Key Points
Question
Does having multiple prior generations affected by depression increase risk of psychopathology in children, and can it be reliably measured in large, diverse samples using informant-reported family history?
Findings
In this secondary analysis of the Adolescent Brain Cognitive Development study including 11 200 children from 9462 families, the highest risks of depressive and other psychiatric disorders were found in children with 2 depression-affected generations compared with those with 1 or no affected generations. This pattern held across sex, socioeconomic status, and race/ethnicity.
Meaning
In this study, family history methods across 3 generations were associated with increased psychiatric risk in offspring and may enable selection of homogenous samples for genetic and biological studies as well as development of screening tools in applied mental health settings.
This secondary analysis of the Adolescent Brain Cognitive Development study examines the association of multigenerational family history of depression with lifetime depressive disorders and other psychopathology in children.
Abstract
Importance
Three-generation family studies of depression have established added risk of psychopathology for offspring with 2 previous generations affected with depression compared with 1 or none. Because of their rigorous methodology, there are few of these studies, and existing studies are limited by sample sizes. Consequently, the 3-generation family risk paradigm established in family studies can be a critical neuropsychiatric tool if similar transmission patterns are reliably demonstrated with the family history method.
Objective
To examine the association of multigenerational family history of depression with lifetime depressive disorders and other psychopathology in children.
Design, Setting, and Participants
In this analysis of the Adolescent Brain Cognitive Development (ABCD) study data, retrospective, cross-sectional reports on psychiatric functioning among 11 200 children (generation 3 [G3]) and parent reports on parents’ (G2) and grandparents’ (G1) depression histories were analyzed. The ABCD study sampling weights were used for generalized estimating equation models and descriptive analyses. Data were collected from September 2016 to November 2018, and data were analyzed from July to November 2020.
Main Outcomes and Measures
Four risk categories were created, reflecting how many prior generations had history of depression: (1) neither G1 nor G2 (G1−/G2−), (2) only G1 (G1+/G2−), (3) only G2 (G1−/G2+), and (4) both G1 and G2 (G1+/G2+). Child lifetime prevalence and relative risks of psychiatric disorders were based on child and caregiver reports and grouped according to familial risk category derived from G1 and G2 depression history.
Results
Among 11 200 included children, 5355 (47.8%) were female, and the mean (SD) age was 9.9 (0.6) years. By parent reports, the weighted prevalence of depressive disorder among children was 3.8% (95% CI, 3.2-4.3) for G1−/G2− children, 5.5% (95% CI, 4.3-7.1) for G1+/G2− children, 10.4% (95% CI, 8.6-12.6) for G1−/G2+ children, and 13.3% (95% CI, 11.6-15.2) for G1+/G2+ children (Cochran-Armitage trend = 243.77; P < .001). The weighted suicidal behavior prevalence among children was 5.0% (95% CI, 4.5-5.6) for G1−/G2− children, 7.2% (95% CI, 5.8-8.9) for G1+/G2− children, 12.1% (95% CI, 10.1-14.4) for G1−/G2+ children, and 15.0% (95% CI, 13.2-17.0) for G1+/G2+ children (Cochran-Armitage trend = 188.66; P < .001). By child reports, the weighted prevalence of depressive disorder was 4.8% (95% CI, 4.3-5.5) for G1−/G2− children, 4.3% (95% CI, 3.2-5.7) for G1+/G2− children, 6.3% (95% CI, 4.9-8.1) for G1−/G2+ children, and 7.0% (95% CI, 5.8-8.5) for G1+/G2+ children (Cochran-Armitage trend = 9.01; P = .002), and the weighted prevalence of suicidal behaviors was 7.4% (95% CI, 6.7-8.2) for G1−/G2− children, 7.0% (95% CI, 5.6-8.6) for G1+/G2− children, 9.8% (95% CI, 8.1-12.0) for G1−/G2+ children, and 13.8% (95% CI, 12.1-15.8) for G1+/G2+ children (Cochran-Armitage trend = 46.69; P < .001). Similar patterns were observed for other disorders for both parent and child reports and across sex, socioeconomic status, and race/ethnicity.
Conclusions and Relevance
In this study, having multiple prior affected generations was associated with increased risk of childhood psychopathology. Furthermore, these findings were detectable even at prepubertal ages and existed in diverse racial/ethnic and socioeconomic groups. Clinically, they underscore the need for screening for family history in pediatric settings and highlight implications for biological research with homogenous subgroups using magnetic resonance imaging or genetic analyses.
Introduction
Family history is among the most reliable risk markers for future mental illness.1,2 The biological offspring of parents with depression have a 2-fold to 5-fold increased risk of major depressive disorder (MDD), other nonpsychotic disorders, and unnatural deaths.3,4,5,6,7,8 These disorders often begin in childhood or adolescence and are sustained over a life course with recurrences and remission as well as impaired social functioning.3,9 Family history also predicts stable brain-based differences, such as cortical thinning,10,11,12,13 smaller subcortical volumes,14,15,16 and altered resting-state functional connectivity,17,18 even in high-risk offspring who never develop psychopathology.
We are aware of just 2 studies19,20 that assessed the association of 2 prior generations of depression in the family with the prevalence of grandchild psychiatric diagnoses. The first is a 3-generation study observing family members for up to 38 years conducted by Weissman and colleagues19 (high-risk study). Grandchildren with 2 previous generations affected by MDD were at highest risk, with 3-fold risk of developing MDD, 2-fold risk of having suicidal thoughts and behaviors, and increased other psychopathology. Furthermore, high-risk offspring had altered hippocampal microstructure, which predicted follow-up depressive symptoms, and individuals with 2 previous generations of depression had the most pronounced differences in microstructure, regardless of if they had depression themselves.21 This sample’s strengths included direct clinical interviews for each generation of participants; a top-down approach of data collection, with prospective observation of the first generation, followed by the second and third generations, thereby limiting recall bias associated with recruiting the youngest generation and retrospectively collecting information on previous generations; and the collection of neural, genetic, and environmental data across multiple generations. But the relatively small, racially and culturally homogenous sample restricted generalizability afforded by large-scale studies.19
The second study, using the national Swedish medical registry,20 also found that grandchildren with 2 previous generations affected by MDD had the highest risk of MDD themselves. However, the authors did not investigate other psychopathology. Thus, to our knowledge, grandchild outcomes beyond MDD have not been extended to a large, representative study.
Smaller family studies with detailed interview-based clinical phenotypes in each generation can identify the highest-risk groups for early intervention. However, they require replication in large samples to examine clinical and demographic variability. The advent of big population studies allows us to extend multigenerational studies to large, diverse samples. These big data studies are a welcome scientific asset but often have the drawback of less detailed, retrospective family history by participant self-report and might not be ideal for studying familial risk.22 However, if we can replicate clinical findings obtained in a relatively small sample with meticulous family history in a large population sample with less complete family data, this opens up opportunity to test neural findings underlying familial risk for psychopathology in big samples. Specifically, individuals with 2 prior generations affected who are at the highest risk of psychopathology19,20 and neural abnormalities21 may be a more clinically homogenous group. Therefore, studying them could increase chances of identifying underlying mechanisms of psychopathology.
Here, by leveraging data from the Adolescent Brain Cognitive Development (ABCD) study,23 a large representative sample of children aged 9 to 11 years, we aimed to extend findings from our high-risk study19 showing that offspring with 2 previous generations with depression are at highest risk of psychopathology. Second, we investigated whether these findings are similar across sex, race/ethnicity, and socioeconomic status (SES). We hypothesized increasing rates of psychopathology, with the lowest rates in children with no depression in the family, slightly higher rates in children with a grandparent with depression, higher rates in children with a parent with depression, and highest rates in children with both a parent and grandparent with depression and that this pattern would be robust across sociodemographic variables.
Methods
Data Source
Analyses were conducted using baseline data from the ABCD study23 version 2.01 (July 2019), which included 11 875 children recruited from primary school and public school systems at 22 sites nationwide. Multistage probability sampling methods were used to maintain national representativeness in accordance with the American Community Survey and to reduce bias in statistically derived estimates.24 The institutional review board of the University of California, San Diego gave centralized approval for the collection of the data and individual study sites where data were collected obtained approval from their local institutional review boards. All parents gave written informed consent and children verbal assent.
Procedures and Variables of Interest
Children and the reporter parents (9609 biological mother [85.7%]; 1123 biological father [9.8%]; 466 adoptive, custodial, or other parent [4.5%]) completed reports on children’s lifetime histories of psychiatric disorders. The self-administered computerized version of the Kiddie Schedule for Affective Disorders and Schizophrenia for DSM-5 (KSADS, Lifetime Version) was the primary mental health assessment instrument.25,26 Additionally, parents completed reports on family history of psychiatric disorders, including MDD, and baseline demographic reports. See the eMethods in the Supplement for detailed description of ABCD study data files and variables.
Measures
Predictor: Family Risk
The participant’s parent reported on a history of depression in first-degree and second-degree relatives using the validated family history measure27 used in the Collaborative Study on the Genetics of Alcoholism.28 The question was, “Has ANY blood relative of your child ever suffered from depression, that is, have they felt so low for a period of at least two weeks that they hardly ate or slept or couldn't work or do whatever they usually do?” Using depressive histories from the 2 generations—grandparents (generation 1 [G1]) and parents (generation 2 [G2])—we formed a 4-category depression risk variable, reflecting how many prior generations were affected with depression: (1) neither G1 nor G2 (G1−/G2−; lowest risk assumed), (2) only G1 (G1+/G2−), (3) only G2 (G1−/G2+), and (4) both G1 and G2 (G1+/G2+; highest risk assumed).
Primary Outcome: Child Lifetime Prevalence of Psychiatric Disorders at Baseline (KSADS Interviews)
Nine psychiatric disorders or conditions were derived from DSM-5 diagnoses reported by both parents and children separately, using lifetime histories as baseline prevalence: MDD, any depressive disorder (including MDD, persistent depressive disorder [formerly dysthymic disorder], and depressive disorder not otherwise specified), social anxiety disorder (SAD), generalized anxiety disorder (GAD), any anxiety disorder (including GAD, SAD, and specific anxiety disorder not meeting criteria for GAD or SAD), bipolar disorder, sleep problems (diagnosis), suicidal behaviors (including active or passive ideation, plans/intention/preparation, and attempts), and any psychiatric disorder/condition. Eight additional diagnoses were derived from parent reports only: agoraphobia, simple/specific phobia, separation anxiety disorder, obsessive-compulsive disorder, posttraumatic stress disorder, attention-deficit hyperactivity disorder, conduct/oppositional defiant disorder, and psychotic disorders.
Potential Moderators
SES, child sex, and child race/ethnicity were examined as moderators of the association between familial risk and baseline prevalence of psychiatric conditions. We defined SES as a 3-category variable (low, medium, and high SES) derived from parental education and combined household income (eMethods in the Supplement). For child race/ethnicity, we selected the 3 largest racial/ethnic groups in the US: non-Hispanic White, non-Hispanic Black, and Hispanic. We collapsed other groups into a fourth category, other race/ethnicity, because of low individual numbers.
Potential Confounders
We controlled for child age, sexual orientation, religion, reporter relationship to child, parent’s age, gender identity, and marital status in the models (eMethods in the Supplement). SES, race/ethnicity, and sex were included as covariates for models in which they were not moderators. These variables were correlated with both familial risk and parent and/or child reports of 1 or more psychiatric disorders.
Statistical Analyses
Analyses were performed using SPSS version 27 (IBM). For descriptive analyses, χ2 tests were used for categorical variables and t tests or analyses of variance for continuous variables, with Bonferroni adjustments for multiple comparisons. We compared included and excluded cases on demographic and clinical characteristics used in our regression models (eTable 1 in the Supplement). Parent and child reports were tested for concordance using Cohen κ measure of interrater reliability. Previous studies indicated that divergence of child and parent responses on psychiatric disorders warrant separate assessments of their reports.29,30 Significance was set at a P value less than .05, and all P values were 2-tailed.
Association of Familial Risk With Prevalence of Psychiatric Disorders/Conditions
Generalized estimating equations (GEEs)31 were used to obtain the relative risks for the psychiatric diagnoses in children as reported by parents and children. GEE represents an extension of the general linear model approach, allowing for correlations among family members and site clusters. Data were modeled with Poisson distributions using the log-link function, controlling for potential confounders. The 4-level family risk variable was analyzed as a categorical variable, with children without a family history of depression as the reference group. Then, we examined the trend across the 4 categories using the Cochran-Armitage trend test,32,33 testing increasing levels of risk. We evaluated separately the role of sex, SES, and race/ethnicity as moderators of the association of familial risk with psychiatric outcomes. We entered the main effect association(s) for risk and the moderating variable and the interaction between risk and moderating variable into the model. We used the ABCD study sampling weights in our GEE models and descriptive analyses. Development of the weighting scores is detailed in Garavan et al.24
Additional and Post Hoc Analyses
To control for the possibility that the informant parent had depression and could therefore bias the reporting of the child’s, spouse’s, or parents’ depression,34 we performed a sensitivity analysis removing any reporter parent who had depression themselves. Finally, we compared results from our analytic sample data with those from an imputed data set. Our missing data analysis showed a pattern consistent with missing at random. The expectation maximization method of multiple imputation35,36 was used to generate complete data for family history and parent and child reports of KSADS diagnoses (eAppendix in the Supplement).
Results
Participants
The baseline ABCD sample comprised 11 875 children. Participants were excluded for missing data on family history (n = 420) or KSADS (n = 165 parent reports; n = 90 child reports), resulting in an analytic sample of 11 200 children from 9462 families. Among 11 200 included children, 5355 (47.8%) were female, and the mean (SD) age was 9.9 (0.6) years. Demographic characteristics of the analytic sample were distributed across the risk categories (Table 1) (eTable 1 in the Supplement).
Table 1. Demographic Characteristics of Sample by Risk Category.
| Characteristic | Familial depression risk category, No. (%)a,b | P valuec | |||
|---|---|---|---|---|---|
| G1−/G2− | G1+/G2− | G1−/G2+ | G1+/G2+ | ||
| Total | 6550 (58.2) | 1480 (12.2) | 1199 (11.3) | 1971 (18.2) | NA |
| Female | 3181 (49.4) | 655 (46.1) | 570 (48.1) | 949 (49.2) | .03 |
| Age, mean (SD), y | |||||
| Child age | 9.9 (0.6) | 9.9 (0.6) | 9.9 (0.6) | 9.9 (0.6) | .41 |
| Parent age | 40.1 (6.9) | 40.2 (6.1) | 39.4 (6.7) | 39.0 (6.7) | <.001 |
| Race/ethnicityd | |||||
| Non-Hispanic White | 3030 (45.0) | 962 (65.8) | 618 (53.2) | 1223 (65.6) | <.001 |
| Non-Hispanic Black | 1181 (16.0) | 91 (5.8) | 208 (15.0) | 195 (8.7) | <.001 |
| Hispanic | 1484 (26.9) | 258 (20.9) | 235 (23.2) | 299 (17.0) | <.001 |
| Other | 848 (12.1) | 167 (7.5) | 134 (8.6) | 252 (8.6) | .50 |
| Parent’s marital status | |||||
| Married | 4474 (63.0) | 1197 (75.6) | 694 (51.6) | 1249 (55.9) | <.001 |
| Never married | 859 (15.5) | 82 (6.0) | 175 (16.8) | 232 (13.8) | <.001 |
| Divorced/widowed/separated | 755 (15.2) | 144 (13.4) | 249 (26.1) | 346 (23.2) | .002 |
| Living with partner | 394 (6.3) | 56 (4.0) | 73 (5.5) | 126 (7.0) | .002 |
| Education and income, mean (SD) | |||||
| Parental education levele | 17.0 (2.8) | 17.8 (2.1) | 16.9 (2.6) | 17.2 (2.3) | <.001 |
| Combined household incomef | 7.2 (2.5) | 8.0 (1.8) | 6.8 (2.5) | 7.1 (2.4) | <.001 |
| SESg | |||||
| Low | 2123 (40.3) | 301 (28.0) | 460 (46.3) | 677 (42.8) | <.001 |
| Medium | 3161 (44.2) | 847 (54.4) | 541 (41.4) | 987 (44.6) | <.001 |
| High | 1204 (15.6) | 331 (17.6) | 192 (12.3) | 300 (12.6) | <.001 |
| Informant’s relationship to child | |||||
| Biological mother | 5509 (83.8) | 1320 (89.4) | 1024 (84.8) | 1756 (89.7) | <.001 |
| Biological father | 722 (10.9) | 138 (8.8) | 123 (10.9) | 140 (6.3) | <.001 |
| Adoptive/custodial/other parent | 317 (5.3) | 22 (1.8) | 52 (4.3) | 75 (4.0) | <.001 |
| Born outside the US | |||||
| Child | 268 (5.3) | 34 (2.8) | 20 (2.3) | 15 (0.7) | <.001 |
| Parent/grandparent | 2367 (38.1) | 421 (28.1) | 335 (30.0) | 487 (22.8) | <.001 |
| Sexual orientation | |||||
| Parent report | |||||
| Yes | 4 (0.1) | 0 | 0 | 0 | NA |
| Maybe | 352 (4.9) | 123 (7.6) | 112 (8.1) | 258 (12.9) | <.001 |
| Child report | |||||
| Yes | 16 (0.2) | 1 (0) | 2 (0.3) | 19 (1.0) | .001 |
| Maybe | 51 (0.9) | 18 (1.2) | 12 (1.2) | 23 (1.1) | .61 |
| Religious preference | |||||
| Denominational | 4650 (76.2) | 1043 (74.7) | 809 (71.7) | 131 (72.1) | <.001 |
| Nondenominational | 1362 (21.1) | 317 (20.5) | 254 (23.0) | 452 (22.4) | .30 |
| Agnostic/atheist | 208 (2.7) | 81 (4.8) | 69 (5.3) | 108 (5.5) | <.001 |
Abbreviations: G1, generation 1 (grandparents); G2, generation 2 (parents); NA, not applicable; SES, socioeconomic status.
Children were grouped into 4 risk categories, reflecting how many prior generations were affected with depression: (1) neither G1 nor G2 (G1−/G2−), (2) only G1 (G1+/G2−), (3) only G2 (G1−/G2+), and (4) both G1 and G2 (G1+/G2+).
Values presented are unweighted counts and weighted percentages within each depression risk categories.
Differences in prevalence among risk categories were calculated using χ2 tests for categorical variables and one-way analysis of variance for continuous variables, with Bonferroni adjustments used for multiple comparisons.
We selected the 3 largest racial/ethnic groups in the US: non-Hispanic White, non-Hispanic Black, and Hispanic. We collapsed other groups into other race/ethnicity because of low individual numbers.
Created using the highest grade or degree completed, using the following values: 0, never attended school/kindergarten only; 1, 1st grade; 2, 2nd grade; 3, 3rd grade; 4, 4th grade; 5, 5th grade; 6, 6th grade; 7, 7th grade; 8, 8th grade; 9, 9th grade; 10, 10th grade; 11, 11th grade; 12, 12th grade, no diploma; 13, high school graduate; 14, GED or equivalent diploma; 15, college credit/postsecondary education, no degree; 16, associate’s degree: occupational, technical, or vocational degree; 17, associate’s degree: academic program; 18, bachelor’s degree; 19, master’s degree; 20, professional school degree (eg, MD, DDS, DVN, JD); 21, doctoral degree (eg, PhD, EdD).
Created using combined household income in the past 12 months before taxes, using the following values: 1, <$5000; 2, $5000-$11 999; 3, $12 000-$15 999; 4, $16 000-$24 999; 5, $25 000-$34 999; 6, $35 000-$49 999; 7, $50 000-$74 999; 8, $75 000-$99 999; 9, $100 000-$199 999; 10, ≥$200 000.
For SES threshold definitions, see the eMethods in the Supplement.
Prevalence of Clinical Diagnoses by Familial Risk Category
There was low agreement between parent and child reports (κ estimates ranged from 0.03 to 0.20; eTable 2 in the Supplement). Consequently, we present results for parent and child reports separately. As reported by parents, higher prevalence of psychiatric disorders was observed with increasing levels of familial risk as confirmed by increasing point estimates across risk categories and significant trend statistics for almost all evaluated disorders (Figure 1) (Table 2). By parent reports, the weighted prevalence of any depressive disorder among children was 3.8% (95% CI, 3.2-4.3) for G1−/G2− children, 5.5% (95% CI, 4.3-7.1) for G1+/G2− children, 10.4% (95% CI, 8.6-12.6) for G1−/G2+ children, and 13.3% (95% CI, 11.6-15.2) for G1+/G2+ children (Cochran-Armitage trend = 243.77; P < .001). The weighted suicidal behavior prevalence among children was 5.0% (95% CI, 4.5-5.6) for G1−/G2− children, 7.2% (95% CI, 5.8-8.9) for G1+/G2− children, 12.1% (95% CI, 10.1-14.4) for G1−/G2+ children, and 15.0% (95% CI, 13.2-17.0) for G1+/G2+ children (Cochran-Armitage trend = 188.66; P < .001). The weighted prevalence of MDD was 1.2% (95% CI, 1.0-1.6) among G1−/G2− children, 2.3% (95% CI, 1.5-3.4) among G1+/G2− children, 4.9% (95% CI, 3.6-6.6) among G1−/G2+ children, and 7.4% (95% CI, 6.2-8.8) among G1+/G2+ children (Cochran-Armitage trend = 202.29; P < .001). This trend was similar for SAD, GAD, any anxiety disorder, sleep problem, and any disorder as reported by the parent (Table 2). When reported by the child, G1+/G2+ children had highest prevalence rates except for MDD and any anxiety disorder (Table 2). By child reports, the weighted prevalence of depressive disorder was 4.8% (95% CI, 4.3-5.5) for G1−/G2− children, 4.3% (95% CI, 3.2-5.7) for G1+/G2− children, 6.3% (95% CI, 4.9-8.1) for G1−/G2+ children, and 7.0% (95% CI, 5.8-8.5) for G1+/G2+ children (Cochran-Armitage trend = 9.01; P = .002), and the weighted prevalence of suicidal behaviors was 7.4% (95% CI, 6.7-8.2) for G1−/G2− children, 7.0% (95% CI, 5.6-8.6) for G1+/G2− children, 9.8% (95% CI, 8.1-12.0) for G1−/G2+ children, and 13.8% (95% CI, 12.1-15.8) for G1+/G2+ children (Cochran-Armitage trend = 46.69; P < .001).
Figure 1. Prevalence of Psychiatric Disorders in Children by Familial Depression Risk Reported by Parents and Children.
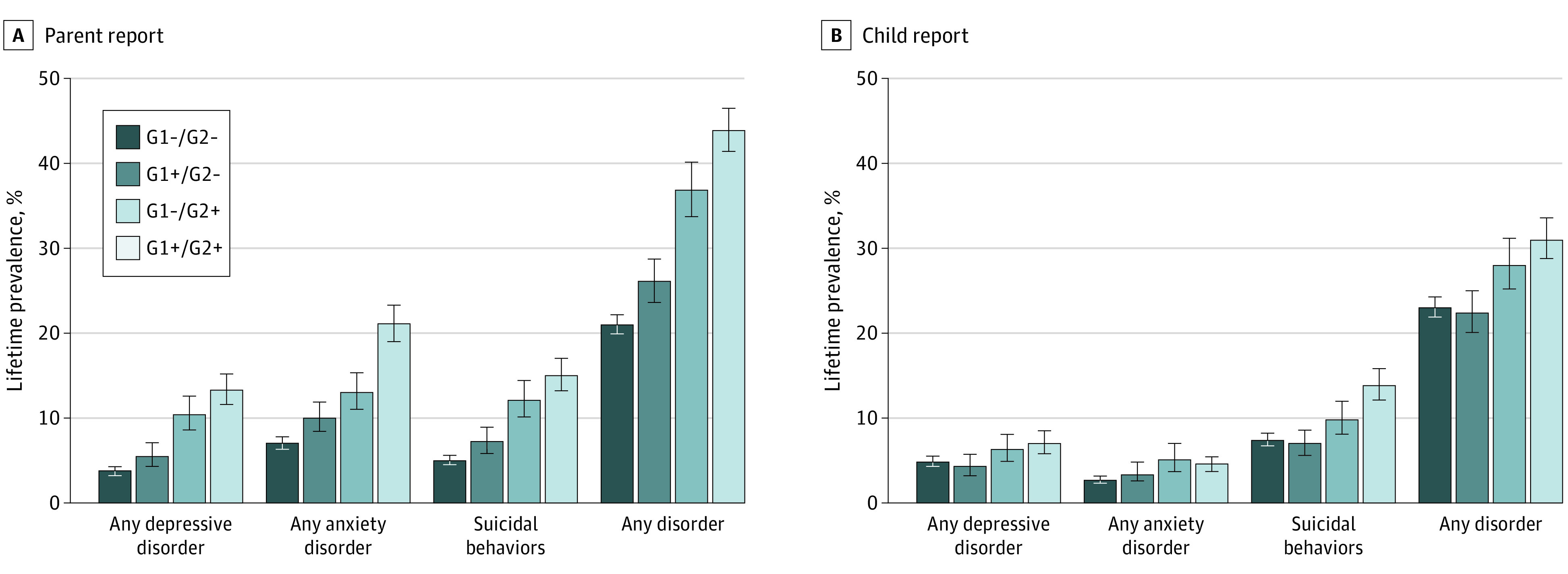
Children were grouped into 4 risk categories, reflecting how many prior generations were affected with depression: (1) neither grandparents (generation 1 [G1]) nor parents (generation 2 [G2]; G1−/G2−), (2) only G1 (G1+/G2−), (3) only G2 (G1−/G2+), and (4) both G1 and G2 (G1+/G2+). Error bars indicate 95% CIs.
Table 2. Prevalence Trends for Psychological Disorders Based on Parent and Child Reports on Kiddie Schedule for Affective Disorders and Schizophrenia for DSM-5 Across Levels of Familial Depression Risk.
| Disorder | Familial depression risk category, weighted % (95% CI)a,b | Cochran-Armitage Trend | |||
|---|---|---|---|---|---|
| G1−/G2− | G1+/G2− | G1−/G2+ | G1+/G2+ | ||
| Parent report | |||||
| Major depressive disorder | 1.2 (1.0-1.6) | 2.3 (1.5-3.4) | 4.9 (3.6-6.6) | 7.4 (6.2-8.9) | 202.29c |
| Any depressive disorderd | 3.8 (3.2-4.3) | 5.5 (4.3-7.1) | 10.4 (8.6-12.6) | 13.3 (11.6-15.2) | 243.77c |
| Social anxiety disorder | 3.4 (2.9-3.9) | 5.0 (3.9-6.4) | 5.8 (4.5-7.5) | 8.0 (6.8-9.5) | 102.77c |
| Generalized anxiety disorder | 2.4 (2.0-2.9) | 3.6 (2.8-4.8) | 5.5 (4.2-7.1) | 12.1 (10.5-14.1) | 229.83c |
| Any anxiety disordere | 7.0 (6.3-7.8) | 10.0 (8.4-11.9) | 13.0 (11.0-15.3) | 21.1 (19.0-23.3) | 289.84c |
| Bipolar disordersf | 5.7 (5.1-6.4) | 4.8 (3.7-6.3) | 11.5 (9.6-13.9) | 11.2 (9.5-12.8) | 61.21c |
| Sleep problem (diagnosis) | 7.2 (6.5-8.0) | 10.3 (8.7-12.2) | 11.8 (9.8-14.2) | 16.7 (14.9-18.7) | 151.23c |
| Suicidal behaviorsg | 5.0 (4.5-5.6) | 7.2 (5.8-8.9) | 12.1 (10.1-14.4) | 15.0 (13.2-17.0) | 188.66c |
| Any disorder/conditionh | 21.0 (19.9-22.2) | 26.1 (23.6-28.7) | 36.8 (33.7-40.1) | 43.9 (41.4-46.5) | 413.66c |
| Child report | |||||
| Major depressive disorder | 2.7 (2.2-3.2) | 2.1 (1.4-3.1) | 3.9 (2.8-5.4) | 3.8 (2.9-5.0) | 2.34 |
| Any depressive disorderd | 4.8 (4.3-5.5) | 4.3 (3.2-5.7) | 6.3 (4.9-8.1) | 7.0 (5.8-8.5) | 9.01i |
| Social anxiety disorder | 0.6 (0.4-0.8) | 0.8 (0.3-1.6) | 1.3 (0.7-2.2) | 1.6 (1.1-2.5) | 16.62c |
| Generalized anxiety disorder | 0.5 (0.3-0.7) | 0.5 (0.3-1.1) | 0.9 (0.4-1.8) | 1.5 (1.0-2.4) | 13.33c |
| Any anxiety disordere | 2.7 (2.3-3.2) | 3.3 (2.6-4.8) | 5.1 (3.7-7.0) | 4.6 (3.7-6.6) | 19.15c |
| Bipolar disordersf | 0.8 (0.6-1.1) | 1.2 (0.7-2.2) | 0.9 (0.4-1.9) | 1.3 (0.8-2.1) | 0.57 |
| Sleep problem (diagnosis) | 14.8 (13.8-15.8) | 15.1 (13.2-17.3) | 17.1 (14.7-19.8) | 18.4 (16.5-20.6) | 10.91i |
| Suicidal behaviorsg | 7.4 (6.7-8.2) | 7.0 (5.6-8.6) | 9.8 (8.1-12.0) | 13.8 (12.1-15.8) | 46.69c |
| Any disorder/conditionh | 23.0 (21.9-24.3) | 22.4 (20.1-25.0) | 28.0 (25.2-31.2) | 31.0 (28.8-33.6) | 39.07c |
Abbreviations: G1, generation 1 (grandparents); G2, generation 2 (parents).
Children were grouped into 4 risk categories, reflecting how many prior generations were affected with depression: (1) neither G1 nor G2 (G1−/G2−), (2) only G1 (G1+/G2−), (3) only G2 (G1−/G2+), and (4) both G1 and G2 (G1+/G2+).
Baseline prevalence was obtained from generalized estimating equations linear models and was adjusted for child characteristics (sex, age, race/ethnicity, sexual orientation, religious preference, and relationship to informant) and parents characteristics (age, marital status, and socioeconomic status based on combined household income and educational level).
P < .001.
Any depressive disorder includes one of major depressive disorder, persistent depressive disorder, or depressive disorder not otherwise specified.
Any anxiety disorder includes one of social anxiety disorder, generalized anxiety disorder, or anxiety disorder not meeting impairment criteria for social or generalized anxiety disorders.
Bipolar disorders include bipolar disorders 1 and 2 and bipolar disorders not otherwise specified.
Suicidal behaviors include suicidal ideation (passive or active), suicidal plans, and suicide attempts.
Any disorder/condition refers to one or more of the 8 previously listed disorders/behaviors or conditions.
P < .01.
According to parents, G1+/G2+ children were 6.0-fold more likely to have MDD and 2.1-fold more likely to have any disorder compared with G1−/G2− children (eTable 3 in the Supplement). KSADS diagnoses only reported by the parent showed a similar trend, with significant trend statistics of higher rates by increasing familial risk (eTable 4 in the Supplement).
Moderation by Sociodemographic Variables
To investigate whether the associations between family risk and diagnoses were moderated by sociodemographic variables, we tested main and interaction statistical effects of sex, race/ethnicity, and SES for depressive disorders, anxiety disorders, suicidal behaviors, and any disorder/condition (Table 3; Figure 2) (eTables 5 and 6 in the Supplement).
Table 3. Moderation (Interaction) Associations of Sex, Socioeconomic Status (SES), and Race/Ethnicity and Familial Depression of Risk on Psychiatric Disorders.
| Interaction | Psychiatric condition/disorder | |||
|---|---|---|---|---|
| Depressive disorders | Anxiety disorders | Suicidal ideation/behaviors | Any psychiatric disorder/condition | |
| Parent reports | ||||
| Sexa | χ21 = 2.3 | χ21 = 0 | χ21 = 40.8b | χ21 = 14.6b |
| Sex × riskc | χ23 = 3.3 | χ23 = 1.2 | χ23 = 2.3 | χ23 = 4.8 |
| SESa | χ22 = 38.9d | χ22 = 7.8 | χ22 = 3.0 | χ22 = 9.9 |
| SES × riskc | χ26 = 16.4b | χ26 = 16.2b | χ26 = 8.3 | χ26 = 10.7e |
| Race/ethnicitya | χ23 = 13.5f | χ23 = 16.0f | χ23 = 6.1 | χ23 = 2.7 |
| Race/ethnicity × riskc | χ29 = 7.1 | χ29 = 18.8b | χ29 = 10.2 | χ29 = 16.4e |
| Child reports | ||||
| Sexa | χ21 = 0.8 | χ21 = 0.8 | χ21 = 2.9e | χ21 = 2.8e |
| Sex × riskc | χ23 = 6.0 | χ23 = 2.1 | χ23 = 2.1 | χ23 = 0.8 |
| SESa | χ22 = 15.0f | χ22 = 2.2 | χ22 = 0.6 | χ22 = 11.6f |
| SES × riskc | χ26 = 1.9 | χ26 = 4.1 | χ26 = 1.7 | χ26 = 0.4 |
| Race/ethnicitya | χ23 = 33.4d | χ23 = 5.2 | χ23 = 3.1 | χ23 = 15.1f |
| Race/ethnicity × riskc | χ29 = 16.8e | χ29 = 5.4 | χ29 = 5.5 | χ29 = 2.3 |
Main effect associations for moderator variable; 2-tailed tests of significance. All χ2 estimates obtained through generalized estimating equation analyses.
P < .05.
Moderation (interaction) associations between moderator variable and familial depression risk; 2-tailed tests of significance.
P < .001.
P < .10.
P < .01.
Figure 2. Prevalence of Any Psychiatric Disorder in Children by Familial Depression Risk by Sex, Socioeconomic Status (SES), and Race/Ethnicity Reported by Parents and Children.
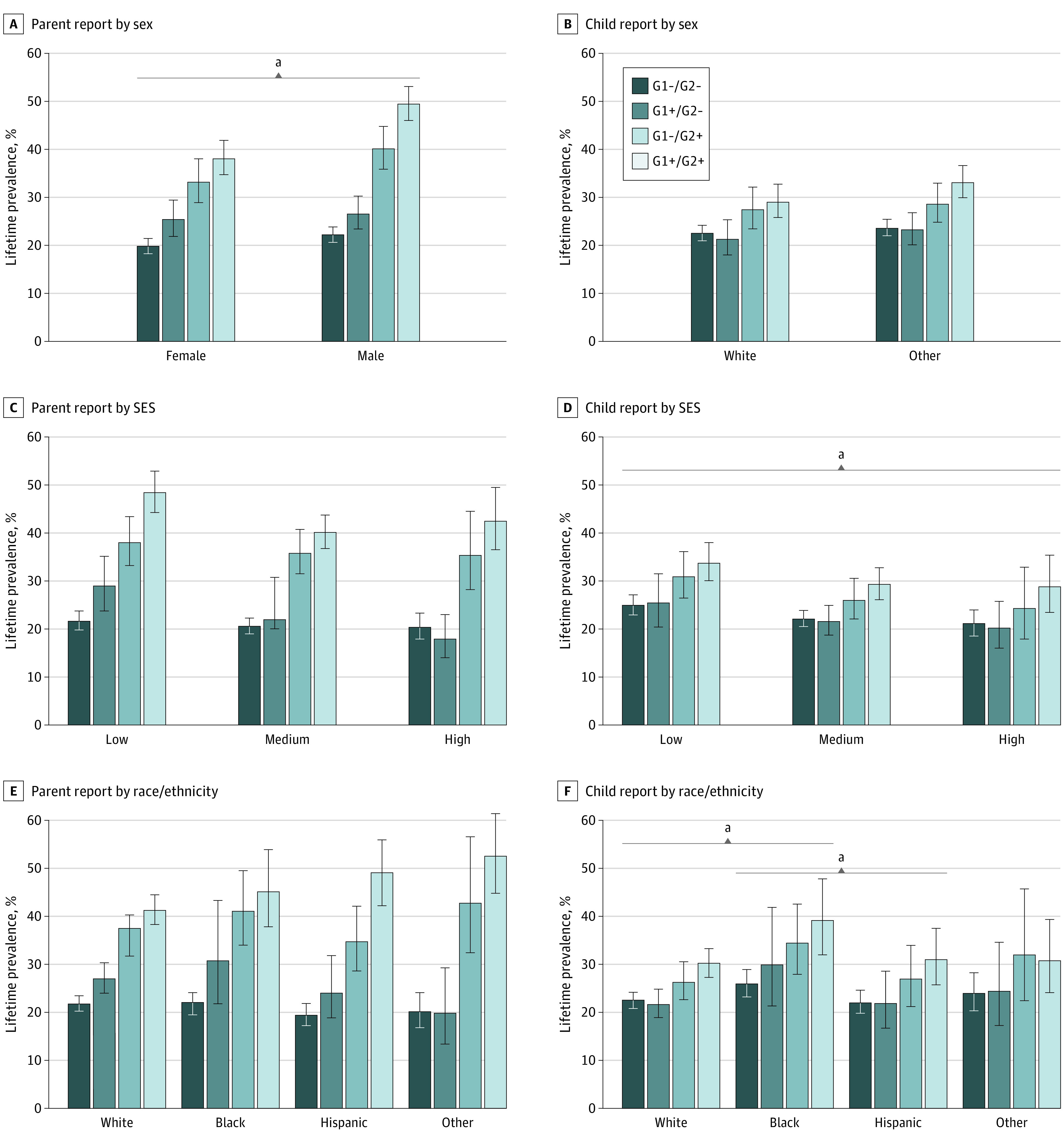
Children were grouped into 4 risk categories, reflecting how many prior generations were affected with depression: (1) neither grandparents (generation 1 [G1]) nor parents (generation 2 [G2]; G1−/G2−), (2) only G1 (G1+/G2−), (3) only G2 (G1−/G2+), and (4) both G1 and G2 (G1+/G2+). A, By parent report, rates of any psychiatric disorder were lower in girls than boys, but both sexes showed increasing prevalence with increasing familial risk. B, By child report, sex did not moderate children’s prevalence rates. C, By parent report, SES did not moderate children’s prevalence rates. D, By child report, children in the low SES category had higher rates of any disorder than those in the medium or high SES categories, but there was no moderating effect of SES by familial risk. E, By parent report, race/ethnicity did not moderate children’s prevalence rates. F, By child report, Black children had higher rates of any disorder than White or Hispanic children, but there was no moderating effect of race/ethnicity by familial risk. The other race/ethnicity group was created because of low individual numbers. Error bars indicate 95% CIs.
aP < .05.
Parent Reports
Rates of any depressive disorder and any anxiety disorder were similar between girls and boys. Boys had higher rates of suicidal behaviors (mean, 11.4%; SE, 0.6) and any disorder (mean, 32.9%; SE, 0.8) than girls (suicidal behavior: mean, 6.3%; SE, 0.5; any disorder: mean, 28.3%; SE, 0.9) (Figure 2A) (eTable 5 in the Supplement). There was no family risk by sex moderation for these diagnoses, indicating that prevalence increased similarly with higher family risk across sex.
Children in the low SES category had higher rates of any depressive disorder (mean, 10.1%; SE, 0.7) compared with those in the medium SES (mean, 5.4%; SE, 0.7) and high SES (mean, 5.7%; SE, 0.4) categories (Figure 2C) (eTable 5 in the Supplement). A significant family risk by SES interaction for depressive disorders (χ26 = 16.4; P = .01) and anxiety disorders (χ26 = 16.2; P = .01) shows that rates in children in the low and medium SES categories increased with family risk, while rates in the high SES category did not (eTable 6 in the Supplement). SES did not moderate associations between family risk and suicidal behaviors or any disorder, indicating that higher family risk corresponded to higher prevalence similarly across SES.
Hispanic children had higher rates of any depressive disorder (mean, 9.1%; SE, 0.9) than White children (mean, 6.5%; SE, 0.4) or children of other races/ethnicities (mean, 5.6%; SE, 0.8) (Figure 2E). White children had higher rates of anxiety disorder (mean, 13.1%; SE, 0.6) compared with Hispanic children (mean, 10.2%; SE, 0.9) and children of other races/ethnicities (mean, 8.7%; SE, 1.1). Race/ethnicity moderated the association between family risk and anxiety disorders (χ29 = 18.8; P = .03). Rates of anxiety increased with increasing family risk for White, Black, and Hispanic children, but White and Hispanic G1+/G2+ children had especially high rates of MDD (eTable 6 in the Supplement). There were no race/ethnicity main or moderation associations with suicidal behaviors or any disorder.
Child Reports
Depressive disorder, anxiety disorder, suicidal behaviors, and any disorder rates reported by the children did not differ by sex (Figure 2B). Prevalence was higher in children in the low SES category compared with those in the medium and high SES categories for depressive disorders (χ22 = 15.0; P = .001) and any disorder (χ22 = 11.6; P = .003) (Figure 2D) (eTable 5 in the Supplement). Depressive disorders were more prevalent in Black children and children of other races/ethnicities, and any disorder was more prevalent in Black children compared with White and Hispanic children (Figure 2F) (eTable 5 in the Supplement). There were no moderation effects of sex, SES, or race/ethnicity, indicating family risk increased rates of disorders similarly across sociodemographic characteristics.
Discussion
We determined whether the association of 2 prior generations of family depression with grandchildren’s psychopathology, established in family studies, could be reliably demonstrated in a larger and representative data set with informant-reported family histories. As hypothesized, we found higher prevalences of psychiatric disorders with increasing family risk in prepubescent children across sociodemographic characteristics. Specifically, children with both a parent and a grandparent with depression had higher rates of psychiatric disorders compared with children with only a parent with depression, who had higher rates compared with children with only a grandparent with depression, who had higher rates than children with no familial history of depression. This pattern was generally observed across sex, SES, and race/ethnicity, although there were some variations within SES and racial/ethnic groups. Our risk patterns are consistent with an additive rather than multiplicative model,37 similar to additive risk effects on children when 1 vs 2 parents are affected by depression or anxiety.38
These results extend our earlier findings19,39 to a representative population of US children. The high-risk study19 also found increased rates of any psychiatric disorders in children with at least 1 grandparent and parent diagnosed with depression compared with just 1 or no prior generations with depression (42 of 71 [59.2%] after first 2 waves with mean age of 12 years39 and 27 of 38 [71%] at a next wave with mean [SD] age of 18.2 [7.3] years19). The rates in the high-risk study are higher than in this study (43.9% as reported by parents), which is likely attributable to participants’ older mean age in the high-risk study.19 The current results suggest that having a grandparent with depression confers lower risk of a psychiatric disorder among children than having a parent with depression, a difference we predict will become more pronounced as the children grow older. The high-risk study19 used a clinician-based KSADS interview and direct family interviews, while the ABCD study used a computerized self-administered KSADS and family history reports. The similarity between the findings from both cohorts show that a bottom-up approach with a family history assessment, with one relative reporting on others, may be a feasible and faster way to study multiple generations than using direct interviews starting with the first generation and waiting for the subsequent generations to age in.
A 2019 study of a register-based Swedish cohort of more than 400 000 mothers and grandmothers also found that grandchildren with 2 previous generations of maternal depression had the highest rates of MDD.20 Other disorders were not reported. Our results extend that study by showing that grandchildren with 2 previous generations affected had highest prevalences for a range of psychiatric diagnoses and across sociodemographic characteristics. Lastly, Pettit and colleagues40 did not assess prevalence rates but found that a parent and grandparent with MDD predicted higher mean Child Behavior Checklist internalizing and anxious depressed scores in children (mean [SD] age, 4.7 [2.5] years) compared with those with only a grandparent or parent with MDD, further establishing a family risk effect.
The mechanisms by which having multiple generations of family with depression increases risk of psychiatric disorders in offspring remain a topic of scientific and clinical interest. MDD is moderately heritable,41 and having multiple generations affected could indicate higher genetic loadings for psychopathology. Additionally, perinatal and postnatal effects,42 parenting styles,43 and higher stress in families with depression44 can have effects through the hypothalamic-pituitary-adrenal axis, epigenetic mechanisms, and inflammatory pathways in offspring.45,46 For example, Hammen and colleagues47 proposed an interpersonal stress model showing an interaction of G1 and G2 depression with parenting and other social factors, which yielded direct and indirect effects on child depression. Furthermore, microstructure in the dentate gyrus of the hippocampus, important for resilience to stress and depression, differed most in offspring with 2 generations compared with 1 and no prior generations of depression.21
Studies such as the ABCD study provide access to large samples of magnetic resonance imaging and other biological data. Our findings suggest that third-generation offspring with 2 prior generations affected by depression may define a clinically more homogenous subgroup for studies of biological mechanisms of psychopathology. The fact that the findings cut across diverse groups makes them even more robust. A parental depression effect on subcortical volume in offspring has already been established,14 and in the future, we aim to study the effects of 2 generations affected on offspring structural and functional neural markers.
Our findings have clinical implications. Screening tools with simple questions on family history could be a valuable addition to pediatric and other clinical care. Familial depression can have a long-term and debilitating clinical course.3,19 Early identification and intervention may break the cycle of transmission or at least the consequences of untreated symptoms.
Limitations
Our study has limitations. First, the ABCD study relies on family history reports from one informant instead of direct interviews with family members. Relying on informant-based histories is common in large data sets but could lead to bias from reporters who themselves have psychopathology. However, our results suggest that this method reasonably approximated results from studies with individual-based assessments, and our sensitivity analyses confirmed that effects were not due to reporter parent depression.
Second, the parent-child discrepancy we observed in KSADS diagnoses is similar to that of other studies comparing parent and child reports.48 However, in contrast to this study, previous studies found that parents underreported their children’s symptoms.29 Our sensitivity analyses did not support overwhelming bias on the part of the parents with depression. Still, this discrepancy warrants tentative interpretation and future replication of the moderation results and further inquiry as to the nature of divergent reports. Depression often manifests in adolescence, and the current sample is relatively young. Rates will likely increase in follow-up ABCD study waves. Nonetheless, seeing high rates at this young age indicates the strength of multiple generations of depression as a risk factor.
Third, we analyzed child-reported and parent-reported diagnoses separately, since the concordance between children and parents was not high. The validating study of the computerized self-report version of the KSADS showed that using algorithms to integrate parent and child report data more closely approximated clinician-derived diagnoses based on interviews with both informants.26 Unfortunately, these integration algorithms are not yet available for the ABCD study. Future refinement of these algorithms could assist with subsequent studies.
Conclusions
These findings validate the reciprocal and complementary nature of big data and family studies in psychiatric epidemiology.22 We demonstrate that the well-established family risk across generations derived from family studies can be mapped on to a larger, diverse study using a time-efficient family history approach and that these effects are generalizable across racial/ethnic groups, sex, and SES categories. The results increase evidence that family history should be interrogated in clinical settings given the often chronic and debilitating outcomes of childhood onset of psychopathology49,50,51,52 and the opportunity for early interventions. The findings also suggest that family history is an important moderator defining a clinically homogenous subgroup at high risk, which may be reliably used to study underlying mechanisms in studies such as the ABCD study that have access to large samples of magnetic resonance imaging and other biological data.
eMethods. Main measures and ABCD study data files.
eTable 1. Demographic and clinical characteristics of study sample with comparisons between included and excluded cases.
eTable 2. Correlation between parent and child reports on KSADS diagnoses.
eTable 3. Relative risks of G3 KSADS diagnoses by familial risk.
eTable 4. Prevalence of psychiatric disorders that were only reported by a parent across levels of familial depression risk.
eTable 5. Main effects of sex, SES, and race/ethnicity as reported by parents and children.
eTable 6. Moderation effects of sex, SES, and race/ethnicity on the influence of familial depression risk on psychiatric outcomes as reported by parents.
eAppendix. Sensitivity analysis and imputed data.
References
- 1.Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta-analysis of family high-risk studies. Schizophr Bull. 2014;40(1):28-38. doi: 10.1093/schbul/sbt114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000;157(10):1552-1562. doi: 10.1176/appi.ajp.157.10.1552 [DOI] [PubMed] [Google Scholar]
- 3.Weissman MM, Wickramaratne P, Gameroff MJ, et al. Offspring of depressed parents: 30 years later. Am J Psychiatry. 2016;173(10):1024-1032. doi: 10.1176/appi.ajp.2016.15101327 [DOI] [PubMed] [Google Scholar]
- 4.Letourneau NL, Tramonte L, Willms JD. Maternal depression, family functioning and children’s longitudinal development. J Pediatr Nurs. 2013;28(3):223-234. doi: 10.1016/j.pedn.2012.07.014 [DOI] [PubMed] [Google Scholar]
- 5.Pearson RM, Evans J, Kounali D, et al. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry. 2013;70(12):1312-1319. doi: 10.1001/jamapsychiatry.2013.2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Batenburg-Eddes T, Brion MJ, Henrichs J, et al. Parental depressive and anxiety symptoms during pregnancy and attention problems in children: a cross-cohort consistency study. J Child Psychol Psychiatry. 2013;54(5):591-600. doi: 10.1111/jcpp.12023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feder A, Alonso A, Tang M, et al. Children of low-income depressed mothers: psychiatric disorders and social adjustment. Depress Anxiety. 2009;26(6):513-520. doi: 10.1002/da.20522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Arch Gen Psychiatry. 2003;60(3):253-258. doi: 10.1001/archpsyc.60.3.253 [DOI] [PubMed] [Google Scholar]
- 9.Katz SJ, Hammen CL, Brennan PA. Maternal depression and the intergenerational transmission of relational impairment. J Fam Psychol. 2013;27(1):86-95. doi: 10.1037/a0031411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peterson BS, Warner V, Bansal R, et al. Cortical thinning in persons at increased familial risk for major depression. Proc Natl Acad Sci U S A. 2009;106(15):6273-6278. doi: 10.1073/pnas.0805311106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hao X, Talati A, Shankman SA, et al. Stability of cortical thinning in persons at increased familial risk for major depressive disorder across 8 years. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2(7):619-625. doi: 10.1016/j.bpsc.2017.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foland-Ross LC, Behzadian N, LeMoult J, Gotlib IH. Concordant patterns of brain structure in mothers with recurrent depression and their never-depressed daughters. Dev Neurosci. 2016;38(2):115-123. doi: 10.1159/000444448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foland-Ross LC, Gilbert BL, Joormann J, Gotlib IH. Neural markers of familial risk for depression: an investigation of cortical thickness abnormalities in healthy adolescent daughters of mothers with recurrent depression. J Abnorm Psychol. 2015;124(3):476-485. doi: 10.1037/abn0000050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pagliaccio D, Alqueza KL, Marsh R, Auerbach RP. Brain volume abnormalities in youth at high risk for depression: Adolescent Brain and Cognitive Development study. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1178-1188. doi: 10.1016/j.jaac.2019.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rao U, Chen L-A, Bidesi AS, Shad MU, Thomas MA, Hammen CL. Hippocampal changes associated with early-life adversity and vulnerability to depression. Biol Psychiatry. 2010;67(4):357-364. doi: 10.1016/j.biopsych.2009.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen MC, Hamilton JP, Gotlib IH. Decreased hippocampal volume in healthy girls at risk of depression. Arch Gen Psychiatry. 2010;67(3):270-276. doi: 10.1001/archgenpsychiatry.2009.202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Posner J, Cha J, Wang Z, et al. Increased default mode network connectivity in individuals at high familial risk for depression. Neuropsychopharmacology. 2016;41(7):1759-1767. doi: 10.1038/npp.2015.342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fischer AS, Camacho MC, Ho TC, Whitfield-Gabrieli S, Gotlib IH. Neural markers of resilience in adolescent females at familial risk for major depressive disorder. JAMA Psychiatry. 2018;75(5):493-502. doi: 10.1001/jamapsychiatry.2017.4516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weissman MM, Berry OO, Warner V, et al. A 30-year study of 3 generations at high risk and low risk for depression. JAMA Psychiatry. 2016;73(9):970-977. doi: 10.1001/jamapsychiatry.2016.1586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Josefsson A, Vikström J, Bladh M, Sydsjö G. Major depressive disorder in women and risk for future generations: population-based three-generation study. BJPsych Open. 2019;5(1):e8-e8. doi: 10.1192/bjo.2018.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Dijk MT, Cha J, Semanek D, et al. Altered dentate gyrus microstructure in individuals at high familial risk for depression predicts future symptoms. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6(1):50-58. doi: 10.1016/j.bpsc.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weissman MM. Big data begin in psychiatry. JAMA Psychiatry. 2020;77(9):967-973. doi: 10.1001/jamapsychiatry.2020.0954 [DOI] [PubMed] [Google Scholar]
- 23.Adolescent Brain Cognitive Development Study. Accessed September 26, 2020. https://abcdstudy.org/
- 24.Garavan H, Bartsch H, Conway K, et al. Recruiting the ABCD sample: design considerations and procedures. Dev Cogn Neurosci. 2018;32:16-22. doi: 10.1016/j.dcn.2018.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980-988. doi: 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- 26.Townsend L, Kobak K, Kearney C, et al. Development of three web-based computerized versions of the Kiddie Schedule for Affective Disorders and Schizophrenia Child Psychiatric Diagnostic Interview: preliminary validity data. J Am Acad Child Adolesc Psychiatry. 2020;59(2):309-325. doi: 10.1016/j.jaac.2019.05.009 [DOI] [PubMed] [Google Scholar]
- 27.Rice JP, Reich T, Bucholz KK, et al. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol Clin Exp Res. 1995;19(4):1018-1023. doi: 10.1111/j.1530-0277.1995.tb00983.x [DOI] [PubMed] [Google Scholar]
- 28.Janca A, Bucholz KK, Janca I, Laster LJ. COGA family history assessment module—FHAM family history screener. Accessed October 6, 2020. https://niaaagenetics.org/coga_instruments/phaseI/fham/Fhamhist4-scr.pdf
- 29.Weissman MM, Wickramaratne P, Warner V, et al. Assessing psychiatric disorders in children. discrepancies between mothers’ and children’s reports. Arch Gen Psychiatry. 1987;44(8):747-753. doi: 10.1001/archpsyc.1987.01800200075011 [DOI] [PubMed] [Google Scholar]
- 30.Janiri D, Doucet GE, Pompili M, et al. Risk and protective factors for childhood suicidality: a US population-based study. Lancet Psychiatry. 2020;7(4):317-326. doi: 10.1016/S2215-0366(20)30049-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hardin JW. Generalized estimating equations (GEE). In: Everitt BS, Howell DC, eds. Encyclopedia of Statistics in Behavioral Science. John Wiley & Sons; 2005. [Google Scholar]
- 32.Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11(3):375-386. doi: 10.2307/3001775 [DOI] [Google Scholar]
- 33.Cochran WG. Some methods for strengthening the common χ2 tests. Biometrics. 1954;10(4):417-451. doi: 10.2307/3001616 [DOI] [Google Scholar]
- 34.Mason T, Margolin G, Dunton G. Convergent and ecological validity of mother and child reports of children’s depressive symptoms: evidence from a diverse sample of mother–child dyads. Psychiatry Int. 2020;1:1-8. doi: 10.3390/psychiatryint1010001 [DOI] [Google Scholar]
- 35.Dong Y, Peng C-YJ. Principled missing data methods for researchers. Springerplus. 2013;2(1):222. doi: 10.1186/2193-1801-2-222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perkins NJ, Cole SR, Harel O, et al. Principled approaches to missing data in epidemiologic studies. Am J Epidemiol. 2018;187(3):568-575. doi: 10.1093/aje/kwx348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiol Methods. 2014;3(1):33-72. doi: 10.1515/em-2013-0005 [DOI] [Google Scholar]
- 38.Meadows SO, McLanahan SS, Brooks-Gunn J. Parental depression and anxiety and early childhood behavior problems across family types. J Marriage Fam. 2007;69(5):1162-1177. doi: 10.1111/j.1741-3737.2007.00439.x [DOI] [Google Scholar]
- 39.Weissman MM, Wickramaratne P, Nomura Y, et al. Families at high and low risk for depression: a 3-generation study. Arch Gen Psychiatry. 2005;62(1):29-36. doi: 10.1001/archpsyc.62.1.29 [DOI] [PubMed] [Google Scholar]
- 40.Pettit JW, Olino TM, Roberts RE, Seeley JR, Lewinsohn PM. Intergenerational transmission of internalizing problems: effects of parental and grandparental major depressive disorder on child behavior. J Clin Child Adolesc Psychol. 2008;37(3):640-650. doi: 10.1080/15374410802148129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kendler KS, Gatz M, Gardner CO, Pedersen NL. A Swedish national twin study of lifetime major depression. Am J Psychiatry. 2006;163(1):109-114. doi: 10.1176/appi.ajp.163.1.109 [DOI] [PubMed] [Google Scholar]
- 42.Sawyer KM, Zunszain PA, Dazzan P, Pariante CM. Intergenerational transmission of depression: clinical observations and molecular mechanisms. Mol Psychiatry. 2019;24(8):1157-1177. doi: 10.1038/s41380-018-0265-4 [DOI] [PubMed] [Google Scholar]
- 43.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20(5):561-592. doi: 10.1016/S0272-7358(98)00100-7 [DOI] [PubMed] [Google Scholar]
- 44.Gershon A, Hayward C, Schraedley-Desmond P, Rudolph KD, Booster GD, Gotlib IH. Life stress and first onset of psychiatric disorders in daughters of depressed mothers. J Psychiatr Res. 2011;45(7):855-862. doi: 10.1016/j.jpsychires.2011.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Curley JP, Champagne FA. Influence of maternal care on the developing brain: mechanisms, temporal dynamics and sensitive periods. Front Neuroendocrinol. 2016;40:52-66. doi: 10.1016/j.yfrne.2015.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brennan PA, Le Brocque R, Hammen C. Maternal depression, parent-child relationships, and resilient outcomes in adolescence. J Am Acad Child Adolesc Psychiatry. 2003;42(12):1469-1477. doi: 10.1097/00004583-200312000-00014 [DOI] [PubMed] [Google Scholar]
- 47.Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. J Consult Clin Psychol. 2004;72(3):511-522. doi: 10.1037/0022-006X.72.3.511 [DOI] [PubMed] [Google Scholar]
- 48.Grills AE, Ollendick TH. Multiple informant agreement and the anxiety disorders interview schedule for parents and children. J Am Acad Child Adolesc Psychiatry. 2003;42(1):30-40. doi: 10.1097/00004583-200301000-00008 [DOI] [PubMed] [Google Scholar]
- 49.Fernando K, Carter JD, Frampton CMA, et al. Childhood-, teenage-, and adult-onset depression: diagnostic and individual characteristics in a clinical sample. Compr Psychiatry. 2011;52(6):623-629. doi: 10.1016/j.comppsych.2010.12.006 [DOI] [PubMed] [Google Scholar]
- 50.Gollan J, Raffety B, Gortner E, Dobson K. Course profiles of early- and adult-onset depression. J Affect Disord. 2005;86(1):81-86. doi: 10.1016/j.jad.2004.12.009 [DOI] [PubMed] [Google Scholar]
- 51.Klein DN, Schatzberg AF, McCullough JP, et al. Early- versus late-onset dythymic disorder: comparison in out-patients with superimposed major depressive episodes. J Affect Disord. 1999;52(1-3):187-196. doi: 10.1016/S0165-0327(98)00079-2 [DOI] [PubMed] [Google Scholar]
- 52.Parker G, Roy K, Hadzi-Pavlovic D, Mitchell P, Wilhelm K. Distinguishing early and late onset non-melancholic unipolar depression. J Affect Disord. 2003;74(2):131-138. doi: 10.1016/S0165-0327(02)00002-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Main measures and ABCD study data files.
eTable 1. Demographic and clinical characteristics of study sample with comparisons between included and excluded cases.
eTable 2. Correlation between parent and child reports on KSADS diagnoses.
eTable 3. Relative risks of G3 KSADS diagnoses by familial risk.
eTable 4. Prevalence of psychiatric disorders that were only reported by a parent across levels of familial depression risk.
eTable 5. Main effects of sex, SES, and race/ethnicity as reported by parents and children.
eTable 6. Moderation effects of sex, SES, and race/ethnicity on the influence of familial depression risk on psychiatric outcomes as reported by parents.
eAppendix. Sensitivity analysis and imputed data.


