Abstract
Research is needed to identify how to effectively tailor evidence-based interventions across cultures with limited resources, particularly for behavioral components in large HIV prevention trials. Through surveys and interviews with counselors of sub-Saharan African women during an open-label microbicide trial (MTN-025), we examined language, education and cultural barriers in delivering a Motivational Interviewing-based adherence counseling intervention (i.e., Options Counseling). Counselors encountered an array of barriers; most prominently, that participants struggled to comprehend culturally incongruent pictorial guides, such as traffic light images, and to uphold product use when primary partners disapproved. Overwhelmingly, counselors cited the intervention’s inherent flexibility as an asset; it encouraged them to tailor language and examples to be more culturally relevant to participants. Future resource-conscious researchers may preemptively offset similar barriers by consulting with communities during intervention development. Similarly, affording counselors flexibility while delivering the chosen intervention may enable them to troubleshoot barriers that arise on the ground.
Keywords: counseling, Africa, HIV prevention, cultural tailoring, intervention development, cultural barriers to adherence
Introduction
Culturally adapting effective evidence-based interventions (EBIs) to accommodate the unique needs of diverse populations remains challenging for behavioral HIV researchers. Researchers have emphasized the need to strike a careful balance between: 1) modifying the chosen EBI to enhance its salience and acceptability among members of the intended target population, and 2) ensuring its fidelity to the original intervention’s internal logic and core components (i.e., the elements believed to be responsible for the intervention’s effectiveness; Barrera Jr., Castro, Strycker, & Toobert, 2013; Bell et al., 2007; Card, Solomon, & Cunningham, 2011; Dévieux, Malow, Rosenberg, & Dyer, 2004; Dworkin, Pinto, Hunter, Rapkin, & Remien, 2008; Kelly et al., 2000; McKleroy et al., 2006; Tortolero et al., 2005; Wainberg et al., 2007; Wingood & DiClemente, 2008). Adaptations that fail to adequately address a new population’s cultural context or that compromise the original intervention’s core components are less likely to be effective in promoting desired behavioral outcomes (Bell et al., 2007; Morrison et al., 2007; Stanton et al., 2006; Tortolero et al., 2005; Wingood & DiClemente, 2008; Zimmerman, Cupp, Donohew, Sionéan, Feist-Price, & Helme, 2008).
Despite potential pitfalls, researchers have used culturally adapted interventions to effectively foster HIV risk-reduction behaviors among new target populations (Darbes, Crepaz, Lyles, Kennedy, & Rutherford, 2008; Gaydos, Hsieh, Galbraith, Barnes, Waterfield, & Stanton, 2008; Kelly et al., 2000; Kennedy, Mizuno, Hoffman, Baume, & Strand, 2000; Kirby 2002; Lightfoot, Kasirye, Comulada, & Rotheram-Borus, 2007; Pedlow & Carey, 2004; Scott, Gilliam, & Braxton, 2005; Stanton et al., 2006; Vinh-Thomas, Bunch, & Card, 2003; Wilson & Miller, 2003). In a systematic review, Barrera Jr. et al. (2013) examined publications from the past decade for recommendations on adapting EBIs effectively for diverse cultures while retaining core components. The authors synthesized this process into five successive stages: 1) information gathering (e.g., formative studies), 2) preliminary adaptation design (e.g., translations and back translations), 3) preliminary adaptation tests (e.g., pilot testing), 4) adaptation refinement (e.g., revisions based on pilot study findings), and 5) cultural adaptation trial (e.g., full scale trial).
As evidenced in this five-stage model, the procedures required to adapt an intervention to meet the needs of a new cultural group can be quite exhaustive, requiring an abundance of time, funding, and resources. However, large biomedical HIV prevention trials are typically designed to evaluate the efficacy of the biomedical product being investigated – not the behavioral EBI intended to foster adherence. Thus, researchers do not generally possess sufficient resources to systematically adapt behavioral interventions in these contexts (Gandelman & Rietmeijer, 2004; Gordon, Forsyth, Stall, & Cheever, 2005; Kelly et al., 2000; Oliva, Rienks, Udoh, & Smith, 2005; Solomon, Card, & Malow, 2006; Stanton et al., 2006). As a workaround, these trials often utilize existing EBIs that were not originally developed to accommodate the cultural nuances of new target populations. Yet, given the potential for culturally adapted EBIs to yield positive behavior change, it is crucial to evaluate even abbreviated attempts to adapt behavioral interventions; such research may elucidate more feasible and less resource-intensive strategies for culturally tailoring EBIs to be more relevant to diverse target populations.
This paper examines counselor perspectives on the language, educational, and cultural barriers experienced by participants receiving an evidenced-based adherence counseling intervention during the HOPE Study (MTN-025), a biomedical HIV prevention trial aimed at characterizing safety and adherence associated with use of the dapivirine ring. Additionally, we explore counselors’ strategies for navigating these challenges and use their accounts to inform recommendations for how researchers could tailor adherence interventions to pre-emptively offset similar challenges in future HIV prevention trials.
Methods
The HOPE Study
The HOPE Study (MTN-025) was a Phase 3B trial to characterize safety and adherence associated with open-label dapivirine ring use among women across fourteen study sites in four African countries (Baeten et al., in press). It was the largest biomedical HIV prevention study in which adherence counseling sessions were audio-recorded to enable systematic fidelity monitoring of the delivery of the adherence intervention – Options Counseling (Balán et al., 2020).
Options was designed to support women in successfully using any HIV prevention method(s) of their choosing, regardless of whether their choice included the ring. This represented a marked shift from the previous ring study, MTN-020/ASPIRE, from which all HOPE Study participants were recruited; in ASPIRE, these women had been required to use the ring at all times. However, there were significant inconsistencies between participants’ self-reports and adherence biomarkers in ASPIRE (Mensch et al., 2019), highlighting a need for a counseling approach that facilitated open discussions of challenges to product use.
Study visits occurred monthly for the first three months and quarterly for the following nine months. Participants underwent Options at each visit. Those who chose to use the ring were instructed to return used rings to the clinic so that the amount of residual dapivirine left in each could be determined. In short, these residual drug levels served as an alternative way to measure and facilitate discussions about adherence. Participants were given a “Protection Level” for each used ring, ranging from 0 (No Protection) to 3 (High Protection); in essence, these levels were numerical approximations that corresponded to the amount of drug, and therefore HIV protection, participants received from each of their rings.
Options Counseling: Development
Options Counseling was a Motivational Interviewing (MI; Miller & Rollnick, 2013)-based intervention developed to foster open conversations about challenges to adherence. MI has been used effectively throughout the world, including sub-Saharan Africa, to facilitate a range of desired behavioral changes (e.g., reduce sexual risk behaviors, increase antiretroviral medication adherence; Carlbring, Jonsson, Josephson, & Forsberg, 2010; Gisore, Kaseje, Were, & Ayuku, 2014; Holstad, Dilorio, Kelley, Resnicow, & Sharma, 2011; Krummenacher, Cavassini, Bugnon, & Schneider, 2011; Mbuagbaw, Ye, & Thebane, 2012; Naar-King, Parsons, & Johnson, 2012; Parsons, Rosof, Punzalan, & Di Maria, 2005; Rongkavilit et al., 2014). It is a person-oriented style of counseling that leverages internal motivations to facilitate behavior change (Oh & Lee, 2016; Miller et al., 2013); thus, the intervention’s focus on participants’ needs supported counselors in tailoring their delivery of Options to address barriers they encountered with participants.
Options included a set series of session tasks geared toward eliciting participants’ experiences with the ring and/or other HIV prevention methods and aimed to help them develop and sustain an HIV prevention plan. Throughout these tasks, Options emphasized global MI concepts, such as collaboration, empathy, respect for participant’s autonomy, and evocation. At follow-up visits, counselors informed participants of their residual drug level results, and this information was used to help inform participants’ future HIV prevention plans. Counselors were equipped with a counseling manual and a tabletop flipchart in local languages that followed the task sequence and could be used as a guide to facilitate a conversational tone during sessions. The flipchart was light on text and included images and visual exercises to engage participants. More detailed descriptions of the counseling intervention, counselor training, and perspectives on residual drug level discussions have been previously published (Giguere et al., in press; Kutner et al., 2020).
Prior to the start of HOPE, counselors attended a brief workshop in client-centered counseling in Durban, South Africa. English language tabletop flipcharts were then developed and utilized by counselors in a subsequent, more extensive in-person training in Cape Town, South Africa; the flipchart was revised based on counselor feedback. Representatives from each study site reviewed the revised flipchart and provided forward and back translations. In turn, the team of New York City-based fidelity raters, who were fluent in the sites’ local languages and were hired to assess completed counseling sessions for intervention fidelity, reviewed the flipchart translations and provided additional input. Feedback from the fidelity team was sent back to the sites so they could clarify discrepancies and finalize the translations.
Further feedback was obtained from counselors during monthly coaching calls with the lead investigator, Dr. Ivan Balán, who developed Options and trained the counselors. This ongoing dialogue provided the study team with an opportunity to guide counselors in tailoring Options concepts that participants were struggling to grasp.
The Counselors’ Study Procedures
To understand counselors’ experiences delivering Options, we initiated an ancillary study, “Implementation of Options in HIV Prevention Counseling in HOPE,” after HOPE had concluded. All HOPE counselors who had conducted at least ten counseling sessions, and were therefore well-versed in Options, were invited to participate.
The study team recruited counselors from HOPE via email outreach to participate in an online survey and, if interested, an in-depth interview (IDI). Counselors who consented to participate were routed to the online survey, which included demographic questions and asked counselors to rate participants’ difficulty comprehending intervention components. Once all counselors at a given site had completed the consent process, the study team randomly selected up to two willing counselors to be interviewed. The audio-recorded IDI was conducted in English via telephone by a trained interviewer who had not worked with the counselor during HOPE.
All study procedures for both the HOPE and subsequent ancillary study were reviewed and approved by the Institutional Review Boards/Ethics Committees at all participating sites, including fourteen sites in South Africa, Malawi, Uganda, and Zimbabwe, and the New York State Psychiatric Institute IRB.
Data Collection
Measures
For the online survey, counselors were asked “In general, how many participants found each of the following Options components difficult to understand?” in tandem with an image from the Options flipchart and a brief description of the session task it portrayed. The nine components they evaluated are listed verbatim in Table 1. Participants responded using a 4-point Likert scale (1= Few participants; 2= Some participants; 3= Many participants; 4= Most participants).
One item in the survey assessed language barriers: “What proportion of sessions did you conduct in a language that was not the participant’s primary language?” Again, counselors responded using a 4-point Likert scale (1= Less than 10%; 2= More than 10% but less than 20%; 3= More than 20% but less than 30%; 4= More than 30%).
The IDI guide covered a variety of topics, including the language, educational, and cultural barriers counselors encountered while conducting Options with participants. For each of these domains, counselors shared any barriers they encountered and responded to two follow-up probes: 1) “What questions or concepts did participants not understand?” and 2) “What did you do to try to help them understand the questions or the concepts?”
Data Analysis
Survey data was analyzed in SPSS (v25); frequencies and percentages are reported where appropriate.
All IDI audio files were transcribed by a professional transcription company and checked for accuracy. The lead investigator and research team developed a qualitative codebook based on the interview guide and study objectives. Interviews were uploaded to NVivo (v11) and were coded by two independent coders who met periodically to assess inter-rater reliability as well as discuss and resolve all coding discrepancies. For this paper, we extracted the coding reports for “Language barriers,” “Educational barriers,” and “Cultural barriers.” Using thematic analysis (Patton 1990), we then identified common themes related to participant barriers as well as strategies that counselors used to help participants overcome these barriers. Finally, we explored the report for cases that contradicted the main trends. All quotes have been cleaned for accuracy and comprehension without compromising their integrity.
Results
Sample Description
In total, 42 counselors spanning all 14 study sites completed the online quantitative survey; twenty-two counselors from 13 sites underwent IDIs. Of the 42 counselors who completed the quantitative assessment, thirty-nine (93%) identified as female and forty (95%) had completed some form of education beyond high school. Thirty-seven (88%) counselors had earned either a counseling degree or a counseling certificate/diploma; only three (7%) reported no counseling experience prior to the HOPE Study.
Online Survey
Counselors’ perceptions of the proportion of participants who had trouble understanding Options tasks are presented in Table 1. Four session tasks were most difficult for participants to comprehend; eight (19.1%) or more counselors indicated that “many” or “most” participants struggled with each. In order of greatest perceived difficulty, these were the tasks pertaining to “Participant’s own drug level results,” “General information about drug level results,” “Assessing how the participant is feeling about her prevention plan,” and “Problem-solving ways to maintain/improve the participant’s prevention plan.” The tabletop flipchart slides that correspond to the latter two tasks, which relied heavily upon pictorial guides, are displayed in Figure 1.
Table 1.
Proportion of Participants Who Had Difficulty Comprehending Each Task (N=42)
| Options Counseling step/component: | Most participants N (%) |
Many participants N (%) |
Some participants N (%) |
Few participants N (%) |
|---|---|---|---|---|
| Respect for participant’s choice to use or not use the Ring | 1 (2.4%) | 3 (7.1%) | 13 (31.0%) | 25 (59.5%) |
| Developing an HIV prevention plan | 0 (0%) | 5 (11.9%) | 11 (26.2%) | 26 (61.9%) |
| General information about drug level results | 4 (9.5%) | 7 (16.7%) | 13 (31.0%) | 18 (42.9%) |
| Participant’s own residual drug level results | 6 (14.3%) | 9 (21.4%) | 14 (33.3%) | 13 (31.0%) |
| Exploring how participant’s HIV prevention plan has been going | 1 (2.4%) | 6 (14.3%) | 11 (26.2%) | 24 (57.1%) |
| Assessing how participant is feeling about the prevention plan | 0 (0%) | 9 (21.4%) | 15 (35.7%) | 18 (42.9%) |
| Problem-solving ways to maintain/improve the prevention plan | 2 (4.8%) | 6 (14.3%) | 15 (35.7%) | 19 (45.2%) |
| Assessing upcoming events that might affect the prevention plan | 2 (4.8%) | 4 (9.5%) | 15 (35.7%) | 21 (50.0%) |
| Assessing confidence in implementing the prevention plan | 2 (4.8%) | 2 (4.8%) | 17 (40.5%) | 21 (50.0%) |
Figure. 1. Options Counseling tasks participants had difficulty comprehending.
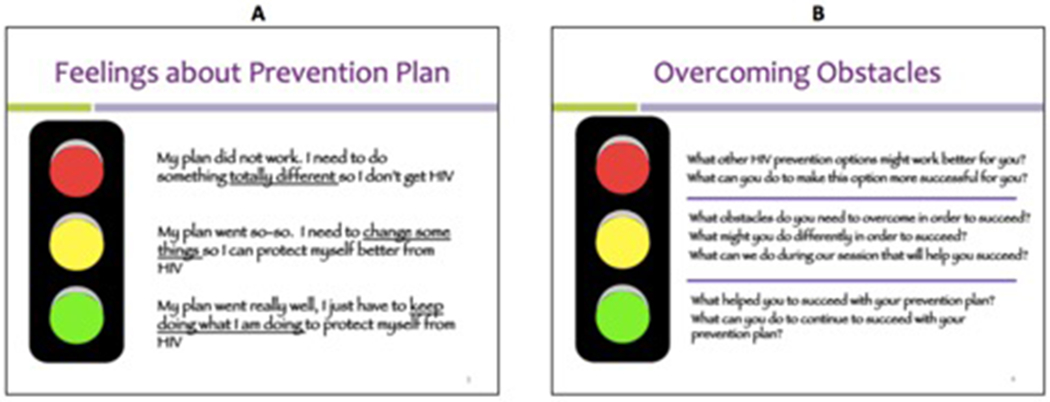
A) Assessing how participant is feeling about the HIV prevention plan
B) Problem-solving ways to maintain/improve the prevention plan
Among the 40 (95%) counselors who reported conducting a session in a language other than their participants’ primary one, 34 (85%) used this second dialect in less than 10% of their sessions, two (5%) for 10–20% of their sessions, and four (10%) for 30% or more of their sessions.
In-Depth Interviews
Language Barriers
Regarding language, half (n=11) of the interviewed counselors did not experience any barriers while conducting Options; most (n=9) attributed this to the fact that the tabletop flipchart had been successfully translated into their site’s local language.
“I think the flipchart messages were well translated to our language, the local language that we use here, such that the language was not a barrier to communication. And I don’t remember encountering someone failing to proceed with the discussion because they didn’t understand the language.” – Counselor #1305
“Because most of our participants understand the local language very well. So, we didn’t have any problem. And our flip chart was well translated.” – Counselor #1202
Consistent with survey data, few (n=3) counselors reported encountering language barriers so major that they needed to conduct Options in a language other than the participant’s primary one. However, some (n=6) counselors experienced a minor language barrier: the intervention’s research-oriented language did not always translate well into the site’s local community language. Counselors attributed this to the fact that, while the scripted language was technically correct, it did not reflect commonly spoken language.
“Coming to the real world, you are no longer doing what you did in the mock sessions, you’re now using your own language. Initially it was a bit difficult -- maybe you use the word “obstacle,” and not that they don’t understand what obstacles are, but it’s different when you say it in your own language. With time you find out, this is the time when I use that Shona word or that certain word.” – Counselor #1302
“What I can indicate is that we all know that here, in South Africa, we are using our local languages. But we also know that we have a universal research language. So, if you translated the research language to the local language, that itself might have a little impact on the meanings and the flow of the communication itself.” – Counselor #305
To rectify these translational discrepancies, some (n=6) counselors relied upon their experience with the local language and adapted the phrasing of the tabletop flipchart to enhance participant comprehension and acceptability.
“I wouldn’t say I had any challenges, because as I was going through the flipchart, I was explaining it and speaking to participants using the common language or the common understanding that we have. I was just using that flip chart very sparingly, so I didn’t come across those challenges. However, if we read through the flipchart, the words are used differently opposed to the kind of way that we speak currently.” – Counselor #904
“When we mention very private parts we -- there are some words that participants don’t feel comfortable using. And those words we don’t normally use. We use words that they could feel comfortable with… Yes. Even the words, the translation of the words. We put them in language that our clients would feel comfortable discussing.” – Counselor #1202
Educational Barriers
As with language, some (n=5) counselors expressed that they had not encountered any educational barriers while delivering Options, asserting that their participants had a baseline education level that was sufficient for comprehending the intervention.
“Because our participants -- I can’t say that their level of education is low. Here in South Africa, we have metric or center 10. From center 10, then you go to TESSA [Teacher Education in Sub-Saharan Africa]. We had a large number of participants that had metric, so they’ve gone through high school or what you call, I think college or something. But at least they had some idea of education.” – Counselor #1102
“When it comes to education level, these are young women. And most of them, they’ve got at least metric when it comes to education level. So, they do understand what we are telling them. Even the options that we are presenting to them for prevention.” – Counselor #1401
However, some (n=8) counselors identified a minor educational barrier: participants with lower education levels had difficulty understanding the research-related language included in the intervention. According to the counselors, the barrier was not the translation of the intervention materials, but rather the participants’ ability to comprehend the messaging. A few (n=3) counselors further noted that this barrier arose specifically when they were describing the technical aspects of the participant’s residual dapivirine drug levels, such as how they were measured and calculated.
“I think it’s the same -- some of those, like, really rare Zulu words that are used in higher grades or in university, or a person that has completed a degree. So that is why I think they had those challenges. Because some of our participants are not matriculated. So, it wasn’t really major things, but you need at some points to make it clearer and look at a word in a different language, then you are able to explain it to them.” – Counselor #904
“The problem we had at first was when you have to explain about the ring residual drugs and how is it done. Sometimes, they would not understand all those things. How do you calculate how much is left on the ring and how much is in my body? How does it fit? How is it absorbed to my body? So, you have to find a way that the participant will understand and like explain it at the participant’s level.”- Counselor #503
Cultural Barriers
Counselors identified an array of cultural barriers that pertained to the intervention and counseling materials. A few (n=5) articulated that participants didn’t fully understand or believe that they could choose their HIV prevention methods; as such, counselors believed some participants selected the ring because they thought the counselors wanted them to, even if they were unlikely to use it consistently. Predominantly, counselors thought this stemmed from the fact that HOPE Study participants were recruited from the previous ASPIRE Study (MTN-020), in which they had been required to use the Dapivirine vaginal ring.
“I guess they were still quite confused about the difference between HOPE and ASPIRE. When you talk about Options, they didn’t understand that you have the right to choose the kind of HIV prevention that works for you. You don’t have to choose the ring. You can use any other HIV prevention. But I think that they didn’t quite believe us because most of them offered to take the ring in the beginning. And then when they got level zero, they explained that they encountered problems, their partner doesn’t want them to use the ring.” – Counselor #604
“I think for the first few participants they didn’t understand when you tell them that they can choose not to use the ring. And most of them will choose using the ring, but as you continue counseling them about their choice, and they started asking questions, they would choose not to continue using the ring. They would understand that they have a choice, and if they want they will continue, but they are not forced to continue using the ring.” – Counselor #503
Some (n=7) counselors also noted that participants struggled to comprehend specific Options Counseling tasks because they were uncertain of how to use the pictorial guides included in the tabletop flipchart; in particular, counselors noticed difficulty engaging with images of traffic lights and metric rulers. Counselors hypothesized that participants had trouble with these steps because they were not typically familiar with the function of traffic lights (locally referred to as ‘robots’). Similarly, they felt participants were not accustomed to using either traffic lights or rulers to assess abstract concepts, such as their feelings about their HIV prevention approach (i.e., with the traffic lights in Figures 1a and 1b), how important they viewed using their selected prevention methods (i.e., with the ruler in Figure 2a), or how confident they were in their ability to utilize their selected methods consistently (i.e., with the ruler in Figure 2b).
Figure 2.
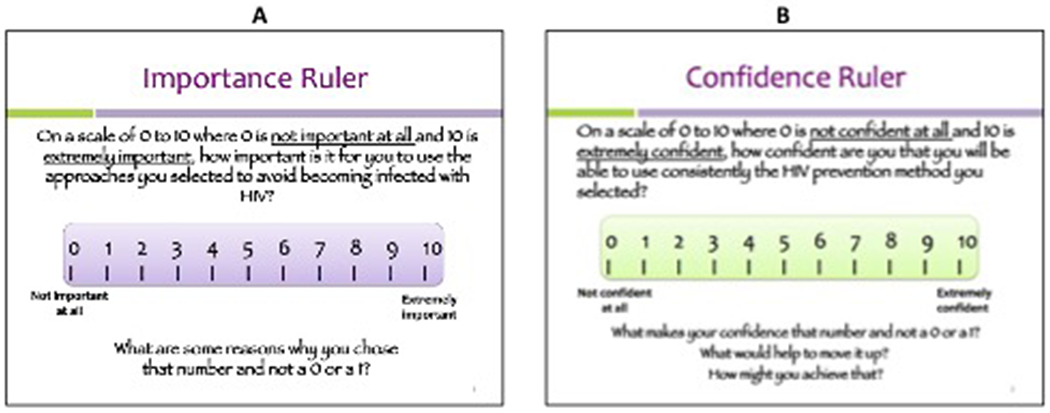
Tabletop flipchart tasks containing metric rulers
“Most participants were questioning us on the flipchart where we have the robot. Most had difficulties understanding what the robot meant, and for them to apply it to their ring use. Because most of our participants see the robot on the road and there are some participants who don’t know, they are not very much aware what they’re supposed to do when the red light is on and the yellow one is on and the green one is on.” – Counselor #804
“There was just a few that had difficulty. For example, if they are to evaluate themselves using the ruler on a scale of zero to ten where they think they are and how they’re using their prevention method. For some reason, you did have to just kind of use your own words to help them respond to the diagrams to help them evaluate themselves. The same with the robots to assess whether they are on the red, the green, or the amber.” – Counselor #701
To address difficulties in understanding the function of the pictorial guides, a few (n=5) counselors incorporated more culturally appropriate analogies into their sessions. This seemed to bolster participant comprehension, particularly of the importance and confidence rulers (Figures 2a and 2b, respectively).
“Let me make an example with a scenario of the ruler, you see. I know that all of them, they went to school. They know if you wrote a test, you have to get the marks in terms of maybe out of 10. You may be required to get a zero to 10. I used that scenario to elaborate the ruler. For an example, in the ruler I used to say -- this is a test of 10 points. So, zero points means that you got nothing. And then when it goes up, it means that you get something more. And up to 10, you get a total of each. So, I used to make that scenario, and it helped me a lot to make the same scenario simpler than it was before.” – Counselor #305
“The confidence ruler, I was using the numbers on the confidence ruler. Although their levels of comprehension would be low, they can count money, they know their numbers, so I would give them examples. Like if you could -- out of 10 cents, we go to fractions, it’s half of 10. So, from 5 to 10, we are looking at something, which is going up high. But from four to zero, we are looking at something decreasing. So according to them, the use of ring or their protections levels… how do you rate yourself from that?” – Counselor #804
Additionally, counselors reported two external cultural barriers that hindered participants’ efforts to engage with Options Counseling and adhere to their self-selected HIV prevention plan outside of the study clinic. First, half (n=11) of the counselors noted that participants struggled to disclose and navigate use of their HIV prevention plan with primary partners who opposed them. Second, a few (n=4) counselors expressed that some women felt they could not always implement their desired HIV prevention plan at home because it did not align with certain religious practices.
“Culturally, the men really have a lot of control over the women. You’d find, in terms of condoms -- I say condoms because I realize that if the partner says ‘I don’t want to use a condom’, that was it. Even though you teach them on using the female condom. They want to please their partner, so some of the decisions -- like male circumcision, they’ll say okay ‘I’m going to talk to my partner.’ Then you ask them, ‘so you chose this, this, and that. What happened?’ And you find, in terms of circumcision they didn’t even talk about it, or they’ll say ‘I didn’t talk about it because I thought I would get in trouble.’”- Counselor #103
“There were a few times that participants said that they had to do a prayer. So, understanding that they couldn’t use the ring or had to take the ring out because of a prayer at home, and they were fasting. So those were some of the things that they said made them take the ring out. Some of them didn’t want something that was not part of the body to be inside them, a foreign object in their body when they were fasting or doing a prayer.” – Counselor #202
In accommodating these external cultural barriers in their counseling, a few (n=3) counselors reported that the element of choice embedded in Options helped them navigate challenges to adherence and ensure the participant retained her agency in making decisions about her own HIV prevention plan.
“And very important as well, the counseling is all about choice -- what they choose to use, whatever they want to use in preventing HIV. It’s very important that they understand that the session that we are having, it’s all about HIV prevention, so if they don’t want to be part of the HIV prevention, then it’s okay for them to say that, you know, ‘We are not using condoms. We are not using this because my partner doesn’t want it’ or ‘my husband doesn’t want it.’ We also try for them to not feel that stigma that, whilst other women are doing this and protecting themselves, she is not and yet she is in the study.” – Counselor #606
“Options really helped with that, you were able to find out how she feels about her cultural system. One participant would say, ‘I’ve had to lie to my partner that I’m no longer using the ring. I still want to use the ring, but he’s the one who’s uncomfortable.’ So, you would respect her, and say, ‘I hear what you’re saying. Let’s say he does find out; how would you deal with that?’ but still respecting her. So, it was good that there was that element of choice; it really came out well, and this element of choice, as I said wasn’t only necessarily about the ring, but even with what she would want and decides to do on her own.” – Counselor #1302
Discussion
Overall, counselors reported that participant comprehension of and receptiveness to Options Counseling were high, suggesting that the study team’s abbreviated attempts to ensure the intervention was culturally relevant to this sample of sub-Saharan African women were successful. Beyond selecting an MI-based intervention and extensive translation efforts, it’s clear that an integral factor in helping participants overcome barriers was counselors’ flexibility to tailor their delivery of certain Options components.
The local translations of the study flipchart were largely successful. Few counselors reported encountering major participant barriers, although some reported that research-oriented or academic text did not translate well into participants’ local dialects. Most often, such language was too formal or relied upon terminology unfamiliar to less educated participants. Fortunately, due to their familiarity with the local languages and the flexibility embedded in Options, counselors were able to overcome these minor barriers by substituting confusing language with more colloquial phrasing. For future HIV prevention and adherence trials, involving laypeople from the target population during the initial translation and intervention development processes could help alleviate such vernacular discrepancies at the onset, ensuring that all intervention materials are tailored to the language and educational faculties of intended participants.
Counselors also shared that participants encountered a variety of cultural barriers, ranging from difficulty engaging with intervention content to challenges adhering to their HIV prevention plans at home due to external factors. In navigating these more sensitive barriers, counselors cited Option Counseling’s inherent flexibility as an asset. For participants who struggled with less culturally relevant pictorial guides, particularly traffic lights and metric rulers, counselors modified their approach and utilized more culturally familiar analogies, such as comparing the markers on the rulers to counting money. Similarly, some participants reported that they were unable to use their HIV prevention methods as anticipated because their partners were opposed or their methods weren’t congruent with religious practices. In these situations, the element of choice embedded in Options was very helpful, allowing counselors to support women in navigating their unique obstacles to avoid further difficulties.
While perfect cultural adaptations are likely impossible to achieve, our findings show that it’s important to consider the cultural landscape of a new target population while preparing all aspects of a given intervention, from the messaging utilized, to the images included on intervention materials, to how counselors are trained. For example, similar to the study counselors’ efforts to frame confusing flipchart images in familiar terms, existing research suggests that incorporating more culturally relevant images and content into adapted interventions can improve participant comprehension and engagement (Dickerson, Brown, Johnson, Schweigman, & D’Amico, 2016; Venner, Feldstein, & Tafoya, 2006). In their work delivering an adapted MI intervention to Native Americans, Venner et al. (2006) also utilized importance and confidence rulers. However, when depicting the rulers in their intervention manual, they included images relevant to the target population, such as different stages of planting and growing crops. In this vein, involving laypeople from the intended population in the development of intervention materials could help future trials to identify culturally incongruent content, as well as external factors (e.g., partner resistance) that may prevent individuals from adhering to interventions in real world settings.
Beyond technical preparations, these findings also highlight the importance of embedding flexibility into interventions intended to be delivered to new target populations. Options required minor tailoring after its initial implementation to be more culturally relevant to sub-Saharan African women. The intervention was flexible enough that, with training and ongoing coaching, counselors could troubleshoot the barriers they encountered on the ground and tailor Options to better meet the needs of their participants. One critical aspect was that Options enabled counselors to support women’s choices regarding HIV prevention method use and navigating partner resistance. At the very least, integrating this element of choice into future trials could help to ensure that women do not subject themselves to social or physical harm while trying to uphold study requirements, thereby increasing their likelihood of adhering to their chosen risk-reduction plans after they leave the clinic.
As with all cultural adaptation efforts, researchers who strive to embed flexibility into similar interventions must tread a fine line between encouraging counselors to tailor their delivery of the intervention to better suit participants’ needs and ensuring that any adaptations implemented on the ground do not compromise the intervention’s core components. To this end, it is critical that counselors grasp the theory underlying the intervention they are delivering so they better understand the goal of each of their interactions with a participant. Arming study counselors with this knowledge could help ensure that they internalize what the intervention, as well as each of its core components, is meant to achieve, thereby enabling them to brainstorm different ways of accomplishing those same goals even when they have to tailor specific questions or tasks to overcome participant language, educational, or cultural barriers.
Limitations
The main limitation of the present work is that all accounts of participant barriers were provided by the study counselors, as opposed to the HOPE Study participants themselves. Given the scope and timeline of the HOPE Study, it was not possible to survey participants about the counseling. Further, due to regulatory delays and to avoid biasing their decision to participate, counselors were not contacted about the present study until up to seven months after the HOPE Study had concluded; as such, their recollections of the counseling and prominent barriers may have diminished over time. Finally, eighteen of the HOPE Study counselors who were invited to participate in the present study either declined participation (n=6) or could not be reached (n=12). As such, it’s possible that those who encountered different or more severe barriers during HOPE were less willing to share their experiences and declined to follow-up with research staff.
Conclusions
This sample of HIV prevention and adherence counselors shared valuable insight on potential barriers that can impact participants’ comprehension of and engagement with adherence counseling interventions in large, biomedical HIV trials in sub-Saharan Africa. Future researchers should consider the language, educational, and cultural barriers presented here during their efforts to culturally tailor similar interventions across diverse populations. Expressly, translation efforts that include consultations with laypeople from the target population are warranted; similarly, it may prove valuable to involve laypeople in the development of intervention content, such as pictorial guides, to ensure relevance to the intended target population. Finally, those who design and/or adapt HIV prevention and adherence counseling interventions should be cognizant of specific external cultural barriers (e.g., partner influence, religious obligations) that may impact a participant’s ability to utilize HIV prevention method(s) at home. When possible, such researchers should integrate ongoing consultation with counselors and encourage sufficient flexibility in the delivery of the intervention so that counselors can support participants as they navigate sensitive obstacles, ensuring they do not feel pressured to adhere to study regimens in ways that might result in social or physical harm.
Acknowledgments
The HOPE study was designed and implemented by the Microbicide Trials Network (MTN), funded by the National Institute of Allergy and Infectious Diseases through individual grants (UM1AI068633, UM1AI068615 and UM1AI106707), with co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health, all components of the U.S. National Institutes of Health (NIH). The work presented here was funded by NIH grant UM1AI068633. The HIV Center for Clinical and Behavioral Studies was also supported through a center grant (P30-MH43520, Remien, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- Baeten JM, Palanee-Phillips T, Mgodi NM, Mayo A, Szydlo DW, Ramjee G, Gati Mirembe B, Mhlanga F, Hunidzarira P, Mansoor LE, Siva S, Govender V, Makanani B, Naidoo L, Singh N, Nair G, Chinula L, Parikh UM, Mellors JW, Balán IC, Ngure K, van der Straten A, Scheckter R, Garcia M, Peda M, Patterson K, Livant E, Bunge K, Singh D, Jacobson C, Hendrix CW, Chirenje ZM, Nakabiito C, Taha TE, Jones J, Torjesen K, Senn T, Chakhtoura N, Nel A, Rosenberg Z, Soto-Torres LE, Hillier S, & Brown ER, for the MTN-025/HOPE Study Team. (in press). Uptake and use of a vaginal ring containing dapivirine for HIV-1 prevention in African women: a multi-country, prospective, open-label cohort study. The Lancet HIV. [Google Scholar]
- Balán IC, Giguere R, Lentz C, Kutner B, Kajura-Manyindo C, Byogero R, Biira Asiimwe F, Makala Y, Jambaya J, Khanyile N, Chetty D, Soto-Torres L, Mayo A, Mgodi NM, Palanee-Phillips T, & Baeten JM (2020). Client-centered adherence counseling with adherence measurement feedback to support use of the dapivirine ring in MTN-025 (The HOPE Study). AIDS and Behavior. Advance online publication. 10.1007/s10461-020-03011-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrera M Jr, Castro FG, Strycker LA, & Toobert DJ (2013). Cultural adaptations of behavioral health interventions: a progress report. Journal of consulting and clinical psychology, 81(2), 196–205. 10.1037/a0027085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell SG, Newcomer SF, Bachrach C, Borawski E, Jemmott JB 3rd, Morrison D, Stanton B, Tortolero S, & Zimmerman R (2007). Challenges in replicating interventions. The Journal of adolescent health, 40(6), 514–520. 10.1016/j.jadohealth.2006.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card JJ, Solomon J, & Cunningham SD (2011). How to adapt effective programs for use in new contexts. Health promotion practice, 12(1), 25–35. 10.1177/1524839909348592 [DOI] [PubMed] [Google Scholar]
- Carlbring P, Jonsson J, Josephson H, & Forsberg L (2010). Motivational interviewing versus cognitive behavioral group therapy in the treatment of problem and pathological gambling: a randomized controlled trial. Cognitive behaviour therapy, 39(2), 92–103. 10.1080/16506070903190245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darbes L, Crepaz N, Lyles C, Kennedy G, & Rutherford G (2008). The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African Americans. AIDS (London, England), 22(10), 1177–1194. 10.1097/QAD.0b013e3282ff624e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dévieux JG, Malow RM, Rosenberg R, & Dyer JG (2004). Context and common ground: cultural adaptation of an intervention for minority HIV infected individuals. Journal of cultural diversity, 11(2), 49–57. [PubMed] [Google Scholar]
- Dickerson DL, Brown RA, Johnson CL, Schweigman K, & D'Amico EJ (2016). Integrating Motivational Interviewing and Traditional Practices to Address Alcohol and Drug Use Among Urban American Indian/Alaska Native Youth. Journal of substance abuse treatment, 65, 26–35. 10.1016/j.jsat.2015.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin SL, Pinto RM, Hunter J, Rapkin B, & Remien RH (2008). Keeping the spirit of community partnerships alive in the scale up of HIV/AIDS prevention: critical reflections on the roll out of DEBI (Diffusion of Effective Behavioral Interventions). American journal of community psychology, 42(1–2), 51–59. 10.1007/s10464-008-9183-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandelman A, & Rietmeijer CA (2004). Translation, adaptation, and synthesis of interventions for persons living with HIV: lessons from previous HIV prevention interventions. Journal of acquired immune deficiency syndromes, 37 Suppl 2, S126–S129. 10.1097/01.qai.0000140612.89757.8a [DOI] [PubMed] [Google Scholar]
- Gaydos CA, Hsieh YH, Galbraith JS, Barnes M, Waterfield G, & Stanton B (2008). Focus-on-Teens, sexual risk-reduction intervention for high-school adolescents: impact on knowledge, change of risk-behaviours, and prevalence of sexually transmitted diseases. International journal of STD & AIDS, 19(10), 704–710. 10.1258/ijsa.2008.007291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giguere R, Lentz C, Kajura-Manyindo C, Kutner BA, Dolezal C, Buthelezi M, Lukas I, Nampiira S, Rushwaya C, Sitima E, Katz A, van der Straten A, & Balán IC (in press). Counselors’ acceptability of adherence counseling session recording, fidelity monitoring, and feedback in a multi-site HIV prevention study in four African countries. AIDS Care. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gisore P, Kaseje D, Were F, & Ayuku D (2014). Motivational Interviewing intervention on health-seeking behaviors of pregnant women in Western Kenya. Journal of applied biobehavioral research, 19, 144–156. 10.1111/jabr.12020 [DOI] [Google Scholar]
- Gordon CM, Forsyth AD, Stall R, & Cheever LW (2005). Prevention interventions with persons living with HIV/AIDS: state of the science and future directions. AIDS education and prevention, 17(1 Suppl A), 6–20. 10.1521/aeap.17.2.6.58697 [DOI] [PubMed] [Google Scholar]
- Holstad MM, DiIorio C, Kelley ME, Resnicow K, & Sharma S (2011). Group motivational interviewing to promote adherence to antiretroviral medications and risk reduction behaviors in HIV infected women. AIDS and behavior, 15(5), 885–896. 10.1007/s10461-010-9865-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, Heckman TG, Stevenson LY, Williams PN, Ertl T, Hays RB, Leonard NR, O'Donnell L, Terry MA, Sogolow ED, & Neumann MS (2000). Transfer of research-based HIV prevention interventions to community service providers: fidelity and adaptation. AIDS education and prevention, 12(5 Suppl), 87–98. [PubMed] [Google Scholar]
- Kennedy MG, Mizuno Y, Hoffman R, Baume C, & Strand J (2000). The effect of tailoring a model HIV prevention program for local adolescent target audiences. AIDS education and prevention, 12(3), 225–238. [PubMed] [Google Scholar]
- Kirby D (2002). Effective approaches to reducing adolescent unprotected sex, pregnancy, and childbearing. Journal of sex research, 39(1), 51–57. 10.1080/00224490209552120 [DOI] [PubMed] [Google Scholar]
- Krummenacher I, Cavassini M, Bugnon O, & Schneider MP (2011). An interdisciplinary HIV-adherence program combining motivational interviewing and electronic antiretroviral drug monitoring. AIDS care, 23(5), 550–561. 10.1080/09540121.2010.525613 [DOI] [PubMed] [Google Scholar]
- Kutner BA, Giguere R, Lentz C, Kajura-Manyindo C, Dolezal C, Butheliezi S, Gwande M, Nampiira S, Ndlovu T, Mvinjelwa P, Mwenda W, & Balán IC, (2020). Sharing objective measures of adherence to a vaginal microbicide promotes candor about actual use and bolsters motivation to prevent HIV. AIDS and Behavior. Advance online publication 10.1007/s10461-020-03026-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightfoot MA, Kasirye R, Comulada WS, & Rotheram-Borus MJ (2007). Efficacy of a culturally adapted intervention for youth living with HIV in Uganda. Prevention science, 8(4), 271–273. 10.1007/s11121-007-0074-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbuagbaw L, Ye C, & Thabane L (2012). Motivational interviewing for improving outcomes in youth living with HIV. The Cochrane database of systematic reviews, (9), CD009748. 10.1002/14651858.CD009748.pub2 [DOI] [PubMed] [Google Scholar]
- McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, Gelaude D, Carey JW, & ADAPT Team (2006). Adapting evidence-based behavioral interventions for new settings and target populations. AIDS education and prevention, 18(4 Suppl A), 59–73. 10.1521/aeap.2006.18.supp.59 [DOI] [PubMed] [Google Scholar]
- Mensch BS, Richardson BA, Husnik M, Brown ER, Kiweewa FM, Mayo AJ, Baeten JM, Palanee-Phillips T, van der Straten A, & MTN-020/ASPIRE study team (2019). Vaginal Ring Use in a Phase 3 Microbicide Trial: A Comparison of Objective Measures and Self-reports of Non-adherence in ASPIRE. AIDS and behavior, 23(2), 504–512. 10.1007/s10461-018-2261-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2013). Motivational Interviewing: Helping people change (3rd ed.). The Guilford Press. [Google Scholar]
- Morrison DM, Hoppe MJ, Wells EA, Beadnell BA, Wilsdon A, Higa D, Gillmore MR, & Casey EA (2007). Replicating a teen HIV/STD preventive intervention in a multicultural city. AIDS education and prevention, 19(3), 258–273. 10.1521/aeap.2007.19.3.258 [DOI] [PubMed] [Google Scholar]
- Naar-King S, Parsons JT, & Johnson AM (2012). Motivational interviewing targeting risk reduction for people with HIV: a systematic review. Current HIV/AIDS reports, 9(4), 335–343. 10.1007/s11904-012-0132-x [DOI] [PubMed] [Google Scholar]
- Oh H, & Lee C (2016). Culture and motivational interviewing. Patient education and counseling, 99(11), 1914–1919. 10.1016/j.pec.2016.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliva G, Rienks J, Udoh I, & Smith CD (2005). A university and community-based organization collaboration to build capacity to develop, implement, and evaluate an innovative HIV prevention intervention for an urban African American population. AIDS education and prevention, 17(4), 300–316. 10.1521/aeap.2005.17.4.300 [DOI] [PubMed] [Google Scholar]
- Parsons JT, Rosof E, Punzalan JC, & Di Maria L (2005). Integration of motivational interviewing and cognitive behavioral therapy to improve HIV medication adherence and reduce substance use among HIV-positive men and women: results of a pilot project. AIDS patient care and STDs, 19(1), 31–39. 10.1089/apc.2005.19.31 [DOI] [PubMed] [Google Scholar]
- Patton MQ (1990). Qualitative evaluation and research methods (2nd ed.). Sage Publications, Inc. [Google Scholar]
- Pedlow CT, & Carey MP (2004). Developmentally appropriate sexual risk reduction interventions for adolescents: rationale, review of interventions, and recommendations for research and practice. Annals of behavioral medicine, 27(3), 172–184. 10.1207/s15324796abm2703_5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rongkavilit C, Wang B, Naar-King S, Bunupuradah T, Parsons JT, Panthong A, Koken JA, Saengcharnchai P, & Phanuphak P (2015). Motivational interviewing targeting risky sex in HIV-positive young Thai men who have sex with men. Archives of sexual behavior, 44(2), 329–340. 10.1007/s10508-014-0274-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott KD, Gilliam A, & Braxton K (2005). Culturally competent HIV prevention strategies for women of color in the United States. Health care for women international, 26(1), 17–45. 10.1080/07399330590885795 [DOI] [PubMed] [Google Scholar]
- Solomon J, Card JJ, & Malow RM (2006). Adapting efficacious interventions: advancing translational research in HIV prevention. Evaluation & the health professions, 29(2), 162–194. 10.1177/0163278706287344 [DOI] [PubMed] [Google Scholar]
- Stanton B, Harris C, Cottrell L, Li X, Gibson C, Guo J, Pack R, Galbraith J, Pendleton S, Wu Y, Burns J, Cole M, & Marshall S (2006). Trial of an urban adolescent sexual risk-reduction intervention for rural youth: a promising but imperfect fit. The Journal of adolescent health, 38(1), 55. 10.1016/j.jadohealth.2004.09.023 [DOI] [PubMed] [Google Scholar]
- Tortolero SR, Markham CM, Parcel GS, Peters RJ Jr, Escobar-Chaves SL, Basen-Engquist K, & Lewis HL (2005). Using intervention mapping to adapt an effective HIV, sexually transmitted disease, and pregnancy prevention program for high-risk minority youth. Health promotion practice, 6(3), 286–298. 10.1177/1524839904266472 [DOI] [PubMed] [Google Scholar]
- Venner KL, Feldstein SW, & Tafoya N (2006). Native American motivational interviewing: Weaving Native American and western practices: A manual for counselors in Native American communities. Centeron Alcoholish, Substance Abuse and Addictions. [Google Scholar]
- Vinh-Thomas P, Bunch MM, & Card JJ (2003). A research-based tool for identifying and strengthening culturally competent and evaluation-ready HIV/AIDS prevention programs. AIDS education and prevention : official publication of the International Society for AIDS Education, 15(6), 481–498. 10.1521/aeap.15.7.481.24050 [DOI] [PubMed] [Google Scholar]
- Wainberg ML, McKinnon K, Mattos PE, Pinto D, Mann CG, de Oliveira CS, de Oliveira SB, Remien RH, Elkington KS, Cournos F, & PRISSMA Project (2007). A model for adapting evidence-based behavioral interventions to a new culture: HIV prevention for psychiatric patients in Rio de Janeiro, Brazil. AIDS and behavior, 11(6), 872–883. 10.1007/s10461-006-9181-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson BD, & Miller RL (2003). Examining strategies for culturally grounded HIV prevention: a review. AIDS education and prevention : official publication of the International Society for AIDS Education, 15(2), 184–202. 10.1521/aeap.15.3.184.23838 [DOI] [PubMed] [Google Scholar]
- Wingood GM, & DiClemente RJ (2008). The ADAPT-ITT model: a novel method of adapting evidence-based HIV Interventions. Journal of acquired immune deficiency syndromes, 47 Suppl 1, S40–S46. 10.1097/QAI.0b013e3181605df1 [DOI] [PubMed] [Google Scholar]
- Zimmerman RS, Cupp PK, Donohew L, Sionéan CK, Feist-Price S, & Helme D (2008). Effects of a school-based, theory-driven HIV and pregnancy prevention curriculum. Perspectives on sexual and reproductive health, 40(1), 42–51. 10.1363/4004 [DOI] [PubMed] [Google Scholar]


