Abstract
Approximately 214 million women of reproductive age lack adequate access to contraception for their family planning needs, yet patterns of contraceptive availability have seldom been examined. With growing demand for contraceptives in some areas, low contraceptive method availability and stockouts are thought to be major drivers of unmet need among women of reproductive age, though evidence for this is limited. In this research, we examined trends in stockouts, method availability and consumption of specific contraceptive methods in urban areas of four sub-Saharan African countries (Burkina Faso, Democratic Republic of Congo, Kenya and Nigeria) and India. We used representative survey data from the Performance Monitoring for Action Agile Project that were collected in quarterly intervals at service delivery points (SDP) stratified by sector (public vs private), with all countries having five to six quarters of surveys between 2017 and 2019. Among SDPs that offer family planning, we calculated the percentage offering at least one type of modern contraceptive method (MCM) for each country and quarter, and by sector. We examined trends in the percentage of SDPs with stockouts and which currently offer condoms, emergency contraception, oral pills, injectables, intrauterine devices and implants. We also examined trends of client visits for specific methods and the resulting estimated protection from pregnancy by quarter and country. Across all countries, the vast majority of SDPs had at least one type of MCM in-stock during the study period. We find that the frequency of stockouts varies by method and sector and is much more dynamic than previously thought. While the availability and distribution of long-acting reversible contraceptives (LARCs) were limited compared to other methods across countries, LARCs nonetheless consistently accounted for a larger portion of couple years of protection. We discuss findings that show the importance of engaging the private sector towards achieving global and national family planning goals.
Keywords: Family planning, contraception, reproductive health, survey methods, surveillance, public/private, health services
KEY MESSAGES.
PMA Agile is a useful platform for routinely tracking the family planning supply environment in urban/suburban areas of low- and middle-income countries
Changes in contraceptive supply are common and vary by method and sector (public vs private)
Pharmacies and drug shops could be further leveraged in addressing unmet need in contraceptives
Introduction
Providing access to contraception is critical for achieving several global health outcomes, such as reducing maternal mortality, maximizing the health benefits of birth spacing, and promoting the economic empowerment of women (Stover and Ross, 2010; Ahmedet al., 2012; Do and Kurimoto, 2012). Considering the efforts of family planning (FP) programs worldwide to address the unmet need for contraception, progress has been slow in many low-resource countries (Darroch et al., 2011). Millions of women continue to lack access to contraception due to ‘supply-side’ barriers such as poor accessibility to health facilities, low levels of contraceptive method availability and contraceptive stockouts (Hubacher et al., 2008; Chandra-Mouliet al., 2014).
In 2017, more than 214 million women of reproductive age worldwide lacked adequate access to contraception (Guttmacher Institute, 2017). Stockouts likely play a role in this lack of access, though the relationship between contraceptive availability and use remains poorly understood. Existing evidence suggests that contraceptive stockouts and method availability range widely across countries and across methods (Ali et al., 2018; Babazadeh et al., 2018; Zimmerman et al., 2019). Different countries may experience different contexts of varying supply chain challenges that ultimately impact method availability and stockouts differentially. The policy environment on family planning also likely contributes to the variation in contraceptive stockouts and method availability across health delivery sectors. For instance, a 2018 USAID report suggested that among the 36 countries providing information on supply chain challenges, 15% cited formal and informal policy barriers that hinder the ability of the private sector to provide contraceptive methods (USAID, 2018).
Stockouts and low method availability restrict choice in contraception, forcing individuals to choose methods that may not suit their preferences and needs. For example, a woman’s contraceptive preferences may vary depending on spousal preferences, cultural acceptability of contraceptive methods, socioeconomic influences, her motivation for spacing or limiting births and her preference for hormonal or non-hormonal methods (Brown and Eisenberg, 1995; Wang and Mallick, 2019). In limiting contraceptive method choice, stockouts and low method availability promote conditions that ultimately discourage the use of modern methods and likely lead to increased contraceptive discontinuation (Ross and Hardee, 2013; Grindlay et al., 2016). Therefore, ensuring an adequate range of methods at various levels of the health care system is crucial to guarantee that individuals and couples can select their contraceptive method of choice, thereby allowing them to achieve their fertility goals.
Despite the importance of measuring stockouts, existing research is limited. Data on the family planning supply side are not systematically available: the Service Provision Assessment (SPA) of the Demographic and Health Surveys (DHS) occurs at irregular intervals and only in a limited set of countries where DHS operates (DHS Program, 2017). Overall, data on stockouts by contraceptive method are scarce, and only a few countries are able to monitor stockouts routinely at the facility level (FP, 2015, 2020). Furthermore, since there have not been many studies that have examined contraceptive stockouts in the context of client volume, it remains unclear whether stockouts are primarily a response to a break-down in the supply chain or increase in demand, or both. It is plausible that stockouts may be broadly problematic for the most popularly used methods, especially short-acting methods that require frequent revisits to maintain protection against unintended pregnancy. Due to these data limitations, little is known about patterns in stockouts, or the FP supply-side picture overall.
Data from the PMA Agile surveys provide an opportunity to address existing knowledge gaps on contraceptive stockouts. A unique feature of the PMA Agile platform is a design that allows the monitoring of progress at the subnational level of each country through the collection of facility-level data in quarterly intervals each year. They thus enable a continuous assessment of contraceptive commodity and service provision in urban facilities, both private and public.
In this research, we describe trends in stockouts, method availability and consumption of specific contraceptive methods using locally representative data from facilities in urban areas of Burkina Faso, the Democratic Republic of Congo (DRC), Kenya, Nigeria and India. We expect that this information may help monitor progress towards FP2020 goals (Brown et al., 2014) and inform cross-country strategies to anticipate, reduce and prevent stockouts.
Methods
Study design, sampling and data collection
Data for this study come from the Performance Monitoring for Action (PMA) Agile Project. PMA Agile is a continuous data monitoring and evaluation system that collects data on family planning service delivery and consumption through quarterly public and private health facility surveys and semi-annual client exit interviews (CEIs) in urban areas. A phone follow-up survey is conducted with consenting female clients four months after their interviews (www.pmadata.org/technical-areas/pma-agile). It operates in selected urban areas of six countries, Burkina Faso, DRC, India, Kenya, Niger and Nigeria. PMA Agile has multiple sites in urban areas of four countries: Lagos, Kano and Ogun in Nigeria; Uasin Gishu, Migori and Kericho in Kenya; Indore, Firozabad and Puri in India; Ouagadougou and Koudougou in Burkina Faso. There is one PMA Agile site in each of the two remaining countries: Kinshasa in the DRC and Niamey in Niger. We note that the sites in Kenya are a mix of urban and suburban sites. Data from Niger are excluded from this study since they were not available at the time of this analysis. The population estimates for each of the aforementioned sites are included in the PMA Agile protocol paper (Tsui et al., 2020).
The surveys in this study were implemented between November 2017 and December 2019 across countries. Within each country survey, data were collected by locally recruited and trained female resident enumerators (REs). Data collection was implemented using questionnaires powered by smartphone and open source software (Open Data Kit—ODK) technologies.
Our analysis included service delivery points (SDPs) data from official listings provided by the country Ministry of Health (MoH) and other government agencies within each PMA Agile study site. The sampling scheme allowed for a 10% non-response rate, and thus a maximum sample of 220 SDPs was randomly selected from each site. The surveys used a two-stage cluster sampling design where SDPs were first stratified by public and private and then further sampled based on probability proportional to size to select facility types with at least 20 SDPs. In smaller areas such as Koudougou where the number of SDPs was relatively limited, the full census of SDPs was used. More information about PMA Agile can be found at the project’s website: www.pmadata.org/technical-areas/pma-agile, and in the PMA Agile protocol paper (Tsui et al., 2020).
Measurement
The main measures of interest were the provision and demand of specific modern contraceptive methods (MCM) among SDPs offering family planning services. We define contraceptive stockouts as when one or more contraceptive methods are temporarily unavailable at a health facility that routinely provides that method (Grindlay et al., 2016). Method availability, in turn, measures the percentage of health facilities offering a given contraceptive method over a period of time. Information on the country-specific brands of contraceptive methods considered is available on the project’s website and dashboard. The availability of family planning services/products at a given SDP was determined by the response to the survey question, ‘Do you usually offer FP services/products?’. If the SDP provided FP services/products, the respondent was then asked about the availability of specific contraceptive methods. If the SDP reported offering a given contraceptive method, the RE then asked if the method was in-stock on the day of the survey and if there had been a stockout of the method at any point within the 3 months preceding the interview. A method was considered in-stock only if the RE could visually confirm its availability on the day of the survey. To assess the demand of contraceptive methods, the RE requested to see the facility logbook and recorded the total number of family planning visits (new and continuing) in the last completed month for each method.
A secondary measure examined in this study was a couple years of protection (CYP). The CYP is a commonly used family planning metric that quantifies the level of protection offered by contraceptives against unintended pregnancies over a period of time (Stover and Ross, 2010). It is obtained by multiplying the quantity of each method distributed to clients by a conversion factor resulting in an estimate of the duration of contraceptive protection provided per unit of that method (USAID, 2019). To obtain the quantity of methods distributed to clients, we combined the total number of contraceptive method units sold with the total number of visits for each method. This was necessary since certain types of SDPs such as pharmacies, drugstores and chemists track product distribution as sales whereas other facility types use clinical visits as measures of client volume. To standardize these different measures, we assumed that clients received six condoms, four sachets of oral pills or one unit of the other methods for each relevant visit to an eligible facility.
We defined the following contraceptive methods as modern according to the WHO (WHO, 2018): oral pills, intrauterine devices (IUDs), injectables, male and female condoms, implants and emergency contraception. Though PMA Agile collects SDP data on other methods such as contraceptive beads, foam/jelly and sterilization, these are excluded from this study since the first two methods (beads, foam/jelly) are uncommon in all PMA Agile settings, and sterilization is a medical procedure for which stock does not directly apply as a measure. We note that PMA Agile did not collect information on implants in India as the method was not offered at the time of this study and is currently undergoing consideration for introduction into the national family planning program (Joshi et al., 2019).
Data analysis
We limited the analysis to SDPs offering family planning and stratified our analyses by sector (i.e. public vs private). The proportions of surveyed SDPs offering family planning for each country are shown in Supplementary Table S1. For each country, we first tabulated SDP types by quarter for those with stock of at least one type of modern contraceptive method. Though the standard in the field is to calculate the percentage of SDPs offering at least three to five methods in order to evaluate the level of client choice in methods, we found these thresholds to be too restrictive for analyses focused on assessing method stockouts. Next, we calculated the quarterly percentages of SDPs that typically offer specific contraceptive methods, those that had the indexed methods in stock, out-of-stock or had experienced a stockout within the 3-month period preceding the survey. We then estimated the total monthly volume of clients visiting SDPs for specific contraceptive methods. Finally, we estimated the percent contribution of individual contraceptive methods to overall CYP units produced.
Based on the sampling procedures, we constructed facility weights using SDP selection probabilities. The weighting process took into account the quarterly changes in non-response rates and any SDP classification change by public/private or facility type that happened over time. We report weighted results to account for the stratified two-stage cluster sampling design and the variances of the estimates are adjusted accordingly using Taylor series linearization. We used Stata version 14.2 (StataCorp LLC, College Station, TX) with the SVY command to conduct design‐based analyses that accounted for stratification, clustering and probability of selection of the SDPs (Heeringa et al., 2017).
Results
In Table 1, we present the number of SDPs by country and quarter, separately for public and private SDPs. We also show the percentage of each offering at least one family planning method in-stock, again by country, quarter and public/private.
Table 1.
Percentage of SDPs (by type, country and quarter) with at least one type of modern contraceptive method in stock at time of survey
| Country name | Quarters | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Public SDPs |
Private SDPs |
|||||||||||||||||||||||
| Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
|||||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |||||
| Burkina Faso | ||||||||||||||||||||||||
| Hospital | 2 | 100.0 | 2 | 73.9 | 2 | 100.0 | 2 | 72.7 | 1 | 100.0 | 2 | 0.0 | 0 | 0.0 | 2 | 0.0 | 2 | 0.0 | 2 | 0.0 | ||||
| Medical Center/ Health Clinic/ Health Center | 27 | 100.0 | 26 | 98.0 | 27 | 100.0 | 30 | 93.3 | 24 | 95.3 | 49 | 69.5 | 44 | 68.7 | 51 | 63.9 | 43 | 72.5 | 45 | 72.8 | ||||
| Maternity clinic | 13 | 56.7 | 11 | 49.9 | 13 | 52.6 | 11 | 48.2 | 11 | 42.7 | 4 | 50.0 | 4 | 55.9 | 3 | 66.7 | 3 | 66.7 | 4 | 50.0 | ||||
| Pharmacy | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 54 | 100.0 | 60 | 90.6 | 55 | 100.0 | 52 | 96.9 | 60 | 100.0 | ||||
| All SDP types | 42 | 86.9 | 39 | 82.7 | 41 | 84.5 | 43 | 81.4 | 36 | 78.9 | 109 | 83.0 | 108 | 80.6 | 111 | 81.2 | 100 | 83.8 | 111 | 85.7 | ||||
| DRC | ||||||||||||||||||||||||
| Hospital | 13 | 81.8 | 19 | 93.8 | 16 | 92.9 | 17 | 100.0 | 17 | 78.6 | 1 | 100.0 | 1 | 100.0 | 1 | 100.0 | 1 | 100.0 | 1 | 100.0 | ||||
| Health Center | 64 | 78.9 | 54 | 93.5 | 60 | 90.5 | 59 | 96.0 | 60 | 94.1 | 11 | 90.0 | 11 | 100.0 | 11 | 100.0 | 12 | 81.8 | 12 | 100.0 | ||||
| Pharmacy | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 58 | 92.9 | 62 | 93.2 | 54 | 98.5 | 54 | 93.6 | 53 | 95.2 | ||||
| All SDP types | 77 | 86.9 | 73 | 93.5 | 76 | 91.0 | 76 | 96.9 | 77 | 90.7 | 70 | 92.6 | 74 | 94.2 | 66 | 98.8 | 67 | 91.4 | 66 | 95.9 | ||||
| India | ||||||||||||||||||||||||
| Hospital | 5 | 88.9 | 4 | 100.0 | 4 | 100.0 | 4 | 100.0 | 4 | 100.0 | 3 | 100.0 | 57 | 24.4 | 61 | 34.1 | 64 | 17.5 | 59 | 10.6 | 62 | 13.4 | 55 | 10.9 |
| Health Clinic/Health Center | 17 | 87.0 | 16 | 93.1 | 13 | 96.6 | 13 | 96.8 | 13 | 96.8 | 11 | 100.0 | 21 | 31.9 | 22 | 30.1 | 21 | 32.1 | 23 | 20.1 | 23 | 20.1 | 19 | 2.0 |
| Pharmacy/Drugstore | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 217 | 94.0 | 224 | 96.8 | 216 | 96.1 | 217 | 78.0 | 216 | 78.8 | 168 | 68.6 |
| Dispensary | 4 | 100.0 | 3 | 100.0 | 4 | 100.0 | 3 | 100.0 | 3 | 100.0 | 3 | 100.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| All SDP types | 25 | 89.3 | 23 | 95.4 | 21 | 97.8 | 20 | 97.9 | 20 | 97.9 | 17 | 100.0 | 295 | 76.1 | 307 | 79.6 | 301 | 74.9 | 299 | 60.1 | 301 | 61.0 | 242 | 50.2 |
| Kenya | ||||||||||||||||||||||||
| Hospital | 14 | 100.0 | 14 | 95.5 | 14 | 90.9 | 14 | 100.0 | 14 | 90.9 | 14 | 90.3 | 15 | 84.0 | 16 | 90.2 | 15 | 95.9 | 16 | 100.0 | 14 | 100.0 | 15 | 100.0 |
| Health Clinic/Health Center | 34 | 95.8 | 33 | 100.0 | 33 | 98.1 | 33 | 96.1 | 33 | 97.9 | 35 | 92.1 | 63 | 94.7 | 66 | 97.0 | 64 | 96.4 | 65 | 95.8 | 67 | 93.0 | 66 | 94.8 |
| Pharmacy | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 166 | 100.0 | 181 | 99.5 | 195 | 100.0 | 202 | 99.5 | 188 | 99.5 | 198 | 99.5 |
| Dispensary | 184 | 97.7 | 175 | 99.3 | 172 | 99.5 | 173 | 97.5 | 171 | 98.6 | 174 | 97.9 | 22 | 91.9 | 25 | 84.7 | 21 | 100.0 | 23 | 100.0 | 22 | 94.6 | 22 | 100.0 |
| All SDP types | 232 | 97.6 | 222 | 99.1 | 219 | 98.7 | 220 | 97.5 | 218 | 98.0 | 223 | 96.5 | 266 | 97.2 | 288 | 97.1 | 295 | 99.0 | 306 | 98.8 | 293 | 97.6 | 301 | 98.6 |
| Nigeria | ||||||||||||||||||||||||
| Hospital | 5 | 94.9 | 6 | 100.0 | 6 | 95.0 | 6 | 95.1 | 5 | 95.0 | 5 | 100.0 | 133 | 70.5 | 164 | 78.8 | 169 | 69.9 | 168 | 59.5 | 151 | 56.9 | 145 | 63.9 |
| Health Post/Health Center | 75 | 89.3 | 83 | 92.8 | 83 | 91.7 | 83 | 91.6 | 77 | 94.3 | 74 | 91.2 | 30 | 26.7 | 43 | 56.3 | 34 | 84.1 | 34 | 88.5 | 30 | 85.6 | 30 | 93.4 |
| Maternity clinic | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 23 | 63.0 | 29 | 63.9 | 31 | 78.7 | 30 | 53.2 | 28 | 63.7 | 27 | 53.5 |
| Pharmacy/Chemist | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 138 | 96.5 | 168 | 99.7 | 180 | 99.5 | 180 | 97.1 | 164 | 99.0 | 158 | 99.0 |
| All SDP types | 80 | 89.7 | 89 | 93.3 | 89 | 91.9 | 89 | 91.8 | 82 | 94.3 | 79 | 91.8 | 324 | 76.9 | 404 | 84.0 | 414 | 84.6 | 412 | 77.9 | 373 | 78.3 | 360 | 81.0 |
N represents the total weighted number of SDPs offering family planning
Overall, some patterns in the health system structure are evident in Table 1. The number of private facilities is larger than public ones in all countries except DRC. Pharmacies are generally private in all countries. In all countries, public facilities are mostly made up of health posts, health centres and medical centres. The overall number of facilities by type is generally stable across quarters for each country.
Of these facilities, the vast majority offers at least one modern method. For example, 86.9% of all public SDPs and 83.0% of all private SDPs in quarter 1 in Burkina Faso offer at least one modern method. In some settings, however, there is variation across SDP facility types in the percentage offering one modern method: relatively few private hospitals or health clinics/centres in India offer at least one method, but the majority of private pharmacies and drugstores offer at least one method. Similarly, most private pharmacies offer at least one method in Burkina Faso but smaller percentages of medical centres/health centres/health clinics do in all quarters.
Stockouts and consumption of contraceptive methods
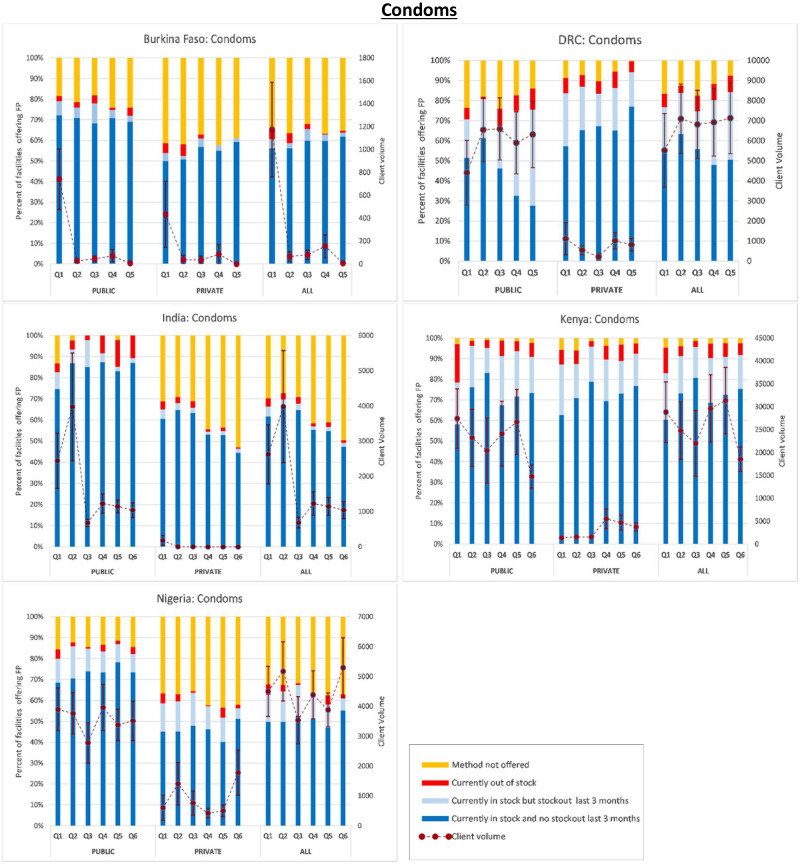
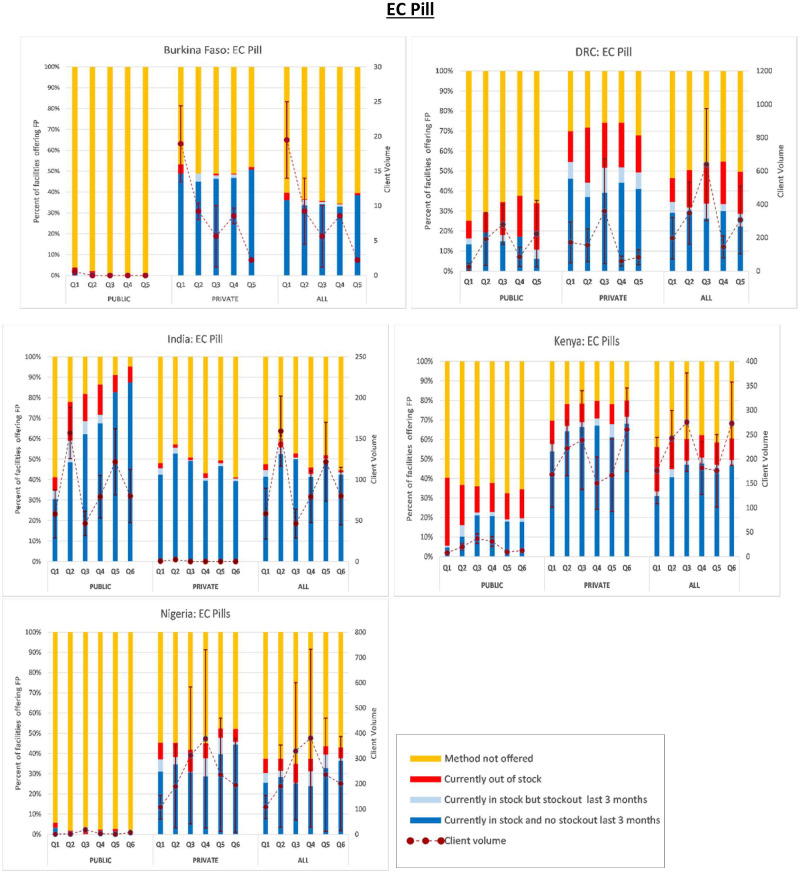
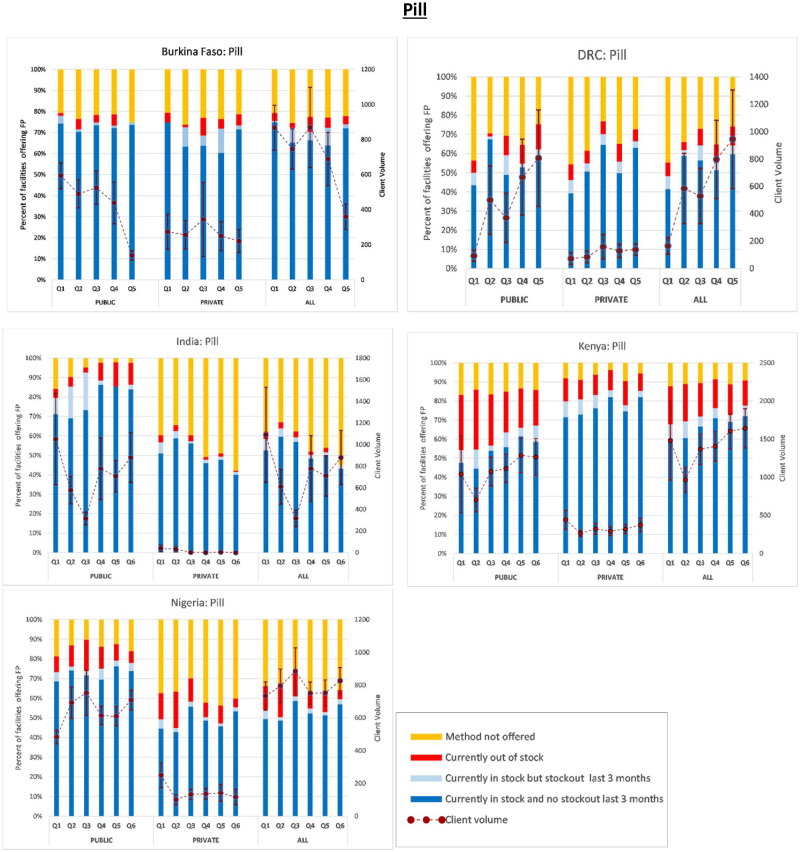
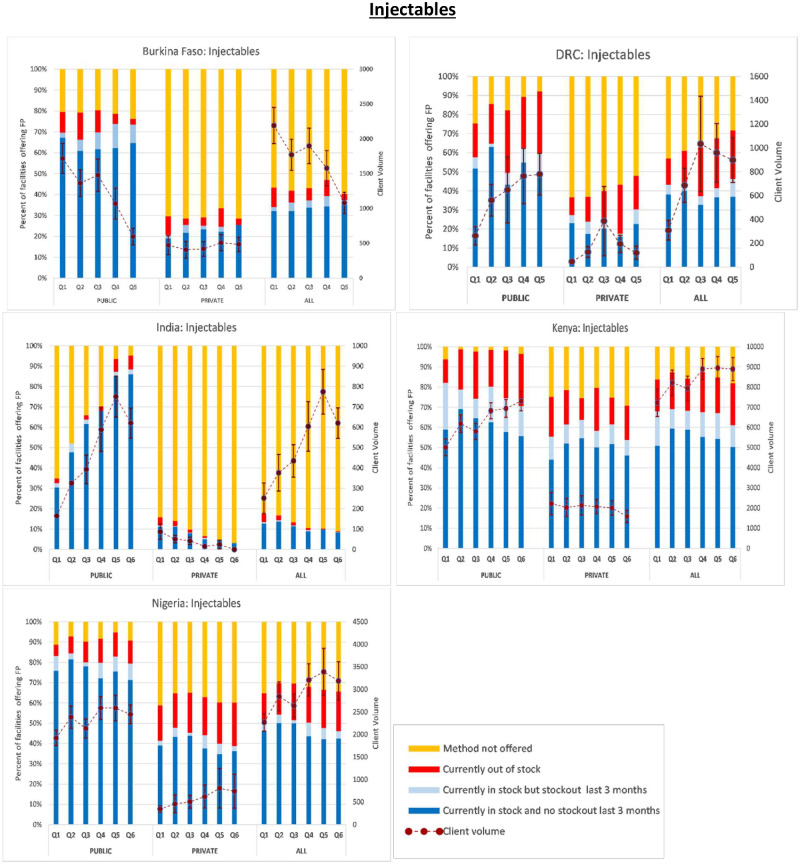
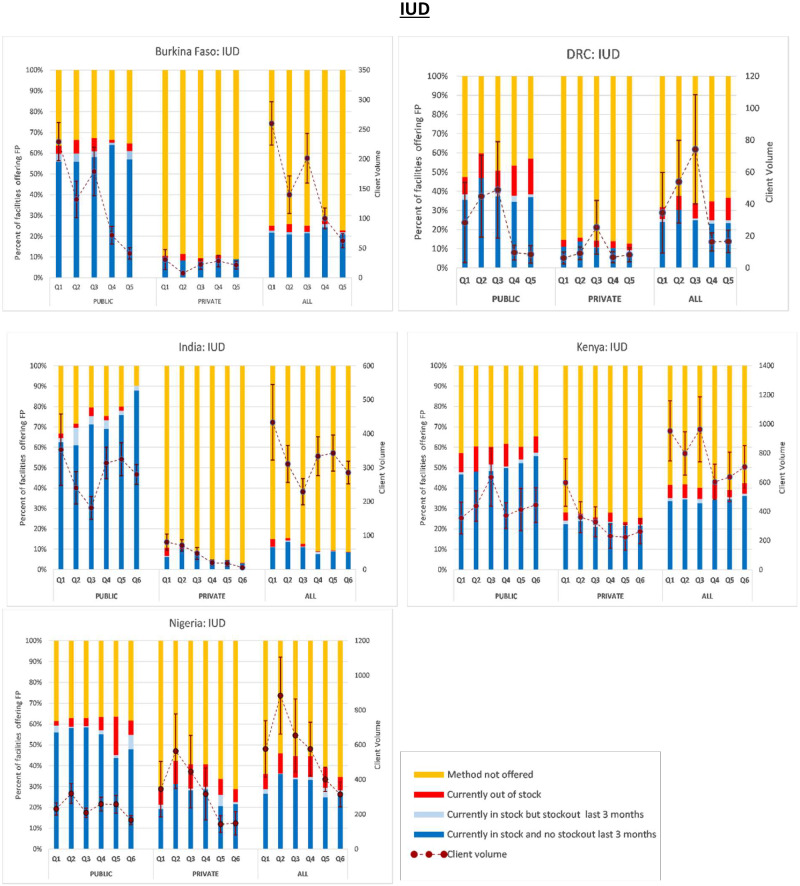
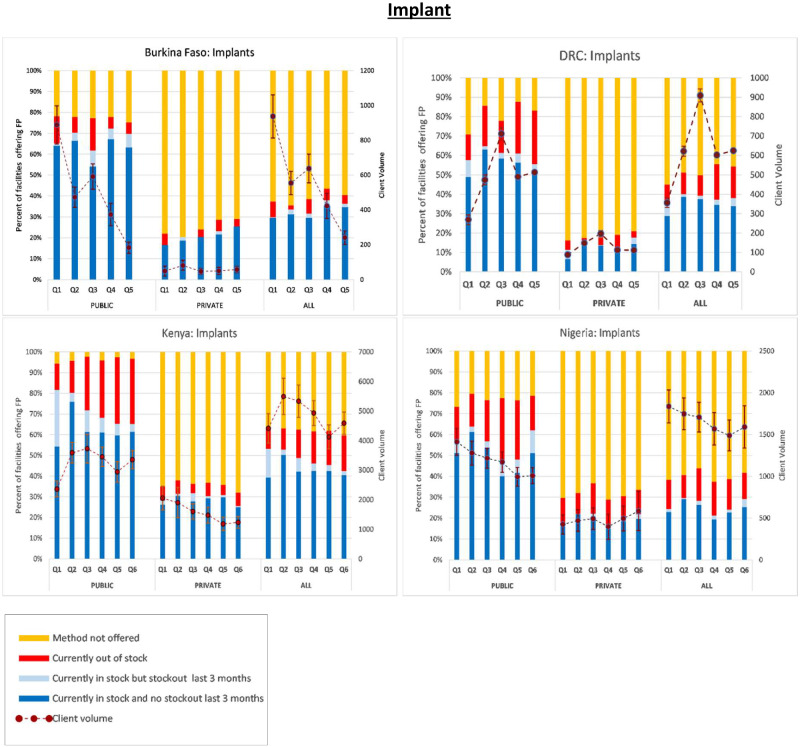
Next, in Figures 1–6, we present trends in stockouts for the different types of MCMs (condoms, EC, oral pills, injectables, IUDs and implants), for the public, private and all facilities. In the same figures, we also show the corresponding trends in monthly client volume (in dotted lines). We present this separately for each of the five PMA Agile countries.
Figure 1.
Contraceptive method availability and client volume by quarter and country. NB: Client volume is measured as the total number of visits by method in the month preceding the interview. Error bars represent standard errors
Figure 2.
EC pill.
Figure 3.
Pill.
Figure 4.
Injectables.
Figure 5.
IUD.
Figure 6.
Implant.
Condoms
In most countries, condoms were more commonly distributed through the public SDPs instead of the private sector, as shown by higher percentages of public SDPs offering condoms and the higher numbers of monthly client visits purchasing condoms from public SDPs. The average percentage of public SDPs not offering condoms was 11.2% compared to 24.8% of the private SDPs. Among the public SDPs, the average client volume for condoms was 6 842 monthly visits, ranging from 178 visits in Burkina Faso to 22 775 in Kenya. Among the private SDPs, the average client volume was 2018 monthly visits ranging from 32 visits in India to 3077 in Kenya. Regardless of SDP managing authority, an average of 7 858 monthly visits for condoms were observed across all countries ranging from 296 in Burkina Faso to 25 852 in Kenya.
The average SDP stockout rate for condoms was 4.2% across all countries and it ranged from 2.5% in Burkina Faso and India to 6.8% in the DRC. Among the surveyed public SDPs, the average condom stockout rate was 5.3% ranging from 2.5% in Nigeria to 7.3% in Kenya. The average condom stockout rate among the private SDPs was 4.1% ranging from 2.2% in India to 6.6% in the DRC. Furthermore, an average of 12.5% of all the SDPs across all countries had experienced a condom stockout within the 3 months preceding the survey. This percentage varied from 2.8% in India to 25.6% in the DRC.
Emergency contraception
We found that the private sector was generally the main distributor of emergency contraceptive pills among the Sub-Saharan African (SSA) countries. In fact, the distribution was conducted almost exclusively through the private sector in Burkina Faso and Nigeria. Among the private facilities with FP, the proportion that did not offer emergency contraception over the study period fluctuated around 28.4% for the DRC, 22.6% for Kenya with that number exceeding 50% for both Burkina Faso and Nigeria. Compared to the other African countries in the study, Burkina Faso had the lowest volume of clients (9 monthly visits on average) purchasing EC with the number progressively decreasing during the study period. In contrast, there were 327, 241 and 221 monthly client visits on average, in the DRC, Nigeria and Kenya, respectively. Across all the African countries, the trends for monthly client visits remained largely highly variable.
Contrary to African countries, the provision of EC in Indian sites was largely via the public sector. The proportion of government-owned SDPs that had EC in stock on the day of the survey increased from 30.6% to 87.4%. The percentage of SDPs experiencing a stockout within the 3 months preceding the survey decreased from 3.1% to 1.1%. This positive trend was further strengthened by the almost 60% reduction in SDPs experiencing a stock out in EC between Q2 and Q6. The steady gains and stability observed in method provision within the public sector were not accompanied by similar increases in client visits for EC. Client visits for EC through the private sector in Indian sites were negligible.
Oral pills
Similar to EC, the distribution of oral pills in India was higher in the public sector compared to the private sector. Over the study period, the proportion of public SDPs that did not offer the method in India decreased from 14.8% to 2.3%. This trend was reversed within the private sector with the percentage of SDPs not offering pills increasing from 39.0% to 57.5%. The average number of monthly visits for pills was 718 among the public SDPs compared to only 13 among the private SDPs.
Similarly, in SSA countries, the number of clients obtaining pills was generally higher among public SDPs compared to private SDPs. The ratio of the average monthly client volume among public SDPs to that among private SDPs ranged from 2.2 in Burkina Faso to 4.4 in Nigeria. Compared to other African geographies, Burkina Faso generally experienced lower stockouts of oral pills with an average stockout rate of 3.8% over the study period. In contrast, Kenya experienced an overall average stockout rate of 17% in oral pills with that number approximating 25% among public SDPs. The overall average stockout rate in the DRC was 19.7% (21.2% among public SDPs; 17.8% private SDPs). In Nigeria, the stockout rate for oral pills varied from quarter to quarter at an overall average of 10.6% across surveyed SDPs (10.1% among public SDPs; 10.8% private SDPs).
With the exception of Burkina Faso, where the percentage of SDPs not offering oral pills increased slightly from 20.7% to 22.2% over the study period, the availability of oral pills generally improved among SSA countries. In the DRC, the average percentage of SDPs that did not offer oral pills was 29%, decreasing from 40% to 21%; a 47.5% decrease (49.5% decrease among public SDPs compared to 45.7% decrease among private SDPs). In Kenya, the percentage of SDPs not offering oral contraceptives decreased by 25% over the study period to an average of approximately only 10%. Only 7% of the private SDPs reported that they do not offer the method compared to 15% of the public SDPs. An average of only 14% of the private Nigerian SDPs compared to 38% of the public SDPs did not offer the method, the overall average being 34%.
Injectables
Across all geographies, public SDPs generally offered injectables at higher rates than private SDPs. While only an average of 15.8% of the public SDPs did not offer injectables during the study period, this figure was 56.5% among the private SDPs. The combined average was 45.6%. With the exception of Burkina Faso, net improvements were generally observed in the average number of monthly client visits. The most remarkable improvements were noted among public SDPs in India where the number of client visits for injectables increased by more than 3.5-fold over the first five quarters with an associated 93% decrease in the percentage of SDPs not offering the method. Despite these gains, however, the overall availability of injectables remains low in India due to the low rates of injectable availability among private SDPs. On average, 91% of the private SDPs in India did not offer injectables compared to 31.4% among public SDPs and the combined average of 87.2%.
Across all SDPs, the average stockout rate in injectable provision was 13.0% and it varied considerably across geographies ranging from 1.6% in India to 21.6% in the DRC over the study period. The average stockout rate for the public SDPs across all geographies was 13.6% compared to the average stockout rate of 11.9% among private SDPs. Roughly, 5.1% of all SDPs reported a stockout in injectables within the previous 3 months. There was geographic variation in this rate ranging from 0.4% in India to 11.9% in Kenya. Of all public SDPs, 7.4% experienced a stockout during the 3-month period preceding the interview compared to 4.0% of the private SDPs.
Intrauterine devices
Compared to the short-acting methods described above, IUDs were generally offered at lower levels across the different geographies. Across all geographies, the percentage of SDPs not offering IUDs was 69.2% and it ranged from 58.8% in Nigeria to 88.4% in India. It was also notable that, across the board, the public sector offered IUDs at considerably higher levels compared to the private sector and was furthermore likely to have the method in-stock over a 3-month period. The average percentage of public SDPs not offering IUDs was 36.0% compared to 81.2% of the private SDPs. Nonetheless, with the exception of Nigeria, IUD stockouts were more common among public SDPs. Of the public SDPs that offered IUDs, the average stockout rate was 7.3% compared to 3.7% among the private SDPs. Across all countries, the combined average stockout rate was 5.4%. On average, 1.1% of the IUD-providing SDPs reported a stockout during the 3-month period preceding the interview. This figure was 2.5% among public SDPs compared to 0.7% among the private SDPs.
Trends in the client visits for the purchase of IUDs were centred at an average of approximately 372 monthly visits. It varied across countries ranging from an average of 39 monthly visits in the DRC to 776 monthly visits in Kenya.
Implants
The average percentage of SDPs not offering implants over the study period was 52.0%, ranging from 38.1% in Kenya to 61.0% in Burkina Faso. In all cases, the percentage of public SDPs offering implants was greater than private SDPs. Overall, only 17.1% of the public SDPs did not offer implants compared to 72.4% of the private SDPs. This contrast was starkest in Kenya where a quarterly average of only 3.7% of the public SDPs did not offer implants compared to 64.3% in the private sector (combined average being 38.1%). Among the African countries, the overall average stockout rate was 11.5% ranging from 5.2% in Burkina Faso to 14% in both Kenya and Nigeria. The DRC had an average implant stockout rate of 13.1%. The stockout rates were higher among the public SDPs and varied more across quarters relative to the private SDPs. Among the public SDPs, the average stockout rate was 18.9% compared to 6.6% observed among the private SDPs. Furthermore, whereas the percentage of public SDPs that experienced a stockout in implants 3 months prior to the interview was 6.3%, this number was only 1.3% among the private SDPs. The average number of monthly client visits was 1 913 monthly visits and ranged from 559 visits in Burkina Faso to 4 815 in Kenya.
Couple-years of protection of contraceptives
CYP data for the different countries are shown in Table 2. Of all the MCMs considered in this study, implants on average accounted for the most CYPs among the public SDPs. With the exception of India where implants are currently not offered, implants accounted for 58.9% of the CYPs provided by the public SDPs across all countries ranging from 55.2% in Burkina Faso to 61.5% in the DRC. This trend did not hold among the private SDPs.
Table 2.
Quarterly changes in couple years of protection (CYP) by country and method
| PUBLIC |
PRIVATE |
|||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country namea | Quarters |
Quarters |
||||||||||||||||||||||
| Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
|||||||||||||
| Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | Total CYP | % | |
| Burkina Faso | N = 34 | N = 32 | N = 34 | N = 29 | N = 15 | N = 82 | N = 73 | N = 75 | N = 73 | N = 79 | ||||||||||||||
| Condoms | 48.4 | 0.8 | 4.1 | 0.1 | 3.0 | 0.1 | 4.3 | 0.3 | 2.1 | 0.2 | 80.8 | 9.8 | 83.9 | 9.9 | 70.6 | 9.4 | 4.3 | 0.3 | 74.9 | 7.9 | ||||
| Pill | 240.3 | 4.2 | 200.6 | 5.4 | 200.7 | 4.8 | 122.8 | 7.4 | 64.2 | 5.2 | 229.8 | 27.9 | 293.8 | 34.7 | 221.7 | 29.7 | 122.8 | 7.4 | 209.0 | 22.1 | ||||
| Injectable | 652.1 | 11.4 | 501.1 | 13.6 | 516.4 | 12.4 | 274.0 | 16.5 | 202.7 | 16.6 | 131.4 | 16.0 | 114.9 | 13.6 | 117.0 | 15.6 | 274.0 | 16.5 | 131.6 | 13.9 | ||||
| EC pill | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 93.5 | 11.4 | 104.4 | 12.3 | 75.1 | 10.0 | 0.0 | 0.0 | 151.7 | 16 | ||||
| IUD | 1545.1 | 26.9 | 962.3 | 26.1 | 1184.5 | 28.4 | 330.3 | 19.8 | 293.9 | 24.0 | 141.2 | 17.2 | 36.3 | 4.3 | 122.4 | 16.4 | 330.3 | 19.8 | 230.0 | 24.3 | ||||
| Implant | 3257.8 | 56.7 | 2016.8 | 54.7 | 2268.8 | 54.4 | 934.3 | 56.1 | 661.5 | 54.0 | 145.5 | 17.7 | 214.5 | 25.3 | 141.0 | 18.9 | 934.3 | 56.1 | 149.0 | 15.7 | ||||
| Total | 5743.7 | 100 | 3684.8 | 100 | 4173.3 | 100 | 1665.6 | 100 | 1224.4 | 100 | 822.2 | 100 | 847.9 | 100 | 747.8 | 100 | 1666 | 100 | 946.2 | 100 | ||||
| DRC | N = 33 | N = 58 | N = 54 | N = 66 | N = 70 | N = 57 | N = 70 | N = 61 | N = 67 | N = 65 | ||||||||||||||
| Condoms | 296.8 | 20.5 | 392.9 | 18.9 | 379.6 | 13.9 | 339.0 | 17.0 | 378.7 | 17.4 | 127.5 | 12.3 | 103.6 | 6.3 | 100.6 | 6.9 | 158.3 | 3.1 | 138.9 | 4.1 | ||||
| Pill | 26.0 | 1.8 | 140.1 | 6.8 | 107.6 | 3.9 | 187.0 | 9.4 | 226.5 | 10.4 | 528.6 | 51.1 | 981.7 | 59.5 | 529.2 | 36.3 | 1199.0 | 23.5 | 773.7 | 22.7 | ||||
| Injectable | 83.4 | 5.7 | 140.2 | 6.8 | 167.5 | 6.1 | 191.1 | 9.6 | 197.2 | 9.1 | 34.6 | 3.4 | 71.2 | 4.3 | 136.0 | 9.3 | 84.5 | 1.7 | 68.2 | 2.0 | ||||
| EC pill | 4.1 | 0.3 | 9.6 | 0.5 | 76.9 | 2.8 | 4.3 | 0.2 | 11.2 | 0.5 | 92.6 | 9.0 | 83.0 | 5.0 | 84.0 | 5.8 | 92.1 | 1.8 | 168.9 | 5.0 | ||||
| IUD | 130.6 | 9.0 | 206.1 | 9.9 | 224.5 | 8.2 | 44.2 | 2.2 | 38.6 | 1.8 | 28.5 | 2.8 | 41.9 | 2.5 | 116.4 | 8.0 | 3280.7 | 64.3 | 994.1 | 29.2 | ||||
| Implant | 910.3 | 62.7 | 1185.8 | 57.2 | 1783.5 | 65.1 | 1225.0 | 61.5 | 1321.8 | 60.8 | 221.8 | 21.5 | 369.3 | 22.4 | 492.5 | 33.8 | 284.3 | 5.6 | 1265.8 | 37.1 | ||||
| Total | 1451.2 | 100 | 2074.6 | 100 | 2739.6 | 100 | 1990.5 | 100 | 2174.0 | 100 | 1033.5 | 100 | 1650.7 | 100 | 1458.5 | 100 | 5098.8 | 100 | 3409.5 | 100 | ||||
| India | N = 24 | N = 22 | N = 20 | N = 19 | N = 20 | N = 17 | N = 205 | N = 246 | N = 190 | N = 213 | N = 227 | N = 193 | ||||||||||||
| Condoms | 164.0 | 12.0 | 238.5 | 20.8 | 41.0 | 7.3 | 73.8 | 4.8 | 69.6 | 5.6 | 62.6 | 4.2 | 231.1 | 14.3 | 377.7 | 27.0 | 336.6 | 26.3 | 288.7 | 8.6 | 305.5 | 26.0 | 134.7 | 13.7 |
| Pill | 303.4 | 22.1 | 162.4 | 14.2 | 89.3 | 15.9 | 217.6 | 14.2 | 197.9 | 16.0 | 246.4 | 16.4 | 319.9 | 19.8 | 297.8 | 21.3 | 240.7 | 18.8 | 117.5 | 3.5 | 235.0 | 20.0 | 173.0 | 17.6 |
| Injectable | 41.3 | 3.0 | 76.2 | 6.7 | 90.0 | 16.0 | 136.1 | 8.9 | 150.7 | 12.1 | 30.0 | 2.0 | 49.3 | 3.1 | 40.0 | 2.9 | 30.5 | 2.4 | 508.3 | 15.1 | 37.9 | 3.2 | 40.6 | 4.1 |
| EC pill | 3.3 | 0.2 | 7.8 | 0.7 | 2.3 | 0.4 | 4.0 | 0.3 | 6.1 | 0.5 | 4.0 | 0.3 | 66.9 | 4.1 | 79.5 | 5.7 | 70.0 | 5.5 | 441.5 | 13.2 | 101.1 | 8.6 | 91.9 | 9.3 |
| IUD | 859.7 | 62.7 | 659.6 | 57.6 | 339.0 | 60.4 | 1102.6 | 71.9 | 816.0 | 65.8 | 1156.9 | 77.1 | 946.2 | 58.6 | 602.1 | 43.1 | 603.5 | 47.1 | 2000.5 | 59.6 | 496.3 | 42.2 | 544.2 | 55.3 |
| Total | 1371.8 | 100 | 1144.6 | 100 | 561.6 | 100 | 1534.0 | 100 | 1240.3 | 100 | 1499.9 | 100 | 1613.4 | 100 | 1397.0 | 100 | 1281.4 | 100 | 3356.4 | 100 | 1175.8 | 100 | 984.4 | 100 |
| Kenya | N = 232 | N = 223 | N = 220 | N = 220 | N = 218 | N = 224 | N = 265 | N = 283 | N = 293 | N = 300 | N = 292 | N = 300 | ||||||||||||
| Condoms | 1647.8 | 15.0 | 1393.7 | 9.8 | 1229.6 | 7.9 | 1447.7 | 10.3 | 1601.4 | 11.9 | 887.4 | 6.4 | 584.5 | 5.3 | 388.7 | 3.4 | 587.4 | 6.0 | 730.0 | 7.9 | 606.2 | 7.9 | 579.1 | 7.2 |
| Pill | 291.9 | 2.7 | 203.5 | 1.4 | 306.4 | 2.0 | 318.3 | 2.3 | 363.9 | 2.7 | 363.6 | 2.6 | 978.6 | 8.9 | 668.8 | 5.9 | 813.3 | 8.3 | 852.8 | 9.3 | 599.3 | 7.8 | 827.9 | 10.3 |
| Injectable | 1260.9 | 11.5 | 1558.3 | 10.9 | 1465.0 | 9.5 | 1724.9 | 12.3 | 1753.7 | 13.1 | 1861.2 | 13.4 | 1565.6 | 14.2 | 1465.4 | 12.9 | 1708.7 | 17.5 | 1674.6 | 18.2 | 1533.4 | 19.9 | 1502.6 | 18.7 |
| EC pill | 0.4 | 0.0 | 1.1 | 0.0 | 1.8 | 0.0 | 1.6 | 0.0 | 0.5 | 0.0 | 0.6 | 0.0 | 231.3 | 2.1 | 703.4 | 6.2 | 947.1 | 9.7 | 826.2 | 9.0 | 687.2 | 8.9 | 635.9 | 7.9 |
| IUD | 1534.1 | 14.0 | 1961.4 | 13.8 | 2922.8 | 18.9 | 1769.2 | 12.6 | 2121.1 | 15.8 | 2035.5 | 14.6 | 2193.7 | 19.9 | 3259.6 | 28.7 | 1575.0 | 16.1 | 1013.8 | 11.0 | 1041.0 | 13.5 | 1177.6 | 14.6 |
| Implant | 6221.0 | 56.8 | 9136.3 | 64.1 | 9553.3 | 61.7 | 8755.0 | 62.5 | 7591.0 | 56.5 | 8768.0 | 63.0 | 5472.0 | 49.6 | 4860.3 | 42.8 | 4159.8 | 42.5 | 4104.0 | 44.6 | 3230.5 | 42.0 | 3326.8 | 41.3 |
| Total | 10956.1 | 100 | 14254.2 | 100 | 15479 | 100 | 14016 | 100 | 13432 | 100 | 13916 | 100 | 11025.7 | 100 | 11346.2 | 100 | 9791.3 | 100 | 9201.5 | 100 | 7697.6 | 100 | 8049.9 | 100 |
| Nigeria | N = 79 | N = 87 | N = 88 | N = 88 | N = 82 | N = 79 | N = 270 | N = 325 | N = 342 | N = 338 | N = 302 | N = 285 | ||||||||||||
| Condoms | 271.0 | 4.7 | 232.1 | 4.0 | 174.9 | 3.4 | 248.6 | 4.1 | 209.1 | 4.0 | 243.0 | 4.4 | 235.2 | 4.7 | 230.1 | 4.1 | 170.1 | 3.7 | 187.3 | 5.0 | 205.8 | 5.3 | 281.4 | 7.8 |
| Pill | 152.7 | 2.7 | 198.5 | 3.4 | 222.6 | 4.3 | 181.8 | 3.0 | 194.6 | 3.7 | 238.7 | 4.3 | 328.5 | 6.6 | 301.4 | 5.4 | 302.8 | 6.5 | 281.1 | 7.5 | 349.1 | 8.9 | 299.8 | 8.4 |
| Injectable | 499.7 | 8.7 | 606.1 | 10.5 | 549.8 | 10.7 | 677.6 | 11.3 | 691.6 | 13.1 | 724.7 | 13.1 | 287.7 | 5.8 | 391.0 | 7.0 | 409.8 | 8.9 | 360.2 | 9.6 | 522.4 | 13.4 | 303.6 | 8.5 |
| EC pill | 0.0 | 0.0 | 0.1 | 0.0 | 1.0 | 0.0 | 0.4 | 0.0 | 0.0 | 0.0 | 0.8 | 0.0 | 153.9 | 3.1 | 206.9 | 3.7 | 163.0 | 3.5 | 248.1 | 6.6 | 511.0 | 13.1 | 319.2 | 8.9 |
| IUD | 1103.1 | 19.2 | 1491.8 | 25.8 | 1013.8 | 19.7 | 1779.3 | 29.6 | 1299.5 | 24.6 | 994.1 | 17.9 | 2499.2 | 50.3 | 2984.5 | 53.1 | 2261.4 | 48.9 | 1587.0 | 42.3 | 845.5 | 21.7 | 753.9 | 21.0 |
| Implant | 3707.8 | 64.7 | 3246.5 | 56.2 | 3184.8 | 61.9 | 3115.5 | 51.9 | 2883.3 | 54.6 | 3337.3 | 60.3 | 1460.3 | 29.4 | 1504.3 | 26.8 | 1320.8 | 28.5 | 1085.3 | 28.9 | 1470.5 | 37.7 | 1627.0 | 45.4 |
| Total | 5734.3 | 100 | 5775.0 | 100 | 5146.8 | 100 | 6003.1 | 100 | 5278.1 | 100 | 5538.5 | 100 | 4964.7 | 100 | 5618.2 | 100 | 4627.8 | 100 | 3748.8 | 100 | 3904.3 | 100 | 3584.9 | 100 |
N represents the total weighted number of SDPs contributing to CYP units
Couple years of protection (CYP) is the estimated protection provided by contraceptive methods during a 1-year period, based upon the volume of all contraceptives sold or distributed free of charge to clients during that period (USAID, 2019). the bold values differentiate country totals from other values for the individual methods
Consistent with the lower availability rates and client volumes observed among public SDPs offering emergency contraception, we found that this method did not provide many CYPs relative to other MCMs offered by the public SDPs.
In Burkina Faso, an average of 4 146 CYPs was provided each quarter, of which 3 298 were provided by public SDPs with the remainder being provided by the private SDPs. The combination of IUDs and implants accounted for 80.2% of the CYPs provided by public SDPs and 33.8% of those provided by private SDPs. In the DRC, public SDPs provided an average of 2 086 CYPs each quarter compared to 2 530 among the private SDPs. Oral pills contributed the highest amount of CYPs in the private sector. They accounted for 38.6% of the total CYPs in the private sector. IUDs and implants together accounted for 45.5% of the CYPs provided by the private SDPs. In India, public SDPs provided an average of 1 225 CYPs whereas the private SDPs contributed 1 635 CYPs. Among the MCMs tracked in this study, IUDs provided the highest amount of CYPs against unintended pregnancies. This was consistent over time among both public and private SDPs. Relative to other MCMs, injectables and emergency contraceptive pills did not seem to provide high levels of protection in India. We found that the public SDPs in Kenya provided 13 676 CYPs against unintended pregnancies on average compared to the 9 519 observed in the private sector. Implants provided the most protection across all SDPs regardless of public–private ownership. Similar to the public SDPs in Kenya, those in Nigeria provided a higher amount of protection (5 579 CYPs) compared to their private counterparts (4 408 CYPS). Together, implants and IUDs generally provided the most couple-years of protection across both public and private SDPs.
Discussion
Modern contraceptive use is a product of both supply of and demand for contraception. While the latter has been examined extensively, the former has been studied less often, largely due to data limitations. In this research, we use locally representative data to measure trends in the family planning supply environment in urban or suburban areas of Burkina Faso, DRC, India, Kenya and Nigeria. Specifically, we describe trends in stockouts, method availability and consumption of specific contraceptive methods.
Although each setting has its own unique FP supply profile, some of our results are consistent across settings. We find that public sector facilities are more likely to have a comprehensive mix of short- and long-acting contraceptive methods, compared to private sector facilities, similar to results from other studies (Hutchinson et al., 2011; Kakoko et al., 2012). There are, however, a few exceptions to this pattern, such as EC in SSA countries and oral pills in Kenyan sites. Indeed, previous work by others has shown that private sector SDPs are the major outlets for EC in a range of SSA countries (Maharaj and Rogan, 2008; Mané et al., 2015; Hernandez et al., 2018) and for oral pills in Kenyan sites (Corroon et al., 2016). Furthermore, it is worthwhile to point out that, for some SSA countries such as Kenya, the distribution of EC in public facilities is usually provided only to victims of sexual assault or rape whereas it is readily available over the counter without a doctor prescription in private pharmacies (Thompson et al., 2018). The exact difference between public and private facilities in contraceptive availability differs by country and method. For example, the levels of condom availability are similar between public and private facilities in Kenya, but the difference is larger for IUD and implant availability.
Analysis of MCM stocks by facility type confirmed previous findings by others that while primary care facilities are important outlets for contraceptives in the public sector, pharmacies and drug shops dominate the private sector. Pharmacies and drug shops have an important role to play in achieving FP2020 objectives particularly in SSA countries where they serve as crucial outlets for addressing the unmet need in short-acting contraceptives for vulnerable and hard-to-reach populations (Corroon et al., 2016; Riley et al., 2018). Recent evidence points to the popularity of drug shops, in particular, as preferred SDPs for young women and unmarried women (High-Impact Practices in Family Planning, 2013; Corroon et al., 2016; Weinberger and Callahan, 2017), though their potential likely remains under-leveraged.
In general, we noted that the patterns of stock supply and client volume corroborated findings from previous studies examining client-level data in contraceptive use. For example, the high client volume and method availability observed across the sites in Kenya relative to other SSA countries is consistent with a previous study showing that Kenya had the highest modern contraceptive rate among the countries in the study (Ahmed et al., 2019).
Consistent with other studies, our findings showed limited availability for long-acting reversible contraceptives (LARCs), including IUDs and implants, with great variability between countries (Grindlay et al., 2016; Thanel et al., 2018). The findings further showed that LARCs were generally more readily available and distributed through the public sector as compared to the private sector. LARCs are highly effective forms of reversible birth control as evidenced by the large proportion of CYPs they provided in our study despite the consistently high levels of stockouts and lower numbers of client visits that they were subject to. Compared to short-acting methods, they have higher upfront costs but are more cost-effective over time, generally well-tolerated by women and thus less likely to be discontinued (World Health Organization, 2012; Diedrich et al., 2015; Thanel et al., 2018; Römer and Linsberger, 2009). Nonetheless, the requirements for service readiness for LARC delivery are decidedly more complex than those for short-acting methods. For instance, service readiness for implant and IUD insertion typically requires the availability of the contraceptive commodity, appropriately trained and credentialed providers and the necessary equipment for insertions. It is thus likely that the low levels of LARC availability observed across countries can be attributed to the limited capacity of country health systems to sustain adequate levels of service readiness for LARCs. With the aim of addressing the shortcomings related to service readiness, some countries, including Nigeria, have made commitments to increase FP program funding while pursuing task-shifting policies geared towards expanding service delivery for LARCs (Scoggins and Bremner, 2020). Nonetheless, our findings suggest that further action is needed from governments, FP program managers and international donors to leverage underutilized private sector primary care providers and continue striving towards improved access to LARCs.
Based on client volume data for LARCs, we observed that implants were consistently distributed at higher levels than IUDs in SSA. This is consistent with previous studies that have shown higher levels of implant use relative to IUDs in several African countries (Duvall et al., 2014; Tsui et al., 2017). While implants possess relative advantages and attributes that users like about them as previously discussed by others (Ortayli, 2002; Jacobstein and Stanley, 2013), it is worthwhile to also note that the introduction of implants in SSA benefitted from considerable international assistance to expand access to the method and manage supply chains (Duvall et al., 2014; Tsui et al., 2017).
Total CYPs in India appeared to be lower than those in SSA countries. This was likely due to the lack of contribution of implants to total CYPs as the method is currently not offered in India. Though implants are offered in the DRC, the total CYPs provided were still low compared to other African geographies likely due to the low client volume for IUDs. These findings not only highlight the importance of ensuring the availability of LARC choice for maximum protection against unintended pregnancies but also the value of examinations of country-specific method mix when attempting cross-country comparisons. As others have previously reported, trends in method mix may vary considerably across and within geographies thereby raising programmatic issues that need to be addressed in order to address client needs (Bertrand et al., 2020).
Our goal in this research is primarily descriptive; we do not seek to explain why stockouts occur or why certain methods are consumed more than others, as doing so would require the measurement of environmental and supply factors that were out of the scope of PMA Agile. For example, we understand from correspondence with PMA Agile personnel that declines in stock of MCMs and in client visits for MCMs in Burkina Faso were due to a public sector strike that took place between June and November of 2019. Additionally, the Indian MoH launched the ‘Antara Programme’ in 2017 with the aim of providing injectables free of charge in public facilities (Ministry of Health and Family Welfare, 2017b). Though this potentially explains the remarkable increase in injectable availability and consumption in the public sector in India, we do not capture information on such programmatic changes, potential disruptions to service delivery or other similar environmental impacts on stockouts.
Although PMA Agile did not collect information on the reason for stockouts, the PMA Core project (PMA, 2020) recently did so in four geographies that overlap with the countries chosen here: Kenya, Burkina Faso, DRC and Nigeria. Across all countries and methods, the most common reason for stockouts is that the facility claims to have ordered the method but did not receive the requested shipment. The delays in making contraceptives available in India are likely due to weak monitoring of the contraceptive method supply and consumption at all levels of the health system (Ministry of Health and Family Welfare, 2017a). In response, the Indian government recently rolled out the Family Planning Logistics Management Information System (FPLMIS) (Ministry of Health and Family Welfare, 2017a). The FPLMIS is expected to empower state-level program managers, facility-level stock managers as well as community health workers manage stocks of contraceptive commodities more effectively.
Although a detailed examination of the relationship between contraceptive procurement, supply chain management and stockouts was beyond the scope of this research, our findings nonetheless have the potential to inform ongoing debates about the merits of different contraceptive distribution models vis-à-vis stockouts. For example, whereas Burkina Faso and DRC use a ‘pull system’ in which procurement is decentralized and multiple low-level actors place contraceptive orders from central hubs based on their forecasted needs (PATH, 2017; Babazadeh et al., 2018), Nigeria uses a variation of the push system in which the central hubs are responsible for resupplying SDPs with contraceptives (USAID | DELIVER PROJECT, 2014) with Kenya using a combination of the two systems (Eliya Msiyaphazi Zulu et al., 2012). Yet, it was not entirely clear from our findings whether contraceptive stockouts vary based on the distribution model employed, considering the differences in contraceptive consumption across countries. Given our observations that stockouts vary based on geographic setting, sector and contraceptive method, we recommend that country stakeholders adopt context-specific and problem-based approaches to address procurement challenges for individual methods. Considering the rapid fluctuations observed in both contraceptive consumption and stockout rates, the approaches will need to be flexible and cost-effective in order to sustainably address unmet need.
On the basis of the PMA Core observation that failure to receive requested contraceptive orders was the most common cause of stockouts among SDPs in African geographies, it is probable that countries may benefit from the Informed Push Model (IPM), which achieved dramatic reductions in stockouts in Senegal largely by transferring the responsibility of order placement and delivery from SDPs to an external professional logistician (Daff et al., 2014) The model’s ability to couple information collection and product distribution by dedicated professionals enhances supply chain performance ultimately strengthening the health system’s ability to respond to the healthcare needs of the population. Furthermore, IPM avoids the requirement for facilities to pay for contraceptive supplies upfront, a situation which may exacerbate supply chain issues (Hasselback et al., 2017). As others have indicated, upfront payments may drive some facilities to use their working capital thus delaying the replenishment of funds until after clients have purchased contraceptive commodities (Hasselback et al., 2017). The funding delays may in turn result in cash flow problems for some facilities or encourage the diversion of the remaining capital towards more profitable non-contraceptive commodities. Given the success of IPM in addressing these issues, we therefore recommend country-specific analyses comparing costs associated with current distribution channels for individual methods to the costs associated with alternative distribution models including IPM.
There is limited data on MCM stockouts in low- and middle-income settings, and most available data offer annual averages that do not provide the opportunity to examine short-term trends in stockouts. The quarterly PMA Agile data therefore fill an important gap in the literature, by tracking within-year changes in stockouts, CYPs and client volume across five different settings. We also provide a contrast between public and private facilities which greatly increases the representativeness of our findings.
This research also has some limitations. The PMA Agile platform offers an online dashboard displaying trends obtained from the analysis of repeated cross-sectional surveys (PMA Agile, 2020). There may be instances where our results differ slightly from the dashboard results since our analytical dataset contained SDPs that were followed longitudinally across at least two quarters. We also note that in some instances, such as in the public sectors for Burkina Faso and India, the sample size of facilities is small. Furthermore, our analyses combine different types of SDPs which are in turn probably subject to different variation in terms of method availability and client volume. In future studies, we plan to conduct facility-level analyses that address these concerns. Though REs were able to access facility logbooks and record product sales and client visit data, we are unable to comment on the extent to which the data were accurate or complete. With the exception of SDPs in Burkina Faso and public SDPs in DRC, the proportion of facilities contributing data was generally high across countries as evidenced by the number of SDPs contributing to CYP units.
Finally, the survey data were subject to sampling and non-sampling errors.
The majority of research on FP and contraceptive use has focused on demand-side measures, such as fertility preferences, individual-level predictors of modern contraceptive use and characteristics associated with unmet need. In this research, we demonstrate the value of supply-side measures by showing trends in contraceptive supply and stockout over a short period of time. We expect that this information may help monitor progress towards addressing an unmet need and inform cross-country strategies to anticipate, reduce and prevent stockouts.
Supplementary Material
Acknowledgements
The PMA Agile team wishes to acknowledge the helpful cooperation of The Challenge Initiative project and DKT International and the support of the many staff on the in-country Agile teams and local health departments.
Contributor Information
Pierre Muhoza, Department of International Health, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe Street, Baltimore, MD 21205, USA.
Alain K Koffi, Department of International Health, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe Street, Baltimore, MD 21205, USA.
Philip Anglewicz, Department of Population, Family and Reproductive Health, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe Street, Baltimore, MD 21205, USA.
Peter Gichangi, International Centre for Reproductive Health Kenya, Nairobi, Kenya.
Georges Guiella, Institut Supérieur des Sciences de la Population (ISSP) of the Joseph Ki-Zerbo University, Ouagadougou, Burkina Faso.
Funmilola OlaOlorun, Department of Community Medicine, University of Ibadan, Ibadan, Nigeria.
Elizabeth Omoluabi, Centre for Research, Evaluation Resources and Development, Ife, Nigeria.
P R Sodani, IIHMR University, Jaipur, India.
Mary Thiongo, International Centre for Reproductive Health Kenya, Nairobi, Kenya.
Pierre Akilimali, Ecole de Santé Publique de l'Université de Kinshasa, Kinshasa, Democratic Republic of Congo.
Amy Tsui, Department of Population, Family and Reproductive Health, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe Street, Baltimore, MD 21205, USA.
Scott Radloff, Department of Population, Family and Reproductive Health, Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe Street, Baltimore, MD 21205, USA.
Funding
This work was supported by the Bill and Melinda Gates Foundation [grant numbers OPP1163884, OPP1079004]. PMA Agile is a survey research project implemented by the Bill and Melinda Gates Institute for Population and Reproductive Health at the Johns Hopkins Bloomberg School of Public Health, funded by the Bill and Melinda Gates Foundation. The findings and conclusions contained within are those of the authors and do not necessarily reflect positions or policies of the Bill and Melinda Gates Foundation.
Conflict of interest statement. None declared.
Ethical approval. PMA Agile data collection protocols were reviewed and approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board and the in-country counterpart review board: Kenyatta National Hospital-University of Nairobi Ethics Research Committee; National Health Research Ethics Committee of Nigeria; MOH-Burkina Comité d’Ethique pour la Recherche en Santé; University of Kinshasa School of Public Health Institutional Review Board; Indian Institute for Health Management Research Ethical Review Board. All participants provided verbal consent in accordance with country-specific approved consent procedures.
References
- Ahmed S, Li Q, Liu L. et al. 2012.Maternal deaths averted by contraceptive use: an analysis of 172 countries. The Lancet 380: 111–25. [DOI] [PubMed] [Google Scholar]
- Ahmed S, Choi Y, Rimon JG. et al. 2019.Trends in contraceptive prevalence rates in sub-Saharan Africa since the 2012 London Summit on Family Planning: results from repeated cross-sectional surveys. The Lancet Global Health 7: e904–e911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali M, Farron M, Dilip TR et al. 2018.Assessment of family planning service availability and readiness in 10 African countries. Global Health: Science and Practice 6: 473–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babazadeh S, Lea S, Kayembe P et al. 2018.Assessing the contraceptive supply environment in Kinshasa. DRC: trend Data from PMA2020, Health Policy and Planning 33: 155–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertrand JT, Ross J, Sullivan TM. et al. 2020.Contraceptive method mix: updates and implications. Global Health: Science and Practice 8: 666–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SS, Eisenberg L.. 1995. Socioeconomic and Cultural Influences on Contraceptive Use the Best Intentions: Unintended Pregnancy and the Well-Being of Children and Families. Washington, DC:National Academies Press (US; ). [PubMed] [Google Scholar]
- Brown W, Druce N, Bunting J. et al. 2014.Developing the “120 by 20” goal for the Global FP2020 Initiative. Studies in Family Planning 45: 73–84. [DOI] [PubMed] [Google Scholar]
- Chandra-Mouli V, McCarraher DR, Phillips SJ. et al. 2014.Contraception for adolescents in low and middle income countries: needs, barriers, and access. Reproductive Health 11: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corroon M, Kebede E, Spektor G. et al. 2016.Key role of drug shops and pharmacies for family planning in urban Nigeria and Kenya. Global Health: Science and Practice 4: 594–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daff BM, Seck C, Belkhayat H et al. 2014.Informed push distribution of contraceptives in Senegal reduces stockouts and improves quality of family planning services. Global Health: Science and Practice 2: 245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darroch JE, Sedgh G, Ball H.. 2011. Contraceptive Technologies: Responding to Women’s Needs, Vol. 201.New York:Guttmacher Institute. [Google Scholar]
- DHS Program. 2017. The Service Provision Assessment (SPA). https://dhsprogram.com/What-We-Do/Survey-Types/SPA.cfm, accessed 7 July 2020.
- Diedrich JT, Zhao Q, Madden T et al. 2015.Three-year continuation of reversible contraception. Am J Obstet Gynecol 213: 662e661–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do M, Kurimoto N.. 2012.Women's empowerment and choice of contraceptive methods in selected African countries. International Perspectives on Sexual and Reproductive Health 38: 23–33. [DOI] [PubMed] [Google Scholar]
- Duvall S, Thurston S, Weinberger M et al. 2014.Scaling up delivery of contraceptive implants in sub-Saharan Africa: operational experiences of Marie Stopes International. Global Health: Science and Practice 2: 72–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliya Msiyaphazi Zulu D, Musila NR, Murunga V et al. 2012. Assessment of Drivers of Progress in Increasing Contraceptive use in sub-Saharan Africa: Case Studies from Eastern and Southern Africa. African Institute for Development Policy (AFIDEP). Lilongwe, Malawi. https://media.africaportal.org/documents/Assessment_of_Drivers.pdf, accessed 19 November 2020. [Google Scholar]
- FP 2020. 2015. FP2020. Momentum at the Midpoint 2015-16. http://2015-2016progress.familyplanning2020.org/page/measurement/contraceptive-stock-outs-and-availability-indicators-10-11, accessed 18 June 2020.
- Grindlay K, Turyakira E, Kyamwanga IT et al. 2016.The experience and impact of contraceptive stockouts among women, providers and policymakers in two districts of Uganda. International Perspectives on Sexual and Reproductive Health 42: 141–50. [DOI] [PubMed] [Google Scholar]
- Guttmacher Institute. 2017. Adding It up: Investing in Contraception and Maternal and Newborn Health, 2017.New York:Guttmacher Institute. [Google Scholar]
- Hasselback L, Dicko M, Viadro C et al. 2017. Understanding and Addressing Contraceptive Stockouts to Increase Family Planning Access and Uptake in Senegal, Vol. 17, 373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa SG, West BT, Berglund PA.. 2017. Applied Survey Data Analysis. Boca Raton, Florida:Chapman and Hall/CRC. [Google Scholar]
- Hernandez JH, Mbadu MF, Garcia M. et al. 2018.The provision of emergency contraception in Kinshasa's private sector pharmacies: experiences of mystery clients. Contraception 97: 57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- High-Impact Practices in Family Planning. 2013. Drug Shops and Pharmacies: sources for family planning commodities and information. Brief. USAID Washington DC, USA. http://www.fphighimpactpractices.org/briefs/drug-shops-and-pharmacies/, accessed 19 November 2020. [Google Scholar]
- Hubacher D, Mavranezouli I, McGinn E.. 2008.Unintended pregnancy in sub-Saharan Africa: magnitude of the problem and potential role of contraceptive implants to alleviate it. Contraception 78: 73–8. [DOI] [PubMed] [Google Scholar]
- Hutchinson PL, Do M, Agha S.. 2011.Measuring client satisfaction and the quality of family planning services: a comparative analysis of public and private health facilities in Tanzania, Kenya and Ghana. BMC Health Services Research 11: 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobstein R, Stanley H.. 2013.Contraceptive implants: providing better choice to meet growing family planning demand. Global Health: Science and Practice 1: 11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi B, Sachina O, Begum S.. 2019. Health Technology Assessment of Long Acting Reversible Contraceptives in India.Mumbai, India:National Institute for Research in Reproductive Health. Indian Council of Medical Research. https://dhr.gov.in/sites/default/files/HTA_%20LARC%20in%20India.pdf, accessed 19 November 2020. [Google Scholar]
- Kakoko DC, Ketting E, Kamazima SR et al. 2012.Provision of family planning services in Tanzania: a comparative analysis of public and private facilities. African Journal of Reproduction Health 16: 140–8. [PubMed] [Google Scholar]
- Maharaj P, Rogan M.. 2008.Emergency contraception in South Africa: a literature review. The European Journal of Contraception & Reproductive Health Care 13: 351–61. [DOI] [PubMed] [Google Scholar]
- Mané B, Brady M, Ramarao S. et al. 2015.Emergency contraception in Senegal: challenges and opportunities. The European Journal of Contraception & Reproductive Health Care 20: 64–73. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Family Welfare. 2017a. Family Planning Logistics Management Information System (FP-LMIS): Training Manual and User Guide.Family Planning Division: Ministry of Health and Family Welfare: Government of India. http://www.rajswasthya.nic.in/FPLIMIS/FP-LMIS%20Training%20Manual.pdf, accessed 23 December 2020. [Google Scholar]
- Ministry of Health and Family Welfare. 2017b. Health Ministry Launches Two New Contraceptives: Press Information Bureau, Government of India.https://pib.gov.in/newsite/PrintRelease.aspx?relid=170537, accessed 19 November 2020. [Google Scholar]
- Ortayli N. 2002.Users’ perspectives on implantable contraceptives for women. Contraception 65: 107–11. [DOI] [PubMed] [Google Scholar]
- PATH. 2017. How to Introduce and Scale up Sayana Press (DMPA-SC in Uniject): Practical Guidance from PATH Based on Lessons Learned during Pilot Introduction.Seattle, WA, USA:PATH. [Google Scholar]
- PMA. 2020. PMA: Results from Phase 1 Baseline Survey. https://www.pmadata.org, accessed 19 November 2020.
- PMA Agile. 2020. www.pmadata.org/technical-areas/pma-agile, accessed 28 June 2020.
- Riley C, Garfinkel D, Thanel K, on behalf of the FPwatch Group et al. 2018.Getting to FP2020: harnessing the private sector to increase modern contraceptive access and choice in Ethiopia, Nigeria, and DRC. PLoS One 13: e0192522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Römer T, Linsberger D.. 2009.User satisfaction with a Levonorgestrel-releasing intrauterine system (LNG-IUS): data from an international survey. The European Journal of Contraception & Reproductive Health Care 14: 391–8. [DOI] [PubMed] [Google Scholar]
- Ross J, Hardee K.. 2013.Access to contraceptive methods and prevalence of use. Journal of Biosocial Science 45: 761–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scoggins S, Bremner J.. 2020. FP2020: The Way Ahead, 2016–2017: Family Planning. [Google Scholar]
- Stover J, Ross J.. 2010.How increased contraceptive use has reduced maternal mortality. Maternal and Child Health Journal 14: 687–95. [DOI] [PubMed] [Google Scholar]
- Thanel K, Garfinkel D, Riley C, on behalf of the FPwatch Group et al. 2018.Leveraging long acting reversible contraceptives to achieve FP2020 commitments in sub-Saharan Africa: the potential of implants. PLoS One 13: e0195228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson J, Undie C-C, Amin A. et al. 2018.Harmonizing national abortion and pregnancy prevention laws and policies for sexual violence survivors with the Maputo Protocol: proceedings of a 2016 regional technical meeting in sub-Saharan Africa. BMC Proceedings 12: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsui A, Anglewicz P, Akinlose T. et al. 2020.Performance monitoring and accountability: the Agile Project’s protocol, record and experience. Gates Open Research 4: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsui AO, Brown W, Li Q.. 2017.Contraceptive practice in sub-Saharan Africa, Population and development review. 43(Suppl 1): 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USAID. 2018. USAID Global Health Supply Chain Program: 2017 Contraceptive Security Indicators Report.Washington DC:Chemonics International Inc. [Google Scholar]
- USAID. 2019. Couple of Years of Protection (CYP). https://www.usaid.gov/global-health/health-areas/family-planning/couple-years-protection-cyp, accessed 18 June, 2020.
- USAID | DELIVER PROJECT, Task Order 4 and Task Order 7. 2014. Nigeria: Direct Delivery and Information Capture Activities: March 2012–August 2014.Abuja, Nigeria:USAID. [Google Scholar]
- Wang W, Mallick L.. 2019.Understanding the relationship between family planning method choices and modern contraceptive use: an analysis of geographically linked population and health facilities data in Haiti. BMJ Global Health 4(Suppl 5): e000765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger M, Callahan S.. 2017. The Private Sector: Key to Achieving Family Planning 2020 Goals. Brief. Bethesda, MD:Sustaining Health Outcomes through Private Sector Project, Abt Associates. [Google Scholar]
- WHO 2018. Family planning/Contraception. https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception, accessed 15 February 2019.
- World Health Organization. 2012.From Evidence to Policy: Expanding Access to Family Planning. Strategies to Increase Use of Long-acting and Permanent Contraception.Geneva:WHO. [Google Scholar]
- Zimmerman LA, Bell SO, Li Q, et al. PMA2020 Principal Investigators Group. 2019.Individual, community and service environment factors associated with modern contraceptive use in five Sub-Saharan African countries: a multilevel, multinomial analysis using geographically linked data from PMA2020. PLoS One 14: e0218157. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.