Abstract
Background:
Despite well-documented cardiovascular disparities between racial groups, within-race determinants of cardiovascular health among Black adults remain understudied. Factors promoting cardiovascular resilience among Black adults in particular, warrant further investigation. Our objective was to examine whether individual psychosocial resilience and neighborhood-level cardiovascular resilience were associated with better cardiovascular health (CVH) in Black adults, measured utilizing Life’s Simple 7 (LS7) scores.
Methods:
We assessed LS7 scores in 389 Black adults (age 53±10, 39% male) living in Atlanta, Georgia. A composite score of individual psychosocial resilience was created by assessing environmental mastery, purpose in life, optimism, resilient coping, and depressive symptoms. Neighborhood-level cardiovascular resilience was separately determined by the census tract-level rates of cardiovascular mortality/morbidity events. Generalized linear mixed regression models were used to examine the association between individual psychosocial resilience, neighborhood cardiovascular resilience, and LS7 scores.
Results:
Higher individual psychosocial resilience was significantly associated with higher LS7 (β=0.38 [0.16 – 0.59] per 1 standard deviation [SD]) after adjustment for sociodemographic factors. Similarly, higher neighborhood-level cardiovascular resilience was significantly associated with higher LS7 (β=0.23 [0.02 – 0.45] per 1 SD). When jointly examined, high individual psychosocial resilience (>median) was independently associated with higher LS7 (β=0.73 [0.31 – 1.17], while living in high-resilience neighborhoods (>median) was not. The largest difference in LS7 score was between those with high and low psychosocial resilience living in low-resilience neighborhoods (8.38 [7.90 – 8.86] vs 7.42 [7.04 – 7.79]).
Conclusions:
Individual psychosocial resilience in Black adults is associated with better cardiovascular health.
Cardiovascular disease (CVD) remains the leading cause of death in the United States (U.S.) and Black Americans suffer from greater burden of CVD than any other racial group.1, 2 Because most studies in the broader CVD literature have focused on comparisons to other racial groups, Black race, in itself, is often treated as a risk factor for CVD.2 Consequently, there have been few within-race studies that allow for an in-depth examination of factors that promote resilience, defined as the absence of adverse outcomes in the presence of exposure to risk,3 to poor CVD outcomes within Black adults. A better understanding of those factors that promote resilience among Black individuals may reveal novel insights into strategies to improve the cardiovascular health of this at-risk population.
Factors promoting cardiovascular resilience are likely multifactorial and multi-level, spanning both individual and environmental factors.4 At the individual level, aspects of positive psychosocial well-being, such as optimism,5 environmental mastery,6 and purpose in life,7 have been increasingly recognized as important determinants of cardiovascular health and disease. However, with few exceptions, the majority of these studies have not included large numbers of Black participants. Therefore, even though studies have consistently shown that Black individuals have higher levels of aspects of psychosocial well-being such as environmental mastery and purpose in life, as well as lower levels of depression compared to White individuals (a concept known as flourishing),8, 9,10 the manner in which individual psychosocial well-being, i.e. psychosocial resilience, contributes to cardiovascular health among Black adults remains relatively understudied.
Residential neighborhoods are increasingly recognized as important determinants of cardiovascular outcomes; thus, the environmental context of individuals should also be considered.11 Neighborhood socioeconomic disadvantage in particular has been consistently linked to CVD risk factors as well as incident CVD and CVD mortality-- driving a large degree of the association between residential environment and CVD outcomes.12, 13 Yet, emerging data suggest that certain residential contexts confer cardiovascular risk (or resilience) even beyond differences in neighborhood socioeconomic status (SES).14 Therefore, neighborhood-level cardiovascular resilience, i.e. areas with lower risk of cardiovascular disease than expected based on neighborhood-level SES, may also contribute to overall cardiovascular health (CVH) among Black adults.
Herein, we conducted a multi-level investigation of factors contributing to cardiovascular resilience among Black adults recruited from a Southern metropolitan city. We conceptualized individual psychosocial resilience as being high in psychosocial well-being and low on depression, consistent with emerging theories of overall resilience and flourishing in the broader public health literature.8, 9, 15, 16 We conceptualized neighborhood-level resilience as residence in communities with lower than expected rates of CVD based on neighborhood-level SES. We hypothesized that Black adults with higher levels of individual psychosocial and neighborhood resilience would have higher ideal CVH, defined by Life’s Simple 7 (LS7), a set of seven CVH metrics (four health behaviors – smoking, weight, physical activity, and diet; three health factors –blood pressure, total cholesterol, and glucose) that is associated with lower CVD and all-cause mortality. 17–19 We further hypothesized that when examined together, those with high levels of both individual psychosocial and neighborhood-level resilience would exhibit the highest ideal CVH, compared to those with low individual or neighborhood-level resilience.
METHODS
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Sample
The current investigation was conducted as part of the Morehouse-Emory Cardiovascular (MECA) Center for Health Equity study, a cross-sectional study designed to understand intra-racial heterogeneity in cardiovascular health among Black Americans, where sampling across census tracts was conducted and a novel measurement of neighborhood-level resilience was purposefully created (see below) to gain a diverse sample of Black Americans.14, 20 We recruited 389 adult volunteers living in the greater Atlanta region, aged 30 to 70, who self-identified as Black or African American using convenience sampling. Those with known history of CVD, such as myocardial infarction, congestive heart failure, cerebrovascular accidents, coronary artery disease, peripheral arterial disease, atrial fibrillation, and cardiomyopathies, were excluded. Other exclusion criteria included concomitant chronic diseases (e.g. human immunodeficiency virus, lupus, or cancer), substance abuse (alcohol or illicit drug), psychiatric illness, pregnant or lactating females, and self-reported inability to participate in increased physical activity. Enrolled participants visited either Morehouse School of Medicine or Emory University School of Medicine for a physical examination, blood draw, and questionnaires completed by trained research personnel. Study participants were compensated. The protocol was approved by the Institutional Review Boards of both institutions and all participants provided written informed consent. Further details on study design have been published elsewhere.20
Individual-level Psychosocial Resilience
Five domains of individual psychosocial well-being were measured via self-reported questionnaires. Four scales were administered to assess positive psychosocial well-being. Optimism was assessed with the Life Orientation Test-Revised.21, 22 Environmental mastery and Purpose in Life were assessed using two separate 14-item scales from Ryff’s Psychological Well-Being scales. 23, 24 Resilient coping was assessed using the 10-item Conner Davidson Resilience Scale.25 Additionally, consistent with prior research that defines psychological health (i.e. “resilience”) as the presence of positive psychological well-being in the absence of negative affect,26, 27 we also assessed depressive symptoms (Beck Depression Inventory II28). Scores on each of the 5 scales were averaged. We created a composite score of individual psychosocial resilience based on conceptual arguments in prior studies, in particular the work of Keyes and colleagues. 16, 29 Because each scale is varied in range and length (see supplemental Table S1), the composite score was calculated as the mean of the standardized scores across the 5 domains (with depressive symptoms reverse-coded). The composite score was further categorized using a median split into a binary low (≤median) or high (>median) variable. Further details can be found in the Supplement.
Neighborhood Cardiovascular Resilience
We determined neighborhood-level cardiovascular resilience by using census tract-level rates of adverse cardiovascular events for Black residents. The details of the census tract-level data used have been published elsewhere.14 Briefly, the census tract-level rates of cardiovascular mortality and morbidity (hospitalization and emergency department visits) for Black residents between 2010 and 2014 were obtained for the 36-county Atlanta-Athens-Clarke-Sandy Springs combined statistical area. As neighborhood SES is a known determinant of cardiovascular outcomes,11 defining cardiovascular risk and resilience of neighborhoods solely based on the distribution of mortality/morbidity rates is confounded by neighborhood SES. Therefore, we defined the cardiovascular resilience of neighborhood relative to neighborhood SES, using the residual percentile method as previously described in detail.14 Using these data, the residential census tracts of the enrolled participants were assigned neighborhood resilience scores, which were subsequently categorized into neighborhoods with low (≤median) or high (>median) cardiovascular resilience, representing neighborhoods that differed in their rates of cardiovascular mortality and morbidity events while having similar median household income of their Black residents (Supplemental Table S2). Further details can be found in the Supplement.
Study Covariates
Information on demographics, residential address, medical history, and socioeconomic status, including annual household income (<$25,000, $25,000 to $50,000, >$50,000, do not know), education (≤ high school graduate, some college or technical school, ≥ college graduate), marital status (married or not), and employment status (currently working for pay or not) were collected via self-report. Vital signs and anthropometric measures were recorded, and blood draws were performed after >6 hours of fasting to measure cholesterol and glucose levels. The presence of hypertension was verified by use of anti-hypertensive medications, systolic blood pressure ≥ 130 mmHg, or diastolic blood pressure ≥ 80 mmHg. The presence of diabetes mellitus was determined by either use of diabetes medications or fasting glucose ≥126 mg/dL. Finally, the presence of hyperlipidemia was defined by either use of lipid-lowering medications or fasting total cholesterol ≥240 mg/dL.
Life’s Simple 7 Scores
Life’s Simple 7 (LS7) score, developed by the American Heart Association, was calculated for the participants as their metric of cardiovascular health (Supplemental Table S3). Seven domains of cardiovascular health (exercise, diet, smoking history, blood pressure, glucose, cholesterol, and body mass index) were scored as 0 (poor), 1 (intermediate), or 2 (optimal), using the previously published scoring algorithm,30 and the summary score was computed by the summation of the 7 sub-scores with the range of 0 to 14. In the Framingham Offspring Study, 1 unit improvement in the LS7 was associated with 13% lower incidence of CVD, and thus, LS7 remains an important metric to target when improving CVH.31
Statistical Analysis
Demographic, socioeconomic, clinical, and psychosocial characteristics were presented by the categories of composite individual psychosocial resilience (low vs high) as well as by the neighborhood-level resilience (low vs. high) for descriptive purposes. Continuous variables were reported as means (± standard deviation [SD]) or as median (25th and 75th interquartile range) while categorical variables were reported as frequency counts and proportions (%), where appropriate. For continuous variables, t-tests were used for normally distributed variables while Mann-Whitney tests were used for non-normally distributed variables. Chi-square tests were used to compare proportions.
Generalized linear mixed regression models (with census tract-specific random intercepts to account for correlations among people living within the same neighborhood) were used to examine the difference in total LS7 score per 1 SD increment in the composite score of individual psychosocial resilience as well as each of the 5 psychosocial measures separately. Covariates were added in a stepwise fashion to examine the effect of additional covariate adjustment: Model 1: unadjusted; Model 2: adjusted for age and sex; Model 3: Model 2 + annual household income, education, marital status, and employment status. This sequence of models was repeated to examine associations between neighborhood-level resilience scores and LS7.
To examine the impact of individual psychosocial resilience on LS7 by neighborhood-level cardiovascular resilience (high vs. low), we ran fully-adjusted generalized mixed regression models as above stratified by neighborhood resilience status. This was followed by a formal test of the individual psychosocial resilience (composite or each of the 5 measures) x neighborhood-level cardiovascular resilience (low vs. high) interaction. We then built a regression model using the categorical individual psychosocial and neighborhood-level scores (high vs. low based on a median split) as predictors of LS7. All statistical analyses were performed using SPSS 25.0 (Armonk, NY) and SAS 9.1 (Cary, NC); P-value < 0.05 was considered statistically significant.
RESULTS
Participant Characteristics
Of the 389 participants enrolled, the mean age was 52.8 ± 10.3 years with 39% males and mean LS7 score was 8.0 ± 2.2. Educational levels ranged from high school or less (10%) to college or higher (30%). The number of census tracts represented in the cohort was 194, and the median number of participants per tract was 1 with the range from 1 to 10. Individual psychosocial resilience and neighborhood-level cardiovascular resilience were not significantly correlated (r= 0.011, P=0.83). Similarly, only modest correlations (ranging from 0.44 to 0.73) were noted among the five domains of individual psychosocial resilience. Table 1 displays the demographic, socioeconomic, and clinical characteristics of the participants stratified by the categories of composite individual psychosocial resilience (low vs high) and neighborhood-level cardiovascular resilience (low vs. high) levels. Those with high individual psychosocial resilience had higher household incomes, higher levels of education, and were more likely to be working than those with low individual resilience levels. There was no significant demographic or socioeconomic differences according to the categories of neighborhood-level resilience. The prevalence of traditional cardiovascular risk factors, such as hypertension, diabetes, hyperlipidemia, or current smokers were lower among those with high individual psychosocial resilience while only the prevalence of diabetes and current smoking differed by neighborhood-level resilience. Similarly, total LS7 scores were significantly higher among those with high composite individual psychosocial resilience than those with low resilience as well as among those living in high-resilience neighborhoods than those living in low-resilience neighborhoods (Table 1).
Table 1.
Demographic, socioeconomic, clinical, and psychosocial characteristics of the cohort stratified by the composite individual psychosocial resilience level (low vs high) as well as the neighborhood-level resilience (low vs high)*
| Individual psychosocial resilience | Neighborhood-level cardiovascular resilience | |||||
|---|---|---|---|---|---|---|
| Low (N=195) | High (N=194) | P-value | Low (N=198) | High (N=191) | P-value | |
| Demographic/socioeconomic variables | ||||||
| Age, years | 52.7 ± 9.8 | 53.0 ± 10.7 | 0.75 | 52.5 ± 10.4 | 53.1 ± 10.1 | 0.57 |
| Male | 85 (44) | 67 (35) | 0.067 | 78 (39) | 74 (39) | 0.90 |
| Annual household income | <0.001 | 0.63 | ||||
| < $10,000 | 61 (31) | 25 (13) | 45 (23) | 41 (22) | ||
| $10,000 to <$25,000 | 44 (23) | 54 (28) | 48 (24) | 50 (26) | ||
| $25,000 to <$50,000 | 51 (26) | 57 (30) | 57 (29) | 51 (27) | ||
| ≥ $50,000 | 29 (15) | 50 (26) | 36 (18) | 43 (23) | ||
| Do not know | 10 (5) | 7 (4) | 11 (6) | 6 (3) | ||
| Education history | 0.003 | 0.66 | ||||
| High school or less | 23 (12) | 9 (5) | 14 (7) | 18 (10) | ||
| Some college/tech school | 119 (61) | 106 (55) | 115 (58) | 110 (58) | ||
| College grad or higher | 53 (27) | 78 (40) | 69 (35) | 62 (33) | ||
| Currently married | 47 (24) | 59 (31) | 0.16 | 56 (28) | 50 (26) | 0.64 |
| Household size, person | 2.3 ± 1.7 | 2.6 ± 1.5 | 0.097 | 2.4 ± 1.6 | 2.4 ± 1.6 | 0.99 |
| Currently working | 85 (44) | 107 (55) | 0.020 | 100 (51) | 92 (48) | 0.68 |
| Objective/Clinical measures | ||||||
| Hypertension | 102 (52) | 77 (40) | 0.013 | 146 (74) | 128 (67) | 0.15 |
| Diabetes mellitus | 46 (24) | 31 (16) | 0.060 | 55 (28) | 28 (15) | 0.002 |
| Hyperlipidemia | 54 (28) | 32 (17) | 0.008 | 59 (30) | 58 (30) | 0.90 |
| Current smoker | 62 (32) | 32 (17) | <0.001 | 60 (30) | 34 (18) | 0.004 |
| BMI, kg/m2 | 32.9 ± 8.4 | 32.7 ± 8.1 | 0.79 | 32.7 ± 8.5 | 32.9 ± 8.0 | 0.75 |
| SBP, mmHg | 130 ± 19 | 131 ± 20 | 0.88 | 130 ± 19 | 131 ± 20 | 0.46 |
| DBP, mmHg | 81 ± 12 | 80 ± 12 | 0.29 | 80 ± 11 | 81 ± 12 | 0.39 |
| Glucose, mg/dL | 94 [87, 105] | 91 [85, 100] | 0.013 | 92 [86, 104] | 91[85, 101] | 0.23 |
| Cholesterol, mg/dL | 190 ± 40 | 194 ± 39 | 0.30 | 189 ± 38 | 196 ± 41 | 0.093 |
| HDL, mg/dL | 56 ± 18 | 58 ± 17 | 0.24 | 57 ± 16 | 58 ± 18 | 0.90 |
| LDL. mg/dL | 113 ± 35 | 116 ± 36 | 0.41 | 111 ± 33 | 117 ± 37 | 0.090 |
| Triglycerides, mg/dL | 89 [66,128] | 90 [62, 126] | 0.69 | 86 [61,126] | 91 [66,131] | 0.20 |
| LS7 scores | ||||||
| Total LS7, score | 7.57 ± 2.14 | 8.39 ± 2.16 | <0.001 | 7.75 ± 2.29 | 8.22 ± 2.04 | 0.035 |
| Exercise, score | 1.43 ± 0.69 | 1.57 ± 0.59 | 0.025 | 1.46 ± 0.64 | 1.53 ± 0.65 | 0.29 |
| Diet, score | 0.78 ± 0.51 | 0.81 ± 0.55 | 0.58 | 0.81 ± 0.55 | 0.80 ± 0.51 | 0.61 |
| Smoking, score | 1.32 ± 0.93 | 1.62 ± 0.75 | 0.001 | 1.35 ± 0.92 | 1.60 ± 0.77 | 0.005 |
| Blood pressure, score | 0.70 ± 0.74 | 0.82 ± 0.85 | 0.13 | 0.71 ± 0.79 | 0.82 ± 0.81 | 0.20 |
| Glucose, score | 1.41 ± 0.80 | 1.56 ± 0.73 | 0.052 | 1.39 ± 0.83 | 1.58 ± 0.68 | 0.016 |
| Cholesterol, score | 1.31 ± 0.68 | 1.40 ± 0.68 | 0.20 | 1.38 ± 0.65 | 1.34 ± 0.71 | 0.53 |
| BMI, score | 0.61 ± 0.78 | 0.56 ± 0.74 | 0.53 | 0.63 ± 0.79 | 0.54 ± 0.73 | 0.29 |
| Psychosocial measures | ||||||
| Environmental mastery, score† | 4.06 ± 0.67 | 5.29 ± 0.50 | <0.001 | 4.69 ± 0.88 | 4.66 ± 0.83 | 0.68 |
| Purpose in life, score† | 4.35 ± 0.77 | 5.50 ± 0.38 | <0.001 | 4.95 ± 0.85 | 4.90 ± 0.82 | 0.54 |
| Optimism, score‡ | 3.64 ± 0.75 | 4.52 ± 0.51 | <0.001 | 4.06 ± 0.79 | 4.10 ± 0.76 | 0.55 |
| Resilient coping, score {} | 2.77 ± 0.73 | 3.55 ± 0.40 | <0.001 | 3.17 ± 0.70 | 3.15 ± 0.71 | 0.78 |
| Depressive symptoms, score|| | 0.54 ± 0.41 | 0.14 ± 0.14 | <0.001 | 0.36 ± 0.40 | 0.33 ± 0.32 | 0.34 |
Values are mean ± standard deviation, median [25th and 75th interquartile range], or n (%).
Scaled 1 to 6, where 1 is the least and 6 is the most
Scaled 1 to 5, where 1 is the least and 5 is the most
Scaled 0 to 4, where 0 is the least and 4 is the most
Scaled 0 to 3, where 0 is the least and 3 is the most
Abbreviations: BMI = body mass index; SBP = systolic blood pressure; DBP = diastolic blood pressure; HDL = high-density lipoprotein; LDL = low-density lipoprotein; LS7 = Life’s Simple
Individual Psychosocial Resilience, Neighborhood-level Cardiovascular Resilience, and LS7
When composite individual psychosocial resilience score was treated as a continuous measure, LS7 was significantly higher by 0.42 points (95% confidence interval [0.21 – 0.64]; P<0.001) per 1 SD increment in composite individual psychosocial resilience score (Table 2). Adjustment for demographic and socioeconomic factors did not result in substantial changes in this relationship between individual composite resilience and LS7 (Table 2). When the 5 domains of psychosocial characteristics consisting of the composite score were examined individually, higher scores in environmental mastery, purpose in life, optimism, and resilient coping were significantly associated with higher LS7 scores in the fully adjusted models (Figure 1). Lower depressive symptoms were also significantly associated with higher LS7 scores.
Table 2.
Association between composite individual psychosocial resilience and Life’s Simple 7 (LS7) score*
| Model | Covariates | Beta | 95% C.I. | P-value |
|---|---|---|---|---|
| Model 1 | Unadjusted | 0.42 | 0.21 – 0.64 | <0.001 |
| Model 2 | Model 1+ age and sex | 0.45 | 0.24 – 0.65 | <0.001 |
| Model 3 | Model 2 + income†, education‡, marital status, and employment status | 0.38 | 0.16 – 0.59 | 0.001 |
Difference in LS7 score per 1 standard deviation increment of individual psychosocial resilience score is depicted.
Four categories of annual household income were included: <$25,000, $25,000 to <$50,000, ≥$50,000, and do not know.
Three categories of the highest education attainment level were included: ≤ high school graduate, some college or technical school, ≥ college graduate).
Abbreviations: C.I. = confidence interval; LS7 = Life’s Simple 7
Figure 1: Association between individual psychosocial resilience and LS7 scores.
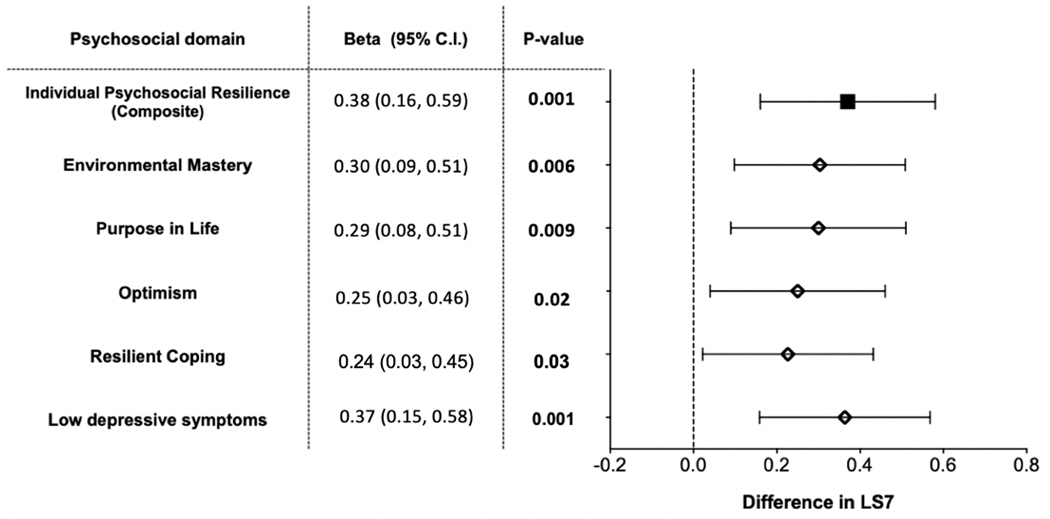
Differences in LS7 scores per 1 standard deviation increment in individual psychosocial resilience scales (the composite and its sub-components) are shown. Estimates were adjusted for age, sex, household income, education, marital status, and employment status. Abbreviations: LS7 = Life’s Simple 7; C.I.= confidence interval.
When the neighborhood resilience score was treated as a continuous variable, LS7 score was significantly higher by 0.27 [0.06 – 0.49] points (P=0.01) for 1 SD increment in neighborhood resilience score (Table 3). This relationship remained unchanged after stepwise adjustment for demographic and socioeconomic variables including age, sex, household income, education level, marital status, and employment status (Table 3).
Table 3.
Association between neighborhood cardiovascular resilience level and Life’s Simple 7 (LS7) score*
| Model | Covariates | Beta | 95% C.I. | P-value |
|---|---|---|---|---|
| Model 1 | Unadjusted | 0.27 | 0.06 – 0.49 | 0.01 |
| Model 2 | Model 1+ age and sex | 0.30 | 0.09 – 0.51 | 0.01 |
| Model 3 | Model 2 + income†, education‡, marital status, and employment status | 0.23 | 0.02 – 0.45 | 0.03 |
Difference in LS7 score per 1 standard deviation increment of neighborhood resilience score is depicted.
Four categories of annual household income were included: <$25,000, $25,000 to <$50,000, ≥$50,000, and do not know.
Three categories of the highest education attainment level were included: ≤ high school graduate, some college or technical school, ≥ college graduate).
Abbreviations: C.I. = confidence interval; LS7 = Life’s Simple
Joint Effects of Individual Psychosocial Resilience and Neighborhood Cardiovascular Resilience on LS7
To examine the impact of individual psychosocial resilience on LS7 by neighborhood-level resilience (low vs. high), we ran stratified analyses within those living in neighborhoods with low and high resilience, along with a test of interaction terms. Overall, the difference in LS7 per 1 SD increment in the individual psychosocial resilience tended to be greater among those living in low-resilience neighborhoods for the composite, resilient coping and depressive symptom scores. While the difference in LS7 per 1 SD increment increase in domains of environmental mastery, purpose in life, and optimism were higher for those in low resilience neighborhoods, there was no statistical difference (Supplemental Table S4). However, the interaction terms between individual psychosocial resilience and neighborhood resilience level (low vs high) were not statistically significant.
Subsequently, in a fully adjusted model including categorical (high vs. low) measures of both individual psychosocial and neighborhood resilience as predictors of LS7, having high individual resilience (vs. low individual resilience) was independently associated with higher LS7 by 0.73 [0.31 – 1.17]. However, high neighborhood-level resilience was not independently associated with higher LS7. The largest difference in adjusted LS7 score was seen between those with high individual psychosocial resilience living in low-resilience neighborhoods and those with low individual psychosocial resilience living in low-resilience neighborhoods (8.38 [7.90 – 8.86] vs 7.42 [7.04 – 7.79]), which corresponds to a 12.5% lower incidence of CVD (Figure 2).31
Figure 2: LS7 scores* according to individual composite psychosocial resilience (high vs low) and neighborhood resilience (high vs low).
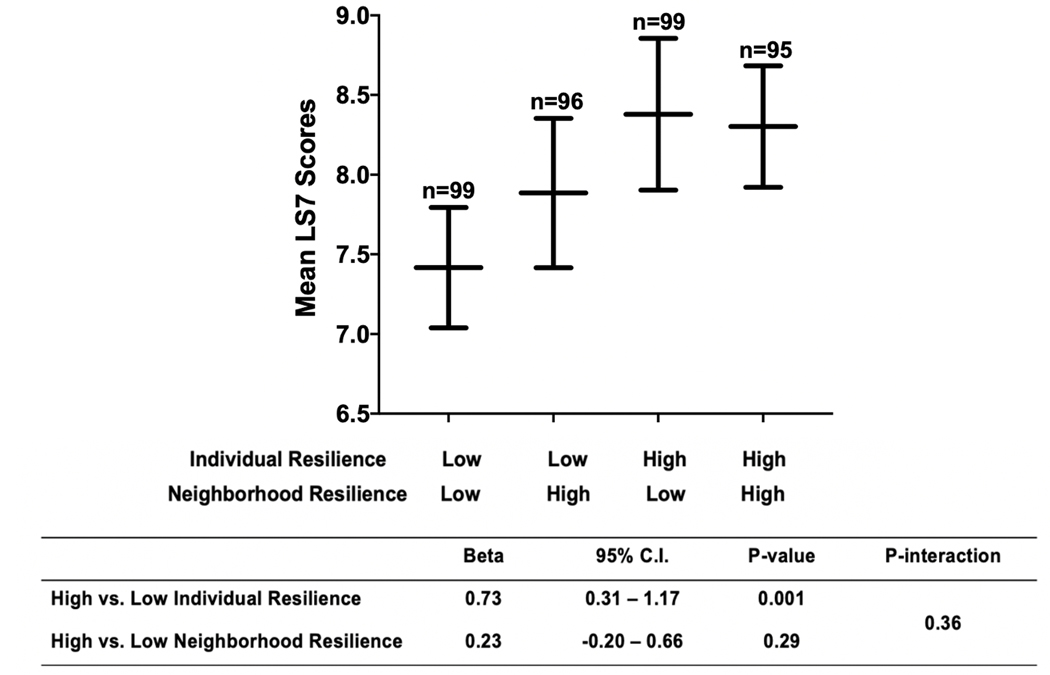
Having high vs. low individual psychosocial resilience was independently associated with higher LS7, while living in neighborhoods with high vs. low cardiovascular resilience was not. The largest difference in LS7 score was between those with high vs. low individual psychosocial resilience living in low-resilience neighborhoods (8.38 [7.90 – 8.86] vs 7.42 [7.04 – 7.79]).
*Adjusted for age, sex, household income, education, marital status, and employment status.
Abbreviations: LS7 = Life’s Simple 7; C.I. = confidence interval.
DISCUSSION
We undertook a novel, multi-level investigation of cardiovascular resilience in a cohort of Black adults recruited from a metropolitan city in the Southeastern U.S. Several key findings emerged. At the individual level, greater psychosocial resilience, assessed via several constructs of psychosocial well-being, such as environmental mastery, purpose in life, optimism, resilient coping, and low depressive symptoms, was associated with better cardiovascular health, measured as a higher LS7 score. Additionally, living in a resilient neighborhood, defined as low neighborhood-level rates of cardiovascular mortality/morbidity events independent of neighborhood SES, was also associated with a higher LS7 score. Observed associations were independent of a range of demographic risk factors, including age, household income, education, marital status, and employment status.
In models examining individual psychosocial and neighborhood-level resilience simultaneously, individual psychosocial resilience demonstrated more robust associations with cardiovascular health than neighborhood-level resilience, which was somewhat surprising, given the wealth of data on the importance of environmental factors for CVD health. However, because LS7 is partly comprised of behavioral components of CVH, it is possible that individual psychosocial states and characteristics have a greater impact on these particular risk factors than neighborhood-level factors would. Other outcomes, such as myocardial infarction, stroke, and heart failure might be more heavily influenced by structural or environmental factors. Future research examining how individual psychosocial and neighborhood-level resilience combine to impact a range of CVD-related outcomes is needed.
In addition to examining the independent associations of individual psychosocial and neighborhood-level resilience with CVH, we also examined the synergistic associations between the two. Because the interaction was not statistically significant, these associations should be viewed with some caution, however, in models stratified by neighborhood level resilience, we found that higher levels of individual psychosocial resilience were significantly associated with the CVH of Black adults living in low-resilience neighborhoods; while there were no significant associations between psychosocial resilience and CVH among Black adults living in high resilience neighborhoods. This was in the opposite direction that we would have expected, but is consistent with some broader conceptual literature which posits that individual psychosocial resilience (specifically purpose in life) matters more under conditions of adversity.32 However, again, because the interaction was not significant, these findings are only suggestive, and should be explored in future research. Nonetheless, our overall results highlight the importance of individual psychosocial resilience in particular, for the CVH of Black adults.
There are several broader public health implications of our study. Although policy level interventions and systemic change that guarantee equal rights and improved access to healthcare, education, and other opportunities for minorities is the ultimate goal, interventions that promote positive well-being and/or capitalize on psychosocial resilience at the individual level might prove beneficial for the CVH of Black Americans, particularly for those living in communities with poorer overall CV health. Prior studies have demonstrated that among Black adults, greater psychosocial well-being was associated with more favorable lifestyle factors linked to better CVH such as lower rates of smoking and improved glycemic control in diabetics.33, 34 Thus, improving psychosocial well-being could represent an entry point to improving CVH through targeting lifestyle factors but further research into implementation strategies is required.
Even given its importance as outlined above, there is a dearth of literature about intervention strategies to improve individual psychosocial well-being in the context of cardiovascular health. In a randomized controlled trial conducted in a predominantly white cohort, positive psychology based interventions were associated with improved health behaviors post acute coronary syndrome but to our knowledge, these types of interventions have not been conducted in Black populations.35 Psychological interventions such as counseling and therapies, psychosocial support groups such as activity groups (which can be implemented in the neighborhood context), and social interventions such as economic and material assistance have been shown to improve psychosocial well-being in vulnerable populations in the context of other diseases.36, 37 Along with positive psychology interventions, these strategies could be leveraged to improve CVH in Black communities. Goodkind et al. has conducted extensive community based participatory research to study the use of empowerment based programs to improve psychosocial well-being of Black girls,38 which represents yet another avenue to improve CVH among Black Americans through targeting psychosocial well-being.
Limitations
Our study recruited Black adults (>99% native born Americans) in a single city using convenience sampling, and therefore, there are limits to its generalizability and further research based in other geographic areas to validate and expand our current findings would be informative. Also, the cross-sectional design limits any inference of causality in observed associations and does not allow us to account determine the long-term effects of having resiliency. In addition, the cross-sectional assessment of resilience may impact results since resilience is a dynamic process3 which we were not able to take into account. Follow-up studies with a prospective design would be helpful to establish the causal relationship of our findings and assess the impact of the dynamic nature of resiliency on CVH.
Furthermore, we created a composite score encompassing mastery, purpose in life, optimism, coping and low depression. The decision to create a composite score to measure individual psychosocial resilience has its basis in prior work;16 however, the score may not have captured relevant domains pertinent for individual psychosocial resilience/well-being (e.g. anxiety). In addition, while the individual components of the score have been validated, the composite score itself is novel, and will require validation and testing for reliability in future studies.
Conclusions
We demonstrate for the first time that individual psychosocial resilience, comprised of constructs of psychosocial health, is associated with better cardiovascular health among Black adults living in a Southern metropolitan city, irrespective of neighborhood-level resilience and neighborhood and individual SES. Our findings highlight the importance of individual psychosocial factors that promote cardiovascular health among Black adults, traditionally considered to be a high-risk population. Further research into the mechanistic links underlying our observed associations is needed to derive more specific insights into developing novel and effective intervention strategies to improve cardiovascular health of Black adults and other vulnerable populations.
Supplementary Material
What is known:
Black Americans suffer from greater burden of cardiovascular disease (CVD) than any other racial group but there are few within race studies that allow for an in-depth examination of factors that promote resilience to CVD in this vulnerable group
Individual psychosocial and neighborhood-level factors can lead to improved cardiovascular health, but they have not been studied as factors contributing to resilience among Black adults
What the study adds:
Individual psychosocial resilience, comprised of constructs of psychosocial health, is associated with better cardiovascular health among Black adults living in a Southern metropolitan city, irrespective of neighborhood-level resilience and neighborhood and individual socioeconomic factors.
Our findings highlight the importance of individual psychosocial factors that promote cardiovascular health among Black adults, especially for those living in neighborhoods with low cardiovascular resilience
Acknowledgments
Funding Sources: The American Heart Association 0000031288, Abraham J. & Phyllis Katz Foundation, and the National Institutes of Health T32 HL130025 & T32 HL007745–26A1.
Abbreviations
- CI
Confidence interval
- CVD
Cardiovascular disease
- CVH
Cardiovascular Health
- SD
standard deviation
- SES
socioeconomic status
- LS7
Life’s Simple 7
Footnotes
Conflicts of Interest: None of the authors report conflict of interest relevant to this article.
REFERENCES
- 1.Van Dyke M, Greer S, Odom E, Schieb L, Vaughan A, Kramer M and Casper M. Heart Disease Death Rates Among Blacks and Whites Aged ≥35 Years - United States, 1968–2015. Morbidity and mortality weekly report Surveillance summaries (Washington, DC : 2002). 2018;67:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA, Willis M and Yancy CW. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. 2017;136:e393–e423. [DOI] [PubMed] [Google Scholar]
- 3.Johnston MC, Porteous T, Crilly MA, Burton CD, Elliott A, Iversen L, McArdle K, Murray A, Phillips LH and Black C. Physical Disease and Resilient Outcomes: A Systematic Review of Resilience Definitions and Study Methods. Psychosomatics. 2015;56:168–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zautra AJ, Hall JS, Murray KE and the Resilience Solutions G. Resilience: a new integrative approach to health and mental health research. Health Psychology Review. 2008;2:41–64. [Google Scholar]
- 5.Boehm JK, Chen Y, Koga H, Mathur MB, Vie LL and Kubzansky LD. Is Optimism Associated With Healthier Cardiovascular-Related Behavior? Circulation Research. 2018;122:1119–1134. [DOI] [PubMed] [Google Scholar]
- 6.Surtees PG, Wainwright NWJ, Luben R, Wareham NJ, Bingham SA and Khaw K-T. Mastery is associated with cardiovascular disease mortality in men and women at apparently low risk. Health Psychology. 2010;29:412–420. [DOI] [PubMed] [Google Scholar]
- 7.Cohen R, Bavishi C and Rozanski A. Purpose in Life and Its Relationship to All-Cause Mortality and Cardiovascular Events: A Meta-Analysis. Psychosom Med. 2016;78:122–33. [DOI] [PubMed] [Google Scholar]
- 8.Ryff CD, Keyes CL and Hughes DL. Status inequalities, perceived discrimination, and eudaimonic well-being: do the challenges of minority life hone purpose and growth? Journal of health and social behavior. 2003;44:275–91. [PubMed] [Google Scholar]
- 9.Keyes CL. The Black-White paradox in health: flourishing in the face of social inequality and discrimination. Journal of personality. 2009;77:1677–706. [DOI] [PubMed] [Google Scholar]
- 10.Kubzansky LD, Huffman JC, Boehm JK, Hernandez R, Kim ES, Koga HK, Feig EH, Lloyd-Jones DM, Seligman MEP and Labarthe DR. Positive Psychological Well-Being and Cardiovascular Disease: JACC Health Promotion Series. Journal of the American College of Cardiology. 2018;72:1382–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diez Roux AV, Mujahid MS, Hirsch JA, Moore K and Moore LV. The Impact of Neighborhoods on CV Risk. Global Heart. 2016;11:353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA and Watson RL. Neighborhood of Residence and Incidence of Coronary Heart Disease. New England Journal of Medicine. 2001;345:99–106. [DOI] [PubMed] [Google Scholar]
- 13.Borrell LN, Diez Roux AV, Rose K, Catellier D and Clark BL. Neighbourhood characteristics and mortality in the Atherosclerosis Risk in Communities Study. Int J Epidemiol. 2004;33:398–407. [DOI] [PubMed] [Google Scholar]
- 14.Kim JH, Lewis TT, Topel ML, Mubasher M, Li C, Vaccarino V, Mujahid MS, Sims M, Quyyumi AA, Taylor HA Jr., and Baltrus PT Identification of Resilient and At-Risk Neighborhoods for Cardiovascular Disease Among Black Residents: the Morehouse-Emory Cardiovascular (MECA) Center for Health Equity Study. Preventing Chronic Disease. 2019;16:E57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tindle HA, Chang YF, Kuller LH, Manson JE, Robinson JG, Rosal MC, Siegle GJ and Matthews KA. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative. Circulation. 2009;120:656–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corey LMK. The Mental Health Continuum: From Languishing to Flourishing in Life. Journal of Health and Social Behavior. 2002;43:207–222. [PubMed] [Google Scholar]
- 17.Effoe VS, Carnethon MR, Echouffo-Tcheugui JB, Chen H, Joseph JJ, Norwood AF and Bertoni AG. The American Heart Association Ideal Cardiovascular Health and Incident Type 2 Diabetes Mellitus Among Blacks: The Jackson Heart Study. Journal of the American Heart Association. 2017;6:e005008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Joseph JJ, Echouffo-Tcheugui JB, Carnethon MR, Bertoni AG, Shay CM, Ahmed HM, Blumenthal RS, Cushman M and Golden SH. The association of ideal cardiovascular health with incident type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis. Diabetologia. 2016;59:1893–1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fang N, Jiang M and Fan Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: A meta-analysis. International Journal of Cardiology. 2016;214:279–283. [DOI] [PubMed] [Google Scholar]
- 20.Islam S, Kim J, Topel M, Liu C, Ko Y, Mujahid M, Quyyumi A and Taylor H. Cardiovascular Risk and Resilience Among Blacks: Rationale and Design of the MECA Study. Journal of the American Heart Association. 2020;9:e015247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scheier MF and Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health psychology. 1985;4:219. [DOI] [PubMed] [Google Scholar]
- 22.Scheier MF, Carver CS and Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67:1063–1078. [DOI] [PubMed] [Google Scholar]
- 23.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology. 1989;57:1069–1081. [Google Scholar]
- 24.Ryff CD and Keyes CLM. The structure of psychological well-being revisited. Journal of Personality and Social Psychology. 1995;69:719–727. [DOI] [PubMed] [Google Scholar]
- 25.Campbell-Sills L and Stein MB. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress. 2007;20:1019–28. [DOI] [PubMed] [Google Scholar]
- 26.Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73:539–48. [DOI] [PubMed] [Google Scholar]
- 27.Keyes CLM. Mental Health as a Complete State: How the Salutogenic Perspective Completes the Picture Bridging Occupational, Organizational and Public Health: A Transdisciplinary Approach Dordrecht: Springer Netherlands; 2014: 179–192. [Google Scholar]
- 28.Beck AT, Ward CH, Mendelson M, Mock J and Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. [DOI] [PubMed] [Google Scholar]
- 29.Westerhof GJ and Keyes CLM. Mental Illness and Mental Health: The Two Continua Model Across the Lifespan. Journal of adult development. 2010;17:110–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW and Rosamond WD. Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction - The American Heart Association’s Strategic Impact Goal Through 2020 and Beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 31.Xanthakis V, Enserro Danielle M, Murabito Joanne M, Polak Joseph F, Wollert Kai C, Januzzi James L, Wang Thomas J, Tofler G and Vasan Ramachandran S. Ideal Cardiovascular Health. Circulation. 2014;130:1676–1683. [DOI] [PubMed] [Google Scholar]
- 32.Schaefer SM, Morozink Boylan J, van Reekum CM, Lapate RC, Norris CJ, Ryff CD and Davidson RJ. Purpose in life predicts better emotional recovery from negative stimuli. PloS one. 2013;8:e80329-e80329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berg CJ, Haardörfer R, McBride CM, Kilaru V, Ressler KJ, Wingo AP, Saba NF, Payne JB and Smith A. Resilience and biomarkers of health risk in Black smokers and nonsmokers. Health Psychology. 2017;36:1047–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeNisco S. Exploring the relationship between resilience and diabetes outcomes in African Americans. Journal of the American Academy of Nurse Practitioners. 2011;23:602–610. [DOI] [PubMed] [Google Scholar]
- 35.Celano CM, Albanese AM, Millstein RA, Mastromauro CA, Chung W-J, Campbell KA, Legler SR, Park ER, Healy BC, Collins LM, Januzzi JL and Huffman JC. Optimizing a Positive Psychology Intervention to Promote Health Behaviors After an Acute Coronary Syndrome: The Positive Emotions After Acute Coronary Events III (PEACE-III) Randomized Factorial Trial. Psychosomatic Medicine. 2018;80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Skeen SA, Sherr L, Croome N, Gandhi N, Roberts KJ, Macedo A and Tomlinson M. Interventions to improve psychosocial well-being for children affected by HIV and AIDS: a systematic review. Vulnerable Children and Youth Studies. 2017;12:91–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Auchincloss AH, Mujahid MS, Shen M, Michos ED, Whitt-Glover MC and Diez Roux AV. Neighborhood health-promoting resources and obesity risk (the multi-ethnic study of atherosclerosis). Obesity (Silver Spring, Md). 2013;21:621–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goodkind S. “You can be anything you want, but you have to believe it”: Commercialized Feminism in Gender‐Specific Programs for Girls. Signs: Journal of Women in Culture and Society. 2009;34:397–422. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


