Abstract
Background
Occupational injuries and hazards related to orthopaedic surgery are not well studied, and what is published on this topic is largely based on in vitro or in vivo animal studies.
Objectives
To evaluate the self-reported prevalence of musculoskeletal (MSK) overuse disorders and other conditions among orthopaedic surgeons, especially those performing total hip (THA) or total knee arthroplasty (TKA), and report the factors placing these surgeons at higher risk for occupational health hazards.
Methods
This was a cross-sectional study of 66 currently practicing orthopaedic surgeons in the Midwestern United States. An online survey was sent to the participants, and all responses were collected anonymously. The survey consisted of 18 multiple-choice questions.
Results
Almost 82% of surgeons surveyed had either a musculoskeletal (MSK) overuse disorder, kidney stones, cataracts, infertility, deafness, or a combination of the above. Fifty-three percent of these respondents believed their medical conditions arose due to their job demands or exposure. A majority of the orthopaedic surgeons surveyed wanted to retire at either 60–65 years of age (31.8%) or 66–70 years of age (47%). Nearly 88% of the survey respondents believed they will be able to meet the demands of their job until their intended retirement age. The prevalence of an overuse disorder was highest for those who have been in practice for 21–30 years (100%). There was a trend toward higher rate of surgery for overuse condition in Adult Reconstruction (AR) surgeons. Rotator cuff disease was the most common MSK disorder affecting AR surgeons.
Conclusion
A majority (>80%) of orthopaedic surgeons suffer from a musculoskeletal overuse disorder, kidney stones, cataracts, infertility, deafness, or a combination of these. A significant proportion (53%) of surgeons believe one or more of their medical conditions developed due to occupational exposure.
Keywords: Occupational hazard, Orthopaedic surgeon, Exposure, Adult reconstruction hazard, Occupational risk, Hazards orthopedics, Musculoskeletal disorder
1. Introduction
No occupation is without its hazards, and surgical specialties are no exception. Occupational injuries and hazards related to surgery are not well studied, and what is published so far on this topic is largely based on in vitro or in vivo animal studies.1 For instance, Choi et al. evaluated the cancer risk based on the compounds commonly found in surgical smoke and reported that the cancer risk was greater than negligible for two carcinogenic compounds—1,2-dichloroethane and benzene.2 They concluded that while surgical smoke is not an immediate health hazard, its long-term health risks to operating room personnel are yet to be elucidated. However, there are no clinical studies to date evaluating the effect of surgical smoke on cancer risk in surgeons.
Furthermore, there is a lack of adequate training in mitigating the risks and occupational hazards associated with surgical specialties. Orthopaedic surgeons are at increased risk of infection due to needlestick injuries. Occupational exposure to hepatitis B virus (HBV) has been shown to result in a seropositivity rate as high as 10–28% among surgeons.3 While this transmission risk is lower for human immunodeficiency virus (HIV), the consequences of seroconversion are no less devastating for the surgeon.3 The risk of glove perforation due to needlestick injuries is nearly twofold higher among surgical trainees than attending physicians.4 This highlights the need for increased awareness of this occupational hazard and better training in mitigating this risk.
Orthopaedic surgery is a field that can place the surgeons at increased risk of infection, exposure to radiation, chemicals, noise, surgical smoke, and musculoskeletal injuries.5 While it is universally acknowledged that orthopaedic surgery presents a potentially hazardous work environment, there is sparse literature quantifying those risks. The purpose of this study was to evaluate the self-reported prevalence of musculoskeletal (MSK) overuse disorders and other conditions among orthopaedic surgeons, especially those performing total hip (THA) or total knee arthroplasty (TKA), and report the factors placing these surgeons at higher risk for occupational health hazards. We chose to analyze total joint replacement in particular because we hypothesized that surgeons in this specialty may experience higher rate of MSK overuse disorders—a label used to categorize all chronic musculoskeletal diagnoses or complaints—due to the physical demands of their specialty.
2. Methods
A cross-sectional study of actively practicing orthopaedic surgeons in the Midwestern United States was undertaken. Institutional review board approval was obtained prior to commencing the study. Participants were identified through a midwestern state orthopaedic society (OS) membership list. All OS members were sent an email requesting their optional participation in an online survey consisting of 18 multiple-choice questions in March 2020 (Table 1). Only currently practicing orthopaedic surgeons were included. Physicians who were not surgeons or those who were not currently practicing were excluded from the study. All responses were collected anonymously over the course of two weeks. These responses were extracted to an excel sheet and analyzed. Statistical analysis was performed for categorical variables of interest where appropriate using the Chi-squared test with an alpha of 0.05.
Table 1.
Survey questions.
| 1. Please specify your sex: | a. Female |
|---|---|
| b. Male | |
| 2. Please indicate your hand dominance: | a. Left |
| b. Right | |
| c. Ambidextrous | |
| 3. The majority of your caseload consists of hip and knee replacement surgeries. | a. Yes |
| b. No | |
| 4. If you answered yes to question 3, which of the following best describes your practice setting? | a. Private |
| b. Academic | |
| c. Hospital employed | |
| d. Other: | |
| 5. How many years have you been in practice after finishing training? | a. 1–5 years |
| b. 6–10 years | |
| c. 11–15 years | |
| d. 16–20 years | |
| e. 21-30 years | |
| f. > 30 years | |
| 6. How many cases of total knee or hip replacement do you perform per week? | a. 5–10 |
| b. 11–15 | |
| c. 16–20 | |
| d. 21–30 | |
| e. 30-40 | |
| f. >40 | |
| g. Not applicable since I do not perform TKA or THA | |
| 7. What percent of your total hip replacement cases are anterior approach? | a. < 25% |
| b. 25–50% | |
| c. 51–75% | |
| d. >75% | |
| e. Not applicable since I do not perform TKA or THA | |
| 8. What percent of your total knee replacement cases are robotic or computer navigated? | a. < 25% |
| b. 25–50% | |
| c. 51–75% | |
| d. >75% | |
| e. Not applicable since I do not perform TKA or THA | |
| 9. What percent of your total hip replacement cases are robotic or computer navigated? | a. < 25% |
| b. 25–50% | |
| c. 51–75% | |
| d. >75% | |
| e. Not applicable since I do not perform TKA or THA | |
| 10. What percent of all of your cases as revision arthroplasties? | a. < 25% |
| b. 25–50% | |
| c. 51–75% | |
| d. >75% | |
| e. Not applicable since I do not perform TKA or THA | |
| 11. Do you suffer from or have you suffered from any of the following issues? Please select all answer choices that apply. | a. Rotator cuff disease |
| b. Other shoulder issues (eg – biceps tendonitis, AC joint arthritis, glenohumeral arthritis, etc) | |
| c. Carpal tunnel syndrome | |
| d. Trigger finger | |
| e. Lateral epicondylitis | |
| f. Medial epicondylitis | |
| g. Other overuse conditions of the upper extremity (eg – thumb CMC arthritis, etc) | |
| h. Neck issues such as pain, radiculopathy, slipped disk, arthritis, or other pathology | |
| i. Back issues such as pain, radiculopathy, slipped disk, arthritis, or other pathology | |
| j. Prostate cancer | |
| k. Breast cancer | |
| l. Thyroid cancer | |
| m. Other cancer – please specify | |
| n. Deafness | |
| o. Cataracts | |
| p. Other eye or ear issues | |
| q. Kidney stones | |
| r. Other urological issues | |
| s. Achilles tendonitis | |
| t. Other chronic foot conditions (eg - plantar fasciitis, pain, etc) | |
| u. Inguinal hernia | |
| v. Other, please specify: | |
| 12. Did you need surgery for any of the following issues? Please select all answers that apply. | a. Rotator cuff disease |
| b. Other shoulder issues (eg – biceps tendonitis, AC joint arthritis, glenohumeral arthritis, etc) | |
| c. Carpal tunnel syndrome | |
| d. Trigger finger | |
| e. Lateral epicondylitis | |
| f. Medial epicondylitis | |
| g. Other overuse conditions of the upper extremity (eg – thumb CMC arthritis, etc) | |
| h. Neck issues such as pain, radiculopathy, slipped disk, arthritis, or other pathology | |
| i. Back issues such as pain, radiculopathy, slipped disk, arthritis, or other pathology | |
| j. Prostate cancer | |
| k. Breast cancer | |
| l. Thyroid cancer | |
| m. Other cancer – please specify | |
| n. Deafness | |
| o. Cataracts | |
| p. Other eye or ear issues | |
| q. Kidney stones | |
| r. Other urological issues | |
| s. Achilles tendonitis | |
| t. Other chronic foot conditions (eg - plantar fasciitis, pain, etc) | |
| u. Inguinal hernia | |
| v. Other, please specify: | |
| 13. Do you think your medical condition/s (if you suffer from one) is related to your job demands or on-the-job exposure? | a. Yes |
| b. No | |
| 14. Did you ever sustain a work-related injury requiring time off from work? | a. Yes |
| b. No | |
| 15. When do you want to retire from operating? | a. Age <60 years |
| b. Age 60–65 years | |
| c. Age 66–70 years | |
| d. Age 71–75 years | |
| e. Age >75 years | |
| 16. Do you think you will be able to meet the physical demands of your job until your intended retirement age? | a. Yes |
| b. No | |
| 17. Do you think most of the tools you use during surgery are ergonomically designed? | a. Yes |
| b. No | |
| 18. What arthroplasty system do you use for the majority of your cases? | a. Depuy |
| b. Stryker | |
| c. Zimmer Biomet | |
| d. Smith and Nephew | |
| e. Other- please specify: |
3. Results
A total of 266 OS members were emailed, and 66 surgeons completed the survey. Of these 66 participants, 59 (89.4%) of them identified as male and 7 (10.6%) as female. A total of 15.2% of the surgeons identified as being left-handed, 81.8% as being right-handed, and 3% as being ambidextrous. The survey respondents varied in terms of their level of experience. The largest proportion (22.7%) of the respondents had been in practice for 1–5 years after completion of residency or fellowship while the smallest proportion (9.1%) of the participants had been in practice for 11–15 years (Fig. 1).
Fig. 1.
Survey respondents' level of clinical experience.
Among all the orthopaedic surgeons who completed the survey, 81.8% (out of 66) had either MSK overuse disorder, kidney stones, cataracts, infertility, deafness, or a combination of the above. Furthermore, 53% of the surgeons who were suffering from one of the aforementioned chronic conditions believed their medical conditions arose due to their job demands or on-the-job exposure. More than a third (35.2%) of the surgeons with the above medical conditions required surgery for one or more of their medical conditions. Fewer than 5% (4.5%) of the respondents reported that they sustained a work-related injury requiring time off from work.
A total of 87.9% of the survey respondents reported that they believe they will be able to meet the demands of their job until their intended retirement age. A majority of the orthopaedic surgeons surveyed said that they wanted to retire at either 60–65 years of age (31.8%) or 66–70 years of age (47%). Nearly 10% (9.1%) of the respondents said that they would like to retire at 71–75 years of age, while another 9.1% said they would like to retire at less than 60 years of age. Three percent said they would like to retire when they are older than 75 years of age or never. Only 42.4% of the surgeons responded that the tools they use during surgery are ergonomically designed. The most commonly used implant system was Zimmer Biomet (33.3%) followed by Stryker (10.6%) and Depuy (9.1%).
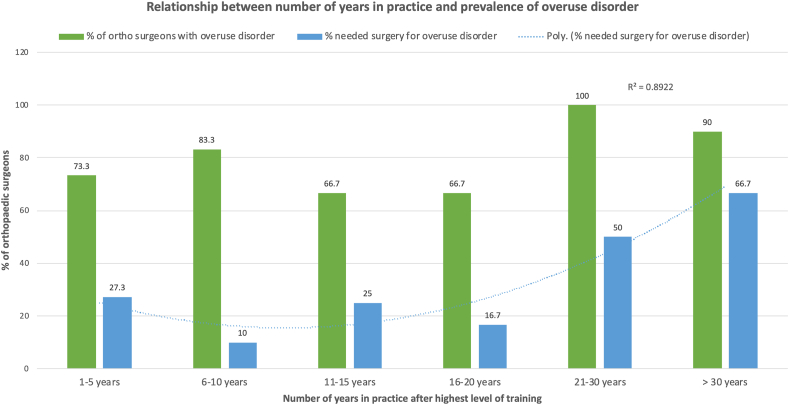
The relationship between number of years in practice and the prevalence of one of the abovementioned MSK overuse or other disorders was analyzed. The prevalence of an overuse disorder was highest for those who have been in practice for 21–30 years (100%), while it was lowest for those who have been in practice for 11–15 years (66.7%) or 16–20 years (66.7%). There was a non-linear, but positive correlation between the number of years in practice and rate of surgery for an overuse disorder (Fig. 2).
Fig. 2.
Relationship between number of years in practice and prevalence of MSK overuse or other medical disorders.
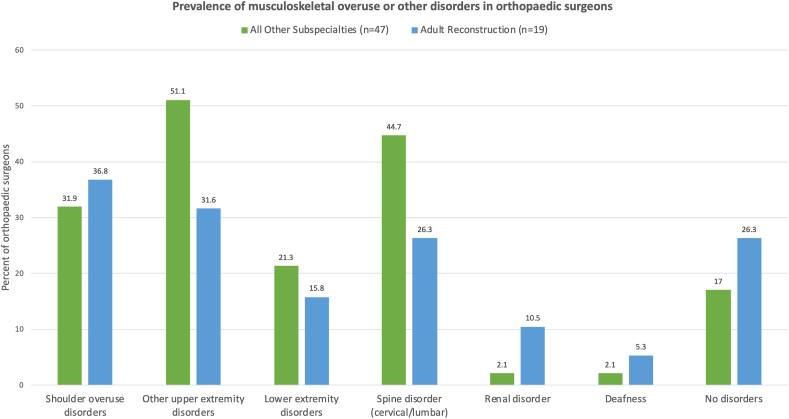
The survey participants were split into two groups for subgroup analysis: “Adult Reconstruction” if a majority of the participant's practice consisted of primary or revision TKA or THA and “All other subspecialties” if they performed some or no THA or TKA in their practice. There were 19 surgeons who fell into the Adult Reconstruction category and 47 orthopaedic surgeons in other subspecialties or practicing general orthopaedics. These two groups were compared in terms of the prevalence of type of overuse disorder, need for surgery for overuse disorder, and belief regarding their ability to meet their job demands. Shoulder overuse disorder—rotator cuff disease, biceps tendonitis, other tendonitis—was the most common MSK overuse condition to affect Adult Reconstruction surgeons while spine disorder (cervical or lumbar spine disease) was the most common MSK condition to affect orthopaedic surgeons in other subspecialties. The second most common MSK condition to affect both groups of surgeons was lateral epicondylitis. The average number of medical conditions affecting Adult Reconstruction surgeons was 2.16 (±1.92) and orthopaedic surgeons from other subspecialties was 2.04 (±1.81) (P-value = 0.8168). None of these differences in prevalence of different medical conditions among the two groups were statistically significant (Fig. 3).
Fig. 3.
Prevalence of MSK overuse or other disorders in orthopaedic surgeons.
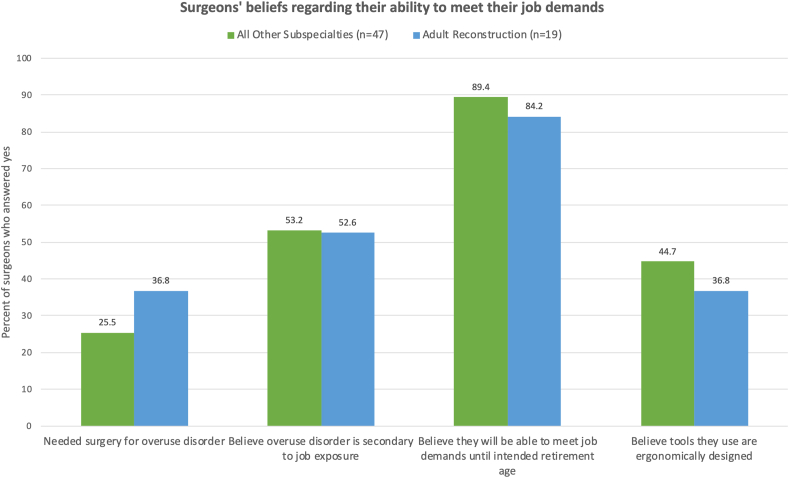
Although there was a trend toward higher rate of surgery for an overuse disorder among Adult Reconstruction surgeons (36.8%) compared to orthopaedic surgeons in other subspecialties (25.5%), there were no statistically significant differences in surgeons’ beliefs between the two groups regarding whether their overuse disorder was caused by on-the-job exposure, their ability to meet their job demands until intended retirement age, or whether they believe the tools they use are ergonomically designed (Fig. 4).
Fig. 4.
Orthopaedic surgeons' beliefs regarding their ability to meet their job demands till intended retirement age and other beliefs.
Subgroup analysis was performed to determine if orthopaedic surgeons who were performing certain procedures—a significant number of cases with anterior approach for THA (>25% of all THA cases), using computer navigation or robot for THA or TKA (>25% of all cases), and performing a significant amount of revision arthroplasty (>25% of all cases) as part of their practice—had a higher prevalence of overuse disorders compared to those who were not. Statistical analysis showed that there were no significant differences between these two subgroups in terms of prevalence of medical conditions or rate of surgery among Adult Reconstruction surgeons (Fig. 5, Fig. 6).
Fig. 5.
No relationship between use of anterior approach for THA, computer navigation, and amount of revision surgery done and prevalence of overuse disorders.
Fig. 6.
No relationship between use of anterior approach for THA, computer navigation, and amount of revision surgery done and percent who underwent surgery for overuse disorder.
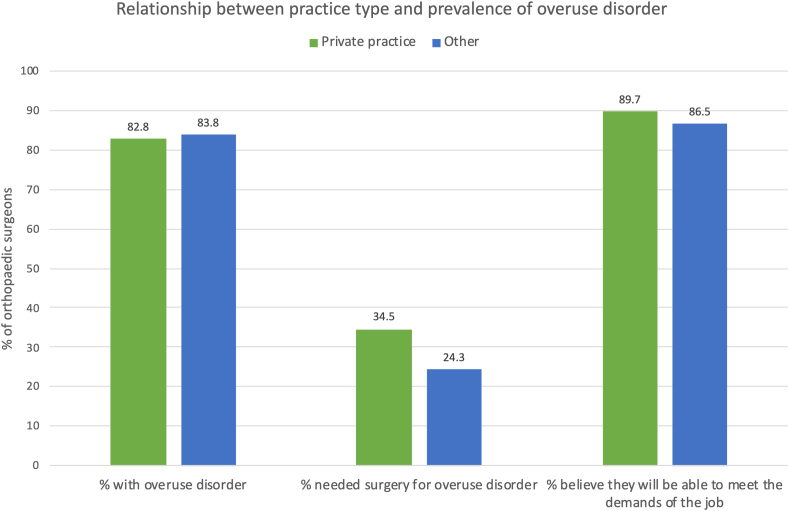
Subgroup analysis was performed to determine if there was any correlation between the type of practice setting and prevalence of overuse disorder. Survey respondents were divided into two groups: “private practice” (n = 29) and “other” (n = 37) consisting of academic tertiary care center, university-affiliated community hospital, and hospital-employed surgeons. The prevalence of overuse disorder, rate of surgery, and surgeon belief regarding ability to meet their job demands until intended retirement age were similar between both groups. There were no statistically significant differences between the two groups (Fig. 7).
Fig. 7.
Relationship between practice setting and orthopaedic surgeons' beliefs regarding job demands.
4. Discussion
The results of this cross-sectional study show that a majority (>80%) of orthopaedic surgeons suffer from a musculoskeletal overuse disorder, kidney stones, cataracts, infertility, deafness, or a combination of the above. A significant proportion (53%) of surgeons suffering from these medical conditions believe one or more of their medical conditions developed due to occupational exposure. There was also a non-linear but positive relationship between number of years in practice and rate of surgery for MSK disorder.
This study is the first to evaluate the occupational hazards related to Adult Reconstruction. The results showed that while there are no statistically significant differences between Adult Reconstruction surgeons and orthopaedic surgeons from other subspecialties, there was a trend toward higher rate of surgery among Adult Reconstructions surgeons suffering from an MSK disorder compared to other orthopaedic surgeons (36.8% vs 25.5%). Furthermore, while shoulder overuse conditions were the most common MSK disorders to affect Adult Reconstruction surgeons, other upper extremity conditions (e.g. lateral epicondylitis) and spine disease (cervical or lumbar) were the most common MSK disorders to affect other subspecialty orthopaedic surgeons. Adult Reconstructive surgeons reported higher incidence of rotator cuff disease, likely due to more strenuous overhead physical activity required of them during surgery (i.e. when impacting a tibial component in TKA or removing a femoral component in explant procedures). These results are different from the results of a similar study published by Al Qahtani et al. evaluating occupational hazards faced by orthopaedic trauma surgeons.6 In their cross-sectional study, Al Qahtani et al. found that the most common MSK disorder affecting orthopaedic trauma surgeons was low back pain (29.3%) followed by wrist/forearm tendonitis (17.4%). However, their results were similar to ours in that the surgeons’ type of practice (private practice vs other) had no effect on number of disorders or type of disorder present.
A limitation of this study is that the survey was sent to orthopaedic surgeons practicing in the Midwestern United States. There may be regional differences among surgeons across the country, and therefore the study results may not be generalizable to all orthopaedic surgeons. Another limitation is the small sample size of the study, which was limited by the low response rate from orthopaedic surgeons surveyed. This puts this study at risk for nonresponder bias. Furthermore, the survey questionnaire did not ask the participants regarding needlestick injuries and consequent HIV, HBV, or hepatitis C virus (HCV) seropositivity, as these questions were thought to be sensitive in nature and potentially would decrease the response rate. The study did not query respondents about exposures outside of work, which could be a confounding factor. However, the results from this study are valuable in that they underscore the need for increased awareness of occupational hazards associated with orthopaedic surgery. Our study also showed that a significant number of orthopaedic surgeons suffer from non-MSK disorders such as kidney stones, cataracts, infertility, or deafness. We hypothesize that these disorders may be the result of radiation exposure, long duration of surgery, and noise pollution during orthopaedic surgery. However, these risks need to be further investigated and will be the subject of study in a separate survey. Our results show that more robust, large-scale studies are warranted to determine the true prevalence of occupational hazards associated with orthopaedic surgery so that appropriate training can be provided to orthopaedic surgeons to mitigate some of the occupational exposures.
5. Conclusion
The results of this cross-sectional study show that a majority (>80%) of orthopaedic surgeons suffer from a musculoskeletal overuse disorder, kidney stones, cataracts, infertility, deafness, or a combination of the above. In this small sample size study, 53% of survey respondents suffering from these medical conditions believed one or more of their medical conditions may have developed due to occupational exposure. There was also a non-linear but positive relationship between number of years in practice and rate of surgery for MSK disorder.
Declaration of competing interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Andrew Glassman receives royalties from ExacTech, Inc.
References
- 1.Okoshi K., Kobayashi K., Kinoshita K., Tomizawa Y., Hasegawa S., Sakai Y. Health risks associated with exposure to surgical smoke for surgeons and operation room personnel. Surg Today. 2015;45:957–965. doi: 10.1007/s00595-014-1085-z. [DOI] [PubMed] [Google Scholar]
- 2.Choi S.H., Kwon T.G., Chung S.K., Kim T.H. Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc. 2014;28:2374–2380. doi: 10.1007/s00464-014-3472-3. [DOI] [PubMed] [Google Scholar]
- 3.Chou L., Reynolds M.R., Esterhai J.L., Jr. Hazards to the orthopaedic trauma surgeon: occupational exposure to HIV and viral hepatitis (a review article) J Orthop Trauma. 1996;10:289–296. doi: 10.1097/00005131-199605000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Green S.E., Gompertz R.H. Glove perforation during surgery: what are the risks? Ann R Coll Surg Engl. 1992;74:306–308. [PMC free article] [PubMed] [Google Scholar]
- 5.Lester J.D., Hsu S., Ahmad C.S. Occupational hazards facing orthopedic surgeons. Am J Orthop (Belle Mead NJ) 2012;41:132–139. [PubMed] [Google Scholar]
- 6.AlQahtani S.M., Alzahrani M.M., Harvey E.J. Prevalence of musculoskeletal disorders among orthopedic trauma surgeons: an OTA survey. Can J Surg. 2016;59:42–47. doi: 10.1503/cjs.014415. [DOI] [PMC free article] [PubMed] [Google Scholar]