Abstract
Objective
This study captured the interrelationships among craving, negative affect, and positive and negative social exchanges in the daily lives of patients in residential treatment for opioid use disorders (OUD).
Method
Participants were 73 patients (77% male), age 19 to 61 (Mage = 30.10, SDage = 10.13) in residential treatment for opioid use disorder. Participants completed a smartphone-based survey 4 times per day for 12 consecutive days that measured positive and negative social exchanges (TENSE scale), negative affect (PA-NA scales), and craving (frequency and intensity). Within-person, day-level associations among daily positive and negative social exchanges, negative affect, and craving were examined using multilevel modeling.
Results
Daily negative social exchanges (M = 1.44, SD = 2.27) were much less frequent than positive social exchanges (M = 6.59, SD = 4.00) during residential treatment. Whereas negative social exchanges had a direct association with same-day craving (β= 0.08; 95% CI = 0.01, 0.16, ΔR2 = 0.01), positive social exchanges related to craving indirectly via moderation of the within-person negative affect-craving link (β= −0.01; 95% CI = −0.01, −0.001, ΔR2 = 0.002). Positive social exchanges decoupled the same-day linkage between negative affect and craving on days when individuals had at least four more positive social exchanges than usual.
Conclusions
These results indicate that both negative affect and negative social exchanges are uniquely related to craving on a daily basis, and that extra positive social interactions can reduce the intraindividual coupling of negative affect and craving during residential treatment for opioid use disorder.
Keywords: Opioids, Craving, Social Exchanges, Affect, Ecological Momentary Assessment
With a presumptive role in maintaining addiction (Tiffany & Conklin, 2000) and driving substance use, craving—most commonly defined as the subjective desire to use drugs—has been central to addiction theory and research for decades (Tiffany, 1990). Despite its presumptive role in addiction, inconsistent findings regarding associations between (typically) single-time self-reports of craving and substance use outcomes have led some researchers to challenge the construct’s utility, at least as conventionally measured (Pickens & Johanson, 1992; Tiffany, 1990; Rosenberg, 2009). These and other researchers have suggested that craving is complex and multifaceted, and that a lack of attention to this complexity may be contributing to the inconsistent findings in this area.
In this paper, we address one specific aspect contributing to the complexity of craving: its daily variability. Conventional single-timepoint assessments do not capture this variability, nor the variability in the factors that co-occur with it. For example, there are a number of both intrapersonal and interpersonal factors (e.g., Scott, Dennis, & Gustafson, 2017) that are related to the intensity and variability of craving, such as negative affect and interpersonal exchanges, respectively. These influences themselves vary over time, and static one-time assessments cannot capture craving’s reactivity to these internal and external stimuli. As others have noted (e.g., Preston et al., 2018b), examining the phenomenon of craving itself and its relationship to other daily life experiences is an important area for research. These examinations of craving should align theory with methods that capture the within-person variation in both craving and co-occurring risk and protective factors. Understanding craving in this fashion will facilitate better understanding of our patients, and the development of better ways to help them.
Theoretical Framework
Marlatt et al.’s dynamic Relapse Prevention (RP) model (Hendershot, Witkiewitz, George, & Marlatt, 2011; Marlatt & Gordon, 1985; Witkiewitz & Marlatt, 2004) argues that relapses are caused by high-risk situations, which are defined broadly as any context that confers vulnerability. These high-risk situations include contextual precursors, such as encounters with people or places that trigger memories of past drug use, as well as internal cues, such as cognitive or emotional states. The situations that confer risk vary across individuals, but they also vary within the same individuals over time (Hendershot et al., 2011). The RP model posits that recovery is a dynamic process that includes both between-person and within-person influences on substance use risk. Between-person influences include static or slow-changing processes, such as genetics and the influence of familial history of substance abuse. Within-person influences include more transient processes, such as craving and affective states. The interactions among these factors not only determines who is vulnerable to substance use, but also when and why use might occur.
In summary, a key component of the Relapse Prevention model is understanding the interactions among internal and external factors associated with substance use risk at the between- and within-person levels. Whereas external influences may confer risk, in the case of positive social exchanges, they may also confer protection. This view of context is consistent with two extensions of the RP model which expand on the role of social variables as modifiers of intraindividual processes (e.g., self-regulation) among individuals with SUDs (Hunter-Reel, Mccrady, & Hildebrandt, 2009; Roos & Witkiewitz, 2017). Further, the within- and between-person structure provides a simplified view of a more complicated process. In fact, many of the measures often considered “between-person”, such as person-level averages, are in fact measures of within-person processes that change sufficiently slowly that they are considered to be constant throughout the measurement period. Similarly, daily averages provide a simplification of faster-changing processes. The within-/between-framework gives us an easy way to conceptualize processes that play out across a range of different timescales (Oravecz & Brick, 2019).
Ecological Momentary Assessment
The ability to examine the dynamic within-person interactions between external and internal contexts proposed by the RP model to be associated with substance use risk are limited by most current approaches that consider differences in treatment experiences and outcomes between patients using single-timepoint assessments. A growing number of studies, however, have used experience sampling approaches, such as ecological momentary assessment (EMA), to assess within-person associations among individual and environmental factors associated with substance use risk. EMA uses technological tools to gather data multiple times per day as participants go about their daily lives, limiting retrospective recall bias and producing data that is more ecologically valid (Smyth, Juth, Ma, & Sliwinski, 2017), making it well-suited for studying the dynamic and complex processes of craving and co-occurring risk and protective factors (Zheng, Cleveland, Molenaar, & Harris, 2015).
EMA has been repeatedly demonstrated as a valid and feasible approach for studying addiction. For example, Preston and colleagues (Furnari et al., 2015; Preston, Kowalczyk, et al., 2018b; Preston et al., 2017) employed EMA to study affect, craving, substance use, and other daily experiences of individuals participating in outpatient opioid treatment. However, despite having a strong theoretical role, relatively few studies have examined the interplay between both interpersonal and intrapersonal phenomena in daily life, and no known EMA studies have been conducted with a sample of patients specifically in residential OUD treatment. Thus, the current study used EMA to evaluate craving in relation to negative affect and positive and negative social interactions among patients in residential treatment for opioid use disorder due to their inclusion in the RP model as inter- and intra-personal influences on relapse risk.
Craving
Craving is a complex construct that is an important component of the RP model. One important element of craving is an individual’s subjective experience of craving. Subjective craving is most commonly defined as the unwanted urge to use a drug (Serre, Fatseas, Swendsen, & Auriacombe, 2015). Research has shown that craving predicts use of all drugs of abuse, including tobacco (Catley, O’Connell, & Shiffman, 2000), alcohol (Litt, Cooney, & Morse, 2000), and opioids (Tsui, Anderson, Strong, & Stein, 2014). However, research has also demonstrated that it is very important how and when craving is measured relative to the time of use–the closer it is in time and place, the better predictor it is (e.g., Moore et al., 2014).
EMA studies across the last decade continue to support the link between craving and substance use across various substances and users at different stages of dependence and addiction (for a review, see Serre et al., 2015). For instance, craving strongly predicts substance use at the next assessment among patients currently in outpatient treatment (Fatseas, Serre, Swendsen, & Auriacombe, 2018) and individuals who have undergone treatment in the past year (Scott, Dennis, & Gustafson, 2018). One study among individuals entering intensive outpatient treatment assessed craving and use three times per day and found that those who reported an increase in craving at one assessment were 14 times more likely to use any substance at the next assessment compared to those who did not report increased craving (Moore et al., 2014). Research specific to certain substances of abuse has found that craving predicts subsequent use among alcohol, tobacco, and cannabis users (Serre, Fatseas, Denis, Swendsen, & Auriacombe, 2018). They did not find an effect for opiate users, but other studies have found evidence of increased craving before and after lapses to drug use among outpatients on opioid-agonist treatment (Preston, Kowalczyk, et al., 2018a). Taken together, the body of research suggests craving may be a critical influence on substance use, but the measurement of craving alone may not be sensitive or specific enough to adequately account for use. We suggest that to be an effective predictor, craving must be measured repeatedly and with respect to context.
Negative Affect
Negative affect (NA) has been defined as a negative and subjective evaluative feeling state in response to internal or external stimuli (Hussong et al., 2011). In contrast to stress, which refers specifically to a high-arousal, sometimes mixed valence state (see Folkman, 2008), NA is operationalized here to include both low-arousal states (e.g., sadness, loneliness) and high-arousal states (e.g., anxious, stressed). Many theories of drug dependence and addiction, including negative reinforcement models such as the self-medication hypothesis (Eissenberg, 2004) and the RP model (Hendershot et al., 2011), posit that avoiding negative affect plays an important role in both initiating and maintaining addictive behavior. Indeed, NA has been found in most EMA studies to have a positive within-person association with craving and substance use across various substances (see Serre et al., 2015). For example, higher NA is associated with same-day levels of craving and consumption among college students not seeking treatment for alcohol problems (Simons, Gaher, Oliver, Bush, & Palmer, 2005), as well as students in recovery from different SUDs (Cleveland & Harris, 2010). The association between NA and craving has also been found for people in treatment for tobacco (Serre et al., 2018) and opioid (Epstein et al., 2009; Huhn et al., 2016) addictions, as well as for non-treatment seeking smokers (Bujarski et al., 2015). Yet, some studies have failed to find an association between NA and subsequent craving (e.g., Fatseas et al., 2018).
Although there is generally strong evidence for the within-person relationship between negative affect and craving, there are likely both between- and within-person differences in the conditions under which NA is associated with craving. At the between-person level, individuals differ in their reactivity to negative mood during post-withdrawal state from opiates (Koob & Le Moal, 2001). At the within-person level, variability in daily experiences may intensify or offset the linkage between negative affect and craving. It may be on days when individuals experience more interpersonal problems, for example, that higher-than-average NA and craving are more strongly coupled. This possibility suggests that it is important to examine within-person moderators of the NA-Craving relationship, such as daily positive and negative social exchanges. Identifying these associations may help patients in treatment identify problematic interactions, and work to develop coping skills to manage them.
Social Exchanges
In addition to craving and negative affect, interpersonal relationships are considered a key exogenous influence in the RP model (Hunter-Reel, Mccrady, & Hildebrandt, 2009). Daily diary research has documented that negative social exchanges, such as interpersonal conflict and social stress, are the most distressing of daily events (e.g., Bolger, DeLongis, Kessler, & Schilling, 1989), and thus may be related to OUD patients’ craving and/or substance use. Indeed, stressful social situations have been found to increase reports of craving for cocaine (Waldrop et al., 2010), alcohol (Clay et al., 2018), cannabis (Buckner, Zvolensky, Ecker, & Jeffries, 2016), and tobacco (Watson, Demarree, & Cohen, 2018). Perceived criticism is associated with use among opioid-dependent patients (Kadam, Sinha, Nimkar, Matcheswalla, & De Sousa, 2017). Additionally, negative family behaviors (e.g., withdrawing, not tolerating behavior) are associated with more drinking (McCrady, Hayaki, Epstein, & Hirsch, 2002), and stressful relationships with friends also predict poorer outcomes (Gordon & Zrull, 1991). Although most of these findings are based on laboratory studies, within-person data have shown that negative social exchanges are positively associated with same-day craving among college students in Twelve-step substance abuse recovery (Cleveland & Harris, 2010). Further, being in an argument has been associated with heroin use in daily life among individuals in outpatient treatment (Preston, Kowalczyk, et al., 2018b). These types of data elucidate the experiences that are linked with craving day-to-day.
There is also a large body of research suggesting that social exchanges in substance-free settings and supportive social relationships with sober friends improve SUD recovery rates (Groh, Jason, Davis, Olson, & Ferrari, 2007; Moos, 2007). For example, interactions with peers through peer-based recovery support services have been found to be effective for increasing abstinence (Bassuk, Hanson, Greene, Richard, & Laudet, 2016). Similarly, attending and being involved in Twelve-Step meetings, where positive social exchanges presumably occur, has also been associated with improved long-term abstinence outcomes (e.g., Kelly, Stout, & Slaymaker, 2013). Numerous daily studies have also investigated the relationships of a variety of positive social exchanges with positive affect and health more broadly, documenting the expected positive relationship (e.g., Bernstein, Zawadzki, Juth, Benfield, & Smyth, 2018; Machell, Kashdan, Short, & Nezlek, 2015; Rook, 2001). On the other hand, positive social events and exchanges have also been linked to appetitive motives (e.g., Gable, 2006) and craving-related outcomes such as desire-to-drink (Armeli & Tennen, 2000; Carney, Armeli, Tennen, Affleck, & O’Neil, 2000). These conflicting findings may result from differences in operationalization of the positive social exchange construct. Positive social events linked to appetitive motives often include examples such as, “going out socializing with friends/date”, “activity/visits with friends/family members”, or “doing something special for a friend”, that is, events in which someone is seeking to achieve positive reward (as opposed to avoiding negative). Among individuals with SUDs, it makes sense that these experiences could be associated with craving or substance use. In contrast, the current study focused on positive social exchanges pertaining strictly to events in which participants were the recipient of a supportive act (e.g., someone showing that they cared) within a residential treatment setting. In line with findings from the social support literature, we suggest that these events are more likely linked to lower craving and/or use.
Importantly, there is not clear evidence of the role of these social influences on difficult days (e.g., a day when negative affect is higher than usual). Changes in social factors could interact with intraindividual processes, such as negative affect. For example, negative social exchanges may exacerbate NA and/or craving and put individuals at increased risk for use, whereas positive social exchanges may mitigate this risk. Studies have found stronger associations between daily negative affect and drinking among those with lower overall social support (Hussong, Hicks, Levy, & Curran, 2001), and weaker relationships among individuals with higher overall support (Hussong, Jones, Stein, Baucom, & Boeding, 2011). Additionally, it is not yet well understood whether negative and positive social exchanges are related to craving in similar or dissimilar ways (in terms of both degree and direction). Different aspects of the social environment could influence one another, such as socially supportive individuals replacing or buffering the negative influences of non-supportive individuals (Humphreys & Noke, 1997; Bond et al., 2003). Considering how multiple internal and external factors interact may provide a unique perspective that elucidates a number of the processes related to daily craving variation.
The Present Study
Guided by the RP model, the current study employed a 12-day EMA design to examine the interplay among fluctuations in mental state (i.e., craving, negative affect) and the occurrence of specific external social events (i.e., positive and negative social exchanges) in daily life during residential treatment for opioid use disorder. The goal was to investigate whether supportive or conflictual social exchanges during daily life were directly related to same-day craving, as well as whether positive and negative social exchanges interacted with one another and/or moderated the relationship between negative affect and same-day craving. Investigating interactions among social exchanges and NA illuminated how daily linkages in one domain (e.g. between NA and craving) varied based upon day-to-day changes in another domain (e.g. social exchanges).
Three research questions guided the current study. First, are within-person fluctuations in daily negative affect, frequency of daily positive social exchanges, and frequency of daily negative social exchanges associated with same-day craving? We hypothesized that higher negative affect and more negative social exchanges than usual would be associated with higher same-day craving, whereas more positive social exchanges than usual would be associated with lower same-day craving. Second, are day-level associations between negative affect and craving moderated by the frequency of daily positive and negative social exchanges, and to the same degree? We hypothesized that there would be a stronger positive association between negative affect and craving on days when participants experienced more negative social exchanges than usual, and a weaker association between negative affect and craving on days when participants experienced more positive social exchanges than usual. Third, are day-level associations between frequency of negative social exchanges and craving moderated by daily frequency of positive social exchanges? We hypothesized that there would be a weaker or nonsignificant association between negative social exchanges and craving on days when participants experienced more positive social exchanges than usual.
Methods
Participants
The participants were 73 patients (77% male), age 19 to 61 (Mage=30.10, SDage=10.13) in residential treatment for opioid use disorder. All participants met criteria for prescription opioid dependence as determined by the Structured Clinical Interview for DSM-IV-TR (SCID; First, 2005), and Form-90D (Westerberg, Tonigan, & Miller, 1998), for whom prescription opioids were the primary drugs of abuse, and who had completed medically assisted withdrawal from prescription opioids in the last 10–14 days. Other inclusion criteria included being at least age 18 years, scheduled to stay in residential treatment for at least 30 days, and willingness to comply with the research protocol. Patients were excluded from participation if they had any history of serious mental illness, traumatic brain injury, or intravenous drug use, as well as any current use of opiate agonists (methadone or buprenorphine) or antagonist (naltrexone). All participants provided written informed consent after the study protocol was fully explained to them. Demographic information on this sample, including information about psychiatric comorbidity, addiction history, and concurrent medication use of the participants, has been published elsewhere (Huhn et al., 2016; Lydon-Staley et al., 2017).
Procedure
Participants were invited to take a smartphone-based survey 4 times per day for up to 12 consecutive days. Residential patients were recruited to participate in the study at approximately 10–14 days post-medically assisted withdrawal. Data were then collected over 12 consecutive days that corresponded roughly to the second through fourth week of residential treatment, after which patients – in consultation with treatment staff – decided whether to remain in residential treatment or transition out. Given that participants were in residential treatment for opioid dependence, we anticipated moderate compliance and chose four assessments per day to allow participants to miss some data entries, while still providing multiple data points per day on most survey days. A preset alarm notified participants that a survey was ready to be taken at early morning, late morning, mid-afternoon, and evening times that did not conflict with their treatment programs. The surveys took approximately 2–3 minutes each to complete. If participants did not choose to take the survey after the first notification, they were given opportunities every 15 minutes for up to one hour, after which the survey was closed until the next measurement occasion. Research staff encouraged survey participation by using brief in-person meetings to answer questions and manage technical difficulties.
The protocol allowed for some variation in EMA start times for each of the four assessments, where participants started the early morning survey between 6:45 – 11:00, the mid-morning survey between 11:00 – 15:32, the afternoon survey between 16:30 – 20:54, and the evening survey between 21:00 – 22:20. Most entries were made soon after the first prompt. Mean entry times were 6:58, 11:25, 16:49, and 21:19 for the four daily assessments, respectively. Person-level variability in average entry time was calculated as the within-person standard deviation (SD) of time-of-entry for each person at each assessment. The average person-level variability was 11.4 minutes for the early morning survey (SD = 16.2 minutes), 16.8 minutes for the mid-morning survey (SD = 41.4 minutes), 9.6 minutes for the afternoon survey (SD = 12 minutes), and 7.8 minutes for the evening survey (SD = 5.4 minutes). All study procedures were approved by the relevant institutional review board.
Measures
Craving
Craving was measured four times per day for up to 12 consecutive days with two items that assessed craving frequency and intensity on a continuous touchpoint visual-analogue scale (VAS; slider-type) with anchors at each end (0=No craving and 100=Very frequent/intense). Specifically, the items were, “Since last data entry [Since waking], how frequent were your drug cravings?” and, “Since last data entry [Since waking], how intense were your drug cravings?”. Correlations between craving intensity and frequency were high within assessment periods, with a correlation of 0.87 at assessments 1, 2, and 3, and 0.90 at assessment 4. Correlations between the two items were also high across study days, ranging from a high of 0.97 on days 2 and 3 of the study to a low of 0.78 on day 10 of the study. Following previous research (Huhn et al., 2016), the product of the frequency and intensity of drug craving was used to create a craving score for each individual at each time point, and then rescaled by dividing by 100. An average craving score was created for each participant for each day of the study by averaging across the four assessments. The measure provided reliable assessment of within-person change, Rc = 0.85 (as per the generalizability theory approach for intensive repeated measures data, see Bolger & Laurenceau, 2013).
Negative Affect
Negative affect (NA) was measured four times per day for up to 12 consecutive days using eight items from the PA-NA Scales (Watson, Clark, & Tellegen, 1988) on a continuous touchpoint VAS scale with anchors at each end (0 = Not at all and 100 = Very). The items took the form, “Since last data entry [Since waking], have you felt… ‘angry’, ‘irritable’, ‘lonely’, ‘sad’, ‘guilty’, ‘ashamed’, ‘anxious’, and ‘stressed’”. A composite NA score was calculated for each participant for each day as the average of the eight responses across the day, Rc = 0.80. Additionally, a person-level variable for negative affect was created for each participant by calculating the arithmetic mean across each participant’s repeated measures.
Negative Social Exchanges
Negative social exchanges were measured three times per day (late morning, mid-afternoon, and evening) with five binary (yes/no) items that were adapted from the Test of Negative Social Exchange (TENSE) scale (Ruehlman & Karoly, 1991). The items were, “Since last data entry, did someone… ‘lose his/her temper with you’, ‘get angry with you’, ‘get impatient with you’, ‘disagree with you’, ‘argue with you’”. Responses to these items were coded (1=exchange occurred, 0=exchange did not occur) and then summed across the three daily measurement occasions to create a measure of negative exchanges for each participant for each day of the study (Rc = 0.82), a method consistent with previous research (e.g., Rook, 2001).
Positive Social Exchanges
Positive social exchanges were measured three times per day with five binary (yes/no) items. The items were, “Since last data entry, did someone… ‘compliment you’, ‘show you that they cared about you’, ‘express sympathy toward you’, ‘let you know they understand your problems’, ‘let you know they understand your stress’”. These items were piloted in a collegiate recovery community (CRC) to capture positive social exchanges that would support recovery, with individual items generated from interviews with CRC staff and members. In the CRC sample, which is detailed in Cleveland, Harris, & Wiebe (2010), the items in general were endorsed about 58% of days, compared to 20% of days for which the negative social exchange items were endorsed. Responses to these items were coded (1=exchange occurred, 0=exchange did not occur) and then summed across the three daily measurement occasions to create a measure of positive exchanges for each participant for each day of the study. The measure provided reliable assessment of within-person change, Rc = 0.75.
Other covariates
Covariates included sex, which was indicated by a dichotomous variable (0 = female, 1 = male), and age, which was indicated by a continuous variable of self-reported age ranging from 19–61.
Data Analysis
We examined within-person, day-level associations among daily positive and negative social exchanges, negative affect, and craving using a multilevel modeling (MLM) framework that accommodated the nested nature of the data (repeated measures nested within persons; Bolger & Laurenceau, 2013; Raudenbush & Bryk, 2002).
Data Preprocessing
The PSE, NSE, and NA variables were decomposed into time-varying and time-invariant components (Bolger & Laurenceau, 2013). Person-level variables representing usual levels of PSE, NSE, and NA were computed for each participant as the arithmetic mean of their repeated measures. Time-varying or “state” variables were computed for each individual on each day as the difference between the observed score and the individual’s person-mean. Person-level variables were grand-mean centered to represent between-person differences in PSE, NSE, and NA on average across the study period. Time was centered on Day 1 of the study.
After running initial models and examining the distribution of model residuals, Tukey’s Ladder of Powers (Tukey, 1977) approach was applied to perform a power transformation on the outcome variable, daily craving, in order to correct for positive skewness and avoid violating the assumption that residuals were normally distributed. Importantly, this procedure was not undertaken a priori, but only after examining the distribution of residuals from our initial models. The “transformTukey” function from the rcompanion package in R performed iterative Shapiro-Wilk tests to find the power transformation that made the data fit the normal distribution as closely as possible. The lambda value that maximized the W statistic for the iterative Shapiro-Wilk tests was 0.275. The change in skew and kurtosis from the original variable (skew = 2.64, kurtosis = 7.83) to the transformed variable (skew = 0.13, kurtosis = −0.86) indicated that the transformed variable more closely approximated a normal distribution. Because generalized linear modeling is another common approach when dealing with outcomes that are not normally distributed, we ran zero-inflated Poisson models and checked them against our linear models with the transformed outcome; the pattern of results did not substantively change. We therefore proceed with the linear models to facilitate interpretability of our results.
A lag-1 variable for daily craving was then created and included in all models to control for the autoregressive effects of craving from day-to-day, allowing us to examine the effects of PSE, NSE, and NA on the daily change in craving. Note that this differs from within-person centering; specifically, person-centering removes the mean across all days, where the lag-1 predictor accounts for day-to-day carryover effects. Within-person centering accounts for differences between individuals in what they consider “high” craving, and differences in, e.g., sociability, where one person might simply have more social experiences than another on an average day. By contrast, the lag-1 predictor accounts for the fact that night does not reset craving to normal—that is, if I had high cravings yesterday, it is likely that today my cravings will still be high. The effects of other predictors is then relative to our best guess at today’s craving given how you felt yesterday. The inclusion of a lag-1 predictor can lead to some biases in multilevel models. However, alternative estimation approaches (e.g., XTDPDML; Williams, Allison, & Moral-Benito, 2016; or manually via ML-SEM tools like Pritikin et al., 2019) are best suited to short-time models, especially for models with a number of predictors (Allison, Williams, & Moral-Benito, 2017; Bhargava & Sargan, 1983) and require a stronger normality assumption. In order to ensure that our results are not simply products of bias, we ran the models again without the lag-1 predictor; the pattern of results did not substantively change. To protect against possible biases in the standard errors, we also computed bootstrap-based standard errors. We therefore proceed with interpretation of the models including the lag-1 predictor.
Participants provided an average of 9.66 (SD = 2.58, Range = 1 – 12) days of craving data each. Roughly half (47%) of participants had more than 10 days of craving data. There were n = 2 participants who provided data on craving for two days or less and were thus excluded from analysis when the lag-1 craving variable was included in the model, leaving 564 days of data nested within 71 persons available for the current analysis.
Multilevel Models
Correlational analyses were first conducted to test whether PSE and NSE were associated with each other or with average daily NA at the between-person level. In multilevel models controlling for age, sex, day of study, previous day’s craving, and between-person differences in negative affect and positive and negative social exchanges, we then tested the relationships of daily negative affect and positive and negative social exchanges with same-day ratings of craving.
Models were constructed as:
| Level 1: |
In the above equation, i indexed individuals and t indexed time points. Cravingit is the reported craving for person i on day t; β0i indicates the expected level of craving on the first day of the study when all predictors are at their mean level for the typical individual; β1i, β2i, β3i, and β4i indicate within-person differences in craving associated with yesterday’s craving, NA, PSE, and NSE variables, respectively; Β5i indicates the effect of time in the study on craving in order to account for time as a third variable (see Bolger & Laurenceau, 2013); and eit are day-specific residuals that were allowed to autocorrelate (AR1). Pairwise interactions between NA, PSE, and NSE variables at Level 1 were then added to this baseline model.
Person-specific intercepts and variance from the Level 1 model were specified at Level 2 as:
| Level 2: |
In the above equations, the gamma (γ) coefficients represent between-person differences in individual effects. Models were tested with six between-person (Level 2) random effects: a random-intercept (ν0i), four random slopes (ν1i,…,ν4i); and residual error terms (e.g., εit). The random intercept captures between-person variability in participants’ average level of craving, whereas each random slope captures between-person variability in the strength of the relation between one predictor and daily craving. Note that our design does not allow for causal inference, and our model does not test temporal direction; although we interpret these results to mean that our predictors influence craving, it is equally possible that craving leads to, for example, more negative social exchanges, or more likely that a more intricate feedback system is at work. We leave these questions to future work.
To get an estimate of effect size for each of the variables of interest, change in pseudo-R2 was calculated as the difference between an intercept-only model and a model in which a single predictor had been added, to estimate the total proportion of variability in craving explained by each of the fixed effects. This process was followed for all predictor variables in the full model. Change in pseudo-R2 (henceforth ΔR2) attributed to the interactions is the difference between a model with both components of the interaction and one with the same components and the interaction term. All models were fit using the lme4 package in R using restricted maximum likelihood estimation, with incomplete data treated using missing at random assumptions. Bootstrapping with 1,000 bootstrap replicates was used to obtain standard errors and 95% confidence intervals for all parameters. Table 3 reports the results from two models, one with main effect associations only and the other with the addition of interaction terms. All results reported below are from the final model with the interaction terms included. Statistical significance was evaluated at α = 0.05. Effect sizes were generally small, with ΔR2 ranging from .001 to .25.
Table 3.
Results of multilevel models examining associations among negative affect, negative social exchanges, and positive social exchanges with same-day craving.
| Model 1 | Model 2 | ||||
|
| |||||
| Fixed effects | Estimate | 95% CI | Estimate | 95% CI | ΔR2 |
|
| |||||
| Intercept | 6.27* | 4.23, 8.23 | 6.31* | 4.09, 8.27 | -- |
| Day of study | −0.06* | −0.11, −0.01 | −0.06* | −0.11, −0.01 | 0.01 |
| Age | −0.05* | −0.10, −0.004 | −0.05* | −0.09, 0.00 | 0.01 |
| Sex | −0.34 | −1.41, 0.73 | −0.40 | −1.53, 0.60 | 0.004 |
| Person-level NA | 0.08* | 0.05, 0.11 | 0.08* | 0.05, 0.11 | 0.25 |
| Person-level PSE | −0.06 | −0.24, 0.09 | −0.08 | −0.25, 0.10 | 0.01 |
| Person-level NSE | 0.26 | −0.07, 0.61 | 0.28 | −0.08, 0.67 | 0.09 |
| Previous day’s craving | 0.19* | 0.10, 0.29 | 0.18* | 0.09, 0.28 | 0.13 |
| Day-level NA | 0.05* | 0.03, 0.07 | 0.05* | 0.03, 0.07 | 0.04 |
| Day-level PSE | −0.01 | −0.07, 0.05 | −0.01 | −0.06, 0.04 | 0.002 |
| Day-level NSE | 0.08* | 0.002, 0.16 | 0.08* | 0.001, 0.16 | 0.005 |
| Day-level NA × PSE | −0.01* | −0.01, −0.001 | 0.002 | ||
| Day-level NA × NSE | 0.003 | −0.01, 0.01 | 0.00 | ||
| Day-level NSE × PSE | 0.004 | −0.02, 0.03 | 0.001 | ||
|
| |||||
| Random effects | Estimate | 95% CI | Estimate | 95% CI | |
|
| |||||
| Intercept | 1.54* | 1.13, 2.02 | 1.56* | 1.14, 2.05 | |
| Day-level NA | 0.03* | 0.00, 0.04 | 0.03* | 0.00, 0.04 | |
| Day-level craving (lag-1) | 0.09* | 0.00, 0.13 | 0.10* | 0.00, 0.14 | |
| Day-level PSE | 0.05* | 0.00, 0.09 | 0.04* | 0.00, 0.09 | |
| Int., NA slope corr. | −0.001 | −0.02, 0.01 | −0.002 | −0.02, 0.01 | |
| Int., craving slope corr. | −0.12* | −0.20, −0.05 | −0.12* | −0.20, −0.05 | |
| Int., PSE slope corr. | −0.02 | −0.06, 0.03 | −0.01 | −0.06, 0.03 | |
| Residual | 1.53* | 1.41, 1.63 | 1.53* | 1.40, 1.63 | |
Note. N = 564.
= p ≤ 0.05. NA = Negative affect. PSE = Positive social exchanges. NSE = Negative social exchanges. Int. = Intercept. Corr. = Correlation. ΔR2 = Change in pseudo-R2.
Results
Descriptive and correlational analyses
Descriptive statistics summarizing the data for all variables included in the analysis are presented in Table 1. Means and standard deviations of all PSE and NSE items are shown in Table 2. Of note, participants reported a mean number of daily PSE of 6.59 (SD = 4.00, Range = 0–15), and a mean number of daily NSE of 1.44 (SD = 2.27, Range = 0–11). In addition, all participants reported experiencing at least one positive social exchange during the 12-day EMA assessment, whereas 8% of participants (N = 6) reported experiencing no negative social exchanges during this period.
Table 1.
Descriptive Statistics and Correlations Among Study Variables
| 1 | 2 | 3 | 4 | 5 | M | SD | Range | ICC | Rc | |
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | ||||||||||
| 1. Age | 30.10 | 10.13 | 19–61 | --- | --- | |||||
| 2. Sex (1 = male) | −.32 | 0.77 | 0.43 | 0–1 | --- | --- | ||||
| Daily | ||||||||||
| 3. Craving | −.13 | −.05 | 4.84 | 3.34 | 0–12.59 | .68 | 0.85 | |||
| 4. Negative affect | .05 | −.09 | .52 | 34.83 | 20.46 | 0–100 | .67 | 0.80 | ||
| 5. Positive social exchanges | .15 | −.05 | −.04 | .002 | 6.59 | 4.00 | 0–15 | .38 | 0.75 | |
| 6. Negative social exchanges | −.06 | .04 | .21 | .23 | .09 | 1.44 | 2.27 | 0–11 | .27 | 0.82 |
Note. M = Mean. SD = Standard deviation. ICC = Intraclass correlation coefficient. Rc = Reliability coefficient.
Table 2.
Types of positive and negative social experiences
| M | SD | |
|---|---|---|
|
Positive Social Experiences
| ||
| Someone showed they cared about me | 1.61 | 0.96 |
| Someone let me know they understood my problems | 1.45 | 0.95 |
| Someone let me know they understood my stress | 1.22 | 0.98 |
| Someone complimented me | 1.22 | 0.97 |
| Someone expressed sympathy toward me | 1.08 | 0.99 |
|
| ||
|
Negative Social Experiences
| ||
| Someone disagreed with me | 0.50 | 0.74 |
| Someone argued with me | 0.28 | 0.56 |
| Someone was impatient with me | 0.28 | 0.56 |
| Someone got angry with me | 0.22 | 0.49 |
| Someone lost their temper with me | 0.16 | 0.42 |
Research Question 1: Are NA, PSE, and NSE associated with same-day craving?
The first research question was to investigate whether day-level NA, PSE, and NSE were uniquely associated with same-day craving after controlling for previous day’s craving and average NA, PSE, and NSE. Results are shown in Table 3. The effect of time revealed a significant main effect of day of study on craving, such that craving decreased over the course of the study (b= −0.06, p < .001, ΔR2 = .01). On days when participants’ NA was higher than their usual, craving was also higher after accounting for daily PSE and NSE (b = 0.05; 95% CI = 0.03, 0.07, ΔR2 = .04). Additionally, on days when participants had more NSE than usual, craving was higher after accounting for daily NA and PSE (b = 0.08; 95% CI = 0.01, 0.16, ΔR2 = .01). The day-level association between PSE and craving was not significant (b = −0.01, n.s.).
Research Question 2: Do PSE or NSE moderate the association between NA and craving?
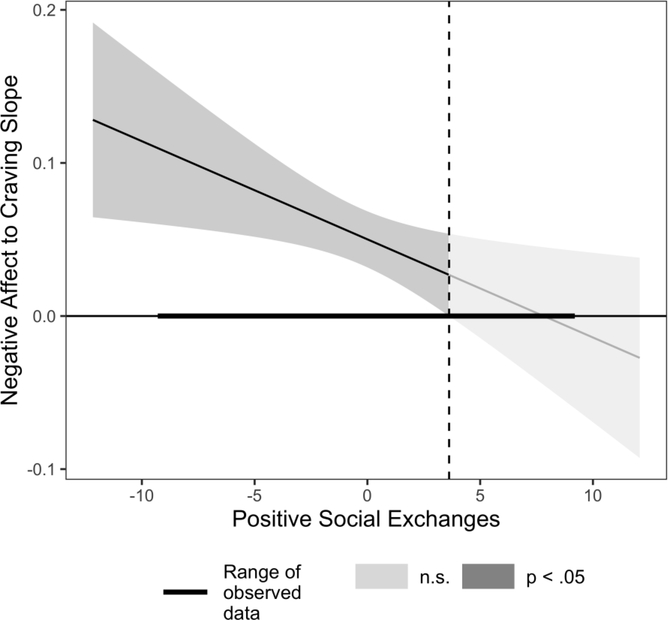
The second research question was to explore whether daily PSE and/or NSE moderated the same-day linkage between NA and craving. Results from the model are shown in Table 3 and depicted in Figure 1. Findings revealed that daily PSE moderated the day-level association between NA and craving (b = −0.01; 95% CI = −0.01, −0.001, ΔR2 = .002). The Johnson-Neyman technique was used to probe the interaction and identify the range of values of PSE at which the association between NA and craving was significant (i.e., the region of significance). This analysis found that when the frequency of daily PSE was outside the interval [3.62, 9.08] for the observed data, the NA-craving slope was significant. Given that reported social exchanges were in whole numbers, this means that there was a significant positive same-day association between NA and craving on days when individuals had fewer than four more positive social exchanges than usual. On days when individuals had at least four more positive exchanges than usual, the same-day linkage between negative affect and craving was no longer significant. Fluctuation in NSE did not moderate the NA-Craving association (b = 0.003; n.s.).
Figure 1.
This figure demonstrates how the within-person, day-level association between negative affect and craving is moderated by the frequency of daily positive social exchanges. Positive social exchanges decoupled the same-day linkage between negative affect and craving on days when individuals had at least four more positive exchanges than usual.
Research Question 3: Do PSE moderate the association between NSE and craving?
The third research question was to explore whether frequency of PSE moderated the same-day association between craving and frequency of NSE. Results are shown in Table 3 and indicated that the interaction was non-significant (b = 0.004; n.s.). The three-way interaction between NA, PSE, and NSE was also tested, and found non-significant (b = 0.00; n.s.).
Discussion
The current study is unique in examining associations of both positive and negative social exchanges with craving at the daily level, as positive social exchanges have received less attention in prior research. Although the relationship between negative affect and craving has received significant attention in the literature, including the EMA literature (Serre et al., 2015), this study is also one of the first to consider the potential role of daily social exchanges in either enhancing or reducing the within-person, same-day linkage between negative affect and craving among individuals in residential treatment for opioid dependence. Craving reported in daily life during residential treatment had positive relationships with same-day ratings of negative affect and negative social interactions. However, although higher-than-usual negative affect was associated with elevated craving, this relationship was decoupled on days when patients had four more positive social exchanges than usual, on average. Taken together, results highlight differences in how positive and negative social exchanges were related to craving; whereas more frequent negative social exchanges were directly related to elevated craving that same day, positive social exchanges decoupled negative affect from heightened drug craving during everyday life in residential treatment. Findings are discussed in more detail below, including important implications for treatment and intervention.
Prior to examining primary research questions, descriptive statistics revealed that positive social exchanges were more frequent than negative social exchanges (M = 6.59 and 1.44, respectively). This ratio of positive to negative experiences is similar to the ratio found in the collegiate recovery community in which the positive social exchange items were piloted (roughly 3:1), and is also consistent with previous research in non-substance using samples. For example, Bernstein et al. (2018) found that adults reported the average pleasantness of social interactions in daily life to be 4.93 on a 0 = unpleasant to 6 = pleasant scale. Machell and colleagues (2015) found that college students reported 3.75 positive social events per day on average compared to 1.28 negative social events (out of 7 possible). Similarly, Rook (2001) found that older adults reported 6.52 positive exchanges per day on average (out of 14 possible) and 0.34 negative exchanges per day (out of 6 possible). An EMA study that reported on daily hassles among individuals in outpatient substance use treatment (Preston, Schroeder, et al., 2018) found that the average number of daily hassles was 2.33 (of course, “daily hassles” also encompassed many non-social experiences). Thus, our findings for the ratio of positive to negative exchanges are relatively consistent with prior work.
Yet, despite the much higher proportion of positive to negative social exchanges, negative exchanges (but not positive exchanges) were directly linked to same-day craving (RQ #1). That negative but not positive exchanges were directly linked to craving is consistent with research demonstrating that negative social exchanges occur less often but are related more consistently to daily mood than positive exchanges (Rook, 2001). The finding for negative social exchanges is also consistent with prior research indicating that negative exchanges are associated with same-day levels of craving among college students in Twelve-step substance abuse recovery (Cleveland & Harris, 2010) and that being in an argument is associated with heroin use in daily life among outpatients (Preston, Kowalczyk, et al., 2018b), and extends it to a sample of opioid-dependent patients in residential treatment. The co-occurrence of negative social exchanges and craving in this study may be particularly concerning given that it was during residential treatment. As individuals are likely to continue experiencing interpersonal exchanges characterized by anger, impatience, and disagreements during daily life post-treatment, it may be particularly important for treatment providers to focus on helping patients develop strategies for decoupling negative interactions and drug craving during their time in residential treatment.
In contrast, positive social exchanges were not directly related to same-day craving; rather, they decoupled the association between negative affect and craving (RQ #2). Because participants reported frequently experiencing positive interactions on any given day, it may be that deviations from one’s typical value for positive exchanges are not as noticeable in and of themselves as deviations from one’s typical value for negative exchanges, which were less frequent on average. Instead, results indicated that higher-than-average negative affect did not co-occur with higher-than-average craving on days when participants reported four more positive social exchanges than usual, compared to days when they reported fewer than four more positive social exchanges than usual. It is important to note that the buffering effect is relatively small—four more positive social exchanges than a participant’s usual number on a given day are required in order to buffer the link between negative affect and craving to the point where it is no longer statistically significant. This suggests that individuals who have recently detoxed and are in the early stages of OUD treatment need those around them to notice when they are having a bad day and give them extra social support. It is not just about increasing the frequency of positive social exchanges, but doing so on days when negative affect is higher than usual. This finding may explain the mixed results for positive social exchanges in prior research: sometimes positive social exchanges have a positive effect because they are needed; other times they have no result.
These findings have important implications for theory and intervention. Regarding theory, the Relapse Prevention model emphasizes the interactions between internal processes and social environments, yet has historically been focused more on environments that confer risk. This study advances the need to consider the dynamic nature of both negative and positive social environments, as well as their interactions with internal processes at the within-person level. Regarding intervention, just-in-time adaptive interventions (JITAI) are being employed that link real time data on behaviors or moods (collected via wearable devices and other sensors; e.g., Brick et al., 2020) to the type and timing of intervention that is delivered via smartphone, and can be tailored to individual needs (Vinci et al., 2018). JITAI have started to be implemented for alcohol use disorder (Gustafson et al., 2014) and smoking cessation (Naughton et al., 2016). The results from the current study suggest that these interventions have potential to intervene at crucial times (e.g., days with higher-than-usual negative affect and frequency of negative social exchanges, and days with lower-than-usual frequency of positive social exchanges) by either targeting the negative mood and negative social interaction directly, or facilitating some form of in-person or remote socially supportive interaction.
Limitations and Future Directions
Despite the contributions of this study to the literature, it is important to note a few limitations. First, patients being in residential treatment likely restricted the range of potential positive and negative social exchanges they experienced. Due to the presence of therapeutic professionals in this setting, patients would seem less likely to experience escalating patterns of negative social experiences. In one respect, studying people in a single residential facility may have reduced some of the noise that would have been inherent if individuals were in their natural environments and self-selecting into (or being selected into) social surroundings that offered greater or lesser access to social support. In the residential setting used here, every participant presumably began with roughly equal access to negative and positive social interactions. Yet, it is important that findings are understood to be restricted to the distributions of these experiences as observed, rather than interpreted as applying to the possible range of positive and negative exchanges. Additionally, positive social exchanges were assessed with a scale that is not yet well-established in the literature, and existed at a different level and range than negative social exchanges within the residential setting in this sample. Thus, direct comparisons between positive and negative exchanges should be viewed as more speculative.
Second, we focused only on the frequency of social experiences without regard for the degree of positivity or negativity experienced from any one particular interaction, and/or whom that interaction was with. For example, we do not know whether social exchanges occurred with professionally trained treatment staff, other staff, or with other residents. We also cannot determine from these self-report data whether participants were actually being treated dismissively, in the case of negative social exchanges, or whether they were having a strong subjective reaction to a neutrally expressed difference of opinion. Different patients could perceive similar interactions quite differently. Future work might examine the role of perceived intensity of a given social exchange, as well as the possible impact of the relationship to the individual with whom the social interaction took place.
Third, we make no attempt here to test the causal structure of our model—our design does not inherently permit such inference, and our model is not amenable to alternative causal approaches (e.g. Granger causality). Although our results are consistent with theory that suggests that negative affect induces craving, it would also be consistent with the suggestion that craving induces negative affect. For example, a spike in craving might make someone irritable, causing them to say something that causes a negative social interaction. However, we decided to examine associations among these variables at the day-level rather than the assessment-level for several reasons. First, day-level aggregates incorporate more information into estimating each construct, and are thus more reliable than utilizing measures at a single assessment. Second, day-level averages help to mitigate the effects of missing data. Finally, life in residential treatment is highly regimented. There may be time-of-day based effects for all variables that disappear during aggregation to the day level. Future work should examine the directionality of these associations using vector-autoregressive (Gates et al., 2010) or state space models (Li et al., 2019).
Conclusion
To our knowledge, this study is among the first to use an EMA design to examine the dynamic interplay among craving, negative affect, and positive and negative social exchanges at the within-person level among individuals in residential OUD treatment. There were differences in how positive and negative social exchanges related to same-day craving; whereas negative social exchanges were directly associated with craving, positive exchanges decoupled the same-day linkage between negative affect and craving. Thus, individuals in the early stages of OUD treatment need those around them to notice when they are having a bad day and give them extra social support. Treatment providers should strive to create an environment that both limits negative exchanges and facilitates positive social exchanges on particularly difficult days within their residential facilities. Increased understanding of how social exchanges and affect contribute to craving variation could aid the development of better treatments, such as mobile just-in-time adaptive interventions, by elucidating intervention targets and guiding the timing of delivery.
Public Health Significance.
This study highlights the importance of daily social interactions for patients in residential treatment for opioid use disorder, indicating that negative interactions are linked with higher craving and that extra positive interactions can decouple the daily linkage between negative affect and craving.
Acknowledgments
Grant Support
This study was supported by grant R01 DA035240 from the National Institute on Drug Abuse. Author Knapp was supported by the Prevention and Methodology Training Program (T32 DA017629; MPIs: J. Maggs & S. Lanza) with funding from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
References
- Allison PD, Williams R, & Moral-Benito E (2017). Maximum likelihood for cross-lagged panel models with fixed effects. Socius: Sociological Research for a Dynamic World, 3, 1–17. 10.1177/2378023117710578. [DOI] [Google Scholar]
- Armeli S, & Tennen H (2000). Does affect mediate the association between daily events and alcohol use? Journal of Studies on Alcohol, 61(6), 862–871. [DOI] [PubMed] [Google Scholar]
- Bassuk EL, Hanson J, Greene RN, Richard M, & Laudet A (2016). Peer-delivered recovery support services for addictions in the United States: A systematic review. Journal of Substance Abuse Treatment, 63, 1–9. 10.1016/j.jsat.2016.01.003 [DOI] [PubMed] [Google Scholar]
- Bernstein MJ, Zawadzki MJ, Juth V, Benfield JA, & Smyth JM (2018). Social interactions in daily life: Within-person associations between momentary social experiences and psychological and physical health indicators. Journal of Social and Personal Relationships, 35(3), 372–394. 10.1177/0265407517691366 [DOI] [Google Scholar]
- Bhargava A, & Sargan JD (1983). Estimating dynamic random effects models from panel data covering short time periods. Econometrica, 51(6), 1635–1659. 10.2307/1912110 [DOI] [Google Scholar]
- Bolger N, DeLongis A, Kessler RC, & Schilling EA (1989). Effects of daily stress on mood. Journal of Personality and Social Psychology, 57, 808–818. [DOI] [PubMed] [Google Scholar]
- Bolger N, & Laurenceau JP (2013). Intensive longitudinal methods: An introduction to diary and experience sampling research. New York, NY: The Guilford Press. [Google Scholar]
- Bond J, Kaskutas LA, & Weisner C (2003). The persistent influence of social networks and Alcoholics Anonymous on abstinence. Journal of Studies on Alcohol, 64, 579–588. [DOI] [PubMed] [Google Scholar]
- Brick TR, Mundie J, Weaver J, Fraleigh R, & Oravecz Z (2020). Wear-IT: Low-burden mobile monitoring and intervention through real-time analysis. Journal of Medical Internet Research (JMIR): Formative Research, 4(6), e16072. doi: 10.2196/16072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Zvolensky MJ, Ecker AH, & Jeffries ER (2016). Cannabis craving in response to laboratory-induced social stress among racially diverse cannabis users: The impact of social anxiety disorder. Journal of Psychopharmacology, 30(4), 363–369. 10.1177/0269881116629115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujarski S, Roche DJO, Sheets ES, Krull JL, Guzman I, & Ray LA (2015). Modeling naturalistic craving, withdrawal, and affect during early nicotine abstinence: A pilot ecological momentary assessment study. Experimental and Clinical Psychopharmacology. 10.1037/a0038861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney MA, Armeli S, Tennen H, Affleck G, & O’Neil TP (2000). Positive and negative daily events, perceived stress, and alcohol use: A diary study. Journal of Consulting and Clinical Psychology, 68(5), 788–798. [PubMed] [Google Scholar]
- Catley D, O’Connell KA, & Shiffman S (2000). Absentminded lapses during smoking cessation. Psychology of Addictive Behaviors, 14(1), 73–76. 10.1037/0893-164X.14.I.73 [DOI] [PubMed] [Google Scholar]
- Clay JM, Adams C, Archer P, English M, Hyde A, Stafford LD, & Parker MO (2018). Psychosocial stress increases craving for alcohol in social drinkers: Effects of risk-taking. Drug and Alcohol Dependence, 185, 192–197. 10.1016/j.drugalcdep.2017.12.021 [DOI] [PubMed] [Google Scholar]
- Cleveland HH, & Harris KS (2010). The role of coping in moderating within-day associations between negative triggers and substance use cravings: A daily diary investigation. Addictive Behaviors, 35, 60–63. 10.1016/j.addbeh.2009.08.010 [DOI] [PubMed] [Google Scholar]
- Cleveland HH, Harris KS, & Wiebe RP (2010). Substance abuse recovery in college: Community supported abstinence. Springer Science & Business Media. [Google Scholar]
- Eissenberg T (2004). Measuring the emergence of tobacco dependence: The contribution of negative reinforcement models. Addiction, 99(1), 5–29. 10.1111/j.1360-0443.2004.00735.x [DOI] [PubMed] [Google Scholar]
- Epstein DH, Willner-Reid J, Vahabzadeh M, Mezghanni M, Lin JG, & Preston K (2009). Real-time electronic diary reports of cue exposure and mood in the hours before cocaine and heroin craving and use. Archives of General Psychiatry, 66(1), 88–94. 10.1001/archgenpsychiatry.2008.509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatseas M, Serre F, Swendsen J, & Auriacombe M (2018). Effects of anxiety and mood disorders on craving and substance use among patients with substance use disorder: An ecological momentary assessment study. Drug and Alcohol Dependence, 187, 242–248. 10.1016/j.drugalcdep.2018.03.008 [DOI] [PubMed] [Google Scholar]
- First MB (2005). Structured clinical interview for DSM-IV-TR axis I disorders (Patient Edition). Biometrics Research Department, Columbia University. [Google Scholar]
- Folkman S (2008). The case for positive emotions in the stress process. Anxiety, Stress, and Coping, 21(1), 3–14. 10.1080/10615800701740457 [DOI] [PubMed] [Google Scholar]
- Furnari M, Epstein DH, Phillips KA, Jobes ML, Kowalczyk WJ, Vahabzadeh M, Lin JL, & Preston KL (2015). Some of the people, some of the time: Field evidence for associations and dissociations between stress and drug use. Psychopharmacology, 232(19), 3529–3537. [DOI] [PubMed] [Google Scholar]
- Gable SL (2006). Approach and avoidance social motives and goals. Journal of Personality, 74(1), 175–222. [DOI] [PubMed] [Google Scholar]
- Gates KM, Molenaar PCM, Hillary FG, Ram N, & Rovine MJ (2010). Automatic search for fMRI connectivity mapping: an alternative to Granger causality testing using formal equivalences among SEM path modeling, VAR, and unified SEM. NeuroImage, 50(3), 1118–1125. 10.1016/j.neuroimage.2009.12.117 [DOI] [PubMed] [Google Scholar]
- Gordon AJ, & Zrull M (1991). Social networks and recovery: One year after inpatient treatment. Journal of Substance Abuse Treatment, 8, 143–152. [DOI] [PubMed] [Google Scholar]
- Groh DR, Jason LA, Davis MI, Olson BD, & Ferrari JR (2007). Friends, family, and alcohol abuse: An examination of general and alcohol-specific social support. The American Journal on Addictions, 16, 49–55. doi: 10.1080/10550490601080084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih M-Y, Atwood AK, Johnson RA, Boyle MG, … Shah D (2014). A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiatry, 71(5), 566–572. 10.1001/jamapsychiatry.2013.4642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendershot CS, Witkiewitz K, George WH, & Marlatt GA (2011). Relapse prevention for addictive behaviors. Substance Abuse Treatment, Prevention, and Policy, 6(17), 141–157. 10.1186/1747-597X-6-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huhn AS, Harris J, Cleveland HH, Lydon DM, Stankoski D, Cleveland MJ, … Bunce SC (2016). Ecological momentary assessment of affect and craving in patients in treatment for prescription opioid dependence. Brain Research Bulletin, 123, 94–101. 10.1016/j.brainresbull.2016.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K, & Noke JN (1997). The influence of posttreatment mutual help group participation on the friendship networks of substance abuse patients. American Journal of Community Psychology, 25(1), 1–16. [DOI] [PubMed] [Google Scholar]
- Hunter-Reel D, McCrady B, & Hildebrandt T (2009). Emphasizing interpersonal factors: An extension of the Witkiewitz and Marlatt relapse model. Addiction, 104(8), 1281–1290. 10.1111/j.1360-0443.2009.02611.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Hicks RE, Levy SA, & Curran PJ (2001). Specifying the relations between affect and heavy alcohol use among young adults. Journal of Abnormal Psychology, 110(3), 449–461. https://doi.org/10.1G37//0021-843X.H0.3.449 [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, & Boeding S (2011). An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors, 25(3), 390–404. 10.1037/a0024519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadam M, Sinha A, Nimkar S, Matcheswalla Y, & De Sousa A (2017). A comparative study of factors associated with relapse in alcohol dependence and opioid dependence. Indian Journal of Psychological Medicine, 39, 627–633. 10.4103/IJPSYM.IJPSYM [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, & Slaymaker V (2013). Emerging adults’ treatment outcomes in relation to 12-step mutual-help attendance and active involvement. Drug and Alcohol Dependence, 129, 151–157. 10.1016/j.drugalcdep.2012.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, & Le Moal M (2001). Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology, 24(2), 97–129. [DOI] [PubMed] [Google Scholar]
- Li Y, Ji L, Oravecz Z, Brick TR, Hunter MD, & Chow S-M (2019). dynr.mi: An R program for multiple imputation in dynamic modeling. International Journal of Computer, Electrical, Automation, Control and Information Engineering, 13(5), 302–311. 10.5281/zenodo [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt MD, Cooney NL, & Morse P (2000). Reactivity to alcohol-related stimuli in the laboratory and in the field: Predictors of craving in treated alcoholics. Addiction, 95(6), 889–900. [DOI] [PubMed] [Google Scholar]
- Lydon-Staley DM, Cleveland HH, Huhn AS, Cleveland MJ, Harris J, Stankoski D, … Bunce SC (2017). Daily sleep quality affects drug craving, partially through indirect associations with positive affect, in patients in treatment for nonmedical use of prescription drugs. Addictive Behaviors, 65, 275–282. 10.1016/j.addbeh.2016.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machell KA, Kashdan TB, Short JL, & Nezlek JB (2015). Relationships between meaning in life, social and achievement events, and positive and negative affect in daily life. Journal of Personality, 83(3), 287–298. 10.1111/jopy.12103 [DOI] [PubMed] [Google Scholar]
- Marlatt GA, & Gordon JR (1985). Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press. [Google Scholar]
- McCrady BS, Hayaki J, Epstein EE, & Hirsch LS (2002). Testing hypothesized predictors of change in conjoint behavioral alcoholism treatment for men. Alcoholism: Clinical and Experimental Research, 26(4), 463–470. [PubMed] [Google Scholar]
- Moore TM, Seavey A, Ritter K, McNulty JK, Gordon KC, & Stuart GL (2014). Ecological momentary assessment of the effects of craving and affect on risk for relapse during substance abuse treatment. Psychology of Addictive Behaviors, 28(2), 619–624. 10.1037/a0034127 [DOI] [PubMed] [Google Scholar]
- Moos RH (2007). Theory-based active ingredients of effective treatments for substance use disorders. Drug and Alcohol Dependence, 88 (2–3), 109–121. doi: 10.1016/j.drugalcdep.2006.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naughton F, Hopewell S, Lathia N, Schalbroeck R, Brown C, Mascolo C, … Sutton S (2016). A context-sensing mobile phone app (Q Sense) for smoking cessation: A mixed-methods study. JMIR Mhealth Uhealth, 4(3). 10.2196/mhealth.5787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oravecz Z, & Brick TR (2019). Associations between slow- and fast-timescale indicators of emotional functioning. Social Psychological and Personality Science, 10(7), 864–873. 10.1177/1948550618797128 [DOI] [Google Scholar]
- Pickens RW, & Johanson CE (1992). Craving: Consensus of status and agenda for future research. Drug & Alcohol Dependence, 30, 127–131. [DOI] [PubMed] [Google Scholar]
- Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin JL, … Epstein DH (2017). Context and craving during stressful events in the daily lives of drug-dependent patients. Psychopharmacology, 234, 2631–2642. 10.1007/s00213-017-4663-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin JL, … Epstein DH (2018a). Before and after: Craving, mood, and background stress in the hours surrounding drug use and stressful events in patients with opioid-use disorder. Psychopharmacology, 235, 2713–2723. 10.1007/s00213-018-4966-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Kowalczyk WJ, Phillips KA, Jobes ML, Vahabzadeh M, Lin J-L, … Epstein DH (2018b). Exacerbated craving in the presence of stress and drug cues in drug-dependent patients. Neuropsychopharmacology, 43, 859–867. 10.1038/npp.2017.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston KL, Schroeder JR, Kowalczyk WJ, Phillips KA, Jobes ML, Dwyer M, … Epstein DH (2018). End-of-day reports of daily hassles and stress in men and women with opioid-use disorder: Relationship to momentary reports of opioid and cocaine use and stress. Drug and Alcohol Dependence, 193, 21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pritikin JN, Hunter MD, Oertzen, von T, Brick TR, & Boker SM (2017). Many-level multilevel structural equation modeling: An efficient evaluation strategy. Structural Equation Modeling: a Multidisciplinary Journal, 24(5), 684–698. doi: 10.1080/10705511.2017.1293542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Rook KS (2001). Emotional health and positive versus negative social exchanges: A daily diary analysis. Applied Developmental Science, 5(2), 86–97. 10.1207/S1532480XADS0502_4 [DOI] [Google Scholar]
- Roos CR, & Witkiewitz K (2017). A contextual model of self-regulation change mechanisms among individuals with addictive disorders. Clinical Psychology Review, 57, 117–128. 10.1016/j.cpr.2017.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg H (2009). Clinical and laboratory assessment of the subjective experience of drug craving. Clinical Psychology Review, 29, 519–34. [DOI] [PubMed] [Google Scholar]
- Ruehlman LS, & Karoly P (1991). With a little flak from my friends: Development and preliminary validation of the test of negative social exchange (TENSE). Journal of Consulting and Clinical Psychology, 3(1), 97–104. [Google Scholar]
- Scott CK, Dennis ML, & Gustafson DH (2017). Using smartphones to decrease substance use via self-monitoring and recovery support: Study protocol for a randomized control trial. Trials, 18(1), 1–11. 10.1186/s13063-017-2096-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott CK, Dennis ML, & Gustafson DH (2018). Using ecological momentary assessments to predict relapse after adult substance use treatment. Addictive Behaviors, 82, 72–78. 10.1016/j.addbeh.2018.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serre F, Fatseas M, Denis C, Swendsen J, & Auriacombe M (2018). Predictors of craving and substance use among patients with alcohol, tobacco, cannabis or opiate addictions: Commonalities and specificities across substances. Addictive Behaviors, 83, 123–129. 10.1016/j.addbeh.2018.01.041 [DOI] [PubMed] [Google Scholar]
- Serre F, Fatseas M, Swendsen J, & Auriacombe M (2015). Ecological momentary assessment in the investigation of craving and substance use in daily life: A systematic review. Drug and Alcohol Dependence, 148, 1–20. 10.1016/j.drugalcdep.2014.12.024 [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM, Oliver MNI, Bush JA, & Palmer MA (2005). An experience sampling study of associations between affect and alcohol use and problems among college students. Journal of Studies on Alcohol, 66(4), 459–469. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Juth V, Ma J, & Sliwinski M (2017). A slice of life: Ecologically valid methods for research on social relationships and health across the life span. Social and Personality Psychology Compass, 11(10), 1–10. 10.1111/spc3.12356 [DOI] [Google Scholar]
- Tiffany ST, & Conklin CA (2000). A cognitive processing model of alcohol craving and compulsive alcohol use. Addiction, 95(2), S145–S153. [DOI] [PubMed] [Google Scholar]
- Tiffany ST (1990). A cognitive model of drug urges and drug-use behavior: Role of automatic and nonautomatic processes. Psychological Review, 97, 147–168. [DOI] [PubMed] [Google Scholar]
- Tsui JI, Anderson BJ, Strong DR, & Stein MD (2014). Craving predicts opioid use in opioid-dependent patients initiating buprenorphine treatment: A longitudinal study. The American Journal of Drug and Alcohol Abuse, 40(2), 163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tukey JW (1977). Exploratory Data Analysis. Addison-Wesley, Reading, MA. [Google Scholar]
- Vinci C, Haslam A, Lam CY, Kumar S, & Wetter DW (2018). The use of ambulatory assessment in smoking cessation. Addictive Behaviors, 83, 18–24. 10.1016/j.addbeh.2018.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldrop AE, Price KL, Desantis SM, Simpson AN, Back SE, Mcrae AL, … Brady KT (2010). Community-dwelling cocaine-dependent men and women respond differently to social stressors versus cocaine cues. Psychoneuroendocrinology, 35(6), 798–806. 10.1016/j.psyneuen.2009.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Watson NL, Demarree KG, & Cohen LM (2018). Cigarette craving and stressful social interactions: The roles of state and trait social anxiety and smoking to cope. Drug and Alcohol Dependence, 185, 75–81. 10.1016/j.drugalcdep.2017.11.037 [DOI] [PubMed] [Google Scholar]
- Westerberg VS, Tonigan JS, & Miller WR (1998). Reliability of Form 90D: An instrument for quantifying drug use. Substance Abuse, 19(4), 179–189. [DOI] [PubMed] [Google Scholar]
- Williams R, Allison P, & Moral-Benito E (2016). “XTDPDML: Stata module to estimate Dynamic Panel Data Models using Maximum Likelihood,” Statistical Software Components S458210, Boston College Department of Economics, revised 07 Jul 2019. [Google Scholar]
- Witkiewitz K, & Marlatt GA (2004). Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist, 59(4), 224–235. 10.1037/0003-066X.59.4.224 [DOI] [PubMed] [Google Scholar]
- Zheng Y, Cleveland HH, Molenaar PCM, & Harris KS (2015). An alternative framework to investigating and understanding intraindividual processes in substance abuse recovery: An idiographic approach and demonstration. Evaluation Review, 39(2), 229–254. [DOI] [PubMed] [Google Scholar]