Abstract
Background
As one of the most widely researched consequence of traumatic events, the prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from coronavirus disease 2019 (COVID-19) outbreak varies greatly across studies. This review aimed at examining the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak.
Methods
Systematic searches of databases were conducted for literature published on PubMed, EMBASE, Web of Science, the Cochrane Library, PsycArticle, and Chinese National Knowledge Infrastructure until October 14, 2020. Statistical analyses were performed using R software (PROSPERO registration number: CRD42020180309).
Results
A total of 106,713 people exposed to the trauma resulting from the COVID-19 outbreak were identified in the 76 articles, of which 33,810 were reported with post-traumatic stress symptoms. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was 28.34%, with a 95% confidence interval of 23.03-34.32%. Subgroup analysis indicated that older age, male and bigger sample size were associated with higher prevalence of post-traumatic stress symptoms. After controlling for other factors, the results of meta-regression showed that the influence of gender and sample size on prevalence is no longer significant.
Conclusions
Symptoms of post-traumatic stress disorder (PTSD) were very common among people exposed to the trauma resulting from COVID-19 outbreak. Further research is needed to explore more possible risk factors for post-traumatic stress symptoms and identify effective strategies for preventing PTSD-related symptoms among people exposed to the trauma resulting from COVID-19 outbreak.
Keywords: COVID-19, meta-analysis, PTSD, prevalence
Background
As of December 14, 2020, 70.4 million confirmed cases of coronavirus disease 2019 (COVID-19) and 1.6 million deaths have been reported to the World Health Organization [1]. The outbreak of COVID-19 spread rapidly, caused enormous losses to individual health, national economy, and social wellbeing [2,3]. Currently, control of the epidemic of COVID-19 is still the dominant task across the world, millions of people are scared and even panic of the possible loss of health, life, and wealth. Although it is too early to predict how many people worldwide will be infected with this emerging virus, it is believed that the numbers of case and death will continue to increase in the forthcoming months.
Some psychologists draw attention toward post-traumatic stress disorder (PTSD) as the second tsunami of the COVID-19 pandemic [4]. According to the Diagnostic and Statistics of Mental Disorders, the fifth edition (DSM-5), the clinical features of PTSD include persistent avoidance of stimuli, persistent intrusion symptoms, negative alterations in cognition or mood and marked alterations in arousal and reactivity, all of which are related to traumatic events [5]. PTSD could cause clinically significant distress or impairment in occupational, social, or other important functioning [6]. The outbreak of COVID-19 is the most severe pandemic since Spanish Influenza, the outbreak itself and the measures taken to bring it under control have likely been highly stressful for many individuals, which is very likely to promote PTSD [7,8]. Additionally, it is said that such new type of infectious diseases were very traumatizing for people across the world with a poor understanding of viruses and spreading mechanisms [4]. The evocation of COVID-19 is thus generating a great anxiety and biased responses to threat, which can also promote PTSD [9].
When COVID-19 breaks out, people may experience many types of psychological trauma, such as directly suffering from the symptoms and traumatic treatment (respiratory failure, tracheotomy, etc.) [8], witness of suffering, struggling, and dying of patients [10]. Additionally, individuals may experience the fear of infection, social isolation, exclusion, and stigmatization, as patients, related caregivers, and workers, or even the general public [11,12]. It is said that there is a dose–response relationship between the degree of trauma and the mental health burden of disasters [13]. The prevalence of PTSD is higher among people who were directly exposed to the disaster, lower among related caregivers and rescue workers, and yet even lower in the general population. These different populations are likely to represent different levels of severity of trauma exposure, with direct victims having the highest exposure and associated PTSD prevalence while people in the general population having the lowest levels of exposure and associated PTSD prevalence [14]. Currently, the relationship between the degree of trauma and the mental health burden of COVID-19 outbreak is unclear.
As one of the most widely researched consequence of traumatic events [14], the prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak varies greatly across studies [15–18]. In addition, many factors have been reported to be associated with the prevalence of PTSD during COVID-19 outbreak, such as gender, age, and degree of trauma exposure [8,19,20], but the results are not consistent in different studies. The possible causes of the inconsistencies in the current estimates were unclear. For taking effective measures to reduce the psychological sequelae caused by COVID-19 across the world, it is necessary to determine a more accurate estimation of the prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak, and to explore the possible causes of the inconsistencies in the current estimates. This review aimed at examining the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak, summarizing possible vulnerability factors of post-traumatic stress symptoms and examining potentially vulnerable populations, try to provide a reference for COVID-19 and possible outbreak of infectious diseases in the future.
Methods
This review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA guideline) and Meta-analyses of Observational Studies in Epidemiology guidelines [21,22]. The protocol of this review is registered in the International Prospective Register of Systematic Reviews (registration number: CRD42020180309). See Supplementary Material for the details.
Search strategy
PubMed, EMBASE, Web of Science, the Cochrane Library, MEDLINE, and Chinese National Knowledge Infrastructure were independently searched for published articles by two reviewers with no restrictions on date or language of publication up until 30 June 2020, and an update search was conducted on October 14, 2020. The following search terms were used: “COVID-19” (including “coronavirus disease 2019,” “SARS-CoV-2,” “severe acute respiratory syndrome coronavirus 2,” “COVID-19,” “Covid 19,” “SARS-CoV,” “novel coronavirus,” “coronavirus,” “CoV-2,” “2019-nCoV,” and “SARS COV2”); “Post-traumatic stress disorder” (including “post-traumatic stress disorder,” “post-traumatic syndrome,” “PTSD,” “stress disorder,” “post-traumatic,” and “post-traumatic syndrome”). See Supplementary Data for a full search strategy.
Study selection
Studies were included if they meet the following criteria: (a) the study was observational study; (b) the participants were adult aged ≥18; (c) information about prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was provided; (d) the full article was written in English or Chinese. Studies were excluded if (a) the report was a review, comments, meta-analysis, or protocol and (b) the participants with comorbid symptoms or chronic disease (such as mental illness, cancer, etc.).
Data extraction
Data extraction was conducted independently in pairs by trained researchers who used standardized data extraction forms. Two reviewers (D.Q. and Y.L.L.) checked the titles, abstracts, and full-texts of the initial search results independently. Data were extracted on first author, country or area, survey period, target population, study design, sample size, response rate, percentage of male participants, mean age of participants, instruments used to identify post-traumatic stress symptoms, prevalence of post-traumatic stress symptoms, and quality score of the included studies. Any discrepancies that emerged in these procedures were discussed and resolved by involving a third reviewer (S.Y.X.).
Quality assessment
Two independent reviewers (J.H. and F.Y.O.Y.) used the established guidelines, the Loney criteria, to evaluate the methodological quality of the included studies, which has been widely used to evaluate observational studies [23,24]. The included papers were scored according to eight criteria, such as study design, sample size, sampling method, response rate, definition of participants, appropriateness of measurement and analysis. The scores range from 0 to 8, with a score of 0–3 as low quality, 4–6 as moderate, and 7–8 as high [25]. See Table S3 for details on the quality assessment.
Statistical analyses
When data were available for three or more papers, prevalence was combined [26]. When there were four or more papers, quantitative subgroup analysis was conducted [27]. All the statistical analyses were performed using the “meta” (4.12-0) and “metafor” package (2.4-0) of R version 4.0.0. Between-study heterogeneity was evaluated by Cochran’s Q test and quantified by the I2 statistic, with values >50% indicating moderate heterogeneity [28,29]. As we expected considerable heterogeneity, we calculated pooled prevalence with the random effects model. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was combined using Logit transformation method by a random effects model [29,30]. If more than one dataset was reported for the same group of participants, the outcomes that were assessed at the baseline were used. In order to compare the prevalence from different papers, we conducted subgroup meta-analysis. Because subgroup analyses should be interpreted with caution [31], we planned a priori to limit our subgroup analyses to a small number of baseline characteristics including gender, age, area, population, survey time after the outbreak, sample size, assessment tool, and quality score. The difference between subgroups was examined using the Cochran’s Q chi-square tests [30]. Mixed-model meta-regression analyses were performed by using Freeman–Tukey double arcsine method to explore potential moderators on the heterogeneity [32]. Publication bias was investigated by funnel plot and Egger’s test [30,33]. To evaluate the consistency of the results, sensitivity analysis was performed. In this study, sensitivity analyses were planned a priori for the primary analyses set by: (a) excluding studies one by one and (b) excluding studies with extreme outcomes [30,31]. All the statistical tests were two-sided, with a significance threshold of p < 0.05.
Results
Literature search
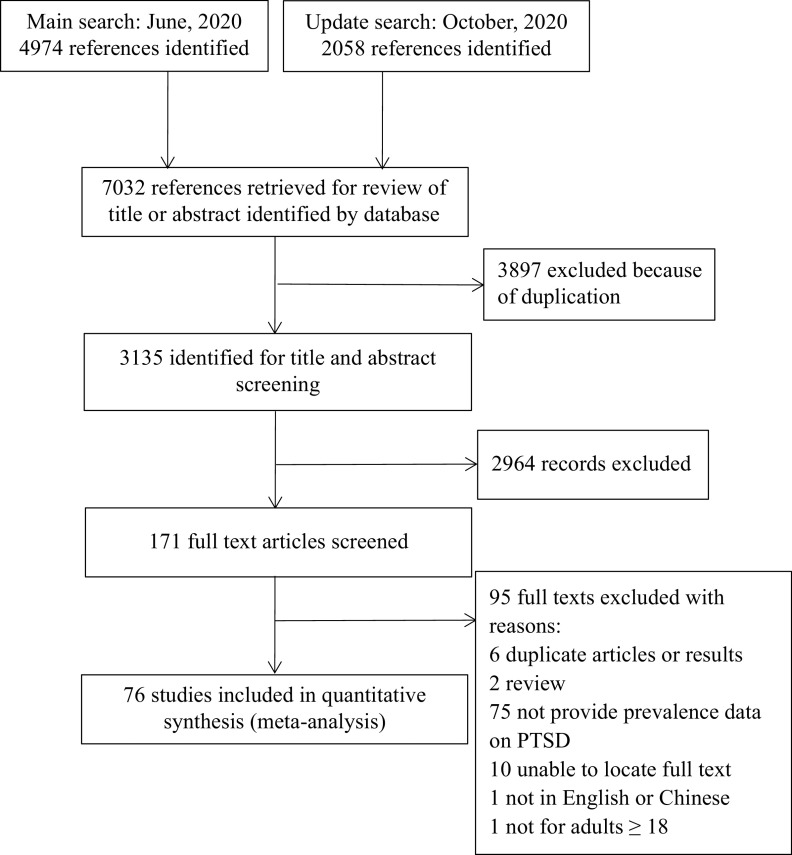
As shown in Figure 1, a total of 7,032 references were identified. Among them, 3,897 duplicates were removed. By screening titles and abstracts, 2,964 irrelevant articles were excluded. A total of 171 potentially relevant full-text articles were independently assessed based on the selection criteria. Further, 95 studies were excluded because of the following reasons: duplicate articles or results (n = 6); review or conference abstract (n = 2); did not provide data on PTSD (n = 75); unable to locate full text (n = 10); not in English or Chinese (n = 1); and not for participants aged ≥18 (n = 1). Finally, 76 eligible studies were included in this review [7–9,19,20,34–104]. The reliability for the full-text review between the two reviewers (D.Q. and Y.L.L.) was rated as good (Kappa = 0.78) [105]. See Figure 1 for the details.
Figure 1.
Flow of studies through review.
Study characteristics
Table 1 presents the main characteristics of the 76 included studies. Among them, 66 were in English and 10 were in Chinese. Most of the included studies were from Asia, such as China, Indian, and Singapore. See Table 1 for the details. From the 76 papers, 1 (1.31%) study was rated as high quality, 70 (92.11%) were rated as moderate, and 5 (6.58%) were rated as low quality. The reliability for the quality assessment between the two reviewers (J.H. and F.Y.O.Y.) was rated as good (Kappa = 0.73) [105]. For data extraction, all the criteria received a kappa value >0.85. Details of the methodological quality assessments of all 76 studies are showed in Tables S2 and S3.
Table 1.
Study characteristics of the included studies.
| First author | Study design | Population | Event/N | Survey time after the outbreak (week) | Mean age | Percentage of male participants (%) | Response rate (%) | Assessment tool | Quality score |
|---|---|---|---|---|---|---|---|---|---|
| Tee [34] | CS | General population | 316/1,879 | 9 | 34.5 ± 13.4 | 31.0 | 75.4 | IES-R (≥24) | 5 |
| Si [35] | CS | Healthcare workers | 347/863 | 4 | / | 29.3 | 76.0 | IES-6 (≥10) | 6 |
| Rodríguez-Rey [36] | CS | General population | 1,559/3,055 | 7 | 32.1 ± 12.9 | 29.3 | / | IES-R (≥24) | 5 |
| Nie [37] | CS | Healthcare workers | 194/263 | 2 | / | 23.3 | 96.3 | IES-R (≥20) | 5 |
| Liang [38] | CS | College students | 1,822/4,164 | 3 | / | 52.0 | / | IES-6 | 6 |
| Li [39] | CC | Healthcare workers | 1,382/4,369 | 2 | / | 0.0 | 82.2 | IES-R (≥34) | 7 |
| Giusti [40] | CS | Healthcare workers | 121/330 | 11 | 44.6 ± 13.5 | 37.4 | 71.2 | IES-6 (≥9) | 6 |
| Chen [41] | CS | Healthcare workers/general population | 900/1,493 | 4 | / | 55.3 | 93.3 | IES-R (≥20) | 6 |
| Caillet [42] | F | General population | 52/208 | 10 | / | 25.0 | / | IES-R | 5 |
| Barbato [43] | CS | General population | 33/148 | 10 | 41.4 ± 7.1 | 24.0 | 40.0 | IES-R (≥33) | 5 |
| Alkhamees [44] | CS | General population | 467/1,160 | 10 | / | 36.1 | / | IES-R (≥24) | 4 |
| Zhou [45] | CC | General population | 23/859 | 5 | 32.7 | 0.0 | / | IES-R (≥33) | 5 |
| Zhao [46] | CS | General population | 29/515 | 1 | / | 33.6 | / | PCL-5 | 3 |
| Zhang [47] | CS | General population | 377/560 | 4 | 25.8 ± 2.7 | 0.0 | 93.3 | IES-R (≥26) | 4 |
| Yin [48] | CS | Healthcare workers | 15/371 | 2 | 35.3 ± 9.4 | 38.5 | / | PCL-5 (≥33) | 4 |
| Wesemann [49] | CS | General population | 23/60 | 6 | 59.0 ± 17.8 | 53.7 | / | PCL-5 | 3 |
| Wang [50] | F | General population | 98/1,210 | 1 | / | 32.7 | 92.7 | IES-R (≥24) | 4 |
| Varshney [51] | CS | General population | 217/653 | 9 | 41.8 | 75.2 | / | IES-R (≥24) | 4 |
| Traunmüller [52] | CS | General population | 2,377/4,126 | 9 | 38.6 ± 13.3 | 26.0 | / | IES-R (≥24) | 5 |
| Tang [53] | CS | General population | 67/2,485 | 4 | 19.8 | 38.3 | 69.3 | PCL-C (≥38) | 6 |
| Tan [54] | CS | General population | 126/673 | 4 | 38.8 ± 7.4 | 74.4 | 50.8 | IES-R (≥18) | 5 |
| Song [55] | CS | Healthcare workers | 1,353/14,825 | 5 | 34.0 ± 8.2 | 35.7 | / | PCL-C (≥38) | 5 |
| Sherman [56] | CS | General population | 29/591 | 17 | 35.9 ± 8.2 | 22.5 | 35.3 | PCL-5 (≥33) | 6 |
| Seyahi [57] | CS | Hospital workers/teachers | 219/535,132/917 | 10 | 42.0/31.0/35.0 | 46.0/51.0/39.0 | 42.8/22.3/41.7 | IES-R (≥33) | 6 |
| Rossi [58] | CS | General population | 6,604/18,147 | 9 | 38.0 ± 23.0 | 20.5 | / | GPS-PTSS | 4 |
| Rossi [59] | CS | Healthcare workers | 681/1,379 | 9 | 39.0 ± 16.0 | 22.8 | 49.3 | GPS-PTSD | 6 |
| Riello [60] | CS | Healthcare workers | 433/1,071 | 15 | / | 24.6 | 53.0 | IES-R (≥26) | 6 |
| Qi [61] | CS | COVID-19 patients | 5/41 | 3 | 40.1 ± 10.1 | 41.9 | 52.4 | PCL-5 (≥50) | 5 |
| Ma [62] | CS | General population | 164/728 | 10 | 32.9 ± 10.4 | 29.8 | 72.8 | IES-R (≥26) | 6 |
| Luceño-Moreno [63] | CS | Healthcare workers | 160/1,422 | 9 | 43.8 ± 10.2 | 13.6 | 75.3 | IES-R (≥20) | 6 |
| Liu [64] | CS | General population | 20/285 | 1 | / | 45.6 | 95.0 | PCL-5 (≥33) | 4 |
| Liu [20] | CS | COVID-19 patients | 84/675 | 8 | / | 47.0 | 90.0 | PCL-5 | 6 |
| Liu [65] | CS | General population | 285/898 | 11 | 24.5 | 14.1 | / | PCL-C (≥38) | 5 |
| Li [66] | F | College students | 160/1,442 | 2 | / | / | 71.2 | IES-R (≥24) | 7 |
| Li [67] | CS | Healthcare workers | 640/3,637 | 2 | 34.4 ± 9.6 | 37.0 | / | IES-R (≥24) | 3 |
| Li [68] | CS | Healthcare workers | 220/356 | 1 | 31.3 | 13.8 | 98.6 | PCL-5 | 6 |
| Li [69] | CS | General population | 271/398 | 13 | / | 50.5 | 70.2 | IES-7 | 5 |
| Li [70] | CS | General population | 744/1,109 | 9 | / | 56.0 | / | IES-R (≥20) | 5 |
| Leng [71] | CS | Healthcare workers | 5/90 | 7 | / | 27.8 | 83.3 | PCL-C (≥50) | 6 |
| Le [72] | CS | General population | 386/1,423 | 10 | 35.0 | 33.4 | / | IES-R (≥24) | 5 |
| Lange [73] | CS | Healthcare workers | 23/135 | 11 | 47.9 ± 11.4 | 40.9 | 31.1 | IES-R | 5 |
| Lai [74] | CS | Healthcare workers | 1,017/1,257 | 1 | / | 23.3 | 68.7 | IES-R (≥26) | 6 |
| Lahav [8] | CS | General population | 112/976 | 10 | 44.3 ± 14.2 | 18.4 | 77.3 | PCL-5 (≥33) | 5 |
| Karatzias [75] | CS | General population | 184/1,041 | 9 | / | 48.2 | / | ITQ | 6 |
| Cardel [76] | CS | General population | 92/250 | 10 | / | 15.0 | / | IES-6 | 4 |
| Guo [77] | CS | General population | 1,944/2,441 | 1 | / | 47.6 | / | PCL-C-2 | 5 |
| González-Sanguino [78] | CS | General population | 550/3,480 | 8 | / | 25.0 | / | PCL-C | 3 |
| González Ramírez [79] | CS | General population | 1,160/3,932 | 9 | 33.0 | 25.5 | / | IES-R | 4 |
| Forte [80] | CS | General population | 635/2,291 | 8 | 30.0 ± 11.5 | 25.4 | / | IES-R(≥33) | 5 |
| Fekih-Romdhane [81] | CS | General population | 199/603 | 10 | 29.2 ± 10.4 | 26.0 | / | IES-R (≥33) | 4 |
| El‑Zoghby [82] | CS | General population | 387/510 | 14 | / | 34.1 | / | IES-R (≥24) | 5 |
| Dobson [83] | CS | Healthcare workers | 93/320 | 12 | / | 18.4 | / | IES-R (≥26) | 6 |
| Di Tella [84] | CS | Healthcare workers | 38/145 | 8 | 42.9 ± 11.2 | 27.6 | / | PCL-5 | 3 |
| Cortés-Álvarez [85] | CS | General population | 555/1,105 | 10 | / | 37.9 | / | IES-R | 6 |
| Civantos [86] | CS | Healthcare workers | 210/349 | 11 | / | 60.7 | / | IES-R (≥26) | 6 |
| Civantos [87] | CS | Healthcare workers | 43/163 | 15 | / | 74.2 | 23.3 | IES-R (≥26) | 5 |
| Chi [88] | CS | College students | 627/2,038 | 3 | 20.5 ± 1.9 | 37.0 | 81.5 | PCL-C | 5 |
| Chew [89] | CS | Healthcare workers | 91/1,146 | 14 | 31.7 ± 7.8 | 34.9 | 88.2 | IES-R (≥24) | 6 |
| Chang [7] | CS | COVID-19 patients | 13/64 | 6 | 54.7 ± 16.6 | 43.7 | 58.7 | PCL-5 (≥33) | 5 |
| Cai [90] | CS | Healthcare workers | 184/709 | 1 | / | 3.5 | / | IES-R | 5 |
| Cai [19] | CS | COVID-19 patients | 39/126 | 4 | 45.7 ± 14.0 | 47.6 | 100.0 | PTSD-SS | 4 |
| Bo [9] | CS | COVID-19 patients | 689/714 | 6 | 50.2 ± 12.9 | 49.1 | 97.8 | PCL-C (⩾50) | 5 |
| Blekas [91] | CS | Healthcare workers | 45/270 | 11 | 37.6 ± 11.9 | 21.9 | / | PSDI-8 | 4 |
| Zhang [92] | CS | General population | 20/263 | 1 | 37.7 ± 14.0 | 40.3 | 65.7 | IES-R | 5 |
| Zhang [93] | CS | Suspected COVID-19 patients | 13/93 | 4 | 38.7 ± 13.6 | 54.8 | 100.0 | PCL-5 (≥33) | 6 |
| Zhang [94] | CS | Suspected COVID-19 patients | 87/306 | 6 | 34.8 ± 8.3 | 7.8 | / | PCL-5 (≥38) | 4 |
| Yuan [95] | CS | Suspected COVID-19 patients | 39/126 | 5 | 45.7 ± 14.0 | 47.6 | / | PTSD-SS | 4 |
| Xie [96] | CS | General population | 72/333 | 3 | 31.0 ± 10.1 | 39.9 | 93.8 | PCL-C (≥40) | 4 |
| Liu [97] | CS | General population | 453/584 | 3 | 35.3 ± 8.9 | 33.0 | 90.9 | PCL-C (≥40) | 6 |
| Liu [98] | CS | Healthcare workers | 20/221 | 8 | / | 1.0 | 99.0 | PCL-C (≥40) | 6 |
| Leng [99] | CS | Healthcare workers | 24/72 | 1 | / | 11.1 | 92.7 | IES-R (≥26) | 4 |
| Chen [100] | CS | Healthcare workers | 23/109 | 6 | / | 11.9 | / | PCL-C (≥38) | 6 |
| Hao [101] | CC | General population | 15/109 | 4 | / | 32.9/ 37.6 | 11.3/81.3 | IES-R (≥24) | 5 |
| Liang [102] | CS | General population | 84/584 | 2 | / | 38.1 | 95.7 | PCL-C (≥38) | 6 |
| Li [103] | CS | Healthcare workers | 104/205 | 3 | / | 14.6 | 99.9 | PCL-C (≥38) | 5 |
| Huang [104] | CS | Healthcare workers | 63/230 | 2 | 32.6 ± 6.2 | 18.7 | 93.5 | PTSD-SS (≥55) | 6 |
Abbreviations: CC, case–control study; COVID-19: coronavirus disease 2019; CS, cross-sectional study; F, follow up study; IES-6, The Impact of Event Scale-6; IES-R, The Impact of Event Scale-Revised; ITQ, The International Trauma Questionnaire; PCL-5, the Post‐traumatic stress disorder checklist‐5; PCL-C, The amended self-reported Post-Traumatic Stress Disorder (PTSD) Checklist-Civilian Version; PSDI-8, Posttraumatic Stress Disorder-8 inventory; PTSD-SS, Post-traumatic stress disorder self-rating scale.
Pooled prevalence of post-traumatic stress symptoms among people influenced by the COVID-19 outbreak
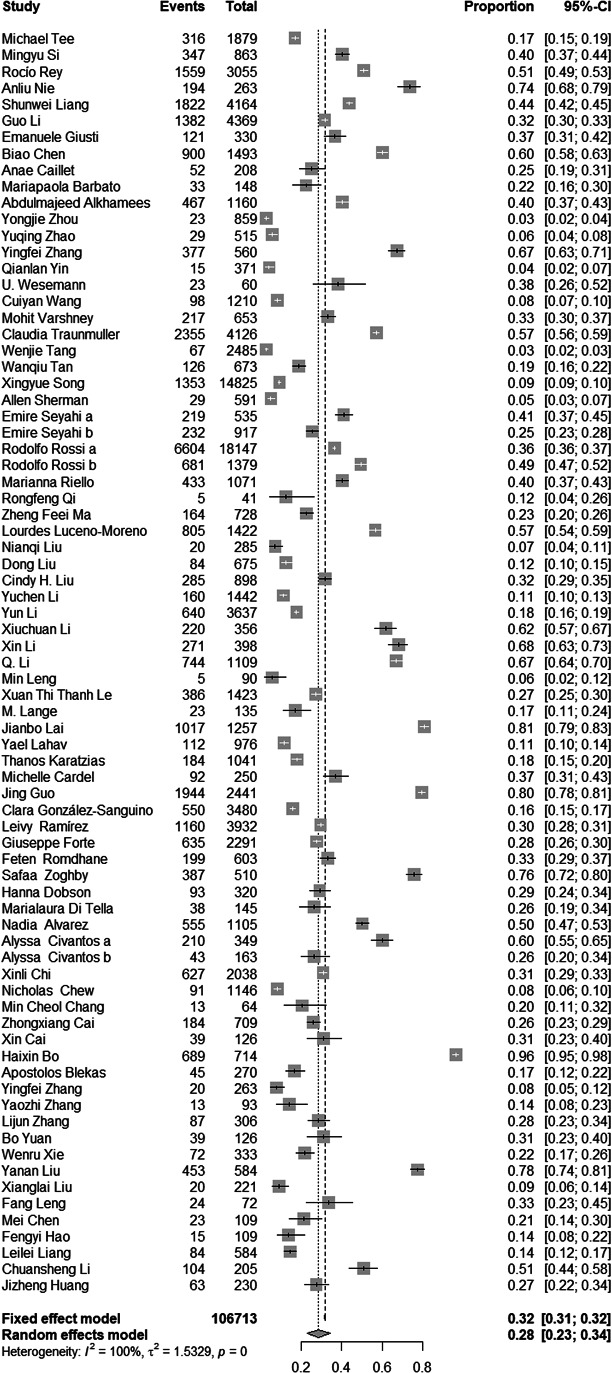
There were 76 studies reported prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from the COVID-19 outbreak. The forest plot in Figure 2 depicts the details. A total of 106,713 people exposed to the trauma resulting from the COVID-19 outbreak were identified in the 76 articles, of which 33,810 were reported with post-traumatic stress symptoms. The random effects model was used to determine the pooled prevalence (Q = 14,854.51, I2 = 99.70%, p < 0.001), the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was 28.34%, with a 95% confidence interval (CI) of 23.03–34.32%.
Figure 2.
Forest plots.
Subgroup analysis for the included studies
The details of subgroup analyses are presented in Table 2. Significant differences in the prevalence of post-traumatic stress symptoms between different ages were found (Q = 221.97, p < 0.001). The results indicated that older participants (with a mean age ≥51) showed higher prevalence of post-traumatic stress symptoms (62.16%), younger participants (with a mean age between 18 and 20) showed lowest prevalence of post-traumatic stress symptoms (2.70%). Significant difference in the prevalence of post-traumatic stress symptoms between different gender was observed, the results indicated that studies with higher percentage of male participants (>50%) showed higher prevalence (26.70 vs. 41.79%; Q = 5.31, p = 0.021). The pooled prevalence of post-traumatic stress symptoms among people in the European region, the America region, the Eastern Mediterranean region, the Western Pacific region, and the South-East Asia region were 32.13%, 30.48%, 37.74%, 26.34%, and 17.16%, respectively. No significant differences in the prevalence of post-traumatic stress symptoms between different region were found (Q = 2.94, p = 0.580). Furthermore, the pooled prevalence of post-traumatic stress symptoms among people in the high-income region, the upper-middle-income region, and the lower-middle-income region were 30.03, 27.26, and 36.07%, respectively. No significant differences in the prevalence of post-traumatic stress symptoms between different income classification were found (Q = 0.81, p = 0.667). Also, the pooled prevalence of post-traumatic stress symptoms among COVID-19 patients, healthcare workers, suspected cases of COVID-19, the general population, and teachers/students were 36.30, 29.22, 24.47, 27.13, and 29.39%, respectively. No significant differences in the prevalence of post-traumatic stress symptoms between different population were found (Q = 0.87, p = 0.928). Although the prevalence of post-traumatic stress symptoms greater in earlier surveys (31.49%) than later surveys (25.79%), there were no significant differences in prevalence of post-traumatic stress symptoms between different survey time after the outbreak (Q = 1.05, p = 0.304). In addition, significant difference in the prevalence of post-traumatic stress symptoms between studies with different sample size was observed, articles with higher sample size showed lower prevalence (20.33 vs. 32.08%; Q = 6.61, p = 0.010). Studies used Impact of Event Scale (IES) as assessment tool showed higher prevalence (33.43%), studies used the amended self-reported PTSD Checklist—Civilian Version as assessment tool showed lowest prevalence (21.41%) and studies used Post-Traumatic Stress Disorder Self-Rating Scale, International Trauma Questionnaire, and Post-Traumatic Stress Disorder-8 Inventory showed moderate prevalence (28.96%). No significant differences in the prevalence of post-traumatic stress symptoms between studies used different assessment tools (Q = 3.47, p = 0.176). Lastly, no significant differences in the prevalence of post-traumatic stress symptoms between studies with different quality scores were observed (28.57 vs. 28.00%; Q = 0.01, p = 0.992).
Table 2.
Subgroup analysis for the general population.
| Subgroup | Studies | Pooled prevalence % (95% CI) | I2 (%) | Test of difference within each subgroup | |
|---|---|---|---|---|---|
| Q | p | ||||
| Mean age | 221.97 | <0.001 | |||
| 18–20 | 1 | 2.70 (2.13–3.41) | 99.20 | ||
| 21–30 | 5 | 37.58 (25.97–50.83) | 98.90 | ||
| 31–40 | 25 | 22.34 (15.74–31.15) | 99.80 | ||
| 41–50 | 10 | 26.53 (19.23–35.39) | 96.50 | ||
| ≥51 | 3 | 62.16 (13.84–94.38) | 98.90 | ||
| Percentage of male participants (%) | 5.31 | 0.021 | |||
| 0–50 | 65 | 26.70 (21.06–33.22) | 99.70 | ||
| 51–100 | 11 | 41.79 (30.64–53.86) | 99.10 | ||
| WHO area | 2.86 | 0.580 | |||
| European | 18 | 32.13 (26.04–38.89) | 99.30 | ||
| Americas | 8 | 30.48 (18.78–45.39) | 99.20 | ||
| Eastern Mediterranean | 4 | 37.74 (16.62–64.82) | 99.40 | ||
| Western Pacific | 45 | 26.34 (18.88–35.46) | 99.70 | ||
| South-East Asia | 2 | 17.16 (5.78–41.16) | 98.80 | ||
| Income classification | 0.81 | 0.667 | |||
| High-income | 26 | 30.03 (24.18–36.62) | 99.40 | ||
| Upper-middle-income | 45 | 27.26 (19.59–36.55) | 99.70 | ||
| Lower-middle-income | 5 | 36.07 (20.16–55.77) | 99.30 | ||
| Population | 0.87 | 0.928 | |||
| COVID-19 patients | 5 | 36.30 (8.86–76.96) | 98.90 | ||
| Suspected COVID-19 patients | 3 | 24.47 (17.00–33.89) | 75.80 | ||
| Healthcare workers | 26 | 29.22 (21.10–38.94) | 99.50 | ||
| General population | 39 | 27.13 (20.00–35.67) | 99.80 | ||
| Teachers/students | 4 | 29.39 (16.98–45.85) | 99.40 | ||
| Survey time after outbreak (week) | 1.05 | 0.304 | |||
| 1–4 | 35 | 31.49 (25.56–38.10) | 99.50 | ||
| ≥5 | 42 | 25.79 (18.17–35.23) | 99.70 | ||
| Sample size | 6.61 | 0.010 | |||
| 0–300 | 22 | 20.33 (15.86–25.68) | 91.80 | ||
| ≥301 | 55 | 32.08 (24.82–40.32) | 99.80 | ||
| Diagnosis assessment | 3.47 | 0.176 | |||
| IER | 42 | 33.43 (26.65–40.98) | 99.60 | ||
| PCL-C | 28 | 21.41 (13.44–32.34) | 99.70 | ||
| Others | 7 | 28.96 (21.62–37.59) | 98.00 | ||
| Quality score | 0.01 | 0.992 | |||
| 0–5 | 46 | 28.57 (21.80–36.45) | 99.70 | ||
| ≥6 | 31 | 28.00 (20.04–37.62) | 99.70 | ||
Abbreviations: COVID-19, coronavirus disease 2019; PCL-C, The amended self-reported Post-Traumatic Stress Disorder (PTSD) Checklist-Civilian Version; WHO, World Health Organization.
Meta-regression analyses for the included studies
Table 3 presents the results of meta-regression analyses. Due to too much missing data (only 57.89% of studies reported data) on the mean age of participants, we were unable to include this variable in the meta-regression model. Bivariate meta-regression suggested that higher prevalence estimates reported in studies which used IES as assessment tool (β = −0.11, p = 0.061). Specifically, assessment tool accounted for 3.16% of the heterogeneity across studies, but the difference between different groups was not significant. In addition, area (β = −0.03, p = 0.568), income (β = 0.01, p = 0.882), population (β = 0.06, p = 0.626), percentage of male participants (β = 0.01, p = 0.473), survey time after the outbreak (β = 0.01, p = 0.775), quality score (β = 0.03, p = 0.407), and sample size (β = −0.01, p = 0.891) were not significant moderators too. Of the multivariate model, no significant moderators for heterogeneity were found (p > 0.05, R2 = 0.00%).
Table 3.
Meta-regression analysis for the included studies.
| Group | Β | 95% CI | p | R2 (%) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Univariate analysis | |||||
| Area (Western Pacific vs. others) | −0.03 | −0.14 | 0.08 | 0.568 | 0.00 |
| Income (high income vs. others) | 0.01 | −0.11 | 0.13 | 0.882 | 0.00 |
| Population (patients of COVID-19 vs. others) | 0.06 | −0.17 | 0.29 | 0.626 | 0.00 |
| Percentage of male (continuous variable, %) | 0.01 | −0.01 | 0.01 | 0.473 | 0.00 |
| Survey time after the outbreak (continuous variable) | 0.01 | −0.01 | 0.02 | 0.775 | 0.00 |
| Quality score (continuous variable) | 0.03 | −0.03 | 0.08 | 0.407 | 0.00 |
| Sample size (continuous variable) | −0.01 | −0.01 | 0.01 | 0.891 | 0.00 |
| Assessment tool (IES vs. others) | −0.11 | −0.22 | 0.01 | 0.061 | 3.16 |
| Multivariate analysis | 0.00 | ||||
| Area (Western Pacific vs. others) | −0.11 | −0.37 | 0.15 | 0.413 | |
| Income (high income vs. others) | −0.02 | −0.23 | 0.19 | 0.852 | |
| Population (patients of COVID-19 vs. others) | 0.15 | −0.11 | 0.41 | 0.271 | |
| Percentage of male (continuous variable, %) | 0.01 | −0.01 | 0.01 | 0.583 | |
| Survey time after the outbreak (continuous variable) | −0.01 | −0.03 | 0.01 | 0.372 | |
| Quality score (continuous variable) | 0.02 | −0.04 | 0.09 | 0.388 | |
| Sample size (continuous variable) | 0.01 | −0.01 | 0.01 | 0.879 | |
| Assessment tool (IES vs. others) | −0.11 | −0.24 | 0.01 | 0.069 | |
Abbreviations: COVID-19: coronavirus disease 2019; IES, The Impact of Event Scale.
Publication bias and sensitivity analysis
Funnel plot of publication bias is presented in Figure 3. The funnel plot of publication bias is basically symmetric, but publication bias cannot be ruled out, so Egger’s test was conducted. The results of the Egger’s test showed that publication bias was not found in this study (t = −0.971, p = 0.334).
Figure 3.
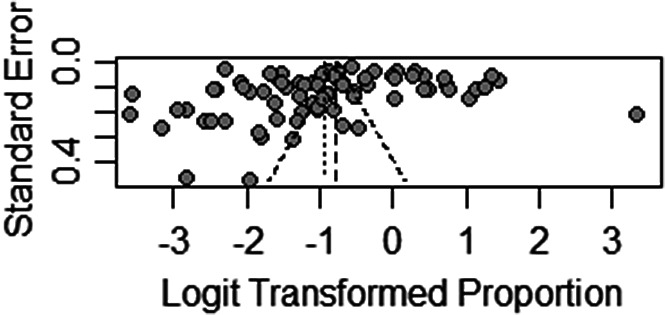
Funnel plot of publication bias.
When each study was excluded one-by-one, the recalculated combined results did not change significantly. The pooled prevalence of post-traumatic stress symptoms ranged from 27.18% (95% CI: 22.40–32.55%) to 28.96% (95% CI: 23.72–34.81%), and the I2 statistic has remained at 99.7%. The results in the current study indicate that no individual study significantly influenced the overall results. In order to examine the influence of extreme cases on the current results, we excluded all the extreme results to conduct a sensitivity analysis (with a prevalence <5% or >70%). After removing eight studies [9,45,53,56,74,77,82,97], the pooled prevalence of post-traumatic stress symptoms was 26.20% (95% CI: 22.17–30.67%), and the I2 statistic was 99.5%. Compared with the initial results, no significant changes were found. See Figure S1 for the details of sensitivity analysis.
Discussion
Key findings
This review has highlighted the importance of considering the psychological impacts of people exposed to the trauma resulting from COVID-19 outbreak. A total of 106,713 people exposed to the trauma resulting from the COVID-19 outbreak were identified in the 76 articles, of which 33,810 were reported with post-traumatic stress symptoms. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was 28.34%, with a 95% CI of 23.03–34.32%.
Comparison with the literature
Based on the results of the World Health Organization World Mental Health Surveys in 2017, the global lifetime prevalence of PTSD-related symptoms among the general population was 3.90–5.60% [106]. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak in this study was 28.34%, which was much higher than the general population. Between December 2019 and May 2020, a few reviews related to mental health and infectious disease outbreak reported limited data on pooled prevalence of PTSD-related symptoms during the COVID-19 outbreak. In Salehi et al.’s [15] study, the pooled prevalence of PTSD-related symptoms during the coronavirus outbreaks (SARS, MERS, and COVID-19) was 18%, which was much lower than our results. In Krishnamoorthy et al.’s [16] study, the pooled prevalence of PTSD-related symptoms during the COVID-19 outbreak ranged from 21.94 to 27.00% [17,18], were lower than our results. Those researches have explored a variety of mental health problems (such as depression, anxiety, and insomnia), PTSD is only one of the outcomes. Thus, we believe their search strategies on PTSD are inaccurate enough and the data they included were limited, which may affect the results. Despite the high heterogeneity in their studies, no subgroup analysis was conducted to explore the source of the heterogeneity on the pooled prevalence of PTSD in most of them [15,16,18], which we think is another limitation. In Cooke et al.’s [17] study, although the source of the heterogeneity was explored, they only included age and gender as moderators. Moreover, we found that the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was higher than flood survivors (15.74%) and hurricane survivors (17.81%) [107,108], but equal to earthquake survivors (23.66%) [109]. Compared with COVID-19 outbreak, some natural disasters such as flood and hurricane can be predicted, while earthquakes, infectious disease like COVID-19 were often happened suddenly and without a warning, pose a huge threat to people’s health and property in a short period of time [109]. Therefore, earthquakes and infectious disease outbreak might have caused more damage to people’s mental health than flood and hurricane.
The prevalence of post-traumatic stress symptoms in older adults is significantly higher than the younger people in the subgroup analysis, which was consistent with other studies [32]. Due to too much amount of missing data (only 57.89% of studies reported data on mean age of participants), we were unable to include this variable in the meta-regression model. Thus, this observation requires further clarification. Based on the current results, healthcare providers should pay more attention to the assessment of early trauma responses among older COVID-19 patients in the clinical practice and implement early psychological interventions accordingly. It is said that females were more likely to develop PTSD [109]. In the current study, however, males were associated with higher prevalence of post-traumatic stress symptoms. The possible reason is that males are more likely to be affected by COVID-19 and reported a higher fatality rate [110], they may experience higher level of severity of trauma exposure. In addition, although the epidemic situation is more serious in Europe and the Americas, no significant difference was found between different regions. It might be related to issues with numbers of studies, we think more prevalence studies in low-income countries are needed to understand the panorama of PTSD among people influenced by COVID-19. Besides, Previous research has shown that patients of infectious disease often directly suffering from the symptoms and traumatic treatment. After being cured, they were more vulnerable to social discrimination than other groups [14]. These experiences may result in higher prevalence of PTSD among them when compared with other populations. Although the prevalence of PTSD among COVID-19 patients is higher than that of other populations in this study, the difference is not significant, which need further exploration. Also, post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak were higher in the immediate aftermath of the outbreak (0–4 weeks), but the difference was not significant, which was inconsistent with other studies [109,111,112]. The possible reason is that the epidemic has not abated over time and has been spreading, people have been exposed to the trauma resulting from COVID-19 outbreak. Thus, we think ongoing surveillance is essential. Furthermore, we found that the pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak identified by different assessment tools was not significant. Studies have indicated that prevalence identified by screening tools were higher than prevalence identified by diagnostic tools [113]. However, all the included studies in this study were used screening tools, we were unable to explore the difference. It is note of worthy that some instruments derived from different conceptualization of the disorder and they may encompass different symptoms (e.g., Impact of Event Scale-Revised derived from the Diagnostic and Statistical Manual-Fourth Edition, Text Revision (DSM-IV-TR) while Post-Traumatic Stress Disorder Checklist-5 from DSM-5, including more symptoms than the former) [114]. Given that the included articles use many different screening tools, we think further research is needed to explore the influence of different screening tools on the prevalence of PTSD among people influenced by COVID-19 outbreak. It is reported that studies with poor methodological quality generally yielded more extreme prevalence estimates [115], the current study showed similar results. After controlling for other factors, however, the results of meta-regression showed that the influence of methodological quality on prevalence is no longer significant. Hence, this observation requires further clarification.
Implications for the future
Epidemiological studies have demonstrated a rather high prevalence of mental health problems among different population after an epidemic of infectious disease [116–118]. While most of these mental health problems will fade out after the epidemic, symptoms of PTSD may last for a prolonged time and result in severe distress and disability [119]. In terms of applicability to COVID-19, we think ongoing surveillance is essential and healthcare policies need to take into account both short-term and long-term preventive strategy of PTSD. In addition, all the included studies identified PTSD by self-reporting questionnaires rather than clinical interviews by professional psychiatrists, as a consequence of which, the pooled prevalence of PTSD may have been overestimated. Only 6.39% reported data on COVID-19 patients. Thus, we think a large multicenter prospective study using a single validated measure of PTSD and measuring possible confounding factors in randomly selected COVID-19 patients is needed in the future, which would provide a more accurate estimate of PTSD among people influenced by COVID-19 outbreak, especially for COVID-19 patients. Although, there is little doubt that there is a dose–response relationship between the degree of trauma and the mental health burden of disasters [14], this relation may not necessarily mean that the principal mental health burden of people exposed to the trauma resulting from COVID-19 outbreak is among those who were most directly affected by the disease [13]. It will be important to establish whether indirect exposure to a trauma during a COVID-19 pandemic was correlated with higher risk of PTSD. Also, it is necessary to assess the relation between exposure to multiple traumas and risk of PTSD in the future. Additionally, subgroup analyses and the meta-regression analysis did not identify major sources of the heterogeneity although a high degree of heterogeneity between studies was observed. Therefore, there might be a considerable amount of uncertainty regarding the pooled prevalence of PTSD among people influenced by COVID-19 outbreak. Future research should, therefore, explore more potential risk factors for PTSD among people influenced by COVID-19 outbreak, especially genetic background as well as social support, previous traumatic events or concomitant psychiatric disorder [109,120].
Limitations
Firstly, we excluded studies were not written in English or Chinese. Besides, although subgroup analyses and meta-regression analyses were conducted to control many moderating factors for the pooled prevalence of post-traumatic stress symptoms, heterogeneity was still remained in this review. It is reported that heterogeneity is difficult to avoid in meta-analysis of epidemiological surveys, [121] which suggesting the need for caution when drawing inferences about estimates of PTSD in post-disaster research. Additionally, although our study included relevant studies across 30 countries, more than half of the eligible studies were from upper-high income countries. Prevalence studies were scarce for many countries, especially for low-income countries. Considering the inconsistency of the healthcare environment and socioeconomic status across the world, more prevalence studies in low-income countries are needed to understand the panorama of PTSD among people influenced by COVID-19 outbreak. Also, we noticed that all the included studies were used screening tools to assess post-traumatic stress symptoms, no studies included were used diagnostic tools. It is possible that the pooled prevalence of post-traumatic stress symptoms caused by COVID-19 outbreak was overestimated in this review. Thus, we think ongoing surveillance is essential. Lastly, some included studies were investigated the prevalence before the time threshold from the first event (usually 30 days), we were unable to check this possible bias between studies. Although we explored the influence of survey time on the pooled prevalence, no significant result was found, which need further clarification.
Conclusion
This review has highlighted the importance of considering the psychological impacts of people exposed to the trauma resulting from COVID-19 outbreak. A total of 106,713 people exposed to the trauma resulting from the COVID-19 outbreak were identified in the 76 articles, of which 33,810 were reported with post-traumatic stress symptoms. The pooled prevalence of post-traumatic stress symptoms among people exposed to the trauma resulting from COVID-19 outbreak was 28.34%, with a 95% CI of 23.03–34.32%. Further research is needed to explore more possible risk factors for post-traumatic stress symptoms and identify effective strategies for preventing and treating PTSD-related symptoms among people exposed to the trauma resulting from COVID-19 outbreak.
Abbreviations
- 95% CI
95% confidence interval;
- COVID-19
coronavirus disease 2019;
- DSM-5
diagnostic and statistics of mental disorders, the fifth edition;
- IES-6
The Impact of Event Scale-6;
- IES-R
The Impact of Event Scale-Revised;
- ITQ
The International Trauma Questionnaire;
- PCL-5
The Post-Traumatic Stress Disorder Checklist-5;
- PCL-C
The amended self-reported Post-Traumatic Stress Disorder (PTSD) Checklist-Civilian Version;
- PSDI-8
Post-Traumatic Stress Disorder-8 Inventory;
- PTSD
post-traumatic stress disorder;
- PTSD-SS
Post-Traumatic Stress Disorder Self-Rating Scale.
Financial Support
This research was supported by the Ministry of Science and Technology of China (Grant no.: 2016YFC0900802). The funding agency did not take part in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Conflict of Interest
The authors declare no conflicts of interest.
Authorship Contributions
D.Q., S.Y.X., and Y.L.L. contributed to the design of the study. D.Q. and Y.L.L. screened the text. D.Q. and L.L. extracted and analyzed the data. J.H. and F.Y.O.Y. conducted the quality assessment. D.Q. wrote the first draft of the manuscript with input from S.Y.X. All the authors approved the final manuscript.
Data Availability Statement
The data that support the findings of this study are available in Table 1 and the Supplementary Material.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/j.eurpsy.2021.24.
click here to view supplementary material
References
- [1].Organization WH. Coronavirus disease (COVID-19) weekly epidemiological update and weekly operational update, WHO, editor; 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [accessed date: 15, December, 2020].
- [2].Steele L, Orefuwa E, Dickmann P. Drivers of earlier infectious disease outbreak detection: a systematic literature review. Int J Infect Dis. 2016;53:15–20. [DOI] [PubMed] [Google Scholar]
- [3].Gardner PJ, Moallef P. Psychological impact on SARS survivors: critical review of the English language literature. Can Psychol. 2015;56:123–35. [Google Scholar]
- [4].Dutheil F, Mondillon L, Navel V. PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol Med. 2020:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Association AP. Diagnostic and statistical manual of mental disorder, 5th edition(DSM-5). Washington: American Psychiatric Publishing; 2013. [Google Scholar]
- [6].Greene T, Neria Y, Gross R. Prevalence, detection, and correlates of PTSD in the primary care setting: a systematic review. J Clin Psychol Med Settings. 2016;23:160–80. [DOI] [PubMed] [Google Scholar]
- [7].Chang MC, Park D. Incidence of post-traumatic stress disorder after coronavirus disease. Healthcare. 2020;8:373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lahav Y. Psychological distress related to COVID-19—the contribution of continuous traumatic stress. J Affect Disord. 2020;277:129–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bo HX, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. 2020:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Morganstein JC, Ursano RJ. Ecological disasters and mental health: causes, consequences, and interventions. Front Psychiatry. 2020;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Galea S, Resnick H. Post-traumatic stress disorder in the general population after mass terrorist incidents: considerations about the nature of exposure. CNS Spectr. 2005;10:107–15. [DOI] [PubMed] [Google Scholar]
- [14].Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38:467–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Salehi M, Amanat M, Mohammadi M, Salmanian M, Rezaei N, Saghazadeh A, et al. The prevalence of post-traumatic stress disorder related symptoms in Coronavirus outbreaks: a systematic-review and meta-analysis. J Affect Disord. 2021;282:527–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers, and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293:113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cooke JE, Eirich R, Racine N, Madigan S. Prevalence of post-traumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2020;292:113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cenat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad PG, Mukunzi JN, McIntee SE, et al. Prevalence of symptoms of depression, anxiety, insomnia, post-traumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295:113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cai X, Hu XP, Ekumi IO, Wang JC, An YW, Li ZW, et al. Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am J Geriat Psychiat. 2020;28:1030–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Liu D, Baumeister RF, Veilleux JC, Chen C, Liu W, Yue Y, et al. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. 2020;292:113297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- [23].Loney PL, Chambers LW, Bennet KJ, Roberts JG, Stratford PW. Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis Can. 1998;19:170–6. [PubMed] [Google Scholar]
- [24].Sanderson S, Tatt ID, Higgins JP. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. 2007;36:666–76. [DOI] [PubMed] [Google Scholar]
- [25].Qiu D, Yu Y, Li RQ, Li YL, Xiao SY. Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Med. 2020;67:258–66. [DOI] [PubMed] [Google Scholar]
- [26].Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. Am J Public Health. 2019;109:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Zachariae R, Lyby MS, Ritterband LM, O’Toole MS. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia—a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2016;30:1–10. [DOI] [PubMed] [Google Scholar]
- [28].Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making. 2005;25:646–54. [DOI] [PubMed] [Google Scholar]
- [29].Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Higgins J. Cochrane Handbook for systematic reviews of interventions version 6.1; 2020. https://training.cochrane.org/handbook [accessed date: 10, September, 2020].
- [31].Jike M, Itani O, Watanabe N, Buysse DJ, Kaneita Y. Long sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med Rev. 2018;39:25–36. [DOI] [PubMed] [Google Scholar]
- [32].Dai WJ, Liu AZ, Kaminga AC, Deng J, Lai ZW, Yang JZ, et al. Prevalence of acute stress disorder among road traffic accident survivors: a meta-analysis. BMC Psychiatry. 2018;18:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Si MY, Su XY, Jiang Y, Wang WJ, Gu XF, Ma L, et al. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. 2020;9:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Rodriguez-Rey R, Garrido-Hernansaiz H, Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front Psychol. 2020;11:1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J Clin Nurs. 2020;29(21–22):4217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Liang SW, Chen RN, Liu LL, Li XG, Chen JB, Tang SY, et al. The psychological impact of the COVID-19 epidemic on Guangdong college students: the difference between seeking and not seeking psychological help. Front Psychol. 2020;11:2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Li G, Miao J, Wang H, Xu S, Sun W, Fan Y, et al. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J Neurol Neurosurg Psychiatry. 2020;91:895–7. [DOI] [PubMed] [Google Scholar]
- [40].Giusti EM, Pedroli E, D’Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. 2020;11:1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Chen B, Li QX, Zhang H, Zhu JY, Yang X, Wu YH, et al. The psychological impact of COVID-19 outbreak on medical staff and the general public. Curr Psychol. 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Caillet A, Coste C, Sanchez R, Allaouchiche B. Psychological impact of COVID-19 on ICU caregivers. Anaesth Crit Care Pain Med. 2020;39(6):717–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Barbato M, Thomas J. Far from the eyes, close to the heart: psychological impact of COVID-19 in a sample of Italian foreign workers. Psychiatry Res. 2020;290:113113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. 2020;102:152192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Zhou Y, Shi H, Liu Z, Peng S, Wang R, Qi L, et al. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl Psychiatry. 2020;10:319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Zhao YQ, An YY, Tan X, Li XH. Mental health and its influencing factors among self-isolating ordinary citizens during the beginning epidemic of COVID-19. J Loss Trauma. 2020;25:580–93. [Google Scholar]
- [47].Zhang YF, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int J Environ Res Public Health. 2020;17:2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Yin Q, Sun Z, Liu T, Ni X, Deng X, Jia Y, et al. Post-traumatic stress symptoms of health care workers during the corona virus disease 2019. Clin Psychol Psychother. 2020;27:384–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Wesemann U, Hadjamu N, Willmund G, Dolff S, Vonderlin N, Wakili R, et al. Influence of COVID-19 on general stress and post-traumatic stress symptoms among hospitalized high-risk patients. Psychol Med. 2020:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Varshney M, Parel JT, Raizada N, Sarin SK. Initial psychological impact of COVID-19 and its correlates in Indian Community: an online (FEEL-COVID) survey. PLoS One. 2020;15:e0233874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Traunmuller C, Stefitz R, Gaisbachgrabner K, Schwerdtfeger A. Psychological correlates of COVID-19 pandemic in the Austrian population. BMC Public Health. 2020;20:1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020;274:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. 2020;87:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun. 2020;88:60–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Sherman AC, Williams ML, Amick BC, Hudson TJ, Messias EL. Mental health outcomes associated with the COVID-19 pandemic: prevalence and risk factors in a southern US state. Psychiatry Res. 2020;293:113476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Seyahi E, Poyraz BC, Sut N, Akdogan S, Hamuryudan V. The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol Int. 2020;40:1229–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry. 2020;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. Open. 2020;3:e2010185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Riello M, Purgato M, Bove C, MacTaggart D, Rusconi E. Prevalence of post-traumatic symptomatology and anxiety among residential nursing and care home workers following the first COVID-19 outbreak in Northern Italy. Roy Soc Open Sci. 2020;7:200880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Qi R, Chen W, Liu S, Thompson PM, Zhang LJ, Xia F, et al. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: prevalence and associated biopsychosocial risk factors. medRxiv. 2020.
- [62].Ma ZF, Zhang YT, Luo XQ, Li XL, Li YS, Liu SC, et al. Increased stressful impact among general population in mainland China amid the COVID-19 pandemic: a nationwide cross-sectional study conducted after Wuhan city’s travel ban was lifted. Int J Soc Psychiatry. 2020;66:770–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Luceno-Moreno L, Talavera-Velasco B, Garcia-Albuerne Y, Martin-Garcia J. symptoms of post-traumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:5514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Li Y, Wang Y, Jiang J, Valdimarsdottir UA, Fall K, Fang F, et al. Psychological distress among health professional students during the COVID-19 outbreak. Psychol Med. 2020:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Li Y, Qin Q, Sun Q, Sanford LD, Vgontzas AN, Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med. 2020;16:1417–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Li XC, Zhou Y, Xu XY. Factors associated with the psychological well-being among front-line nurses exposed to COVID-2019 in China: a predictive study. J Nurs Manag. 2020;29(2):240–9. [DOI] [PubMed] [Google Scholar]
- [69].Li X, Lu PX, Hu LT, Huang TH, Lu L. Factors associated with mental health results among workers with income losses exposed to COVID-19 in China. Int J Environ Res Public Health. 2020;17:5627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Li Q. Psychosocial and coping responses toward 2019 coronavirus diseases (COVID-19): a cross-sectional study within the Chinese general population. QJM. 2020;113:731–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Leng M, Wei LL, Shi XH, Cao GR, Wei YL, Xu H, et al. Mental distress and influencing factors in nurses caring for patients with COVID-19. Nurs Crit Care. 2020;19(3):14–17. doi: 10.3969/j.issn.1671-8933.2020.03.005. [DOI] [PubMed] [Google Scholar]
- [72].Le XTT, Dang AK, Toweh J, Nguyen QN, Le HT, Do TTT, et al. Evaluating the psychological impacts related to COVID-19 of Vietnamese people under the first nationwide partial lockdown in Vietnam. Front Psychiatry. 2020;11:824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Lange M, Joo S, Couette PA, de Jaegher S, Joly F, Humbert X. Impact on mental health of the COVID-19 outbreak among community pharmacists during the sanitary lockdown period. Ann Pharm Fr. 2020;78:459–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Lai JB, Ma SM, Wang Y, Cai ZX, Hu JB, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Karatzias T, Shevlin M, Murphy J, McBride O, Ben-Ezra M, Bentall RP, et al. Post-traumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: a population-based study. J Trauma Stress. 2020;33(4):365–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Cardel MI, Manasse S, Krukowski RA, Ross K, Shakour R, Miller DR, et al. COVID-19 impacts mental health outcomes and ability/desire to participate in research among current research participants. Obesity. 2020;28(12):2272–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Guo J, Feng XL, Wang XH, van IJzendoorn MH. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int J Environ Res Public Health. 2020;17:3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Gonzalez-Sanguino C, Ausin B, Castellanos MA, Saiz J, Lopez-Gomez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Gonzalez Ramirez LP, Martinez Arriaga RJ, Hernandez-Gonzalez MA, De la Roca-Chiapas JM. Psychological distress and signs of post-traumatic stress in response to the COVID-19 health emergency in a Mexican sample. Psychol Res Behav Manag. 2020;13:589–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Forte G, Favieri F, Tambelli R, Casagrande M. The enemy which sealed the world: effects of COVID-19 diffusion on the psychological state of the Italian population. J Clin Med. 2020;9(6):1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Fekih-Romdhane F, Ghrissi F, Abbassi B, Cherif W, Cheour M. Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatry Res. 2020;290:113131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].El-Zoghby SM, Soltan EM, Salama HM. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J Commun Health. 2020;45:689–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Dobson H, Malpas CB, Burrell AJC, Gurvich C, Chen L, Kulkarni J, et al. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas Psychiatry. 2020;29(1):26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Di Tella M, Romeo A, Benfante A, Castelli L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract. 2020;26:1583–7. [DOI] [PubMed] [Google Scholar]
- [85].Cortes-Alvarez NY, Pineiro-Lamas R, Vuelvas-Olmos CR. Psychological effects and associated factors of COVID-19 in a Mexican sample. Disaster Med Public. 2020;14:413–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Civantos AM, Byrnes Y, Chang CG, Prasad A, Chorath K, Poonia SK, et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: national study. Head Neck-J Sci Spec. 2020;42:1597–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Civantos AM, Bertelli A, Gonçalves A, Getzen E, Chang C, Long Q, et al. Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: a national study. Am J Otolaryngol. 2020;41(6):102694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Chi XL, Becker B, Yu Q, Willeit P, Jiao C, Huang LY, et al. Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the coronavirus disease (COVID-19) pandemic. Front Psychiatry. 2020;11:803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Chew NWS, Ngiam JN, Tan BYQ, Tham SM, Tan CYS, Jing MX, et al. Asian-Pacific perspective on the psychological well-being of healthcare workers during the evolution of the COVID-19 pandemic. Bjpsych Open. 2020;6 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. 2020;131:132–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Blekas A, Voitsidis P, Athanasiadou M, Parlapani E, Chatzigeorgiou AF, Skoupra M, et al. COVID-19: PTSD symptoms in Greek health care professionals. Psychol Trauma. 2020;12:812–9. [DOI] [PubMed] [Google Scholar]
- [92].Zhang YF, Ma ZF. Psychological responses and lifestyle changes among pregnant women with respect to the early stages of COVID-19 pandemic. Int J Soc Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Zhang Y, Liu X, Xue M, Luo L, He G, Feng P, et al. The correlation between post-traumatic stress disorder and perceived stress in suspected COVID-19 patients quarantined in hospital. Chin J Respir Crit Care Med. 2020;19:325–9. [Google Scholar]
- [94].Lijun Z, Sheng C, Lei Y, Qi W, Hongzhi Y. A study on post-traumatic stress reaction to the first-line medical staffs against COVID-19. Health Med Res Pract. 2020;17 15–18. [Google Scholar]
- [95].Yuan B, Cai X, Wang J, Hu X, Li Z, Lu T, et al. Investigation of psychological stress state of during early convalescence of patients with coronavirus disease 2019 and analysis of its influencing factors. Chin J Clin Neurosurg. 2020;25:531–4. [Google Scholar]
- [96].Xie R, Zhu X, Huang X. Anxiety state of ordinary residents under novel coronavirus pneumonia epidemic situation and related factors of emergency level. China J Health Psychol. 2020;28:1670–4. [Google Scholar]
- [97].Liu Y, Jiang P, Cao Y, Zhou Y, Li Y. Investigation on the psychological stress of nursing staff during the novel coronavirus pneumonia epidemic and analysis of related factors. Nurs Integr Trad Chin Weste Med. 2020;6:179–83. [Google Scholar]
- [98].Liu X, Lin Z, Zhu H, Zhan D, Han T, Yao Q. Investigation of mental health status of medical stuff from hainan who aided Hubei Province to fight against COVID-19. J Hanan Med Univ. 2020;26:1285–8. [Google Scholar]
- [99].Leng F. Correlation analysis of anxiety, depression, and post-traumatic stress disorder among frontline nurses fighting against new coronavirus pneumonia. J Clin Nurs. 2020;19:14–7. [Google Scholar]
- [100].Chen M, Yue F, Liu G. Investigation and study on mental status among first line nurses against new type coronavirus pneumonia epidemic under systematic support. J Mod Med Health. 2020;36:2671–4. [Google Scholar]
- [101].Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case–control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, et al. The effect of COVID-19 on youth mental health. Psychiatr Q. 2020;91:841–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Li c, Mi Y, Chu J, Zhu L, Zhang Z, Liang L, et al. Post-traumatic stress disorder of frontline nurses for COVID-19. J Nurses Train. 2020;35:615; –8. [Google Scholar]
- [104].Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:192–5. [DOI] [PubMed] [Google Scholar]
- [105].Sands ML, Murphy JR. Use of kappa statistic in determining validity of quality filtering for meta-analysis: a case study of the health effects of electromagnetic radiation. J Clin Epidemiol. 1996;49:1045–51. [DOI] [PubMed] [Google Scholar]
- [106].Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the world mental health surveys. Psychol Med. 2017;47:2260–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Wang Z, Wu X, Dai W, Kaminga AC, Wu X, Pan X, et al. The prevalence of post-traumatic stress disorder among survivors after a typhoon or hurricane: a systematic review and meta-analysis. Disaster Med Public Health Prep. 2019;13:1065–73. [DOI] [PubMed] [Google Scholar]
- [108].Liu H, Petukhova MV, Sampson NA, Aguilar-Gaxiola S, Alonso J, Andrade LH, et al. Association of DSM-IV post-traumatic stress disorder with traumatic experience type and history in the world health organization world mental health surveys. JAMA Psychiatry. 2017;74:270–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Dai W, Chen L, Lai Z, Li Y, Wang J, Liu A. The incidence of post-traumatic stress disorder among survivors after earthquakes:a systematic review and meta-analysis. BMC Psychiatry. 2016;16:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Del Sole F, Farcomeni A, Loffredo L, Carnevale R, Menichelli D, Vicario T, et al. Features of severe COVID-19: a systematic review and meta-analysis. Eur J Clin Invest. 2020;50:e13378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Righy C, Rosa RG, da Silva RTA, Kochhann R, Migliavaca CB, Robinson CC, et al. Prevalence of post-traumatic stress disorder symptoms in adult critical care survivors: a systematic review and meta-analysis. Crit Care. 2019;23:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Heron-Delaney M, Kenardy J, Charlton E, Matsuoka Y. A systematic review of predictors of post-traumatic stress disorder (PTSD) for adult road traffic crash survivors. Injury. 2013;44:1413–22. [DOI] [PubMed] [Google Scholar]
- [113].Edmondson D, Richardson S, Fausett JK, Falzon L, Howard VJ, Kronish IM. Prevalence of PTSD in survivors of stroke and transient ischemic attack: a meta-analytic review. PLoS One. 2013;8:e66435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [114].Murphy D, Ross J, Ashwick R, Armour C, Busuttil W. Exploring optimum cut-off scores to screen for probable post-traumatic stress disorder within a sample of UK treatment-seeking veterans. Eur J Psychotraumatol. 2017;8:1398001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, et al. Prevalence of depression and depressive symptoms among resident physicians a systematic review and meta-analysis. JAMA-J Am Med Assoc. 2015;314:2373–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Tucci V, Moukaddam N, Meadows J, Shah S, Galwankar SC, Kapur GB. The forgotten plague: psychiatric manifestations of Ebola, Zika, and emerging infectious diseases. J Glob Infect Dis. 2017;9:151–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [117].Catalan J, Harding R, Sibley E, Clucas C, Croome N, Sherr L. HIV infection and mental health: suicidal behaviour—systematic review. Psychol Health Med. 2011;16:588–611. [DOI] [PubMed] [Google Scholar]
- [118].Hong X, Currier GW, Zhao X, Jiang Y, Zhou W, Wei J. Post-traumatic stress disorder in convalescent severe acute respiratory syndrome patients: a 4-year follow-up study. Gen Hosp Psychiatry. 2009;31:546–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Vyas KJ, Delaney EM, Webb-Murphy JA, Johnston SL. Psychological impact of deploying in support of the U.S. response to Ebola: a systematic review and meta-analysis of past outbreaks. Mil Med. 2016;181:e1515–31. [DOI] [PubMed] [Google Scholar]
- [120].Koenen KC, Nugent NR, Amstadter AB. Gene-environment interaction in post-traumatic stress disorder: review, strategy, and new directions for future research. Eur Arch Psychiatry Clin Neurosci. 2008;258:82–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Winsper C, Ganapathy R, Marwaha S, Large M, Birchwood M, Singh SP. A systematic review and meta-regression analysis of aggression during the first episode of psychosis. Acta Psychiatr Scand. 2013;128:413–21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/j.eurpsy.2021.24.
click here to view supplementary material
Data Availability Statement
The data that support the findings of this study are available in Table 1 and the Supplementary Material.