Abstract
Background: Despite the recognized benefits of telemedicine use for pediatric emergency consultations, there are barriers to the widespread uptake of this technology. Quality improvement methods can be used to rapidly test implementation strategies. Our objective was to test telemedicine implementation strategies in real-world application using quality improvement methods. Our quality improvement aim was to achieve high rates of telemedicine use for pediatric transfer consultations.
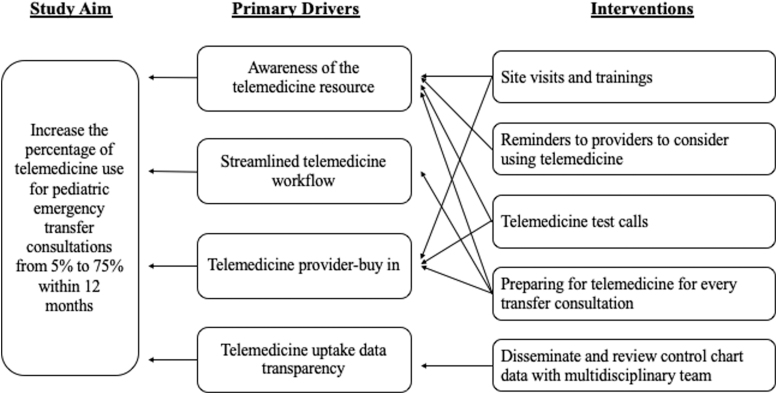
Methods: A multidisciplinary multisite improvement team identified that key drivers of increasing telemedicine use included telemedicine resource awareness, streamlined telemedicine workflow, provider buy-in, and data transparency. Interventions focused on telemedicine trainings, disseminating telemedicine uptake data, telemedicine reminders, telemedicine test calls, and preparing for telemedicine use for every transfer consultation. The outcome measure was percentage of pediatric emergency transfer consultations that used telemedicine. The balancing measure was time (minutes) from the initial transfer center call to completion of the consultation.
Results: Multiple plan-do-study-act cycles were associated with special cause variation, with an upward shift in mean percentage of telemedicine use from 5% to 22%. Time from initial call to consultation completion remained unchanged.
Conclusion: Our study supports the use of quality improvement methods to test telemedicine implementation strategies for pediatric telemedicine emergency consultations.
Keywords: pediatric, child, telemedicine, quality improvement, patient transfers, communication, health care transitions, hospitals, pediatric, emergency service, hospital, referral and consultation
Introduction
Pediatric transfers are a common source of overutilization1–6 and impose excessive burdens to families.7 Use of telemedicine to virtually provide expert consultation before initiating a transfer has potential to mitigate these problems7–12; however, impediments to the widespread adoption of pediatric emergency telemedicine exist.12–16
Quality improvement (QI) methods can address implementation challenges by permitting rapid-cycle process adaptations to increase uptake and sustainability.17 We used nurse and physician interviews to identify strategies to increase telemedicine use for pediatric emergency transfer consultations,12 then translated these strategies from concept to real-world application. Our objective was to test telemedicine implementation strategies in real-world application using QI methods. Our QI aim was to increase the percentage of pediatric emergency transfer consultations from two referring emergency departments (EDs) that use telemedicine from a mean baseline of 5% to a goal of 75% within 12 months.
Methods
Context
Our quaternary care children's hospital receives transfers from >130 hospitals and accepts >2,500 pediatric transfers annually. Referring ED physicians initiate a transfer by calling our transfer center to request a transfer consultation. The transfer center then connects the referring and consulting physicians by telephone or, if requested by either physician, telemedicine. Many telemedicine consultations begin by telephone and are converted to telemedicine at the request of the consulting physician. Our hospital uses two telemedicine platforms, Zoom (San Jose, CA) and InTouch (Santa Barbara, CA). The platform used depends on the community hospital's preferred platform.
The referring EDs in this study included two community hospitals in our telemedicine program with low rates of pediatric telemedicine use. The first hospital uses InTouch, has an annual pediatric ED volume of ∼15,000 patients, and transfers ∼120 children annually across 269 kilometers to our hospital. The second hospital uses Zoom, has an annual pediatric ED volume of ∼8,000 patients, and transfers ∼165 children annually across 58 kilometers to our hospital.
Eligible patients were children aged 8 days to 18 years who presented to the referring ED and had a transfer consultation by a pediatric hospitalist, neonatologist, or intensivist. The baseline study period was July 1, 2018 through June 31, 2019. The intervention period was July 1, 2019 through December 31, 2019, which was 6 months shorter than planned.
Planning the Interventions
We assembled a multidisciplinary multisite QI team that included a QI specialist, telemedicine program manager, two ED nurses, neonatologist, three pediatric intensivists, and seven pediatric hospitalists. This team met monthly to review progress and develop tests of change. The team developed a key driver diagram (Fig. 1) and a PICK chart to prioritize interventions with highest potential benefit and lowest projected effort. Key drivers of increasing telemedicine use included awareness of the telemedicine resource, streamlined telemedicine workflow, provider buy-in, and data transparency.
Fig. 1.
Key driver diagram summarizing the project aim and interventions implemented.
Improvement Activities
Throughout the plan-do-study-act cycles, feedback from consulting physicians was gathered through (1) a secure text messaging system from individual physicians within 3 days of each eligible transfer consultation and (2) discussion at hospitalists', neonatologists', and intensivists' division meetings. These feedback data were reviewed at the monthly QI meetings to guide the iterative improvements. Table 1 presents the plan-do-study-act tests of change, which shows that adopted interventions focused on telemedicine trainings, disseminating telemedicine uptake data, telemedicine reminders, telemedicine test calls, and preparing for telemedicine use for every transfer consultation.
Table 1.
Plan-Do-Study-Act Table for Telemedicine Interventions
| TEST OF CHANGE | DATE OF TEST | DESCRIPTION OF TEST | STATUS OF TEST |
|---|---|---|---|
| Project introduction at meetings | 7/9/19 | Attended division meetings to introduce the project; adapted the intervention to continue attending meetings to remind physicians to use telemedicine, identify training needs, and obtain feedback | Adapt |
| Real-time feedback through text message | 7/17/19 | Text messaged consulting physicians who used/did not use telemedicine for transfers from intervention sites for their feedback; text messages also served as reminders to use telemedicine | Adopt |
| Site visits and training | 7/18/19 | Visited intervention sites to introduce the project, solicited their feedback on the current state of telemedicine, and provided staff training | Adopt |
| Data transparency | 8/20/19 | Disseminated and reviewed control chart data on telemedicine uptake at monthly multidisciplinary meetings | Adopt |
| Reminders on computers | 8/26/19 | Placed bright yellow reminder on/behind computers at physician computer workstations to remind them to use telemedicine at intervention sites | Adopt |
| Preparing for telemedicine use for every transfer consultation | 8/28/19 | Established new workflow whereby referring emergency department nurses universally placed the telemedicine cart at the patient's bedside before the transfer consultation to omit delays if physicians chose to use telemedicine | Adopt |
| Text physicians before their shifts | 9/23/19 | Project manager reviewed hospitalists', neonatologists', and intensivists' schedules daily to determine who was on; text messaged reminder to use telemedicine | Abandon |
| Telemedicine training refreshers | 9/30/19 | Identified consulting physicians needing refresher training on telemedicine through text messaging intervention; provided training when needed (e.g., telemedicine software refresher training, login assistance, and downloading the secure software on personal devices) | Adopt |
| Test calls with sites | 10/16/19 | Conduct telemedicine test calls with the sites to demonstrate ease and reliability of using the technology | Adopt |
Measures
The outcome measure was the percentage of all pediatric emergency transfer consultations that used telemedicine from the two referring EDs. As a balancing measure, we monitored the time (minutes) from the initial transfer center call to completion of the consultation. Consultation completion was documented by the transfer center nurse when the patient's disposition was determined and all necessary transfer paperwork, if applicable, was received.
Analysis
Telemedicine use data were analyzed using statistical process control in SPCforExcel.16 Upper and lower control limits were defined as greater than or less than three sigma.17 Duration of time from initial call to consultation completion was compared for the pre- to postintervention periods using t-tests. The University of California Davis Institutional Review Board determined this study to be not human subjects research.
Results
During the 12-month baseline period, there were 403 patient transfer consultations; telemedicine was used for 19 consultations. For the 6-month study period, there were 132 patient transfer consultations; telemedicine was used for 29 consultations. The most common diagnostic groupings among the telemedicine consultations included respiratory infections (n = 15), ill-defined conditions (e.g., fever, vomiting, and sepsis) (n = 6), and epilepsy or convulsions (n = 3).
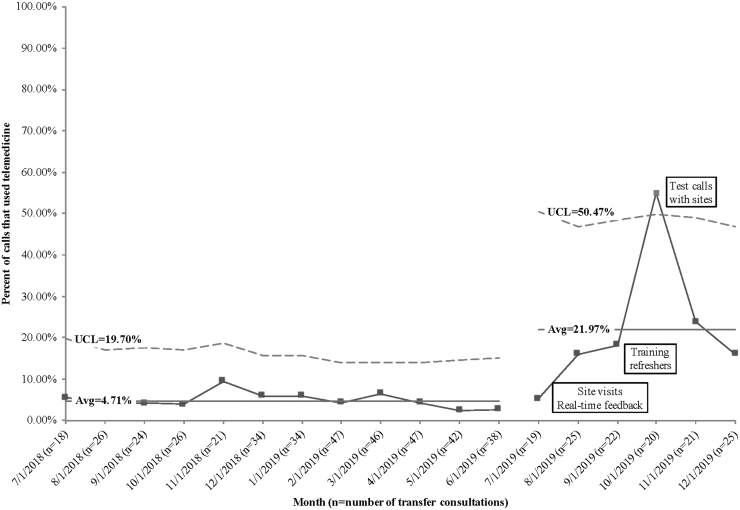
The percentage of consultations that used telemedicine increased from mean of 5% monthly at baseline to 22% monthly in the postintervention period, with a stable process in the baseline period and special cause variation in the postintervention period (Fig. 2). For the balance measure, the time from initial call to consultation completion was similar for the pre- versus postintervention periods (267 minutes vs. 257 minutes, p = 0.70).
Fig. 2.
P-chart depicting telemedicine use for transfer consultations. Avg, average; UCL, upper control limit.
The project duration was shortened due to feedback that the objective of achieving 75% telemedicine use was unobtainable. Physicians perceived telemedicine to only be beneficial for specific circumstances, such as for patients whose illness severity was unclear. However, there was no consensus among specific diagnoses for when telemedicine should be used. Ubiquitous application was seen as burdensome and not valuable. After 6 months, our team determined that the objective of testing telemedicine implementation strategies was achieved, and thus the study was concluded.
Discussion
Our rapid-cycle tests of change identified that strategies to increasing the use of telemedicine for pediatric emergency transfer consultations include ongoing telemedicine trainings, disseminating telemedicine uptake data, telemedicine use reminders, test calls, and having telemedicine equipment ready at the bedside. Although the promotion of ubiquitous application of telemedicine use for transfer consultations was not supported by our consulting physicians, we effectively used QI methods to identify successful telemedicine implementation strategies.
QI methods are a valuable systematic process for increasing uptake and sustainability of interventions,17 yet QI and other approaches that ensure systems are effective, efficient, and usable (e.g., participatory design methods) remain underutilized for telemedicine programs.18 We anticipate that this present description of applying QI methods to increase telemedicine uptake will help other telemedicine researchers and program leaders to incorporate this useful approach. Future strategies that could be explored include interventions that were categorized on the PICK chart as high payoff but hard to implement, such as engaging the transfer center nurses to encourage the use of telemedicine.
This study was limited to a single telemedicine program at a children's hospital. Although our results may not be generalizable, the application of QI methods and the implemented interventions could be used in other settings. Our multidisciplinary team largely consisted of physicians. However, we targeted physicians, because prior research identified physicians as the greatest source of resistance to telemedicine uptake.12 Despite these limitations, our study supports the use of QI to test strategies for increasing telemedicine use for pediatric telemedicine emergency consultations.
Authors' Contributions
J.L.R. conceptualized and designed the study, designed and executed interventions, interpreted the data, drafted the initial article, revised the article, and approved the final article as submitted. H.S.S-.F. participated in the conceptualization and design of the study, designed and executed interventions, collected data, interpreted the data, reviewed and revised the article, and approved the final article as submitted. M.S., M.Y.H., A.S.B., S.J., J.E.N., and J.L.P. designed and executed interventions, interpreted the data, reviewed and revised the article, and approved the final article as submitted.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
Funding Information
The project described was supported by a University of California Davis Academic Senate New Research Grant and a University of California Children's Miracle Network research award. The project was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860 and linked award KL2 TR001859.
References
- 1. Mohr NM, Harland KK, Shane DM, Miller SL, Torner JC. Potentially avoidable pediatric interfacility transfer is a costly burden for rural families: A cohort study. Acad Emerg Med 2016;23:885–894 [DOI] [PubMed] [Google Scholar]
- 2. Li J, Monuteaux MC, Bachur RG. Interfacility transfers of noncritically III children to academic pediatric emergency departments. Pediatrics 2012;130:83–92 [DOI] [PubMed] [Google Scholar]
- 3. Gattu RK, Teshome G, Cai L, Wright C, Lichenstein R. Interhospital pediatric patient transfers—Factors influencing rapid disposition after transfer. Pediatr Emerg Care 2014;30:26–30 [DOI] [PubMed] [Google Scholar]
- 4. Peebles ER, Miller MR, Lynch TP, Tijssen JA. Factors associated with discharge home after transfer to a pediatric emergency department. Pediatr Emerg Care 2018;34:650–655 [DOI] [PubMed] [Google Scholar]
- 5. Ray KN, Marin JR, Li J, Davis BS, Kahn JM. Referring hospital characteristics associated with potentially avoidable emergency department transfers. Acad Emerg Med 2019;26:205–216 [DOI] [PubMed] [Google Scholar]
- 6. Harvey JB, Yeager BE, Cramer C, Wheeler D, David MS. The impact of telemedicine on pediatric critical care triage. Pediatr Crit Care Med 2017;18:e555–e560 [DOI] [PubMed] [Google Scholar]
- 7. Rosenthal JL, Li ST, Hernandez L, Alvarez M, Rehm RS, Okumura MJ. Familial caregiver and physician perceptions of the family-physician interactions during interfacility transfers. Hosp Pediatr 2017;7:344–351 [DOI] [PubMed] [Google Scholar]
- 8. Desai S, Williams ML, Smith AC. Teleconsultation from a secondary hospital for paediatric emergencies occurring at rural hospitals in Queensland. J Telemed Telecare 2013;19:405–410 [DOI] [PubMed] [Google Scholar]
- 9. Tachakra S, Uche CU, Stinson A. Four years' experience of telemedicine support of a minor accident and treatment service. J Telemed Telecare 2002;8:87–89 [DOI] [PubMed] [Google Scholar]
- 10. Marcin JP, Nesbitt TS, Struve S, Traugott C, Dimand RJ. Financial benefits of a pediatric intensive care unit-based telemedicine program to a rural adult intensive care unit: Impact of keeping acutely ill and injured children in their local community. Telemed J E Health 2004;10:S-1–S-5. [PubMed] [Google Scholar]
- 11. Harvey JB, Yeager BE, Cramer C, Wheeler D, David MS. The impact of telemedicine on pediatric critical care triage. Pediatr Crit Care Med 2017;18:e555–e560 [DOI] [PubMed] [Google Scholar]
- 12. Sauers-Ford H, Hamline M, Gosdin M, et al. Acceptability, usability, and effectiveness: A qualitative study evaluating a pediatric telemedicine program. Acad Emerg Med 2019;26:1022–1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Uscher-Pines L, Kahn JM. Barriers and facilitators to pediatric emergency telemedicine in the United States. Telemed J E Health 2014;20:990–996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ray KN, Felmet KA, Hamilton MF, et al. Clinician attitudes toward adoption of pediatric emergency telemedicine in rural hospitals. Pediatr Emerg Care 2017;33:250–257 [DOI] [PubMed] [Google Scholar]
- 15. Kim JW, Tiyyagura G, Langhan M. A qualitative analysis of general emergency medicine providers' perceptions on pediatric emergency telemedicine. Pediatr Emerg Care 2019;35:856–861 [DOI] [PubMed] [Google Scholar]
- 16. Haimi M, Brammli-Greenberg S, Waisman Y, Baron-Epel O. Physicians' experiences, attitudes and challenges in a Pediatric Telemedicine Service. Pediatr Res 2018;84:650–656 [DOI] [PubMed] [Google Scholar]
- 17. Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide: A practical approach to enhancing organizational performance. San Francisco, CA: John Wiley & Sons, 2009 [Google Scholar]
- 18. Demiris G, Charness N, Krupinski E, et al. The role of human factors in telehealth. Telemed J E Health 2010;16:446–453 [DOI] [PubMed] [Google Scholar]