A 31-year-old male with HIV infection visited our outpatient department because he had suffered from blurred vision in the left eye (LE) for 2 days. On examination, the best-corrected visual acuity (BCVA) was 6/6 in the right eye and no light perception (NLP) in the LE. The slit lamp showed no specific findings. Fundoscopic examination revealed papillitis and small multifocal grayish yellow lesions located mostly in the postequatorial fundus [Figure 1a]. After 2 days, these grayish yellow lesions became confluent, and a large grayish plaque-like chorioretinal lesion with typical placoid edges was observed at the posterior pole [Figure 1b]. Laboratory studies showed positive Treponema pallidum hemagglutination (TPHA; 1:1280). Under the impression of acute syphilitic posterior placoid chorioretinopathy (ASPPC) with papillitis, penicillin was administrated intravenously. Two weeks after treatment, the confluent grayish placoid lesion was resolved, and multiple yellowish subretinal lesions developed [Figure 1c]. Four weeks after treatment, these yellowish subretinal lesions diminished, and papillitis improved [Figure 1d]. However, the BCVA remained NLP in the LE.
Figure 1.
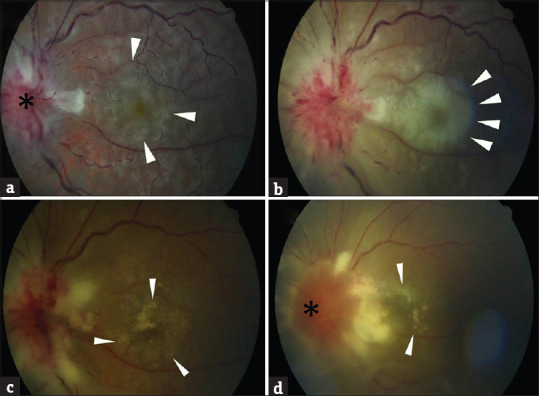
At the first visit, the fundus revealed significant papillitis (star) with small multifocal grayish yellow lesions (arrow) located mostly in the postequatorial fundus (a). After two days, these grayish lesions became confluent, and a large placoid lesion with typical edge (arrow) was observed mainly within the posterior pole (b). Two weeks after treatment, this confluent grayish placoid lesion was resolved, and multiple yellowish subretinal lesions developed (arrow; c). Four weeks after treatment, these yellowish subretinal lesions diminished (arrow), and papillitis (star) improved (d)
Ocular syphilis is uncommon and occurs in 1%–8% of Treponema pallidum infections. ASPPC is a rare but unique manifestation of ocular syphilis [1]. Only limited cases have been reported previously. The diagnosis for ASPPC is defined by the presence of one or more grayish yellow placoid outer retinal lesions, which typically occur in the macular region [1]. ASPPC may be accompanied by variable ocular lesions such as retinal hemorrhages, vasculitis, and papillitis. Huang et al. first reported a case of ASPPC mimicking central serous chorioretinopathy (CSCR) in Taiwan [2]. However, our patient did not show CSCR-like manifestations. Our patient revealed small multifocal grayish yellow lesions located mostly in the postequatorial fundus [Figure 1a] at the time of his first visit. Papillitis and vasculitis were also noted. After 2 days, these grayish lesions became confluent and a large placoid lesion with typical edges developed mainly within the posterior pole [Figure 1b]. Our case showed positive TPHA finding and revealed a large grayish yellow macular placoid chorioretinal lesion with typical placoid edges. These findings are compatible with a diagnosis of ASPPC.
The pathogenesis of ASPPC remains unknown. However, previous reports have suggested that placoid lesions result from inflammation at the level of the outer retina. Eandi et al. analyzed 44 cases and found significant thickening at the level of the retinal pigment epithelium (RPE)–choriocapillaris complex in the ASPPC area in most cases, but the presence of retinal fluid just around 12% cases [1]. Sekine et al. found hyperautofluorescent areas corresponding to the yellowish lesions, which were suggestive of lipofuscin accumulation in the outer retina [3]. Brito et al. observed loss of the external limiting membrane and loss of choroidal vascular detail in an eye with ASPPC [4]. The grayish yellow placoid lesions of ASPPC are, therefore, postulated to be the result of an active inflammatory reaction at the level of the choriocapillaris–RPE–photoreceptor complex.
There are some placoid lesions in the posterior segment that need to be differentiated from ASPPC, such as acute posterior multifocal placoid pigment epitheliopathy and relentless placoid chorioretinitis. Therefore, a syphilis serology test should be done for this group of diseases. Compared to ASPPC, the lesions in acute posterior multifocal placoid pigment epitheliopathy are smaller, and the course is usually self-limited. The lesions in relentless placoid chorioretinitis are also smaller but require immunosuppressors to achieve disease remission.
Visual prognosis is usually good for patients with ASPPC who receive prompt therapy. However, the BCVA of our case revealed NLP before and after treatment. Loss of function of the optic nerve due to the significant papillitis in LE at the first visit may account for this visual impairment even though the patient underwent treatment.
The global incidence of syphilis has markedly increased [1,5]. The presence of posterior placoid chorioretinopathy is highly suggestive of ocular syphilis. Careful retinal examination is important in the early diagnosis and treatment of syphilis.
Declaration of patient consent
The authors certify that the patient have obtained appropriate patient consent form. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Eandi CM, Neri P, Adelman RA, Yannuzzi LA, Cunningham ET, Jr International Syphilis Study Group. Acute syphilitic posterior placoid chorioretinitis: report of a case series and comprehensive review of the literature. Retina. 2012;32:1915–41. doi: 10.1097/IAE.0b013e31825f3851. [DOI] [PubMed] [Google Scholar]
- 2.Huang CY, Kang EY, Chen KJ, Wang NK. Acute syphilitic posterior placoid chorioretinopathy mimicking central serous chorioretinopathy: A case report. Taiwan J Ophthalmol. 2018;8:176–8. doi: 10.4103/tjo.tjo_18_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sekine Y, Yashiro S, O'hira A, Yoshida N, Morinaga M, Nagashima N, et al. Multimodal imaging of a case of acute syphilitic posterior placoid chorioretinitis. Nippon Ganka Gakkai Zasshi. 2015;119:266–72. [PubMed] [Google Scholar]
- 4.Brito P, Penas S, Carneiro A, Palmares J, Reis FF. Spectral-domain optical coherence tomography features of acute syphilitic posterior placoid chorioretinitis: The role of autoimmune response in pathogenesis. Case Rep Ophthalmol. 2011;2:39–44. doi: 10.1159/000324086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horng CT, Tsai PF, Tsai ML. Multiple preretinal yellowish dots in a patient with syphilis. Ci Ji Yi Xue Za Zhi. 2018;30:255–6. doi: 10.4103/tcmj.tcmj_79_18. [DOI] [PMC free article] [PubMed] [Google Scholar]


