Abstract
Objective
Case-based collaborative learning (CBCL) models that incorporate learner-guided content review, structured preparatory assessment, and interactive case-based classroom sessions have been shown to promote content mastery among medical students. However, limited research has explored the viability of CBCL in resident populations, particularly in dermatology. We therefore sought to investigate the impact of a CBCL curriculum covering complex medical dermatology topics on resident knowledge and learning preferences.
Methods
This prospective cohort study included dermatology and combined internal medicine-dermatology resident trainees of all levels (postgraduate years 2–5) in a single residency program in Boston, Massachusetts. Four CBCL sessions covering complex medical dermatology topics were delivered to program residents between March and April 2019. Preparatory material for each session included a 20-minute concept video and a multiple-choice readiness assessment. During the sessions, residents applied their nascent understanding to newly introduced clinical vignettes and cases covering the preassigned materials. To assess knowledge and learner preferences, 15-question surveys were administered before and immediately after curriculum delivery. Changes in knowledge and learner preferences were determined using Student t tests to compare means and χ2 tests to compare proportions.
Results
Of the 30 residents, 29 (96.7%) completed the precurriculum survey and 17 (56.7%) completed the postcurriculum survey. Mean content scores improved significantly (p < .01) from presession (x̅ 5.70; σ 1.88) to postsession (x̅ 9.71; σ 1.88). The majority of respondents indicated a preference for future CBCL sessions, with learning preferences remaining stable over time.
Conclusion
In this single-center prospective cohort study, resident knowledge improved significantly after CBCL curriculum delivery. Most resident learners viewed the curriculum as worthwhile and preferred it to traditional lecture-based didactics. Collectively, our findings suggest that CBCL models can be feasibly implemented and durably convey complex content to resident learners.
Keywords: Dermatology resident education, Case-based collaborative learning, Graduate medical education, Medical education, Complex medical dermatology
Introduction
Over the last decade, case-based collaborative learning (CBCL) models and other curricular structures combining learner-guided content review, structured preparatory assessment, and case-based classroom activities have become the dominant educational paradigm in U.S. medical schools, propelled by a growing body of literature suggesting that these types of curricula enhance content mastery and foster engagement (Al-Azri and Ratnapalan, 2014, Burgess et al., 2014, Chen et al., 2017, Hew and Lo, 2018, Koh et al., 2008, Krupat et al., 2016, Lin and Hwang, 2018, Ramnanan and Pound, 2017, Schmidt et al., 2011, Zeng et al., 2017). However, similar changes have not occurred in graduate medical education (King et al., 2019, Wittich et al., 2018). Despite data indicating variable knowledge transfer with lecture-based didactics, residency programs continue to rely heavily on this approach (FitzGerald and Wenger, 2003, King et al., 2019, Picciano et al., 2003, Winter et al., 2007, Wittich et al., 2018, Woodfield and Mainiero, 2008). Limited research has explored the viability of CBCL curricula in resident populations, particularly in dermatology (Allenbaugh et al., 2019, Boespflug et al., 2015, Dolan et al., 2015, Graham et al., 2019, Kerfoot et al., 2007, Liu et al., 2019, Martinelli et al., 2017, Muzumdar et al., 2019, Young et al., 2014).
During training, residents must continuously juggle knowledge acquisition and clinical responsibilities, integrating these two domains where appropriate. In this setting, CBCL curricula may prove uniquely useful because CBCL sessions intrinsically explore content within a team-based clinical context (Haemel et al., 2019, Krupat et al., 2016, Maudsley, 1999, Parmelee et al., 2012). Among undergraduate medical students, randomized controlled trials have demonstrated the CBCL format to be a viable, engaging, active learning method that may be of particular benefit to learners with lower academic performance (Krupat et al., 2016). Recently, several small studies evaluating curricular structures at the graduate level with CBCL components also demonstrated efficacy for selected surgical skills and dermatopathology topics, underscoring the potential benefits of this approach for a variety of learners (Liu et al., 2019, Muzumdar et al., 2019). However, whether CBCL teaching models have a broader utility for content areas such as complex medical dermatology remains unknown. To better support trainees in an era of dermatology defined by rapidly changing immunomodulatory therapies and new paradigms of disease management, more information about the generalizability of CBCL approaches to these domains is needed.
We sought to address this gap by investigating the impact of a complex medical dermatology CBCL curriculum on resident knowledge and learning preferences. Specifically, we implemented four CBCL sessions in the residency program at our institution covering systemic medication use in a range of disorders, including bullous disorders, neoplastic disease, and inflammatory dermatoses. We assessed resident knowledge and learning preferences before and after curriculum delivery, hypothesizing that residents would demonstrate stable content retention and prefer the CBCL curriculum to traditional lecture.
Methods
Setting
We obtained approval from the Partners Health Institutional Review Board for this prospective cohort study. Between March and April 2019, we implemented four CBCL sessions in the Harvard Combined Dermatology Residency program, a large subspecialty program of 30 resident trainees in Dermatology and Combined Internal Medicine-Dermatology in Boston, Massachusetts. At baseline, this group of learners received 8 hours of didactic instruction per week, delivered by faculty or peers. Although no institutional rules existed dictating didactic structure, prior to intervention implementation, sessions were predominantly lecture-based, with limited opportunities in several sections (journal club, dermatopathology) for large-group discussion. No preexisting sessions used a CBCL structure.
Curriculum development
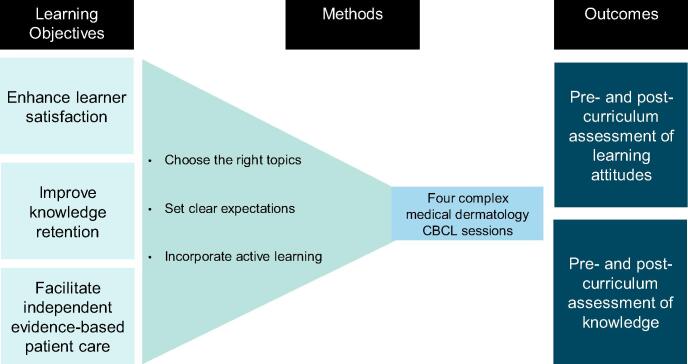
The curriculum included four 1-hour CBCL sessions focused on systemic medication use in a range of disorders, including bullous disorders, neoplastic disease, and inflammatory dermatoses. These topics were identified by a panel of residents, administrators, and faculty as areas of complex dermatology meriting additional didactic sessions. Curriculum development for the four sessions began with identification of three core learning objectives: enhancing learner satisfaction, improving knowledge retention, and facilitating independent, evidence-based patient care (Fig. 1; Frank et al., 2010, Moore et al., 2006). Using a backwards design model, these objectives were used to identify optimal methods for content delivery and to develop outcome measures. The content of the first three sessions included novel material, with each presenting a discrete group of diseases with overlapping pathophysiology and management (i.e., inflammatory dermatoses). The final consolidative session interleaved material from the three prior sessions, illuminating central themes and facilitating the application of foundational concepts to new clinical contexts (Krupat et al., 2016).
Fig. 1.
Model of curriculum design. CBCL, case-based collaborative learning.
The structure of all four sessions fulfilled the core tenets of the CBCL teaching model. Before each session, residents reviewed a 20-minute concept video (Suppl. Fig. S1; Kim et al., 2018, Krathen et al., 2012, Lopez et al., 2018, Talpur et al., 2012) and completed a set of multiple-choice questions (“readiness assessment exercise”) to ensure adequate preparation (Suppl. Fig. S2; Kim et al., 2018, Krupat et al., 2016, Martinelli et al., 2017). During each session, residents applied this content to novel cases and clinical vignettes, first in small teams and then with the entire group of learners (Suppl. Fig. S3; Kim et al., 2018).
Curriculum assessment
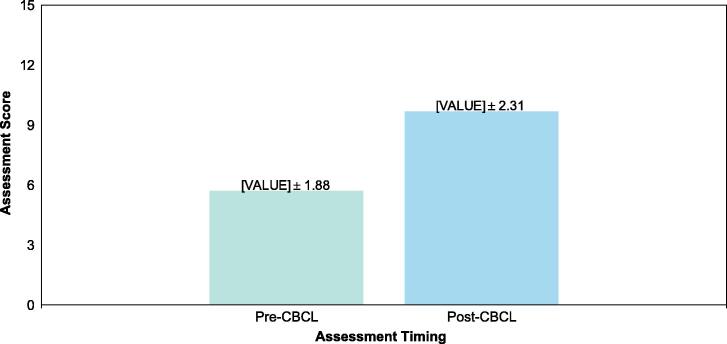
To determine whether curricular learning objectives were met, resident learners completed assessments of their knowledge and learning preferences before and after curriculum delivery (Fig. 2; Suppl. Figs. S2 and S4; Kim et al., 2018). All assessments contained 15 content-related questions of comparable difficulty evaluating resident knowledge developed by program faculty. All assessments also contained items related to learning preferences. These items asked learners to use a five-point Likert agreement scale (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree) to express whether they believed traditional lectures were a good use of time, whether CBCL sessions were a good use of time, and whether they preferred CBCL to traditional sessions. Residents were entered into a drawing for a $20 gift card to the hospital coffee shop for completing each survey.
Fig. 2.
Knowledge scores before and after CBCL delivery. CBCL, case-based collaborative learning.
Statistical analyses
We used descriptive statistics to summarize residents’ assessment responses before and after CBCL curriculum delivery. We determined change over time in resident knowledge and learning preferences using Student t tests for comparison of means and χ2 tests for comparison of proportions. All statistical analyses were performed with STATA (version 16, StataCorp, College Station, TX).
Results
Thirty residents participated in the CBCL curriculum. Demographic and training characteristics are detailed in Table 1. Of these 30 participants, 29 (96.7%) completed the precurriculum assessment and 17 (56.7%) the postcurriculum assessment. Mean scores on the 15-point knowledge assessment improved significantly (p < .001) from a presession score of 5.70 (standard deviation: 1.88) to a postsession score of 9.71 (standard deviation: 1.88; Fig. 2). Prior to curriculum delivery, most resident learners (79.0%) characterized CBCL sessions as a valuable use of time, but only a quarter (27.6%) viewed traditional lectures as similarly worthy of didactic time. On initial assessment, most learners (52.0%) also preferred CBCL sessions to traditional lectures (Table 2). Interestingly, response rates across both the pre- and postsession assessments were higher among residents with stable negative attitudes toward the CBCL intervention, resulting in a sequentially greater representation of this group in the sample. However, the overall distribution of learning preferences remained stable over time, without statistically significant differences observed across assessments.
Table 1.
Learner demographics.
| Characteristic | Finding, n (%) |
|---|---|
| Resident, n | 30 |
| Sex | |
| Female | 17 (56.7) |
| Male | 13 (43.3) |
| Class year | |
| PGY-2 | 9 (30.0) |
| PGY-3 | 10 (33.3) |
| PGY-4 | 9 (30.0) |
| PGY-5 | 2 (6.7) |
PGY, postgraduate year.
Table 2.
Learning preferences before and after CBCL curriculum implementation.
| Learning preference | Before CBCL | After CBCL | ppre→posta |
|---|---|---|---|
| CBCL worthwhile, n (%)b | |||
| Yes | 23 (79.3) | 13 (76.5) | 0.820 |
| Neutral | 3 (10.3) | 2 (11.8) | |
| No | 3 (10.3) | 2 (11.8) | |
| Traditional worthwhile, n (%)c | |||
| Yes | 8 (48.3) | 5 (29.4) | 0.138 |
| Neutral | 9 (34.5) | 6 (35.3) | |
| No | 12 (17.2) | 6 (35.3) | |
| Prefer CBCL to traditional, n (%)d | |||
| Yes | 15 (51.7) | 9 (52.9) | 0.938 |
| Neutral | 9 (31.0) | 4 (23.5) | |
| No | 5 (17.2) | 4 (23.5) |
CBCL, case-based collaborative learning curriculum.
Likert responses of strongly disagree (1) and disagree (2) were aggregated as a “no” response, neutral (3) was preserved as a “neutral” response, and agree (4) and strongly agree (5) were aggregated as a “yes” response.
p-value when comparing proportion of respondents with each answer response before and after CBCL implementation.
Resident responses to the question “Are CBCL sessions are a good use of time?”
Resident responses to the question “Are traditional lectures are a good use of time?”
Resident responses to the question “Do you prefer CBCL sessions to traditional lectures?”
Discussion
In this prospective study of resident learners, we assessed the impact of a CBCL curriculum covering a range of complex dermatology topics on resident knowledge and learning preferences. We found that the CBCL curriculum significantly improved resident knowledge of systemic medication uses in bullous disease, lymphoma, and inflammatory dermatoses. Notably, most resident learners also viewed the curriculum as a valuable use of time and preferred this approach to traditional lecture. Collectively, these results demonstrate that CBCL can feasibly be implemented in residency programs to teach complex dermatology topics and enhance learner engagement.
Current training models require trainees to rapidly master a panoply of immunomodulatory therapies to manage the care of patients with rheumatology, oncology, and dermatology disorders. Encouragingly, our findings suggest that CBCL curricula using active learning strategies can efficiently convey this dynamic content, particularly among younger trainees, who may face the steepest learning curve. Notably, the curriculum demonstrated knowledge acquisition while simultaneously requiring <20 minutes of resident preparation per session, highlighting the potential longitudinal efficiency of this approach.
Given potential linkages between trainees’ perceptions of their learning environment and burnout, refining dermatology resident didactic curricula to incorporate more CBCL sessions may not only enhance knowledge but also contribute to resident well-being (van Vendeloo et al., 2018a, van Vendeloo et al., 2018b). Concerningly, we found that less than half of resident respondents viewed traditional lectures as a valuable use of time, suggesting that traditional didactic approaches may not provide optimal support from the perspective of some trainees. In contrast, the CBCL intervention was stably characterized by most trainees as valuable, corroborating prior work (Chen et al., 2017). Collectively, these findings suggest that CBCL may offer benefits beyond content mastery, fostering a greater sense of curricular investment and belief in educational efficacy among trainees.
Several limitations of this study merit discussion. With regard to our study population, we drew our sample from a single dermatology residency program, which may limit the generalizability of our findings. In addition, the proportion of respondents completing session assessments sequentially declined, which may have introduced an element of response bias into the data. With regard to the intervention, the four-session CBCL curriculum focused on a small number of content areas, and so the broader applicability of our findings to other domains of dermatology remains unknown. The 15-question content assessments were also written by unblinded faculty who teach in the dermatology residency program, introducing the potential for observer effects or confirmation bias. Finally, although our dermatology program is one of the largest in the country, the sample size of our cohort was still relatively small. Given our cohort size, we were unable to perform a randomized trial of our CBCL intervention, limiting our ability to account for background contributors such as secular trends of knowledge attainment in residency. Although we could not directly compare knowledge acquisition in intervention and control groups, our study design did allow us to directly compare resident learners’ preferences for one learning model over another; in this domain, residents exhibited a clear preference for CBCL over didactic lectures.
Future work should investigate CBCL curricula for a broader array of dermatologic content. Isolating specific CBCL components may also provide more granular information about the relative value of different curricular interventions, which could further support residency directors in optimizing their educational efforts toward improving didactic curricula. Given the duration of clinical careers, examining longer-term learning outcomes would also be beneficial. By providing a novel indication of the benefits of a CBCL curriculum for a range of complex medical dermatology topics at the resident level, we hope our work provides scaffolding for these important future investigations.
Acknowledgments
Acknowledgements
The authors thank the Harvard dermatology program’s leadership and residents who participated and for their willingness to allow this work to occur.
Conflicts of interest
None.
Funding
None.
Study Approval
The author(s) confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies.
Footnotes
Meeting presentation: This study was presented in abstract form at the 2019 Association of Professors of Dermatology Annual Meeting, held on September 13 and 14, 2019 in Chicago, Illinois.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijwd.2020.06.002.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Al-Azri H., Ratnapalan S. Problem-based learning in continuing medical education: review of randomized controlled trials. Can Fam Physician. 2014;60(2):157–165. [PMC free article] [PubMed] [Google Scholar]
- Allenbaugh J., Spagnoletti C., Berlacher K. Effects of a flipped classroom curriculum on inpatient cardiology resident education. J Grad Med Educ. 2019;11(2):196–201. doi: 10.4300/JGME-D-18-00543.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boespflug A., Guerra J., Dalle S., Thomas L. Enhancement of customary dermoscopy education with spaced education e-learning. JAMA Dermatol. 2015;151(8):847. doi: 10.1001/jamadermatol.2015.0214. [DOI] [PubMed] [Google Scholar]
- Burgess A.W., McGregor D.M., Mellis C.M. Applying established guidelines to team-based learning programs in medical schools: a systematic review. Acad Med. 2014;89(4):678–688. doi: 10.1097/ACM.0000000000000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Lui A.M., Martinelli S.M. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017;51(6):585–597. doi: 10.1111/medu.13272. [DOI] [PubMed] [Google Scholar]
- Dolan B.M., Yialamas M.A., McMahon G.T. A randomized educational intervention trial to determine the effect of online education on the quality of resident-delivered care. J Grad Med Educ. 2015;7(3):376. doi: 10.4300/JGME-D-14-00571.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FitzGerald J.D., Wenger N.S. Didactic teaching conferences for IM residents: Who attends, and is attendance related to medical certifying examination scores? Acad Med. 2003;78(1):84–89. doi: 10.1097/00001888-200301000-00015. [DOI] [PubMed] [Google Scholar]
- Frank J.R., Snell L.S., Cate O.T., Holmboe E.S., Carraccio C., Swing S.R. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638–645. doi: 10.3109/0142159X.2010.501190. [DOI] [PubMed] [Google Scholar]
- Graham K.L., Cohen A., Reynolds E.E., Huang G.C. Effect of a flipped classroom on knowledge acquisition and retention in an internal medicine residency program. J Grad Med Educ. 2019;11(1):92–97. doi: 10.4300/JGME-D-18-00536.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haemel A., Kahl L., Callen J., Werth V.P., Fiorentino D., Fett N. Supplementing dermatology physician resident education in vasculitis and autoimmune connective tissue disease: a prospective study of an online curriculum. JAMA Dermatol. 2019;155(3):381. doi: 10.1001/jamadermatol.2018.4837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hew K., Lo C. Flipped classroom improves student learning in health professions education: S meta-analysis. BMC Med Educ. 2018;18(1):38. doi: 10.1186/s12909-018-1144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerfoot B.P., Baker H.E., Koch M.O., Connelly D., Joseph D.B., Ritchey M.L. Randomized, controlled trial of spaced education to urology residents in the United States and Canada. J Urol. 2007;177(4):1481–1487. doi: 10.1016/j.juro.2006.11.074. [DOI] [PubMed] [Google Scholar]
- Kim Y.H., Bagot M., Pinter-Brown L., Rook A.H., Porcu P., Horwitz S.M. Mogamulizumab versus vorinostat in previously treated cutaneous T-cell lymphoma (MAVORIC): an international, open-label, randomised, controlled phase 3 trial. Lancet Oncol. 2018;19(9):1192–1204. doi: 10.1016/S1470-2045(18)30379-6. [DOI] [PubMed] [Google Scholar]
- King A.M., Gottlieb M., Mitzman J., Dulani T., Schulte S.J., Way D.P. Flipping the classroom in graduate medical education: a systematic review. J Grad Med Educ. 2019;11(1):18–29. doi: 10.4300/JGME-D-18-00350.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh G.C., Khoo H.E., Wong M.L., Koh D. The effects of problem-based learning during medical school on physician competency: a systematic review. Can Med Assoc J. 2008;178(1):34–41. doi: 10.1503/cmaj.070565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krathen M., Sundram U., Bashey S., Sutherland K., Salva K., Wood G.S. Brentuximab vedotin demonstrates significant clinical activity in relapsed or refractory mycosis fungoides with variable CD30 expression. Blood. 2012;120(21):797. [Google Scholar]
- Krupat E., Richards J.B., Sullivan A.M., Fleenor T.J., Schwartzstein R.M. Assessing the effectiveness of case-based collaborative learning via randomized controlled trial. Acad Med. 2016;91(5):723–729. doi: 10.1097/ACM.0000000000001004. [DOI] [PubMed] [Google Scholar]
- Lin H.C., Hwang G.J. Research trends of flipped classroom studies for medical courses: a review of journal publications from 2008 to 2017 based on the technology-enhanced learning model. Interact Learn Environ. 2018:1–17. [Google Scholar]
- Liu K.J., Tkachenko E., Waldman A., Boskovski M.T., Hartman R.I., Levin A.A. A video-based, flipped-classroom, simulation curriculum for dermatologic surgery: a prospective, multi-institution study. J Am Acad Dermatol. 2019;81(6):1271–1276. doi: 10.1016/j.jaad.2019.03.078. [DOI] [PubMed] [Google Scholar]
- Lopez A.T., Bates S., Geskin L. Current status of HDAC inhibitors in cutaneous T-cell lymphoma. Am J Clin Dermatol. 2018;19(6):805–819. doi: 10.1007/s40257-018-0380-7. [DOI] [PubMed] [Google Scholar]
- Martinelli S.M., Chen F., DiLorenzo A.N., Mayer D.C., Fairbanks S., Moran K. Results of a flipped classroom teaching approach in anesthesiology residents. J Grad Med Educ. 2017;9(4):485–490. doi: 10.4300/JGME-D-17-00128.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maudsley G. Do we all mean the same thing by “problem-based learning”? A review of the concepts and a formulation of the ground rules. Acad Med. 1999;74(2):178–185. doi: 10.1097/00001888-199902000-00016. [DOI] [PubMed] [Google Scholar]
- Moore M.M., Geller A.C., Zhang Z., Hayes B.B., Bergstrom K., Graves J.E. Skin cancer examination teaching in U.S. medical education. Arch Dermatol. 2006;142(4):439–444. doi: 10.1001/archderm.142.4.439. [DOI] [PubMed] [Google Scholar]
- Muzumdar S., Waldman R.A., Grant-Kels J.M., Kerr P. Implementing the flipped classroom approach to dermatopathology and dermoscopy resident education: a single-institution experience. J Cutan Pathol. 2019;1(1):753–755. doi: 10.1111/cup.13515. [DOI] [PubMed] [Google Scholar]
- Parmelee D., Michaelsen L.K., Cook S., Hudes P.D. Team-based learning: a practical guide: AMEE guide no. 65. Med Teach. 2012;34(5):e275–e287. doi: 10.3109/0142159X.2012.651179. [DOI] [PubMed] [Google Scholar]
- Picciano A., Winter R., Ballan D., Birnberg B., Jacks M., Laing E. Resident acquisition of knowledge during a noontime conference series. Fam Med. 2003;35(6):418–422. [PubMed] [Google Scholar]
- Ramnanan C.J., Pound L.D. Advances in medical education and practice: student perceptions of the flipped classroom. Adv Med Educ Pract. 2017;8:63–73. doi: 10.2147/AMEP.S109037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt H.G., Rotgans J.I., Yew E.H.J. The process of problem-based learning: what works and why. Med Educ. 2011;45(8):792–806. doi: 10.1111/j.1365-2923.2011.04035.x. [DOI] [PubMed] [Google Scholar]
- Talpur R., Singh L., Daulat S., Liu P., Seyfer S., Trynosky T. Long-term outcomes of 1263 patients with mycosis fungoides and sézary syndrome from 1982 to 2009. Clin Cancer Res. 2012;18(18):5051–5060. doi: 10.1158/1078-0432.CCR-12-0604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Vendeloo S.N., Godderis L., Brand P.L.P., Verheyen K.C.P.M., Rowell S.A., Hoekstra H. Resident burnout: evaluating the role of the learning environment. BMC Med Educ. 2018;18(1):54. doi: 10.1186/s12909-018-1166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Vendeloo S.N., Prins D.J., Verheyen C.C.P.M., Prins J.T., van den Heijkant F., van der Heijden F.M.M.A. The learning environment and resident burnout: a national study. Perspect Med Educ. 2018;7(2):120–125. doi: 10.1007/s40037-018-0405-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winter R.O., Picciano A., Birnberg B., Chae M., Chae S., Jacks M. Resident knowledge acquisition during a block conference series. Fam Med. 2007;39(7):498–503. [PubMed] [Google Scholar]
- Wittich C.M., Agrawal A., Wang A.T., Halvorsen A.J., Mandrekar J.N., Chaudhry S. Flipped classrooms in graduate medical education. Acad Med. 2018;93(3):471–477. doi: 10.1097/ACM.0000000000001776. [DOI] [PubMed] [Google Scholar]
- Woodfield C.A., Mainiero M.B. Radiology resident dictation instruction: effectiveness of the didactic lecture. J Am Coll Radiol. 2008;5(7):842–846. doi: 10.1016/j.jacr.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Young T., Bailey C., Guptill M., Thorp A., Thomas T. The flipped classroom: a modality for mixed asynchronous and synchronous learning in a residency program. West J Emerg Med. 2014;15(7):938–944. doi: 10.5811/westjem.2014.10.23515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng R., Xiang L., Zeng J., Zuo C. Applying team-based learning of diagnostics for undergraduate students: assessing teaching effectiveness by a randomized controlled trial study. Adv Med Educ Pract. 2017;8:211–218. doi: 10.2147/AMEP.S127626. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.