Dear Editors,
A 70-year-old immunocompetent Korean woman living in southern California presented for a second opinion regarding a recalcitrant 7-year facial rash. The rash started as a burning sensation, and the patient then developed swelling and redness on the lower forehead and eyelids, followed by persistent bumps. She had no history of similar lesions. The patient denied systemic symptoms, external trauma, or travel prior to the rash onset. Her medical history was noncontributory. Prior to presentation to our clinic, topical mometasone, triamcinolone, desonide, pimecrolimus, metronidazole, oral doxycycline, and prednisone had previously been tried. Topical and oral steroids reduced the redness and swelling temporarily, but never fully resolved the rash.
Edematous erythematous plaques, some crusted, and discrete eroded erythematous papules were present centrofacially on the patient’s forehead, nose, and cheeks. (Fig. 1A and B). The differential diagnosis included papulopustular rosacea, pyoderma faciale, cutaneous T-cell lymphoma, and actinic prurigo.
Fig. 1.
(A) Edematous erythematous plaques, some crusted; (B) discrete eroded erythematous papules located centrofacially on the patient’s forehead, nose, and cheeks; and (C) facial rash improvement after 1 month of oral fluconazole.
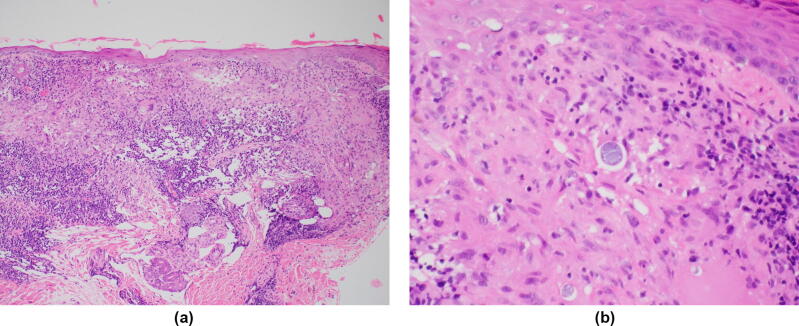
A punch biopsy revealed dermal granulomatous inflammation with focal microabscess formation (Fig. 2A), and a high-power examination showed thick-walled spherules within multi-nucleated giant cells, consistent with Coccidioides organisms (Fig. 2B). A chest radiograph and urine Coccidioides antigen, serum immunoglobulins G and M Coccidioides antibodies, and Coccidioides quantitative antigen tests were all negative. Of note, serological tests may not become positive for weeks after infection, and both urine and serological tests may remain negative in patients without extensive infection (Galgiani et al., 2016). HIV test was negative, and given that the patient was otherwise healthy without systemic systems, further work-up for underlying immunosuppression was not pursued. Based on the patient’s test results, a diagnosis of primary cutaneous coccidioidomycosis was made. Further testing for other fungi was not performed. The patient may have sustained traumatic inoculation on her face; however, she could not recall any specific incident prior to the onset of the rash, which was more than 7 years ago.
Fig. 2.
(A) Dermal granulomatous inflammation with focal microabscess formation (10×, hematoxylin and eosin stain); and (B) high-power examination showing thick-walled spherules within multi-nucleated giant cells, consistent with Coccidioides (40×, hematoxylin and eosin stain).
Coccidioidomycosis, also known as San Joaquin Valley Fever, is a mycosis caused by Coccidioides immitis and Coccidiodies posadasii. These dimorphic fungi are endemic to soil in semiarid to arid areas of the southwestern United States, Mexico, Central America, and South America (Garcia Garcia et al., 2015). Infections most commonly occur via inhalation of airborne arthroconidia. Coccidioidomycosis has a wide range of systemic manifestations, with pulmonary disease being the most common (Garcia Garcia et al., 2015). The patient resides in southern California, which is an endemic location for coccidioidomycosis (Garcia Garcia et al., 2015).
Cutaneous coccidioidomycosis without systemic involvement is rare and has been reported as nodules and plaques, sometimes ulcerated. Patients may report a history of trauma, such as cactus thorn implantation (Chang et al., 2003). The gold standard for diagnosis is either histologic identification showing double-walled 10–80 μm spherules containing endospores, barrel-shaped arthroconidia, or septate hyphae, or isolation of Coccidioides organisms in culture (Garcia Garcia et al., 2015, Laniado-Laborin et al., 2012). When dermatologists encounter cutaneous coccidioidomycosis, testing for systemic disease, which includes a chest radiograph and serologic tests, is warranted. History of skin trauma and systemic symptoms (cough, fever, night sweats, arthralgia, and pleuritic pain) should be queried. A skin examination for reactive cutaneous manifestations, such as erythema nodosum or erythema multiforme, should also be performed (Laniado-Laborin et al., 2012).
Patients with cutaneous coccidioidomycosis are frequently treated with fluconazole or itraconazole with consideration for amphotericin B in severe cases (Garcia Garcia et al., 2015). Our patient was treated with oral fluconazole 400 mg daily for 6 months, and her facial rash improved drastically after just 1 month of treatment (Fig. 1C). This case highlights the importance of clinicopathologic correlation and serves as a reminder to biopsy recalcitrant facial rashes even though the face is a cosmetically sensitive area.
Conflicts of Interest
None.
Funding
None.
Study Approval
N/A.
References
- Chang A., Tung R.C., McGillis T.S., Bergfeld W.F., Taylor J.S. Primary cutaneous coccidioidomycosis. J Am Acad Dermatol. 2003;49(5):944–949. doi: 10.1016/s0190-9622(03)00462-6. [DOI] [PubMed] [Google Scholar]
- Galgiani J.N., Ampel N.M., Blair J.E., Catanzaro A., Geertsma F., Hoover S.E. 2016 Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of Coccidioidomycosis. Clin Infect Dis. 2016;63(6):e112–e146. doi: 10.1093/cid/ciw360. [DOI] [PubMed] [Google Scholar]
- Garcia Garcia S.C., Salas Alanis J.C., Gomez Flores M., Gonzalez Gonzalez S.E., Vera Cabrera L., Ocampo C.J. Coccidioidomycosis and the skin: A comprehensive review. An Bras Dermatol. 2015;90(5):610–621. doi: 10.1590/abd1806-4841.20153805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laniado-Laborin R., Alcantar-Schramm J.M., Cazares-Adame R. Coccidioidomycosis: An update. Curr Fungal Infect Rep. 2012;6(2):113–120. [Google Scholar]