Abstract
Objectives:
Caregiving within a spousal partnership marks a novel relationship stage for couples. Caregiving introduces new stressors and affects couples’ ability to cope, and potentially alters perceptions of emotional support. Prior research on older married couples illustrates how perceived support not only affects an individual’s mental health, but also that of their partner. To date, the dyadic relationship between emotional support and mental health is largely unexamined among caregiving partners, where support expectations may differ.
Method:
Actor partner interdependence models using linear mixed modeling were applied to data from spouses where one partner received caregiving within the 2014 and 2016 waves of the Health and Retirement Study. We examined the cross-sectional and lagged associations between perceived emotional support and strain from a spouse on actor and partner depression scores, as well as whether one was the caregiver or the care recipient moderated associations.
Results:
More positive perceptions of support were associated with lower depression scores for oneself (b=−0.55, p-value<0.001) and one’s partner (b= −0.24, p-value<0.001). Actor effects—how one’s own perceptions of support associate with one’s own depressive symptomology—were stronger for care recipients than for caregivers (b=−0.83, p-value<0.001 v. b=−0.26, p-value<0.05). Higher perceptions of strain were also associated with higher depression scores for oneself (b=0.57, p-value<0.001) and one’s partner (b=0.39 p- value<0.001), associations that remained even in lagged models.
Conclusion.
The observation of both actor and partner effects in this study suggests opportunities to improve care recipient outcomes through intervention with caregivers or both members of the care dyad.
Keywords: caregiving, depression, social support
Introduction
In the U.S., there are 3.7 million family caregivers who provide assistance to a spouse or partner living with an illness or disability (Schulz et al., 2016). Among spouses (also referred to as partners or couples), caregiving can represent a novel relationship stage, as couples adapt to new roles and realities wrought by disease processes (Knobloch, Nichols, & Martindale-Adams, 2019). As a primary source of emotional support, spousal partners may serve as either/both a resource or threat in relation to one’s own mental health (Rook, 2015). Disappointed expectations of emotional support may diminish one’s mental health, while high levels of perceived emotional support may bolster it (Lawrence et al., 2008; Uchino, 2006). How each spouse perceives emotional support received from their partner is inter-related with their partner’s perceptions; that is, each spouse is likely to affect the other’s perceptions of emotional support (Carr, Cornman, & Freedman, 2016). In order to better understand how emotional support affects the mental health of spouses in a caregiving partnership, we apply actor partner interdependence models to dyadic data from the Health and Retirement Study (Cook & Kenny, 2010; Health and Retirement Study, 2017). Findings from this research will inform development of interventions to support the mental health of caregiving partners, who disproportionately experience poor mental health relative to non-caregivers (Riffin, Van Ness, Wolff, & Fried, 2017).
Caregiving introduces novel relationship stressors and may upend couple’s coping
Onset of caregiving among spouses is marked by the introduction of novel stressors and, in some cases, exacerbation of pre-existing relationship tensions. Couples must renegotiate social roles: caregiving spouses may assume additional responsibilities within the household in addition to caregiving, whilst care recipients may experience distress from loss of autonomy (Anderson & Keating, 2018; Carr, Cornman, & Freedman, 2017; Roberto, McCann, & Blieszner, 2011). Disagreement over the appropriate balance between supporting the care recipients’ independence and promoting safety can also become a source of conflict throughout the caregiving trajectory. Caregivers, for example, may believe that the care recipient can perform certain tasks more independently than they do, while care recipients may feel their independence is being unnecessarily curbed by their spouses (Avent, Rath, Meyer, Benton, & Nash, 2019). A recent application of relational turbulence theory to adult caregiving describes how transitioning into a caregiving relationship can lead to uncertainty, biased appraisals by care partners, and result in relationship discord (Knobloch et al., 2019). Further, coping processes that could otherwise allow partners to handle stressors may also be upended with caregiving, such as when caregivers conceal from care recipients stressors such as witnessing their partner suffer, resentment about the loss of social opportunities due to caregiving responsibilities, anticipated loss of a partner in cases of terminal disease, and loss of intimate desire (Anderson & Keating, 2018; JK Monin & Schulz, 2009). Breakdown in dyadic coping contributes to mental health morbidity, including depression, within caregiving partners (Perndorfer, Soriano, Siegel, & Laurenceau, 2019).
Spousal relationship quality is closely linked to partners’ health outcomes
Support from a partner is an important contributor to individuals’ physical and mental health and wellbeing (Birditt, Newton, Cranford, & Ryan, 2016; Whisman, Robustelli, & Labrecque, 2018). In a daily diary study, caregivers who felt that care recipient spouses appreciated the emotional support they gave, reported fewer negative physical symptoms (e.g., lack of energy) (J Monin, Poulin, Stephanie, & Langa, 2017). The relevance of social support from a spouse on one’s own health may be particularly salient among older adults, whose shortened time horizons contribute to a tendency to value close social relationships, as described within socio-emotional selectivity theory (Carstensen, Fung, & Charles, 2003). In a study of spouses drawn from a population survey data, Umberson, Williams, Powers, Liu, and Needham (2006) found that marital discord had more harmful effects on the health trajectory of older adults compared to effects found in younger cohorts.
Spousal partners relationships perceptions may affect each other’s health outcomes
It is increasingly recognized that one’s own health outcomes may be affected by a partner’s experiences, rather than one’s own experiences alone, and thus data from both partners should be incorporated into analyses to understand dyadic effects (Cook & Kenny, 2010). Actor partner interdependence modeling (APIMs) allow for simultaneous analysis of data from both members of a dyad, including actor and partner effects. Actor effects refer to the effects of an individual’s scores on their own outcomes. Partner effects refer to the effects of an individual’s score on outcomes for the other member of the dyad.
Using dyadic methods like APIMs, researchers are finding that partner perceptions of support and strain may not only affect one’s own health, but also that of one’s partner. In a survey study of couples ages 50 and older, Carr, Freedman, Cornman, and Schwarz (2014) found an association between perceived partner support and one’s own positive affect and global life satisfaction, though these effects did not extend to one’s partner outcomes in this initial study. Later research by these authors, however, uncovered partner effects and identified gender differences: whereas husbands’ reports of relationship strain were associated with wives’ frustration, wives’ reports of receiving greater marital support from their husbands were associated with increased frustration among husbands (Carr et al., 2016). Microlongitudinal studies also demonstrate actor and partner effects. In their experience sampling study, Michalowski, Hoppmann, and Gerstorf (2016) discovered an association between higher spousal support and lower levels of negative affect for both oneself and one’s partner.
It is also plausible that depression lends itself to increased perceptions of strain and lower support within couples, such as when depressive symptoms elicit negative reactions from others, as described in Coyne’s interpersonal theory of depression (Coyne, 1976). Previous longitudinal studies with older couples suggest that, although perceptions of support and strain do precede depression, depression may also precede perceptions of relationship strain. In a secondary analysis of the English Longitudinal Study of Aging, Whisman and Uebelacker (2009) found that older adults’ (at least 50 years old) own perceptions of marital discord were associated with depression symptomology two years later, and that individuals’ depressive symptomology associated with their future perceptions of marital discord. In addition to this bi-directional actor effect, the authors also discovered a partner effect, such that individuals’ depressive symptomology also associated with their partners’ perceptions of relationship discord two years later. Later these authors conducted a similar analysis using the The Irish Longitudinal Study on Ageing (Whisman et al., 2018). Again, the authors discovered actor effects for marital discord and future depressive symptoms, but no partner effects in couples. Cumulatively, these findings indicate a need to account for time-ordering of depression and perceptions of strain and support within partnerships.
While there have been multiple studies examining how perceptions of support and strain affect depression among older couples, dyadic effects of partner support on mental health remain underexplored among older couples where one partner requires care from the other, even while the context in which support is exchanged among caregiving spouses is different from that of non-caregiving spouses (Braun et al., 2009; Gellert et al., 2018). For example, some caregivers expect less support from their partner while their partner experiences illness (Anderson & Keating, 2018; Quinn, Clare, & Woods, 2009). We are unaware of any prior studies that examine the dyadic effects of partner support and strain, specifically on depression within an older adult caregiving population. Given evolving care needs, renegotiation of social roles, and alteration of coping techniques during caregiving, perceptions of support among spousal care partners and how perceived support affects depressive outcomes may differ within care partners as compared to non-caregiving couples and merits further study.
To address the lack of dyadic research about how perceived support from one’s spouse affects experiences of depression for individuals and their care partners, we apply actor partner interdependence models to data from the Health and Retirement Study (HRS). We focus our analysis on depression given the clinical relevance of this outcome within care dyads and its association with low-levels of social support (Cornwell & Waite, 2009; Uchino, 2006). Depression is one of the most common health outcomes associated with caregiving (Capistrant, Moon, Berkman, & Glymour, 2012), such that 13% of caregivers report depression at any given time (Riffin et al., 2017). In the general population, prevalence of depression is 8.1% among adults (Brody, Pratt, & Hughes, 2018). Similarly, physical disability, chronic disease, and frailty among older adults who require care are associated with greater incidence and severity of depression (Lohman, Dumenci, & Mezuk, 2014).
We use a modified version of the Stress Process Model to conceptualize how perceptions of social support within spousal care partnerships affect an outcome of depression in both partners. The Stress Process Model is frequently employed to examine the effects of primary and secondary stressors of negative caregiver outcomes (Pearlin, Mullan, Semple, & Skaff, 1990). According to this model, contextual factors interact with primary and secondary stressors, which accumulate and affect outcomes, such as depression. Coping and social support may modify this trajectory. Some researchers have called for greater integration of aspects of the care relationships, as a stressor and a resource, within the Stress Process Model (Quinn et al., 2009; S. Zarit & Edwards, 2008). As such, we hypothesize that higher levels of perceived negative support—a stressor—will be associated with higher levels of depression in both the actor (i.e., the perceiver) and their partner, and that the association between positive support on depression—a stress buffer— will be inverse for both actors and partners. To better understand how actor and partner effects vary between caregivers and recipients, we also explore caregiver compared to care recipient status as a moderator, but do not make any hypotheses about the directionality of the moderating effects. Further, we examine lagged models, wherein we control for prior depression so as to account for the possibility of a bidirectional relationship between social support with depression among caregiving couples.
Methods
Data
We used data from the 2014 and 2016 waves of the Health and Retirement Study (HRS). The HRS is a publicly available panel dataset of older adults ages 51 and older in the U.S. and is regularly replenished with younger cohorts. Survey data about health and financial wellbeing are collected from participants, their spouses, and household members every two years. For additional information about the HRS study, see Fisher and Ryan (2018). In addition to core HRS modules, every 4 years a randomly selected subsample including one-half of participants receive a module asking about psychosocial wellbeing and lifestyle, also called the “Leave Behind” survey. Smith, Ryan, Sonnega, and Weir (2017) and colleagues provide additional information about administration of the Leave Behind module. As the Leave Behind survey is administered to mutually exclusive samples, we followed Wang, Kim, and Boerner (2018) and merged data from participants from the 2014 and 2016 waves. To learn about the relationship between social support and caregiver and recipient depression, we used data from the Leave Behind and “Helper” HRS modules. The Helper module asks about participants’ need for assistance with functional tasks, who assists them, and other aspects of caregiving. This study used data exclusively from spousal caregivers, as spouses tend to be the first choice of caregivers among older adults needing care and because caregiving uniquely affects spousal care relationships (Pinquart & Sorensen, 2011). Non-caregivers were excluded from the sample. Data was merged with the 2016 RAND Fat File, a user-friendly datafile that includes demographic and health data from all participants for each wave. Once files were merged, the sample included 2,459 individuals. We excluded dyads where: both partners received care (n=158) (i.e., partners were not distinguishable by caregiving status, and thus moderation analyses could not be completed), there were multiple care dyads within a household (n=4), partners did not participate (n=71), and those cases with any missing predictor variables (n=1,022), and cases where partner was not included in the sample following listwise deletion of missing predictor variables (n=286). Listwise deletion of predictors ensured that sample sizes did not vary between models, in contrast to pairwise deletion. These exclusions resulted in a final analytic sample of N=918.
Measures
Dependent variable
Depressive symptomology was measured using the 8-item Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977). Participants were asked to affirm (1) or negate (0) 8 different statements that described their experiences during the previous week (e.g., “You felt lonely.”). Two items indicating non-depressive symptoms were reverse coded (e.g., “You felt happy.”). Scores from this measure were summed. The CES-D 8 demonstrates high internal consistency (alpha=0.84) and nomological validity when administered among older adult samples (Karim, Weisz, Bibi, & ur Rehman, 2014). A lagged variable was also generated using CES-D 8 depression scores from two years prior for both care partners.
Independent variables
Positive and negative perceived support were measured using items based on those from Schuster, Kessler, and Aseltine (1990) and Walen and Lachman (2000). These measures demonstrate high reliability when used to describe social support from a spouse (alpha=0.86 for positive support and alpha=0.81 for negative support) (Walen & Lachman, 2000). Participants are asked 3 items pertaining to positive support from a partner including: (a) “How much do they really understand the way you feel about things?”, (b) “How much can you rely on them if you have a serious problem?”, and (c) “How much can you open up to them if you need to talk about your worries?”. Questions to assess negative support, also called strain, included: (d) “How often do they make too many demands on you?”, (e) “How much do they criticize you?”, (f) “How much do they let you down when you are counting on them?”, and (g) “How much do they get on your nerves?” Response options include “A lot” (1), “Some” (2), “A little” (3), and “Not at all” (4). Following HRS recommendations, items were reverse coded and the average for negative and positive support components were computed to create positive and negative support index scores (Smith et al., 2017).
Covariates
Individual variables.
Models included demographic covariates for each partner and characteristics that applied to both partners. Each participant could report male or female gender, as prior studies describe gender differences in the strength of associations between support and strain with depression (Carr et al., 2016; Whisman et al., 2018). We only included actor gender (i.e., an individual’s gender rather than their partner’s) in analytic models given that all couples were heterosexual, and thus inclusion of partner gender would create a redundant parameter. All other covariates were included for both actors and partners. Age was included in models as older adults may experience more adverse effects when close social relationships become strained (Umberson et al., 2006). Age was calculated by subtracting the participant’s year of birth from the year when the participant completed the leave behind survey. Prior studies reveal cultural differences in the strength of associations between support and depression within spouses (Salinger, Whisman, Randall, & Hilpert, 2020). As such, race and ethnicity were included to partially account for possible cultural differences within this U.S. sample. Race was coded as either non-white or white. Ethnicity for each partner was recorded as Hispanic or non-Hispanic. We followed prior researchers in including education as a covariate in our models (Carr et al., 2016; Umberson et al., 2006) since, as a proxy of socioeconomic status, lower educational attainment may represent an environmental stressor contributing to both depressive symptoms and relationship strain. Years of education was a continuous variable and ranged from 0 (none) to 17 (graduate school). We controlled for the number of chronic conditions experienced by each partner given that chronic illness may alter expectations of support within couples (Anderson & Keating, 2018). This variable was generated by summing affirmative responses to ever experiencing any of the following serious health conditions: stroke, diabetes, cancer, lung disease, heart disease.
Dyad variables.
We also included dyad-level covariates in models. We controlled for the length of marriage in years and whether or not the couple had children. We included relationship length since the association between perceived support and depression within marriage may change over time (Brock & Lawrence, 2011). Further, couples with children may have had an alternative source of support if relationships with spouses became strained. Covariates for different kinds of caregiving intensity were also accounted for at the dyad level, since care stressors serve as possible source of strain within partnerships and differentially associated with support needs (e.g., reassurance). A binomial variable for intensity of care was generated based on the 2016 National Academies’ report, Caring for an Aging America, such that high intensity care meant providing assistance with 2 or more activities of daily living (Schulz et al., 2016). This variable was coded at the dyad level because care intensity dually reflected care recipient functional ability as well as the intensity of care provided by caregivers. Whether the recipient of care ever experienced a stroke, diabetes, cancer, lung disease, heart disease, or lived with dementia were each included in models as binomial covariates to control for additional aspects of care intensity that increase the extent of complex care tasks undertaken by family members (Lee, Ryoo, Campbell, Hollen, & Williams, 2019).
Analyses
We employed actor-partner interdependence models using multi-level modeling to detect actor and partner effects of perceived spousal support on depressive symptomology (Cook & Kenny, 2010; Kenny, Kashy, & Cook, 2006). We also tested caregiver status as a moderating factor for actor and partner effects. By testing caregiver versus care recipient status as a moderator, we could determine whether the strength of actor and partner effects varied according to whether someone was a caregiver or care recipient. A second set of models was also run with the lagged variable for depression in case the relationship between strain and support with depression was bi-directional.
To begin this analysis, data were restructured to a pairwise dataset after merging modules from the HRS public data files. After restructuring data, we reviewed descriptive and bivariate analyses to compare caregivers and recipients on demographic characteristics, perceived support from their partner, and depression. Continuous variables were grand mean centered (depression, negative and positive social support, age, years of education, number of conditions, length of the relationship) and standardized. We report two sets of coefficients in results tables: one set from models that used grand mean centered variables and the other using standardized coefficients. Results reported in the text use estimates derived from models that used grand mean binomial variables and were effects coded. Two separate correlation matrices that included 1) positive support and 2) negative support were evaluated to detect correlations above r=0.90 indicating potential multicollinearity. Next, we applied a chi-squared difference test with maximum likelihood (ML) estimation to test caregiver status as a distinguishing variable for models of negative and positive support. We evaluated actor and partner effects while including caregiver status as a moderator of actor and partner effect sizes. Linear mixed models were run using restricted maximum likelihood estimation (REML) using compound heterogeneous symmetry (CHS) to structure residuals. We used a product interaction term to evaluate caregiver status as a moderator in these models. An interaction model was used to detect significant actor and partner effects, as well as whether moderator terms were significant. In addition to the interaction model, we applied a two-intercept model to observe the extent to which effect sizes varied according to caregiver status. Linear mixed models with the product interaction terms were re-run while including the lagged depression variable. Pseudo-R2 statistics for actor and partner effects according to caregiver status were generated by again using nested ML models—one set that include actor and partner effects and a null model without these effects. We subtracted the ratio of error variance from the full and null models from 1 to derive a pseudo-R2 statistic. Finally, we applied a chi-squared deviance tests with nested models to determine whether the inclusion of actor and partner effects significantly improved models. All analyses were conducted in SPSS 16.1.
Results
Sample characteristics
The analytic sample included N=918 participants comprised of 459 caregivers and 459 care recipients. Caregivers were more likely than care recipients to be women (60% vs. 40%). There were no notable differences between caregivers and recipients in terms of race or ethnicity. Eighty-two percent of the sample was white/Caucasian and 13% of the sample was Hispanic. On average, participants had 12 years of education. Caregivers were slightly more educated than care recipients (M=13 years vs. M=12 years respectively). Caregiving couples had been married for an average of 41 years and 96% had children. Thirty-four percent of care recipients received assistance with at least 2 ADLs. Care recipients were slightly older than caregivers (72 vs. 71 years-old respectively). They had an average of 1.45 chronic conditions, whereas caregivers had approximately 1.19 conditions. Care recipients also reported higher levels of depressive symptomology than caregivers (M=2.18 vs. M=1.10, respectively). Levels of depressive symptoms were lower two years earlier in caregivers and recipients of care, though recipients of care still reported higher depressive symptomology than caregivers (M=1.85 vs. M=1.10 respectively). Care recipients perceived their partners as being more supportive than caregivers did (M=3.56 v. M=3.41 respectively). There was no difference in perceptions of negative support between recipients of care and caregivers (M=1.95 vs. M=2.02, respectively). Additional sample characteristics are shown in Table 1.
Table 1.
Descriptive and bivariate information about caregivers and care recipients
| Variable | Full Sample | Caregiver | Care recipient | X2/ |
|---|---|---|---|---|
| Age (mean/SD) | 71.37(10.71) | 70.54(10.74) | 72.20(10.62) | −2.36 |
| Female | 459(50.00% | 275(59.91) | 184(40.09) | 36.08*** |
| Non-white race | 167(18.19) | 79(17.21) | 88(19.17) | 0.59 |
| Hispanic | 119(12.96) | 58(12.64) | 61(13.29) | 0.09 |
| Years of education (mean/SD) | 12.35(3.14) | 12.66(2.92) | 12.05(3.33) | 2.93 |
| Relationships length (mean/SD) | 40.70(17.62) | N/A | N/A | N/A |
| CR living with 2 or more ADLs | 312(33.99) | N/A | N/A | N/A |
| Children | 882(96.08) | N/A | N/A | N/A |
| Caring for someone with dementia | 84(9.15) | N/A | N/A | N/A |
| Care recipient conditions | ||||
| Care recipient stroke, ever | 162(17.65) | N/A | N/A | N/A |
| Care recipient diabetes, ever | 342(37.25) | N/A | N/A | N/A |
| Care recipient cancer, ever | 240(26.14) | N/A | N/A | N/A |
| Care recipient lung condition, ever | 184(20.04) | N/A | N/A | N/A |
| Care recipient heart condition, ever | 406(44.23) | N/A | N/A | N/A |
| Number of conditions (mean/SD) | 1.19(1.08) | 0.92(0.92) | 1.45(1.16) | −7.69*** |
| Depression (mean/SD) | 1.64(2.02) | 1.10(1.72) | 2.18(2.16) | −8.34*** |
| Depression two years prior | 1.46(1.93) | 1.06(1.66) | 1.85(2.09) | −6.28*** |
| Positive perceived social support (mean/SD), (1 to 3) | 3.49(0.62) | 3.41(0.67) | 3.56(0.55) | −3.70*** |
| Negative perceived social support (mean/SD), (1 to 4) | 1.99(0.68) | 2.02(0.68) | 1.95(0.68) | 1.50 |
p<0.05;
0.01;
0.001
Testing Distinguishability and Correlations
Examination of Pearson correlations did not indicate any variables to be correlated above r=0.90. The variables with the highest correlation were actor and partner ethnicity (r=0.87, p<0.01). After running nested models with and without caregiver status, we found that caregiver status was a statistically meaningful distinguishing characteristic both when modeling perceived positive support (χ2(4) = 103.94, p-value < 0.001) and perceived negative support from a partner (χ2(4) = 95.43, p-value< 0.001). As such, we ran distinguishable models so that dyad members would be treated differently according to whether they were a caregiver or care recipient.
Actor and partner effects for perceived positive support from a partner on depression
Even after controlling for covariates, caregivers experienced less depressive symptomology than did care recipients (b=−0.58, p-value<0.001). Application of the interaction model to data revealed both a significant actor effect (b= −0.55, p-value<0.001) and partner effect (b= −0.24, p-value<0.05), where high levels of positive perceived support from a partner were associated with lower levels of depression. Further, caregiver status demonstrated a significant moderating effect with perceived positive support on actor’s depression. (See Table 2.) A two-intercept model was used to determine the difference in effect size according to whether one was the caregiver or the care recipient. This model showed that the effect size of perceived positive support on an actor’s depression was stronger for care recipients than for caregivers (b=−0.83, p<0.001 vs. b=−0.26, p-value<0.05). (See Table 3.) That is, if care recipients perceived their partner to be more supportive, it had a stronger negative association (positive outcome) with their own depression than was the case for caregivers. A deviance tested derived from nested models demonstrated that actor and partner effects from caregiver status were statistically significant (χ2(4) =39.87, p-value< .001). For care recipients, we obtained a pseudo-R2 of 0.08, while for caregivers we found a pseudo-R2 of just 0.01. This indicates that actor and partner effects of perceived positive support explained considerably more variance in depression for care recipients than for caregivers. Figure 1 illustrates actor and partner effects according to caregiver status. Results from the lagged model that controlled for depression two years prior differed somewhat from the cross-sectional model: while actor effects remained (b=−0.06, p<0.05), partner effects were wiped out. There was no moderating effect for actor effects according to caregiver status in the lagged model.
Table 2.
Multilevel regression coefficients estimating actor and partner effects of positive perceived support on depression
| b | β | t(df) | |
|---|---|---|---|
| Intercept | 0.09 | 0.04 | 0.24(445.20) |
| Caregiver | −0.58 | −0.29 | −9.40***(451.49) |
| Actor perceived positive support | −0.55 | −0.17 | −5.15***(802.13) |
| Partner perceived positive support | −0.24 | −0.07 | −2.33*(879.77) |
| Caregiver*Actor perceived positive support | 0.29 | 0.09 | 2.71**(723.61) |
| Caregiver*Partner perceived positive support | 0.12 | 0.04 | 1.15(790.30) |
| Age (actor) | −0.01 | −0.07 | −1.27(675.38) |
| Age(partner) | −0.02 | −0.09 | −1.62(648.24) |
| Female (actor) | 0.23 | 0.11 | 3.42**(449.12) |
| Non-white race (actor) | 0.12 | 0.06 | 0.55(649.87) |
| Non-white race (partner) | 0.01 | 0.01 | 0.06(640.08) |
| Hispanic (actor) | 0.20 | 0.10 | 1.12(566.72) |
| Hispanic (partner) | −0.12 | −0.06 | −0.68(552.42) |
| Years of education (actor) | 0.01 | 0.01 | 0.24(784.41) |
| Years of education (partner) | −0.06 | −0.09 | −2.37*(730.41) |
| Relationships length (mean/SD) | −0.01 | −0.05 | −1.07(472.46) |
| Children | −0.15 | −0.07 | −0.46(442.05) |
| Living with 2 or more ADLs | 0.42 | 0.21 | 3.01**(441.90) |
| Caring for someone living with dementia | 0.15 | 0.07 | 0.68(442.39) |
| Number of conditions (actor) | 0.25 | 0.13 | 3.23**(548.52) |
| Number of conditions (partner) | 0.12 | 0.06 | 1.37(607.81) |
| Care recipient stroke, ever | 0.15 | 0.08 | 0.82(446.52) |
| Care recipient diabetes, ever | 0.06 | 0.03 | 0.40(447.45) |
| Care recipient cancer, ever | −0.25 | −0.12 | −1.53(447.56) |
| Care recipient lung condition, ever | 0.07 | 0.04 | 0.4(447.00) |
| Care recipient heart condition, ever | −0.12 | −0.06 | −0.78(447.79) |
p<0.05;
0.01;
0.001
Table 3.
Simple slope regression coefficients estimating separate positive perceived support actor and partner effects for caregivers and recipients on depression
| b | β | t(df) | |
|---|---|---|---|
| Intercepts | |||
| Caregiver | −0.50 | −0.24 | −1.33(456.38) |
| Care recipient | 0.67 | 0.33 | 1.78(479.83) |
| Actor’s perceived spouse support | |||
| Caregiver | −0.26 | −0.08 | −2.11*(452.99) |
| Care recipient | −0.83 | −0.25 | −4.81***(451.53) |
| Partner’s perceived spouse support | |||
| Caregiver | −0.12 | −0.04 | −0.82(450.79) |
| Care recipient | −0.36 | −0.11 | −2.48*(456.26) |
p<0.05;
0.01;
0.001
The table has been abridged such that covariates not shown.
Figure 1:
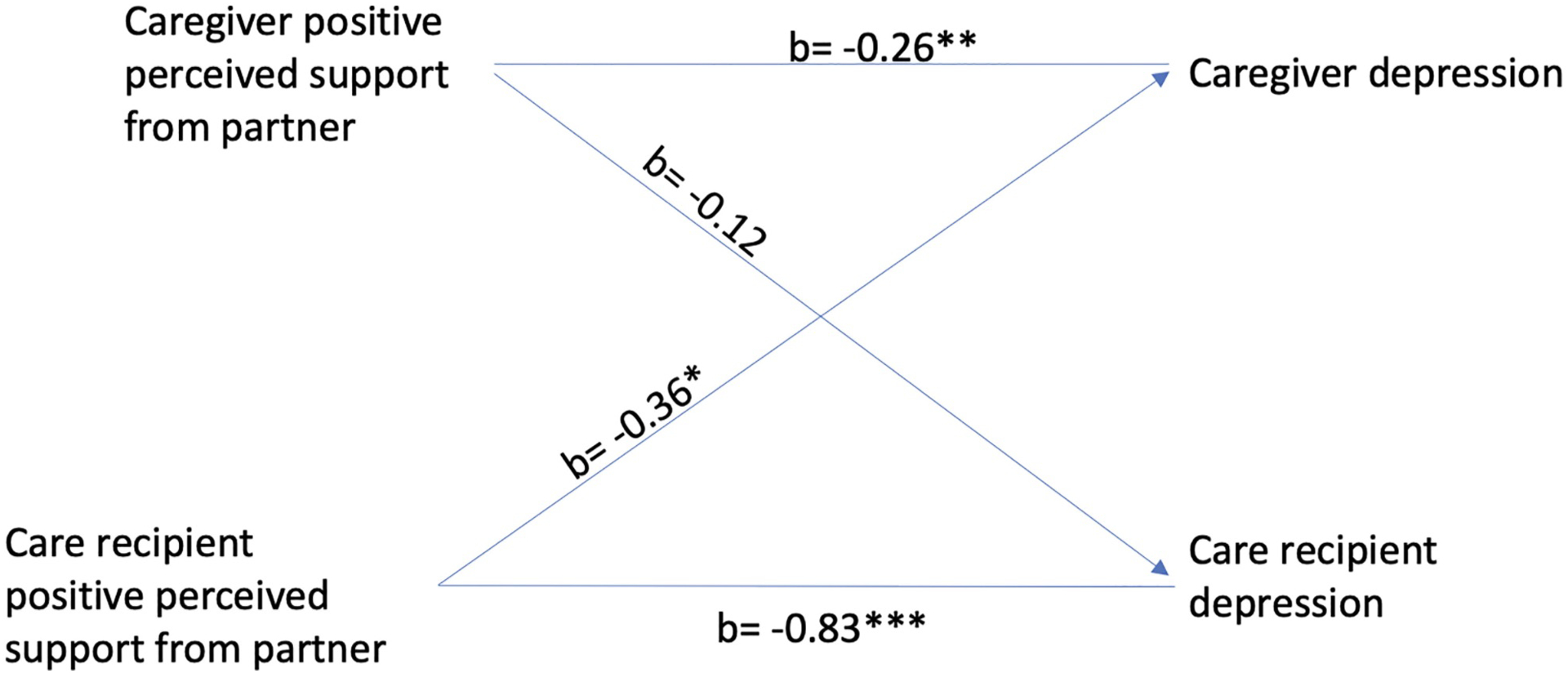
An illustration of actor and partner effects for perceived positive support on depression according to caregiver status
Actor and partner effects for perceived negative support from a partner on depression
Findings were different when depression was regressed on perceived negative support from one’s partner. Application of the interaction model revealed significant actor (b=0.57, p-value<0.001) and partner (b=0.39 p-value<0.001) effects, such that greater perceived negative support was associated with higher levels of depression both for oneself and one’s partner. (See Table 4.) However, in this model, caregiver status was not a significant moderator of either actor or partner effects. A deviance test revealed actor and partner effects significantly improved model fit (χ2(4) = 71.85, p-value< .001). The pseudo-R2 for actor and partner effects for caregivers was 0.06 compared with 0.10 for care recipients with this model. Once again, this suggests actor and partner effects of perceived support explained greater variance in depressive symptomology for care recipients than for caregivers. Actor and partner effects remained in the lagged model, but were weakened (b=0.09, p<0.001 v. b=0.08, p-value<0.01, respectively). We observed no moderating effects by caregiver status in the lagged model.
Table 4.
Multilevel regression coefficients estimating actor and partner effects of negative perceived support on depression
| b | β | t(df) | |
|---|---|---|---|
| Intercept | −0.01 | −0.01 | −0.03(445.52) |
| Caregiver | −0.57 | −0.28 | −9.16***(451.83) |
| Actor perceived negative support | 0.57 | 0.19 | 6.24***(823.13) |
| Partner perceived negative support | 0.39 | 0.13 | 4.25***(819.37) |
| Caregiver*Actor perceived negative support | −0.08 | −0.03 | −0.81(752.83) |
| Caregiver*Partner perceived negative support | −0.10 | −0.03 | −1.06(749.07) |
| Age (actor) | −0.01 | −0.06 | −1.18(655.70) |
| Age(partner) | −0.01 | −0.06 | −1.03(630.78) |
| Female (actor) | 0.23 | 0.11 | 3.44*(449.13) |
| Non-white race (actor) | 0.16 | 0.08 | 0.76(629.46) |
| Non-white race (partner) | 0.07 | 0.03 | 0.32(619.72) |
| Hispanic (actor) | 0.18 | 0.09 | 1.03(555.25) |
| Hispanic (partner) | −0.14 | −0.07 | −0.77(541.00) |
| Years of education (actor) | 0.01 | 0.01 | 0.34(762.37) |
| Years of education (partner) | −0.06 | −0.09 | −2.56*(704.56) |
| Relationships length (mean/SD) | −0.01 | −0.07 | −1.75(469.36) |
| Children | −0.15 | −0.07 | −0.48(441.89) |
| Living with 2 or more ADLs | 0.48 | 0.24 | 3.66***(441.77) |
| Caring for someone living with dementia | 0.22 | 0.12 | 1.04(442.32) |
| Number of conditions (actor) | 0.24 | 0.13 | 3.156**(558.28) |
| Number of conditions (partner) | 0.10 | 0.05 | 1.17*(618.76) |
| Care recipient stroke, ever | 0.11 | 0.05 | 0.61(446.97) |
| Care recipient diabetes, ever | 0.09 | 0.04 | 0.58(448.02) |
| Care recipient cancer, ever | −0.19 | −0.09 | −1.23(448.18) |
| Care recipient lung condition, ever | 0.16 | 0.08 | 0.95(447.51) |
| Care recipient heart condition, ever | −0.16 | −0.08 | −1.11(448.41) |
Discussion
We used actor partner interdependence models to test associations between perceived support from a partner and depression in spousal caregiving dyads. Both positive and negative perceived support were associated with depressive symptomology in the hypothesized directions: greater positive perceived support from a partner was associated with lower levels of depression, whereas greater negative perceived support from a partner was associated with higher levels of depression. Effects were in the same direction for both actor and partner effects, although partner effects were of lower magnitude compared to actor effects, consistent with previous research (Cook & Kenny, 2010). We also explored the effects of caregiver status as a moderator of actor and partner effects. Positive perceived support had a stronger negative association with one’s own depression for care recipients than for caregivers. No moderating effects were found for negative perceived support according to caregiver status. Results were generally consistent when we examined lagged variables, although observed associations were weakened and partner effects were eliminated in the model of positive support on depression.
This is the first study of which we are aware where the dyadic effects of perceived partner support on mental health were observed in a sample of spousal care partners. Our findings contrast with some prior findings among non-care partners, where actor effects but not partner effects have been generally observed (Carr et al., 2014; Whisman & Uebelacker, 2009), although this is not consistent across studies (Carr et al., 2016; Whisman et al., 2018). Observed partner effects for perceived strain lend support to the relationship turbulence theory within caregiving, wherein individual’s uncertainty is posited to contribute to interpersonal challenges, such as disrupted communication and undermined dyadic coping, and, in turn, harms partner mental health (Knobloch et al., 2019). Future research should examine whether partner effects for strain and depression remain after several years of caregiving, since couples may learn to better cope with evolving roles to prevent depressive outcomes over time. We also found support for our hypothesis that social support would protect against depression for both care partners, as anticipated according to the stress process model (Pearlin et al., 1990).
The strong moderating effect of caregiver status on the association between social support and depression is noteworthy. One reason for the stronger association between more positive perceived support with lower depression for care recipients than caregivers may be that care recipients had higher levels of depressive symptomology to begin with, such that there was greater variance that could be explained by analytic models. Alternatively, care recipients may be more invested in their relationships than caregivers; this is supported by the higher pseudo-R2 we observed for care recipients in both models. According to socio-emotional selectivity theory, perceived proximity to death affects behaviour such that individuals attempt to increase positive emotional experiences, including spending more time with close friends and family (Carstensen et al., 2003). Care recipients were older and had more chronic conditions than caregivers in our study, and thus may have had shortened time horizons that caused them to value positive support from a partner to a greater degree than did caregivers. Related, the positivity effect suggests older individuals more readily perceive positive compared to negative information (Charles & Carstensen, 2008). Care recipients in this study perceived more positive and less negative support than caregivers, suggesting a possible positivity effect among care recipients when considering their relationships. This is consistent with prior research where care recipients report higher satisfaction with their relationships than caregivers (Clare et al., 2012). In contrast, caregivers may have engaged in emotional distancing to protect themselves from being negatively affected by recipient’s poor health. Previous research demonstrates that witnessing a partner suffer induces high blood pressure and heart rate within spousal caregivers (J. K. Monin et al., 2010). As such, perceived support from a partner may have less impact on caregiver depression relative to other factors.
Limitations
This study has several limitations. First, the variables selected for social support, do no account for spouse’s preferences for support provision. Preference for support is an importance consideration since prior research has found that support preferences differentially associate with marital satisfaction as compared to amount of support, for example (Lawrence et al., 2008). Measures of social support accounting for over- and under-provision may be particularly relevant in caregiving scenarios, where over-provision of support for care recipients may lower self-efficacy given already limited functional abilities, and is known to be associated with depression in older adults (Carr et al., 2017; Miller et al., 2019). Secondly, in this study we examined differences in effect magnitude according to caregiver compared to care recipient status. Prior studies on spousal partnerships have studied the magnitude of effects for husbands compared to wives, and uncovered gender differences in how perceived support associates with depression. For example, Whisman et al. (2018) found a stronger longitudinal association between marital discord and depression for husbands than in wives. Future studies should consider not only caregiver and care recipient status as a modifier of effects, but also the gender of care partners. Finally, our analysis is subject to missing data bias given high missing information for predictor variables pertaining to social support, and thus parameter estimates may be biased and generalizability weakened. Missing data bias from listwise deletion of cases with missing predictors is a recognized limitation of APIM modeling using MLMs (Ledermann & Kenny, 2017). At the same time, these biases are not beyond those we would expect from primary data studies reporting on convenience samples that characterize the majority of dyadic research.
Implications and Conclusion
Our findings have implications for caregiver intervention. Although there are hundreds of caregiver interventions, few have demonstrated improvement in care recipient outcomes (Griffin et al., 2015). The persistent actor effects we observed for perceptions of support on depression among care recipients suggests that interventions that promote positive perceptions of support from caregivers may be particularly beneficial. For example, interventions which encourage caregivers to promote supportive interactions through communication skills (e.g., active listening) or wherein care recipients are counseled on identifying positive aspects of an altered spousal relationship (e.g., cognitive reframing). Given the observation of partner effects for relationship strain, we also recommend dyadic interventions with both caregivers and recipients to reduce perceptions of strain within relationships, such as family counseling and group-based support inclusive of both partners (Peluso, Watts, & Parsons, 2013; S. H. Zarit, Femia, Watson, Rice-Oeschger, & Kakos, 2004). Further research is needed to isolate intervention targets (e.g., timing with regards to when changes in social support occur within care partners) and to further examine of long-term changes in support as care partners cope with care challenges.
Acknowledgements:
This study employs a secondary analysis of the Health and Retirement Study (HRS). Data files and documentation are for public use and available at http://hrs.isr.umich.edu. The HRS is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan. This study was not pre-registered. Information regarding analyses are available upon request.
Funding: The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant TL1 TR002647. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Declaration of interest statement: The authors have no conflicts of interest to declare.
References
- Anderson S, & Keating N (2018). Marriage after the transition to stroke: a systematic review. Ageing & Society, 38(11), 2241–2279. [Google Scholar]
- Avent ES, Rath L, Meyer K, Benton D, & Nash P (2019). Supporting Family Caregivers: How Does Relationship Strain Occur in Caregiving Dyads? A Qualitative Study. Innovation in Aging, 3(Supplement_1), S289–S289. doi: 10.1093/geroni/igz038.1066 [DOI] [Google Scholar]
- Birditt KS, Newton NJ, Cranford JA, & Ryan LH (2016). Stress and Negative Relationship Quality among Older Couples: Implications for Blood Pressure. J Gerontol B Psychol Sci Soc Sci, 71(5), 775–785. doi: 10.1093/geronb/gbv023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun M, Scholz U, Bailey B, Perren S, Hornung R, & Martin M (2009). Dementia caregiving in spousal relationships: a dyadic perspective. Aging Ment Health, 13(3), 426–436. doi: 10.1080/13607860902879441 [DOI] [PubMed] [Google Scholar]
- Brock RL, & Lawrence E (2011). Marriage as a risk factor for internalizing disorders: clarifying scope and specificity. J Consult Clin Psychol, 79(5), 577–589. doi: 10.1037/a0024941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody D, Pratt L, & Hughes J (2018). Prevalence of Depression Among Adults Aged 20 and Over: United States, 2013–2016. Retrieved from https://www.cdc.gov/nchs/data/databriefs/db303.pdf [PubMed]
- Capistrant BD, Moon JR, Berkman LF, & Glymour MM (2012). Current and long-term spousal caregiving and onset of cardiovascular disease. J Epidemiol Community Health, 66(10), 951–956. doi: 10.1136/jech-2011-200040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D, Cornman JC, & Freedman VA (2016). Marital Quality and Negative Experienced Well-Being: An Assessment of Actor and Partner Effects Among Older Married Persons. J Gerontol B Psychol Sci Soc Sci, 71(1), 177–187. doi: 10.1093/geronb/gbv073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D, Cornman JC, & Freedman VA (2017). Disability and Activity-related Emotion in Later Life: Are Effects Buffered by Intimate Relationship Support and Strain? J Health Soc Behav, 58(3), 387–403. doi: 10.1177/0022146517713551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D, Freedman VA, Cornman JC, & Schwarz N (2014). Happy Marriage, Happy Life? Marital Quality and Subjective Well-Being in Later Life. J Marriage Fam, 76(5), 930–948. doi: 10.1111/jomf.12133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL, Fung HH, & Charles ST (2003). Motivation and Emotion, 27(2), 103–123. doi: 10.1023/A:1024569803230 [DOI] [Google Scholar]
- Charles ST, & Carstensen LL (2008). Unpleasant Situations Elicit Different Emotional Responses in Younger and Older Adults. Psychol Aging, 23(3), 495–504. doi: 10.1037/a0013284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clare L, SM N, CJ W, A M, IS M, I R, … RG M (2012). Marital relationship quality in early-stage dementia: perspectives from people with dementia and their spouses. Alzheimer Dis Assoc Disord, 26(2). doi: 10.1097/WAD.0b013e318221ba23 [DOI] [PubMed] [Google Scholar]
- Cook WL, & Kenny DA (2010). The Actor–Partner Interdependence Model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development, 29(2), 101–109. doi: 10.1080/01650250444000405 [DOI] [Google Scholar]
- Cornwell EY, & Waite LJ (2009). Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav, 50(1), 31–48. doi: 10.1177/002214650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC (1976). Toward an interactional description of depression. Psychiatry, 39(1), 28–40. doi: 10.1080/00332747.1976.11023874 [DOI] [PubMed] [Google Scholar]
- Fisher GG, & Ryan LH (2018). Overview of the Health and Retirement Study and Introduction to the Special Issue. Work Aging Retire, 4(1), 1–9. doi: 10.1093/workar/wax032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gellert P, Hausler A, Gholami M, Rapp M, Kuhlmey A, & Nordheim J (2018). Own and partners’ dyadic coping and depressive symptoms in individuals with early-stage dementia and their caregiving partners. Aging Ment Health, 22(8), 1008–1016. doi: 10.1080/13607863.2017.1334759 [DOI] [PubMed] [Google Scholar]
- Griffin J, Meis L, Greer N, MacDonald R, Jensen A, Rutks I, … Wilt T (2015). Effectiveness of caregiver interventions on patient outcomes in adults with dementia or Alzheimer’s disease: A systematic review. Gerontology and Geriatric Medicine. doi: 10.1177/2333721415595789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study, t. H. C. (2017). Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740).
- Karim J, Weisz R, Bibi Z, & ur Rehman S (2014). Validation of the Eight-Item Center for Epidemiologic Studies Depression Scale (CES-D) Among Older Adults. Current Psychology, 34(4), 681–692. doi: 10.1007/s12144-014-9281-y [DOI] [Google Scholar]
- Kenny D, Kashy D, & Cook W (2006). Dyadic Analysis. New York: Guildford. [Google Scholar]
- Knobloch LK, Nichols LO, & Martindale-Adams J (2019). Applying Relational Turbulence Theory to Adult Caregiving Relationships. Gerontologist. doi: 10.1093/geront/gnz090 [DOI] [PubMed] [Google Scholar]
- Lawrence E, Bunde M, Barry RA, Brock RL, Sullivan KT, Pasch LA, … Adams EE (2008). Partner support and marital satisfaction: Support amount, adequacy, provision, and solicitation. Personal Relationships, 15(4), 445–463. doi: 10.1111/j.1475-6811.2008.00209.x [DOI] [Google Scholar]
- Ledermann T, & Kenny DA (2017). Analyzing dyadic data with multilevel modeling versus structural equation modeling: A tale of two methods. J Fam Psychol, 31(4), 442–452. doi: 10.1037/fam0000290 [DOI] [PubMed] [Google Scholar]
- Lee M, Ryoo JH, Campbell C, Hollen PJ, & Williams IC (2019). Exploring the challenges of medical/nursing tasks in home care experienced by caregivers of older adults with dementia: An integrative review. J Clin Nurs, 28(23–24), 4177–4189. doi: 10.1111/jocn.15007 [DOI] [PubMed] [Google Scholar]
- Lohman M, Dumenci L, & Mezuk B (2014). Sex differences in the construct overlap of frailty and depression: evidence from the Health and Retirement Study. J Am Geriatr Soc, 62(3), 500–505. doi: 10.1111/jgs.12689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalowski VI, Hoppmann CA, & Gerstorf D (2016). Associations Between Perceived Support in Older Adult Marriages and Dyadic Covariations in Momentary Affect and Aches. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 71(3), 425–430. doi: 10.1093/geronb/gbu151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KJ, Mesagno C, McLaren S, Grace F, Yates M, & Gomez R (2019). Exercise, Mood, Self-Efficacy, and Social Support as Predictors of Depressive Symptoms in Older Adults: Direct and Interaction Effects. Front Psychol, 10, 2145. doi: 10.3389/fpsyg.2019.02145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin J, Poulin M, Stephanie B, & Langa K (2017). Spouses’ daily feelings of appreciation and self-reported well-being. Health Pscyhology, 36(12), 1135–1139. doi: 10.1037/hea0000527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin J, & Schulz R (2009). Interpersonal effects of suffering in older adult caregiving relationships. Psychol Aging, 24(3), 681–695. doi: 10.1037/a0016355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R, Martire LM, Jennings JR, Lingler JH, & Greenberg MS (2010). Spouses’ cardiovascular reactivity to their partners’ suffering. J Gerontol B Psychol Sci Soc Sci, 65B(2), 195–201. doi: 10.1093/geronb/gbp133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, & Skaff MM (1990). Caregiving and the stress process: an overview of concepts and their measures. Gerontologist, 30(5), 583–594. doi: 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Peluso PR, Watts RE, & Parsons M (2013). Changing Aging, Changing Family Therapy: practicing with 21st century realities. New York: Taylor & Francis. [Google Scholar]
- Perndorfer C, Soriano EC, Siegel SD, & Laurenceau JP (2019). Everyday protective buffering predicts intimacy and fear of cancer recurrence in couples coping with early-stage breast cancer. Psychooncology, 28(2), 317–323. doi: 10.1002/pon.4942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, & Sorensen S (2011). Spouses, adult children, and children-in-law as caregivers of older adults: a meta-analytic comparison. Psychol Aging, 26(1), 1–14. doi: 10.1037/a0021863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn C, Clare L, & Woods B (2009). The impact of the quality of relationship on the experiences and wellbeing of caregivers of people with dementia: a systematic review. Aging Ment Health, 13(2), 143–154. doi: 10.1080/13607860802459799 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Riffin C, Van Ness PH, Wolff JL, & Fried T (2017). Family and Other Unpaid Caregivers and Older Adults with and without Dementia and Disability. Journal of the American Geriatrics Society, 65(8), 1821–1828. doi: 10.1111/jgs.14910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberto K, McCann B, & Blieszner R (2011). Trajectories of care: Spouses coping with changes related to mild cognitive impairment. Dementia, 12(1), 45–62. doi: 10.1177/147130121142123 [DOI] [PubMed] [Google Scholar]
- Rook KS (2015). Social Networks in Later Life: Weighing Positive and Negative Effects on Health and Well-Being. Curr Dir Psychol Sci, 24(1), 45–51. doi: 10.1177/0963721414551364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salinger JM, Whisman MA, Randall AK, & Hilpert P (2020). Associations Between Marital Discord and Depressive Symptoms: A Cross-Cultural Analysis. Fam Process. doi: 10.1111/famp.12563 [DOI] [PubMed] [Google Scholar]
- Schulz R, Aranda M, Beane S, Czaja S, Duke B, Feder J, & Hinton L (2016). Families caring for an aging America. Retrieved from Washington, DC: [Google Scholar]
- Schuster TL, Kessler RC, & Aseltine RH Jr. (1990). Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol, 18(3), 423–438. doi: 10.1007/BF00938116 [DOI] [PubMed] [Google Scholar]
- Smith J, Ryan L, Sonnega A, & Weir D (2017). Psychosocial and Lifestyle Questionnaire 2006 – 2016. Retrieved from Ann Arbor, Michigan: https://hrs.isr.umich.edu/sites/default/files/biblio/HRS%202006-2016%20SAQ%20Documentation_07.06.17.pdf [Google Scholar]
- Uchino B (2006). Social Support and Health: A Review of Physiological Processes Potentially Underlying Links to Disease Outcomes. Journal of Behavioral Medicine, 29(4), 377–387. [DOI] [PubMed] [Google Scholar]
- Umberson D, Williams K, Powers DA, Liu H, & Needham B (2006). You make me sick: marital quality and health over the life course. J Health Soc Behav, 47(1), 1–16. doi: 10.1177/002214650604700101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walen H, & Lachman M (2000). Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships, 17, 5–3-. doi: 10.1177/0265407500171001 [DOI] [Google Scholar]
- Wang S, Kim K, & Boerner K (2018). Personality similarity and marital quality among couples in later life. Personal Relationships, 25, 565–580. doi:0.1111/pere.12260 [Google Scholar]
- Whisman MA, Robustelli BL, & Labrecque LT (2018). Specificity of the Association between Marital Discord and Longitudinal Changes in Symptoms of Depression and Generalized Anxiety Disorder in the Irish Longitudinal Study on Ageing. Fam Process, 57(3), 649–661. doi: 10.1111/famp.12351 [DOI] [PubMed] [Google Scholar]
- Whisman MA, & Uebelacker LA (2009). Prospective associations between marital discord and depressive symptoms in middle-aged and older adults. Psychol Aging, 24(1), 184–189. doi: 10.1037/a0014759 [DOI] [PubMed] [Google Scholar]
- Zarit S, & Edwards A (2008). Handbook of the Clinical Psychology of Ageing. In Wood B & Clare L (Eds.), (2 ed.). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Zarit SH, Femia EE, Watson J, Rice-Oeschger L, & Kakos B (2004). Memory Club: a group intervention for people with early-stage dementia and their care partners. Gerontologist, 44(2), 262–269. doi: 10.1093/geront/44.2.262 [DOI] [PubMed] [Google Scholar]


