Abstract
Recently published data indicates that high ivermectin (IVM) concentrations suppress in vitro SARS-CoV-2 replication. Nasal IVM spray administration may contribute to attaining high drug concentrations in nasopharyngeal tissue, a primary site of virus entrance/replication. The safety and pharmacokinetic performances of a novel IVM spray formulation were assessed in a pig model. Piglets received IVM either orally (0.2 mg/kg) or by one or two nasal spray doses. The overall safety, and histopathology of the IVM-spray application site tissues, were assessed. The IVM concentration profiles measured in plasma and respiratory tract tissues after the nasal spray were compared with those achieved after the oral administration. Animals tolerated well the nasal spray formulation. No local/systemic adverse events were observed. After nasal administration, the highest IVM concentrations were measured in nasopharyngeal and lung tissues. The nasal/oral IVM concentration ratios in nasopharyngeal and lung tissues markedly increased by repeating (12 h apart) the spray application. The fast attainment of high and persistent IVM concentrations in nasopharyngeal tissue is the main advantage of the nasal over the oral route. These original results support the undertaking of future clinical trials to evaluate the safety/efficacy of the nasal IVM spray application in the prevention and/or treatment of COVID-19.
Keywords: Ivermectin, Covid 19, Nasal-spray formulation
Introduction
Ivermectin (IVM) [a mixture of 22, 23-dihydro-avermectin B1a (80%) and 22, 23-dihydro-avermectin B1b (20%)], is a macrocyclic lactone, discovered in 1975 by Satoshi Omura as a fermentation product of the actinomycete Streptomyces avermitilis and developed in the early eighties to treat parasitic diseases. Its high lipophilicity and efficacy allow its use through different routes, being effective to control endo and ecto-parasites in animals and humans. Shortly after its introduction in the veterinary market, the drug was approved for human use. Nowadays, after decades of intensive, safe and effective use, IVM is indicated to treat several neglected tropical diseases, including onchocerciasis, helminthiases, and scabies. It had also been evaluated for its potential to reduce the rate of malaria transmission by killing mosquitoes.1 Overall, IVM has been widely used, demonstrating an excellent safety profile. Additionally, in the last few years, new knowledge guided the repurposing of the drug towards the treatment of other diseases. IVM antibacterial,2 antiviral3 and antimitotic activities4, 5, 6 have been experimentally observed.
IVM antiviral activity against Dengue virus,3 West Nile virus,7 Venezuelan Equine Encephalitis virus,8 and Influenza virus,9 has been reported. Recently, Caly et al.10 reported that IVM inhibits in vitro the replication of SARS-CoV-2 (severe acute respiratory syndrome coronavirus) using high concentrations in the range of 2.5–5 μM. The mechanism by which IVM inhibits SARS-CoV-2, seems to be the same described for other RNA viruses, i.e. inhibition of transport across the nuclear membrane mediated by importin α/β1 heterodimer, carrier of some viral molecules indispensable for the replication process.11 , 12 Furthermore, there is now available information from randomized clinical trials, on IVM favourable effects in SARS-CoV-2 infected patients.13, 14, 15
SARS-CoV-2 is the etiological agent of Covid-19, a viral infection causing a pandemic since December 2019, inducing from asymptomatic to life-threatening disease. It is highly transmissible with a primary respiratory entrance and airborne transmission, which explains its extensive distribution worldwide. The information available to date indicates that SARS-CoV-2 colonizes the oropharynx and nasopharynx, from where transmission begins even before the appearance of any symptoms. With viral replication in this area,16 the first symptoms (odynophagia, anosmia, dry cough, fever) and lung parenchyma colonization appear. In the context of the current Covid-19 pandemic, it is relevant to determine the best way to administer IVM to optimise its potential in vivo therapeutic usefulness.
The IVM pharmacokinetic features, based on high lipophilicity and a large volume of distribution, allow its high availability in the respiratory tract.17 , 18 Thus, considering the gateway of the virus, the administration of a nasal IVM spray (N-IVM spray) intended to deposit the drug in the upper respiratory tract, could represent a practical tool to expose the of SARS-CoV-2 virus (or the cells where the viral particles are located) to high IVM concentrations. Hence, a reduction of the viral load at the early stage of the infection, preventing viral replication, transmission and disease aggravation might be achieved.
Only limited information on inhaled IVM is available19 and a nebulized IVM has been recently tested in rats.20 In an attempt to attain high IVM concentrations in tissues where the entry and initial transmission of SARS-CoV-2 occurs (where a large viral load is found at the early stages of the infection), the main goal of the work described here was to assess the safety and pharmacokinetic performances of a novel IVM spray formulation for intranasal administration in piglets. The IVM concentration profiles measured in plasma, nasopharyngeal and lung tissues after the intranasal treatment (one and two applications 12 h apart) were compared with those achieved in the same tissues after the oral (tablets) administration of the antiparasitic dose of 0.2 mg/kg approved for human use.
Material and Methods
Study Formulations
N-IVM spray formulation, N-IVM-free methylene blue coloured spray formulation, IVM tablets 2.0 mg and IVM tablets 0.5 mg were developed, manufactured and quality controlled according to Good Manufacturing Practices and supplied by Laboratorio Elea-Phoenix, Argentina. The N-IVM spray was designed to deliver 1 mg IVM, in a 0.1 mL puff. The accuracy of the dose delivered by the device was tested. Each container provides 100 puffs and calibrated microdroplets to produce a high tissue deposit in the nasopharyngeal area. The device was prepared in a 19 mL plain base aluminium can with a 100 μL inverted metering valve and a white polyethylene nasal actuator. The composition of the nasal spray and oral tablet formulations used in the current trials is as follows.
| Composition | Nasal spray (quantity/dose) | Oral tablets (mg/tablet) |
|
|---|---|---|---|
| 2 mg tablet | 0.5 mg tablet | ||
| Ivermectin | 1.00 mg (micronized) | 2.00 mg | 0.50 mg |
| Ethanol absolute | 18.35 mg | – | – |
| Oleic acid | 0.055 mg | – | – |
| Propellant 134 a Pharma q.s. | 100.00 μL | – | – |
| Lactose monohydrate | – | 11.00 mg | 11.00 mg |
| Sodium starch glycolate | – | 2.00 mg | 2.00 mg |
| Cellactose 80 | – | 80.00 mg | 81.50 mg |
| Talc | – | 3.00 mg | 3.00 mg |
| Magnesium stearate | – | 2.00 mg | 2.00 mg |
Experimental Animals
Forty healthy Landrace-Duroc Jersey-Yorkshire crossbred piglets (weighing 11.2 ± 0.52 kg)kg) were used. The animals were housed in the farm of origin. They were kept with the usual diet during the trial (antibiotic-free diet) and ad libitum access to water. Management and euthanasia of the animals were performed according to approved Good Veterinary Practices21 and Principles of Animal Welfare.22 The study was fully performed in compliance with ethical, animal procedures and management protocols approved by the Ethics Committee on Animal Welfare Policy of Biogenesis Bago, Argentina (Pol-UE 0001), and by the Animal Welfare Policy (act 087/02) of the Faculty of Veterinary Medicine, Universidad Nacional del Centro de la Provincia de Buenos Aires (UNCPBA), Tandil, Argentina (protocol number 12/2020).
Pre-Trial
A pre-trial with the N-IVM-free coloured spray was performed in two animals to assure that the target tissue areas were properly covered after one dose application and to determine the sampling methodology for nasopharyngeal tissue, based on the observation of colorant presence. The device and composition of the IVM-free nasal spray was identical to that described in 2.1. and 2.1.1. with the inclusion of 1 mg methylene blue.
Study Design
The animal phase of the study was conducted at an intensive pig farming establishment (“El Campito”, SieteBochos S.R.L., Buenos Aires, Argentina). Clinical laboratory evaluations were performed at Microdiag Laboratory, La Plata, Argentina. The tissue histopathological evaluations, drug analysis and pharmacokinetic evaluation were performed at Centro de Investigación Veterinaria de Tandil (CIVETAN), UNCPBA-CICPBA-CONICET, Tandil, Argentina.
The experimental design was based on a three-group animal phase study. Group 1 (22 animals) received one dose (2 mg, 1 puff/nostril) of N-IVM-spray, Group 2 (10 animals) received two (2 mg each, 1 puff/nostril) doses N–IVM-spray 12 h apart, and animals in Group 3 (8 animals) were treated with IVM (0.2 mg/kg) oral tablets. Animal's selection was weight-based (approximately 10 kg body weight) to allow an equivalent total standard-dose treatment for one N-IVM administration (2 mg) and one dose oral (0.2 mg/kg) treatment.
Safety Assessment of the N-IVM Spray Formulation
The overall safety and local tissue tolerability of the N-IVM spray formulation were assessed. The IVM-treated animals were monitored by a careful clinical examination. Vital signs, haematological/serum biochemistry analysis and histopathology of tissues at the drug application area were assessed. All the experimental animals were carefully monitored for adverse effects throughout each dosing period.
During the first 6 h after administration and then at 12 and 24 h careful clinical control was performed, looking for any signs of ivermectin-induced neurotoxicity, nasal or respiratory discomfort, abnormal behavior, the appearance of the stool, feed and water consumption. Immediately after each drug administration and at 2, 6, 12 and 24 h after treatment, physical/visual examination of the application sites was performed. External and internal mouth inspection was performed to determine any possible adverse effect, which included visual observation of any possible abnormal manifestation in the epithelium of the nasopharynx as a consequence of the N-IVM spray application.
Clinical Laboratory Evaluation
Blood samples were collected at baseline (before treatment) (12 samples) and 24 h after single-dose (6 samples) and double-dose (6 samples) treatments to perform the hematologic and serum biochemical analysis. Hematology included measurements of hematocrit, red blood cell count, hemoglobin, mean corpuscular volume (MCV), mean corpuscular hemoglobin (HCM), mean-corpuscular hemoglobin concentration (MCHC) and counts of leukocytes, band neutrophils, segmented neutrophils, eosinophils, basophils, lymphocytes, monocytes and platelets. Serum concentrations of urea, creatinine, and the activities of alanine aminotransferase (ALT), aspartate aminotransferase (AST) and alkaline phosphatase (ALP) enzymes were determined.
Histopathological Study
Nasopharynx and oropharynx epithelia were carefully examined post-mortem for assessing possible macroscopic abnormalities induced by the N-IVM spray application. Samples of nasopharyngeal tissue from the soft palate region were obtained at 24 h post-administration of the N-IVM spray formulation (animals receiving one or two intranasal applications) to perform the histopathological assessment.
Blood, Nasopharyngeal and Lung Tissues Sampling for Drug Measurement
Four (4) animals from each of the experimental groups were randomly selected to be euthanized at each sampling time following approved animal guidelines. The head of the animals was opened following a sagittal line, the nasal septum removed and discarded, and a scrape of nasopharyngealmucosa, submucosa, turbinates and soft palate were integrated to form the nasopharynx-tissue sample. After opening the chest, a portion of the upper lobe of the right lung was obtained.
Following a single dose of the IVM nasal spray administration (Group 1), samples of blood, nasopharynx and lung tissue were collected at 2, 6, 12 and 24 h post-dosing to measure IVM concentrations. After the double dose IVM spray administration (Group 2), samples of blood, nasopharyngeal and lung tissues were taken at 6 and 24 h post administration of the second dose to evaluate potential IVM accumulation. After the single oral administration (Group 3), samples of the same tissues were collected at 6 and 24 h post-dosing. Plasma was separated by centrifugation at 2500 rpm for 15 min. The plasma and collected tissue samples were placed into plastic tubes and frozen at −20 °C until analysis by High Performance Liquid Chromatography (HPLC).
Analytical Development. Measurement of IVM Tissue Concentration Profiles
Concentrations of IVM in nasopharynx, lung and plasma samples were determined by HPLC with fluorescence detection following the technique previously described.17 An aliquot of plasma and tissues were homogenized and combined with moxidectin as an internal standard. Full validation of the analytical procedures used to measure IVM concentrations in the different tissues was performed. After acetonitrile-mediated chemical extraction, IVM was converted into a fluorescent molecule using N-methylimidazole and trifluoroacetic anhydride (Sigma Chemical, St Louis, MO, USA). An aliquot (100 μL) of this solution was injected directly into the HPLC system (Shimadzu Corporation, Kyoto, Japan). The determination coefficients (r2) of the calibration curves for the different tissues analysed ranged between 0.989 and 0.999. The mean absolute drug recovery percentages were 94% (nasopharyngeal tissue), 86% (lung tissue) and 97% (plasma). The relative error values (accuracy) was in the range between 2.9% and 9.4%. The method exhibited a high degree of inter-day precision with a coefficient of variation below 7%. The limits of drug detection were 0.45 ng/g (nasopharyngeal tissue), 0.19 ng/g (lung) and 0.20 ng/mL (plasma). The limits of quantification (LOQ) were 0.70 ng/g (nasopharyngeal tissue), 0.30 ng/g (lung) and 0.34 ng/mL (plasma). Concentration values below the quantitation limits were not considered for the pharmacokinetic analysis.
Pharmacokinetic and Statistical Analysis of the Data
The IVM concentration versus time curves obtained for each tissue/fluid after each experimental treatment were fitted with the PK Solutions 2.0 (Ashland, Ohio, US) computer software. The area under the concentration-time curves (AUC) was calculated by the trapezoidal rule23 to determine the IVM exposure (tissue availability) at each assayed tissue. The statistical analysis was performed using the Instat 3.0 software (GraphPad Software, CA, US). IVM concentrations after the different treatments were statistically compared using a non-parametric Kruskal-Wallis test. The data from the hematological and biochemical determinations were compared by basic statistical analysis using the Info Stat, 2016 software.
Results
Spray Formulation Features
The novel developed nasal IVM spray formulation was designed to attain high drug concentrations in nasopharyngeal tissue, a primary site of virus entrance/replication. The N-IVM spray was designed to deliver 1 mg IVM, in a 0.1 mL puff with calibrated microdroplets to produce a high tissue deposit in the nasopharyngeal area. The delivery performance of the device was adequate. The use of a drug free coloured spray (pre-clinical trial) was very useful to assure that the target tissue areas were properly covered after one dose application as well as to determine the sampling methodology to collect the appropriate nasopharyngeal tissue for drug measurement. The coloured spray permitted the confirmation of the homogeneous distribution of the formulation along the nasal epithelium, turbinates, nasal septum, nasopharynx and pharynx of the experimental animals. The appropriate delivery performance and the fast attainment of a nasopharyngeal tissue deposit are well supported by the IVM concentration profiles recovered in the nasopharyngeal anatomical area following the spray application.
Safety Assessment
The N-IVM spray was well tolerated after either one or two applications to the animal model. The piglets were considered clinically healthy by specialised veterinarians throughout the whole experimental trial. No signs of ivermectin-induced neurotoxicity were observed. All had normal skin and mucous membranes color, body condition and behaviour activity. No adverse events or intolerance were evident along the whole study period in animals treated either orally or with the spray formulation once or twice.
There were no macroscopic changes at the tissue area of spray application at different examination times. Furthermore, no histopathological changes (lesions) were observed in the mucosa or submucosa of the soft palate in spray-treated animals. A mild to moderate inflammation was observed in the tonsils (both before and after spray application), which is normal in pigs because of the immunological role of the area. The serum biochemical and hematological values did not show any alteration that would lead to adverse effects. Range values for hematological and biochemical determinations before and after the administration of the N-IVM spray formulation are summarized in Table 1 .
Table 1.
Haematological and Serum Biochemical Range Values Obtained in Experimental Pigs Before and After the Treatment With Either One or Two Doses of the N-IVM Spray Formulation.
| Hematology | Unit | Pre-Treatment | Post-Treatment |
|
|---|---|---|---|---|
| 1 Dose | 2 Dose | |||
| RBC | m/μL | 5.6–7.0 | 5.3–7.1 | 5.5–6.4 |
| HGB | g/dL | 9–12 | 8.4–11 | 9–11.5 |
| WBC | /μL | 11,700–27000 | 9300–25900 | 15,500–27300 |
| Neutrophils | /μL | 4329–16055 | 3534–17395 | 7130–15288 |
| Eosinophils | /μL | 0–1080 | 0–1554 | 0–1204 |
| Basophils | /μL | 0 | 0 | 0 |
| Lymphocytes | /μL | 5518–11520 | 3990–9842 | 4347–10374 |
| Monocytes | /μL | 438–2070 | 490–1881 | 688–1638 |
| Platelets | /μL | 283–500 | 353–470 | 303–407 |
| Serum biochemistry | ||||
| Urea | g/L | 0.13–0.30 | 0.15–0.24 | 0.10–0.20 |
| Creatinine | mg/dL | 1.00–1.35 | 0.90–1.17 | 0.90–1.10 |
| GOT (AST) | U/L | 47–74 | 34–120 | 32–67 |
| GPT (ALT) | U/L | 57–98 | 58–92 | 60–103 |
RBC: red blood cell counts, HGB: hemoglobin, WBC: white blood counts.
AST: aspartate aminotransferase ALT: alanine aminotransferase.
The dataexpress range values obtained for each parameter in all the animals in each experimental Groupbefore and after treatment. No statistically significant differences (P > 0.05) were observed between pre- and post-treatment values for any of the studied parameters.
Pharmacokinetic Assessment
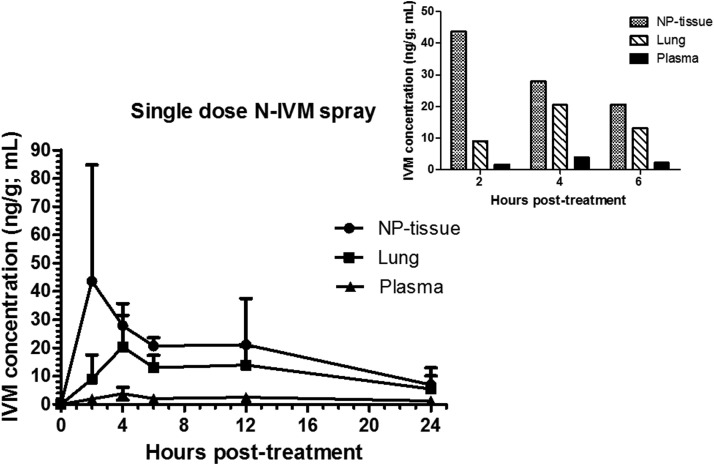
IVM was recovered in plasma, nasopharyngeal and lung tissues following a single dose application of the N-IVM-spray formulation (Group 1). Although some degree of variability was observed in the patterns of tissue concentration among the animals treated with the spray formulation, the highest IVM concentrations were always measured in nasopharyngeal tissue. Additionally, high IVM concentrations were measured in lung tissue, with a limited passage into the central compartment (systemic absorption), reflected in the low plasma levels recovered in the animals treated with N-IVM spray. The comparative IVM concentration profiles in nasopharyngeal tissue, lung and plasma obtained over the first 24 h post-administration (one dose) of the N-IVM spray formulation, are shown in Fig. 1 .
Fig. 1.
Mean ivermectin (IVM) concentration profiles in nasopharyngeal (NP) tissue, lung and plasma following administration of one intranasal (N-IVM-spray) dose to piglets. The insert shows the comparative IVM concentrations obtained between 2 and 6 h post spray administration.
A significant positive correlation between the IVM concentrations in nasopharyngeal and lung tissues (r = 0.735) was observed between the 4 h and 24 h post-administration. The IVM exposure (measured as AUC values) was calculated for each of the assayed tissues and plasma. The highest drug exposure after the one dose nasal application was observed at the nasopharynx and lung tissue. The drug availability (exposure) expressed as AUC values in each tissue and the relationship (ratio) between IVM exposure in lung and plasma compared to nasopharyngeal tissue are shown in Table 2 .
Table 2.
Ivermectin (IVM) Exposure (availability) Expressed as AUC Values in Nasopharyngeal (NP) Tissue, Lung Tissue and Plasma Following Administration of One N-IVM-Spray Dose.
| IVM Exposure (Mean AUC Values) | Relationship with NP Exposurea | |
|---|---|---|
| NP tissue | 457 ng h/g | – |
| Lung Tissue | 268 ng h/g | 0.59 |
| Plasma | 49.5 ng h/mL | 0.11 |
Drug exposure (AUC) ratios in lung/NP tissues and plasma/NP tissue.
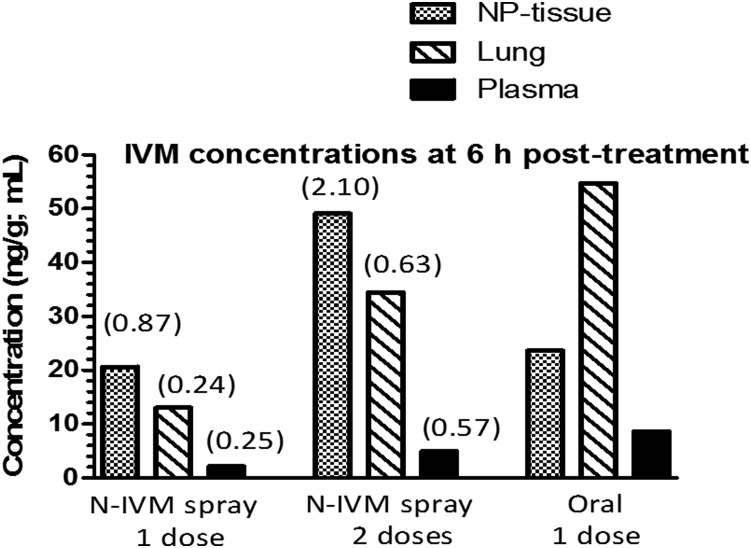
IVM concentrations were also measured following the two doses of N-IVM-spray administration as well as after the single oral tablets administration to pigs. The repeated spray treatment increased significantly the IVM concentrations in nasopharynx and lung tissues compared to those measured after the single intranasal administration, without any significant increment on IVM concentrations in the bloodstream, which reflects a limited IVM systemic absorption. These results confirm the hypothesis that a high IVM availability in the nasopharyngeal tissue area is achieved following the nasal spray administration. The high nasopharyngeal IVM exposure after the nasal spray treatment was confirmed by the observed nasopharyngeal tissue to plasma concentration ratios. At 6 h post-treatment, this ratio was significantly higher (P < 0.05) after the nasal spray application compared to the oral administration. Besides, a high distribution of IVM was observed after its oral administration, with higher lung concentration profiles compared to those in the nasopharyngeal tissue measured at 6 h post-treatment. The comparative mean IVM concentrations in each tissue after the three experimental treatments are shown in Table 3 . The ratios of nasopharyngeal tissue to plasma concentrations measured at 6 and 24 h post-treatment, are shown in Table 4 .
Table 3.
Mean (±SD) Comparative Ivermectin (IVM) Concentrations Measured in Nasopharyngeal Tissue, Lung Tissue and Plasma at 6 and 24 h After its Intranasal (N-IVM Spray) (As One and Two Applications) and Oral Administration to Piglets.
| IVM Concentration (ng/g; ng/mL) |
|||
|---|---|---|---|
| N-IVM spray (one 2 mg dose) | N-IVM spray (two 2 mg doses, 12 h apart) |
Oral (one 0.2 mg/kg dose) | |
| Nasopharyngeal | |||
| 6 h | 20.7 ± 2.92a | 49.1 ± 18.7b | 23.6 ± 10.8a |
| 24 h |
6.96 ± 6.01a |
10.9 ± 7.58a |
13.0 ± 5.33a |
| Lung tissue |
|||
| 6 h | 13.0 ± 4.38a | 34.4 ± 10.2b | 54.7 ± 14.0c |
| 24 h |
5.42 ± 4.69a |
13.0 ± 9.41a |
25.4 ± 10.3b |
| Plasma |
|||
| 6 h | 2.13 ± 0.50a | 4.95 ± 2.92ab | 8.60 ± 3.39b |
| 24 h | 1.20 ± 1.04a | 3.37 ± 2.61b | 3.65 ± 0.88b |
Different letters in each row indicate statistically significant differences at P < 0.05. The statistical analyses compares the IVM concentrations measured after N-IVM -spray (one and two doses) and oral treatments for each tissue at the different time sampling points.
Table 4.
Mean (±SD) Comparative Ratios of Nasopharyngeal to Plasma IVM Concentrations Measured at 6 and 24 h after its Intranasal (N-IVM Spray) (As One and Two Applications) and Oral Administrations to Piglets.
| Ratios of Nasopharyngeal to Plasma Concentrations |
|||
|---|---|---|---|
| N-IVM spray (one 2 mg dose) | N-IVM spray (two 2 mg doses, 12 h apart) | Oral (one 0.2 mg/kg dose) | |
| 6 h | 10.3 ± 3.69a | 11.0 ± 4.22a | 2.74 ± 0.60b |
| 24 h | 6.47 ± 3.67a | 4.59 ± 3.02a | 3.64 ± 1.40a |
Different letters in each row indicate statistically significant differences at P < 0.05. The statistical analyses compares the IVM concentrations measured after N-IVM -spray (one and two doses) and oral treatments for each tissue at the different time sampling points.
The relationship between IVM concentrations recovered at 6 h in both target tissues (nasopharynx and lung) following the spray application was estimated, using the oral tablet administration as a reference. The spray/oral concentration relationship in nasopharyngeal tissue increased significantly from 0.88 (one spray application) to 2.10 (two spray applications). The same spray/oral ratio increased from 0.24 to 0.63 in lung tissue. A less marked increase in the spray/oral ratio was observed in plasma (from 0.25 to 0.57), as it can be observed in Fig. 2 .
Fig. 2.
Comparative ivermectin (IVM) concentrations in nasopharyngeal (NP) tissue, lung and plasma measured at 6 h after the oral and N-IVM-spray (one and two doses) treatments. The spray to oral IVM concentration ratios (values in brackets) are shown for each of the target tissues/plasma.
Discussion
The pig was chosen as the test animal model to assess the safety, application site tolerability and kinetic performance of the new formulation and innovative route of IVM administration. There are strong evidences to consider the pig as the most adequate animal model to assess this novel spray formulation intended for human use. Pigs and humans have anatomical and physiological similarities. The pig is the animal species most used in translational research in studies of pathophysiology, cardiovascular and gastrointestinal surgery, preclinical toxicological testing of pharmaceuticals, and lately for the understanding of the anatomy of the respiratory system and training in lung transplantation.24
The work reported illustrates the safety and pharmacokinetic assessments of a novel pharmaceutical formulation aimed to attain high IVM concentrations in nasopharynx and lungs with low systemic availability. The appropriate delivery performance of the novel spray preparation reaching tissues (nasal epithelium, nasal septum, nasopharynx) identified as primary sites of virus entrance/replication, and the fast attainment of a nasopharyngeal tissue IVM deposit, are key findings emerging from the work described here. The overall assessment of an IVM spray formulation in a pig model, measuring the IVM concentration profiles attained in the nasopharyngeal anatomical area, is described for the first time.
Considering the well known safety of IVM at several times the therapeutic doses orally and/or parenterally administered both in animals and humans, the intranasal administration of 1 mg in each nostril could be “a priori” considered as completely safe. However, the intranasal administration has some particularities that turns it unique in comparison to other routes of drug administration. The most serious IVM toxicity may be related to its penetration into the central nervous system, and considering that the nose-to-brain delivery of drugs can bypass the blood-brain barrier, the safety assessment following intranasal IVM administration was a primary goal in the current trial. There was a need to rule out any risk of acute IVM neurotoxicity after the intranasal administration. The nasal IVM spray was shown to be safe and well tolerated. The absence of any sign of neurotoxicity after the application of the nasal spray was a first relevant safety-related finding. Neither clinical adverse effects, haematological, serum biochemical nor histopathological changes on the tissue area of drug application, were observed in intranasally treated animals.
The work reports original data on IVM concentration profiles on nasopharyngeal tissue after an intranasal and oral administration in a pig animal model. While the repetition of the intranasal dose at a 12 h interval determined a significant increase in IVM concentrations in nasopharynx and lungs, both identified as target tissues for SARS-CoV-2, only minimal drug systemic exposure (low plasma levels) was observed. After 0.2 mg/kg oral tablet administration, IVM plasma concentration levels were in agreement with those previously published for piglets.25 , 26 IVM was well absorbed and extensively distributed, resulting in higher concentrations in lung tissue than in plasma (see Fig. 2), a pattern already observed in cattle subcutaneously treated with IVM,17 and confirmed by a recent pharmacokinetic simulation report looking at IVM lung exposure in humans. Using a minimal physiological pharmacokinetic model, this work establishes that a lung mean concentration as high as 193 ng/g may be achieved after a single oral treatment of 30 mg18 The high IVM nasopharyngeal exposure obtained after the spray application was well reflected by the nasopharynx/plasma concentration ratio, which was significantly higher than that observed after the oral dosing at 6 h post-treatment (Table 4).
The variability observed among treated animals on the patterns of IVM concentration in nasopharyngeal and lung tissues may be related to the fact that it is not possible to control the ventilator state of the animals at the moment of the spray drug application. As a consequence, some animals could have different degrees of inspiration during the spray administration, which may help to understand individual variation on drug concentrations measured both in nasopharynx and lungs. The situation could be different if this type of IVMspray preparation is used by humans, since the user could be instructed to slightly inspire or remain in apnea, with a predictable increase in drug penetration into the respiratory tree achieving higher lung drug concentrations.
There is now recently published evidence on the efficacy of IVM against SARS-CoV-2, using oral treatments at different dose rates. IVM treatment has now been associated with lower mortality during treatment of Covid-19.13 Additionally, early treatment promotes faster viral clearance during disease.14 We have also recently demonstrated a concentration-dependent IVM effect on the viral clearance in a controlled clinical trial in Covid-19 infected patients.15 Furthermore, in addition to the therapeutic effect of IVM in infected patients, it was recently shown the potential preventive effect of IVM in SARS-CoV-2 transmission.27 The scientific evidence of the in vivo effects of IVM on reducing the SARS-CoV-2 viral load gives prominence to the data on the assessment of the spray formulation in a pig model described here, as well as to the potential usefulness of nebulized IVM has recently been described in rats.20
It may be expected that repeated intranasal administration increases IVM concentrations in the nasopharynxarea and lungs. As a low systemic absorption was observed, and considering the intrinsic safety of the drug, there would be no anticipated significant risks of IVM systemic toxicity after repeated nasal administration. Compared to the oral administration, the intranasal administration in humans may provide fast, high and persistent IVM concentration at the nasopharynx area at much lower doses. For instance, in a 60 kg body weight person, higher IVM concentrations in nasopharyngeal tissue may be attained with 4 mg intranasally (2 spray doses 12 h apart) than giving 12 mg orally (1 dose 0.2 mg/kg). Thus, the daily administration of one puff in each nostril to health workers would allow the persistence of high IVM concentrations in nasopharyngeal epithelium during an entire working period.
Even with some limitations related to the reduced number of animals, difficulties to obtain extra sampling points and further safety characterization after several spray applications, the data reported here constitutes a solid novel contribution to the repurposing of IVM as an antiviral compound. Next steps are related to the design and execution of future clinical trials in humans to confirm safety, particularly after application of several intranasal doses, and to determine the efficacy of the developed IVM spray formulation. This could include recently diagnosed Covid-19 patients, their close contacts, and/or a preventive usage in health workers. Based on the pharmacokinetic data shown here, the administration of more than one puff per nostril a day would allow IVM accumulation in nasopharyngeal tissue, reaching a local drug exposure not feasible to be achieved by the oral route. In the same direction, further research is also needed to evaluate the potential advantages of a combined nasal plus oral treatment regimen to further contribute to IVM repurposing in Covid-19 therapy.
Funding
The work described here was mainly supported by funding from Laboratorio Elea Phoenix, Argentina. The Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), Argentina, The Facultad de CienciasMédicas de la Universidad Nacional de La Plata, Argentina, and INCAM S.A. partially contributed through payment of salaries for several of the authors in this article. The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Author Contributions
J. Errecalde. Protocol design, IVM spray design. Animal phase work (Spray administration and sampling). Data analysis. Overall integration/discussion of the data. Manuscript writing. A. Lifschitz. Protocol design. HPLC analysis. PK data analysis. Overall integration/discussion of the data. Manuscript writing. G. Vecchioli. Protocol design. Data analysis. Overall integration/discussion of the data. Manuscript writing. L. Ceballos. Analytical development. Method validation. HPLC analysis. Data integration. F. Errecalde. Animal phase work (treatments/sampling). M. Ballent. Analytical development. Method validation. G. Marín. Dosage calculation. Manuscript's revision. M. Daniele. Animal phase work (treatments/sampling). E. Spitzer, F. Toneguzzo, S. Gold., Protocol Design. Pharmaceutical Spray development. Regulatory Discussion. Overall Integration/analysis/discussion of the data. A. Krolewiecki. Protocol design. Overall integration/discussion of the data. L. Alvarez. Protocol design. Overall discussion of the data. Manuscript writing. C. Lanusse. Protocol design. Overall integration/discussion of the data. Manuscript writing.
Acknowledgements
The authors wish to thank all those collaborators (at each of the involved institutions) who have anonymously contributed with the execution of the work reported here.
Footnotes
J. Errecalde and A. Lifschitz equally contributed to this work.
References
- 1.Campbell W.C. Ivermectin and malaria-putting an elderly drug to a new test. Am J Trop Med Hyg. 2020;102:1. doi: 10.4269/ajtmh.19-0889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lim L.E., Vilchèze C., Ng C., Jacobs W., Jr., Ramón-García S., Thompson C. Anthelmintic avermectins kill Mycobacterium tuberculosis, including multidrug-resistant clinical strains. Antimicrobial Agents Chemother. 2013;57:1040–1046. doi: 10.1128/AAC.01696-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tay M.Y., Fraser J.E., Chan W.K. Nuclear localization of dengue virus (DENV) 1-4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor IVM. Antiviral Res. 2013;99:301–306. doi: 10.1016/j.antiviral.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Ashraf S., Prichard R. IVM exhibits potent antimitotic activity. Vet Parasitol. 2016;226:1–4. doi: 10.1016/j.vetpar.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Juarez M., Schcolnik-Cabrera A., Dueñas-Gonzalez A. The multitargeted drug IVM: from an antiparasitic agent to a repositioned cancer drug. Am J Cancer Res. 2018;8:317–331. [PMC free article] [PubMed] [Google Scholar]
- 6.Intuyod K., Hahnvajanawong C., Pinlaor P., Pinlaor S. Anti-parasitic drug IVM exhibits potent anticancer activity against gemcitabine-resistant cholangiocarcinoma in vitro. Anticancer Res. 2019;39:4837–4843. doi: 10.21873/anticanres.13669. [DOI] [PubMed] [Google Scholar]
- 7.Yang S.N., AtkinsonSC, Wang C. The broad spectrum antiviral IVM targets the host nuclear transport importin α/β1 heterodimer. Antiviral Res. 2020;177:104760. doi: 10.1016/j.antiviral.2020.104760. [DOI] [PubMed] [Google Scholar]
- 8.Lundberg L., Pinkham C., Baer A. Nuclear import and export inhibitors alter capsid protein distribution in mammalian cells and reduce Venezuelan Equine Encephalitis Virus replication. Antiviral Res. 2013;100:662–672. doi: 10.1016/j.antiviral.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Götz V., Magar L., Dornfeld D. Influenza A viruses escapes from MxA restriction at the expense of efficient nuclear vRNASOPHARYNX import. Sci Rep. 2016;6:23138. doi: 10.1038/srep23138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caly L., Druce J., Catton M., Jans D.A., Wagstaff K.M. The FDA-approved Drug IVM inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. 2020;178:104787. doi: 10.1016/j.antiviral.2020.104787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagstaff K.M., Rawlinson S.M., Hearps A., Jans D.A. An AlphaScreen(R)-based assay for high-throughput screening for specific inhibitors of nuclear import. J Biomol Screen. 2011;16:192–200. doi: 10.1177/1087057110390360. [DOI] [PubMed] [Google Scholar]
- 12.Wagstaff K.M., Sivakumaran H., Heaton S.M., Harrich D., Jans D.A. IVM is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus. Biochem J. 2012;443:851–856. doi: 10.1042/BJ20120150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cepelowicz Rajter J., Sherman M.S., Fatteh N., Vogel F., Sacks J., Rajte J.J. Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: the ICON study. Chest. 2020 doi: 10.1016/j.chest.2020.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed S., Karim M.M., Ross A.G. A five day course of ivermectin for the treatment of COVID-19 may reduce the duration of illness. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.11.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krolewiecki A., Lifschitz A., Moragas M. Antiviral effect of high-dose ivermectin in adults with COVID-19: a pilot randomised, controlled, open label, multicentre trial. 2020. https://ssrn.com/abstract=3714649
- 16.Wölfel R., Corman V.M., Guggemos W. Virological assessment of hospilatalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 17.Lifschitz A., Virkel G., Sallovitz J. Comparative distribution of ivermectin and doramectin to parasite location tissues in cattle. Vet Parasitol. 2000;87:327–338. doi: 10.1016/s0304-4017(99)00175-2. [DOI] [PubMed] [Google Scholar]
- 18.Jermain B., Hanafin P.O., Cao Y., Lifschitz A., Lanusse C., Rao G. Development of a minimal physiologically-based pharmacokinetic model to simulate lung exposure in humans following oral administration of Ivermectin for COVID-19 drug repurposing. J Pharm Sci. 2020 doi: 10.1016/j.xphs.2020.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ji L., Cen J., Lin S. Study on the subacute inhalation toxicity of ivermectin TC in rats. Comp Med. 2016;26:70–74. [Google Scholar]
- 20.Chaccour C., Abizanda G., Casellas A. Nebulized ivermectin for COVID-19 and other respiratory diseases, a proof of concept, dose-ranging study in rats. Sci Rep. 2020;10(1):17073. doi: 10.1038/s41598-020-74084-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.VICH Guideline 9 . The European Agency for the Evaluaion of Medicinal Products (EMEA) 2001. Veterinary medicines and information technology unit.CVMP/VICH/595/98-FINAL. [Google Scholar]
- 22.Chambers P.G., Grandin T., Heinz G., Srisuvan T. (FAO) Publishers; Thailand: 2001. Guidelines for Human Handling, Transport and Slaughter of livestock.Food and Agriculture Organisation. [Google Scholar]
- 23.Gibaldi M., Perrier D. Revised and Expanded. second ed. Marcel Dekker; New York, USA: 1982. Pharmacokinetics; pp. 45–109. [Google Scholar]
- 24.Fernández L., Velásquez M., Sua L.F. The porcine biomodel in translational medical research: from biomodel to human lung transplantation. Biomedica. 2019;39:300–313. doi: 10.7705/biomedica.v39i3.3820. [DOI] [PubMed] [Google Scholar]
- 25.Lees P., Cheng Z., Chambers M., Hennessy D., Abbott E.M. Pharmacokinetics and bioequivalence in the pig of two ivermectin feed formulations. J Vet Pharmacol Ther. 2013;36:350–357. doi: 10.1111/j.1365-2885.2012.01428.x. [DOI] [PubMed] [Google Scholar]
- 26.Pasay C.J., Yakob L., Meredith H.R. Treatment of pigs with endectocides as a complementary tool for combating malaria transmission by Anopheles farauti (s.s.) in Papua New Guinea. Parasit Vectors. 2019;12:124. doi: 10.1186/s13071-019-3392-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.ClinicalTrials.gov [Internet].Prophylactic ivermectin in COVID-19 contacts. https://clinicaltrials.gov/ct2/show/results/NCT04422561?view=results