Abstract
Background
Malaria is one of the most public health important and life-threatening parasitic infections caused by the protozoan parasite. Since children are immunologically naive to the malaria parasite, they are the main vulnerable groups. During malaria infection, they might have a complication of anemia, cerebral malaria, coma, respiratory distress, and a decrease in cognitive and behavioral improvement. Therefore, this review was aimed at determining the pooled prevalence of malaria among children in Ethiopia.
Methods
The current systematic review and meta-analysis were conducted based on the guideline of Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement guideline. Electronic bibliographic databases such as Google Scholar, PubMed, and Science Direct were used for searching relevant literature. Besides, the Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) was used for critical appraisal of studies. Using the STATA 14 software, the pooled Meta logistic regression was computed to present the pooled prevalence with a 95% confidence interval (CI).
Result
The overall estimated pooled prevalence of malaria among children in Ethiopia was 9.07 (95% CI: 6.32, 11.82). Subgroup analysis based on malaria signs and symptoms showed that the pooled prevalence of malaria among asymptomatic and symptomatic children was 6.67% (95% CI: 0.36, 12.98) and 27.17% (95% CI: 18.59, 35.76), respectively.
Conclusion
The findings revealed a high prevalence of malaria among children in Ethiopia. As a result, still there is a need of improving and rechecking the existing malaria prevention and control measures of the country.
1. Background
Malaria is one of the most important public health and life-threatening parasitic infections caused by the protozoan parasite. It is still a major concern in tropical and subtropical parts of the world. Plasmodium falciparum, P. vivax, P. ovale, P. knowlesi, and P. malariae are the five Plasmodium species that cause malaria in humans [1]. In 2018, the World Health Organization (WHO) report indicates that globally an estimated 228 million new cases of malaria were documented. The WHO African region accounted for 93% of all cases followed by the Southeast Asia region (3.4%) and Eastern Mediterranean region (2%). Likewise, there were an estimated 405000 deaths due to malaria in the globe. Children under the age of five-year were accounted for two-thirds (67%) of the world's malaria deaths in 2018 [2].
Around 75% of the landmass in Ethiopia is estimated to be malarious, and 68% of the total population in the area are at risk of malaria. According to the Ethiopian Federal Minister of Health (EFMH) report, malaria is on the list of the top ten leading causes of morbidity. Plasmodium falciparum accounts for 60%-70% of malaria cases, with the rest caused by P. vivax. The primary vector that plays an important role in malaria transmission is Anopheles arabiensis; moreover, An. pharoensis, An. funestus, and An. nili are less important vectors [3].
The EFMH indicates that around five up to six million malaria cases and tens of thousands of deaths of malaria were estimated each year. Moreover, in Ethiopia, malaria has a seasonal transmission and predominantly unstable, with frequent and often large-scale epidemics [4]. At this time, the diagnosis of malaria is by using microscopy or rapid diagnostic tests (RDTs) and treatment with artemisinin-based combination therapies (ACTs), promotion of long-lasting insecticidal nets (LLINs) ownership and use by the community, and application of indoor residual spraying (IRS) with insecticides were scaled up to improve access and equity to prevent and control malaria [5].
Since children are immunologically naïve to malaria parasites, they are the main vulnerable groups. They encounter severe clinical manifestation during P. falciparum infection. It may cause as many as 10% of all deaths in children [6]. Children during malaria infection might have a complication of anemia, cerebral malaria, coma, and respiratory distress and a decrease in cognitive and behavioral improvement [7]. Furthermore, despite the rapid administration of the best available antimalarial drugs, in sub-Saharan Africa, a minimum of one in ten children was admitted to hospitals as a result of severe and complicated malaria. Around 1200 children die from malaria in this region every day, accounting for the majority of the 631,000 deaths annually on the continent [8].
Different studies were conducted to assess the prevalence rate of malaria among children in Ethiopia having a great difference and varying findings. Besides, there is no previous systematic review and meta-analysis that assessed the prevalence of malaria among children in Ethiopia. Consequently, it was designed to assess the prevalence of malaria among children in Ethiopia. Its finding will support the execution of the most significant malaria prevention and control measure.
2. Methods
2.1. Searching Strategy
The current systematic review and meta-analysis were conducted by following the guideline of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [9]. The following electronic bibliographic databases were used for searching relevant literature: Google Scholar, PubMed, and Science Direct, to identify studies conducted on the prevalence of malaria among children. Only articles published in the English language up to August 2019 were retrieved. We used the search terms in correspondence with the Medical Subject Heading (MeSH) using the arrangement of keywords. In addition, the search terms were used separately and in combination using Boolean operators like “OR” or “AND”. The search strategy applied to retrieve important articles was as follows: (Prevalence) OR Prevalence [MeSH Terms]) AND Malaria) OR Malaria [MeSH Terms]) AND children) OR children [MeSH Terms]) AND Ethiopia) OR Ethiopia [MeSH Terms]. We had excluded duplicate data for the selection of the final studies included in this systematic review and meta-analysis. For managing references and remove repeated literature, the EndNote version X7 software was used.
2.2. Inclusion and Exclusion Criteria
2.2.1. Inclusion Criteria
Primary research articles conducted to determine the prevalence of malaria among children in Ethiopia published in reputable peer review journal, studies used cross-sectional study design, and studies used malaria microscopy as a laboratory method were included. These studies could be conducted on symptomatic or asymptomatic children, studies either on health center and/or hospitals, or it could be studies on primary school or/and community-based studies.
2.2.2. Exclusion Criteria
Small communication reports, review, poster, and studies reported on malaria prevalence by using only clinical signs and symptoms and studies used RDT as a laboratory method were excluded.
2.3. Search Methods and Quality Assessment
After we had searched the published research papers, it was imported into the EndNote X7 version, and then, duplicates were removed. All the authors (YT, SA, AD, and AW) had separately screened literature by their title, abstract, and full text to identify potentially appropriate articles according to the preset inclusion criteria. Then, the quality of all the incorporated studies was appraised by using the Joanna Briggs Institute (JBI) quality assessment checklist tool [10]. By looking at abstracts and titles, five hundred sixty-seven research articles were checked for eligibility criteria. Ninety-seven of them were selected for full-text evaluation by all of the authors. The discrepancy in choosing research papers to be included in this systematic review and meta-analysis were resolved by decision; in fact, we did have a very limited discrepancy between the authors in the selection of literature.
2.4. Data Extraction
All the authors of this paper came together and established the data extraction form in Microsoft Excel Spreadsheet. This data extraction sheet included the name of the first author, year of publication, study population, study design, study period, sample size, sampling technique, diagnostic method, the overall prevalence of malaria, the prevalence of P. vivax, the prevalence of P. falciparum, and the prevalence of mixed infection. Finally, the extracted data files were scientifically checked for reliability, and the existence of any discrepancies between the extracted data was resolved by detailed discussion among authors.
2.5. Data Analysis
Once we had extracted the data by using Microsoft Excel, the Stata version 14 software was used for statistical analysis. We use random-effects models as there is high heterogeneity across the study. Otherwise, it produces study encumbrances that principally indicates between study variation [11]. Basically, the I2 statistics predicates the existence of the main difference between studies included in a systematic review and meta-analysis due to heterogeneity rather than by chance, and its value range from 0 to 100%. I2 values of 25%, 50%, and 75% denote low, medium, and high heterogeneity between studies, respectively [12]. The existence of heterogeneity was determined when a p value was less than 0.05. Furthermore, we had checked the presence of publication bias, conducted subgroup analysis and sensitivity analysis.
3. Result
3.1. Characteristics of the Included Studies
By considering all the inclusion and exclusion criteria, a total of seven published studies on the prevalence of malaria among children were included. Initially, 12,579 published articles were identified via a database search engine. After that, 12,012 duplicates were removed from the total 12,579 searched research papers. Then, five hundred sixty-seven studies were screened by their title and abstract. Finally, after we had evaluated the full text of ninety-seven studies, seven of them were found to be eligible for this systematic review and meta-analysis. Full steps of screening and eligibility and the number of research articles were selected at each step as described in the diagram below (Figure 1). With regard to the type of study design used in the included studies, all of them utilized cross-sectional study design. On the other hand, from all the included studies, a study conducted in the Benishangul Gumuz region, Ethiopia, had the least sample size with 263 study participants [13]. However, another study conducted in the Oromia region, Ethiopia, had the highest sample size of 20,899 [14]. Microscopic diagnosis of malaria was the type of laboratory method used by all of the included studies. Also, most of the studies were from the Oromia region [14, 15], followed by the South Nation Nationality and People of Ethiopia [16, 17], and a single study was obtained from each region of Amhara and Benishangul Gumuz [13, 18]. But no studies were reported from the rest regions of Ethiopia.
Figure 1.
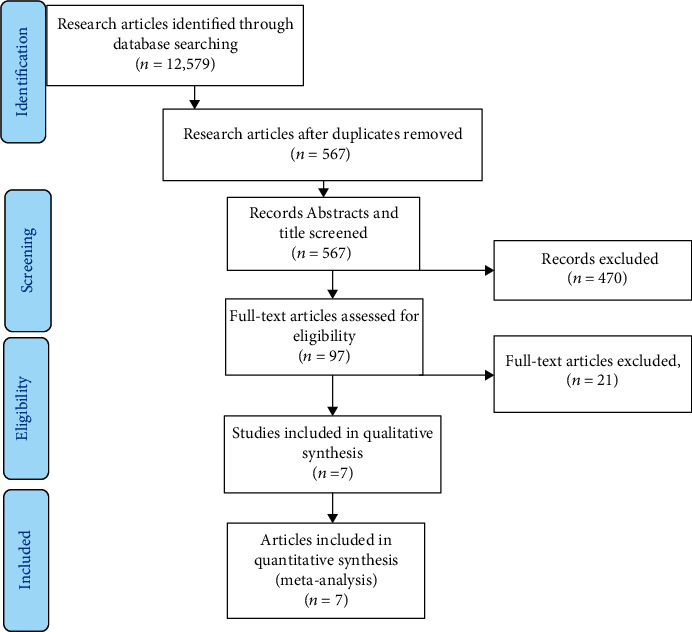
The flow diagram refers to the selection of studies included for a systematic review and meta-analysis of the prevalence of malaria among children.
In the current systematic review and meta-analysis, the total number of children included were 26,148. We had classified the included studies based on the type of cases so that most of the articles were conducted among children with asymptomatic malaria 4 (57%). Whereas 3 (43%) of the included studies were conducted among children with symptomatic malaria. In this systematic review and meta-analysis, most of the regions were included. The JBI quality assessment tool was used for assessing the quality of all the studies included in this systematic review; as a result, all of them have a good quality (Table 1).
Table 1.
The included studies general characteristics in the systematic review and meta-analysis of the prevalence of malaria among children in Ethiopia, 2020.
| Author/year | Region | Type of study design used | Type of cases | Type of laboratory method | Sample size | Prevalence of malaria (%) | Study quality |
|---|---|---|---|---|---|---|---|
| Ruth A et al., 2011 | Oromia | Cross-sectional | Asymptomatic | Microscopic | 20899 | 0.56 | Good |
| Ligabaw W et al., 2014 | Amhara | Cross-sectional | Asymptomatic | Microscopic | 385 | 6.75 | Good |
| Tsige K et al., 2013 | SNNP | Cross-sectional | Symptomatic | Microscopic | 1497 | 32.59 | Good |
| Yusuf H et al., 2012 | Oromia | Cross-sectional | Symptomatic | Microscopic | 830 | 20.48 | Good |
| Delenasaw Y et al., 2009 | Oromia | Cross-sectional | Asymptomatic | Microscopic | 1855 | 10.46 | Good |
| Getachew G et al., 2016 | Benishangul Gumuz | Cross-sectional | Symptomatic | Microscopic | 263 | 28.52 | Good |
| Aklilu R, 2017 | SNNP | Cross-sectional | Asymptomatic | Microscopic | 419 | 9.07 | Good |
3.2. The Prevalence of Malaria among Children
By including the seven published research articles, we had estimated the prevalence of malaria among children in Ethiopia. Accordingly, the overall estimated pooled prevalence of malaria among children was 9.07 (95% CI (6.32, 11.82)). The prevalence of malaria in each study as well as the pooled estimate was indicated by forest plot. According to the subgroup analysis, based on the existence of malaria symptoms, the prevalence of malaria among asymptomatic and symptomatic children was 6.67% (95% CI: 0.36, 12.98) and 27.17% (95% CI: 18.59, 35.76), respectively (Figure 2).
Figure 2.
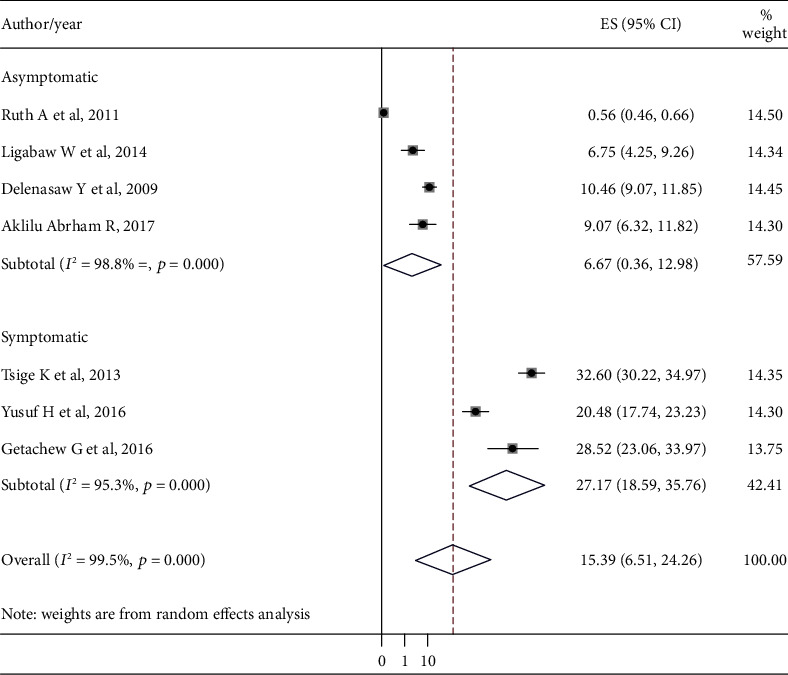
The pooled prevalence of malaria among children from random-effects model.
4. Discussion
Basic information is generated in this systematic review and meta-analysis about the estimated pooled prevalence of malaria among children in Ethiopia. In endemic areas, the risk of severe malaria is high among children. Despite symptoms of severe malaria such as severe anemia and respiratory distress occur at all ages, anemia and hypoglycemia are particularly common in young children [19]. Besides, in Africa, approximately 20 percent of all child deaths are caused by malaria. Certain children may have an acute attack of cerebral malaria that rapidly proceeds to coma and death [20].
The estimated combined pooled prevalence of malaria among children in Ethiopia in this systematic review and meta-analysis was 15.39 (95% CI: 6.51, 24.26). The result of this systematic review and meta-analysis was much higher than the recent national prevalence of malaria among the general population in Ethiopia. Parasite prevalence in Ethiopia was 0.5% by microscopy and 1.2% by RDTs for areas below 2,000 meters and less than 0.1% prevalence above 2,000 meters [21]. This might be due to the fact that children are a group of people with low immunity and immunity for them developed over years of exposure so that most malaria cases and deaths occurred among children [22].
Moreover, the result of this systematic review and meta-analysis was also higher when compared with meta-analysis done in sub-Saharan African countries 1.44% [23]. The high prevalence of malaria in Ethiopia as compared with countries in sub-Saharan Africa might be due to differences in the insecticide-treated bed nets, the type of test method used, the difference in the climatic conditions, and inadequate treatment of children with malaria cases. So that this systematic review and meta-analysis indicate for better decrement of malaria burden among children the world health organization malaria prevention and control strategies such as applying enhanced case management, and wide use of long-lasting insecticidal nets (LLINs) and indoor residual spraying (IRS) and early diagnosis and treatment and environmental managements should always be practiced in Ethiopia.
Surprisingly, a wide variation was observed in the prevalence of malaria among children in the current systematic review and meta-analysis compared with different national studies conducted in East Africa such as Uganda 19.7% [24], Rwanda 5.5% [25], and Kenya 16.27% [26]. The variation in the prevalence of malaria might be related to the difference in the type of laboratory method used, time of the study, and the difficulty of implementing the existing malaria prevention and control measures practice.
According to the subgroup analysis carried out in this systematic review and meta-analysis, the prevalence of malaria was found to be higher among children with malaria signs and symptoms 27.7% compared with asymptomatic children 6.67%. The high prevalence of malaria among symptomatic children might be related to the level of malaria parasitemia, and the chance of detecting malaria parasites is mostly higher whenever patients had signs and symptoms like fever.
The studies incorporated in this systematic review and meta-analysis showed a high heterogeneity. Despite all the authors involved in this review have tried to assess the possible sources of heterogeneity via subgroup analysis, the sources of inconsistency were not recognized. The possible source of heterogeneity might be related to the seasons in which each of the included studies was conducted because some of the studies were conducted during the high malaria transmission seasons, whereas the rest of included studies were done during the low malaria transmission seasons.
5. Conclusion
In conclusion, compared with the national prevalence of malaria among all the age groups, the estimated pooled prevalence of malaria among children was found to be higher. As a result, still, there is a need of improving and rechecking the existing malaria prevention and control measures of the country.
Acknowledgments
All the financial support was provided by Amhara regional state health bureau. But, the institution has no role in the design of the study, collection, analysis, and interpretation of the data and in writing the manuscript.
Abbreviations
- EFMH:
Ethiopian Federal Minister of Health
- IRS:
Indoor residual spraying
- JBI:
Joanna Briggs Institute
- LLINs:
Long-lasting insecticidal nets
- PRISMA:
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RDTs:
Rapid diagnostic tests
- WHO:
World Health Organization.
Data Availability
In this systematic review and meta-analysis, the main part of the data generated or analyzed during this study is included. Additional relevant data will be available from the corresponding author upon the need.
Consent
All participants provided written informed consent to publish this study.
Conflicts of Interest
All the authors announce that they have no any conflicts of interest.
Authors' Contributions
Yalewayker Tegegne conducted research protocol conceptualization, organizing the study design, literature review, data extraction, and statistical analysis. Sintayehu Ambachew and Yalewayker Tegegne participated in performing data analysis and interpretation and writing the draft drafting. Adane Derso and Abebaw Worede prepared data clarification and reviewed the final prepared manuscript. Data extraction and quality assessment were done by Yalewayker Tegegne, Abebaw Worede, and Sintayehu Ambachew.
References
- 1.White N. Plasmodium Knowlesi: The Fifth Human Malaria Parasite. The University of Chicago Press; 2008. [DOI] [PubMed] [Google Scholar]
- 2.WHO. World malaria report Brifing kit. WHO; 2019. [Google Scholar]
- 3.FMoH F. National malaria guidelines. Malaria Diagnosis and Treatment. third. Vol. 2012. Addis Ababa, Ethiopia: Federal Minstery of Health Ethiopia; 2012. [Google Scholar]
- 4.MoH F. D. E. National Malaria Guidelines. Third. Addis Ababa: Federal Minstery of Health Ethiopia; [Google Scholar]
- 5.Jakubowski A., Stearns S. C., Kruk M. E., Angeles G., Thirumurthy H. The US President’s Malaria Initiative and under-5 child mortality in sub-Saharan Africa: a difference-in-differences analysis. PLoS Medicine. 2017;14(6, article e1002319) doi: 10.1371/journal.pmed.1002319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perlman J. I., Khanna A. Nelson Textbook of Pediatrics. 17th 2004.
- 7.Holding P. A., Snow R. W. Impact of Plasmodium falciparum malaria on performance and learning: review of the evidence. The American Journal of Tropical Medicine and Hygiene. 2001;64(1_Supplement):68–75. doi: 10.4269/ajtmh.2001.64.68. [DOI] [PubMed] [Google Scholar]
- 8.Maitland K. Severe malaria in African children—the need for continuing investment. New England Journal of Medicine. 2016;375(25):2416–2417. doi: 10.1056/NEJMp1613528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.PRISMA-P Group, Moher D., Shamseer L., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4(1):p. 1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Munn Z., Moola S., Lisy K., Riitano D., Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. International Journal of Evidence-Based Healthcare. 2015;13(3):147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 11.Borenstein M., Hedges L. V., Higgins J. P., Rothstein H. R. Introduction to Meta-Analysis. John Wiley & Sons; 2011. [Google Scholar]
- 12.Ades A. E., Lu G., Higgins J. P. T. The interpretation of random-effects meta-analysis in decision models. Medical Decision Making. 2005;25(6):646–654. doi: 10.1177/0272989X05282643. [DOI] [PubMed] [Google Scholar]
- 13.Geleta G., Ketema T. Severe malaria associated with Plasmodium falciparum and P. vivax among children in Pawe Hospital, Northwest Ethiopia. Malaria Research and Treatment. 2016;2016:7. doi: 10.1155/2016/1240962.1240962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haji Y., Fogarty A. W., Deressa W. Prevalence and associated factors of malaria among febrile children in Ethiopia: a cross-sectional health facility-based study. Acta Tropica. 2016;155:63–70. doi: 10.1016/j.actatropica.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Yewhalaw D., Legesse W., van Bortel W., et al. Malaria and water resource development: the case of Gilgel-Gibe hydroelectric dam in Ethiopia. Malaria Journal. 2009;8(1):p. 21. doi: 10.1186/1475-2875-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ketema T., Bacha K. Plasmodium vivax associated severe malaria complications among children in some malaria endemic areas of Ethiopia. BMC Public Health. 2013;13(1):p. 637. doi: 10.1186/1471-2458-13-637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aklilu A. R. Preventing malaria among under five children in Damot Gale Woreda, Wolayta zone, Ethiopia: the role of parents knowledge and treatment seeking. Prim Health Care. 2017;7(4) doi: 10.4172/2167-1079.1000284. [DOI] [Google Scholar]
- 18.Worku L., Damtie D., Endris M., Getie S., Aemero M. Asymptomatic malaria and associated risk factors among school children in Sanja town, Northwest Ethiopia. International Scholarly Research Notices. 2014;2014:6. doi: 10.1155/2014/303269.303269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trampuz A., Jereb M., Muzlovic I., Prabhu R. M. Clinical review: severe malaria. Critical Care. 2003;7(4):315–323. doi: 10.1186/cc2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.UNICEF. Malaria: a major cause of child death and poverty in Africa. UNICEF; 2004. [Google Scholar]
- 21.Ethiopia U. President’s Malaria Initiative Ethiopia-Malaria Operational Plan FY 2017. Presedent Malaria Inisative Ethiopia; 2017. [Google Scholar]
- 22.Organization WH. World malaria report 2015. World Health Organization; 2016. [Google Scholar]
- 23.van Eijk A. M., Hill J., Noor A. M., Snow R. W., ter Kuile F. O. Prevalence of malaria infection in pregnant women compared with children for tracking malaria transmission in sub-Saharan Africa: a systematic review and meta-analysis. The Lancet Global Health. 2015;3(10):e617–e628. doi: 10.1016/S2214-109X(15)00049-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roberts D., Matthews G. Risk factors of malaria in children under the age of five years old in Uganda. Malaria Journal. 2016;15(1):p. 246. doi: 10.1186/s12936-016-1290-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gahutu J.-B., Steininger C., Shyirambere C., et al. Prevalence and risk factors of malaria among children in southern highland Rwanda. Malaria Journal. 2011;10(1):p. 134. doi: 10.1186/1475-2875-10-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sultana M., Sheikh N., Mahumud R. A., Jahir T., Islam Z., Sarker A. R. Prevalence and associated determinants of malaria parasites among Kenyan children. Tropical Medicine and Health. 2017;45(1):p. 25. doi: 10.1186/s41182-017-0066-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
In this systematic review and meta-analysis, the main part of the data generated or analyzed during this study is included. Additional relevant data will be available from the corresponding author upon the need.


