructs. Second, the study design did not allow for a clear picture of participant diagnostic status. As such, it is unknown whether, and how many, participants may have a major depressive disorder, bipolar disorder, or an anxiety disorder. Further research is needed to explore these diagnostic differences. Third, this study relied exclusively on self-report measures. Incorporating objective measures of sleep (i.e. actigraphy), for example, would complement existing self-report measures of sleep behaviors, attitudes, and beliefs. Lastly, participants needed access to the internet in order to participate, and it is possible that important differences exist within individuals who do not have internet access.
Although the study does contain limitations, there are several strengths. First, through this data we examined a broad range of adults living in the US. Of particular note, the sample included a wide age-range of adults, with 15% of participants aged 65+ years. Second, this study extended the study of sleep by examining more than one aspect of sleep. Third, we used well-validated measures of mental health symptoms, regularity of social rhythms, and sleep health/thoughts.
Conclusions
The current study presented evidence that both higher symptoms of depression and anxiety are associated with disruptions in social rhythms through both poorer sleep health and lower sleep self-efficacy. Social rhythms, sleep thoughts, sleep behaviors, and mental health are critical facets of daily functioning in adults. Therefore, continued research efforts are needed to extend our understanding of their profound impact on health given their daily reoccurrence.
Highlights.
Social rhythmicity is linked to fewer depressive and anxiety symptoms in a wide age range of adults
Both sleep behaviors and thoughts link rhythmicity and mental health symptoms
Sleep health measured by the RU SATED scale ties rhythmicity and mental health
Sleep self-efficacy is a tie between rhythmicity and mental health
Daily lifestyle regularity has important benefits for mental health
Acknowledgements
This was supported by a grant from the National Institute on Aging under Grant K23AG049955.
Role of the Funding Source
This work was supported by a grant from the National Institute on Aging (NIA) of the National Institutes of Health (NIH) under Grant K23AG049955 (PI: Dzierzewski).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The data that support the findings of this study are available from the corresponding author, Joseph M. Dzierzewski, upon reasonable request.
Declaration of Competing Interest
None
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Alvaro PK, Roberts RM, & Harris JK (2013). A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep, 36(7), 1059–1068. 10.5665/sleep.2810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashman SB, Monk TH, Kupfer DJ, Clark CH, Myers FS, Frank E, & Leibenluft E (1999). Relationship between social rhythms and mood in patients with rapid cycling bipolar disorder. Psychiatry Research, 86(1), 1–8. 10.1016/S0165-1781(99)00019-0 [DOI] [PubMed] [Google Scholar]
- Becker NB, Martins RIS, Jesus S. de N., Chiodelli R, & Rieber MS (2018). Sleep health assessment: A scale validation. Psychiatry Research, 259, 51–55. 10.1016/j.psychres.2017.10.014 [DOI] [PubMed] [Google Scholar]
- Bluestein D, Healey AC, & Rutledge CM (2011). Acceptability of behavioral treatments for insomnia. The Journal of the American Board of Family Medicine, 24(3), 272–280. 10.3122/jabfm.2011.03.100246 [DOI] [PubMed] [Google Scholar]
- Bluestein D, Rutledge CM, & Healey AC (2010). Psychosocial correlates of insomnia severity in primary care. The Journal of the American Board of Family Medicine, 23(2), 204–211. 10.3122/jabfm.2010.02.090179 [DOI] [PubMed] [Google Scholar]
- Boland EM, Bender RE, Alloy LB, Conner BT, LaBelle DR, & Abramson LY (2012). Life events and social rhythms in bipolar spectrum disorders: An examination of social rhythm sensitivity. Journal of Affective Disorders, 139(3), 264–272. 10.1016/j.jad.2012.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LF, Reynolds CF, Monk TH, Prigerson HG, Dew MA, Houck PR, Mazumdar S, Buysse DJ, Hoch CC, & Kupfer DJ (1996). Social rhythm stability following late-life spousal bereavement: Associations with depression and sleep impairment. Psychiatry Research, 62(2), 161–169. 10.1016/0165-1781(96)02914-9 [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk: A New Source of Inexpensive, Yet High-Quality, Data? Perspectives on Psychological Science, 6(1), 3–5. 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Bullock B, Judd F, & Murray G (2011). Social rhythms and vulnerability to bipolar disorder. Journal of Affective Disorders, 135(1–3), 384–388. 10.1016/j.jad.2011.06.006 [DOI] [PubMed] [Google Scholar]
- Coles ME, Schubert JR, & Nota JA (2015). Sleep, Circadian Rhythms, and Anxious Traits. Current Psychiatry Reports, 17(9), 73. 10.1007/s11920-015-0613-x [DOI] [PubMed] [Google Scholar]
- Ehlers CL (1988). Social zeitgebers and biological rhythms: A unified approach to understanding the etiology of depression. Archives of General Psychiatry, 45(10), 948. 10.1001/archpsyc.1988.01800340076012 [DOI] [PubMed] [Google Scholar]
- Grandin LD, Alloy LB, & Abramson LY (2006). The social zeitgeber theory, circadian rhythms, and mood disorders: Review and evaluation. Clinical Psychology Review, 26(6), 679–694. 10.1016/j.cpr.2006.07.001 [DOI] [PubMed] [Google Scholar]
- Harvey AG, Watkins E, & Mansell W (2004). Cognitive behavioural processes across psychological disorders: A transdiagnostic approach to research and treatment. Oxford University Press. [Google Scholar]
- Harvey AG (2002). A cognitive model of insomnia. Behaviour Research and Therapy, 40(8), 869–893. 10.1016/S0005-7967(01)00061-4 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, Üstün TB, & Wang PS (2009). The global burden of mental disorders: An update from the WHO World Mental Health (WMH) Surveys. Epidemiologia e Psichiatria Sociale, 18(1), 23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (n.d.). The Patient Health Questionnaire-2: validity of a two-item depression screener. 41(11), 10. [DOI] [PubMed] [Google Scholar]
- Margraf J, Lavallee K, Zhang X, & Schneider S (2016). Social rhythm and mental health: a cross-cultural comparison. PLOS ONE, 11(3), e0150312. 10.1371/journal.pone.0150312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk TH, Frank E, Potts JM, & Kupfer DJ (2002). A simple way to measure daily lifestyle regularity. Journal of Sleep Research, 11(3), 183–190. 10.1046/j.1365-2869.2002.00300.x [DOI] [PubMed] [Google Scholar]
- Monk TH, Kupfer DJ, Frank E, & Ritenour AM (1991). The social rhythm metric (SRM): Measuring daily social rhythms over 12 weeks. Psychiatry Research, 36(2), 195–207. 10.1016/0165-1781(91)90131-8 [DOI] [PubMed] [Google Scholar]
- Monk TH, Reynolds CF, Buysse DJ, DeGrazia JM, & Kupfer DJ (2003). The relationship between lifestyle regularity and subjective sleep quality. Chronobiology International, 20(1), 97–107. 10.1081/CBI-120017812 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2017). Mental Health Information: Statistics. https://www.nimh.nih.gov/health/statistics/any-anxiety-disorder.shtml
- Neckelmann D, Mykletun A, & Dahl AA (2007). Chronic insomnia as a risk factor for developing anxiety and depression. Sleep, 30(7), 873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravyts SG, Dzierzewski JM, Perez E, Donovan EK, & Dautovich ND (2019). Sleep Health as Measured by RU SATED: A Psychometric Evaluation. Behavioral Sleep Medicine, 1–9. 10.1080/15402002.2019.1701474 [DOI] [PMC free article] [PubMed]
- Rutledge CM, Guardia ACL, & Bluestein D (2013). Predictors of self-efficacy for sleep in primary care. Journal of Clinical Nursing, 22(9–10), 1254–1261. 10.1111/jocn.12005 [DOI] [PubMed] [Google Scholar]
- Schimitt RL, Zanetti T, Mayer M, Koplin C, Guarienti F, & Hidalgo MP (2010). Psychometric properties of Social Rhythm Metric in regular shift employees. Revista Brasileira de Psiquiatria, 32(1), 47–55. 10.1590/S1516-44462010000100010 [DOI] [PubMed] [Google Scholar]
- Shear MK, Randall J, Monk TH, Ritenour A, Tu X, Frank E, Reynolds C, & Kupfer DJ (1994). Social rhythm in anxiety disorder patients. Anxiety, 1(2), 90–95. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, & Williams JBW (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA, 282(18), 1737. 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A brief measure for sssessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2018). Mental Disorders: Key Facts. https://www.who.int/news-room/fact-sheets/detail/mental-disorders


